Possibilities of Ultrasound Examination in the Assessment of Age-Related Changes in the Soft Tissues of the Face and Neck: A Review
Abstract
:1. Introduction
1.1. Ultrasound Diagnostics in Dermatology and Cosmetology
1.2. Ultrasound Diagnostics in Maxillofacial Surgery
1.3. Ultrasound Diagnostics in Aesthetic Surgery of the Face and Neck
2. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Iyengar, S.; Makin, I.R.; Sadhwani, D.; Moon, E.; Yanes, A.F.; Geisler, A.; Silapunt, S.; Servaes, S.; Weil, A.; Poon, E.; et al. Utility of a High-Resolution Superficial Diagnostic Ultrasound System for Assessing Skin Thickness: A Cross-Sectional Study. Dermatol. Surg. 2018, 44, 855–864. [Google Scholar] [CrossRef]
- Vachiramon, V.; Techakajornkeart, R.; Leerunyakul, K.; Chayavichitsilp, P. Accuracy of a high-intensity focused ultrasound device with and without real-time visualization system in face and neck treatment of skin laxity. J. Cosmet. Dermatol. 2021, 20, 132–137. [Google Scholar] [CrossRef] [PubMed]
- Chammas, M.C.; Takahashi, M.S.; Moyses, R.; Pompeia, C.; Tavares, M.R.; Cerri, G.G. Correction: Ultrasonography in the Assessment of Tumors of the Cheek: Water Mouth Distension Technique. Ultraschall Med. 2022. [Google Scholar] [CrossRef] [PubMed]
- Wortsman, X. Top Advances in Dermatologic Ultrasound. J. Ultrasound Med. 2022. [Google Scholar] [CrossRef] [PubMed]
- Crisan, D.; Wortsman, X.; Alfageme, F.; Catalano, O.; Badea, A.; Scharffetter-Kochanek, K.; Sindrilaru, A.; Crisan, M. Ultrasonography in dermatologic surgery: Revealing the unseen for improved surgical planning. J. Dtsch. Dermatol. Ges. 2022, 20, 913–926. [Google Scholar] [CrossRef]
- Pescarini, E.; Butler, D.P.; Perusseau-Lambert, A.; Nduka, C.; Kannan, R.Y. Targeted chemodenervation of the posterior belly of the digastric muscle for the management of jaw discomfort in facial synkinesis. J. Plast. Reconstr. Aesthet. Surg. 2021, 12, 3437–3442. [Google Scholar] [CrossRef] [PubMed]
- Bengtson, B.P.; Eaves, F.F. High-resolution ultrasound in the detection of silicone gel breast implant shell failure: Background, in vitro studies, and early clinical results. Aesthetic Surg. J. 2012, 32, 157–174. [Google Scholar] [CrossRef] [Green Version]
- Javaid, I.; Tazeen, A.; Khadija, S.; Fatima, Z.; Saleem, M.A.; Fatima, M.; Rubab, U. Evaluation of blood flow in superficial arteries of face by Doppler ultrasound in young adults: Blood Flow in Superficial Arteries of Face by Doppler Ultrasound. Pak. BioMed. J. 2022, 5, 165–168. [Google Scholar] [CrossRef]
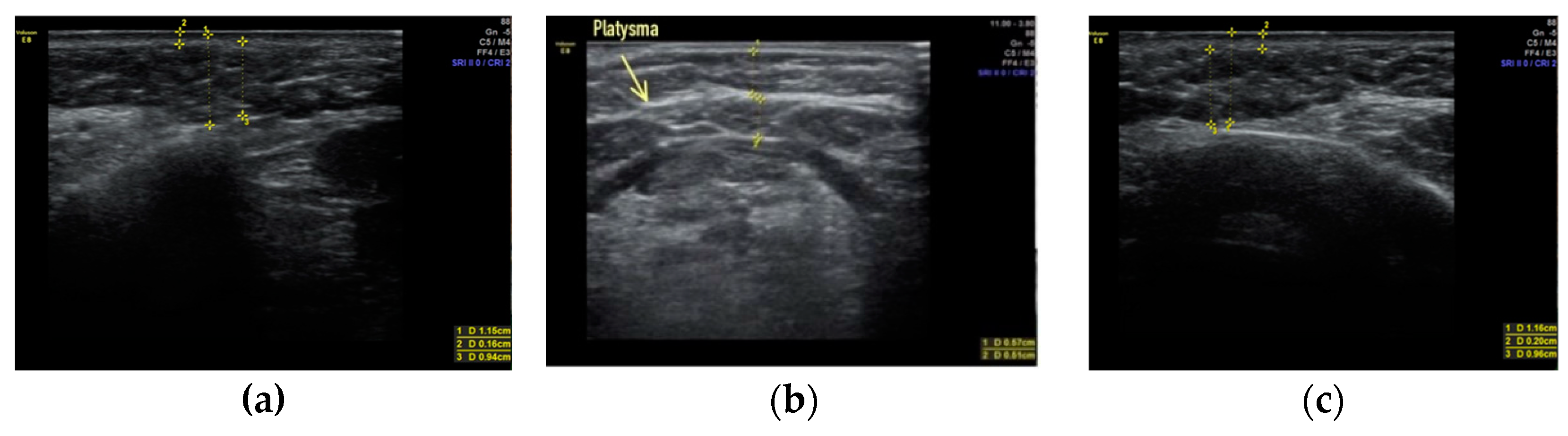
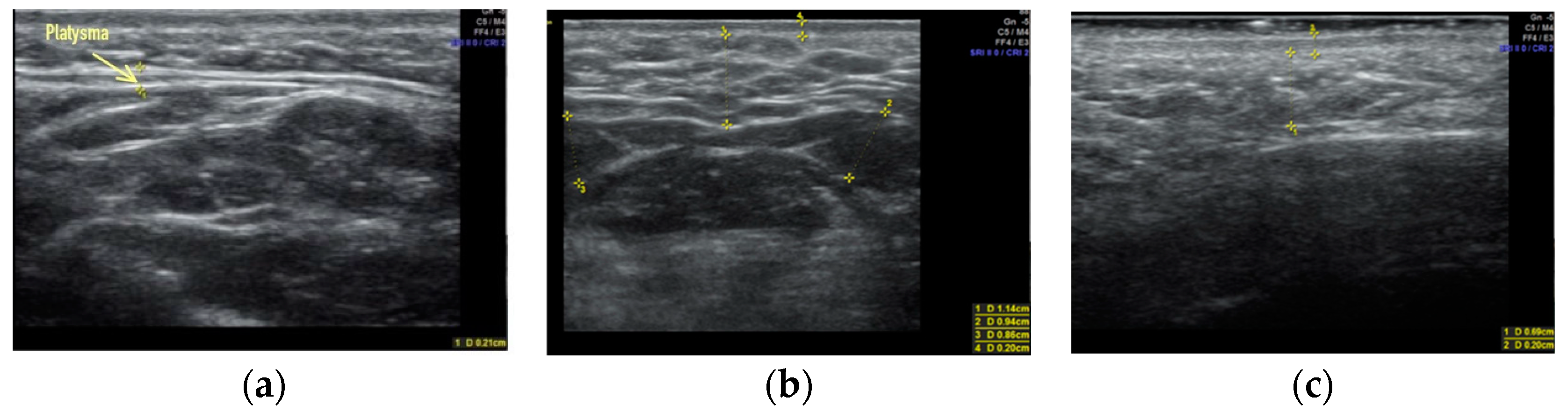
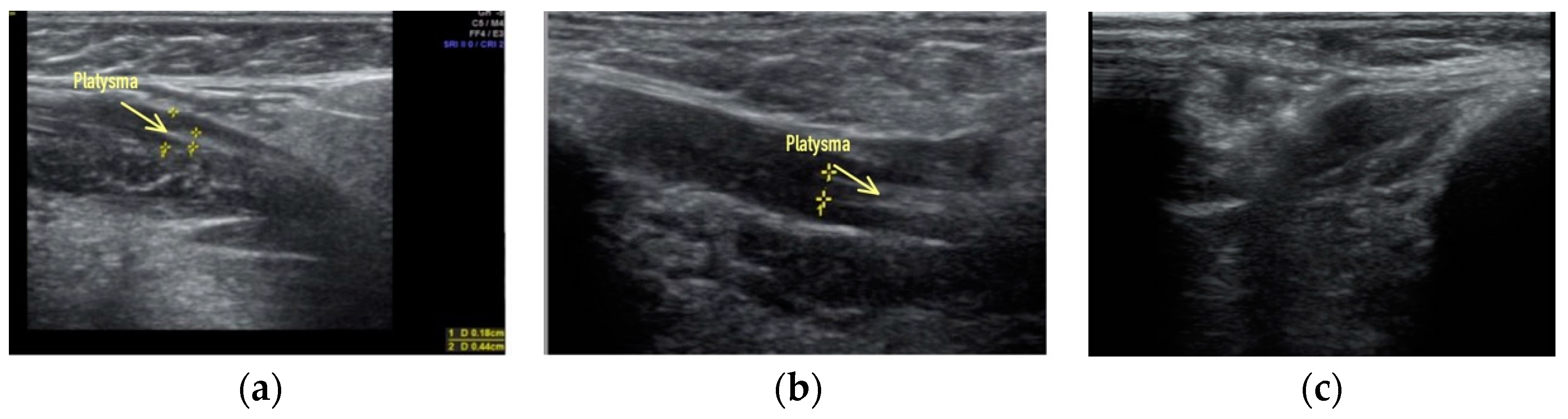
- Sharobaro, V.; Alimova, S.; Telnova, A.; Shamanaeva, L. Ultrasound diagnosis of age-related involutional changes in the lower third of face and neck to determine treatment techniques. Pak. J. Med. Sci. 2021, 37, 272–276. [Google Scholar] [CrossRef]
- Abraham, M.T.; Klimczak, J.A.; Abraham-Aggarwal, M. Comparing Lateral Rhytidectomy With and Without Neck Suture Suspension. Plast. Surg. 2021. [Google Scholar] [CrossRef]
- Casabona, G.; Frank, K.; Koban, K.C.; Schenck, T.L.; Lopez, V.P.; Webb, K.L.; Hamade, H.; Freytag, D.L.; Green, J.B.; Cotofana, S. Influence of Age, Sex, and Body Mass Index on the Depth of the Superficial Fascia in the Face and Neck. Dermatol. Surg. 2019, 45, 1365–1373. [Google Scholar] [CrossRef]
- Altman, A.; Sin, Z.; Tran, E.D.; Nguyen, J.; Mowlavi, A. The Effect of Extended SMAS Face-lift on Earlobe Ptosis and Pseudoptosis. Am. J. Cosmet. Surg. 2022, 39, 190–195. [Google Scholar] [CrossRef]
- Kutter, O.; Shams, R.; Navab, N. Visualization and GPU-accelerated simulation of medical ultrasound from CT images. Comput. Methods Programs Biomed. 2009, 94, 250–266. [Google Scholar] [CrossRef]
- Choi, D.Y.; Bae, H.; Bae, J.H.; Kim, H.J.; Hu, K.S. Effective Locations for Injecting Botulinum Toxin into the Mentalis Muscle; Cadaveric and Ultrasonographic Study. Toxins 2021, 13, 96. [Google Scholar] [CrossRef]
- Yang, Y.; Wang, L.; Yan, F.; Xiang, X.; Tang, Y.; Zhang, L.; Liu, J.; Qiu, L. Determination of Normal Skin Elasticity by Using Real-time Shear Wave Elastography. J. Ultrasound Med. 2018, 37, 2507–2516. [Google Scholar] [CrossRef] [Green Version]
- Dybiec, E.; Pietrzak, A.; Adamczyk, M.; Michalska-Jakubus, M.; Wawrzycki, B.; Lotti, T.; Rutkowski, P.; Krasowska, D. High frequency ultrasonography of the skin and its role as an auxillary tool in diagnosis of benign and malignant cutaneous tumors--a comparison of two clinical cases. Acta Dermatovenerol. Croat. 2015, 23, 43–47. [Google Scholar]
- Alexander, H.; Miller, D.L. Determining skin thickness with pulsed ultrasound. J. Investig. Dermatol. 1979, 72, 17–19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Volk, G.F.; Sauer, M.; Pohlmann, M.; Guntinas-Lichius, O. Reference values for dynamic facial muscle ultrasonography in adults. Muscle Nerve 2014, 50, 348–357. [Google Scholar] [CrossRef] [PubMed]
- Migda, M.S.; Migda, M.; Słapa, R.; Mlosek, R.K.; Migda, B. The use of high-frequency ultrasonography in the assessment of selected female reproductive structures: The vulva, vagina and cervix. J. Ultrason. 2019, 19, 261–268. [Google Scholar] [CrossRef]
- Kehrer, A.; Ruewe, M.; Platz Batista da Silva, N.; Lonic, D.; Heidekrueger, P.I.; Knoedler, S.; Jung, E.M.; Prantl, L.; Knoedler, L. Using High-Resolution Ultrasound to Assess Post-Facial Paralysis Synkinesis—Machine Settings and Technical Aspects for Facial Surgeons. Diagnostics 2022, 12, 1650. [Google Scholar] [CrossRef] [PubMed]
- Mlosek, R.K.; Migda, B.; Migda, M. High-frequency ultrasound in the 21st century. J. Ultrason. 2021, 20, e233–e241. [Google Scholar] [CrossRef]
- Alfageme, F.; Wortsman, X.; Catalano, O.; Roustan, G.; Crisan, M.; Crisan, D.; Gaitini, D.E.; Cerezo, E.; Badea, R. European Federation of Societies for Ultrasound in Medicine and Biology (EFSUMB) Position Statement on Dermatologic Ultrasound. Ultraschall Med. 2021, 42, 39–47. [Google Scholar] [CrossRef] [PubMed]
- Jenssen, C.; Gilja, O.; Serra, A.; Piscaglia, F.; Dietrich, C.; Rudd, L.; Sidhu, P. European Federation of Societies for Ultrasound in Medicine and Biology (EFSUMB) Policy Document Development Strategy—Clinical Practice Guidelines, Position Statements and Technological Reviews. Ultrasound Int. Open 2019, 5, E2–E10. [Google Scholar] [CrossRef] [Green Version]
- Wortsman, X.; Alfageme, F.; Roustan, G.; Arias-Santiago, S.; Martorell, A.; Catalano, O.; Scotto di Santolo, M.; Zarchi, K.; Bouer, M.; Gonzalez, C.; et al. Guidelines for Performing Dermatologic Ultrasound Examinations by the DERMUS Group. J. Ultrasound Med. 2016, 35, 577–580. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Niu, Z.; Wang, Y.; Zhu, Q.; Liu, J.; Liu, Y.; Jin, H. The value of high-frequency ultrasonography in the differential diagnosis of early mycosis fungoides and inflammatory skin diseases: A case-control study. Skin Res. Technol. 2021, 27, 453–460. [Google Scholar] [CrossRef]
- Wortsman, X. Ultrasound in Dermatology: Why, How, and When? Semin. Ultrasound CT MR 2013, 34, 177–195. [Google Scholar] [CrossRef] [Green Version]
- Polanska, A.; Dannczak-Pazdrowska, A.; Jalowska, M.; Zaba, R.; Adamski, Z. Current applications of high-frequency ultrasonography in dermatology. Postepy Dermatol. Alergol. 2017, 34, 535–542. [Google Scholar] [CrossRef] [PubMed]
- Quezada-Gaon, N.; Wortsman, X.; Penaloza, O.; Carrasco, J.E. Comparison of clinical marking and ultrasound-guided injection of Botulinum type A toxin into the masseter muscles for treating bruxism and its cosmetic effects. J. Cosmet. Dermatol. 2016, 15, 238–244. [Google Scholar] [CrossRef]
- Wu, W.-T.; Chang, K.-V.; Chang, H.-C.; Chen, L.-R.; Kuan, C.-H.; Kao, J.-T.; Wei, L.-Y.; Chen, Y.-J.; Han, D.-S.; Ozcakar, L. Ultrasound Imaging of the Facial Muscles and Relevance with Botulinum Toxin Injections: A Pictorial Essay and Narrative Review. Toxins 2022, 14, 101. [Google Scholar] [CrossRef]
- Reddy, S.; Nguyen, T.A.; Gharavi, N. Complications associated with infraorbital filler injection. J. Cosmet. Laser Ther. 2020, 22, 226–229. [Google Scholar] [CrossRef]
- Safran, T.; Swift, A.; Cotofana, S.; Nikolis, A. Evaluating safety in hyaluronic acid lip injections. Expert Opin. Drug Saf. 2021, 20, 1473–1486. [Google Scholar] [CrossRef] [PubMed]
- Skrzypek, E.; Górnicka, B.; Skrzypek, D.M.; Krzysztof, M.R. Granuloma as a complication of polycaprolactone-based dermal filler injection: Ultrasound and histopathology studies. J. Cosmet. Laser Ther. 2019, 21, 65–68. [Google Scholar] [CrossRef] [PubMed]
- Waller, J.M.; Maibach, H.I. Age and skin structure and function, a quantitative approach (I): Blood flow, pH, thickness, and ultrasound echogenicity. Skin Res. Technol. 2005, 11, 221–235. [Google Scholar] [CrossRef]
- Wortsman, X.; Wortsman, J.; Orlandi, C.; Cardenas, G.; Sazunic, I.; Jemec, G.B. Ultrasound detection and identification of cosmetic fillers in the skin. J. Eur. Acad. Dermatol. Venereol. 2012, 26, 292–301. [Google Scholar] [CrossRef] [PubMed]
- Schelke, L.W.; Van Den Elzen, H.J.; Erkamp, P.P.; Neumann, H.A. Use of ultrasound to provide overall information on facial fillers and surrounding tissue. Dermatol. Surg. 2010, 36, 1843–1851. [Google Scholar] [CrossRef] [PubMed]
- Bousquet-Rouaud, R.; Bazan, M.; Chaintreuil, J.; Echague, A. High-frequency ultrasound evaluation of cellulite treated with the 1064 nm Nd:YAG laser. J. Cosmet. Laser Ther. 2009, 11, 34–44. [Google Scholar] [CrossRef]
- Mlosek, R.K.; Dębowska, R.M.; Lewandowski, M.; Malinowska, S.; Nowicki, A.; Eris, I. Imaging of the skin and subcutaneous tissue using classical and high-frequency ultrasonographies in anti-cellulite therapy. Skin Res. Technol. 2011, 17, 461–468. [Google Scholar] [CrossRef]
- Kerscher, M.J.; Korting, H.C. Topical glucocorticoids of the non-fluorinated double-ester type. Lack of atrophogenicity in normal skin as assessed by high-frequency ultrasound. Acta Derm. Venereol. 1992, 72, 214–216. [Google Scholar]
- Polanska, A.; Jenerowicz, D.; Paszynska, E.; Zaba, R.; Adamski, Z.; Danczak-Pazdrowska, A. High-Frequency Ultrasonography-Possibilities and Perspectives of the Use of 20 MHz in Teledermatology. Front. Med. 2021, 8, 619965. [Google Scholar] [CrossRef]
- Jasaitiene, D.; Valiukeviciene; Linkeviciute, G.S.; Raisutis, R.; Jasiuniene, E.; Kazys, R. Principles of high-frequency ultrasonography for investigation of skin pathology. J. Eur. Acad. Dermatol. Venereol. 2011, 25, 375–382. [Google Scholar] [CrossRef]
- Carvalho, C.P.; Costa-Júnior, J.F.S.; Ferreira da Silva, F.F.; DAgostinho, J.G.; Kruger, M.A.V.; Pereira, W.C.A. Using high-resolution ultrasound imaging to characterize dermal striae in human skin. Skin Res. Technol. 2020, 26, 465–475. [Google Scholar] [CrossRef]
- Cammarota, T.; Pinto, F.; Magliaro, A.; Sarno, A. Current uses of diagnostic high-frequency US in dermatology. Eur. J. Radiol. 1998, 27, 215–223. [Google Scholar] [CrossRef]
- Polanska, A.; Silny, W.; Jenerowicz, D.; Kniola, K.; Molinska-Glura, M.; Danczak-Pazdrowska, A. Monitoring of therapy in atopic dermatitis--observations with the use of high-frequency ultrasonography. Skin Res. Technol. 2015, 21, 35–40. [Google Scholar] [CrossRef]
- Izzetti, R.; Vitali, S.; Aringhieri, G.; Nisi, M.; Oranges, T.; Dini, V.; Ferro, F.; Baldini, C.; Romanelli, M.; Caramella, D.; et al. Ultra-High Frequency Ultrasound, A Promising Diagnostic Technique: Review of the Literature and Single-Center Experience. Can. Assoc. Radiol. J. 2021, 72, 418–431. [Google Scholar] [CrossRef]
- Meikle, B.; Kimble, R.M.; Tyack, Z. Ultrasound measurements of pathological and physiological skin thickness: A scoping review protocol. BMJ Open 2022, 12, e056720. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Shan, J.L.; Chen, H.Y.; Wu, Z.F. Comparison of 2-D shear wave elastography with clinical score in localized scleroderma: A new method to increase the diagnostic accuracy. J. Dermatol. 2019, 46, 131–138. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Yan, F.; Yang, Y.; Xiang, X.; Qiu, L. Quantitative Assessment of Skin Stiffness in Localized Scleroderma Using Ultrasound Shear-Wave Elastography. Ultrasound Med. Biol. 2017, 43, 1339–1347. [Google Scholar] [CrossRef] [PubMed]
- Jia, K.; Li, H.; Wu, X.; Xu, C.; Xue, H. The Value of High-Resolution Ultrasound Combined with Shear-Wave Elastography under Artificial Intelligence Algorithm in Quantitative Evaluation of Skin Thickness in Localized Scleroderma. Comput. Intell. Neurosci. 2022, 2022, 1613783. [Google Scholar] [CrossRef]
- Asano, Y.; Fujimoto, M.; Ishikawa, O.; Sato, S.; Jinnin, M.; Takehara, K.; Hasegawa, M.; Yamamoto, T.; Ihn, H. Diagnostic criteria, severity classification and guidelines of localized scleroderma. J. Dermatol. 2018, 45, 755–780. [Google Scholar] [CrossRef] [Green Version]
- Schmid-Wendtner, M.H.; Dill-Müller, D. Ultrasound technology in dermatology. Semin. Cutan. Med. Surg. 2008, 27, 44–51. [Google Scholar] [CrossRef]
- Wortsman, X.; Wortsman, J.; Sazunic, I.; Carreño, L. Activity assessment in morphea using color Doppler ultrasound. J. Am. Acad. Dermatol. 2011, 65, 942–948. [Google Scholar] [CrossRef]
- Kinoshita-Ise, M.; Ohyama, M.; Ramjist, J.M.; Foster, F.S.; Yang, V.X.D.; Sachdeva, M.; Sade, S.; Shear, N.H. Ultra high-frequency ultrasound with seventy-MHz transducer in hair disorders: Development of a novel noninvasive diagnostic methodology. J. Dermatol. Sci. 2021, 102, 167–176. [Google Scholar] [CrossRef] [PubMed]
- Dill-Muller, D.; Maschke, J. Ultrasonography in dermatology. J. Dtsch. Dermatol. Ges. 2007, 5, 689–707. [Google Scholar] [CrossRef]
- Bhatta, A.K.; Keyal, U.; Liu, Y. Application of high frequency ultrasound in dermatology. DiscovMed 2018, 26, 237–242. [Google Scholar]
- Chai, K.; Zhu, R.; Luo, F.; Shi, Y.; Liu, M.; Xiao, Y.; Xiao, R. Updated Role of High-frequency Ultrasound in Assessing Dermatological Manifestations in Autoimmune Skin Diseases. Acta Derm. Venereol. 2022, 102, adv00765. [Google Scholar] [CrossRef]
- Bungardean, R.M.; Şerbanescu, M.S.; Colosi, H.A.; Crisan, M. High-frequency ultrasound: An essential non-invasive tool for the pre-therapeutic assessment of basal cell carcinoma. Rom. J. Morphol. Embryol. 2021, 62, 545–551. [Google Scholar] [CrossRef] [PubMed]
- Pellacani, G.; Seidenari, S. Preoperative melanoma thickness determination by 20-MHz sonography and digital videomicroscopy in combination. Arch. Dermatol. 2003, 139, 293–298. [Google Scholar] [CrossRef] [Green Version]
- Volk, G.F.; Leier, C.; Guntinas-lichius, O. Correlation between electromyography and quantitative ultrasonography of facial muscles in patients with facial palsy. Muscle Nerve 2016, 53, 755–761. [Google Scholar] [CrossRef] [PubMed]
- Sigaux, N.; Viremouneix, L.; Guibaud, L.; Breton, P. Malformations veineuses superficielles cervico-faciales. Mise au point [Head and neck superficial venous malformations]. Rev. Stomatol. Chir. Maxillofac. Chir. Orale 2015, 116, 201–208. [Google Scholar] [CrossRef]
- Nokovitch, L.; Peyrachon, B.; Chaux-Bodard, A.-G.; Poupart, M.; Roux, P.-E.; Devauchelle, B.; Deneuve, S. Reverse blood flow in cervicofacial veins after venous ligations: Potential implications in microsurgery. J. Plast. Reconstr. Aesthetic Surg. 2021, 74, 2042–2049. [Google Scholar] [CrossRef]
- Alfen, N.V.; Gilhuis, H.J.; Keijzers, J.P.; Pillen, S.; Van Dijk, J.P. Quantitative facial muscle ultrasound: Feasibility and reproducibility. Muscle Nerve 2013, 48, 375–380. [Google Scholar] [CrossRef] [PubMed]
- Volk, G.F.; Pohlmann, M.; Sauer, M.; Finkensieper, M.; Guntinas-Lichius, O. Quantitative ultrasonography of facial muscles in patients with chronic facial palsy. Muscle Nerve 2014, 50, 358–365. [Google Scholar] [CrossRef]
- Wortsman, X.; Ferreira-Wortsman, C.; Quezada, N. Facial Ultrasound Anatomy for Noninvasive Cosmetic and Plastic Surgery Procedures. In Atlas of Dermatologic Ultrasound; Springer: Cham, Switzerland, 2018; pp. 147–178. [Google Scholar] [CrossRef]
- Shadfar, S.; Perkins, S.W. Anatomy and physiology of the aging neck. Facial Plast. Surg. Clin. N. Am. 2014, 22, 161–170. [Google Scholar] [CrossRef]
- Luu, N.N.; Friedman, O. Facelift Surgery: History, Anatomy, and Recent Innovations. Facial Plast. Surg. 2021, 37, 556–563. [Google Scholar] [CrossRef]
- Jacono, A.A. A Novel Volumizing Extended Deep-Plane Facelift: Using Composite Flap Shifts to Volumize the Midface and Jawline. Facial Plast. Surg. Clin. N. Am. 2020, 28, 331–368. [Google Scholar] [CrossRef]
- Fedok, F.G. Another Look at Platysmaplasty in Facelifting. Facial Plast. Surg. 2020, 36, 395–403. [Google Scholar] [CrossRef]
- Sykes, J.M.; Riedler, K.L.; Cotofana, S.; Palhazi, P. Superficial and Deep Facial Anatomy and Its Implications for Rhytidectomy. Facial Plast. Surg. Clin. N. Am. 2020, 28, 243–251. [Google Scholar] [CrossRef]
- Ramirez, O.M. Multidimensional evaluation and surgical approaches to neck rejuvenation. Clin. Plast. Surg. 2014, 41, 99–107. [Google Scholar] [CrossRef]
- Smith, R.M.; Papel, I.D. Difficult Necks and Unresolved Problems in Neck Rejuvenation. Clin. Plast. Surg. 2018, 45, 611–622. [Google Scholar] [CrossRef]
- Alimova, S.M.; Sharobaro, V.I.; Telnova, A.V.; Stepanyan, E.E. Planning of methods of surgical correction of soft tissues of the face and neck. Med. Vis. 2021, 25, 47–52. [Google Scholar] [CrossRef]
- Manturova, N.E.; Stupin, V.A.; Ryzhkin, A.N.; Ryzhkina, E.N.; Lesnyakov, A.F. Temporal region as an object for plastic surgeon and artist. Plast. Surg. Aesth. Med. 2021, 4, 7–13. [Google Scholar] [CrossRef]
- Oz Cakar, L.; Kara, M.; Chang, K.V. Nineteen reasons why physiatrists should do musculoskeletal ultrasound: EURO-MUSCULUS/USPRM recommendations. Am. J. Phys. Med. Rehabil. 2015, 94, e45–e49. [Google Scholar] [CrossRef] [PubMed]
- Sethia, R.; Mahida, J.B.; Subbarayan, R.A.; Deans, K.J.; Minneci, P.C.; Elmaraghy, C.A.; Essig, G.F. Evaluation of an imaging protocol using ultrasound as the primary diagnostic modality in pediatric patients with superficial soft tissue infections of the face and neck. Int. J. Pediatr. Otorhinolaryngol. 2017, 96, 89–93. [Google Scholar] [CrossRef] [PubMed]
- Stenner, M.; Rudack, C. Ultrasound imaging of the nose in septorhinoplasty patients. Eur. Arch. Otorhinolaryngol. 2015, 272, 2831–2837. [Google Scholar] [CrossRef] [PubMed]
- Migda, M.S.; Migda, M.; Migda, B.; Slapa, R.Z.; Mlosek, R.K. Feasibility of using high-frequency skin ultrasound (HFSU) in vulvar skin assess- ment—Initial report with the description of HFSU anatomy. Ginekol. Pol. 2016, 87, 19–25. [Google Scholar] [CrossRef]
- Mlosek, R.K.; Skrzypek, E.; Skrzypek, D.M.; Malinowska, S. High-frequency ultrasound-based differentiation between nodular dermal filler deposits and foreign body granulomas. Skin Res. Technol. 2018, 24, 417–422. [Google Scholar] [CrossRef] [PubMed]
- Scotto di Santolo, M.; Sagnelli, M.; Tortora, G.; Santoro, M.A.; Canta, P.L.; Molea, G.; Schonauer, F.; Imbriaco, M. The utility of the high-resolution ultrasound technique in the evaluation of autologous adipose tissue lipofilling, used for the correction of post-surgical, post-traumatic and post-burn scars. Radiol. Med. 2016, 121, 521–527. [Google Scholar] [CrossRef]
- Mashkevich, G.; Wang, J.; Rawnsley, J.; Keller, G.S. The Utility of Ultrasound in the Evaluation of Submental Fullness in Aging Necks. Arch. Facial Plast. Surg. 2009, 11, 240–245. [Google Scholar] [CrossRef]



| Frequency (MHz) | Depth of Penetration (mm) | Visualized Structures |
|---|---|---|
| 7.5 MHz | >40 | Lymph nodes, deep structures |
| 10 MHz | 35 | Epidermis, dermis, subcutis |
| 20 MHz (high frequency ultrasound) | 10 | Epidermis, dermis, part of subcutaneous tissue |
| 50 MHz | 3–4 | Epidermis and dermis |
| 75 MHz | 3 | Epidermis and part of dermis |
| 100 MHz | 1.5 | Epidermis only |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alimova, S.; Sharobaro, V.; Yukhno, A.; Bondarenko, E. Possibilities of Ultrasound Examination in the Assessment of Age-Related Changes in the Soft Tissues of the Face and Neck: A Review. Appl. Sci. 2023, 13, 1128. https://doi.org/10.3390/app13021128
Alimova S, Sharobaro V, Yukhno A, Bondarenko E. Possibilities of Ultrasound Examination in the Assessment of Age-Related Changes in the Soft Tissues of the Face and Neck: A Review. Applied Sciences. 2023; 13(2):1128. https://doi.org/10.3390/app13021128
Chicago/Turabian StyleAlimova, Sekina, Valentin Sharobaro, Anna Yukhno, and Elizaveta Bondarenko. 2023. "Possibilities of Ultrasound Examination in the Assessment of Age-Related Changes in the Soft Tissues of the Face and Neck: A Review" Applied Sciences 13, no. 2: 1128. https://doi.org/10.3390/app13021128






