Study of Root Canal Length Estimations by 3D Spatial Reproduction with Stereoscopic Vision
Abstract
:1. Introduction
2. Materials and Methods
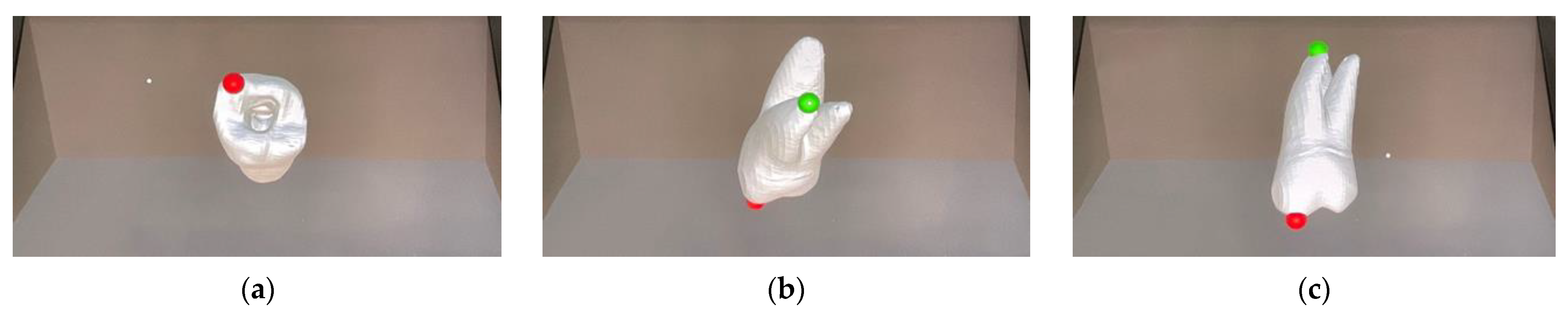
2.1. Construction of Dental Models
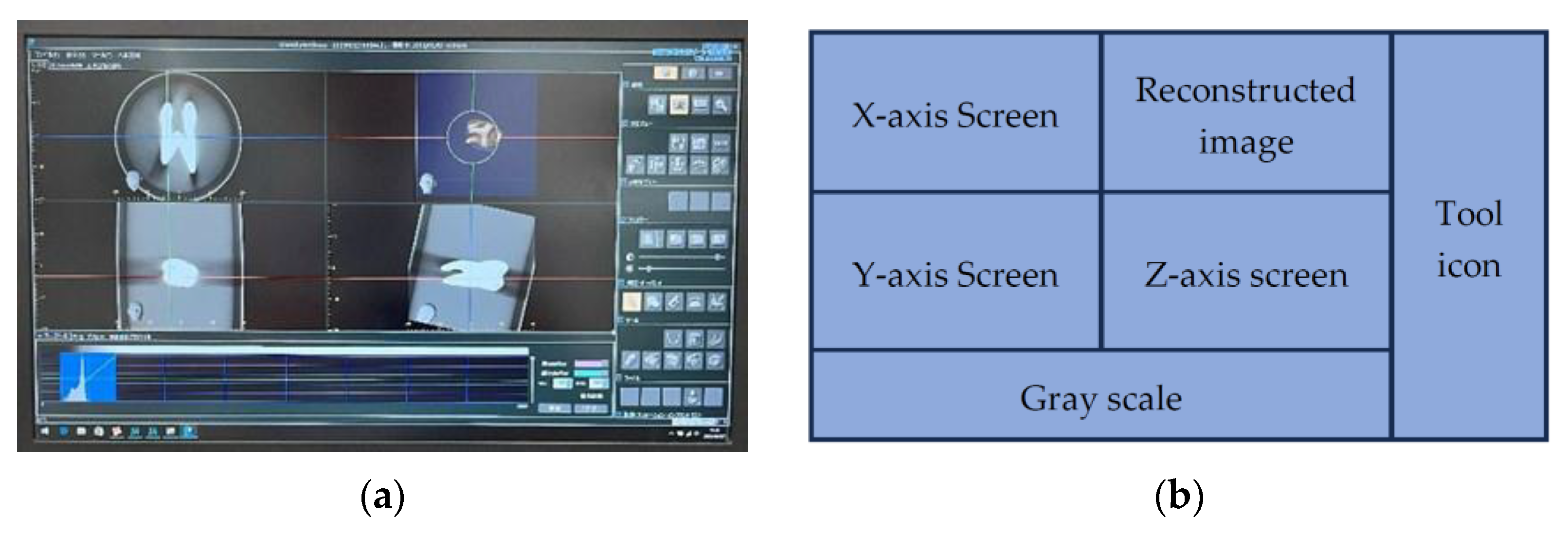
2.2. Construction of a Three-Dimensional Space Reproduction (3DCG) Environment Using SRD
2.3. Software “SR View for Endo”
2.4. Conventional 2D Devices
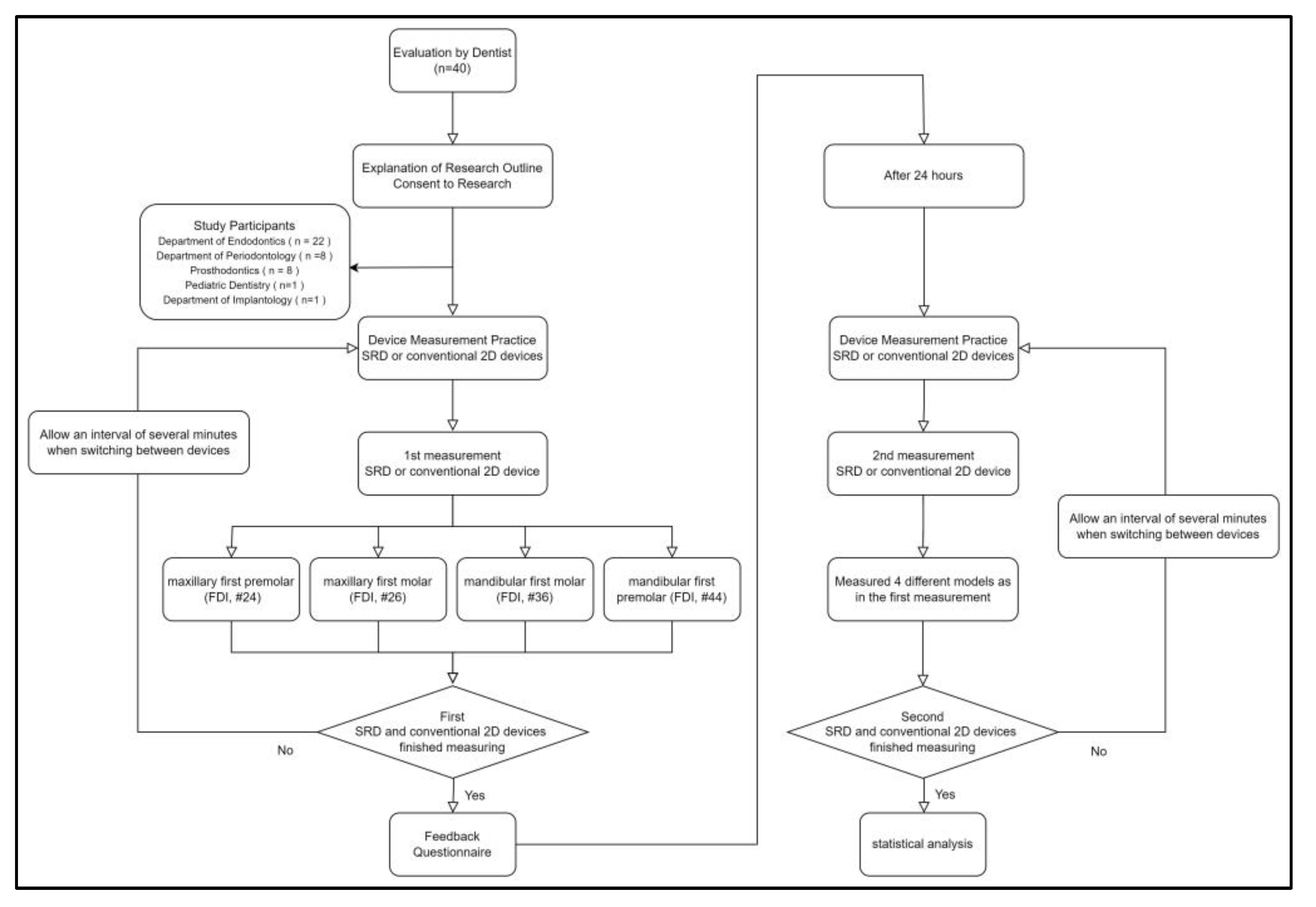
2.5. Evaluation by Dentists
2.6. Statistical Processing
3. Results
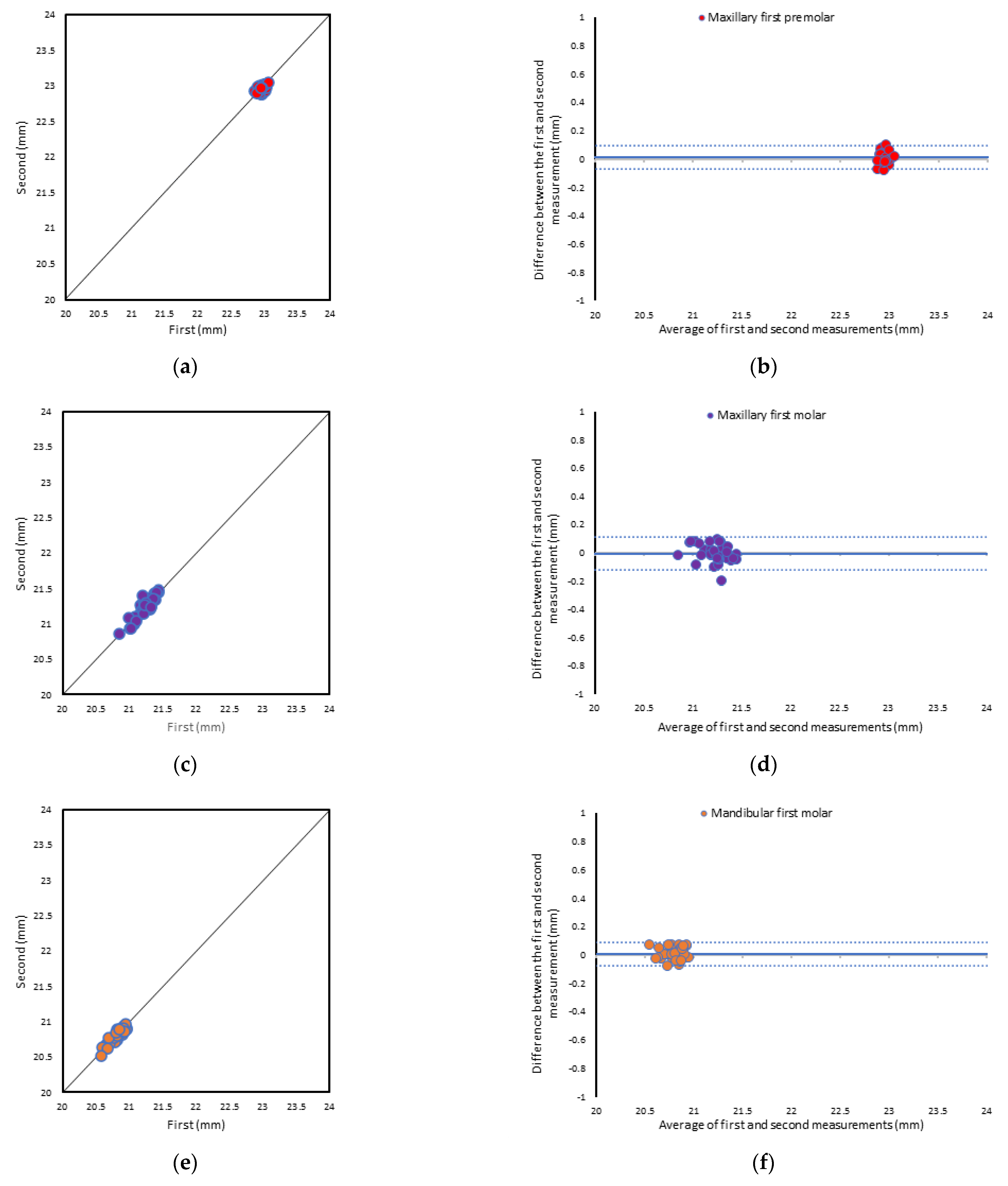
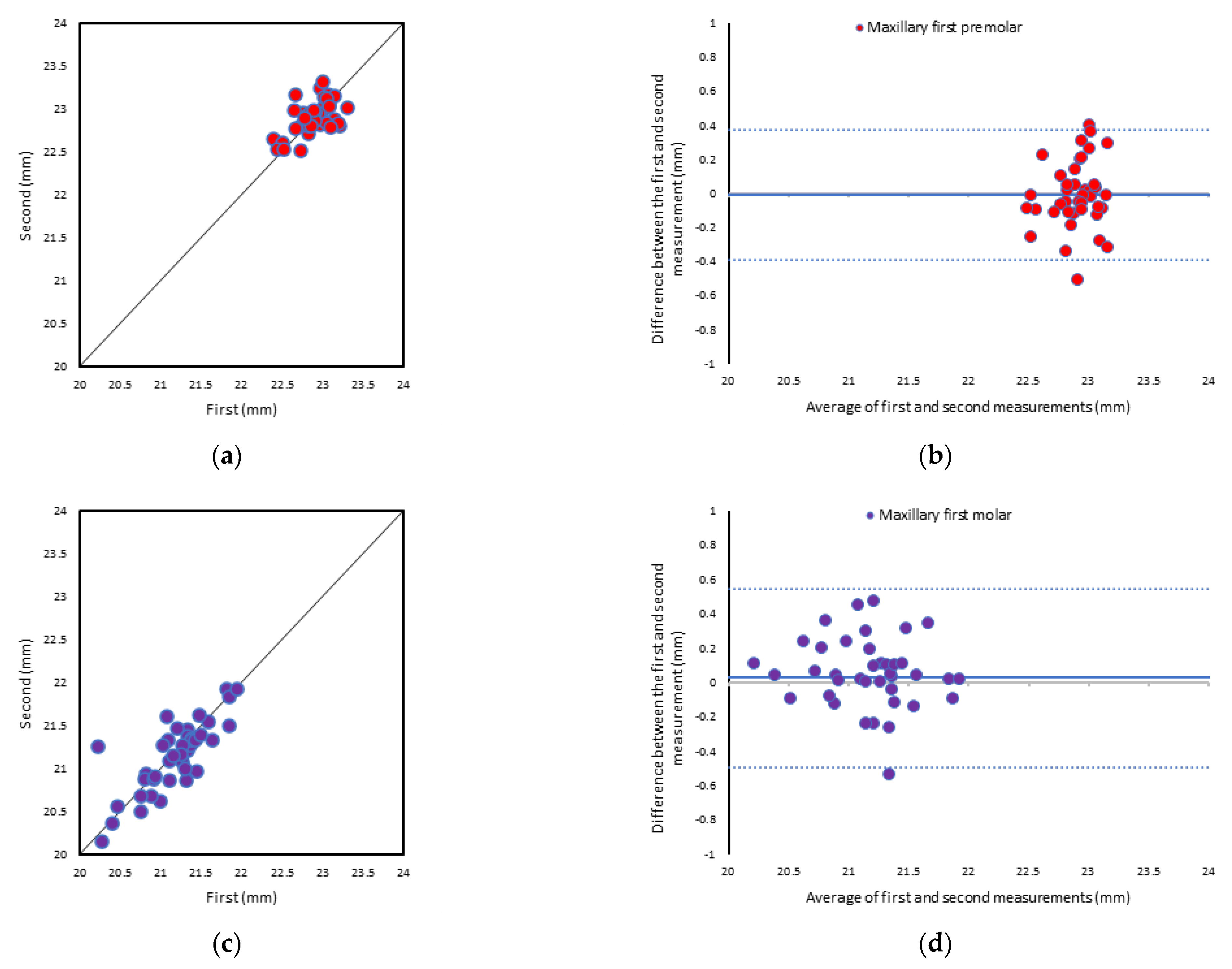
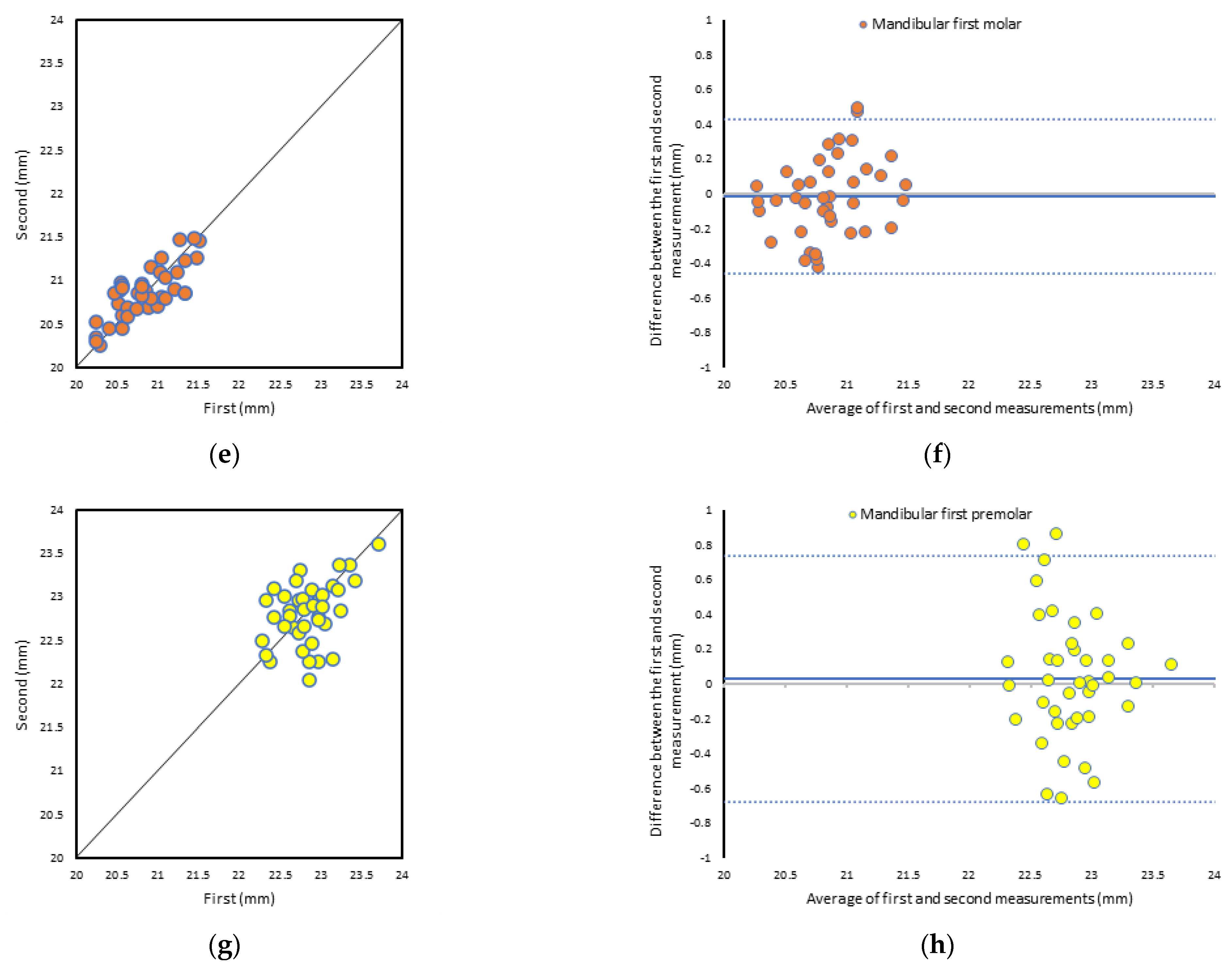
3.1. Consistency among Measurers
3.2. Objective Evaluation
3.3. Subjective Evaluation
3.4. Multivariate Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pottle, J. Virtual reality and the transformation of medical education. Future Health J. 2019, 6, 181–185. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barteit, S.; Lanfermann, L.; Barnighausen, T.; Neuhann, F.; Beiersmann, C. Augmented, Mixed, and Virtual Reality-Based Head-Mounted Devices for Medical Education: Systematic Review. JMIR Serious Games 2021, 9, e29080. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Lu, V.; Khanduja, V. The impact of extended reality on surgery: A scoping review. Int. Orthop. 2023, 47, 611–621. [Google Scholar] [CrossRef]
- Kamphuis, C.; Barsom, E.; Schijven, M.; Christoph, N. Augmented reality in medical education? Perspect. Med. Educ. 2014, 3, 300–311. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, S.; Zhu, J.; Cheng, C.; Pan, Z.; Liu, L.; Du, J.; Shen, X.; Shen, Z.; Zhu, H.; Liu, J.; et al. Can virtual reality improve traditional anatomy education programmes? A mixed-methods study on the use of a 3D skull model. BMC Med. Educ. 2020, 20, 395. [Google Scholar] [CrossRef]
- Gnanasegaram, J.J.; Leung, R.; Beyea, J.A. Evaluating the effectiveness of learning ear anatomy using holographic models. J. Otolaryngol. Head Neck Surg. 2020, 49, 63. [Google Scholar] [CrossRef]
- Zhao, J.; Xu, X.; Jiang, H.; Ding, Y. The effectiveness of virtual reality-based technology on anatomy teaching: A meta-analysis of randomized controlled studies. BMC Med. Educ. 2020, 20, 127. [Google Scholar] [CrossRef]
- Zackoff, M.W.; Real, F.J.; Cruse, B.; Davis, D.; Klein, M. Medical Student Perspectives on the Use of Immersive Virtual Reality for Clinical Assessment Training. Acad. Pediatr. 2019, 19, 849–851. [Google Scholar] [CrossRef]
- Gerup, J.; Soerensen, C.B.; Dieckmann, P. Augmented reality and mixed reality for healthcare education beyond surgery: An integrative review. Int. J. Med. Educ. 2020, 11, 1–18. [Google Scholar] [CrossRef] [Green Version]
- Reymus, M.; Liebermann, A.; Diegritz, C. Virtual reality: An effective tool for teaching root canal anatomy to undergraduate dental students—A preliminary study. Int. Endod. J. 2020, 53, 1581–1587. [Google Scholar] [CrossRef]
- Elbashti, M.E.; Itamiya, T.; Aswehlee, A.M.; Sumita, Y.I.; Ella, B.; Naveau, A. Augmented Reality for Interactive Visualization of 3D Maxillofacial Prosthetic Data. Int. J. Prosthodont. 2020, 33, 680–683. [Google Scholar] [CrossRef]
- Pulijala, Y.; Ma, M.; Pears, M.; Peebles, D.; Ayoub, A. Effectiveness of Immersive Virtual Reality in Surgical Training-A Randomized Control Trial. J. Oral. Maxillofac. Surg. 2018, 76, 1065–1072. [Google Scholar] [CrossRef] [Green Version]
- Mladenovic, R.; Dakovic, D.; Pereira, L.; Matvijenko, V.; Mladenovic, K. Effect of augmented reality simulation on administration of local anaesthesia in paediatric patients. Eur. J. Dent. Educ. 2020, 24, 507–512. [Google Scholar] [CrossRef]
- Mladenovic, R.; Pereira, L.A.P.; Mladenovic, K.; Videnovic, N.; Bukumiric, Z.; Mladenovic, J. Effectiveness of Augmented Reality Mobile Simulator in Teaching Local Anesthesia of Inferior Alveolar Nerve Block. J. Dent. Educ. 2019, 83, 423–428. [Google Scholar] [CrossRef] [Green Version]
- Vincent, M.; Joseph, D.; Amory, C.; Paoli, N.; Ambrosini, P.; Mortier, E.; Tran, N. Contribution of Haptic Simulation to Analogic Training Environment in Restorative Dentistry. J. Dent. Educ. 2020, 84, 367–376. [Google Scholar] [CrossRef]
- Joda, T.; Gallucci, G.O.; Wismeijer, D.; Zitzmann, N.U. Augmented and virtual reality in dental medicine: A systematic review. Comput. Biol. Med. 2019, 108, 93–100. [Google Scholar] [CrossRef]
- Clemente, M.P.; Moreira, A.; Pinto, J.C.; Amarante, J.M.; Mendes, J. The Challenge of Dental Education After COVID-19 Pandemic—Present and Future Innovation Study Design. Inquiry 2021, 58, 469580211018293. [Google Scholar] [CrossRef] [PubMed]
- Condino, S.; Turini, G.; Parchi, P.D.; Viglialoro, R.M.; Piolanti, N.; Gesi, M.; Ferrari, M.; Ferrari, V. How to Build a Patient-Specific Hybrid Simulator for Orthopaedic Open Surgery: Benefits and Limits of Mixed-Reality Using the Microsoft HoloLens. J. Healthc. Eng. 2018, 2018, 5435097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McKnight, R.R.; Pean, C.A.; Buck, J.S.; Hwang, J.S.; Hsu, J.R.; Pierrie, S.N. Virtual Reality and Augmented Reality-Translating Surgical Training into Surgical Technique. Curr. Rev. Musculoskelet. Med. 2020, 13, 663–674. [Google Scholar] [CrossRef]
- Lu, S.; Sanchez Perdomo, Y.P.; Jiang, X.; Zheng, B. Integrating Eye-Tracking to Augmented Reality System for Surgical Training. J. Med. Syst. 2020, 44, 192. [Google Scholar] [CrossRef] [PubMed]
- Itamiya, T.; To, M.; Oguchi, T.; Fuchida, S.; Matsuo, M.; Hasegawa, I.; Kawana, H.; Kimoto, K. A Novel Anatomy Education Method Using a Spatial Reality Display Capable of Stereoscopic Imaging with the Naked Eye. Appl. Sci. 2021, 11, 7323. [Google Scholar] [CrossRef]
- Ariwa, M.; Itamiya, T.; Koizumi, S.; Yamaguchi, T. Comparison of the Observation Errors of Augmented and Spatial Reality Systems. Appl. Sci. 2021, 11, 12076. [Google Scholar] [CrossRef]
- Kobayashi, C. Electronic canal length measurement. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1995, 79, 226–231. [Google Scholar] [CrossRef]
- Nekoofar, M.H.; Ghandi, M.M.; Hayes, S.J.; Dummer, P.M. The fundamental operating principles of electronic root canal length measurement devices. Int. Endod. J. 2006, 39, 595–609. [Google Scholar] [CrossRef] [PubMed]
- Tsesis, I.; Blazer, T.; Ben-Izhack, G.; Taschieri, S.; Del Fabbro, M.; Corbella, S.; Rosen, E. The Precision of Electronic Apex Locators in Working Length Determination: A Systematic Review and Meta-analysis of the Literature. J. Endod. 2015, 41, 1818–1823. [Google Scholar] [CrossRef] [PubMed]
- Martins, J.N.; Marques, D.; Mata, A.; Carames, J. Clinical efficacy of electronic apex locators: Systematic review. J. Endod. 2014, 40, 759–777. [Google Scholar] [CrossRef]
- Unity. Available online: https://unity.com/ja (accessed on 7 July 2023).
- Al Janabi, H.F.; Aydin, A.; Palaneer, S.; Macchione, N.; Al-Jabir, A.; Khan, M.S.; Dasgupta, P.; Ahmed, K. Effectiveness of the HoloLens mixed-reality headset in minimally invasive surgery: A simulation-based feasibility study. Surg. Endosc. 2020, 34, 1143–1149. [Google Scholar] [CrossRef] [Green Version]
- LaViola, J.J. A discussion of cybersickness in virtual environments. ACM SIGCHI Bull. 2000, 32, 47–56. [Google Scholar] [CrossRef]
- Chang, E.; Kim, H.T.; Yoo, B. Virtual Reality Sickness: A Review of Causes and Measurements. Int. J. Hum. Comput. Interact. 2020, 36, 1658–1682. [Google Scholar] [CrossRef]


| Device | Teeth | ICC (95% CI) | p-Values |
|---|---|---|---|
| SRD | #24 | 0.662 (0.365–0.821) | p < 0.001 |
| #26 | 0.952 (0.910–0.975) | p < 0.001 | |
| #36 | 0.952 (0.910–0.975) | p < 0.001 | |
| #44 | 0.894 (0.801–0.944) | p < 0.001 | |
| 2D | #24 | 0.707 (0.448–0.844) | p < 0.001 |
| #26 | 0.885 (0.784–0.939) | p < 0.001 | |
| #36 | 0.871 (0.758–0.932) | p < 0.001 | |
| #44 | 0.606 (0.259–0.791) | p < 0.002 |
| Device | Model | Number of Measurement | Measurements of Root Canal (mm) | Measurement Time (s) | ||||
|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Min | Max | Mean (SD) | Min | Max | |||
| SRD | #24 | 1 | 22.97 (0.04) | 22.85 | 23.06 | 20.31 (8.01) | 6.72 | 43.06 |
| 2 | 22.95(0.04) | 22.88 | 23.04 | 14.82 (3.79) | 6.48 | 23.76 | ||
| #26 | 1 | 21.24 (0.13) | 20.84 | 21.44 | 20.86 (6.90) | 8.65 | 39.19 | |
| 2 | 21.25 (0.15) | 20.86 | 21.48 | 17.40 (5.52) | 8.17 | 31.94 | ||
| #36 | 1 | 20.81 (0.10) | 20.58 | 20.96 | 22.06 (8.10) | 8.17 | 40.98 | |
| 2 | 20.81 (0.10) | 20.51 | 20.96 | 15.79 (5.09) | 6.14 | 26.73 | ||
| #44 | 1 | 22.86 (0.13) | 22.57 | 23.08 | 19.32 (5.85) | 8.96 | 28.73 | |
| 2 | 22.85 (0.14) | 22.50 | 23.02 | 14.38 (4.00) | 6.89 | 22.64 | ||
| 2D device | #24 | 1 | 22.90 (0.21) | 22.39 | 23.30 | 48.15 (15.68) | 23.39 | 79.69 |
| 2 | 22.91 (0.19) | 22.51 | 23.32 | 44.48 (13.71) | 22.55 | 74.23 | ||
| #26 | 1 | 21.18 (0.41) | 20.23 | 21.94 | 54.69 (20.12) | 21.73 | 105.84 | |
| 2 | 21.15 (0.40) | 20.16 | 21.92 | 51.73 (19.03) | 22.21 | 101.06 | ||
| #36 | 1 | 20.84 (0.36) | 20.24 | 21.51 | 56.43 (20.06) | 25.45 | 107.86 | |
| 2 | 20.86 (0.30) | 20.25 | 21.48 | 51.46 (18.71) | 23.34 | 95.50 | ||
| #44 | 1 | 22.85 (0.32) | 22.28 | 23.71 | 51.84 (15.68) | 23.98 | 83.57 | |
| 2 | 22.82 (0.35) | 22.05 | 23.60 | 48.66 (16.63) | 25.12 | 90.27 | ||
| Mean (SD) | Min | Max | |
|---|---|---|---|
| Three-dimensionality | 9.4 (±0.9) | 7 | 10 |
| Image lag | 9.3 (±1.1) | 5 | 10 |
| Operability | 8.9 (±1.3) | 5 | 10 |
| Articulation | 8.7 (±1.3) | 5 | 10 |
| Screen sickness | 7.9 (±1.9) | 4 | 10 |
| Image quality | 8.1 (±2.2) | 4 | 10 |
| Eye fatigue | 7.4 (±2.1) | 3 | 10 |
| I feel the SRD will have a role within education | 9.3 (±1.2) | 6 | 10 |
| I feel the SRD will have a role within practice | 9.3 (±0.9) | 6 | 10 |
| Rating (1 = strongly disagree, 10 = strongly agree) |
| r | p | |
|---|---|---|
| Age group 1 | 0.276 | 0.084 |
| Gender 2 | −0.022 | 0.894 |
| Frequency of 2D device use 3 | −0.358 | 0.023 |
| Eye fatigue (Riccardo scale) 4 | −0.088 | 0.587 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsukuda, T.; Mutoh, N.; Nakano, A.; Itamiya, T.; Tani-Ishii, N. Study of Root Canal Length Estimations by 3D Spatial Reproduction with Stereoscopic Vision. Appl. Sci. 2023, 13, 8651. https://doi.org/10.3390/app13158651
Tsukuda T, Mutoh N, Nakano A, Itamiya T, Tani-Ishii N. Study of Root Canal Length Estimations by 3D Spatial Reproduction with Stereoscopic Vision. Applied Sciences. 2023; 13(15):8651. https://doi.org/10.3390/app13158651
Chicago/Turabian StyleTsukuda, Takato, Noriko Mutoh, Akito Nakano, Tomoki Itamiya, and Nobuyuki Tani-Ishii. 2023. "Study of Root Canal Length Estimations by 3D Spatial Reproduction with Stereoscopic Vision" Applied Sciences 13, no. 15: 8651. https://doi.org/10.3390/app13158651
APA StyleTsukuda, T., Mutoh, N., Nakano, A., Itamiya, T., & Tani-Ishii, N. (2023). Study of Root Canal Length Estimations by 3D Spatial Reproduction with Stereoscopic Vision. Applied Sciences, 13(15), 8651. https://doi.org/10.3390/app13158651






