Pilot Study on the Influence of Incentive Spirometry on Percutaneous Image-Guided Intra-Abdominal Drainage Catheter Pressure: A Potential Method to Enhance Drainage
Abstract
:1. Introduction
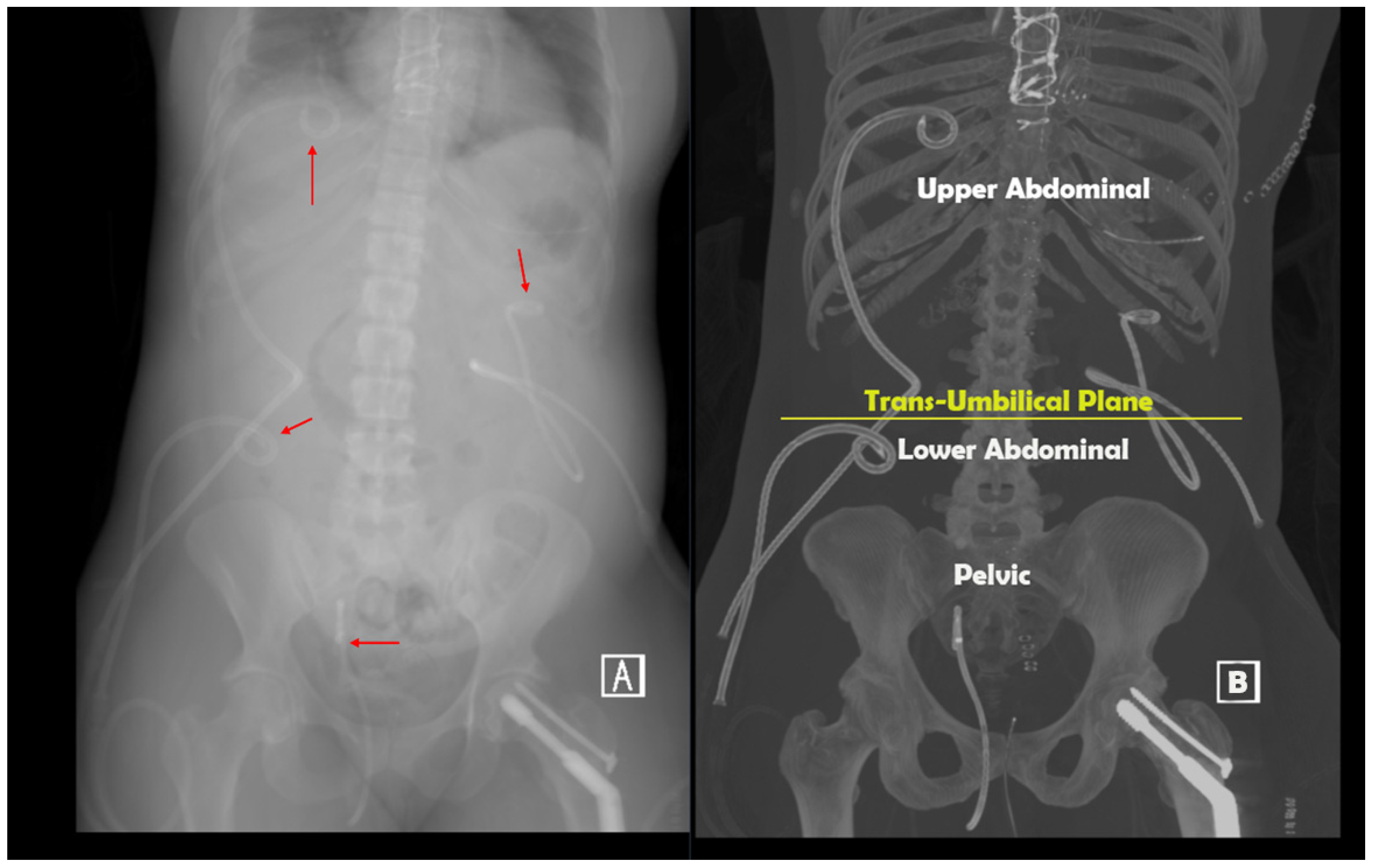
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Baker, T.A.; Aaron, J.M.; Borge, M.; Pierce, K.; Shoup, M.; Aranha, G.V. Role of interventional radiology in the management of complications after pancreaticoduodenectomy. Am. J. Surg. 2008, 195, 386–390. [Google Scholar] [CrossRef]
- Sohn, T.A.; Yeo, C.J.; Cameron, J.L.; Geschwind, J.F.; Mitchell, S.E.; Venbrux, A.C.; Lillemoe, K.D. Pancreaticoduodenectomy: Role of interventional radiologists in managing patients and complications. J. Gastrointest. Surg. 2003, 7, 209–219. [Google Scholar] [CrossRef]
- Ng, S.; Tan, K.; Anil, G. The role of interventional radiology in complications associated with liver transplantation. Clin. Radiol. 2015, 70, 1323–1335. [Google Scholar] [CrossRef]
- Wittich, G.R.; Goodacre, B.W.; Casola, G.; D’Agostino, H.B. Percutaneous abscess drainage: Update. World J. Surg. 2001, 25, 362. [Google Scholar]
- Bassetti, M.; Eckmann, C.; Giacobbe, D.R.; Sartelli, M.; Montravers, P. Post-operative abdominal infections: Epidemiology, operational definitions, and outcomes. Intensive Care Med. 2020, 46, 163–172. [Google Scholar] [CrossRef]
- Zhang, Y.; Stringel, G.; Bezahler, I.; Maddineni, S. Nonoperative management of periappendiceal abscess in children: A comparison of antibiotics alone versus antibiotics plus percutaneous drainage. J. Pediatr. Surg. 2020, 55, 414–417. [Google Scholar] [CrossRef]
- Leanza, V.; Presti, L.; Di Guardo, F.; Leanza, G.; Palumbo, M. CT-guided drainage with percutaneous approach as treatment of E. Faecalis post caesarean section severe abscess: Case report and literature review. G Chir. 2019, 40, 368–372. [Google Scholar] [PubMed]
- Gao, D.; Medina, M.G.; Alameer, E.; Nitz, J.; Tsoraides, S. A case report on delayed diagnosis of perforated Crohn’s disease with recurrent intra-psoas abscess requiring omental patch. Int. J. Surg. Case Rep. 2019, 65, 325–328. [Google Scholar] [CrossRef] [PubMed]
- EÁ, D.C.; Salazar, L.; JI, M. A giant liver abscess due to Fasciola hepatica infection. Rev. Esp. Enferm. Dig. 2019, 111, 815–816. [Google Scholar]
- Shafa, J.; Kee, S.T. Learning Interventional Radiology eBook; Elsevier Health Sciences: Amsterdam, The Netherlands, 2019. [Google Scholar]
- Levin, D.C.; Eschelman, D.; Parker, L.; Rao, V.M. Trends in use of percutaneous versus open surgical drainage of abdominal abscesses. J. Am. Coll. Radiol. 2015, 12, 1247–1250. [Google Scholar] [CrossRef] [PubMed]
- Lorenz, J.; Thomas, J.L. Complications of percutaneous fluid drainage. In Seminars in Interventional Radiology; Thieme Medical Publishers, Inc.: New York, NY, USA, 2006; Volume 23, pp. 194–204. [Google Scholar]
- Brolin, R.; Nosher, J.; Leiman, S.; Lee, W.; Greco, R. Percutaneous catheter versus open surgical drainage in the treatment of abdominal abscesses. Am. Surgeon. 1984, 50, 102–108. [Google Scholar]
- Ballard, D.; Alexander, J.; Weisman, J.; Orchard, M.; Williams, J.; D’Agostino, H. Number and location of drainage catheter side holes: In vitro evaluation. Clin. Radiol. 2015, 70, 974–980. [Google Scholar] [CrossRef]
- Patel, A.; Davis, C.; Davis, T. Percutaneous catheter drainage of secondary abdominal compartment syndrome: A case report. Radiol. Case Rep. 2021, 16, 670–672. [Google Scholar] [CrossRef]
- De Cleva, R.; de Assumpção, M.S.; Sasaya, F.; Chaves, N.Z.; Santo, M.A.; Fló, C.; Lunardi, A.C. Correlation between intra-abdominal pressure and pulmonary volumes after superior and inferior abdominal surgery. Clinics 2014, 69, 483–486. [Google Scholar] [CrossRef]
- Toor, H.; Kashyap, S.; Yau, A.; Simoni, M.; Farr, S.; Savla, P.; Kounang, R.; Miulli, D.E.; Yau, A.C.L. Efficacy of Incentive Spirometer in Increasing Maximum Inspiratory Volume in an Out-Patient Setting. Cureus 2021, 13, e18483. [Google Scholar] [CrossRef]
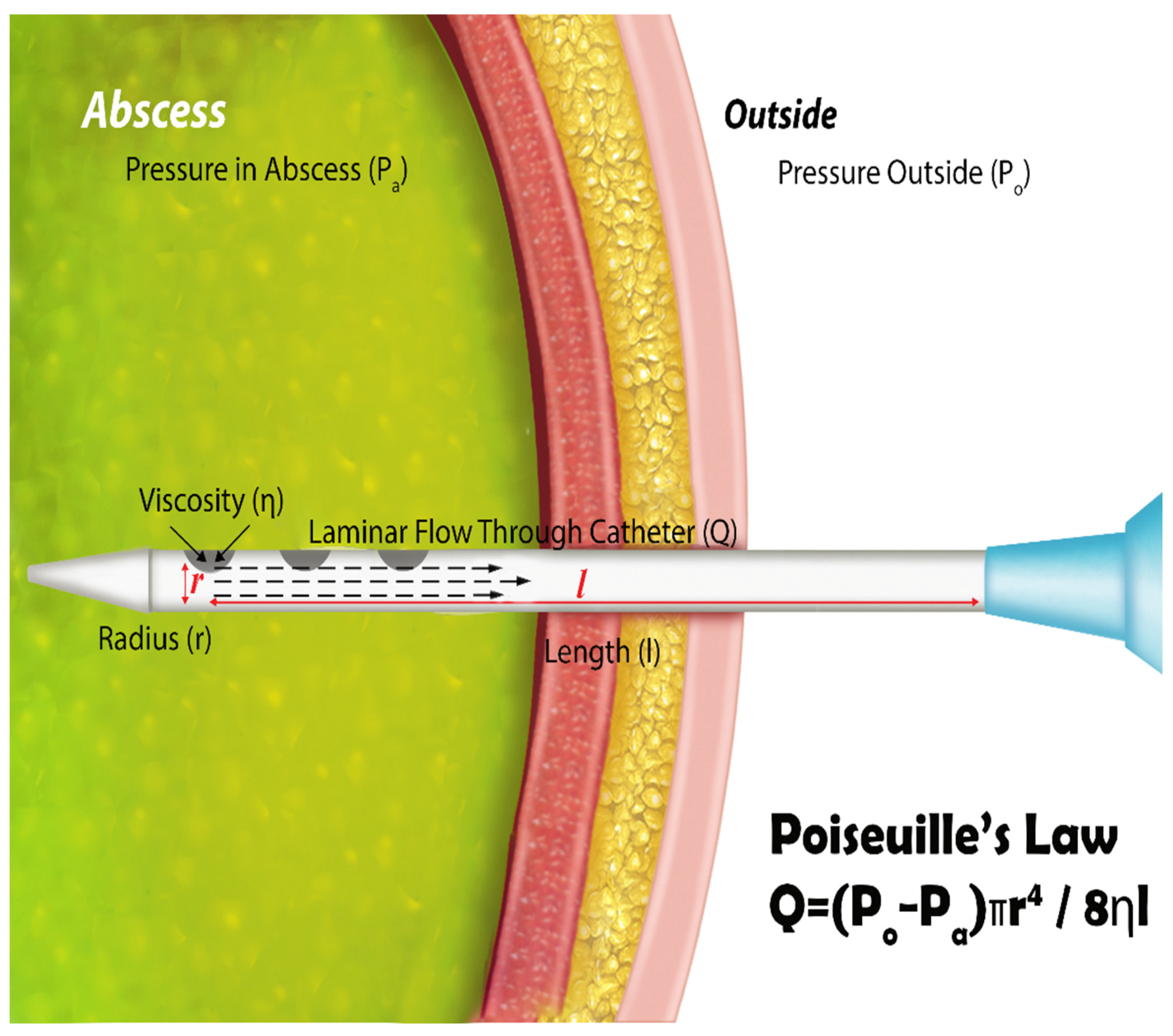
- Park, J.; Kraus, F.; Haaga, J. Fluid flow during percutaneous drainage procedures: An in vitro study of the effects of fluid viscosity, catheter size, and adjunctive urokinase. AJR Am. J. Roentgenol. 1993, 160, 165–169. [Google Scholar] [CrossRef]
- Ferguson, M.K. Preoperative assessment of pulmonary risk. Chest 1999, 115, 58S–63S. [Google Scholar] [CrossRef] [PubMed]
- Chetta, A.; Tzani, P.; Marangio, E.; Carbognani, P.; Bobbio, A.; Olivieri, D. Respiratory effects of surgery and pulmonary function testing in the preoperative evaluation. Acta Biomed. Ateneo Parm. 2006, 77, 69. [Google Scholar]
- Siafakas, N.; Mitrouska, I.; Bouros, D.; Georgopoulos, D. Surgery and the respiratory muscles. Thorax 1999, 54, 458–465. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vassilakopoulos, T.; Mastora, Z.; Katsaounou, P.; Doukas, G.; Klimopoulos, S.; Roussos, C.; Zakynthinos, S. Contribution of pain to inspiratory muscle dysfunction after upper abdominal surgery: A randomized controlled trial. Am. J. Respir. Crit. Care Med. 2000, 161, 1372–1375. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, V.A.; Cornell, J.E.; Smetana, G.W. Strategies to reduce postoperative pulmonary complications after noncardiothoracic surgery: Systematic review for the American College of Physicians. Ann. Intern. Med. 2006, 144, 596–608. [Google Scholar] [CrossRef] [Green Version]
- Pereira, E.D.B.; Fernandes, A.L.G.; Anção, M.d.S.; Peres, C.d.A.; Atallah, Á.N.; Faresin, S.M. Prospective assessment of the risk of postoperative pulmonary complications in patients submitted to upper abdominal surgery. Sao Paulo Med. J. 1999, 117, 151–160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Overend, T.J.; Anderson, C.M.; Lucy, S.D.; Bhatia, C.; Jonsson, B.I.; Timmermans, C. The effect of incentive spirometry on postoperative pulmonary complications: A systematic review. Chest 2001, 120, 971–978. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thomas, J.A.; McIntosh, J.M. Are incentive spirometry, intermittent positive pressure breathing, and deep breathing exercises effective in the prevention of postoperative pulmonary complications after upper abdominal surgery? A systematic overview and meta-analysis. Phys. Ther. 1994, 74, 3–10. [Google Scholar] [CrossRef]
- Hallböök, T.; Lindblad, B.; Lindroth, B.; Wolff, T. Prophylaxis against pulmonary complications in patients undergoing gall-bladder surgery. A comparison between early mobilization, physiotherapy with and without bronchodilatation. Ann. Chir. Gynaecol. 1984, 73, 55–58. [Google Scholar] [PubMed]
- Pontoppidan, H. Mechanical Aids to Lung Expansion in Non-lntubated Surgical Patients. Am. Rev. Respir. Dis. 1980, 122, 109–119. [Google Scholar] [CrossRef]
- Van de Water, J.; Watring, W.; Linton, L.; Murphy, M.; Byron, R. Prevention of postoperative pulmonary complications. Surg. Gynecol. Obstet. 1972, 135, 229–233. [Google Scholar]
- Schuppisser, J.-P.; Brändli, O.; Meili, U. Postoperative intermittent positive pressure breathing versus physiotherapy. Am. J. Surg. 1980, 140, 682–686. [Google Scholar] [CrossRef]
- Kotta, P.A.; Ali, J.M. Incentive Spirometry for Prevention of Postoperative Pulmonary Complications After Thoracic Surgery. Respir. Care 2021, 66, 327–333. [Google Scholar] [CrossRef]
- Takimoto, R.; Kimura, M.; Yokoba, M.; Ichikawa, T.; Matsunaga, A. Relationship between abdominal pressure and diaphragmatic movement in abdominal breathing. Eur. Respir. Soc. 2016, 48, PA1372. [Google Scholar]
- Hodges, P.W.; Gandevia, S.C. Changes in intra-abdominal pressure during postural and respiratory activation of the human diaphragm. J. Appl. Physiol. 2000, 89, 967–976. [Google Scholar] [CrossRef]
- Grillner, S.; Nilsson, J.; Thorstensson, A. Intra-abdominal pressure changes during natural movements in man. Acta Physiol. Scand. 1978, 103, 275–283. [Google Scholar] [CrossRef]
- Cheatham, M.L.; Malbrain, M.L.; Kirkpatrick, A.; Sugrue, M.; Parr, M.; De Waele, J.; Balogh, Z.; Leppäniemi, A.; Olvera, C.; Ivatury, R.; et al. Results from the international conference of experts on intra-abdominal hypertension and abdominal compartment syndrome. II. Recommendations. Intensive Care Med. 2007, 33, 951–962. [Google Scholar] [CrossRef] [PubMed]
- Bailey, J.; Shapiro, M.J. Abdominal compartment syndrome. Crit. Care 2000, 4, 23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coleman, T.J.; Hamad, N.M.; Shaw, J.M.; Egger, M.J.; Hsu, Y.; Hitchcock, R.; Jin, H.; Choi, C.K.; Nygaard, I.E. Effects of walking speeds and carrying techniques on intra-abdominal pressure in women. Int. Urogynecol. J. 2015, 26, 967–974. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hoyt, A.C.; D’Agostino, H.B.; Carrillo, A.J.; Vasconcellos-Viera, M.; Kim, S.; O’Laoide, R. Drainage efficiency of double-lumen sump catheters and single-lumen catheters: An in vitro comparison. J. Vasc. Interv. Radiol. 1997, 8, 267–270. [Google Scholar] [CrossRef] [PubMed]
- Sharma, M.; Madambath, J.G.; Somani, P.; Pathak, A.; Rameshbabu, C.S.; Bansal, R.; Ramasamy, K.; Patil, A. Endoscopic ultrasound of peritoneal spaces. Endosc. Ultrasound. 2017, 6, 90–102. [Google Scholar] [CrossRef] [PubMed] [Green Version]



| Intra-Abdominal Pressure Increases by Region | |||
|---|---|---|---|
| Standardized Pull (1500 cc) | Max Pull (Average 1999 cc) | ||
| Upper Abdomen | Upper Abdomen | ||
| Mean ± STD | 61.6 ± 54.2 | Mean ± STD | 82.5 ± 54.8 |
| Median | 54.4 | Median | 54.4 |
| Min-Max | 18.1–154 | Min-Max | 27.2–154 |
| Lower Abdomen | Lower Abdomen | ||
| Mean ± STD | 42.3 ± 18.9 | Mean ± STD | 39.3 ± 13.8 |
| Median | 36.2 | Median | 36.2 |
| Min-Max | 27.2–63.4 | Min-Max | 27.2–54.4 |
| Pelvis | Pelvis | ||
| Mean ± STD | 48.7 ± 35.9 | Mean ± STD | 54.4 ± 35.3 |
| Median | 40.8 | Median | 43.1 |
| Min-Max | 27.2–136 | Min-Max | 22.7–136 |
| Abscess | Ascites | Biloma | Cyst | Hematoma | |
|---|---|---|---|---|---|
| Mean (SD) | 52.7 ± 36.3 | 40.8 | 95.2 ± 83.3 | 71.4 ± 37.1 | 27.2 |
| Median | 43.1 | NA | 95.2 | 54.4 | NA |
| Min-Max | 22.7–136 | NA | 36.2–154 | 49.8–127 | NA |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ganapathy, A.; Ballard, D.H.; Bishop, G.L.; Hoegger, M.J.; Abraham, N.; D’Agostino, H.B. Pilot Study on the Influence of Incentive Spirometry on Percutaneous Image-Guided Intra-Abdominal Drainage Catheter Pressure: A Potential Method to Enhance Drainage. Appl. Sci. 2023, 13, 7308. https://doi.org/10.3390/app13127308
Ganapathy A, Ballard DH, Bishop GL, Hoegger MJ, Abraham N, D’Agostino HB. Pilot Study on the Influence of Incentive Spirometry on Percutaneous Image-Guided Intra-Abdominal Drainage Catheter Pressure: A Potential Method to Enhance Drainage. Applied Sciences. 2023; 13(12):7308. https://doi.org/10.3390/app13127308
Chicago/Turabian StyleGanapathy, Aravinda, David H. Ballard, Grace L. Bishop, Mark J. Hoegger, Nihil Abraham, and Horacio B. D’Agostino. 2023. "Pilot Study on the Influence of Incentive Spirometry on Percutaneous Image-Guided Intra-Abdominal Drainage Catheter Pressure: A Potential Method to Enhance Drainage" Applied Sciences 13, no. 12: 7308. https://doi.org/10.3390/app13127308
APA StyleGanapathy, A., Ballard, D. H., Bishop, G. L., Hoegger, M. J., Abraham, N., & D’Agostino, H. B. (2023). Pilot Study on the Influence of Incentive Spirometry on Percutaneous Image-Guided Intra-Abdominal Drainage Catheter Pressure: A Potential Method to Enhance Drainage. Applied Sciences, 13(12), 7308. https://doi.org/10.3390/app13127308






