Symptomatic Diastasis Rectus Abdominis in Children: Review of Current Management Options and Presentation of a Novel Minimally Invasive Epifascial Repair Technique
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Collection
2.2. Patient Inclusion
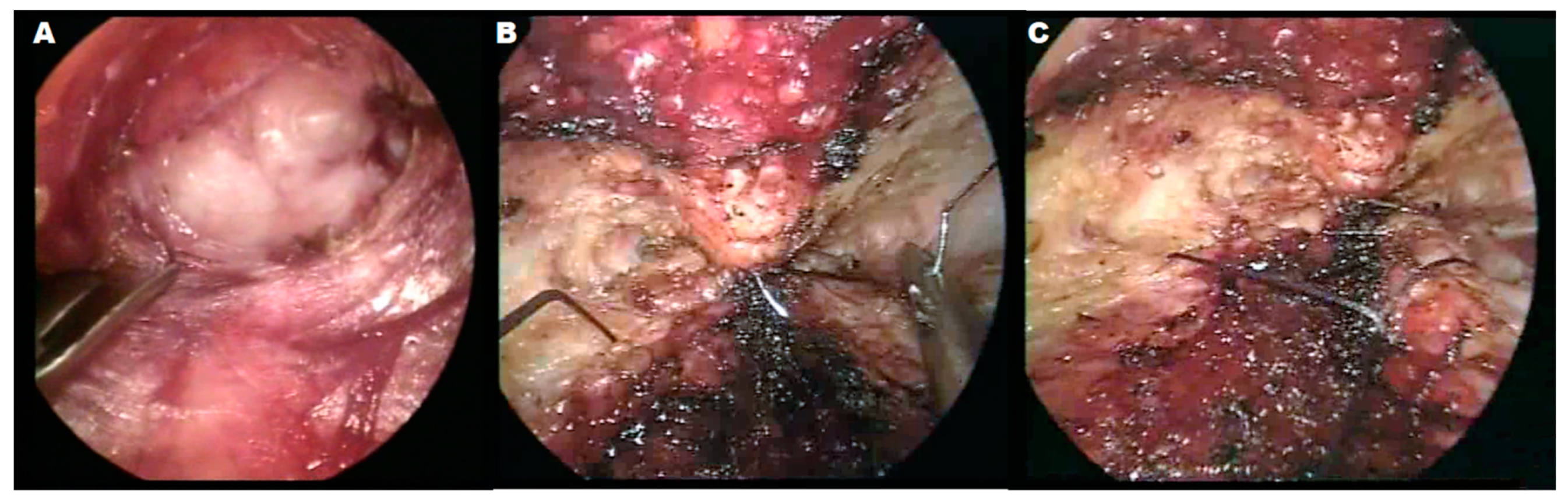
2.3. Surgical Technique
3. Results
3.1. Patient 1
3.2. Patient 2
3.3. Patient 3
3.4. Patient 4
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Maurice Nahabedian, M.; Brooks, D.C. Rectus Abdominis Diastasis; UpToDate: Waltham, MA, USA, 2021. [Google Scholar]
- Sperstad, J.B.; Tennfjord, M.K.; Hilde, G.; Ellström-Engh, M.; Bø, K. Diastasis recti abdominis during pregnancy and 12 months after childbirth: Prevalence, risk factors and report of lumbopelvic pain. Br. J. Sports Med. 2016, 50, 1092–1096. [Google Scholar] [CrossRef] [PubMed]
- Hsia, M.; Jones, S. Natural resolution of rectus abdominis diastasis. Two single case studies. Aust. J. Physiother. 2000, 46, 301–307. [Google Scholar] [CrossRef] [PubMed]
- Human Embryology. Available online: http://www.embryology.ch/anglais/mmuskel/skelett05.html (accessed on 4 October 2021).
- Digilio, M.C.; Capolino, R.; Dallapiccola, B. Autosomal dominant transmission of nonsyndromic diastasis recti and weakness of the linea alba. Am. J. Med. Genet. Part A 2008, 146A, 254–256. [Google Scholar] [CrossRef] [PubMed]
- McKee-Garrett, T.M. Assessment of the Newborn Infant; UpToDate: Waltham, MA, USA, 2021. [Google Scholar]
- E Drutz, J.E. The Pediatric Physical Examination: Chest and Abdomen; UpToDate: Waltham, MA, USA, 2021. [Google Scholar]
- Uffman, C. Surgically Correctable Hernias in Children. Available online: https://cookchildrens.org/SiteCollectionDocuments/professionals/CCPNsurgicallycorrectablehernias_nov2012.pdf (accessed on 1 April 2020).
- Tupler Technique Treatment for Diastasis Recti. Available online: https://diastasisrehab.com/pages/start-it-kids (accessed on 8 August 2021).
- Gluppe, S.L.; Hilde, G.; Tennfjord, M.K.; Engh, M.E.; Bø, K. Effect of a Postpartum Training Program on the Prevalence of Diastasis Recti Abdominis in Postpartum Primiparous Women: A Randomized Controlled Trial. Phys. Ther. 2018, 98, 260–268. [Google Scholar] [CrossRef]
- Michalska, A.; Rokita, W.; Wolder, D.; Pogorzelska, J.; Kaczmarczyk, K. Diastasis recti abdominis—A review of treatment methods. Ginekol. Pol. 2018, 89, 97–101. [Google Scholar] [CrossRef]
- Thabet, A.A.; Alshehri, M.A. Efficacy of deep core stability exercise program in postpartum women with diastasis recti abdominis: A randomised controlled trial. J. Musculoskelet. Neuronal Interact. 2019, 19, 62–68. [Google Scholar]
- Feins, N.R.; Dzakovic, A.; Papadakis, K. Minimally invasive closure of pediatric umbilical hernias. J. Pediatr. Surg. 2008, 43, 127–130. [Google Scholar] [CrossRef]
- Hartenstein, H.J. On injection therapy of umbilical hernia in childhood. Kinderarztl. Prax. 1959, 27, 361–365. [Google Scholar]
- Strauchman, M.; Morningstar, M. Prolotherapy Injections for Diastasis Recti: A Case Report. Case Rep. Clin. Med. 2016, 5, 342–346. [Google Scholar] [CrossRef]
- Köhler, G.; Luketina, R.R.; Emmanuel, K. Sutured repair of primary small umbilical and epigastric hernias: Concomitant rectus diastasis is a significant risk factor for recurrence. World J. Surg. 2015, 39, 121–126; discussion 127. [Google Scholar] [CrossRef]
- Helal, O.F.; Alshehri, M.A.; Alayat, M.S.; Alhasan, H.; Tobaigy, A. The effectiveness of short-term high-intensity exercise on ventilatory function, in adults with a high risk of chronic obstructive pulmonary disease. J. Phys. Ther. Sci. 2017, 29, 927–930. [Google Scholar] [CrossRef][Green Version]
- Mavros, M.N.; Athanasiou, S.; Alexiou, V.G.; Mitsikostas, P.K.; Peppas, G.; Falagas, M.E. Risk factors for mesh-related infections after hernia repair surgery: A meta-analysis of cohort studies. World J. Surg. 2011, 35, 2389–2398. [Google Scholar] [CrossRef] [PubMed]
- Kao, A.M.; Arnold, M.R.; Augenstein, V.A.; Heniford, B.T. Prevention and Treatment Strategies for Mesh Infection in Abdominal Wall Reconstruction. Plast. Reconstr. Surg. 2018, 142, 149s–155s. [Google Scholar] [CrossRef] [PubMed]
- Palanivelu, C.; Rangarajan, M.; Jategaonkar, P.A.; Amar, V.; Gokul, K.S.; Srikanth, B. Laparoscopic repair of diastasis recti using the ’Venetian blinds’ technique of plication with prosthetic reinforcement: A retrospective study. Hernia J. Hernias Abdom. Wall Surg. 2009, 13, 287–292. [Google Scholar] [CrossRef] [PubMed]
- Chan, D.L.; Ravindran, P.; Fan, H.S.; Elstner, K.E.; Jacombs, A.S.W.; Ibrahim, N.; Talbot, M.L. Minimally invasive Venetian blinds ventral hernia repair with botulinum toxin chemical component separation. ANZ J. Surg. 2020, 90, 67–71. [Google Scholar] [CrossRef] [PubMed]
- Siddiky, A.H.; Kapadia, C.R. Laparoscopic plication of the linea alba as a repair for diastasis recti—A mesh free approach. J. Surg. Case Rep. 2010, 2010, 3. [Google Scholar] [CrossRef]
- Ismail, M.; Shalaby, R. Single instrument intracorporeal knot tying during single port laparoscopic hernia repair in children: A new simplified technique. J. Pediatr. Surg. 2014, 49, 1044–1048. [Google Scholar] [CrossRef]
- Gireev, G.I.; Zagirov, U.Z.; Shakhnazarov, A.M. Treatment of linea alba hernia and diastasis of rectus abdominis. Khirurgiia 1997, 7, 58–61. [Google Scholar]
- Köckerling, F.; Botsinis, M.D.; Rohde, C.; Reinpold, W. Endoscopic-Assisted Linea Alba Reconstruction plus Mesh Augmentation for Treatment of Umbilical and/or Epigastric Hernias and Rectus Abdominis Diastasis—Early Results. Front. Surg. 2016, 3, 27. [Google Scholar] [CrossRef]
- Reinpold, W.; Schröder, M.; Berger, C.; Stoltenberg, W.; Köckerling, F. MILOS and EMILOS repair of primary umbilical and epigastric hernias. Hernia J. Hernias Abdom. Wall Surg. 2019, 23, 935–944. [Google Scholar] [CrossRef]
- Bellido Luque, J.; Bellido Luque, A.; Valdivia, J.; Suarez Gráu, J.M.; Gomez Menchero, J.; García Moreno, J.; Guadalajara Jurado, J. Totally endoscopic surgery on diastasis recti associated with midline hernias. The advantages of a minimally invasive approach. Prospective cohort study. Hernia J. Hernias Abdom. Wall Surg. 2015, 19, 493–501. [Google Scholar] [CrossRef] [PubMed]
- Medina, P.; Busnelli, G.L.; Nardi, W. Diastasis Recti and Other Midline Defects: Totally Subcutaneous Endoscopic Approach. New Horiz. Laparosc. Surg. 2018, 13. [Google Scholar] [CrossRef]
- Juárez Muas, D.M. Preaponeurotic endoscopic repair (REPA) of diastasis recti associated or not to midline hernias. Surg. Endosc. 2019, 33, 1777–1782. [Google Scholar] [CrossRef] [PubMed]
- Champault, G.; Catheline, J.M.; Barrat, C. Video-parietoscopic surgery of the abdominal wall. A study of 15 cases. Chir. Mem. De L’academie De Chir. 1998, 123, 474–477. [Google Scholar] [CrossRef]
- Ramirez, O.M. Abdominoplasty and abdominal wall rehabilitation: A comprehensive approach. Plast. Reconstr. Surg. 2000, 105, 425–435. [Google Scholar] [CrossRef]
- Scheuerlein, H.; Thiessen, A.; Schug-Pass, C.; Köckerling, F. What Do We Know About Component Separation Techniques for Abdominal Wall Hernia Repair? Front. Surg. 2018, 5, 24. [Google Scholar] [CrossRef]
- Levy, S.; Tsao, K.; Cox, C.S., Jr.; Phatak, U.R.; Lally, K.P.; Andrassy, R.J. Component separation for complex congenital abdominal wall defects: Not just for adults anymore. J. Pediatr. Surg. 2013, 48, 2525–2529. [Google Scholar] [CrossRef]
- Ikoma, N.; Chen, L.; Andrassy, R.J. Technical note: Component separation technique with double-layered biologic mesh placement for neonate with large gastroschisis. J. Plast. Reconstr. Aesthetic Surg. JPRAS 2014, 67, e230–e231. [Google Scholar] [CrossRef]
- Miller, E.A.; Goldin, A.; Tse, G.N.; Tse, R. Extended Component Separation for Repair of High Ventral Hernia in Pediatric Omphalocele. Plast. Reconstr. Surg. Glob. Open 2015, 3, e503. [Google Scholar] [CrossRef]
- van Eijck, F.C.; van Vlimmeren, L.A.; Wijnen, R.M.; Klein, W.; Kruijen, I.; Pillen, S.; Nijhuis-van der Sanden, M.W. Functional, motor developmental, and long-term outcome after the component separation technique in children with giant omphalocele: A case control study. J. Pediatr. Surg. 2013, 48, 525–532. [Google Scholar] [CrossRef]
- Inoue, M.; Aoi, S.; Taniguchi, A.; Sakai, K.; Higashi, M.; Fumino, S.; Furukawa, T.; Tajiri, T. Laparoscopic intraperitoneal onlay mesh for pediatric incisional hernia—A case report. Surg. Case Rep. 2017, 3, 122. [Google Scholar] [CrossRef] [PubMed]
- Albanese, C.T.; Rengal, S.; Bermudez, D. A novel laparoscopic technique for the repair of pediatric umbilical and epigastric hernias. J. Pediatr. Surg. 2006, 41, 859–862. [Google Scholar] [CrossRef] [PubMed]
- Jun, Z.; Na, J.; Zhen, C.; Xuan, Y.; Yan-Dong, W.; Shu-Li, L.; Long, L. Single-incision laparoscopic approach for linea alba hernia in children. J. Minim. Access. Surg. 2019, 15, 42–45. [Google Scholar] [CrossRef] [PubMed]
- Babsail, A.A.; Abelson, J.S.; Liska, D.; Muensterer, O.J. Single-incision pediatric endosurgical epigastric hernia repair. Hernia J. Hernias Abdom. Wall Surg. 2014, 18, 357–360. [Google Scholar] [CrossRef]
- Michael, A.I.; Ademola, S.A.; Olawoye, O.A.; Iyun, A.O.; Adebayo, W.; Oluwatosin, O.M. Pediatric keloids: A 6-year retrospective review. Pediatr. Dermatol. 2017, 34, 673–676. [Google Scholar] [CrossRef]
- Czerkasij, V. Skin of color: A basic outline of unique differences. Nurse Pract. 2013, 38, 34–40. [Google Scholar] [CrossRef]

| Male/Female | 1/3 |
|---|---|
| Age (mean, range) | 4 (2–8) years |
| Dehiscence (maximum, n = 2) | 4 and 2 cm measured with sonography |
| Secondary diagnosis | Umbilical hernia (1×) |
| Clinical complaints | Progredience of the rectus diastasis (8 mm within 7 months) with significant prolapse of intrabdominal structures, periumbilical pain, postprandial pain, pain on passing stool |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Denzinger, M.; Stark, D.; Memmel, C.; Reis Wolfertstetter, P.; Knorr, C. Symptomatic Diastasis Rectus Abdominis in Children: Review of Current Management Options and Presentation of a Novel Minimally Invasive Epifascial Repair Technique. Appl. Sci. 2023, 13, 9841. https://doi.org/10.3390/app13179841
Denzinger M, Stark D, Memmel C, Reis Wolfertstetter P, Knorr C. Symptomatic Diastasis Rectus Abdominis in Children: Review of Current Management Options and Presentation of a Novel Minimally Invasive Epifascial Repair Technique. Applied Sciences. 2023; 13(17):9841. https://doi.org/10.3390/app13179841
Chicago/Turabian StyleDenzinger, Markus, Domitille Stark, Clemens Memmel, Patricia Reis Wolfertstetter, and Christian Knorr. 2023. "Symptomatic Diastasis Rectus Abdominis in Children: Review of Current Management Options and Presentation of a Novel Minimally Invasive Epifascial Repair Technique" Applied Sciences 13, no. 17: 9841. https://doi.org/10.3390/app13179841
APA StyleDenzinger, M., Stark, D., Memmel, C., Reis Wolfertstetter, P., & Knorr, C. (2023). Symptomatic Diastasis Rectus Abdominis in Children: Review of Current Management Options and Presentation of a Novel Minimally Invasive Epifascial Repair Technique. Applied Sciences, 13(17), 9841. https://doi.org/10.3390/app13179841






