A Diagonal Movement Pattern of Arm Elevation and Depression in Overhead Throwing Athletes: An Exploratory Kinematic Analysis for Clinical Application
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.1.1. Athletes
2.1.2. Non-Athletes
2.2. Procedures
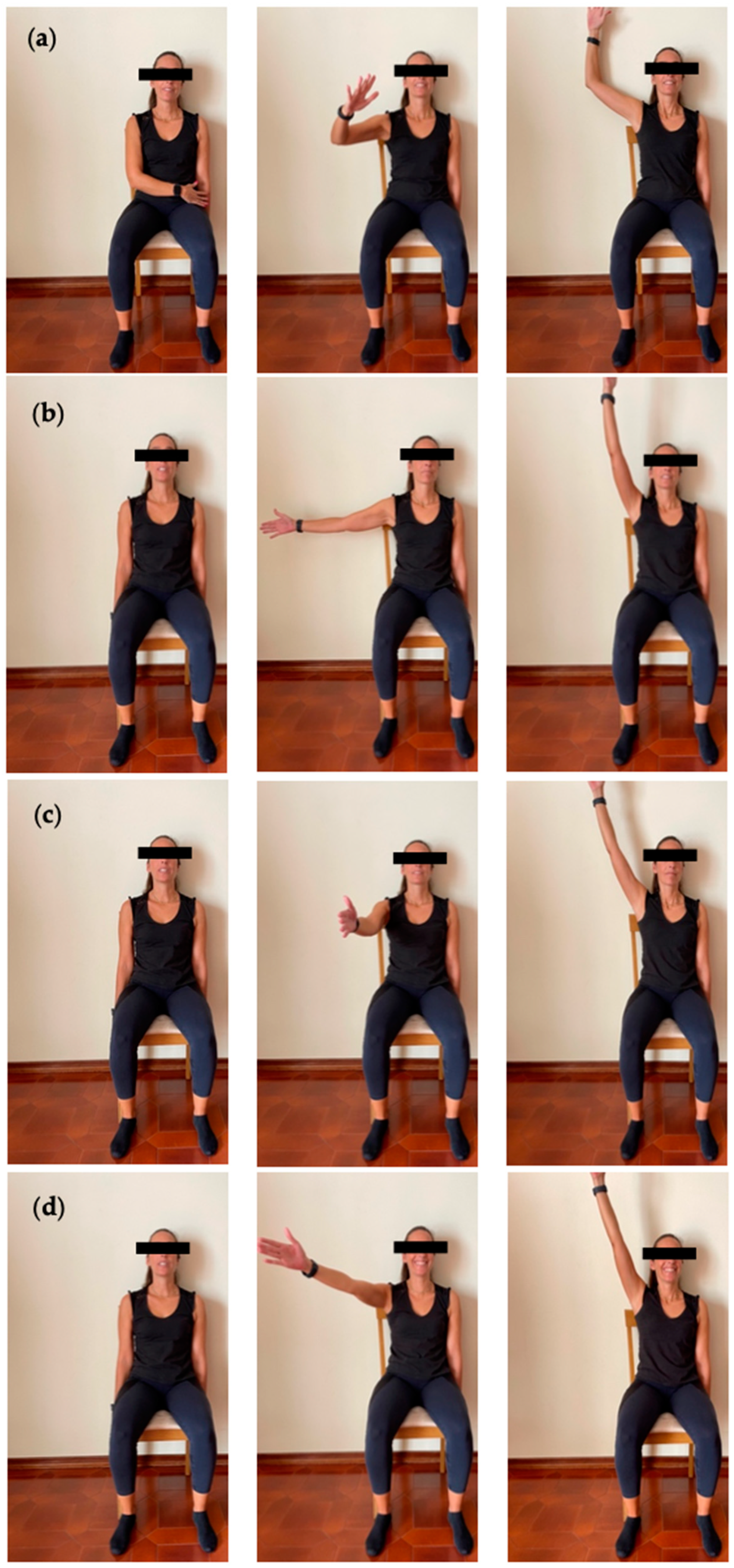
2.2.1. Tasks
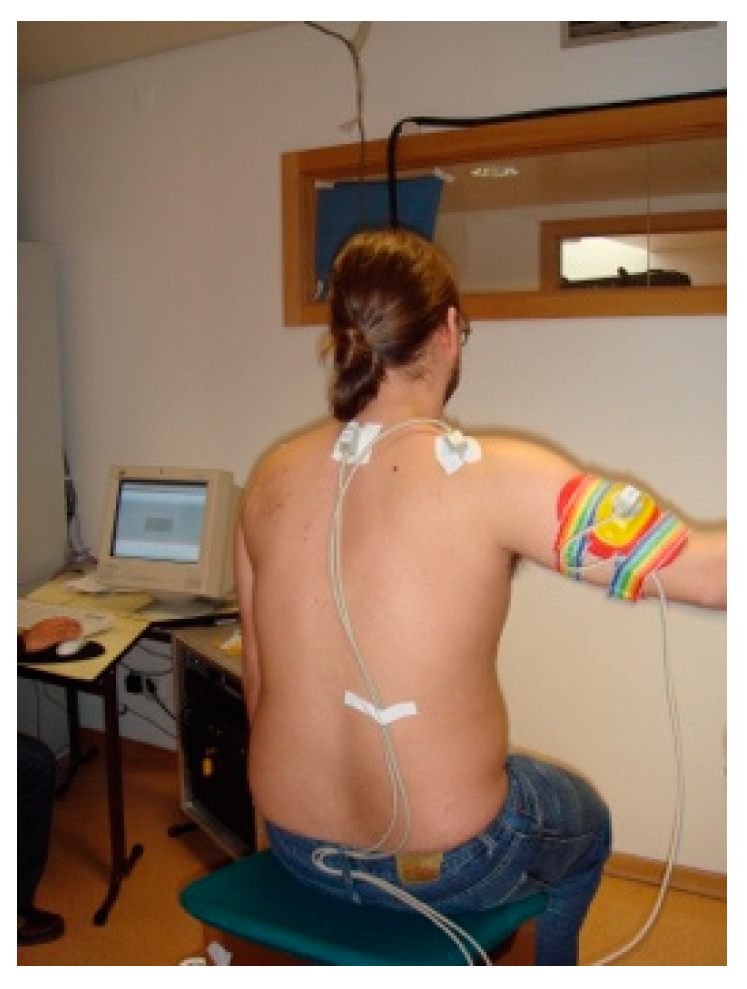
2.2.2. Kinematics
2.3. Data Analysis
3. Results
3.1. Participants
3.1.1. Athletes
3.1.2. Non-Athletes
3.2. Three-Dimensional Scapular Kinematics
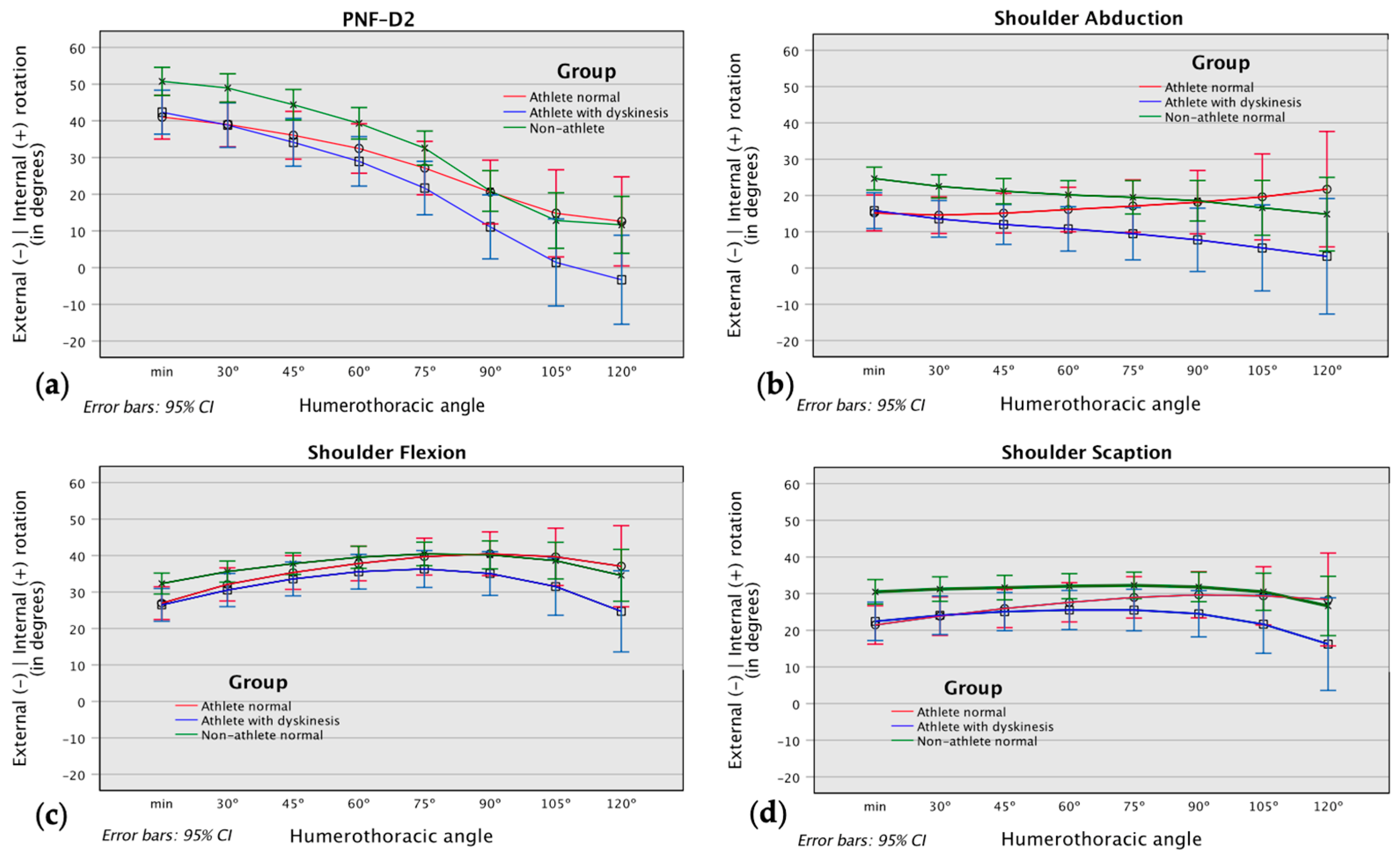
3.2.1. Scapular Internal/External Rotation
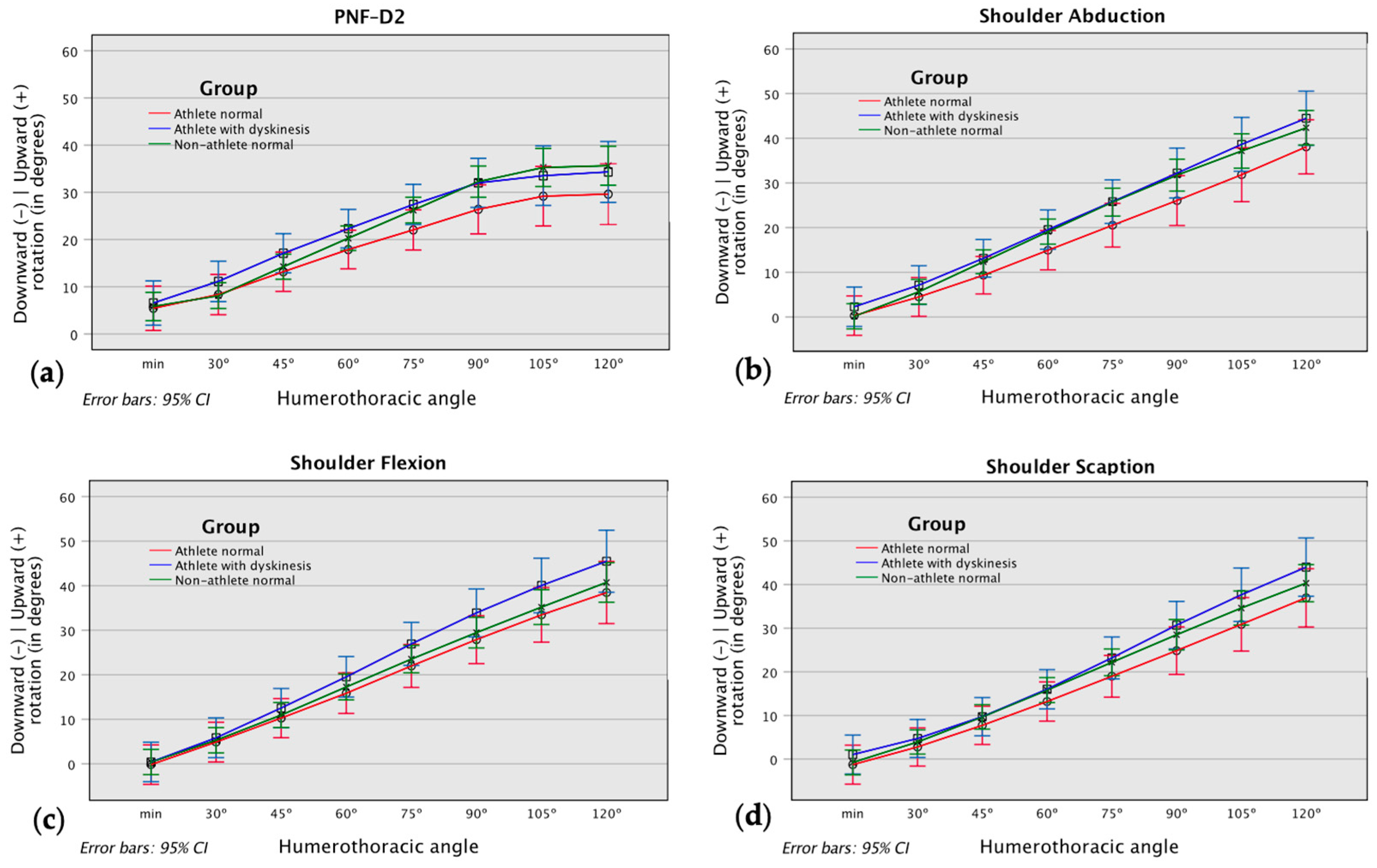
3.2.2. Scapular Upward/Downward Rotation
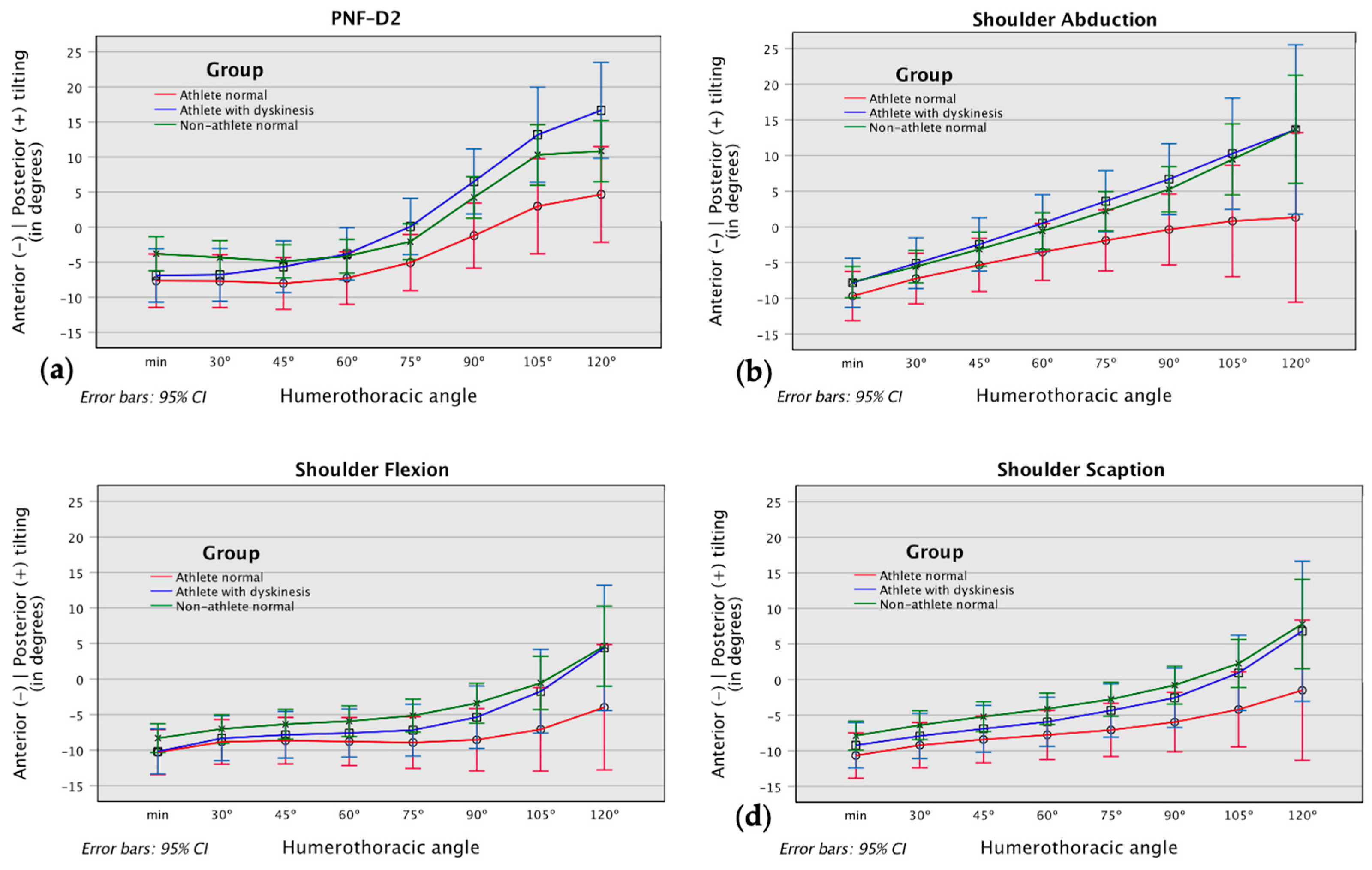
3.2.3. Scapular Anterior/Posterior Tilting
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sciascia, A.; Kibler, W.B. Current Views of Scapular Dyskinesis and its Possible Clinical Relevance. Int. J. Sports Phys. Ther. 2022, 17, 117–130. [Google Scholar] [CrossRef] [PubMed]
- Kibler, W.B.; Stone, A.V.; Zacharias, A.; Grantham, W.J.; Sciascia, A.D. Management of Scapular Dyskinesis in Overhead Athletes. Oper. Tech. Sports Med. 2021, 29, 150797. [Google Scholar] [CrossRef]
- Fu, X.; Yung, P.S.-H.; Ma, C.C.; Leong, H.T. Scapular Kinematics in Athletes With and Without Rotator Cuff Tendinopathy: A Systematic Review. J. Sport Rehabil. 2020, 29, 820–829. [Google Scholar] [CrossRef] [PubMed]
- Amasay, T.; Karduna, A.R. Scapular Kinematics in Constrained and Functional Upper Extremity Movements. J. Orthop. Sports Phys. Ther. 2009, 39, 618–627. [Google Scholar] [CrossRef]
- Lang, A.E.; Dickerson, C.R.; Kim, S.Y.; Stobart, J.; Milosavljevic, S. Impingement pain affects kinematics of breast cancer survivors in work-related functional tasks. Clin. Biomech. 2019, 70, 223–230. [Google Scholar] [CrossRef]
- Lang, A.E.; Milosavljevic, S.; Dickerson, C.R.; Kim, S.Y. Examining assessment methods of scapular motion: Comparing results from planar elevations and functional task performance. Clin. Biomech. 2020, 80, 105203. [Google Scholar] [CrossRef]
- Roren, A.; Lefevre-Colau, M.-M.; Roby-Brami, A.; Revel, M.; Fermanian, J.; Gautheron, V.; Poiraudeau, S.; Fayad, F. Modified 3D scapular kinematic patterns for activities of daily living in painful shoulders with restricted mobility: A comparison with contralateral unaffected shoulders. J. Biomech. 2012, 45, 1305–1311. [Google Scholar] [CrossRef]
- Spinelli, B.A.; Silfies, S.; Jacobs, L.A.; Brooks, A.D.; Ebaugh, D. Scapulothoracic and Glenohumeral Motions During Functional Reaching Tasks in Women With a History of Breast Cancer and Healthy Age-Matched Controls. Rehabil. Oncol. 2016, 34, 127–136. [Google Scholar] [CrossRef]
- Pascoal, A.G.; Morais, N. Kinematic Comparison and Description of the 3-Dimensional Shoulder Kinematics of 2 Shoulder Rotation Tests. J. Manip. Physiol. Ther. 2015, 38, 288–294. [Google Scholar] [CrossRef]
- Oliveira, L.d.S.; Moura, T.B.M.A.; Rodacki, A.L.F.; Tilp, M.; Okazaki, V.H.A. A systematic review of volleyball spike kinematics: Implications for practice and research. Int. J. Sports Sci. Coach. 2020, 15, 239–255. [Google Scholar] [CrossRef]
- Trasolini, N.A.; Nicholson, K.F.; Mylott, J.; Bullock, G.S.; Hulburt, T.C.; Waterman, B.R. Biomechanical Analysis of the Throwing Athlete and Its Impact on Return to Sport. Arthrosc. Sports Med. Rehabil. 2022, 4, e83–e91. [Google Scholar] [CrossRef] [PubMed]
- Ludewig, P.M.; Phadke, V.; Braman, J.P.; Hassett, D.R.; Cieminski, C.J.; LaPrade, R.F. Motion of the Shoulder Complex During Multiplanar Humeral Elevation. J. Bone Jt. Surg. Am. 2009, 91-A, 378–389. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, A.; Pascoal, A.G.; Morais, N. The Scapular Contribution to the Amplitude of Shoulder External Rotation on Throwing Athletes. In Technologies for Medical Sciences; Natal Jorge, R.M., Tavares, J.M.R.S., Pinotti Barbosa, M., Slade, A.P., Eds.; Springer: Amsterdam, The Netherlands, 2012; Volume 1, pp. 227–242. [Google Scholar]
- Karduna, A.R.; McClure, P.W.; Michener, L.A.; Sennett, B. Dynamic measurements of three-dimensional scapular kinematics: A validation study. J. Biomech. Eng. 2001, 123, 184–190. [Google Scholar] [CrossRef] [PubMed]
- Meyer, K.E.; Saether, E.E.; Soiney, E.K.; Shebeck, M.S.; Paddock, K.L.; Ludewig, P.M. Three-Dimensional Scapular Kinematics During the Throwing Motion. J. Appl. Biomech. 2008, 24, 24–34. [Google Scholar] [CrossRef]
- Rogowski, I.; Creveaux, T.; Sevrez, V.; ChÈZe, L.; Dumas, R. How Does the Scapula Move during the Tennis Serve? Med. Sci. Sports Exerc. 2015, 47, 1444–1449. [Google Scholar] [CrossRef]
- Saka, M.; Yamauchi, H.; Yoshioka, T.; Hamada, H.; Gamada, K. Scapular Kinematics During Late Cocking of a Simulated Throwing Activity in Baseball Players With Shoulder Injury: A Cross-Sectional Study Using a 3D-to-2D Registration Technique. J. Sport Rehabil. 2015, 24, 91–98. [Google Scholar] [CrossRef]
- Shih, Y.-F.; Wang, Y.-C. Spiking Kinematics in Volleyball Players With Shoulder Pain. J. Athl. Train. 2019, 54, 90–98. [Google Scholar] [CrossRef]
- Cools, A.M.; Maenhout, A.G.; Vanderstukken, F.; Declève, P.; Johansson, F.R.; Borms, D. The challenge of the sporting shoulder: From injury prevention through sport-specific rehabilitation toward return to play. Ann. Phys. Rehabil. Med. 2021, 64, 101384. [Google Scholar] [CrossRef]
- Padua, D.A.; Guskiewicz, K.M.; Prentice, W.E.; Schneider, R.E.; Shields, E.W. The Effect of Select Shoulder Exercises on Strength, Active Angle Reproduction, Single-Arm Balance, and Functional Performance. J. Sport. Rehabil. 2004, 13, 75–95. [Google Scholar] [CrossRef]
- Moreira, R.; Lial, L.; Teles Monteiro, M.G.; Aragão, A.; Santos David, L.; Coertjens, M.; Silva-Júnior, F.L.; Dias, G.; Velasques, B.; Ribeiro, P.; et al. Diagonal movement of the upper limb produces greater adaptive plasticity than sagittal plane flexion in the shoulder. Neurosci. Lett. 2017, 643, 8–15. [Google Scholar] [CrossRef]
- Youdas, J.W.; Arend, D.B.; Exstrom, J.M.; Helmus, T.J.; Rozeboom, J.D.; Hollman, J.H. Comparison of Muscle Activation Levels During Arm Abduction in the Plane of the Scapula vs. Proprioceptive Neuromuscular Facilitation Upper Extremity Patterns. J. Strength Cond. Res. 2012, 26, 1058–1065. [Google Scholar] [CrossRef] [PubMed]
- Santos, J.D.; Gonçalves, R.S. Adaptação e validação cultural da versão portuguesa do Disabilities of the Arm Shoulder and Hand—DASH. Rev. Port. Ortop. E Traumatol. 2006, 4, 30–45. [Google Scholar]
- Alberta, F.G.; ElAttrache, N.S.; Bissell, S.; Mohr, K.; Browdy, J.; Yocum, L.; Jobe, F. The Development and Validation of a Functional Assessment Tool for the Upper Extremity in the Overhead Athlete. Am. J. Sports Med. 2010, 38, 903–911. [Google Scholar] [CrossRef]
- Tucci, H.T.; Martins, J.; Sposito Gde, C.; Camarini, P.M.; de Oliveira, A.S. Closed Kinetic Chain Upper Extremity Stability test (CKCUES test): A reliability study in persons with and without shoulder impingement syndrome. BMC Musculoskelet. Disord. 2014, 15, 1. [Google Scholar] [CrossRef] [PubMed]
- Sciascia, A.; Uhl, T. Reliability Of Strength And Performance Testing Measures And Their Ability To Differentiate Persons With And Without Shoulder Symptoms. Int. J. Sports Phys. Ther. 2015, 10, 655–666. [Google Scholar] [PubMed]
- McClure, P.; Tate, A.R.; Kareha, S.; Irwin, D.; Zlupko, E. A Clinical Method for Identifying Scapular Dyskinesis, Part 1: Reliability. J. Athl. Train. 2009, 44, 160–164. [Google Scholar] [CrossRef]
- Fayad, F.; Hoffmann, G.; Hanneton, S.; Yazbeck, C.; Lefevre-colau, M.M.; Poiraudeau, S.; Revel, M.; Roby-Brami, A. 3-D scapular kinematics during arm elevation: Effect of motion velocity. Clin. Biomech. 2006, 21, 932–941. [Google Scholar] [CrossRef]
- Lopes, A.D.; Timmons, M.K.; Grover, M.; Ciconelli, R.M.; Michener, L.A. Visual Scapular Dyskinesis: Kinematics and Muscle Activity Alterations in Patients With Subacromial Impingement Syndrome. Arch. Phys. Med. Rehabil. 2015, 96, 298–306. [Google Scholar] [CrossRef]
- Wu, G.; van der Helm, F.C.; Veeger, H.E.; Makhsous, M.; Van Roy, P.; Anglin, C.; Nagels, J.; Karduna, A.R.; McQuade, K.; Wang, X.; et al. ISB recommendation on definitions of joint coordinate systems of various joints for the reporting of human joint motion--Part II: Shoulder, elbow, wrist and hand. J. Biomech. 2005, 38, 981–992. [Google Scholar] [CrossRef]
- Gillet, B.; Begon, M.; Diger, M.; Berger-Vachon, C.; Rogowski, I. Alterations in scapulothoracic and humerothoracic kinematics during the tennis serve in adolescent players with a history of shoulder problems. Sports Biomech. 2021, 20, 165–177. [Google Scholar] [CrossRef]
- McQuade, K.J.; Borstad, J.; de Oliveira, A.S. A Critical and Theoretical Perspective on Scapular Stabilization: What Does It Really Mean, and Are We On the Right Track? Phys. Ther. 2016, 96, 1162–1169. [Google Scholar] [CrossRef] [PubMed]
- Pascoal, A.G.; Ribeiro, A.; Infante, J. Scapular Resting Posture and Scapulohumeral Rhythm Adaptations in Volleyball Players: Implications for Clinical Shoulder Assessment in Athletes. Sports 2023, 11, 114. [Google Scholar] [CrossRef] [PubMed]
- Turgut, E.; Colakoglu, F.F.; Baltaci, G. Scapular motion adaptations in junior overhead athletes: A three-dimensional kinematic analysis in tennis players and non-overhead athletes. Sports Biomech. 2019, 18, 308–316. [Google Scholar] [CrossRef] [PubMed]
- Salamh, P.A.; Hanney, W.J.; Boles, T.; Holmes, D.; McMillan, A.; Wagner, A.; Kolber, M.J. Is it Time to Normalize Scapular Dyskinesis? The Incidence of Scapular Dyskinesis in Those With and Without Symptoms: A Systematic Review of the Literature. Int. J. Sports Phys. Ther. 2023, 18, 558–576. [Google Scholar] [CrossRef]
- Burn, M.B.; McCulloch, P.C.; Lintner, D.M.; Liberman, S.R.; Harris, J.D. Prevalence of Scapular Dyskinesis in Overhead and Nonoverhead Athletes: A Systematic Review. Orthop. J. Sports Med. 2016, 4, 2325967115627608. [Google Scholar] [CrossRef]
- Hogan, C.; Corbett, J.A.; Ashton, S.; Perraton, L.; Frame, R.; Dakic, J. Scapular Dyskinesis Is Not an Isolated Risk Factor for Shoulder Injury in Athletes: A Systematic Review and Meta-analysis. Am. J. Sports Med. 2021, 49, 2843–2853. [Google Scholar] [CrossRef]
- Hickey, D.; Solvig, V.; Cavalheri, V.; Harrold, M.; McKenna, L. Scapular dyskinesis increases the risk of future shoulder pain by 43% in asymptomatic athletes: A systematic review and meta-analysis. Br. J. Sports Med. 2018, 52, 102–110. [Google Scholar] [CrossRef]
- Tooth, C.; Gofflot, A.; Schwartz, C.; Croisier, J.L.; Beaudart, C.; Bruyère, O.; Forthomme, B. Risk Factors of Overuse Shoulder Injuries in Overhead Athletes: A Systematic Review. Sports Health 2020, 12, 478–487. [Google Scholar] [CrossRef]
- Seitz, A.L.; McClelland, R.I.; Jones, W.J.; Jean, R.A.; Kardouni, J.R. A comparison of change in 3D scapular kinematics with maximal contractions and force production with scapular muscle tests between asymptomatic overhead athletes with and without scapular dyskinesi. Int. J. Sports Phys. Ther. 2015, 10, 309–318. [Google Scholar]
- Bullock, G.S.; Strahm, J.; Hulburt, T.C.; Beck, E.C.; Waterman, B.R.; Nicholson, K.F. Relationship Between Clinical Scapular Assessment and Scapula Resting Position, Shoulder Strength, and Baseball Pitching Kinematics and Kinetics. Orthop. J. Sports Med. 2021, 9, 2325967121991146. [Google Scholar] [CrossRef]
- Thomas, S.J.; Swanik, K.A.; Swanik, C.; Huxel, K.C. Glenohumeral rotation and scapular position adaptations after a single high school female sports season. J. Athl. Train. 2009, 44, 230–237. [Google Scholar] [CrossRef] [PubMed]
- Tooth, C.; Schwartz, C.; Gofflot, A.; Bornheim, S.; Croisier, J.-L.; Forthomme, B. Preseason shoulder screening in volleyball players: Is there any change during season? JSES Int. 2023, 7, 662–667. [Google Scholar] [CrossRef] [PubMed]
| Variable | Athletes (n = 11) | Athletes w/ScDk (n = 11) | Non-Athletes (n = 27) | p | |
|---|---|---|---|---|---|
| Age (years) | 25.55 ± 5.43 | 23.1 ± 4.99 | 22.36 ± 2.41 | 0.098 | 0.099 |
| Height (m) | 1.88 ± 0.09 | 1.84 ± 0.07 | 1.78 ± 0.07 | <0.001 * | 0.269 |
| Body mass (Kg) | 83.94 ± 9.38 | 78.55 ± 8.92 | 75.25 ± 9.60 | 0.044 * | 0.127 |
| BMI (Kg/m2) | 23.71 ± 2.72 | 23.95 ± 2.71 | 23.85 ± 2.68 | 0.828 | 0.019 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Morais, N.; Ferreira, J.; Gordo, J.; Vilas-Boas, J.P.; Pascoal, A.G. A Diagonal Movement Pattern of Arm Elevation and Depression in Overhead Throwing Athletes: An Exploratory Kinematic Analysis for Clinical Application. Appl. Sci. 2023, 13, 10691. https://doi.org/10.3390/app131910691
Morais N, Ferreira J, Gordo J, Vilas-Boas JP, Pascoal AG. A Diagonal Movement Pattern of Arm Elevation and Depression in Overhead Throwing Athletes: An Exploratory Kinematic Analysis for Clinical Application. Applied Sciences. 2023; 13(19):10691. https://doi.org/10.3390/app131910691
Chicago/Turabian StyleMorais, Nuno, Joana Ferreira, Jéssica Gordo, João Paulo Vilas-Boas, and Augusto G. Pascoal. 2023. "A Diagonal Movement Pattern of Arm Elevation and Depression in Overhead Throwing Athletes: An Exploratory Kinematic Analysis for Clinical Application" Applied Sciences 13, no. 19: 10691. https://doi.org/10.3390/app131910691







