Surgical Wound Repair with Innovative Hemostatic Glue: Clinical Case Report
Abstract
1. Introduction
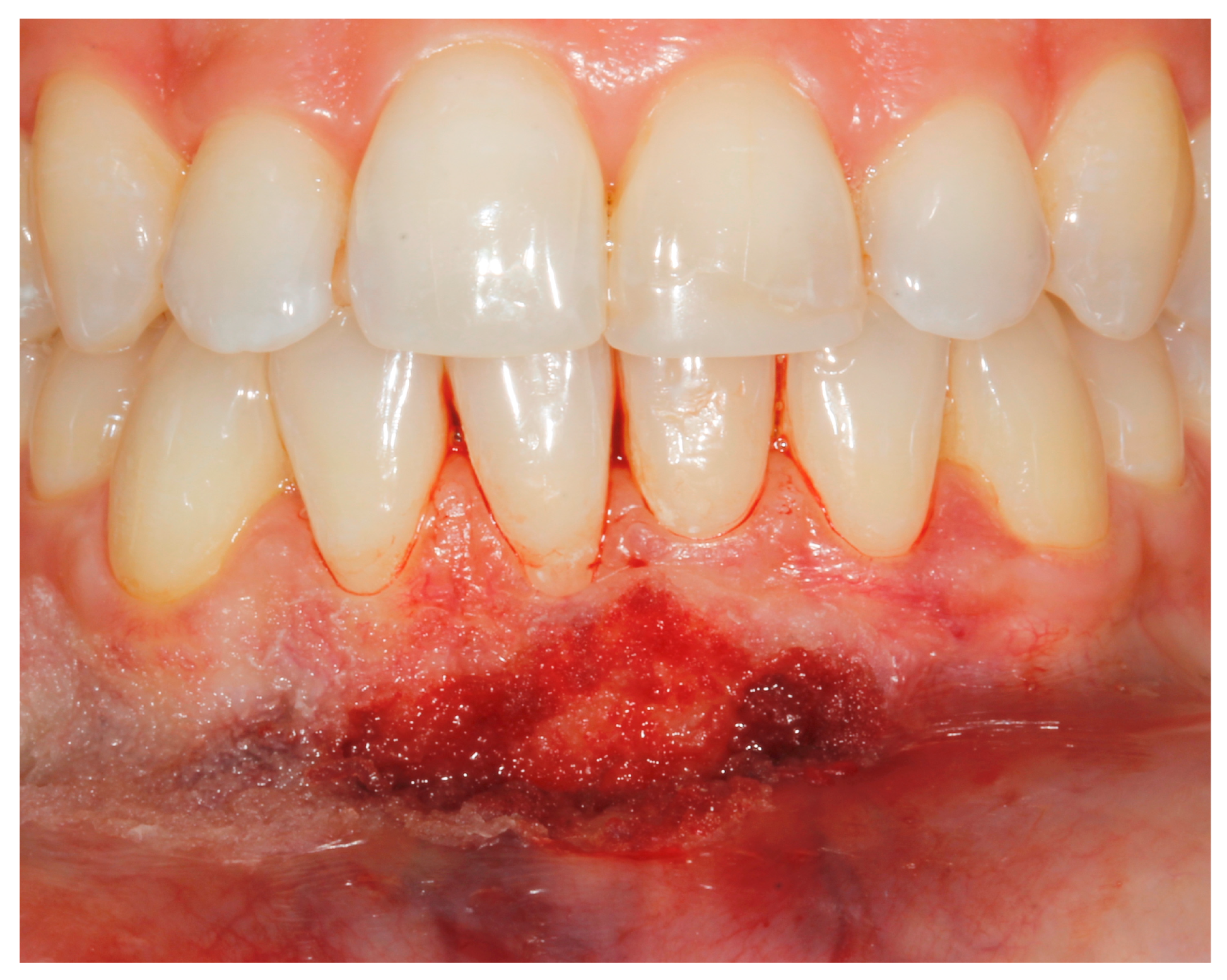
2. Case Study
- (a)
- deep partial thickness incision (blade parallel to the periosteum) made at the level of the external insertion of the frenulum;
- (b)
- elimination of superficial mucous tissue and muscle of the frenulum;
- (c)
- a series of detached points with periosteal anchorage for the apical positioning of the lining mucosa of the lip and the second intention healing of the exposed periosteum.
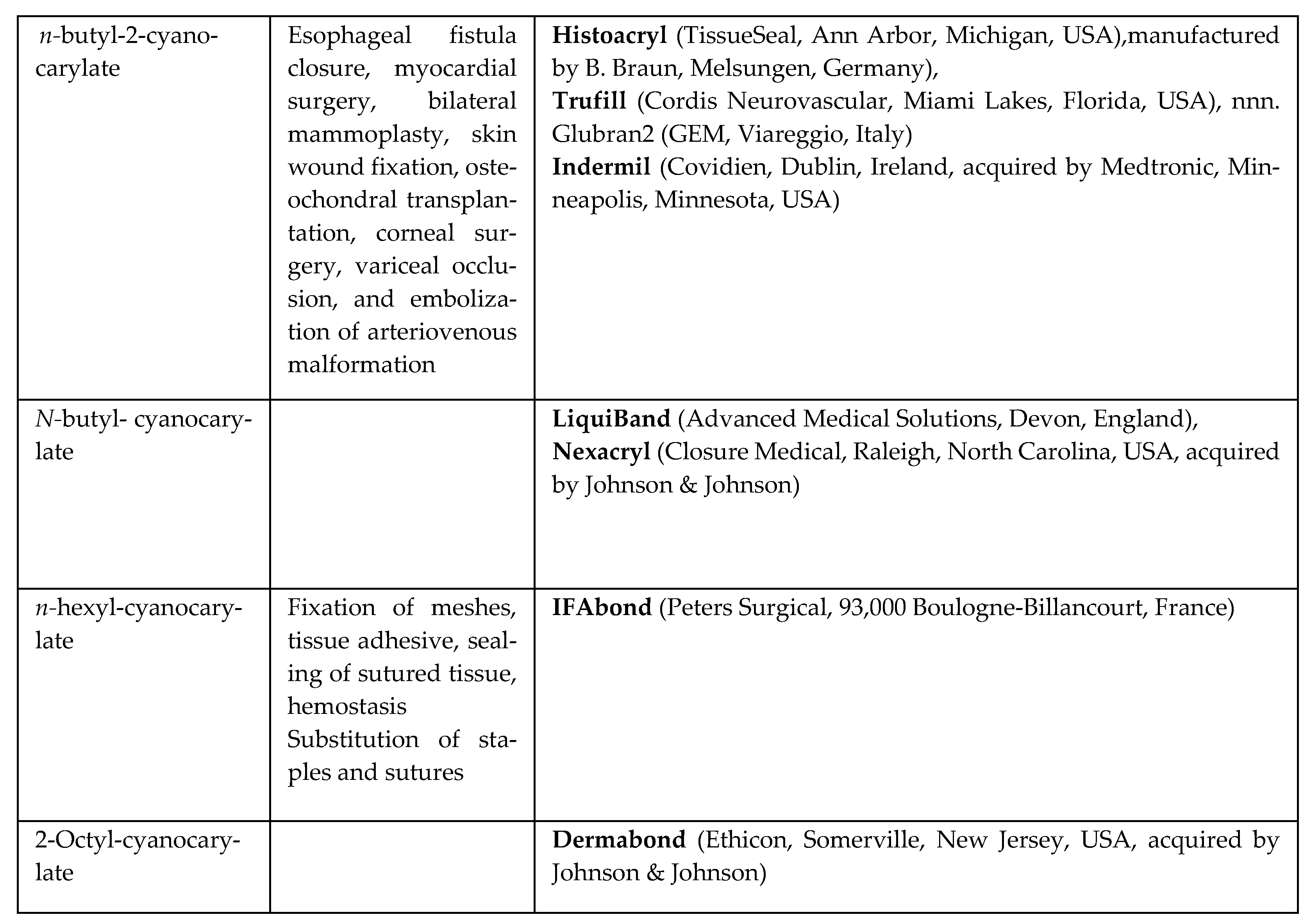
3. Discussion
- mucous attachment frenulum when the frenulum inserts into the mucosa.
- frenulum with gingival attachment when it is inserted into adherent gingiva.
- the papillary-attached frenulum when inserted into the papilla.
- frenulum with penetrating papillary attachment when the frenulum fibers pass through the interincisive papilla and insert into the adherent palatine or lingual gingiva.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gartner, L.P.; Schein, D. The superior labial frenum: A histologic observation. Quintessence Int. 1991, 22, 443–445. [Google Scholar] [PubMed]
- Özener, H.; Meseli, S.E.; Sezgin, G.; Kuru, L. Clinical Efficacy of Conventional and Diode Laser-Assisted Frenectomy in Patients with Different Abnormal Frenulum Insertions: A Retrospective Study. Photobiomodulation Photomed. Laser Surg. 2020, 38, 565–570. [Google Scholar] [CrossRef] [PubMed]
- Delli, K.; Livas, C.; Sculean, A.; Katsaros, C.; Bornstein, M. Facts and myths regarding the maxillary midline frenum and its treatment: A systematic review of the literature. Quintessence Int. 2013, 44, 177–187. [Google Scholar] [CrossRef] [PubMed]
- Dioguardi, M.; Ballini, A.; Quarta, C.; Caroprese, M.; Maci, M.; Spirito, F.; Caloro, G.A.; Alovisi, M.; Basile, E.; Muzio, L.L. Labial Frenectomy using Laser: A Scoping Review. Int. J. Dent. 2023, 2023, 7321735. [Google Scholar] [CrossRef]
- Biradar, S.M.; Patil, A.Y.; Kotnoor, S.S.; Bacha, S.; Bijjaragi, S.C.; Kattimani, P.T. Assessment of Diverse Frenal Morphology in Primary, Mixed, and Permanent Dentition: A Prevalence Study. J. Contemp. Dent. Pract. 2020, 21, 562–567. [Google Scholar] [CrossRef]
- Mintz, S.; Siegel, M.; Seider, P. An overview of oral frena and their association with multiple syndromic and non- syndromic conditions. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2005, 99, 321–324. [Google Scholar] [CrossRef]
- Harris, R.J. Creeping Attachment Associated With the Connective Tissue With Partial-Thickness Double Pedicle Graft. J. Periodontol. 1997, 68, 890–899. [Google Scholar] [CrossRef]
- Devishree; Gujjari, S.; Gujjari, S.K.; Shubhashini, P.V. Frenectomy: A review with the reports of surgical techniques. J. Clin. Diagn. Res. 2012, 6, 1587–1592. [Google Scholar]
- Silverstein, L.H.; Kurtzman, G.M.; Shatz, P.C. Suturing for Optimal Soft-Tissue Management. J. Oral Implantol. 2009, 35, 82–90. [Google Scholar] [CrossRef]
- Borie, E.; Rosas, E.; Kuramochi, G.; Etcheberry, S.; Olate, S.; Weber, B. Oral Applications of Cyanoacrylate Adhesives: A Literature Review. BioMed Res. Int. 2019, 2019, 8217602. [Google Scholar] [CrossRef]
- Zheng, K.; Gu, Q.; Zhou, D.; Zhou, M.; Zhang, L. Recent progress in surgical adhesives for biomedical applications. Smart Mater. Med. 2021, 3, 41–65. [Google Scholar] [CrossRef]
- Shupak, R.P.; Blackmore, S.; Kim, R.Y. Skin hypersensitivity following application of tissue adhesive (2-octyl cyanoacrylate). Bayl. Univ. Med. Cent. Proc. 2021, 34, 736–738. [Google Scholar] [CrossRef]
- Yusuf, I.H.; Patel, C.K. A sticky sight: Cyanoacrylate ‘superglue’ injuries of the eye. BMJ Case Rep. 2010, 2010, bcr1120092435. [Google Scholar] [CrossRef] [PubMed]
- Oladega, A.A.; James, O.; Adeyemo, W.L. Cyanoacrylate tissue adhesive or silk suture for closure of surgical wound following removal of an impacted mandibular third molar: A randomized controlled study. J. Cranio-Maxillofac. Surg. 2018, 47, 93–98. [Google Scholar] [CrossRef]
- Maia, G.V.; Sousa, C.W.; de Lima, J.C.R.; Vecchio, J.L.; Silva, P.G.d.B.; Carvalho, A.C.G.d.S. Cyanoacrylate glue in socket repair: A comparative study. Br. J. Oral Maxillofac. Surg. 2021, 60, 145–151. [Google Scholar] [CrossRef] [PubMed]
- Vastani, A.; Maria, A. Healing of Intraoral Wounds Closed Using Silk Sutures and Isoamyl 2-Cyanoacrylate Glue: A Comparative Clinical and Histologic Study. J. Oral Maxillofac. Surg. 2013, 71, 241–248. [Google Scholar] [CrossRef]
- Gümüş, P.; Buduneli, E. Graft stabilization with cyanoacrylate decreases shrinkage of free gingival grafts. Aust. Dent. J. 2014, 59, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Ghoreishian, M.; Gheisari, R.; Fayazi, M. Tissue adhesive and suturing for closure of the surgical wound after removal of impacted mandibular third molars: A comparative study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2009, 108, e14–e16. [Google Scholar] [CrossRef]
- Kramer, P.F.; de Amorim, L.M.; Alves, N.d.M.; Ruschel, H.C.; Bervian, J.; Feldens, C.A. Maxillary Labial Frenum in Preschool Children: Variations, Anomalies and Associated Factors. J. Clin. Pediatr. Dent. 2022, 46, 51–57. [Google Scholar] [CrossRef]
- Tadros, S.; Ben-Dov, T.; Catháin, É.Ó.; Anglin, C.; April, M.M. Association between superior labial frenum and maxillary midline diastema—A systematic review. Int. J. Pediatr. Otorhinolaryngol. 2022, 156, 111063. [Google Scholar] [CrossRef]
- Wheeler, B.; Carrico, C.K.; Shroff, B.; Brickhouse, T.; Laskin, D.M. Management of the Maxillary Diastema by Various Dental Specialties. J. Oral Maxillofac. Surg. 2018, 76, 709–715. [Google Scholar] [CrossRef] [PubMed]
- Ranjbaran, M.A.; Aslani, F.; Jafari-Naeimi, A.; Rakhshan, V. Associations among the occurrence or types of maxillary canine impaction, labial frenum attachment types, lateral incisor anomalies, and midline diastema in patients with and without impaction: A case-control study. Int. Orthod. 2023, 21, 100743. [Google Scholar] [CrossRef] [PubMed]
- Ahn, J.H.; Newton, T.; Campbell, C. Labial frenectomy: Current clinical practice of orthodontists in the United Kingdom. Angle Orthod. 2022, 92, 780–786. [Google Scholar] [CrossRef] [PubMed]
- Sinha, J.; Kumar, V.; Tripathi, A.K.; Saimbi, C.S. Untangle lip through Z-plasty. BMJ Case Rep. 2014, 2014, bcr2014206258. [Google Scholar] [CrossRef]
- Chaubey, K.; Thakur, R.; Arora, V.; Narula, I. Perio-esthetic surgery: Using LPF with frenectomy for prevention of scar. J. Indian Soc. Periodontol. 2011, 15, 265–269. [Google Scholar] [CrossRef] [PubMed]
- Miller, P.D. The Frenectomy Combined with a Laterally Positioned Pedicle Graft: Functional and Esthetic Considerations. J. Periodontol. 1985, 56, 102–106. [Google Scholar] [CrossRef]
- Hema, D.; Prasanna, J.S. Radiosurgery in periodontics: Have we forgotten it? J. Indian Soc. Periodontol. 2021, 25, 6–10. [Google Scholar] [CrossRef]
- Gontijo, I.; Navarro, R.S.; Haypek, P.; Ciamponi, A.L.; Haddad, A.E. The applications of diode and Er:YAG lasers in labial frenectomy in infant patients. J. Dent. Child. 2005, 72, 10–15. [Google Scholar]
- Kulkarni, S.; Dodwad, V.; Chava, V. Healing of periodontal flaps when closed with silk sutures and N-butyl cyanoacrylate: A clinical and histological study. Indian J. Dent. Res. 2007, 18, 72. [Google Scholar]
- Giray, C.B.; Sungur, A.; Atasever, A.; Araz, K. Comparison of silk sutures and n-butyl-2-cyanoacrylate on the healing of skin wounds. A pilot study. Aust. Dent. J. 1995, 40, 43–45. [Google Scholar] [CrossRef]
- Raj, M.; Raj, G.; Sheng, T.K.; Jsp, L. Use of cyanoacrylate tissue adhesives for wound closure in the head and neck region: A systematic review. J. Plast. Reconstr. Aesthetic Surg. 2021, 75, 183–198. [Google Scholar] [CrossRef]
- Nitsch, A.; Pabyk, A.; Honig, J.F.; Verheggen, R.; Merten, H.-A. Cellular, Histomorphologic, and Clinical Characteristics of a New Octyl-2-Cyanoacrylate Skin Adhesive. Aesthetic Plast. Surg. 2005, 29, 53–58. [Google Scholar] [CrossRef]
- Alhourani, M.A.; Kasem, T.; Hamadah, O. Comparative study between using a tissue adhesive (N-BCA & OCA) and surgical sutures in free gingival graft surgery: A randomized controlled clinical trial. Dent. Med. Probl. 2022, 59, 241–248. [Google Scholar] [CrossRef]
- Montanaro, L.; Arciola, C.; Cenni, E.; Ciapetti, G.; Savioli, F.; Filippini, F.; Barsanti, L. Cytotoxicity, blood compatibility and antimicrobial activity of two cyanoacrylate glues for surgical use. Biomaterials 2000, 22, 59–66. [Google Scholar] [CrossRef]
- Verma, D.; Ahluwalia, T. Cyanoacrylate tissue adhesives in oral and maxillofacial surgery. J. Indian Dent. Assoc. 2002, 73, 171–174. [Google Scholar]
- Bellón, J.M.; Fernández-Gutiérrez, M.; Rodríguez, M.; Pérez-López, P.; Pérez-Köhler, B.; Kühnhardt, A.; Pascual, G.; Román, J.S. Behavior of a new long-chain cyanoacrylate tissue adhesive used for mesh fixation in hernia repair. J. Surg. Res. 2016, 208, 68–83. [Google Scholar] [CrossRef]
- Bellón, J.M.; Fernández-Gutiérrez, M.; Rodríguez, M.; Sotomayor, S.; Pérez-Köhler, B.; Kuhnhardt, A.; Pascual, G.; Román, J.S. Bioassay of cyanoacrylate tissue adhesives used for intraperitoneal mesh fixation. J. Biomed. Mater. Res. Part B Appl. Biomater. 2015, 105, 312–319. [Google Scholar] [CrossRef]
- Pascual, G.; Rodríguez, M.; Pérez-Köhler, B.; Mesa-Ciller, C.; Fernández-Gutiérrez, M.; Román, J.S.; Bellón, J.M. Host tissue response by the expression of collagen to cyanoacrylate adhesives used in implant fixation for abdominal hernia repair. J. Mater. Sci. Mater. Med. 2017, 28, 58. [Google Scholar] [CrossRef] [PubMed]
- Pascual, G.; Rodríguez, M.; Mesa-Ciller, C.; Pérez-Köhler, B.; Fernández-Gutiérrez, M.; Román, J.S.; Bellón, J.M. Sutures versus new cyanoacrylates in prosthetic abdominal wall repair: A preclinical long-term study. J. Surg. Res. 2017, 220, 30–39. [Google Scholar] [CrossRef]
- Estrade, J.-P.; Gurriet, B.; Franquebalme, J.-P.; Chinchole, J.-M.; Glowaczower, E.; Ferry, C.; Crochet, P.; Agostini, A. Laparoscopic sacrocolpopexy with a vaginal prosthetic adhesive. Gynecol. Obstet. Fertil. 2015, 43, 419–423. [Google Scholar] [CrossRef]
- Giudice, A.F.S.-L.; Ortiz, A.M.; Sánchez-Labrador, L.; Brinkmann, J.C.-B.; Cobo-Vázquez, C.M.; Meniz-García, C. Current status of split-mouth controlled clinical trials comparing cyanoacrylate vs. conventional suture after lower third molar surgeries: A systematic literature review. Acta Odontol. Scand. 2022, 81, 349–357. [Google Scholar] [CrossRef]







Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alovisi, M.; Erovigni, F.; Bianchi, L.; Longhi, B.; Scotti, N.; Pasqualini, D.; Berutti, E. Surgical Wound Repair with Innovative Hemostatic Glue: Clinical Case Report. Appl. Sci. 2023, 13, 8979. https://doi.org/10.3390/app13158979
Alovisi M, Erovigni F, Bianchi L, Longhi B, Scotti N, Pasqualini D, Berutti E. Surgical Wound Repair with Innovative Hemostatic Glue: Clinical Case Report. Applied Sciences. 2023; 13(15):8979. https://doi.org/10.3390/app13158979
Chicago/Turabian StyleAlovisi, Mario, Francesco Erovigni, Lorenzo Bianchi, Beatrice Longhi, Nicola Scotti, Damiano Pasqualini, and Elio Berutti. 2023. "Surgical Wound Repair with Innovative Hemostatic Glue: Clinical Case Report" Applied Sciences 13, no. 15: 8979. https://doi.org/10.3390/app13158979
APA StyleAlovisi, M., Erovigni, F., Bianchi, L., Longhi, B., Scotti, N., Pasqualini, D., & Berutti, E. (2023). Surgical Wound Repair with Innovative Hemostatic Glue: Clinical Case Report. Applied Sciences, 13(15), 8979. https://doi.org/10.3390/app13158979








