Abstract
This case report presents a study of unwanted tooth movements during the retention phase after orthodontic treatment. The early recognition of these unwanted tooth movements is paramount for patients and clinicians to prevent the associated negative consequences. A 21-year-old male presented with aesthetic complaints regarding his upper front teeth. He underwent orthodontic treatment at the age of 9 years and 11 months and finished his treatment 2 years and 11 months later. Flexible spiral wires (FSW) were bonded to the anterior segment of the upper and lower jaws to stabilize the end result. The failure of the fixed retainers had never occurred previously. The diagnostic assessment demonstrated a previously orthodontically treated class I malocclusion with excessive angulation and torque differences in the maxillary anterior segment. To correct the position of the maxillary anterior segment and prevent further misalignment, the patient received orthodontic re-treatment. Thereafter, the result was retained with fixed braided-rectangular-wire (BRW) retainers located at 12–22 and 33–43 and a vacuum-formed retainer (VFR) in the maxilla. The end result appeared to be stable after 28 months of retention. Unwanted tooth movements can occur during the orthodontic retention phase and might result from the use of fixed flexible spiral wire retainers. Follow-up appointments are recommended to monitor the stability and recognize these movements.
1. Introduction
The retention phase of an orthodontic treatment aims to maintain the end result of orthodontic treatment and is of great importance for both patients and orthodontists. In 1934, Oppenheim stated: “Retention is one of the most difficult problems in orthodontia; in fact, it is the problem” [1]. Without retention, teeth have the possibility of (1) returning to their initial position, also known as ‘relapse’ [2], or (2) displacement as a result of growth and aging [3]. Orthodontic retention can be performed in two ways: (1) by placing fixed or removable appliances on the teeth or (2) by additional treatments of the teeth and periodontal structures in order to achieve stability. Fixed retainers are usually bonded to the palatal or lingual side of the anterior teeth [4]. Hawley or vacuum-formed retainers (VFR) can be taken off by the patient. Additional treatments used to prevent relapse are (1) small surgical procedures that cut the supra-crestal periodontal fibers around the teeth to reduce the chance of relapse [5] or (2) interproximal enamel reduction of the lower front teeth to create space for the corrected crowding and to compensate in advance for the expected reduction in the inter-canine width during aging [6].
Currently, fixed retention is commonly used in orthodontic practice [7,8]. Previous research on the long-term outcomes showed that when using a flexible spiral wire (FSW) retainer bonded to the mandibular anterior segment, the alignment is stabilized in 90.5% (200/221) of cases after 5 years of retention [9]. However, these fixed retention appliances may also fail or have adverse effects. Recently, a systematic review was conducted to evaluate the available evidence on the failure of fixed retainers and reported that fixed retainers fail in a range of 7.3% to 50%, according to which detachment at the adhesive–enamel interface was the most commonly reported type of failure [10]. Other observed adverse effects of fixed retainers in the orthodontic literature are detachment at the adhesive–wire interface [11], wire fracture [12], wire untwisting [13], and calculus accumulation [14,15]. Wire untwisting may lead to unwanted changes in the tooth position and can be associated with the development of gingival recessions [13,16,17]. Other causes of unwanted tooth movements can be tongue thrust or personal habits [18,19]. A clinical case of unwanted tooth movements during the retention phase is presented in this case report. This case showed that the unwanted tooth movement was the direct result of an untwisting FSW, because the maxillary teeth were displaced in a different direction from the original tooth position (Figure 1), which clearly showed that this was not a case of simple relapse. The early recognition of these unwanted tooth movements is paramount for patients and clinicians to prevent the associated negative consequences [20].

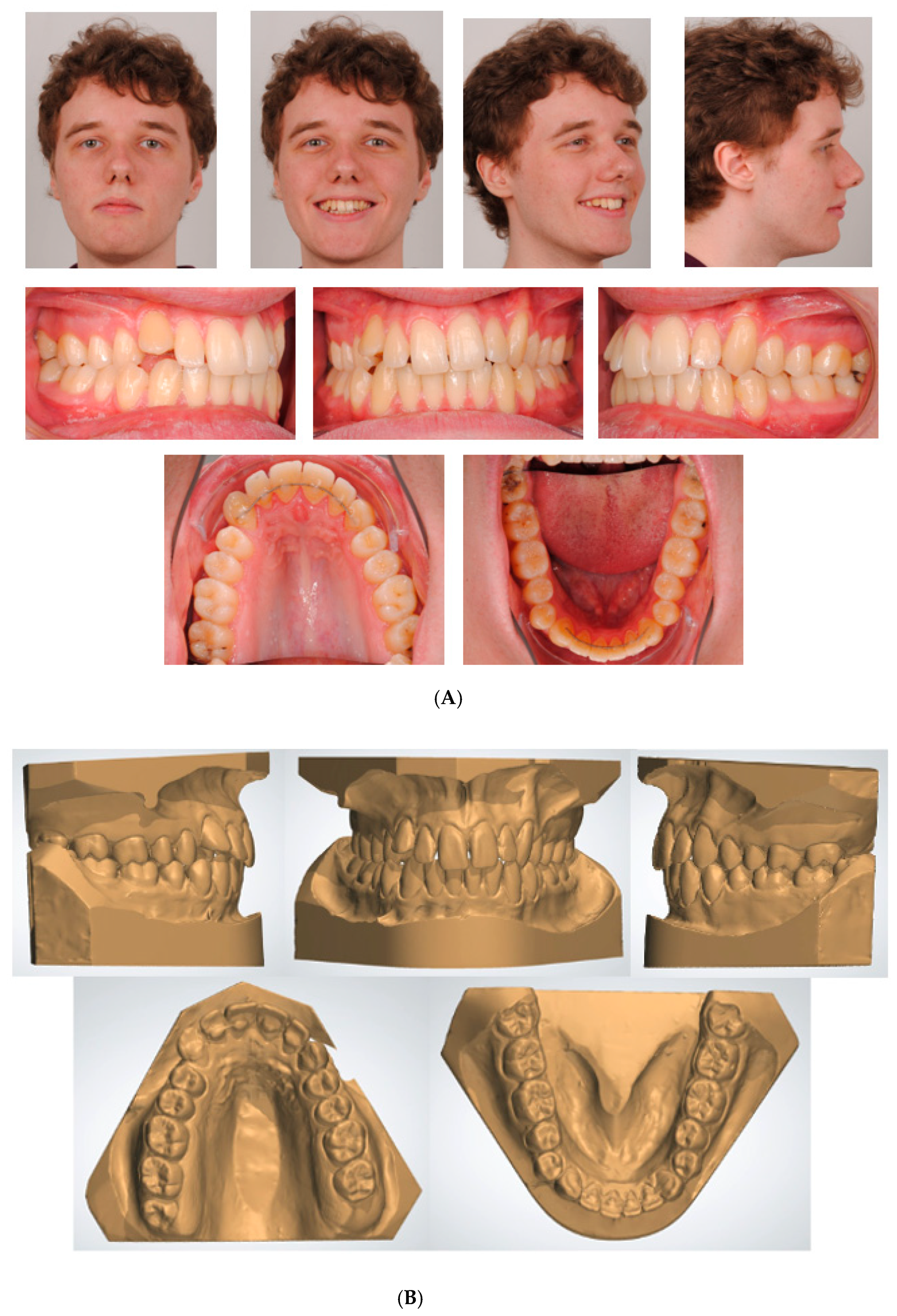
Figure 1.
Extra-oral and intra-oral photographs before first orthodontic treatment.
2. Materials and Methods
This case was reported according to the Case Report (CARE) guidelines [21]. The CARE checklist of items used for this case report is presented in Supplementary File S1.
- Patient information
A 21-year-old Caucasian male presented with aesthetic complaints regarding his upper front teeth. He previously underwent orthodontic treatment for a deep bite at the age of 9 years and 11 months for 2 years and 11 months. He was treated with high-pull headgear (Headgear, Dentsply GAC International, NY, USA) followed by full fixed appliances (3M Victory Series APC conventional twin brackets, 3M Health Care Division, London, Canada), and flexible spiral wires (0.0195-inch, 3-strand, heat-treated twist wire, Wildcat, GAC International, Bohemia, NY, USA) were bonded to all the anterior teeth between 13–23 and 33–43 to stabilize the end result (Figure 2). Over the last few years (the moment of onset was unknown), he noted a continuing shift in the position of his upper front teeth (Figure 3A). Aside from his aesthetic complaints, he was concerned that the situation would deteriorate. With regard to his medical history, he only used antihistamines for hay fever if necessary. There was no record of dental trauma, and he was unfamiliar with oral parafunctions. The failure of the fixed retainers had never occurred, and he did not experience any pain or functional constraints.

Figure 2.
Extra-oral and intra-oral photographs after first orthodontic treatment.
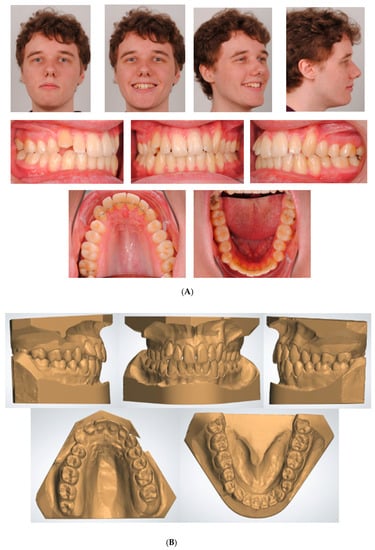
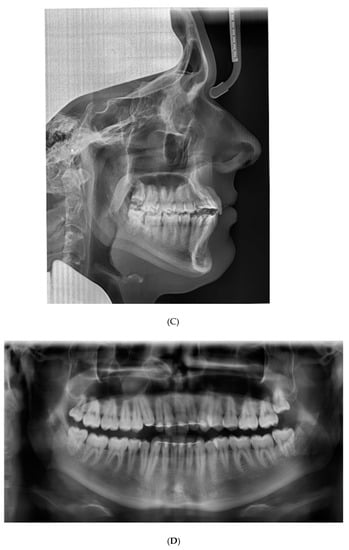
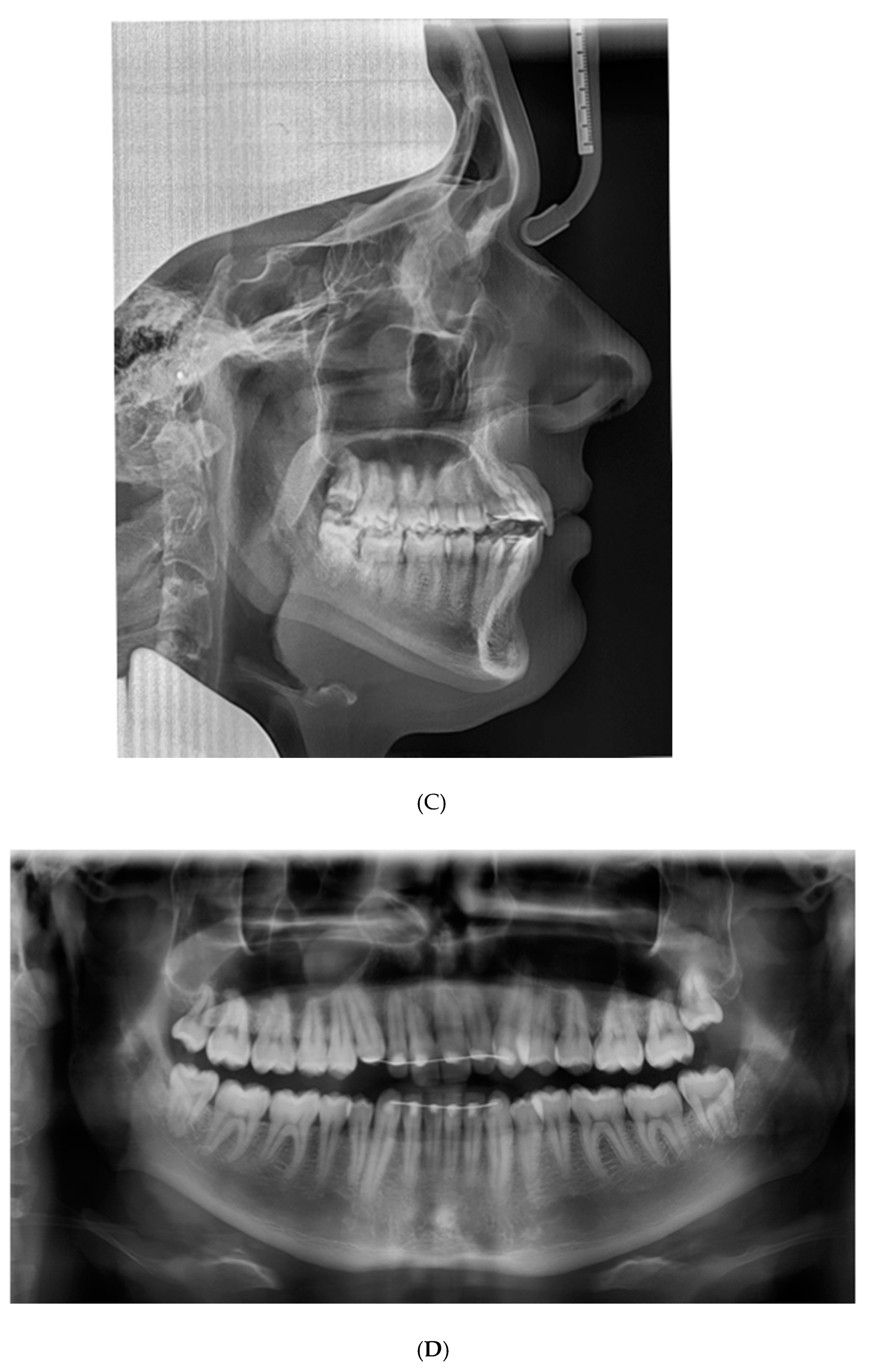
Figure 3.
Documentation before orthodontic re-treatment. (A) Extra-oral and intra-oral photographs. (B) Dental casts. (C) Lateral cephalometric radiograph. (D) Panoramic radiograph.
- Clinical Findings
Figure 3A shows the case at the first presentation. The photographs demonstrate that the 13 shows excessive palatal root torque, and the 23 shows excessive buccal root torque. A cant of the upper incisors can be observed. Moreover, cross-bites are present between the 14 and the 44 and between the 23 and the 34.
- Timeline
The timeline for this patient is presented in Supplementary File S2.
- Diagnostic Assessment
The patient presented with a Class I profile and a chin point deviation to the right side (Figure 3A). The intra-oral assessment showed good oral hygiene, a thin gingival biotype, group function on the left and right side, and fixed retainers (0.0195-inch, 3-strand, heat-treated twist wire, Wildcat, GAC International, Bohemia, NY, USA) in the upper anterior segment and lower anterior segment (Figure 3A). The dental cast assessment showed a Class I molar and canine occlusion, an overjet of 2 mm, and an overbite of 3 mm. A cant of the upper incisors was present with palatal root torque of the 13 and buccal root torque of the 23. Crossbites were present between the 14/44 and the 23/34. The arch length discrepancy measurement resulted in values of 0 mm in the case of the maxillary arch and −4 mm in the case of the mandibular arch. No tooth size discrepancy was present. The PAR index resulted in a score of 12 points [22] (Figure 3B). The lateral cephalometric radiograph showed a Class I intermaxillary relationship with an ANB angle of 3.2° (VistaPano S Ceph, Dürr Dental imaging software, Dürr Dental SE, Bietigheim-Bissingen, Germany) (Figure 3C). The panoramic radiograph (VistaPano S Ceph, Dürr Dental imaging software, Dürr Dental SE, Bietigheim-Bissingen, Germany) showed a maxillary sinus mucosal cyst (MSMC) on the right side and external apical root resorption located at the 12, 11, and 21 (Figure 3D).
2.1. Diagnosis
This clinical, radiographic, and dental cast examination contributed to the following orthodontic diagnosis: A 21-year-old male with an Angle Class I malocclusion, angulation, and torque differences in the maxillary anterior segment, with cross-bites located at 14/44 and 23/34, a thin gingival biotype, external apical root resorption located at 12, 11, and 21, and the presence of fixed retainers (0.0195-inch, 3-strand, heat-treated twist wire, Wildcat, GAC International, Bohemia, NY, USA) located between 13–23 and 33–43.
2.2. Prognosis
The torque and angulation differences in the maxillary anterior segment were not observed before (Figure 1) or after the orthodontic treatment from 2006 to 2009 (Figure 2). From 2009 to 2017, no failure of the fixed retainers had occurred, and no oral parafunctions were present. It was hypothesized that the FSW retainer caused these unwanted tooth movements [9,16]. Since the patient identified a continued worsening of the position of the upper front teeth, it is likely that this process of unwanted tooth movement was persistent and consequently resulted in a worse prognosis. For example, the development of gingival recessions may occur [17]. A recent case report showed a similar situation that resulted in the exposure of the apex of a canine [20]. A pilot study based on a retrospective data analysis showed that the removal of the FSW retainer led to the cessation of further unwanted tooth movement [23].
- Therapeutic intervention
To correct the position of the maxillary anterior segment and prevent further misalignment, the patient received orthodontic re-treatment for 2 years and 4 months. The fixed FSWs (0.0195-inch, 3-strand, heat-treated twist wire, Wildcat, GAC International, Bohemia, NY, USA) in the maxilla and mandible were removed. Afterward, fixed appliances were placed (3M Victory Series APC conventional twin brackets, 3M Health Care Division, London, Canada). To correct the excessive palatal root torque of the 13, we incorporated the 13 into the fixed appliances with a 0.012-inch NiTi overlay wire (Sentalloy, Dentsply GAC international, Bohemia, NY, USA) on a 0.016 × 0.022-inch SS base wire (Stainless Steel Ideal® Form, Dentsply GAC international, Bohemia, NY, USA). In this way, the risk of unwanted reactionary tooth movements was reduced. During the active orthodontic treatment, a panoramic radiograph (VistaPano S, Dürr Dental imaging software, Dürr Dental SE, Bietigheim-Bissingen, Germany) was performed to monitor the root resorption observed in the maxillary anterior region in the initial stage of the treatment [24] (Figure 4). It appeared to be stable. However, it was difficult to reach a conclusion in this regard, since (1) a great difference in the tooth position between the two panoramic radiographs and (2) variations in quality between the panoramic radiographs were observed due to the use of different radiographic devices. The oral hygiene was checked at every orthodontic appointment. If necessary, instructions were given to maintain the quality of the patient’s oral hygiene during the orthodontic treatment. After active orthodontic treatment over 2 years and 4 months, the treatment result was stabilized with fixed braided-rectangular-wire (BRW) retainers (Forestaflex, Forestadent®, Bernhard Förster GmbH, Pforzheim, Germany) located at 12–22 and 33–43. We opted for the BRW retainers, which achieve better torque control compared to flexible spiral wires (FSW) [25]. In addition, a VFR was prescribed for approximately 10 h a day to cover all the maxillary teeth. According to the current literature, the part-time wear of the VFR should be sufficient enough to generate stability [26]. Table 1 provides a detailed overview of the interventions.

Figure 4.
Panoramic radiograph during orthodontic treatment for monitoring root resorption.

Table 1.
Interventions for the orthodontic re-treatment.
3. Results
3.1. Follow-Up and Outcomes
3.1.1. Clinician- and Patient-Assessed Outcomes
The end result of the orthodontic re-treatment is shown in Figure 5. The cant of the upper incisors, the excessive palatal and buccal root torque of the 13 and 23, and the crossbites were corrected. In addition to aesthetic improvement, cuspid guidance on the left and right sides was achieved. However, the panoramic radiograph showed an increase in root resorption (Figure 4), and a buccal gingival recession was observed at the 23 (Figure 5). To assess the outcome of this orthodontic re-treatment, the Peer Assessment Rating (PAR) index was consulted and resulted in a PAR score of 2 [22]. Compared to the PAR score measured before the orthodontic re-treatment (PAR score of 12), the malocclusion improved by 83% (10/12). The patient participated in the ESAS patient satisfaction evaluation questionnaire to assess the outcome of the orthodontic re-treatment. ESAS (EFOSA Self Assessment System) is a quality assessment system available to all orthodontists in Europe [27]. This patient satisfaction evaluation questionnaire rates different aspects of the treatment, e.g., patient satisfaction with the orthodontist, assistants, practice, and overall treatment. The completed questionnaire is provided (Supplementary File S3). The answers indicated that the patient was satisfied with nearly all aspects. Nevertheless, the treatment duration was slightly longer than expected, and he believed that the waiting room was not comfortable enough.

Figure 5.
Extra-oral and intra-oral photographs after orthodontic re-treatment.
3.1.2. Important Follow-Up Test Results
Since the patient went abroad for 3 years, the first follow-up appointment was scheduled for April 2022 (28 months after the end of the orthodontic re-treatment). At that moment, the bonded retainers were still fixed and had not been displaced. He still wore the VFR for approximately 10 h a day. An intra-oral examination showed a class I occlusion with an overjet of 2 mm and an overbite of 3 mm (Figure 6). These findings implied that the end result of the orthodontic re-treatment seemed to be stable. Unfortunately, the patient’s oral hygiene was insufficient because, plaque and calculus were present around the fixed retainer in the mandibular anterior segment.

Figure 6.
Extra-oral and intra-oral photographs 28 months after orthodontic re-treatment.
3.1.3. Intervention Adherence and Tolerability
The patient was compliant with the intervention. The oral hygiene was sufficient during the orthodontic treatment, and all the check-up appointments were undertaken. According to the patient, his aesthetic concerns and awareness of the need for orthodontic treatment could be attributed to this adherence.
3.1.4. Adverse and Unanticipated Events
During the active orthodontic re-treatment, an increase in root resorption occurred, and a buccal gingival recession was observed at the 23.
4. Discussion
This case report illustrates an adverse effect in orthodontics. This concerned unwanted tooth movement during the retention phase, probably due to the fixed retainer in the upper jaw. Even though fixed retainers are effective in preventing relapse, previous research has shown that fixed FSWs may also lead to unwanted effects and can complicate oral hygiene, with negative consequences for the periodontium [9,16,28,29,30]. Katsaros et al. described two possible effects of fixed FSWs during the retention phase: (1) the X-effect, a torque difference between two adjacent mandibular incisors, and (2) the twist-effect, an increase in the buccal inclination of the canine [16]. The X-effect or twist effect was observed in 2.7% (6/221) of the evaluated patients during a retention period of 5 years [9]. Recently, Singh described a case in which a combination of the X-effect and twist-effect was present, leading to the avulsion of the canine [20]. These reported ‘twist-effects’ are similar to the tooth movements described in this case report. However, in the current case report, the fixed FSW retainer was located in the upper jaw, while previous studies investigated fixed FSWs in the lower jaw [9,16,20,28]. It is hypothesized that the forces that contribute to the etiology of these unwanted tooth movements might be generated in three ways: (1) by the untwisting of the round flexible spiral wires (tooth movements generated by these forces might also be the reason for the observed root resorption localized at the 12, 11, and 21 on the panoramic radiograph from July 2017 (Figure 3D) [31]), (2) the mechanical deformation of the wire as a result of masticatory forces, and (3) the elastic deflection of the wire due to an inadequate passive bonding procedure [25]. One or more of the aforementioned etiologic factors might explain the situation described in this case report. To prevent a recurrence of these unwanted tooth movements, BRWs were bonded to the upper and lower jaws after the second orthodontic treatment. Fiber-reinforced composite or polyethylene splints could represent a viable alternative to conventional metallic bonded retention [32]. However, these materials have been shown to be less clinically reliable over time than stainless steel retainers [33]. A rectangular chain retainer could also have been a good alternative for the fixed retention in the upper and lower jaws. However, according to Arnold et al., BRWs achieve higher torque control [25]. Therefore, we chose to apply BRWs. Due to occlusal interferences with the lower canine, the retainer in the upper jaw was bonded to the incisors alone. However, it has been shown that significantly fewer rotational changes occur when fixed retainers are bonded from 13 to 23 compared to fixed retainers bonded from 12 to 22 [34]. Therefore, a VFR was prescribed to prevent rotational changes of the 13 and 23. According to a systematic review conducted by Bellini-Pereira et al., fixed retainers and VFRs in the upper jaw are equally effective in maintaining the end result of an orthodontic treatment (with a moderate level of certainty) [14]. Hence, a VFR placed in the upper jaw should stabilize the cuspids adequately. It has been shown that the failure of fixed orthodontic retainers occurs more frequently in the upper jaw compared to the lower jaw [10]. Therefore, if the fixed retainer fails from 12 to 22, the VFR will stabilize the alignment until the retainer can be repaired. The limitations of this case report include (1) the delay of the first follow-up appointment, which was eventually scheduled after 28 months due to the patient’s departure abroad and the COVID-19 pandemic. Fortunately, the fixed retainers did not fail in this period. However, the first follow-up appointment should have been scheduled earlier, since most failures of fixed retention occur in the first 6 months after the bonding of fixed retainers. In addition, failure is more frequent in the upper jaw [10]. (2) The existing root resorption should have been monitored earlier and more often during the active orthodontic re-treatment. (3) Moreover, case reports are considered to represent the lowest level of evidence. Implications for future research could include the design of studies with a long-term follow-up that assess variables that could influence the stability of fixed orthodontic retention, such as the periodontal and dental status of the patient, the type and dimensions of the retainer wire, the type and quantity of the composite used, and the placement technique.
5. Conclusions
In conclusion, fixed retainers appear to be effective in maintaining alignment after orthodontic treatment. However, unwanted tooth movements might result from the use of fixed flexible spiral wire retainers, requiring orthodontic re-treatment. Follow-up appointments are recommended to monitor the stability and to recognize unwanted tooth movements at an early stage. The results of this case report are of great importance for researchers, patients, and clinicians. In particular, dentists should be aware of these possible adverse effects of fixed flexible spiral wire retainers, since they regularly perform dental check-ups after orthodontic treatment. Therefore, dentists play an important role in recognizing these unwanted tooth movements.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/app13020922/s1, Supplementary File S1: CARE Checklist of information to include when writing a case report. Supplementary File S2: Timeline. Supplementary File S3: ESAS patient satisfaction evaluation part.
Author Contributions
This case report was conceived and designed by P.A.J.S. The final submitted manuscript was reviewed, revised, and approved by all three authors. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding. The APC was funded by the Academic Center for Dentistry Amsterdam.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Written informed consent was obtained from the patient to publish this paper.
Data Availability Statement
The dataset used for this case report is available from the corresponding author.
Acknowledgments
We thank the patient for his participation in this case report.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Oppenheim, A. Crisis in orthodontia. Part I. Tissue changes during retention. Int. J. Orthod. 1934, 20, 639–644. [Google Scholar]
- Thilander, B. Orthodontic relapse versus natural development. Am. J. Orthod. Dentofac. Orthop. 2000, 117, 562–563. [Google Scholar] [CrossRef] [PubMed]
- Massaro, C.; Miranda, F.; Janson, G.; Rodrigues de Almeida, R.; Pinzan, A.; Martins, D.R.; Garib, D. Maturational changes of the normal occlusion: A 40-year follow-up. Am. J. Orthod. Dentofac. Orthop. 2018, 154, 188–200. [Google Scholar] [CrossRef] [PubMed]
- Knierim, R.W. Invisible lower cuspid to cuspid retainer. Angle Orthod. 1973, 43, 218–220. [Google Scholar] [PubMed]
- Al-Jasser, R.; Al-Subaie, M.; Al-Jasser, N.; Al-Rasheed, A. Rotational relapse of anterior teeth following orthodontic treatment and circumferential supracrestal fiberotomy. Saudi Dent. J. 2020, 32, 293–299. [Google Scholar] [CrossRef] [PubMed]
- Aasen, T.O.; Espeland, L. An approach to maintain orthodontic alignment of lower incisors without the use of retainers. Eur. J. Orthod. 2005, 27, 209–214. [Google Scholar] [CrossRef] [PubMed]
- Fudalej, P.S.; Renkema, A.M. A brief history of orthodontic retention. Br. Dent. J. 2021, 230, 777–780. [Google Scholar] [CrossRef] [PubMed]
- Padmos, J.A.D.; Fudalej, P.S.; Renkema, A.M. Epidemiologic study of orthodontic retention procedures. Am. J. Orthod. Dentofac. Orthop. 2018, 153, 496–504. [Google Scholar] [CrossRef] [PubMed]
- Renkema, A.M.; Renkema, A.; Bronkhorst, E.; Katsaros, C. Long-term effectiveness of canine-to-canine bonded flexible spiral wire lingual retainers. Am. J. Orthod. Dentofac. Orthop. 2011, 139, 614–621. [Google Scholar] [CrossRef] [PubMed]
- Jedliński, M.; Grocholewicz, K.; Mazur, M.; Janiszewska-Olszowska, J. What causes failure of fixed orthodontic retention?—Systematic review and meta-analysis of clinical studies. Head Face Med. 2021, 17, 32. [Google Scholar] [CrossRef]
- Gelin, E.; Seidel, L.; Bruwier, A.; Albert, A.; Charavet, C. Innovative customized CAD/CAM nickel-titanium lingual retainer versus standard stainless-steel lingual retainer: A randomized controlled trial. Korean J. Orthod. 2020, 50, 373–382. [Google Scholar] [CrossRef] [PubMed]
- Radlanski, R.J.; Zain, N.D. Stability of the Bonded Lingual Wire Retainer? A Study of the Initial Bond Strength. J. Orofac. Orthop. 2004, 65, 321–335. [Google Scholar] [CrossRef] [PubMed]
- Shaughnessy, T.G.; Proffit, W.R.; Samara, S.A. Inadvertent tooth movement with fixed lingual retainers. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 277–286. [Google Scholar] [CrossRef] [PubMed]
- Bellini-Pereira, S.A.; Aliaga-Del Castillo, A.; Dos Santos, C.C.O.; Henriques, J.F.C.; Janson, G.; Normando, D. Treatment stability with bonded versus vacuum-formed retainers: A systematic review of randomized clinical trials. Eur. J. Orthod. 2022, 44, 187–196. [Google Scholar] [CrossRef]
- Juloski, J.; Glisic, B.; Vandevska-Radunovic, V. Long-term influence of fixed lingual retainers on the development of gingival recession: A retrospective, longitudinal cohort study. Angle Orthod. 2017, 87, 658–664. [Google Scholar] [CrossRef]
- Katsaros, C.; Livas, C.; Renkema, A.M. Unexpected complications of bonded mandibular lingual retainers. Am. J. Orthod. Dentofac. Orthop. 2007, 132, 838–841. [Google Scholar] [CrossRef]
- Renkema, A.M.; Fudalej, P.S.; Renkema, A.A.P.; Abbas, F.; Bronkhorst, E.; Katsaros, C. Gingival labial recessions in orthodontically treated and untreated individuals: A case-control study. J. Clin. Periodontol. 2013, 40, 631–637. [Google Scholar] [CrossRef]
- Seo, Y.J.; Kim, S.J.; Munkhshur, J.; Chung, K.R.; Ngan, P.; Kim, S.H. Treatment and retention of relapsed anterior open-bite with low tongue posture and tongue-tie: A 10-year follow-up. Korean J. Orthod. 2014, 44, 203–216. [Google Scholar] [CrossRef]
- Sfondrini, M.F.; Pascadopoli, M.; Beccari, S.; Beccari, G.; Rizzi, C.; Gandini, P.; Scribante, A. Orthodontic Fixed Retainer and Unwanted Movements of Lower Anterior Teeth: Case report. Case Rep. Dent. 2022, 2, 3100360. [Google Scholar] [CrossRef]
- Singh, P. Canine avulsion: An extreme complication of a fixed mandibular lingual retainer. Am. J. Orthod. Dentofac. Orthop. 2021, 160, 473–477. [Google Scholar] [CrossRef]
- Riley, D.S.; Barber, M.S.; Kienle, G.S.; Aronson, J.K.; von Schoen-Angerer, T.; Tugwell, P.; Kiene, H.; Helfand, M.; Altman, D.G.; Sox, H.; et al. CARE guidelines for case reports: Explanation and elaboration document. J. Clin. Epidemiol. 2017, 89, 218–235. [Google Scholar] [CrossRef]
- Richmond, S.; Shaw, W.C.; O'Brien, K.D.; Buchanan, I.B.; Jones, R.; Stephens, C.D.; Roberts, C.T.; Andrews, M. The development of the PAR Index (Peer Assessment Rating): Reliability and validity. Eur. J. Orthod. 1992, 14, 125–139. [Google Scholar] [CrossRef] [PubMed]
- Knaup, I.; Bartz, J.R.; Schulze-Späte, U.; Craveiro, R.B.; Kirschneck, C.; Wolf, M. Side effects of twistflex retainers—3D evaluation of tooth movement after retainer debonding. J. Orofac. Orthop. 2021, 82, 121–130. [Google Scholar] [CrossRef] [PubMed]
- Årtun, J.; Van ’t Hullenaar, R.; Doppel, D.; Kuijpers-Jagtman, A.M. Identification of orthodontic patients at risk of severe apical root resorption. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 448–455. [Google Scholar] [CrossRef] [PubMed]
- Arnold, D.T.; Dalstra, M.; Verna, C. Torque resistance of different stainless steel wires commonly used for fixed retainers in orthodontics. J. Orthod. 2016, 43, 121–129. [Google Scholar] [CrossRef]
- Littlewood, S.J.; Millett, D.T.; Doubleday, B.; Bearn, D.R.; Worthington, H.V. Retention procedures for stabilising tooth position after treatment with orthodontic braces. Cochrane Database Syst. Rev. 2016, 1, 1–139. [Google Scholar] [CrossRef]
- EFOSA’s Self Assessment System Quality Development in Orthodontics. Available online: https://esas.nu/ (accessed on 6 June 2022).
- Kučera, J.; Marek, I. Unexpected complications associated with mandibular fixed retainers: A retrospective study. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 202–211. [Google Scholar] [CrossRef]
- Pazera, P.; Fudalej, P.; Katsaros, C. Severe complication of a bonded mandibular lingual retainer. Am. J. Orthod. Dentofac. Orthop. 2012, 142, 406–409. [Google Scholar] [CrossRef]
- Kartal, Y.; Kaya, B. Fixed Orthodontic Retainers: A review. Turk. J. Orthod. 2019, 32, 110–114. [Google Scholar] [CrossRef]
- Segal, G.R.; Schiffman, P.H.; Tuncay, O.C. Meta analysis of the treatment-related factors of external apical root resorption. Orthod. Craniofac Res. 2004, 7, 71–78. [Google Scholar] [CrossRef]
- Karaman, A.I.; Kir, N.; Belli, S. Four applications of reinforced polyethylene fiber material in orthodontic practice. Am. J. Orthod. Dentofac. Orthop. 2002, 121, 650–654. [Google Scholar] [CrossRef] [PubMed]
- Scribante, A.; Sfondrini, M.F.; Broggini, S.; D'Allocco, M.; Gandini, P. Efficacy of Esthetic Retainers: Clinical Comparison between Multistranded Wires and Direct-Bond Glass Fiber-Rein forced Composite Splints. Int. J. Dent. 2011, 2011, 548356. [Google Scholar] [CrossRef] [PubMed]
- Naraghi, S.; Ganzer, N.; Bondemark, L.; Sonesson, M. Stability of maxillary anterior teeth after 2 years of retention in adolescents: A randomized controlled trial comparing two bonded and a vacuum-formed retainer. Eur. J. Orthod. 2021, 43, 152–158. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).