Abstract
Psoriasis is an inflammatory dermatosis manifested by the appearance of brown-red papules on the body, covered with silver scales. One of the most common and effective treatments for psoriasis is narrow-band UVB phototherapy. Narrow-band UVB has a wavelength of 311 nm, which results in shallow skin penetration, is absorbed only by the epidermis and the superficial layers of the dermis. The aim of the study was to assess the effect of narrow-band UVB 311 nm phototherapy on skin covered with psoriatic scales and without psoriatic lesions in patients with psoriasis vulgaris on the total directional hemispherical reflectance (DHR) of the skin, skin density and epidermis thickness. For this purpose, a 410 Solar DHR reflectometer and high-frequency ultrasonography DUB SkinScanner were used. A total of 48 volunteers were enrolled. There was a difference in the reflectance of skin without psoriatic scales and psoriatic skin. Depending on the wavelength range, the skin was characterized by different reflectance values. During the course of phototherapy, the reflectance values decreased, both in the psoriatic skin and skin without psoriatic scales. After the phototherapy, the epidermis thickness and SLEB layer decreased and skin density increased in the area with psoriatic plaque. The density of the skin without psoriasis after a series of 20 irradiations increased, while the thickness of the epidermis did not change.
1. Introduction
Psoriasis is an inflammatory dermatosis manifested by the appearance of brown-red papules on the body, covered with a silver scales. Genetic, immunological and environmental factors play an important role in the etiopathogenesis of psoriasis. Psoriasis is characterized by excessive proliferation of keratinocytes and skin vascular endothelial cells. A hallmark of psoriasis is abnormal communication between keratinocytes and cells of the immune system, including T cells, dendritic cells, macrophages and neutrophils [1,2,3].
One of the most common and effective treatments for psoriasis is narrow-band UVB phototherapy. Narrow-band UVB has a 311 nm wavelength, which results in shallow skin penetration, is absorbed only by the epidermis and the superficial layers of the dermis [4]. UVB phototherapy has an immunosuppressive effect and regulates cell division. It reduces inflammation by reducing the expression of pro-inflammatory cytokines and increasing the production of anti-inflammatory cytokines. NB-UVB inhibits the TH1 and TH17 signaling pathways. It leads to a reduction in the number of Langerhans cells and dendritic cells, causes keratinocytes apoptosis and increases reactive oxygen species [5,6].
Narrow-band UVB phototherapy is associated with the irradiation of the patient’s entire body and contributes to a large amount of cumulative UVB exposure. During the treatments, the skin with psoriatic lesions is irradiated, as well as the skin without psoriatic lesions [7].
Microvascular abnormalities are a characteristic feature of psoriasis. Within psoriatic lesions, there are microvascular changes of superficial vessels. Patients have an increased number and size of blood vessels in the skin, as well as increased infiltration of inflammatory cells and the formation of Munro micro-abscesses. The blood vessels are twisted, woody, and their endothelium has gaps through which the migration of inflammatory cells is facilitated [8].
The aim of the study was to assess the effect of narrow-band UVB 311 nm photo-therapy on skin covered with psoriatic scales and without lesions in patients with psoriasis vulgaris on the total skin directional reflectance, skin density and epidermis thickness.
Skin reflectance measurement determines the qualitative and quantitative interaction with electromagnetic radiation in the spectral range of 335–2500 nm. It allows us to determine what range of radiation is reflected and what is absorbed/transmitted, which is important in phototherapy.
Skin reflectance depends on many factors. Light propagating in the skin was absorbed mostly by chromophores. Melanin is one of the skin pigments mainly located in the basal layer of the epidermis. The volume fraction of melanin in the epidermis depends on sunlight exposition and hormonal regulations. There are two forms of melanin—brown-black eumelanin and yellow-red pheomelanin. Absorption coefficients of both types of melanin are similar in the visible light range; however, they can influence the diffuse reflectance slightly. In the dermis, the dominant chromophore is hemoglobin. Depending on whether it is oxygenated or not, it shows different absorption spectra. Hemoglobin has absorption peaks in the green-yellow region of the light spectrum and absorbs little light in the red range, while melanin’s absorption decreases linearly in the red range. The contents of β–carotene, bilirubin and water also have an impact of DHR. The structure of the collagen fibers affects scattering in the skin. Their arrangement and size influences the type of scattering that will occur in the skin tissue—Rayleigh scattering or Mie scattering, which also affects the HDR measurement [9,10,11].
Thickness of the epidermis and the structure of its surface have an influence on HDR. Psoriatic lesions are clearly demarcated from the surrounding skin and are characterized by a rough surface. A hallmark of psoriasis is hyperkeratosis, which contributes to an increase in the thickness of the stratum corneum. Abnormal proliferation, incomplete maturation of keratinocytes and retention of nuclei in the stratum corneum can affect the light propagation in the skin. The inflammatory process, the larger diameter of the capillaries within the psoriatic lesions and greater blood perfusion affect the content of the volume fraction of hemoglobin.
2. Materials and Methods
2.1. Volunteers
A total of 48 patients (27 men aged 46 ± 17 and 21 women aged 46 ± 16) with psoriasis vulgaris participated in the study. Patients were subjected to 20 narrow-band UVB 311 irradiation performed three times a week. Patients were not allowed to use any other psoriatic treatment during the study besides skin care preparations. Home care products were based on emollients and were devoid of additional exfoliating substances. The inclusion and exclusion criteria for the study are presented in the Table 1.

Table 1.
Inclusion and exclusion criteria.
This study was approved by the Ethics Committee of the SUM No. PCN/0022/KB1/12/I/20 on 19 May 2020 and was conducted according to the principles of the Declaration of Helsinki. All volunteers gave informed consent to participate in the study.
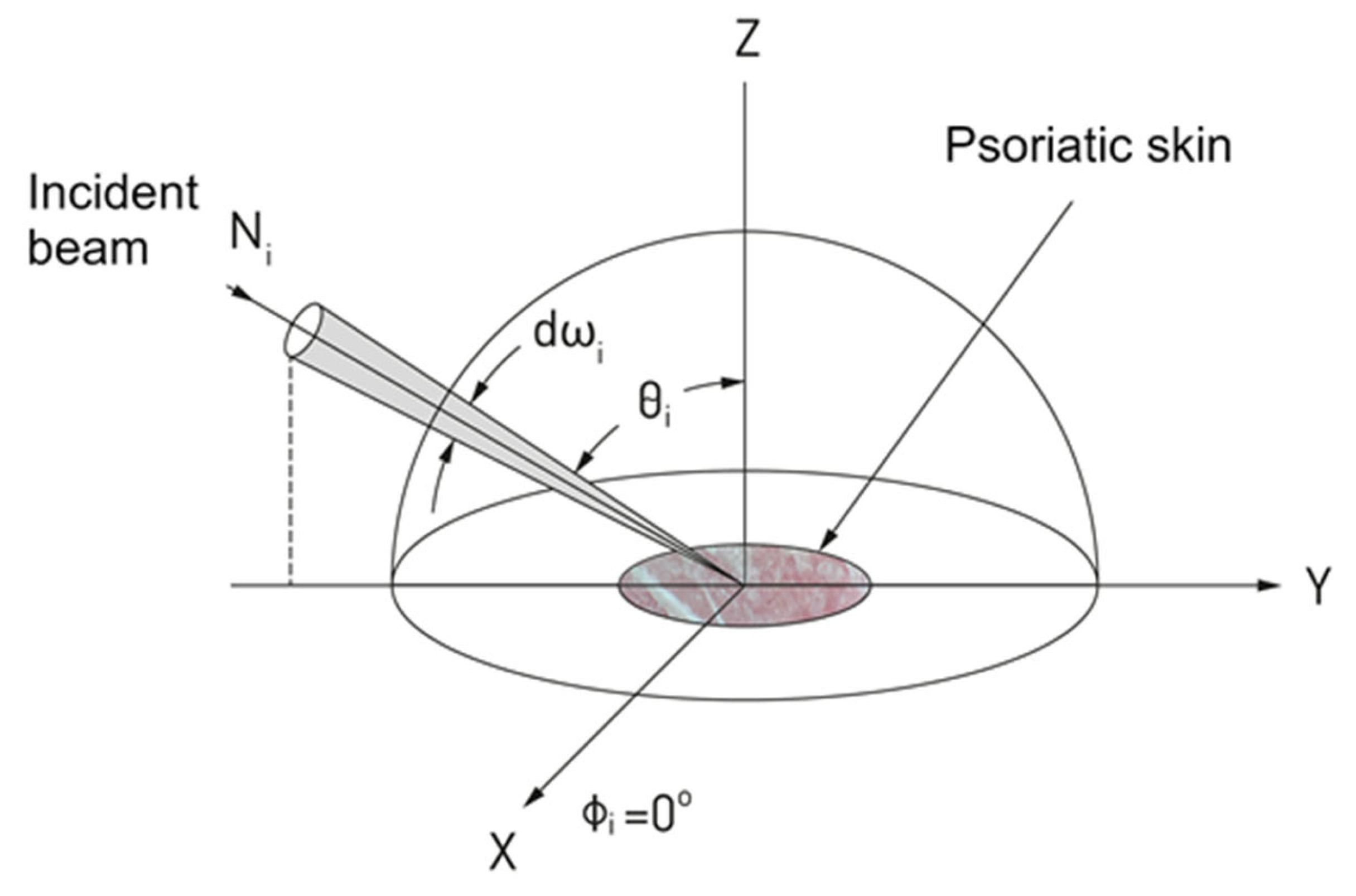
2.2. Directional Reflectance Measurements
A 410 Solar DHR reflectometer (Surface Optics Corporation, San Diego, CA, USA) was used to measure the total reflection from the skin surface in the range of 335 to 2500 nm. The 410 Solar reflectometer measures the integrated surface reflectance of a surface at 20 degrees incidence in seven wavebands in the visible and near infrared spectral regions. The integrating sphere captures the reflected light from the skin surface, integrating reflections in all directions. Detectors located in the integrating sphere measure the amount of reflected light and convert it into an analog electrical signal, which is processed to determine the reflectance of the test sample for an angle of incidence of 20 degrees and each of the wavelength bands.
The directional reflectance is defined as the ratio of the total energy reflected of the light reflected from the skin to the measuring hemisphere, to the energy of the light incident on the surface [12].
Directional hemispherical reflectance was measured in following wavelength bands (nm): 335–380, 400–540, 480–600, 590–720, 700–1100, 1000–1700 and 1700–2500 of both psoriatic skin and skin not covered with psoriatic scales. Before starting measurements, the reflectometer was calibrated with calibration coupons—specular and diffuse. The measurement regions were without hair on the surface. Measurements were made before the start of therapy, after 10 and after 20 irradiations. Each skin region was measured three times, and the results were averaged. Measurements were always made at the same locations (Figure 1).
Figure 1.
Diagram illustrating the concept of directional reflectance measurements of skin.
2.3. High Frequency Ultrasound Imaging
DUB SkinScanner high-frequency ultrasonography in B-scan projection with a 33 MHz transducer was used to examine skin density (echo-intensity) and epidermis thickness (entrance echo). Among the images of the affected skin, the sub-epidermal low-echogenic band (SLEB) was also measured. The epidermis thickness was calculated in millimeters based on the A-scan. SLEB thickness was evaluated in micrometers by measuring the vertical distance between the epidermal entrance echo and the dermis. Skin density was measured directly under the epidermis, or under the SLEB if present, by using the “region of interest” (ROI) function in the DUB SkinScanner software (DUB-SkinScanner75 5.21.) The images were acquired at the skin with psoriatic lesion and non-lesional skin area, before, after 10 and 20 UVB irradiations. Measurements were always made at the same locations. All images were obtained using the same setting. Before the measurements, ultrasonographical gel was applied to the examined surface. The images were captured perpendicularly to the skin surface with minimal pressure from the operator.
Total directional reflectance measurements and high frequency ultrasound imaging were performed during the same visit. On the day the measurements were performed, the patients did not use any skincare products. Volunteers were subjected to 20 min of acclimatization before starting the measurements. The measurements occurred in the same environmental conditions with the same ambience and room setting. The measurement of the skin without psoriatic lesions was performed in close proximity to the psoriatic lesion.
2.4. Statistical Analysis
The statistical analysis of the results was performed with the use of Excel 2016 and Statistica 13.1 software. Normality was checked with the Shapiro–Wilk test. The results at the level of p < 0.05 were considered statistically significant. The significance of the differences between skin density, epidermis thickness and skin reflectance were assessed using the Friedman’s ANOVA and Dunn’s post-hoc test.
3. Results
Skin with psoriasis and skin without psoriatic changes are characterized by different reflectance values depending on the examined wavelength range. Over the course of phototherapy, there were changes in the reflectance of both psoriatic and non-psoriatic skin, as shown in the Table 2.

Table 2.
Skin reflectance values at different wavelength ranges.
The lowest values of psoriatic skin reflectance before therapy occurred at the wavelengths of 1700–2500 nm (median 0.077 mm). For skin with no psoriasis lesions, the lowest values were also observed in the range 1700–2500 nm (median 0.073 mm).
The highest reflectance values before therapy of psoriatic skin occurred in the wavelength range of 590–720 nm (median 0.529 mm). In the case of skin without psoriasis lesions, the highest reflectance values were observed in the wavelength range 700–1100 nm (median 0.553 mm).
Before the therapy, psoriatic skin was characterized by a higher reflectance than the skin without psoriatic changes in the wavelength ranges 335–380 nm and 1700–2500 nm. After 10 and 20 irradiations the same dependence was observed.
Psoriatic skin after 20 irradiations showed lower reflectance at each of the measured wavelengths than the skin without psoriatic lesions before the therapy. Skin without psoriatic after 20 irradiations showed lower reflectance at each of the measured wavelengths than before therapy (Table 2).
Differences in the thickness of the epidermis were observed between skin without psoriatic lesion and psoriatic skin. There was no statistically significant difference in the thickness of the epidermis of the non-psoriatic areas before, after 10 and after 20 sessions of phototherapy. The difference in epidermis thickness within psoriatic skin before and after the series of the 20 irradiations were statistically significant. After the end of phototherapy, the epidermis thickness decreased from median 0.289 to median 0.204 (Table 3).

Table 3.
Epidermis thickness of psoriatic and non-lesional skin before, after 10 and after 20 irradiations.
Higher skin density values were observed in uninvolved skin compared with psoriatic skin (Me = 32.165 vs. Me = 11.145). During phototherapy, there was an increase in skin density relative to baseline in both psoriatic and non-psoriatic skin. After 20 irradiations, there was a statistically significant increase in skin density from median 11.145 to 21.210 in the skin with psoriatic scales. Skin without psoriatic lesion also increased from median 32.165 at the baseline to 34.275 after 20 irradiations (Table 4).

Table 4.
Density of psoriatic and non-lesional skin before, after 10 and after 20 irradiations.
In the skin without psoriatic lesions, no SLEB layer was observed both before or after the series of 10 and 20 irradiations. Before the therapy, the median value of the SLEB (sub-epidermal low-echogenic band) in psoriatic skin was 0.285 mm, while after the therapy it decreased to 0.201 mm (Table 5).

Table 5.
SLEB layer in psoriatic skin before, after 10 and 20 phototherapy sessions.
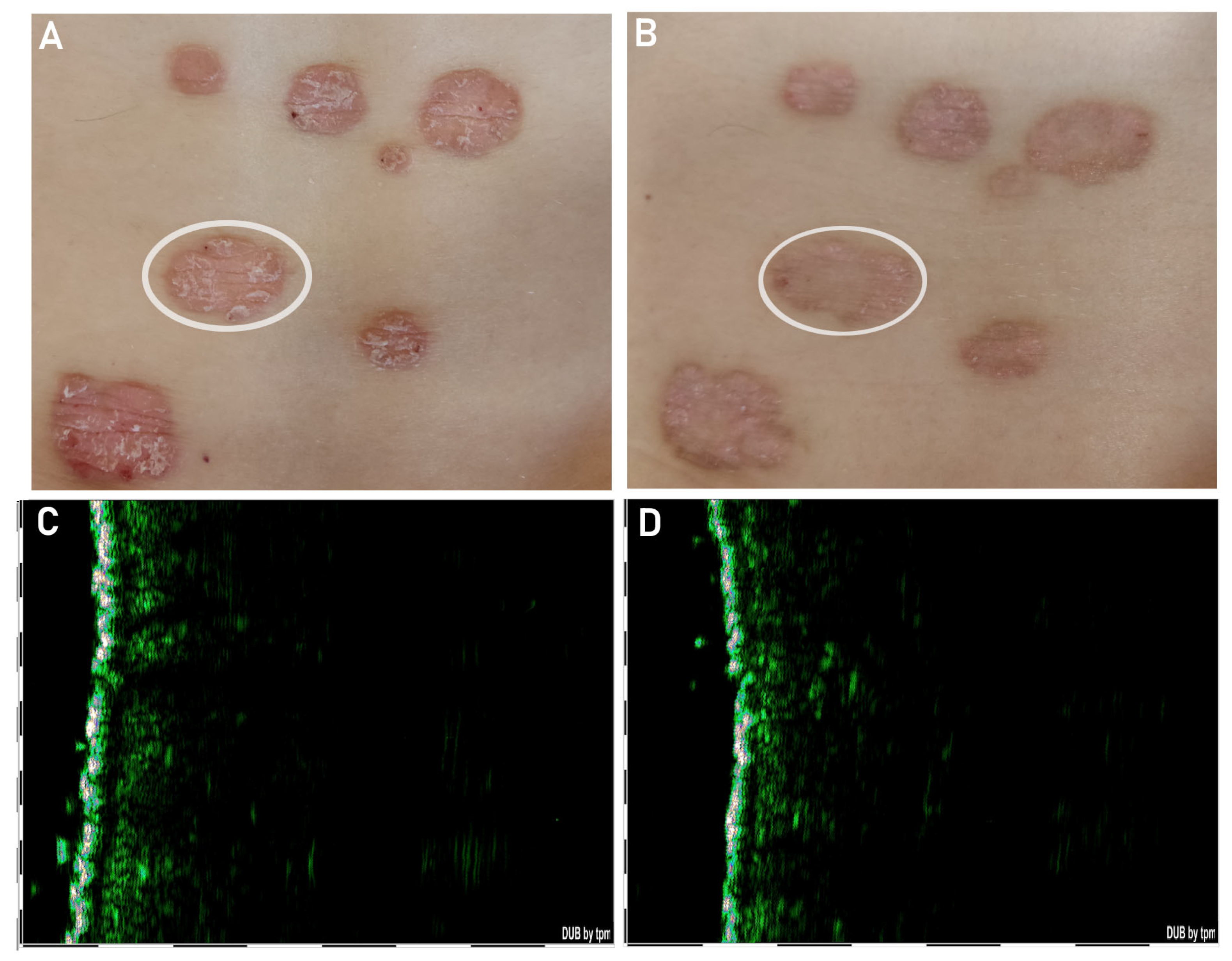
Phototherapy did not contribute to complete remission of psoriasis lesions. After a series of 20 irradiations, the epidermis was thinned, but the psoriatic lesions were still visible. The SLEB (subepidermal low-echogenic band) layer under the epidermis had also decreased (Figure 2).
Figure 2.
Psoriatic skin before the therapy (A) and the ultrasound image corresponding to the lesion marked in the photograph (C). Psoriatic skin after 20 irradiations (B) and the ultrasound image corresponding to the lesion marked (white circle) in the photograph (D).
4. Discussion
Directional hemispherical reflectance enables the determination of the reflectance ratio in a wide spectral range. The reflectance assessment may prove useful in monitoring the course of therapy in many dermatoses, including psoriasis. The skin’s reflectance value is influenced by the chromophores it contains, mainly melanin and hemoglobin, as well as structural protein.
The penetration of the radiation into the tissue increases with wavelength from the UV to the visible light range and decreases in the IR range in accordance with the selected optical properties. The depth increases with the decrease in the thickness of the stratum corneum [13]. Penetration depths of UV radiation in human skin depend also on anatomical location and content of chromophores. Meinhardt et al. showed that regardless of phototype and location, radiation at a wavelength of 311 nm does not penetrate deeper than 60 µm [14].
Batani et al. showed that in psoriatic lesions there was an increased number of capillary vessels per dermal papilla present as compared with skin without psoriatic lesions. A statistically significantly larger Feret’s diameter and perimeter of dermal capillaries in psoriatic skin was also observed compared to healthy skin [15]. The epidermis within the psoriatic lesion is thicker than the epidermis in the non-psoriatic area [16].
In our research, a decrease in reflectance values over the course of psoriatic therapy was observed for both affected and unchanged skin for each of the seven wavelength ranges. At the wavelengths of 335–380 nm, reflectance of psoriatic skin decreases, which may indicate the reduction of the plaque as a result of the therapy. The thickness of the epidermis also decreased, which means that radiation in this wavelength range could penetrate deeper and melanin content could increase. Reflectance in non-lesional skin also decreased at the wavelengths of 335–380 nm, while the thickness of the epidermis did not change, which may indicate an increase in melanin content.
In the skin without psoriatic lesion, the decrease in reflectance at the wavelength of 400–540 and 480–600 nm may be related to the increase in melanin component. At the same wavelength range, reflectance of psoriatic skin did not statistically change after 20 irradiations. Lack of changes in reflectance in this wavelength range may be the result of a decrease in the thickness of the epidermis and a possible increase in melanin content with a simultaneous decrease in hemoglobin content. Thinning of the SLEB layer after the end of phototherapy suggests a decrease in inflammation. Wolberink et al. used reflectance confocal microscopy (RCM) to visualize capillary blood flow in the dermal papillae of six patient with psoriasis to monitor the therapeutic response of UVB phototherapy. The research shows that the number of dermal papillae with blood flow decreased from 84% at baseline to 40%, 12 weeks after clearance. The size and diameter of blood vessels markedly decreased and capillary blood flow was minimal or absent [17].
No statistically significant differences were found between skin without psoriatic lesions and healthy skin before the start of phototherapy in the wavelength range of 1700–2500 nm, despite differences in epidermal thickness and skin density. In this wavelength range, the main components of the skin responsible for absorption are collagen and water [18,19]. After phototherapy at the wavelengths of 1700–2500 nm, the reflectance of skin without psoriatic lesion decreased, skin density increased and no changes in epidermal thickness were observed. Reflectance of psoriatic skin also decreased, skin density increased, whereas epidermal thickness decreased. A decrease in this wavelength range may be indicated by higher absorption of chromophores such as water and collagen. Waves in the range of 1850–2500 nm are absorbed mainly in the epidermis [20]. The use of skin care preparations by patients during treatment could have changed the optical parameters of the epidermis and contribute to a decrease in reflectance.
The light spectrum determines the depth of its penetration into the skin. The wavelength can be matched to a variety of target cells or tissues in order to achieve specific effects. A combination of various light’s spectra affecting different targets may allow for better therapeutic effects and lead to longer periods of remission in patients with psoriasis. Phototherapy also affects skin unchanged from psoriasis. Changes in skin reflectance without psoriasis during therapy indicate the effect of UVB radiation on non-lesional skin. No changes in the thickness of the epidermis and an increase in the density of non-lesional skin after a series of 20 irradiations proves the safety of this method of treatment.
Hemispheric directional reflectance enables the measurement of the total reflectance of the healthy and diseased skin. Knowledge of the spectral reflectance of human skin in a wide spectral range may contribute to the development of non-invasive methods of diagnosing skin diseases. Research with the use of HDR may assess the response of healthy and diseased skin to the ultraviolet ray [21].
Limitations
- The patients did not use the same home care products.
- Home care was used by patients with varying frequency.
- The measuring range of the wavelength for the reflectometer used in the research is from 335 to 2500 nm.
5. Conclusions
UVB phototherapy has an influence on skin directional reflectance, skin density and epidermal thickness. The use of the 410 Solar Reflectometer makes it possible to conduct total reflectance measurements for skin with psoriatic lesion and without any sign of psoriatic plaque, which allows us to assess the impact of phototherapy on the skin. Depending on the wavelength range, the skin was characterized by different reflectance values. During the course of phototherapy, the reflectance values decreased, both in the psoriatic skin and skin without psoriatic scales. Under the influence of 20 sessions of narrow-band UVB 311 nm irradiation, the thickness of the epidermis within the psoriatic scales thinned, while the epidermis of the skin without psoriatic lesion does not change. Phototherapy also contributes to the increase in the density of non-lesional and psoriatic skin.
Author Contributions
All authors were responsible for the concept and design of the study, provided critical feedback and helped shape the research. W.O. conceived the study, contributed to the interpretation of the results, analyzed the data, wrote the manuscript and designed the figures; A.D. and D.W.-D. conceived and planned the experiments, worked on the manuscript, J.Z.-N. analyzed the data, verified the analytical methods; S.W. worked on the manuscript; B.B.-F. carried out the experiments, supervised the findings of this work and drafted the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This study is supported by the Medical University of Silesia (PCN-2-019/K/2/O, PCN-1-074/N/2/K).
Institutional Review Board Statement
This study was approved by the Ethics Committee of the SUM No. PCN/0022/KB1/12/I/20 on 19 May 2020 and was conducted according to the principles of the Declaration of Helsinki. All volunteers gave informed consent to participate in the study.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Reid, C.; Griffiths, C.E.M. Psoriasis and treatment: Past, present and future aspects. Acta Derm. Venereol. 2020, 100, 69–79. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Chen, Y.; Cui, L.; Shi, Y.; Guo, C. Advances in the pathogenesis of psoriasis: From keratinocyte perspective. Cell Death Dis. 2022, 13, 81. [Google Scholar] [CrossRef] [PubMed]
- Rendon, A.; Schäkel, K. Psoriasis pathogenesis and treatment. Int. J. Mol. Sci. 2019, 20, 1475. [Google Scholar] [CrossRef] [PubMed]
- Rathod, D.G.; Muneer, H.M.S. Phototherapy; StatPearls Publishing: St. Petersburg, FL, USA, 2021. [Google Scholar]
- Myers, E.; Kheradmand, S.; Miller, R. An Update on Narrowband Ultraviolet B Therapy for the Treatment of Skin Diseases. Cureus 2021, 13, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Zhang, P.; Wu, M.X. A clinical review of phototherapy for psoriasis. Lasers Med. Sci. 2018, 33, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Ibbotson, S.H. A perspective on the use of NB-UVB Phototherapy vs. PUVA photochemotherapy. Front. Med. 2018, 5, 184. [Google Scholar] [CrossRef] [PubMed]
- Huang, T.-H.; Lin, C.-F.; Alalaiwe, A.; Yang, S.-C.; Fang, J.-Y. Apoptotic or Antiproliferative Activity of Natural Products against Keratinocytes for the Treatment of Psoriasis. Int. J. Mol. Sci. 2019, 20, 2558. [Google Scholar] [CrossRef] [PubMed]
- Li, S. Human Skin Characterization and Analysis Based on Hyperspectral Reflectance Using Machine Learning. 2021. Available online: https://theses.hal.science/tel-03412032/document (accessed on 10 June 2023).
- Duan, R.; Zhang, J.; Du, X.; Yao, X.; Konno, K. Properties of collagen from skin, scale and bone of carp (Cyprinus carpio). Food Chem. 2009, 112, 702–706. [Google Scholar] [CrossRef]
- Del Bino, S.; Duval, C.; Bernerd, F. Clinical and Biological Characterization of Skin Pigmentation Diversity and Its Consequences on UV Impact. Int. J. Mol. Sci. 2018, 19, 2668. [Google Scholar] [CrossRef] [PubMed]
- Nicodemus, F.E. Reflectance Nomenclature and Directional Reflectance and Emissivity. Appl. Opt. 1970, 9, 1474. [Google Scholar] [CrossRef] [PubMed]
- Finlayson, L.; Barnard, I.R.M.; McMillan, L.; Ibbotson, S.H.; Brown, C.T.A.; Eadie, E.; Wood, K. Depth Penetration of Light into Skin as a Function of Wavelength from 200 to 1000 nm. Photochem. Photobiol. 2021, 98, 974–981. [Google Scholar] [CrossRef] [PubMed]
- Meinhardt, M.; Krebs, R.; Anders, A.; Heinrich, U.; Tronnier, H. Wavelength-dependent penetration depths of ultraviolet radiation in human skin. J. Biomed. Opt. 2008, 13, 044030. [Google Scholar] [CrossRef] [PubMed]
- Batani, A.; Brănișteanu, D.E.; Ilie, M.A.; Boda, D.; Ianosi, S.; Ianosi, G.; Caruntu, C. Assessment of dermal papillary and microvascular parameters in psoriasis vulgaris using in vivo reflectance confocal microscopy. Exp. Ther. Med. 2018, 15, 1241–1246. [Google Scholar] [CrossRef] [PubMed]
- Suárez-Fariñas, M.; Li, K.; Fuentes-Duculan, J.; Hayden, K.; Brodmerkel, C.; Krueger, J.G. Expanding the psoriasis disease profile: Interrogation of the skin and serum of patients with moderate-to-severe psoriasis. J. Investig. Dermatol. 2012, 132, 2552–2564. [Google Scholar] [CrossRef] [PubMed]
- Wolberink, E.A.W.; Van Erp, P.E.J.; De Boer-Van Huizen, R.T.; Van De Kerkhof, P.C.M.; Gerritsen, M.J.P. Reflectance confocal microscopy: An effective tool for monitoring ultraviolet B phototherapy in psoriasis. Br. J. Dermatol. 2012, 167, 396–403. [Google Scholar] [CrossRef] [PubMed]
- Caplan, J.D.; Waxman, S.; Nesto, R.W.; Muller, J.E. Near-infrared spectroscopy for the detection of vulnerable coronary artery scales. J. Am. Coll. Cardiol. 2006, 47 (Suppl. 8), C92–C96. [Google Scholar] [CrossRef] [PubMed]
- Sekar, S.K.; Bargigia, I.; Mora, A.D.; Taroni, P.; Ruggeri, A.; Tosi, A.; Pifferi, A.; Farina, A. Diffuse optical characterization of collagen absorption from 500 to 1700 nm. J. Biomed. Opt. 2017, 22, 15006. [Google Scholar] [CrossRef] [PubMed]
- Hale, G.M.; Querry, M.R. Optical Constants of Water in the 200-nm to 200-μm Wavelength Region. Appl. Opt. 1973, 12, 555–563. [Google Scholar] [CrossRef] [PubMed]
- Cooksey, C.C.; Allen, D.W.; Tsai, B.K. Reference data set of human skin reflectance. J. Res. Natl. Inst. Stand. Technol. 2017, 122, 26. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).