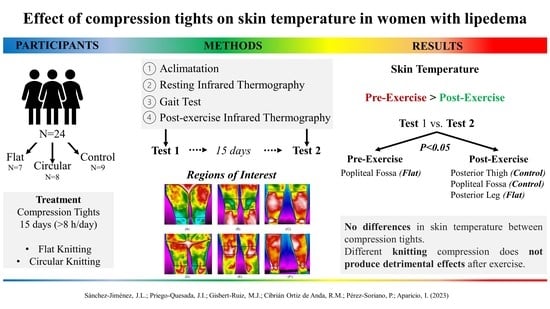
Effect of Compression Tights on Skin Temperature in Women with Lipedema
Abstract
:1. Introduction
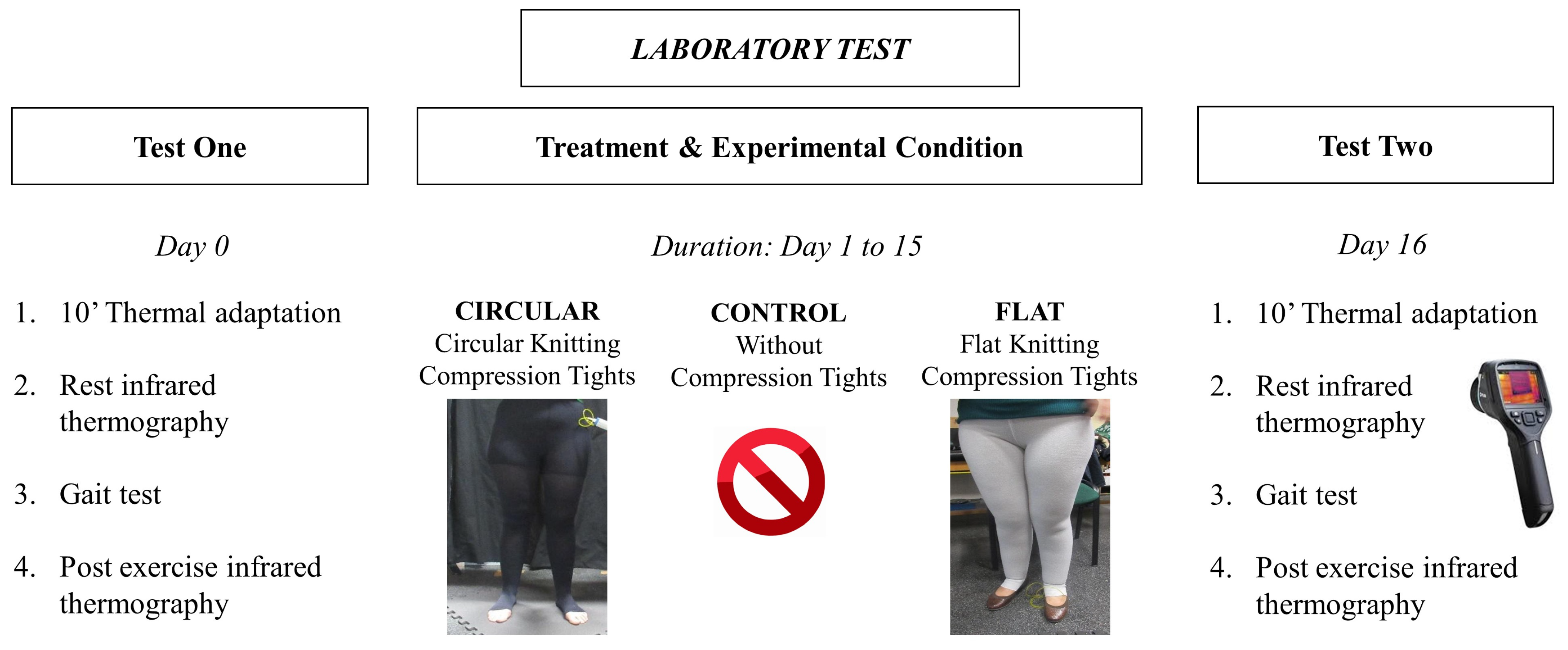
2. Materials and Methods
2.1. Participants
2.2. Protocol
2.3. Compression Tights
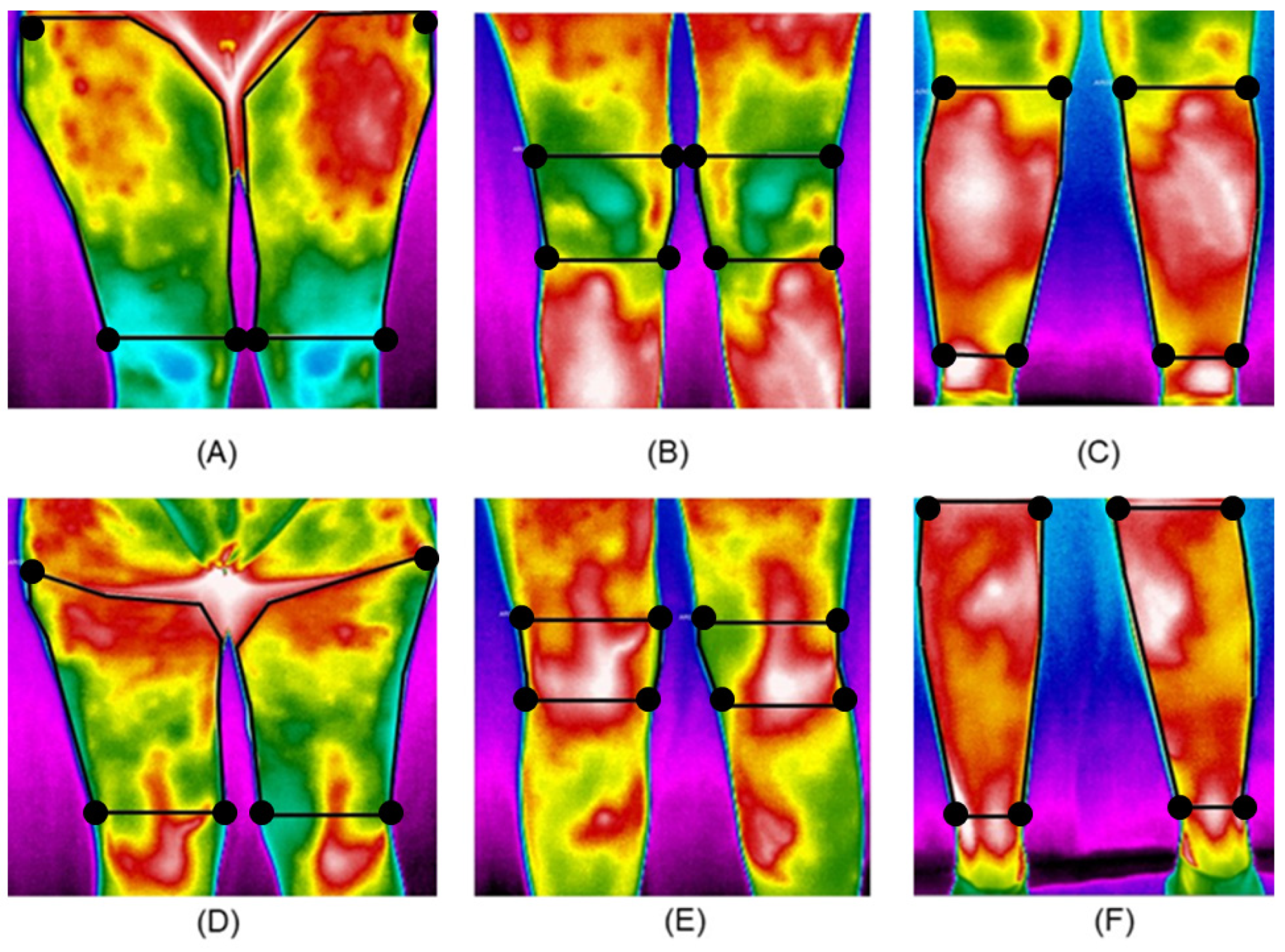
2.4. Data Collection
2.5. Data Analysis
3. Results
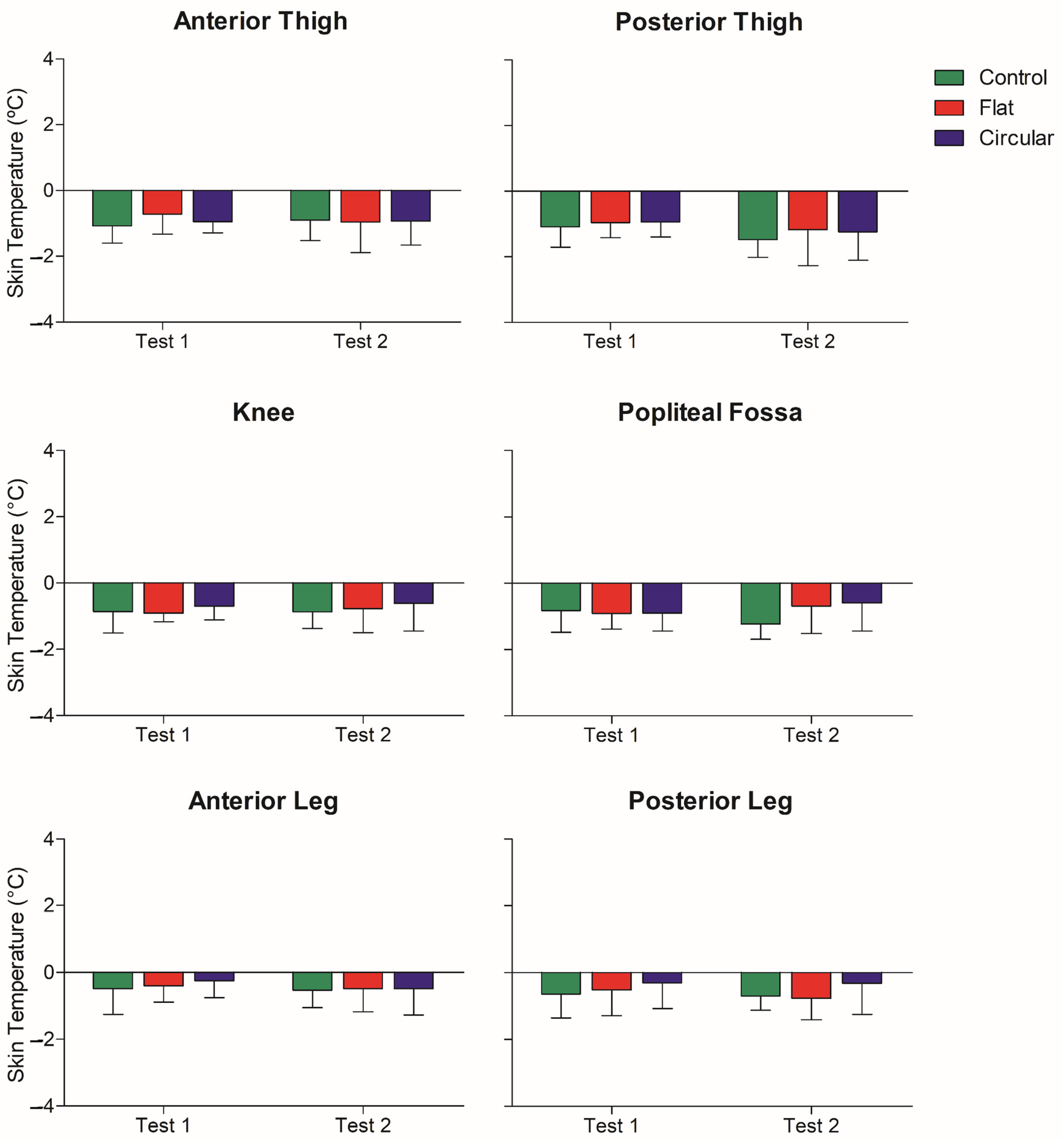
3.1. Mean Skin Temperature
3.2. Maximum Skin Temperature
3.3. Mean Skin Temperature Variation
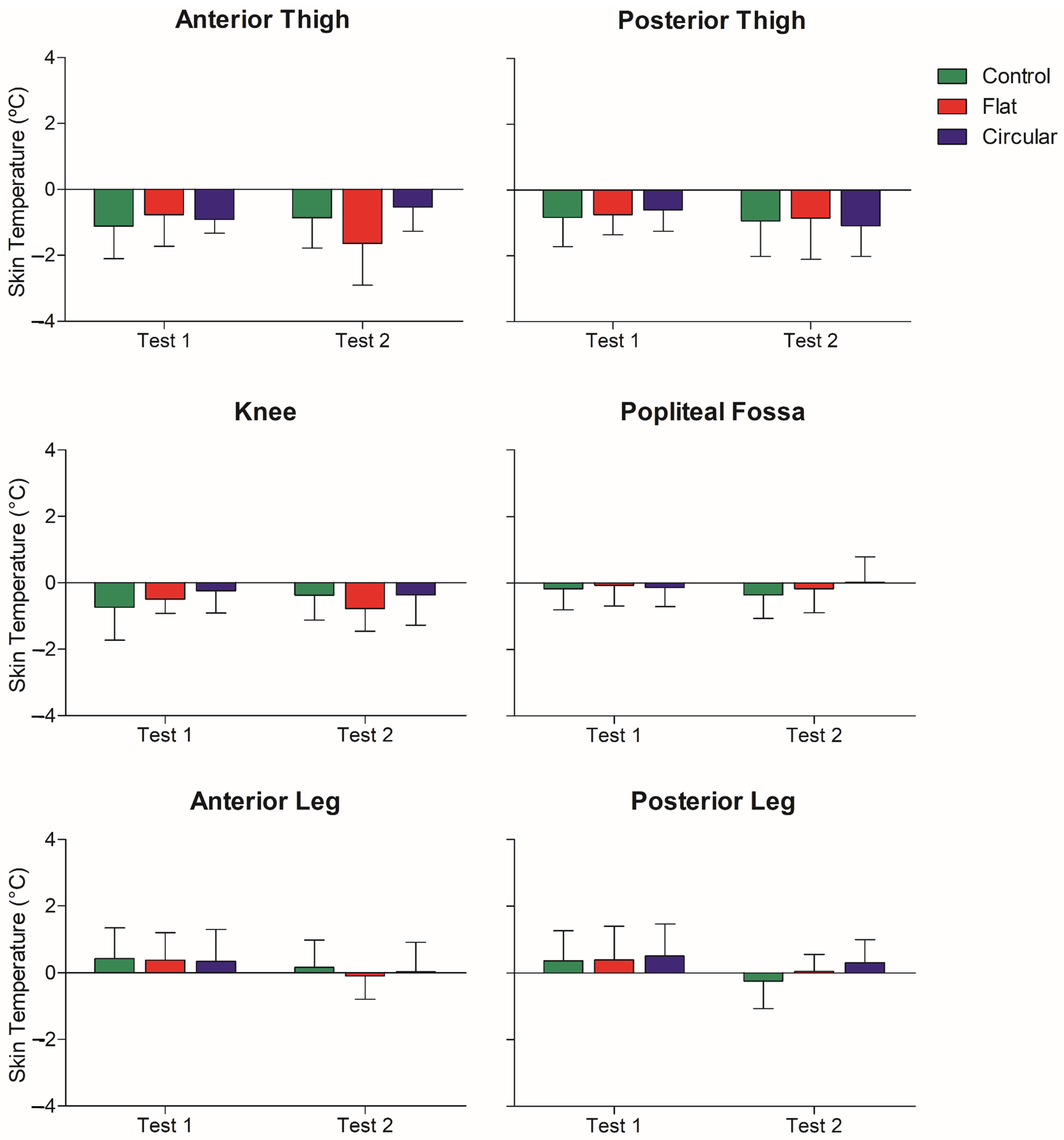
3.4. Maximum Skin Temperature Variation
4. Discussion
4.1. Skin Temperature at Rest
4.2. Skin Temperature after Exercise
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kruppa, P.; Georgiou, I.; Ghods, M.; Biermann, N.; Prantl, L.; Klein-Weigel, P. Lipedema-Pathogenesis, Diagnosis, and Treatment Options. Dtsch. Arztebl. Int. 2020, 117, 396–403. [Google Scholar] [CrossRef] [PubMed]
- La Torre, Y.S.D.; Wadeea, R.; Rosas, V.; Herbst, K.L. Lipedema: Friend and Foe. Horm. Mol. Biol. Clin. Investig. 2018, 33, 20170076. [Google Scholar] [CrossRef] [PubMed]
- Dudek, J.; Białaszek, W.; Gabriel, M. Quality of Life, Its Factors, and Sociodemographic Characteristics of Polish Women with Lipedema. BMC Womens Health 2021, 21, 27. [Google Scholar] [CrossRef] [PubMed]
- Alwardat, N.; Di Renzo, L.; Alwardat, M.; Romano, L.; De Santis, G.L.; Gualtieri, P.; Carrano, E.; Nocerino, P.; De Lorenzo, A. The Effect of Lipedema on Health-Related Quality of Life and Psychological Status: A Narrative Review of the Literature. Eat. Weight Disord.-Stud. Anorex. Bulim. Obes. 2019, 25, 851–856. [Google Scholar] [CrossRef] [PubMed]
- Grada, A.A.; Phillips, T.J. Lymphedema: Pathophysiology and Clinical Manifestations. J. Am. Acad. Dermatol. 2017, 77, 1009–1020. [Google Scholar] [CrossRef] [PubMed]
- Shavit, E.; Wollina, U.; Alavi, A. Lipoedema Is Not Lymphoedema: A Review of Current Literature. Int. Wound J. 2018, 15, 921–928. [Google Scholar] [CrossRef]
- Fetzer, A.; Wise, C. Living with Lipoedema: Reviewing Different Self-Management Techniques. Br. J. Community Nurs. 2015, 20, S14–S19. [Google Scholar] [CrossRef] [Green Version]
- Langendoen, S.I.; Habbema, L.; Nijsten, T.E.C.; Neumann, H.A.M. Lipoedema: From Clinical Presentation to Therapy. A Review of the Literature. Br. J. Dermatol. 2009, 161, 980–986. [Google Scholar] [CrossRef]
- Kröger, K. Lymphoedema and Lipoedema of the Extremities. Vasa-J. Vasc. Dis. 2008, 37, 39–51. [Google Scholar] [CrossRef]
- Reich, S.; Schmeller, W.; Brauer, W.J.; Cornely, M.E.; Faerber, G.; Ludwig, M.; Lulay, G.; Miller, A.; Rapprich, S.; Richter, D.F.; et al. S1 Guidelines: Lipedema. JDDG—J. Ger. Soc. Dermatol. 2017, 15, 758–767. [Google Scholar] [CrossRef]
- Todd, M. Diagnosis and Management of Lipoedema in the Community. Br. J. Community Nurs. 2016, 21, S6–S12. [Google Scholar] [CrossRef]
- Doherty, D.; Morgan, P.; Moffatt, C. Role of Hosiery in Lower Limb Lymphoedema; MEP Ltd.: London, UK, 2006. [Google Scholar]
- Gavin, T. Clothing and Thermoregulation During Exercise. Sport. Med. 2012, 33, 941–947. [Google Scholar] [CrossRef]
- Duffield, R.; Portus, M. Comparison of Three Types of Full-Body Compression Garments on Throwing and Repeat-Sprint Performance in Cricket Players. Br. J. Sports Med. 2007, 41, 409–414. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hillen, B.; Pfirrmann, D.; Nägele, M.; Simon, P. Infrared Thermography in Exercise Physiology: The Dawning of Exercise Radiomics. Sport. Med. 2020, 50, 263–282. [Google Scholar] [CrossRef] [PubMed]
- Moreira, D.G.; Costello, J.T.; Brito, C.J.; Adamczyk, J.G.; Ammer, K.; Bach, A.J.E.; Costa, C.M.A.; Eglin, C.; Fernandes, A.A.; Fernández, I.; et al. Thermographic Imaging in Sports and Exercise Medicine: A Delphi Study and Consensus Statement on the Measurement of Human Skin Temperature. J. Therm. Biol. 2017, 69, 155–162. [Google Scholar] [CrossRef]
- Kandlikar, S.G.; Perez, I.; Raghupathi, P.A.; Gonzalez, J.L.; Dabydeen, D.; Medeiros, L.; Phatak, P. Infrared Imaging Technology for Breast Cancer Detection—Current Status, Protocols and New Directions. Int. J. Heat Mass Transf. 2017, 108, 2303–2320. [Google Scholar] [CrossRef]
- Carbonell, L.; Priego, J.I.; Retorta, P.; Benimeli, M.; Cibrián Ortiz De Anda, R.M.; Salvador Palmer, R.; González Peña, R.J.; Galindo, C.; Pino Almero, L.; Blasco, M.C.; et al. Thermographic Quantitative Variables for Diabetic Foot Assessment: Preliminary Results. Comput. Methods Biomech. Biomed. Eng. Imaging Vis. 2019, 7, 660–666. [Google Scholar] [CrossRef]
- Priego, J.I.; Lucas, A.G.; Gil, M.; Giménez, J.V.; Aparicio, I.; Cibrián Ortiz de Anda, R.M.; Salvador, R.; Llana, S.; Pérez, P. Effects of Graduated Compression Stockings on Skin Temperature after Running. J. Therm. Biol. 2015, 52, 130–136. [Google Scholar] [CrossRef]
- Chudecka, M.; Lubkowska, A.; Kempińska, A. Body Surface Temperature Distribution in Relation to Body Composition in Obese Women. J. Therm. Biol. 2014, 43, 1–6. [Google Scholar] [CrossRef]
- Dȩbiec, A.; Skrzek, A.; Wozniewski, M.; Malicka, I. Using Thermography in the Diagnostics of Lymphedema: Pilot Study. Lymphat. Res. Biol. 2020, 18, 247–253. [Google Scholar] [CrossRef]
- Kelly, L.A.; Karim, M.; Sultan, A.; Al Kawsar, A.; Khair, A.; Betts, H.; Douglass, J.; Forrer, A.; Taylor, M.J. Infrared Thermal Imaging as a Novel Non-Invasive Point-of-Care Tool to Assess Filarial Lymphoedema. J. Clin. Med. 2021, 10, 2301. [Google Scholar] [CrossRef] [PubMed]
- Zasadzka, E.; Trzmiel, T.; Kleczewska, M.; Pawlaczyk, M. Comparison of the Effectiveness of Complex Decongestive Therapy and Compression Bandaging as a Method of Treatment of Lymphedema in the Elderly. Clin. Interv. Aging 2018, 13, 929–934. [Google Scholar] [CrossRef] [Green Version]
- Sanchís, R.; Blasco, C.; Encarnación, A.; Pérez, P. Changes in Plantar Pressure and Spatiotemporal Parameters during Gait in Older Adults after Two Different Training Programs. Gait Posture 2020, 77, 250–256. [Google Scholar] [CrossRef]
- Sanchís, R.; Blasco, C.; Camacho, A.; Encarnación, A.; Pérez, P. Evaluation of Impact-Shock on Gait after the Implementation of Two Different Training Programs in Older Adults. Clin. Biomech. 2020, 80, 105131. [Google Scholar] [CrossRef]
- Pérez, P.; Llana, S.; Encarnación-Martínez, A.; Martínez-Nova, A.; Morey-Klapsing, G. Nordic Walking Practice Might Improve Plantar Pressure Distribution. Res. Q. Exerc. Sport 2011, 82, 593–599. [Google Scholar] [CrossRef]
- Neumann, H.; Partsch, H.; Mosti, G.; Flour, M. Classification of Compression Stockings: Report of the Meeting of the International Compression Club, Copenhagen. Int. Angiol. J. Int. Union Angiol. 2016, 35, 122–128. [Google Scholar]
- Wardiningsih, W.; Troynikov, O. Interface Pressure Generated by Knitted Fabrics of Different Direction, Composition and Number of Layers in Sport Compression Garments. J. Text. Inst. 2018, 110, 882–890. [Google Scholar] [CrossRef]
- Marins, J.C.B.; Moreira, D.G.; Cano, S.P.; Quintana, M.S.; Soares, D.D.; De Andrade Fernandes, A.; Da Silva, F.S.; Costa, C.M.A.; Dos Santos Amorim, P.R. Time Required to Stabilize Thermographic Images at Rest. Infrared Phys. Technol. 2014, 65, 30–35. [Google Scholar] [CrossRef] [Green Version]
- Forner, I.; Szolnoky, G.; Forner, A.; Kemény, L. Lipedema: An Overview of Its Clinical Manifestations, Diagnosis and Treatment of the Disproportional Fatty Deposition Syndrome—Systematic Review. Clin. Obes. 2012, 2, 86–95. [Google Scholar] [CrossRef]
- Fujii, N.; Nikawa, T.; Tsuji, B.; Kenny, G.P.; Kondo, N.; Nishiyasu, T. Wearing Graduated Compression Stockings Augments Cutaneous Vasodilation but Not Sweating during Exercise in the Heat. Physiol. Rep. 2017, 5, e13252. [Google Scholar] [CrossRef]
- Venckunas, T.; Trinkunas, E.; Kamandulis, S.; Poderys, J.; Grunovas, A.; Brazaitis, M. Effect of Lower Body Compression Garments on Hemodynamics in Response to Running Session. Sci. World J. 2014, 2014, 353040. [Google Scholar] [CrossRef]
- Kenefick, R.W.; Cheuvront, S.N. Physiological Adjustments to Hypohydration: Impact on Thermoregulation. Auton. Neurosci. Basic Clin. 2016, 196, 47–51. [Google Scholar] [CrossRef]
- Kenny, G.P.; Mcginn, R. Restoration of Thermoregulation after Exercise. J. Appl. Physiol. 2017, 122, 933–944. [Google Scholar] [CrossRef]
- De Andrade, A.; Dos Santos, P.R.; Brito, C.J.; De Moura, A.G.; Moreira, D.G.; Costa, C.M.A.; Sillero, M.; Marins, J.C.B. Measuring Skin Temperature before, during and after Exercise: A Comparison of Thermocouples and Infrared Thermography. Physiol. Meas. 2014, 35, 189–203. [Google Scholar] [CrossRef] [Green Version]
- Vargas, N.T.; Chapman, C.L.; Johnson, B.D.; Gathercole, R.; Schlader, Z.J. Skin Wettedness Is an Important Contributor to Thermal Behavior during Exercise and Recovery. Am. J. Physiol.-Regul. Integr. Comp. Physiol. 2018, 315, R925–R933. [Google Scholar] [CrossRef] [Green Version]
- Priego, J.I.; De la Fuente, C.; Kunzler, M.; Perez, P.; Hervás, D.; Carpes, F.P. Relationship between Skin Temperature, Electrical Manifestations of Muscle Fatigue, and Exercise-Induced Delayed Onset Muscle Soreness for Dynamic Contractions: A Preliminary Study. Int. J. Environ. Res. Public Health 2020, 17, 6817. [Google Scholar] [CrossRef]
- Priego, J.I.; Kunzler, M.R.; Carpes, F.P. Methodological Aspects of Infrared Thermography in Human Assessment. In Application of Infrared Thermography in Sports Science; Springer International Publishing: Valencia, Spain, 2017; pp. 49–79. ISBN 978-3-319-47409-0. [Google Scholar]


| Characteristics | Total Sample (n = 24) | Control Group (n = 9) | Flat Knitting Group (n = 7) | Circular Knitting Group (n = 8) | p Value |
|---|---|---|---|---|---|
| Age (years) | 41.1 ± 9.6 | 39.3 ± 6.8 | 42.3 ± 11.2 | 42.0 ± 11.4 | >0.05 |
| Body mass (kg) | 69.3 ± 11.8 | 76.1 ± 11.5 | 62.7 ± 10.6 | 68.2 ± 10.3 | >0.05 |
| Height (cm) | 154.5 ± 32.4 | 163.6 ± 3.3 | 157.4 ± 5.5 | 141.4 ± 7.0 | >0.05 |
| BMI (kg/m2) | 26.9 ± 4.5 | 28.5 ± 4.9 | 25.4 ± 4.9 | 26.5 ± 4.5 | >0.05 |
| Grade | I = 25% | I = 22% | I = 14% | I = 25% | >0.05 |
| II = 75% | II = 78% | II = 86% | II = 75% | ||
| Compressive experience (hours/day) | 10.71 ± 2.39 | 0 ± 0 | 9.9 ± 3.2 | 11.9 ± 1.5 | >0.05 |
| ROI | Test One | Test Two | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-Exercise | Post-Exercise | Pre-Exercise | Post-Exercise | ||||||||||||||
| Control | Circular | Flat | p | Control | Circular | Flat | p | Control | Circular | Flat | p | Control | Circular | Flat | p | ||
| Mean Tsk (°C) | Anterior Thigh | 29.1 ± 1.3 | 29.0 ± 0.9 | 28.6 ± 1.2 | 1.00 | 28.0 ± 1.4 | 28.0 ± 1.0 | 27.9 ± 0.9 | 1.00 | 28.5 ± 1.5 | 28.8 ± 1.5 | 28.3 ± 1.3 | 1.00 | 27.7 ± 1.3 | 27.9 ± 1.1 | 27.3 ± 0.7 | 1.00 |
| Knee | 28.7 ± 1.0 | 28.6 ± 1.3 | 28.6 ± 1.3 | 1.00 | 27.9 ± 1.1 | 28.0 ± 1.0 | 27.7 ± 1.2 | 1.00 | 28.3 ± 1.3 | 28.2 ± 1.7 | 27.8 ± 1.2 | 1.00 | 27.4 ± 1.3 | 27.6 ± 1.2 | 27.0 ± 0.9 | 1.00 | |
| Anterior Leg | 29.1 ± 1.0 | 29.3 ± 1.2 | 29.0 ± 1.5 | 1.00 | 28.7 ± 1.2 | 29.0 ± 1.1 | 28.6 ± 1.5 | 1.00 | 28.8 ± 1.3 | 29.0 ± 1.0 | 28.3 ± 1.5 | >0.9 | 29.7 ± 4.5 | 28.5 ± 1.0 | 27.8 ± 1.5 | >0.6 | |
| Posterior Thigh | 29.2 ± 1.4 | 29.2 ± 1.1 | 29.2 ± 1.5 | 1.00 | 28.1 ± 1.3 | 28.3 ± 1.0 | 28.3 ± 1.1 | 1.00 | 28.9 ± 1.4 | 29.4 ± 1.4 | 28.8 ± 1.6 | 1.00 | 27.4 ± 1.4 | 28.1 ± 0.9 | 27.6 ± 0.8 | >0.5 | |
| Popliteal Fossa | 29.7 ± 0.8 | 30.2 ± 1.0 | 29.9 ± 1.1 | >0.7 | 28.9 ± 0.8 | 29.3 ± 1.0 | 29.0 ± 0.8 | >0.8 | 29.2 ± 1.0 | 29.7 ± 1.0 | 29.2 ± 1.2 | 1.00 | 28.0 ± 1.0 | 29.2 ± 0.6 | 28.5 ± 0.9 | # 0.046 | |
| Posterior Leg | 28.7 ± 0.8 | 28.7 ± 1.2 | 28.6 ± 1.3 | 1.00 | 28.1 ± 1.1 | 28.4 ± 0.8 | 28.1 ± 1.0 | 1.00 | 28.2 ± 1.2 | 28.2 ± 1.2 | 27.8 ± 1.5 | 1.00 | 27.5 ± 1.3 | 27.8 ± 0.8 | 27.0 ± 1.5 | >0.6 | |
| Maximum Tsk (°C) (°C)(°C)Temperature | Anterior Thigh | 31.7 ± 1.6 | 31.9 ± 1.1 | 31.3 ± 1.4 | 1 | 30.6 ± 2.0 | 31.0 ± 1.1 | 30.6 ± 0.7 | 1 | 31.2 ± 1.9 | 31.4 ± 1.8 | 31.2 ± 1.4 | 1 | 30.4 ± 2.1 | 30.9 ± 1.4 | 29.6 ± 0.8 | >0.3 |
| Knee | 30.9 ± 1.6 | 30.9 ± 1.5 | 30.6 ± 1.3 | 1 | 30.2 ± 1.6 | 30.7 ± 1.2 | 30.1 ± 1.4 | 1 | 30.7 ± 1.8 | 30.7 ± 1.8 | 30.2 ± 0.8 | 1 | 30.3 ± 1.8 | 30.3 ± 1.7 | 29.4 ± 1.0 | >0.7 | |
| Anterior Leg | 32.1 ± 1.2 | 31.9 ± 1.0 | 32.0 ± 1.3 | 1 | 32.5 ± 1.4 | 32.2 ± 1.0 | 32.3 ± 1.2 | 1 | 32.1 ± 1.4 | 31.7 ± 1.3 | 31.6 ± 1.3 | 1 | 32.2 ± 1.5 | 31.8 ± 1.5 | 31.5 ± 1.3 | >0.9 | |
| Posterior Thigh | 31.5 ± 1.7 | 31.8 ± 1.0 | 31.6 ± 1.5 | 1 | 30.7 ± 1.7 | 31.2 ± 1.0 | 30.9 ± 1.6 | 1 | 31.4 ± 1.5 | 31.8 ± 1.2 | 31.2 ± 1.7 | 1 | 30.5 ± 1.7 | 30.7 ± 1.2 | 30.4 ± 1.2 | 1 | |
| Popliteal Fossa | 32.3 ± 1.2 | 32.8 ± 0.9 | 32.4 ± 1.1 | 1 | 32.2 ± 1.1 | 32.6 ± 0.9 | 32.3 ± 0.9 | >0.9 | 32.0 ± 1.0 | 32.6 ± 0.9 | 32.0 ± 1.1 | >0.7 | 31.7 ± 1.3 | 32.6 ± 0.8 | 31.8 ± 1.0 | >0.2 | |
| Posterior Leg | 30.9 ± 0.9 | 31.2 ± 1.1 | 31.2 ± 1.1 | 1 | 31.3 ± 1.1 | 31.7 ± 1.0 | 31.6 ± 1.3 | 1 | 30.8 ± 1.1 | 30.8 ± 1.5 | 30.8 ± 1.6 | 1 | 30.6 ± 1.6 | 31.1 ± 1.5 | 30.8 ± 1.7 | 1 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sanchez-Jimenez, J.L.; Priego-Quesada, J.I.; Gisbert-Ruiz, M.J.; Cibrian-Ortiz de Anda, R.M.; Perez-Soriano, P.; Aparicio, I. Effect of Compression Tights on Skin Temperature in Women with Lipedema. Appl. Sci. 2023, 13, 1133. https://doi.org/10.3390/app13021133
Sanchez-Jimenez JL, Priego-Quesada JI, Gisbert-Ruiz MJ, Cibrian-Ortiz de Anda RM, Perez-Soriano P, Aparicio I. Effect of Compression Tights on Skin Temperature in Women with Lipedema. Applied Sciences. 2023; 13(2):1133. https://doi.org/10.3390/app13021133
Chicago/Turabian StyleSanchez-Jimenez, Jose Luis, Jose Ignacio Priego-Quesada, María José Gisbert-Ruiz, Rosa M. Cibrian-Ortiz de Anda, Pedro Perez-Soriano, and Inmaculada Aparicio. 2023. "Effect of Compression Tights on Skin Temperature in Women with Lipedema" Applied Sciences 13, no. 2: 1133. https://doi.org/10.3390/app13021133
APA StyleSanchez-Jimenez, J. L., Priego-Quesada, J. I., Gisbert-Ruiz, M. J., Cibrian-Ortiz de Anda, R. M., Perez-Soriano, P., & Aparicio, I. (2023). Effect of Compression Tights on Skin Temperature in Women with Lipedema. Applied Sciences, 13(2), 1133. https://doi.org/10.3390/app13021133