Preliminary Results of Measurements of Frontal Plane Knee Alignment Using a Standardized, Sonographic-Assisted Digital Photograph—A Reliable and Accurate Alternative to a Full-Leg Radiograph?
Abstract
:1. Introduction
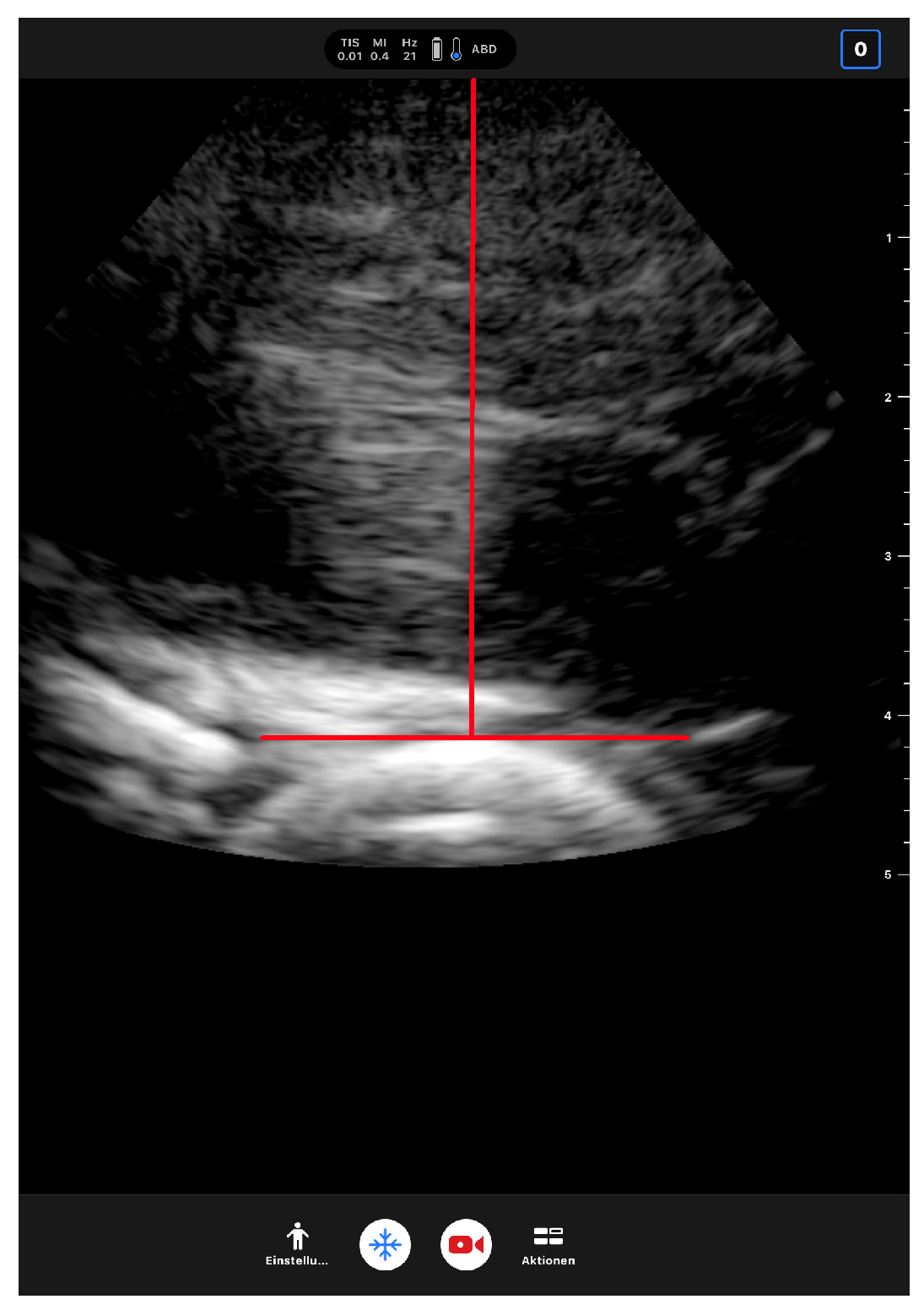
2. Materials and Methods
3. Results
3.1. Inter-Rater Reliability
3.2. Comparison between SPM and FLR of Subjects with BMI < 30 kg/m2
3.3. Comparison between SPM and FLRs of Subjects with BMI ≥ 30 kg/m2
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sharma, L.; Song, J.; Felson, D.T.; Cahue, S.; Shamiyeh, E.; Dunlop, D.D. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA 2001, 286, 188–195. [Google Scholar] [CrossRef] [Green Version]
- Tanamas, S.; Hanna, F.S.; Cicuttini, F.M.; Wluka, A.E.; Berry, P.; Urquhart, D.M. Does knee malalignment increase the risk of development and progression of knee osteoarthritis? A systematic review. Arthritis Rheum 2009, 61, 459–467. [Google Scholar] [CrossRef]
- Kadam, U.T.; Croft, P.R. Clinical comorbidity in osteoarthritis: Associations with physical function in older patients in family practice. J. Rheumatol. 2007, 34, 1899–1904. [Google Scholar]
- Kadam, U.T.; Croft, P.R. Clinical multimorbidity and physical function in older adults: A record and health status linkage study in general practice. Fam. Pract. 2007, 24, 412–419. [Google Scholar] [CrossRef]
- Hunter, D.J.; Bierma-Zeinstra, S. Osteoarthritis. Lancet 2019, 393, 1745–1759. [Google Scholar] [CrossRef] [PubMed]
- Wallace, I.J.; Worthington, S.; Felson, D.T.; Jurmain, R.D.; Wren, K.T.; Maijanen, H.; Woods, R.J.; Lieberman, D.E. Knee osteoarthritis has doubled in prevalence since the mid-20th century. Proc. Natl. Acad. Sci. USA 2017, 114, 9332–9336. [Google Scholar] [CrossRef]
- Lamark, K. The whole leg radiograph and radiation exposure in paediatrics. In Proceedings of the European Congress of Radiology 2013, Vienna, Austria, 7–11 March 2013. [Google Scholar]
- Colyn, W.; Agricola, R.; Arnout, N.; Verhaar, J.A.N.; Bellemans, J. How does lower leg alignment differ between soccer players, other athletes, and non-athletic controls? Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 3619–3626. [Google Scholar] [CrossRef]
- Becker, C.; Ross, C. Ganzbeinaufnahmen—Wieso, weshalb, warum? [Whole-leg radiographs—Why?]. Radiopraxis 2010, 3, 11–21. [Google Scholar] [CrossRef]
- Abreu, A.V.D.; Barbosa, J.R.P.; Paiva, F.J.D. Alinhamento dos joelhos no plano frontal dos 12 aos 17 anos [Alignment of the knees in the frontal plane from 12 to 17 years]. Rev. Bras. Ortop. 1996, 31, 83–88. [Google Scholar]
- Asadi, K.; Mirbolook, A.; Heidarzadeh, A.; Mardani Kivi, M.; Emami Meybodi, M.K.; Rouhi Rad, M. Association of Soccer and Genu Varum in Adolescents. Trauma Mon. 2015, 20, e17184. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hinman, R.S.; May, R.L.; Crossley, K.M. Is there an alternative to the full-leg radiograph for determining knee joint alignment in osteoarthritis? Arthritis Rheumatol. 2006, 55, 306–313. [Google Scholar] [CrossRef] [PubMed]
- Navali, A.M.; Bahari, L.A.S.; Nazari, B. A comparative assessment of alternatives to the full-leg radiograph for determining knee joint alignment. Sports Med. Arthrosc. Rehabil. Ther. Technol. 2012, 4, 40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schmitt, H.; Kappel, H.; Moser, M.T.; Cardenas-Montemayor, E.; Engelleiter, K.; Kuni, B.; Clarius, M. Determining knee joint alignment using digital photographs. Knee Surg. Sports Traumatol. Arthrosc. 2008, 16, 776–780. [Google Scholar] [CrossRef]
- Sheehy, L.; Cooke, T.D.V.; McLean, L.; Culham, E. Standardized standing pelvis-to-floor photographs for the assessment of lower-extremity alignment. Osteoarthr. Cartil. 2015, 23, 379–382. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Witvrouw, E.; Danneels, L.; Thijs, Y.; Cambier, D.; Bellemans, J. Does soccer participation lead to genu varum? Knee Surg. Sports Traumatol. Arthrosc. 2009, 17, 422–427. [Google Scholar] [CrossRef]
- Omololu, B.; Tella, A.; Ogunlade, S.O.; Adeyemo, A.A.; Adebisi, A.; Alonge, T.O.; Salawu, S.A.; Akinpelu, A.O. Normal values of knee angle, intercondylar and intermalleolar distances in Nigerian children. West Afr. J. Med. 2003, 22, 301–304. [Google Scholar] [CrossRef] [Green Version]
- Memmel, C.; Denzlein, A.; Szymski, D.; Huber, L.; Achenbach, L.; Gerling, S.; Alt, V.; Krutsch, W.; Koch, M. Playing Football as a Risk Factor for Lower Leg Malalignment?—Comparing Lower Leg Axis of Male Adolescent Football Players and Referees. Appl. Sci. 2023, 13, 7928. [Google Scholar] [CrossRef]
- Paley, D. Radiographic Assessment of Lower Limb Deformities. In Principles of Deformity Correction; Paley, D., Ed.; Springer: Berlin/Heidelberg, Germany, 2002; pp. 31–60. [Google Scholar]
- McGraw, K.O.; Wong, S.P. Forming inferences about some intraclass correlation coefficients. Psychol. Methods 1996, 1, 30–46. [Google Scholar] [CrossRef]
- Shrout, P.E.; Fleiss, J.L. Intraclass correlations: Uses in assessing rater reliability. Psychol. Bull. 1979, 86, 420–428. [Google Scholar] [CrossRef]
- Portney, L.G.; Watkins, M.P. Foundations of Clinical Research: Applications to Practice, 2nd ed.; Prentice Hall: Upper Saddle River, NJ, USA, 2000. [Google Scholar]
- Jeon, M.R.; Park, H.J.; Lee, S.Y.; Kang, K.A.; Kim, E.Y.; Hong, H.P.; Youn, I. Radiation dose reduction in plain radiography of the full-length lower extremity and full spine. Br. J. Radiol. 2017, 90, 20170483. [Google Scholar] [CrossRef]
- Kloth, J.K.; Neumann, R.; von Stillfried, E.; Stiller, W.; Kauczor, H.-U.; Ewerbeck, V.; Weber, M.-A. Quality-controlled dose reduction of full-leg radiography in patients with knee malalignment. Skeletal Radiol. 2015, 44, 423–429. [Google Scholar] [CrossRef]
- Bundesamt für Strahlenschutz. Natural Radiation in Germany. 2022. Available online: https://www.bfs.de/DE/themen/ion/umwelt/natuerliche-strahlung/natuerliche-strahlung_node.html (accessed on 18 May 2023).
- Legrand, T.; Richard, V.; Bonnefoy-Mazure, A.; Armand, S.; Miozzari, H.H.; Turcot, K. The impact of body-mass index on the frontal knee alignment estimation using three-dimensional reconstruction based on movement analysis. Knee 2020, 27, 89–94. [Google Scholar] [CrossRef]
- Kromeyer-Hauschild, K.; Wabitsch, M.; Kunze, D.; Geller, F.; Geiß, H.C.; Hesse, V.; von Hippel, A.; Jaeger, U.; Johnsen, D.; Korte, W.; et al. Percentiles for the body mass index for childhood and adolescence using different German samples. Monatsschrift Kinderheilkd. 2001, 149, 807–818. [Google Scholar] [CrossRef] [Green Version]
- Bergmann, K.E.; Mensink, G.B.M. Body measurements and overweight. Gesundheitswesen 1999, 61, 115–120. [Google Scholar]
- Hauner, H. Obesity. Med. Klin. 2009, 104, 851–866. [Google Scholar] [CrossRef] [PubMed]
- Max-Rubner-Institute—Federal Research Institute of Nutrition and Food; Result Report Part 1—National Consumption Study II. 2008. Available online: https://www.bmel.de/SharedDocs/Downloads/DE/_Ernaehrung/NVS_Ergebnisbericht.html (accessed on 6 August 2023).
- McCann, H.; Stanitski, D.F.; Barfield, W.R.; Leupold, J.A.; Nietert, P.J. The effect of tibial rotation on varus deformity measurement. J. Pediatr. Orthop. 2006, 26, 380–384. [Google Scholar] [CrossRef]
- Cooke, T.D.V.; Sled, E.A.; Scudamore, R.A. Frontal plane knee alignment: A call for standardized measurement. J. Rheumatol. 2007, 34, 1796–1801. [Google Scholar]
- Sabharwal, S.; Zhao, C. The Hip-Knee-Ankle Angle in Children: Reference Values Based on a Full-Length Standing Radiograph. J. Bone Jt. Surg. 2009, 91, 2461–2468. [Google Scholar] [CrossRef]
- Boewer, M.; Arndt, H.; Ostermann, P.A.W.; Petersein, J.; Mutze, S. Length and angle measurements of the lower extremity in digital composite overview images. Eur. Radiol. 2005, 15, 158–164. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, G.L.; Altman, G.T.; Dougherty, J.T.; DeMeo, P.J. Reproducibility and reliability of the anatomic axis of the lower extremity. J. Knee Surg. 2004, 17, 141–143. [Google Scholar] [CrossRef]
- Ilahi, O.A.; Kadakia, N.R.; Huo, M.H. Inter- and intraobserver variability of radiographic measurements of knee alignment. Am. J. Knee Surg. 2001, 14, 238–242. [Google Scholar]
- Goker, B.; Block, J.A. Improved precision in quantifying knee alignment angle. Clin. Orthop. Relat. Res. 2007, 458, 145–149. [Google Scholar] [CrossRef] [PubMed]
- Moreland, J.R.; Bassett, L.W.; Hanker, G.J. Radiographic analysis of the axial alignment of the lower extremity. J. Bone Jt. Surg. 1987, 69, 745–749. [Google Scholar] [CrossRef]
- Specogna, A.V.; Birmingham, T.B.; DaSilva, J.J.; Milner, J.S.; Kerr, J.; Hunt, M.A.; Jones, I.C.; Jenkyn, T.R.; Fowler, P.J.; Giffin, J.R. Reliability of lower limb frontal plane alignment measurements using plain radiographs and digitized images. J. Knee Surg. 2004, 17, 203–210. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Group | Overall | I | II |
|---|---|---|---|
| Inclusion criterion | BMI < 30 kg/m2 | BMI ≥ 30 kg/m2 | |
| n (participants) | 18 | 13 | 5 |
| n (lower extremities) | 34 | 24 | 10 |
| Height in cm (mean/SD/range) | 173/10/158–190 | 169/7/158–183 | 183/9/165–190 |
| Weight in kg (mean/SD/range) | 79.5/24.6/43–120 | 66.4/14.4/43–85 | 110.8/13.4/85–120 |
| BMI in kg/m2 (mean/SD/range) | 25.5/5.8/15–34 | 22.6/4.2/15–29 | 32.4/1.6/30–34 |
| Group | I | II | Overall | |||
|---|---|---|---|---|---|---|
| BMI < 30 kg/m2 | BMI ≥ 30 kg/m2 | |||||
| n | 24 | 10 | 34 | |||
| method | FLR | SPM | FLR | SPM | FLR | SPM |
| HKA range (°) | 166.4–195.1 | 168.6–195.2 | 177.0–183.8 | 182.5–190.0 | 166.4–195.1 | 168.6–195.2 |
| HKA (mean ± SD; °) | 180.4 ± 5.9 | 182.0 ± 6.4 | 180.3 ± 2.2 | 185.8 ± 2.7 | 180.4 ± 5.1 | 183.1 ± 5.8 |
| mean deviation and range (MD/range; °) | 2.4/0.1–6.0 | 5.5/2.6–8.1 | 3.3/0.1–8.1 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Memmel, C.; Meier, C.; Huber, L.; Szymski, D.; Achenbach, L.; Koch, M.; Alt, V.; Krutsch, W.; Weber, J. Preliminary Results of Measurements of Frontal Plane Knee Alignment Using a Standardized, Sonographic-Assisted Digital Photograph—A Reliable and Accurate Alternative to a Full-Leg Radiograph? Appl. Sci. 2023, 13, 9074. https://doi.org/10.3390/app13169074
Memmel C, Meier C, Huber L, Szymski D, Achenbach L, Koch M, Alt V, Krutsch W, Weber J. Preliminary Results of Measurements of Frontal Plane Knee Alignment Using a Standardized, Sonographic-Assisted Digital Photograph—A Reliable and Accurate Alternative to a Full-Leg Radiograph? Applied Sciences. 2023; 13(16):9074. https://doi.org/10.3390/app13169074
Chicago/Turabian StyleMemmel, Clemens, Christoph Meier, Lorenz Huber, Dominik Szymski, Leonard Achenbach, Matthias Koch, Volker Alt, Werner Krutsch, and Johannes Weber. 2023. "Preliminary Results of Measurements of Frontal Plane Knee Alignment Using a Standardized, Sonographic-Assisted Digital Photograph—A Reliable and Accurate Alternative to a Full-Leg Radiograph?" Applied Sciences 13, no. 16: 9074. https://doi.org/10.3390/app13169074





