The Relationship between Dietary Intake and Adiposity in South African Female Adolescents: A Systematic Review
Abstract
:1. Introduction
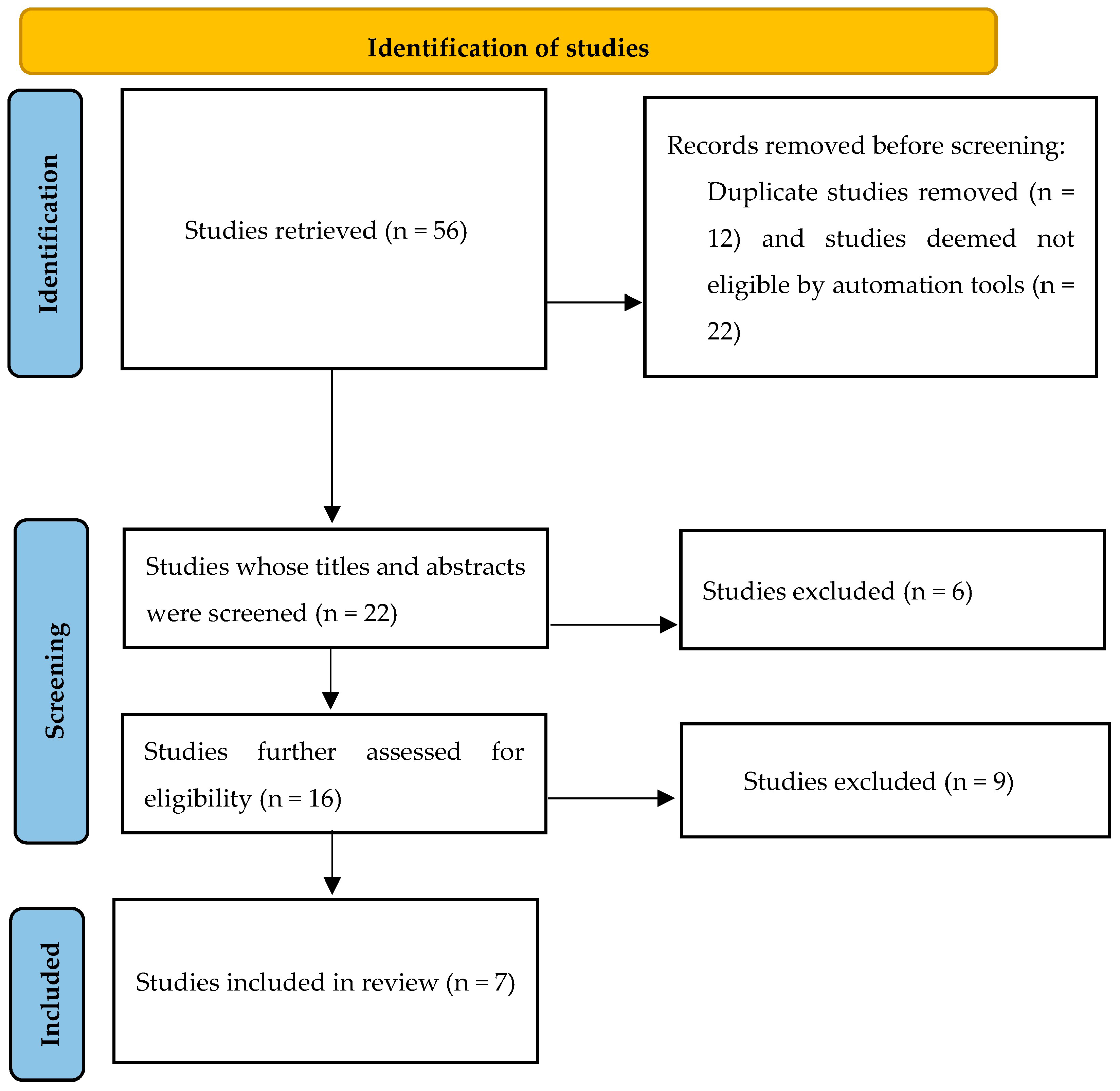
2. Materials and Method
2.1. Inclusion and Exclusion Criteria
2.2. Search Strategy
2.3. Definition of Terms
- Adiposity is an increase in body fat. This could be total body fat as indicated by BMI ≥ 25 kg/m2, central fat (WHR > 0.8 or WC > 88 cm), and fat deposits and accumulation in other regions of the body [4].
- Obesity is a state of being excessively overweight classified according to WHO Reference 2007 (5–19 years) BMI-for-age, where the +2 SD (equivalent to the 97th centile) coincides at 19 years with the adult’s cut-off of BMI = 30 kg/m2 [12].
- Nutrient intake or dietary intake or dietary patterns are used to refer to the combinations, amounts, variety, and frequency of different foods, beverage, and nutrients habitually consumed by an individual [13].
- Dietary practice refers to preference in food consumption or behaviours related to the ways in which individuals consume food, which can be classified as good or poor dietary practices [14].
2.4. Selection Process and Data Extraction
2.5. Data Analysis
3. Results
| Reference | Objective of Study | Study Population | No. of Subjects | Results | Observed Trends | Statistical Significance | Factors Implicated in Dietary/ Nutrient/Practice and Adiposity Link | Factors Corrected for in the Study |
|---|---|---|---|---|---|---|---|---|
| Pisa, Pedro, Kahn et al., 2015 [16] | To identify and explain the association between dietary diversity and socio-demographic factors, lifestyle factors, and BMI in rural black South African adolescents. | Adolescents aged between 11 and 15 years in Agincourt sub-district of Mpumalanga Province, South Africa | n = 388 | A positive and significant association was observed between BMI-for-age and animal driven nutrients, characterized by high positive loadings of nutrients from animal derived sources. No significant associations were observed between BMI-for-age Z scores and vitamins, fibre, vegetable oil nutrients, and plant derived nutrients. | Single mothers of adolescents, aged between 35 and 49 years were positively and significantly associated with a high intake of animal driven nutrients, while being in the lowest SES status tercile was negatively associated with the intake of animal driven nutrients. | p ≤ 0.05 | High animal driven nutrients were associated with increase in BMI for age Z scores. | Physical activity; educational level of mother. |
| Sedibe, Pisa, Feeley et al., 2018 [17] | To examine the existence of differences and/or similarities in the dietary practices of rural and urban adolescents in specific environments and their links with overweight and obesity. | The rural population was taken from Agincourt, a sub-district of Bushbuckridge, in the Mpumalanga province and the urban adolescent population was from Soweto, in Johannesburg, South African. | n = 3490 | Being from a rural setting was associated with a reduction in the risk of overweight and obesity among early-adolescents, while eating the main meal with family some days, and almost every day, and an irregular breakfast consumption on weekdays; were associated with increased risk of being overweight and obese. Irregular breakfast consumption on weekends among mid-adolescents was associated with an increased risk of being overweight and obese. | An increase in the frequency of irregular breakfast consumption during the week and weekends and eating the main meal with family “some days” and “almost every day”, was associated with an increases risk of overweight and obesity | p ≤ 0.05 | Breakfast, main meal with/without family, urban setting | Gender |
| Feeley, Musenge, Pettifor et al., 2012 [18] | To assess the relationship between dietary habits, change in socio-economic status and obesity (BMI and fat mass) in adolescents. | Black participants aged 13, 15, and 17 years participating in the Birth to Twenty (Bt20) study, living in Soweto-Johannesburg. | n = 1298 | A positive association was found between irregular breakfast consumption on weekends and obesity. | Increase in frequency of irregular breakfast consumption on weekends was associated with an increase in obesity. | p < 0.05 | Irregular breakfast consumption on weekends | Household assets. |
| Debeila, Modjadji and Madiba, 2021 [19] | To determine the prevalence of overweight/obesity and the association with selected factors amongst adolescents in rural high schools. | Adolescents from high schools at Fetakgomo Municipality in rural Limpopo Province, South Africa. | n = 378 | Overweight and obesity amongst adolescent girls was associated with the number of employed adults in the household, age, and sex, while eating breakfast reduced the risk. | Being an older adolescent girl, and living in a household with employed adults was associated with overweight/obesity. The overall overweight/obesity prevalence in this study was higher than the national range of 8.6–27.0% amongst adolescents aged 15–19 years reported by the United Nations Children’s Fund. | p < 0.05 | Eating breakfast, energy-dense and nutrient-poor (mainly based on starches). | |
| Kruger, Kruger and Macintyre, 2006 [20] | To investigate overweight status according to BMI and body fat percentage and identify the determinants of overweight and obesity among adolescent schoolchildren in a population in transition. | Schoolchildren aged 10- to 15-years in the North West Province, South Africa. | n = 1257 | Prevalence was higher in female white children, in urban areas, living in smaller households, and parents with low- or high-income occupations. Inactivity and increasing age in girls were found to be influential in the development of overweight/obesity. Being a female of post-menarche age was identified as a determinant of higher body fat content | Low activity levels, living in urban areas (towns/cities or informal settlements close to towns/cities) were associated with increases in overweight or obesity. There was also an association between exposure to a Western, urbanised lifestyle and an increase in the prevalence of obesity. | p < 0.05 | Consuming more fat for energy per day. High intake of cereal- or starch-based staple foods (maize meal, bread, rice), empty-kilojoule snack foods (cheese curls) and cold drinks, and low consumption of nutrient-dense foods (milk, meat, fruit, vegetables). | |
| Napier and Oldewage-Theron, 2015 [21] | To ascertain the food intake practices and nutritional status of female adolescents (14–18 year) and young women post school (19–28 years). | Adolescent girls (aged 14 to 18 years) and young women (aged 19 to 28) post-school living in informal settlements in the eThekwini municipal district, Durban, province of KwaZulu Natal. | n = 523 (adolescent girls n =156) | Of the adolescent girls, 43% were classified as possibly at risk of overweight, 12.8% were classified as overweight, and 1.9% were classified as obese. The diet consumed by the adolescents was reportedly low in dairy, fruit, and vegetables. As a result, nutrients for calcium in 27.6%, vitamin A in 70.9%, vitamin C in 46.7%, and Iron in 42.3% of the sample did not meet the Estimated Average Requirement (EA) for their age group. In addition, large number of the adolescents had inadequate intakes of energy (89,1%), and total dietary fibre (93.6%), and 25% of the adolescents had inadequate protein intake. | High consumption of the carbohydrate-rich and sugary food with a low milk, legume, vegetable, and fruit consumption. | p < 0.05 | High carbohydrate-rich and sugary food intake, and low milk, legume, vegetable, and fruit consumption. | Age |
| Kruger, Margetts and Vorster, 2004 [22] | To examine if any differences in body weight, subcutaneous skinfold thicknesses, and waist circumferences (body composition) exist between stunted and non-stunted girls. | African adolescent girls, of school going age (10 to 15 years), in the North West Province, South Africa | n = 478 | As a result of the high energy consumption, stunted girls had higher triceps skinfold (TSF) and subscapular skinfold thicknesses (SSF) compared to non-stunted girls. The TSF and SSF levels among the stunted adolescents were found to increase with increase in age. | At a given energy intake and level of physical activity, stunted adolescent girls were found to store more body fat than non-stunted girls, which increased for each year of ages. | p < 0.05 | Stunted girls had a higher dietary energy and macronutrient intakes, and the percentage contribution of each macronutrient per kilogram of body weight; however, it has been proposed that stunted children have lower energy requirements and should have lower total energy intakes than non-stunted children. | Adjustments for confounding factors such as dietary intake and physical activity. |
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tiwari, A.; Balasundaram, P. Public Health Considerations Regarding Obesity; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Moore, J.B. COVID-19, childhood obesity, and NAFLD: Colliding pandemics. Lancet Gastroenterol. Hepatol. 2022, 7, 499–501. [Google Scholar] [CrossRef] [PubMed]
- Abarca-Gómez, L.; Abdeen, Z.A.; Hamid, Z.A.; Abu-Rmeileh, N.M.; Acosta-Cazares, B.; Acuin, C.; Adams, R.J.; Aekplakorn, W.; Afsana, K.; Aguilar-Salinas, C.A.; et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Obesity and Overweight. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight#:~:text=In%202016%2C%2039%25%20of%20adults,tripled%20between%201975%20and%202016 (accessed on 22 August 2022).
- Ng, M.; Fleming, T.; Robinson, M.; Thomson, B.; Graetz, N.; Margono, C.; Mullany, E.C.; Biryukov, S.; Abbafati, C.; Abera, S.F.; et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014, 384, 766–781. [Google Scholar] [CrossRef] [PubMed]
- Seabi, T.M.; Wagner, R.G.; Norris, S.A.; Tollman, S.M.; Twine, R.; Dunger, D.B.; Kahn, K. Adolescents’ understanding of obesity: A qualitative study from rural South Africa. Glob. Health Action 2021, 14, 1968598. [Google Scholar] [CrossRef] [PubMed]
- Ford, N.D.; Patel, S.A.; Narayan, K.V. Obesity in low-and middle-income countries: Burden, drivers, and emerging challenges. Ann. Rev. Public Health 2017, 38, 145–164. [Google Scholar] [CrossRef] [PubMed]
- Sodjinou, R.; Agueh, V.; Fayomi, B.; Delisle, H. Obesity and cardio-metabolic risk factors in urban adults of Benin: Relationship with socio-economic status, urbanisation, and lifestyle patterns. BMC Public Health 2008, 8, 84. [Google Scholar] [CrossRef] [PubMed]
- Ajayi, I.O.; Adebamowo, C.; Adami, H.-O.; Dalal, S.; Diamond, M.B.; Bajunirwe, F.; Guwatudde, D.; Njelekela, M.; Nankya-Mutyoba, J.; Chiwanga, F.S.; et al. Urban–rural and geographic differences in overweight and obesity in four sub-Saharan African adult populations: A multi-country cross-sectional study. BMC Public Health 2016, 16, 1126. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gotzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef]
- World Health Organisation. Adolescent Health. 2015. Available online: http://www.who.int/topics/adolescent_health/en/ (accessed on 22 August 2022).
- Blössner, M.; Siyam, A.; Borghi, E.; Onyango, A.; De Onis, M. WHO AnthroPlus for Personal Computers Manual: Software for Assessing Growth of the World’s Children and Adolescents; World Health Organization: Geneva, Switzerland, 2009. [Google Scholar]
- Sánchez-Villegas, A.; Martínez-Lapiscina, E.H. A healthy diet for your heart and your brain. In The Prevention of Cardiovascular Disease through the Mediterranean Diet; ULPGC: Las Palmas, Spain, 2018; pp. 169–197. [Google Scholar]
- Worku, A.; Mekonnen Abebe, S.; Wassie, M.M. Dietary practice and associated factors among type 2 diabetic patients: A cross sectional hospital based study, Addis Ababa, Ethiopia. SpringerPlus 2015, 4, 15. [Google Scholar] [CrossRef]
- Academy of Nutrition and Dietetics. Evidence Analysis Manual: Steps in the Academy Evidence Analysis Process; Academy of Nutrition and Dietetics: Chicago, IL, USA, 2012; p. 111. [Google Scholar]
- Pisa, P.T.; Pedro, T.M.; Kahn, K.; Tollman, S.M.; Pettifor, J.M.; Norris, S.A. Nutrient patterns and their association with socio-demographic, lifestyle factors and obesity risk in rural South African adolescents. Nutrients 2015, 7, 3464–3482. [Google Scholar] [CrossRef]
- Sedibe, M.H.; Pisa, P.T.; Feeley, A.B.; Pedro, T.M.; Kahn, K.; Norris, S.A. Dietary habits and eating practices and their association with overweight and obesity in rural and urban black South African adolescents. Nutrients 2018, 10, 145. [Google Scholar] [CrossRef] [PubMed]
- Feeley, A.B.; Musenge, E.; Pettifor, J.M.; Norris, S.A. Investigation into longitudinal dietary behaviours and household socio-economic indicators and their association with BMI Z-score and fat mass in South African adolescents: The Birth to Twenty (Bt20) cohort. Public Health Nutr. 2013, 16, 693–703. [Google Scholar] [CrossRef] [PubMed]
- Debeila, S.; Modjadji, P.; Madiba, S. High prevalence of overall overweight/obesity and abdominal obesity amongst adolescents: An emerging nutritional problem in rural high schools in Limpopo Province, South Africa. Afr. J. Prim. Health Care Fam. Med. 2021, 13, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Kruger, R.; Kruger, H.; Macintyre, U. The determinants of overweight and obesity among 10- to 15-year-old schoolchildren in the North West Province, South Africa–the THUSA BANA (Transition and Health during Urbanisation of South Africans; BANA, children) study. Public Health Nutr. 2006, 9, 351–358. [Google Scholar] [CrossRef] [PubMed]
- Napier, C.; Oldewage-Theron, W. Dietary intake and nutritional status of adolescent girls and young women in Durban, South Africa. J. Consum. Sci. 2015, 43, 1–15. [Google Scholar]
- Kruger, H.S.; Margetts, B.M.; Vorster, H.H. Evidence for relatively greater subcutaneous fat deposition in stunted girls in the North West Province, South Africa, as compared with non-stunted girls. Nutrition 2004, 20, 564–569. [Google Scholar] [CrossRef] [PubMed]
- González-Álvarez, M.A.; Lázaro-Alquézar, A.; Simón-Fernández, M.B. Global trends in child obesity: Are figures converging? Int. J. Env. Res. Public Health. 2020, 17, 9252. [Google Scholar] [CrossRef]
- Kanter, R.; Caballero, B. Global gender disparities in obesity: A review. Adv. Nutr. 2012, 3, 491–498. [Google Scholar] [CrossRef]
- Jones-Smith, J.C.; Gordon-Larsen, P.; Siddiqi, A.; Popkin, B.M. Cross-national comparisons of time trends in overweight inequality by socioeconomic status among women using repeated cross-sectional surveys from 37 developing countries, 1989–2007. Am. J. Epidemiol. 2011, 173, 667–675. [Google Scholar] [CrossRef]
- Swinburn, B.A.; Sacks, G.; Hall, K.D.; McPherson, K.; Finegood, D.T.; Moodie, M.L.; Gortmaker, S.L. The global obesity pandemic: Shaped by global drivers and local environments. Lancet 2011, 378, 804–814. [Google Scholar] [CrossRef]
- Pisa, P.T.; Pisa, N.; Chikandiwa, P.; Chikandiwa, A. Economic growth as an underlying probable systemic driver for childhood obesity in South Africa: A Joinpoint regression and ecological analysis over 10 years. S. Afr. Med. J. 2021, 111, 220–226. [Google Scholar] [CrossRef] [PubMed]
- Pisa, P.T.; Pisa, N.M. Economic growth and obesity in South African adults: An ecological analysis between 1994 and 2014. Eur. J. Public Health 2017, 27, 404–409. [Google Scholar] [CrossRef]
- Popkin, B.M.; Adair, L.S.; Ng, S.W. Global nutrition transition and the pandemic of obesity in developing countries. Nutr. Rev. 2012, 70, 3–21. [Google Scholar] [CrossRef] [PubMed]
- Denova-Gutiérrez, E.; Castanon, S.; Talavera, J.O.; Flores, M.; Macias, N.; Rodríguez-Ramírez, S.; Flores, Y.N.; Salmerón, J. Dietary patterns are associated with different indexes of adiposity and obesity in an urban Mexican population. J. Nutr. 2011, 141, 921–927. [Google Scholar] [CrossRef] [PubMed]
- Magarey, A.; Daniels, L.; Boulton, T.; Cockington, R. Does fat intake predict adiposity in healthy children and adolescents aged 2–15 y? A longitudinal analysis. Eur. J. Clin. Nutr. 2001, 55, 471–481. [Google Scholar] [CrossRef] [PubMed]
- Baxter-Jones, A.D.; Faulkner, R.A.; Forwood, M.R.; Mirwald, R.L.; Bailey, D.A. Bone mineral accrual from 8 to 30 years of age: An estimation of peak bone mass. J. Bone Miner. Res. 2011, 26, 1729–1739. [Google Scholar] [CrossRef] [PubMed]
- Reilly, J.J.; Kelly, J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: Systematic review. Int. J. Obes. 2011, 35, 891–898. [Google Scholar] [CrossRef]
- Lobstein, T.; Baur, L.; Uauy, R. Obesity in children and young people: A crisis in public health. Report to the World Health Organization by the International Obesity Task Force. Obes. Rev. 2005, 5, 5–104. [Google Scholar]
- Wachira, L.-J.; Muthuri, S.; Ochola, S.; Onywera, V.; Tremblay, M. Association between dietary behaviours and weight status of school children: Results from the International Study of Childhood Obesity, Lifestyle and the Environment (ISCOLE)-Kenya. Child Adolesc. Obes. 2021, 4, 1–22. [Google Scholar] [CrossRef]
- Hruby, A.; Hu, F.B. The epidemiology of obesity: A big picture. Pharmacoeconomics 2015, 33, 673–689. [Google Scholar] [CrossRef]
- Peltzer, K.; Pengpid, S. Overweight and obesity and associated factors among school-aged adolescents in Ghana and Uganda. Int. J. Environ. Res. Public Health 2011, 8, 3859–3870. [Google Scholar]
- Kimani-Murage, E.W.; Kahn, K.; Pettifor, J.M.; Tollman, S.M.; Dunger, D.B.; Gómez-Olivé, X.F.; Norris, S.A. The prevalence of stunting, overweight and obesity, and metabolic disease risk in rural South African children. BMC Public Health 2010, 10, 158. [Google Scholar] [CrossRef] [PubMed]
- Smetanina, N.; Albaviciute, E.; Babinska, V.; Karinauskiene, L.; Albertsson-Wikland, K.; Petrauskiene, A.; Verkauskiene, R. Prevalence of overweight/obesity in relation to dietary habits and lifestyle among 7–17 years old children and adolescents in Lithuania. BMC Public Health 2015, 15, 1001. [Google Scholar] [CrossRef] [PubMed]
- Keats, E.C.; Rappaport, A.I.; Shah, S.; Oh, C.; Jain, R.; Bhutta, Z.A. The dietary intake and practices of adolescent girls in low-and middle-income countries: A systematic review. Nutrients 2018, 10, 1978. [Google Scholar] [CrossRef] [PubMed]
- Lin, X.; Li, H. Obesity: Epidemiology, pathophysiology, and therapeutics. Front. Endocrinol. 2021, 12, 706978. [Google Scholar] [CrossRef] [PubMed]
- Sahoo, K. Bishnupriya Sahoo, 2 Ashok Kumar Choudhury, 3 Nighat Yasin Sofi, 4 Raman Kumar and Ajeet Singh Bhadoria. Childhood obesity: Causes and consequences. J. Fam. Med. Prim. Care 2015, 4, 187–192. [Google Scholar]
- Golay, A.; Bobbioni, E. The role of dietary fat in obesity. Int. J. Obes. Relat. Metab. Disord. 1997, 21, S2–S11. [Google Scholar] [PubMed]
- Sacks, F.M.; Bray, G.A.; Carey, V.J.; Smith, S.R.; Ryan, D.H.; Anton, S.D.; McManus, K.; Champagne, C.M.; Bishop, L.M.; Laranjo, N.; et al. Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates. N. Engl. J. Med. 2009, 360, 859–873. [Google Scholar] [CrossRef]
- Gray, L.A.; Hernandez Alava, M.; Kelly, M.P.; Campbell, M.J. Family lifestyle dynamics and childhood obesity: Evidence from the millennium cohort study. BMC Public Health 2018, 18, 500. [Google Scholar] [CrossRef]
- Kunin-Batson, A.S.; Seburg, E.M.; Crain, A.L.; Jaka, M.M.; Langer, S.L.; Levy, R.L.; Sherwood, N.E. Household factors, family behavior patterns, and adherence to dietary and physical activity guidelines among children at risk for obesity. J. Nutr. Educ. Behav. 2015, 47, 206–215.e1. [Google Scholar] [CrossRef]
- Noonan, R.J. Poverty, weight status, and dietary intake among UK adolescents. Int. J. Env. Res. Public Health 2018, 15, 1224. [Google Scholar] [CrossRef] [PubMed]
- Poulsen, P.H.; Biering, K.; Winding, T.N.; Nohr, E.A.; Andersen, J.H. How does childhood socioeconomic position affect overweight and obesity in adolescence and early adulthood: A longitudinal study. BMC Obes. 2018, 5, 34. [Google Scholar] [CrossRef] [PubMed]
- Gilliland, J.A.; Rangel, C.Y.; Healy, M.A.; Tucker, P.; Loebach, J.E.; Hess, P.M.; He, M.; Irwin, J.D.; Wilk, P. Linking childhood obesity to the built environment: A multi-level analysis of home and school neighbourhood factors associated with body mass index. Can. J. Public Health 2012, 103, S15–S21. [Google Scholar] [CrossRef] [PubMed]
- Micklesfield, L.K.; Pedro, T.M.; Kahn, K.; Kinsman, J.; Pettifor, J.M.; Tollman, S.; Norris, S.A. Physical activity and sedentary behavior among adolescents in rural South Africa: Levels, patterns and correlates. BMC Public Health 2014, 14, 40. [Google Scholar] [CrossRef] [PubMed]
- Mokabane, M.; Mashao, M.M.; van Staden, M.; Potgieter, M.; Potgieter, A. Low levels of physical activity in female adolescents cause overweight and obesity: Are our schools failing our children? S.Afr. Med. 2014, 104, 665–667. [Google Scholar] [CrossRef] [PubMed]
- Spinelli, S.; Monteleone, E. Food Preferences and Obesity. Endocrinol. Metab. 2021, 36, 209–219. [Google Scholar] [CrossRef] [PubMed]
- Patterson, R.E. CHAPTER 4—Overview of Nutritional Epidemiology. In Nutrition in the Prevention and Treatment of Disease; Coulston, A.M., Rock, C.L., Monsen, E.R., Eds.; Academic Press: San Diego, CA, USA, 2001; pp. 59–68. [Google Scholar]
- Potischman, N. Biologic and methodologic issues for nutritional biomarkers. J. Nutr. 2003, 133 (Suppl. S3), 875S–880S. [Google Scholar] [CrossRef]
- Shim, J.S.; Oh, K.; Kim, H.C. Dietary assessment methods in epidemiologic studies. Epidemiol. Health 2014, 36, e2014009. [Google Scholar] [CrossRef]
- Reedy, J.; Subar, A.F.; George, S.M.; Krebs-Smith, S.M. Extending Methods in Dietary Patterns Research. Nutrients 2018, 10, 571. [Google Scholar] [CrossRef]
- Hassan, S.; Oladele, C.; Galusha, D.; Adams, O.P.; Maharaj, R.G.; Nazario, C.M.; Nunez, M.; Nunez-Smith, M. Anthropometric measures of obesity and associated cardiovascular disease risk in the Eastern Caribbean Health Outcomes Research Network (ECHORN) Cohort Study. BMC Public Health 2021, 21, 399. [Google Scholar] [CrossRef]
- Boachie, M.K.; Thsehla, E.; Immurana, M.; Kohli-Lynch, C.; Hofman, K.J. Estimating the healthcare cost of overweight and obesity in South Africa. Glob. Health Action 2022, 15, 2045092. [Google Scholar] [CrossRef]
- Sharma, M.; Branscum, P. Novel and emerging approaches to combat adolescent obesity. Adolesc. Health Med. Ther. 2010, 1, 9–19. [Google Scholar] [CrossRef]
- Erzse, A.; Abdool Karim, S.; Rwafa, T.; Kruger, P.; Hofman, K.; Foley, L.; Oni, T.; Goldstein, S. Participatory prioritisation of interventions to improve primary school food environments in Gauteng, South Africa. BMC Public Health 2023, 23, 1263. [Google Scholar] [CrossRef]
- Devereux, S.; Hochfeld, T.; Karriem, A.; Mensah, C.; Morahanye, M.; Msimango, T.; Mukubonda, A.; Naicker, S.; Nkomo, G.; Sanders, D. School Feeding in South Africa: What We Know, What We Don’t Know: DST-NRF Centre of Excellence in Food Security; Food Security SA Working Paper Series; COE: Huntsville, AL, USA, 2018. [Google Scholar]
- Qila, V.; Tyilo, N. Implementing National School Nutrition Programme (NSNP): How Involved are the Stakeholders? Mediterr. J. Soc. Sci. 2014, 5, 381–390. [Google Scholar] [CrossRef]
- Reddy, P.; Dukhi, N.; Sewpaul, R.; Ellahebokus, M.A.A.; Kambaran, N.S.; Jobe, W. Mobile Health Interventions Addressing Childhood and Adolescent Obesity in Sub-Saharan Africa and Europe: Current Landscape and Potential for Future Research. Front. Public Health 2021, 9, 604439. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vilakazi, N.; Mathunjwa, S.; Legodi, H.; Pisa, P.T. The Relationship between Dietary Intake and Adiposity in South African Female Adolescents: A Systematic Review. Appl. Sci. 2023, 13, 10813. https://doi.org/10.3390/app131910813
Vilakazi N, Mathunjwa S, Legodi H, Pisa PT. The Relationship between Dietary Intake and Adiposity in South African Female Adolescents: A Systematic Review. Applied Sciences. 2023; 13(19):10813. https://doi.org/10.3390/app131910813
Chicago/Turabian StyleVilakazi, Nokuthula, Sithabile Mathunjwa, Heather Legodi, and Pedro Terrence Pisa. 2023. "The Relationship between Dietary Intake and Adiposity in South African Female Adolescents: A Systematic Review" Applied Sciences 13, no. 19: 10813. https://doi.org/10.3390/app131910813





