Abstract
The purpose of this systematic review was to assess the postoperative facial swelling (FS) and occlusion attained with clear aligner therapy (CAT) and fixed orthodontic therapy (OT) after orthognathic surgery (OS). The focused question was “Is there a difference in postoperative FS and occlusion attained with CAT and fixed OT after OS?” Indexed databases were searched up to and including October 2023 using different keywords. Original clinical studies that compared postoperative FS and occlusion attained with CAT and fixed OT after OS were included. Risk of bias (RoB) and quality of evidence were also assessed. Four retrospective studies were included. One study reported no difference in postoperative FS among patients that underwent CAT or fixed OT after OS. In one study, patients treated with CAT demonstrated less FS in the first post-surgical week than individuals that underwent fixed OT. In one study, postoperative occlusion was comparable among patients that underwent CAT or fixed OT, whereas in another, postoperative occlusion was better in patients that underwent fixed OT than CAT. All studies had a moderate RoB and none of the investigations were based on power-adjusted data. Based upon the sparsity and questionable quality of available evidence, there is a need to render a firm conclusion. However, it seems that CAT and fixed OT are comparable in relation to postoperative occlusion and FS after OS.
1. Introduction
Orthognathic surgery (OS) is usually performed to improve functional and esthetic parameters by repositioning the maxilla, mandible and/or the symphysis, particularly among patients that have either passed the pubertal growth spurt or may be unsuitable for orthodontic camouflage [1]. Surgical interventions such as LeFort and sagittal split osteotomies are often performed in conjunction to orthodontic tooth movement (OTM), particularly in patients with severe craniofacial deformities to produce a functional and stable occlusal outcome [2,3]. Following OS, orthodontic therapy (OT) using fixed appliances is conventionally performed to attain the desired tooth movement [4,5]. Clear aligner therapy (CAT) emerged as a potential therapeutic approach to induce OTM and treat dental malocclusions over two decades ago. These are removable appliances that can produce clinically acceptable orthodontic outcomes (OO) that are comparable to clinically satisfactory outcomes achieved using fixed OT [6,7]. With advancements in clinical orthodontics and related research, CAT has been shown to be an effective approach for the correction of not only mild to moderate but severe malocclusions [8], and it can also be used successfully after OS to attain OTM [9,10,11,12,13]. However, according to Robitaille et al. [13] esthetic outcomes in terms of occlusion are superior with fixed OT in contrast to CAT after OS. Papageorgiou et al. [14] also concluded that OT in adults using CAT is associated with worse esthetic outcomes in contrast to OT performed using fixed appliances.
Postoperative facial swelling (FS) after OS is a common yet significant concern as it can cause discomfort, hinder oral intake, affect speech and prolong the recovery period [9,10,11,12,13]. However, there is a paucity of research specifically comparing the impact of CAT and fixed OT on postoperative FS following OS. Guktaka et al. [10] used three-dimensional (3D) subtraction imaging to compare the volume of FS after OS in patients undergoing CAT (n = 11 patients) and fixed OT (n = 11 patients). In this study [10], OS interventions comprised LeFort-1 osteotomy (L1O), genioplasty and bilateral sagittal split osteotomy (BSSO). The results showed that patients undergoing CAT displayed a significantly smaller volume of FS compared with individuals undergoing fixed OT at a one-week follow-up [10]. The authors concluded that in the short term (up to the first post-operative week), FS is less in patients undergoing CAT than those undergoing fixed OT [10]. On the other hand, in a retrospective chart review and 3D morphometric study, Kankam et al. [12] showed no significant difference in FS among patients that either underwent CAT or fixed OT 6 months after OS. The authors suggested CAT can be used as an alternative to fixed OT after OS [12]. It is, however, pertinent to mention that the studies by Guktaka et al. [10] and Kankam et al. [12] were based on the supposition that peri-operative OT with CAT causes less post-operative FS than fixed OT; however, a scientific justification in this regard remained unclarified in these studies [10,12]. A systematic review of studies comparing FS and OO of CAT and fixed OT after OS is not yet reported in indexed databases.
With this background, the purpose of this systematic review was to assess the postoperative FS and OO attained with CAT and fixed OT after OS.
2. Materials and Methods
2.1. Focused Question and PICOS
The focused question was “Is there a difference in postoperative FS and occlusion attained with CAT and fixed OT after OS?” The PICOS format included P = patients undergoing OT after OS; I = patients treated with CAT; C = patients treated with fixed OT; O = FS and occlusion; S = clinical studies.
2.2. Inclusion and Exclusion Criteria
Original clinical studies that compared postoperative FS and occlusion attained with CAT and fixed OT after OS were included. Review articles, commentaries, perspectives, expert opinions and letters to the editor were excluded. Guidelines of the preferred reporting outcomes for systematic reviews and meta-analysis were followed to identify pertinent studies.
2.3. Literature Search
A comprehensive literature search was conducted up to and including October 2023 using indexed databases (PubMed/Medline, Scopus, EMBASE and ISI Web of Knowledge) and Google Scholar. The search was performed using various combinations of keywords: clear aligner therapy; clear aligners; complications; edema; facial swelling; fixed orthodontic therapy; orthodontics; orthognathic surgery; and tooth movement. Boolean operators (AND/OR) were utilized to refine the search and retrieve relevant articles without imposing any restrictions on language or publication date. Two authors (SAR and FJ) independently reviewed the titles and abstracts of potentially relevant original articles and matched them with the FQ and eligibility criteria (EC) to identify potentially suitable studies. In the subsequent step, full texts of the identified relevant studies were obtained and independently examined by the same authors (SAR and FJ). The full texts were matched against the FQ and eligibility criteria (EC) to finalize the selection of appropriate studies for inclusion in the review. Reference lists of potentially relevant original and review articles were also hand-searched to identify studies that could have remained unidentified during the initial electronic search. Any discrepancies or disagreements that arose during the study selection process were resolved through discussions among the two primary authors (SAR and FJ). If any conflicts remained unresolved, the opinions of two additional authors (PER and DM) were sought to reach a consensus and make final decisions regarding study inclusion. The involvement of these additional authors ensured a thorough and objective resolution of any disagreements, thus enhancing the overall validity and reliability of the study selection process. The literature search was performed according to the guidelines of the preferred reporting items for systematic reviews and meta-analyses [15].
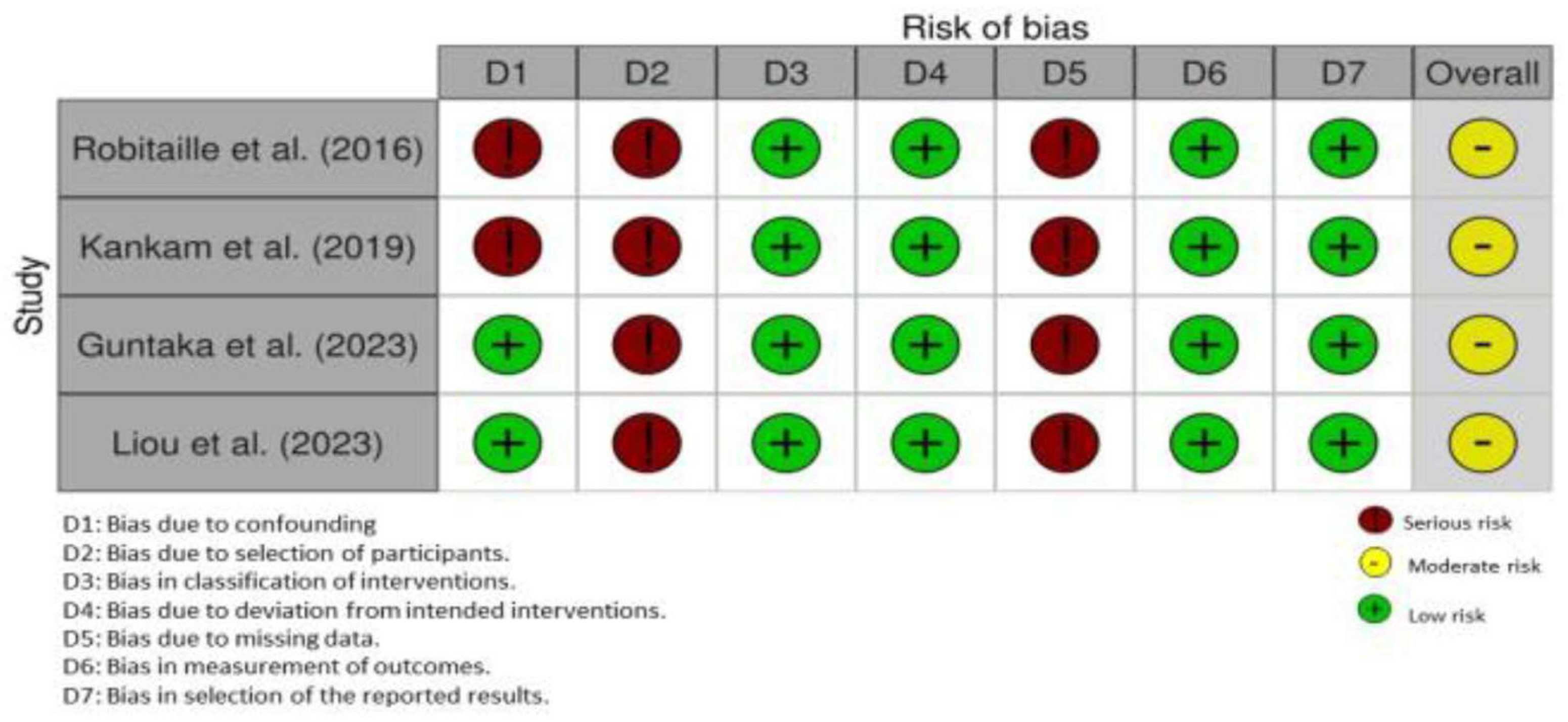
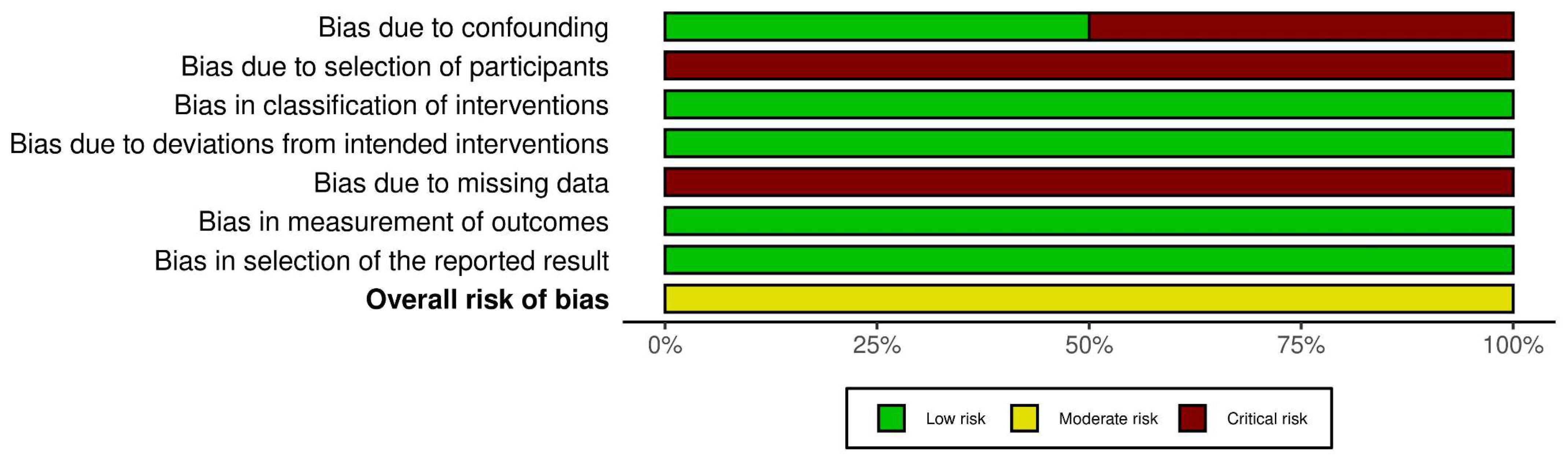
2.4. Risk of Bias Assessment
The risk of bias (RoB) was assessed using the Risk of Bias In Non-randomized Studies of Interventions (ROBINS-I) tool [16]. This tool comprises seven potential sources of bias: (a) bias due to confounding; (b) bias in selection of participants; (c) bias in classification of interventions; (d) bias due to deviations from intended interventions; (e) bias due to missing data; (f) bias in measurement of outcomes; and (g) bias in selection of the reported results. [16] Based on these criteria, studies were categorized as having a “low”, “moderate” or “critical” RoB.
2.5. Data Items and Extraction
Data extraction was independently performed by two authors (SR and FJ). The pertinent information was tabulated as follows: (a) study design; (b) reference; (c) number of participants; (d) groups (CAT and Fixed OT); (e) subject characteristics (mean age and gender in respective groups); (f) Body Mass Index (BMI); (g) type of orthognathic surgery; (h) operating time; (i) duration of hospital stay; (j) post-operative follow-up; (k) postoperative parameters (occlusal outcomes and FS); (l) duration of surgical orthodontic treatment; and (m) main outcomes and conclusions. Any discrepancies or disagreements related to the data extraction were resolved through discussion among the authors (SR and FJ). Remaining conflicts were resolved with two additional authors (DM and ER).
2.6. GRADE Analysis
The quality of evidence and strength of recommendations were assessed using the GRADE approach [17]. This methodological framework was employed to evaluate the certainty of evidence and inform the development of our recommendations based on the available literature.
3. Results
3.1. General Characteristics of Included Studies
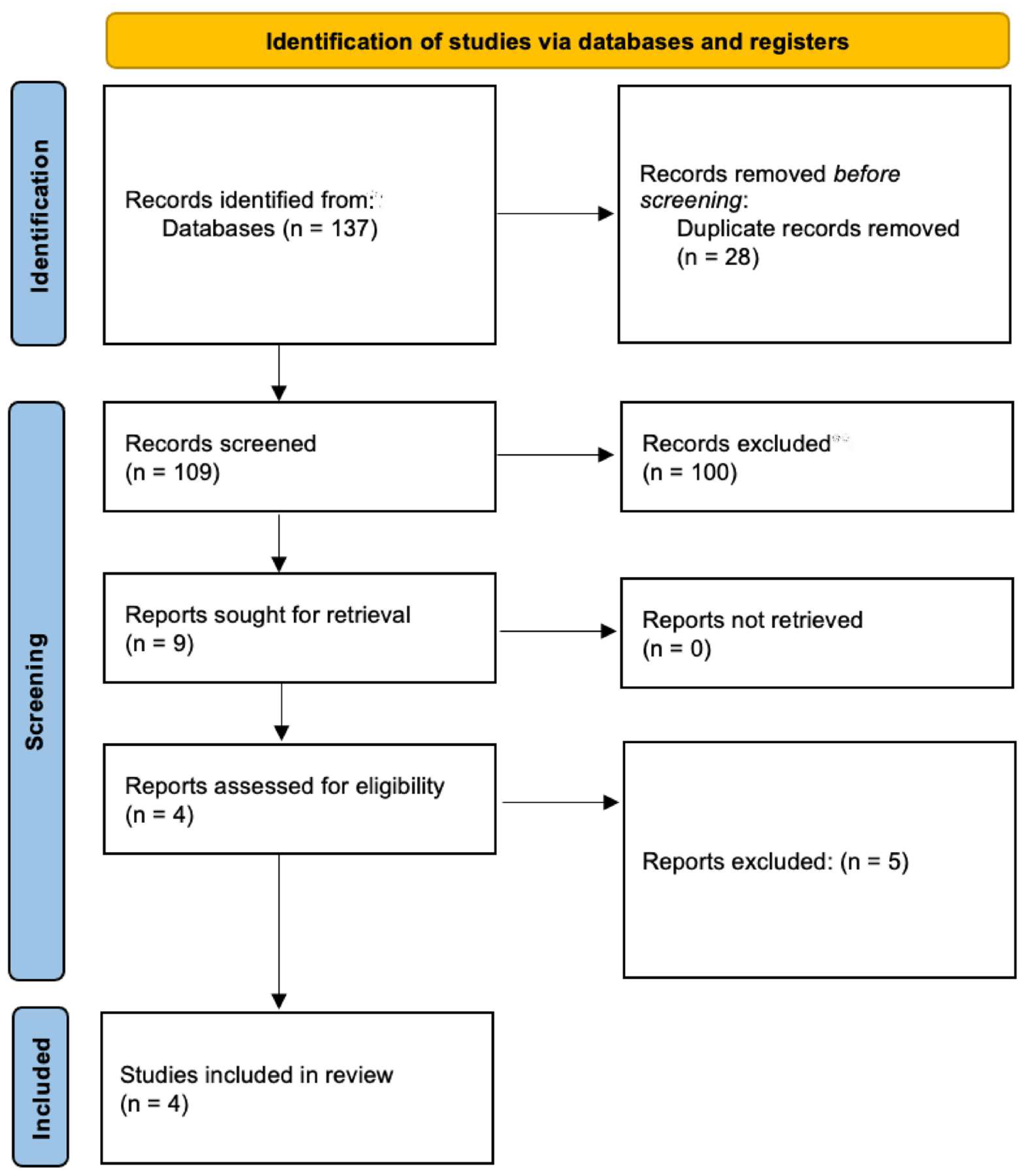
The initial search yielded 137 studies. After removal of duplicates, full texts of 109 studies were retrieved and assessed with reference to the FQ and EC. Four retrospective studies [10,11,12,13] addressed the FQ and fulfilled the EC. In these studies [10,11,12,13], the number of participants and their ages ranged between 22 and 29 and ~16 and 55.1 years, respectively. In the CAT and fixed OT groups, the number of males ranged between 46–64% and 24–64%, respectively [10,11,12,13]. Two studies [10,12] assessed the BMI of patients in the CAT and fixed OT groups. In the study by Kankam et al. [12], the BMI of patients in the CAT and fixed OT groups was 24.18 ± 3.79 and 23.49 ± 5.11 Kg/m2, respectively. The BMI of patients in the CAT and fixed OT groups was 20.9 ±2.4 and 25 ± 6.4 Kg/m2, respectively, in the study by Guntaka et al. [10]. In the study by Robitaille et al. [13] 37.5%, 50% and 12.5% individuals had skeletal class-II, skeletal class-III and anterior open bite, respectively, in the CAT group. In this study [13], 52%, 32%, 12% and 4% patients in the fixed OT group had skeletal class-II, skeletal class-III, anterior open bite and skeletal class-I with asymmetry, correspondingly. Data pertaining to baseline dental malocclusion were not reported in all studies (Table 1 and Figure 1) [10,11,12,13].

Table 1.
General characteristics of retrospective studies included.
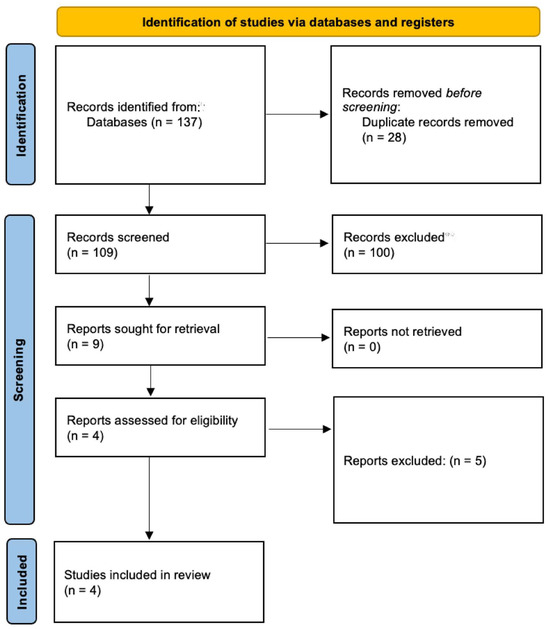
Figure 1.
PRISMA flow diagram.
3.2. Orthognathic Surgery-Related Parameters
In the study by Kankam et al. [12] all patients underwent BSSO and LeFort-1 osteotomy, whereas BSSO alone was performed in 50% and 36% patients in the CAT and fixed OT groups, respectively, in the study by Robitaille et al. [13] In this study [13], LeFort-1 osteotomy alone was performed in 37.5% and 8% individuals in the CAT and fixed OT groups, respectively. Nine% and 9% underwent BSSO alone in the CAT and fixed OT groups, respectively, in the study by Guntaka et al. [10], whereas 55% and 55% patients in the CAT and fixed OT groups, respectively, underwent LeFort-1 osteotomy alone [10]. In this study, 18% and 18% underwent LeFort-1 osteotomy with BSSO and genioplasty in the CAT and fixed OT groups, respectively [10]. In the study by Liou et al. [11] LeFort-1 osteotomy with BSSO and genioplasty was performed in 78.9% and 71.4% individuals in the CAT and fixed OT groups, respectively. In this study [11], LeFort-1 osteotomy with BSSO was performed in 21.1% and 28.6% of individuals in the CAT and fixed OT groups, respectively. Duration of follow-up was reported in studies by Guntaka et al. [10] and Kankam et al. [12], which was up to 7 weeks and 6 months, correspondingly (Table 2).

Table 2.
Orthognathic surgery-related parameters.
3.3. Main Study Outcomes
Two [10,12] and two [11,13] studies assessed FS and postoperative occlusion among patients who received CAT and fixed OT, respectively.
3.3.1. Postoperative Occlusion
In the study by Liou et al. [11] postoperative occlusion was comparable among patients that underwent CAT or fixed OT after OS. Liou et al. [11] assessed occlusal outcome using %reduction in the PAR index score, which had no significant difference between both the CAT and fixed OT groups (p = 0.142). Robitaille et al. [13] assessed occlusal outcome using the American Board of Orthodontics Objective Grading System. Results by Robitaille et al. [13] demonstrated that postoperative occlusion was better in patients that underwent fixed OT compared to CAT after OS (Table 3).

Table 3.
Outcomes of patients undergoing CAT and fixed OT after orthognathic surgery.
3.3.2. Facial Swelling
One study [12] reported that there is no difference in postoperative FS among patients that undergo CAT or FS after OS. In the study by Guntaka et al. [10] patients treated with CAT demonstrated less FS in the first post-surgical week compared with individuals that underwent fixed OT. In this study [10], postoperative FS was comparable in both groups at seven-weeks’ follow-up. Both studies [10,12] used 3D images to compare FS. The study by Guntaka et al. [10] measured between the middle and lower third of the face, excluding the nose. The study by Kankam et al. [12] measured between the middle and lower face.
3.3.3. Duration of Orthognathic Surgery
Two studies [10,12] reported the duration (in minutes) of OS. In the study by Kankam et al. [12] there was no significant difference in the duration of OS in patients that underwent CAT (303.9 ± 64.5 min) and fixed OT (287.3 ± 58.9 min). In the study by Guntaka et al. [10] the duration of OS was 180.5 ± 71.7 and 167.4 ± 44.1 min for patients in the CAT and fixed OT groups, respectively.
3.3.4. Hospitalization Rates
In one study [12], patients in the CAT and fixed OT were hospitalized post-operatively for 1.77 ± 0.6 and 2.2 ± 1.1 days, respectively.
3.3.5. Risk of Bias Assessment, Sample Size Estimation and GRADE Analysis
All studies [10,11,12,13] had a moderate RoB (Figure 2 and Figure 3). A prior sample size estimation was performed in none of the studies [10,11,12,13]. The quality of available evidence regarding the difference in postoperative FS and occlusion attained with CAT and fixed OT was very low (Table 4).
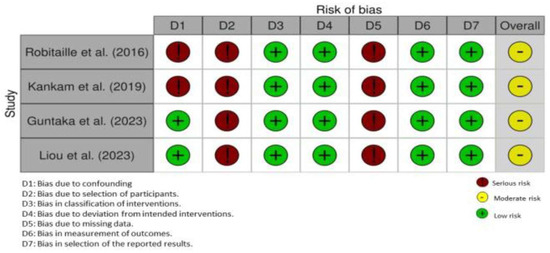
Figure 2.
Risk of bias assessment for each study using the traffic light plot [10,11,12,13].
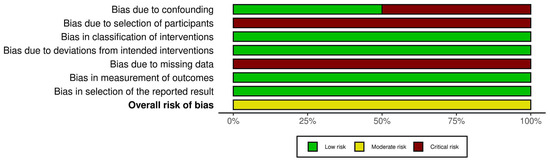
Figure 3.
Risk of bias assessment of each study using the weighted bar plot.

Table 4.
Grade analysis.
4. Discussion
The intended focus of the present systematic review was on identifying high-quality, evidence-based clinical studies, such as randomized controlled trials that evaluated the post-operative outcomes (in terms of FS and occlusion) in patients who underwent CAT or fixed OT after OS. With particular regard to FS, it is challenging to label this manifestation as a complication of OS as “post-operative swelling” when it is a normal bodily response to surgical trauma and is part of the normal healing process. While post-surgical swelling is not a complication per se, it is essential for healthcare professionals to monitor the extent and duration of swelling, as excessive or prolonged swelling may indicate other underlying issues or complications such as an abscess [18]. It is crucial to highlight that none of the studies [10,11,12,13] included in the investigation assessed both post-operative FS and occlusion simultaneously. Instead, out of the four clinical investigations [10,11,12,13] two studies [11,13] specifically addressed occlusion-related outcomes, while the remaining studies [10,12] assessed post-operative FS. Due to the limited number of studies available on either of the two parameters, FS or dentoskeletal occlusion, it was challenging to dedicate the entire manuscript to either topic exclusively. Instead, authors of the present investigation decided to incorporate all four available studies [10,11,12,13] to provide the most comprehensive and up-to-date review on the subject. The absence of studies assessing both aspects and potential post-surgical complications emphasize the need for further research to comprehensively and prospectively explore the effects of CAT and fixed OT in such a patient cohort. Nonetheless, by including all relevant studies [10,11,12,13], the authors aimed to present a thorough analysis of the current state of research on the topic despite the scarcity of individual studies on each parameter.
Based on a comprehensive review of the currently available literature, it is alluring to conclude that both CAT and fixed OT can produce satisfactory outcomes in relation to postoperative FS and occlusion following OS. However, it is crucial to exercise caution when interpreting such a conclusion. Prior sample-size estimation (SSE) or power analysis (PA) plays a pivotal role in ensuring the validity and reliability of study findings [19,20]. In other words, it is critical to determine an appropriate sample size (number of participants as in the present scenario) before conducting a study to avoid underpowered or overpowered investigations, which can otherwise lead to publication bias and/or inaccurate conclusions [21,22]. Amongst the studies [10,11,12,13] assessed, the number of participants and their ages ranged between 22 and 29; however, a prior SSE was performed in none of them. It is worth mentioning that a small sample may not adequately represent the target population, leading to limited external validity or generalizability of the study findings, [23] and it can result in imprecise estimates of population parameters, such as means, proportions, or effect sizes [24]. From the design perspective, all studies [10,11,12,13] were retrospective. Evaluation of retrospective studies comes with several limitations including selection bias (as the studies rely on pre-existing data), uncontrolled confounding factors, blinding of operators, allocation concealment of interventions and limited generalizability and validity [23,25]. Furthermore, all studies had a moderate RoB and the GRADE analysis revealed that the importance of the included studies were either uncertain or limited. Therefore, the findings of the included studies [10,11,12,13] should be interpreted with prudence, recognizing the potential for biases and uncertainties that could influence the results. The authors suggest that additional well-designed and adequately powered studies, preferably randomized controlled trials with well-defined primary and secondary outcome variables and long-term follow-up (of at least 12 months) are required to determine whether the orthodontic treatment mode (CAT versus fixed OT) has any impact on the esthetic and functional outcome in patients after OS.
A BMI ranging between 18.5 and 24.9 Kg/m2 is considered normal [26]. In a prospective volumetric analysis, van der Vlis et al. [27] used three-dimensional photographs to quantify post-operative FS after OS (L1O and/or BSSO) in relation to BMI. The results showed that patients with a higher BMI experience a greater amount of FS and fastest rate of its resolution in initial postoperative weeks compared with individuals with a lower BMI [27]. In the present systematic review, two studies [10,12] reported the mean BMI of patients that underwent CAT or fixed OT after OS, which ranged between approximately 24 and 25 Kg/m2. Due to the divergent results observed in these studies [10,12] concerning facial symmetry (FS) and the limited range of average BMI, establishing a direct correlation between FS and BMI is challenging. Moreover, the severity of post-surgical edema/FS is influenced by factors such as operator(s’) skills and the complexity and duration of the intervention [28]. Based on the methodology of the included studies [10,11,12,13], all surgical and post-operative orthodontic interventions were performed by experienced operators. The mean duration of intervention (operating time [OT]) and follow-up was reported in 50% of the studies [10,12] which ranged between approximately 180 and 300 min and 7 and 24 weeks, respectively. Despite variations in OT and duration of follow-up, these studies [10,12] reported conflicting results in terms of post-operative FS. There were limited results regarding the surgical duration and total treatment duration with CAT versus fixed OT.
From a clinical perspective, CAT has allowed clinicians to plan presurgical decompensatory tooth movements in digital platforms such as Invisalign’s ClinCheck and virtually simulate the surgery through a bite jump. A study by Cong et al. evaluated presurgical orthodontic decompensation with CAT and reported that common tooth movements for decompensation were highly accurate with the use of CAT [29]. Despite the results in this study, it is incumbent on clinicians to approach the virtually planned tooth movements with caution as the planned tooth movements made by the technician may not be predictable or attainable clinically. Moreover, the use of aligners instead of fixed orthodontic appliances (brackets, wires and surgical hooks) during the operative and postoperative phases of treatment may pose challenges to orthognathic surgeons and orthodontists particularly regarding the use of intermaxillary elastics for occlusal stabilization and settling during and after the OS, respectively [30]. Nonetheless, this perceived deficiency in CAT can be overcome by using auxiliaries such as buttons, brackets, Ivy loops, Erich arch bars and intermaxillary fixation screws, amongst others, in conjunction with the conventional clear aligners. Another important consideration regarding the use of CAT in OS, is that in the postoperative phase, OS patients oftentimes have limited mouth opening from stripping of muscles intraoperatively and from postoperative edema. In the setting of these postoperative limitations, rescanning for ordering finishing and detailing aligners can be challenging. It was noted by Moshiri that a presurgical scan of patients, that has been fully decompensated, can be used to order more aligners to have immediately after surgery for finishing and detailing [31]. However, Moshiri noted that this is not recommended in multi-piece LeFort osteotomies due to aligners not fitting properly postoperatively [31]. Regarding postoperative stability, a study by Moon et al. found no significant difference between the CAT and fixed OT groups up to 6 months after OS [32]. Another study by Mangat et al. had similar results of no significant difference in postoperative stability after one year between the CAT and fixed OT groups [33]. However, limitations in the use of CAT have been reported in the case of multiple piece LeFort-I osteotomies due to the challenges associated with stabilizing the transverse dimension of the maxilla during the postoperative phase with clear aligners [9]. Despite these perceived limitations with the use of CAT in OS, patient comfort and oral hygiene are typically reported to be better in patients with CAT. For instance, a study by de Leyva et al. [34] showed that patients who underwent OS treated with CAT had superior periodontal health and quality of life than those treated with fixed OT. There is a pressing requirement for the execution of studies, particularly randomized controlled trials, that focus on evaluating and contrasting patient-centric outcome measures, also known as patient-reported outcome measures (PROMs), between fixed orthodontic appliances and clear aligners. Similar comparisons have been conducted in the context of complex orthodontic cases without the necessity for orthognathic surgical intervention [35]. Such comparisons have been made when treating difficult cases by ordinary orthodontic treatment without resorting to orthognathic surgery. Facilitating oral/periodontal health and improving patient comfort with treatment may be of particular importance in patients undergoing OS who often exhibit challenges in effectively maintaining proper oral hygiene through the course of OT and may also face psychological challenges associated with overall treatment adaptation [34,36,37]. The aforementioned studies indicate potential advantages and limitations regarding the use of CAT on OS, as well as highlight the need to develop standardized and evidence-based treatment protocols. Further research is needed in this respect.
5. Conclusions
Based upon the sparsity and questionable quality of available evidence it is necessary to render a firm conclusion. However, it seems that CAT and fixed OT are comparable in relation to postoperative occlusion and FS after OS.
Author Contributions
Conceptualization, S.A.R.; methodology, S.A.R., B.A.B., F.J., P.E.R. and D.M.; software, F.J. and B.A.B.; formal analysis, S.A.R., B.A.B. and F.J.; investigation, S.A.R. and F.J.; writing—S.A.R., B.A.B., F.J., P.E.R. and D.M.; writing—review and editing, S.A.R., B.A.B., F.J., P.E.R. and D.M.; supervision, F.J., P.E.R. and D.M; project administration, F.J. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data is available upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Huang, C.S.; Hsu, S.S.; Chen, Y.R. Systematic review of the surgery-first approach in orthognathic surgery. Biomed. J. 2014, 37, 184–190. [Google Scholar] [CrossRef] [PubMed]
- Yuan, H.; Zhu, X.; Lu, J.; Dai, J.; Fang, B.; Shen, S.G. Accelerated orthodontic tooth movement following le fort I osteotomy in a rodent model. J. Oral. Maxillofac. Surg. 2014, 72, 764–772. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.M.; Hsu, H.J.; Liang, S.W.; Chen, P.H.; Hsu, K.J.; Tseng, Y.C. Two-thirds anteroposterior ramus length is the preferred osteotomy point for intraoral vertical ramus osteotomy. Clin. Oral. Investig. 2022, 26, 1229–1239. [Google Scholar] [CrossRef] [PubMed]
- Hohoff, A.; Joos, U.; Meyer, U.; Ehmer, U.; Stamm, T. The spectrum of Apert syndrome: Phenotype, particularities in orthodontic treatment, and characteristics of orthognathic surgery. Head Face Med. 2007, 3, 10. [Google Scholar] [CrossRef]
- Breuning, K.H.; van Strijen, P.J.; Prahl-Andersen, B.; Tuinzing, D.B. Duration of orthodontic treatment and mandibular lengthening by means of distraction or bilateral sagittal split osteotomy in patients with Angle Class II malocclusions. Am. J. Orthod. Dentofac. Orthop. 2005, 127, 25–29. [Google Scholar] [CrossRef] [PubMed]
- Robertson, L.; Kaur, H.; Fagundes, N.C.F.; Romanyk, D.; Major, P.; Flores Mir, C. Effectiveness of clear aligner therapy for orthodontic treatment: A systematic review. Orthod. Craniofac. Res. 2020, 23, 133–142. [Google Scholar] [CrossRef]
- Ke, Y.; Zhu, Y.; Zhu, M. A comparison of treatment effectiveness between clear aligner and fixed appliance therapies. BMC Oral. Health 2019, 19, 24. [Google Scholar] [CrossRef]
- Jaber, S.T.; Hajeer, M.Y.; Burhan, A.S. The Effectiveness of In-house Clear Aligners and Traditional Fixed Appliances in Achieving Good Occlusion in Complex Orthodontic Cases: A Randomized Control Clinical Trial. Cureus 2022, 14, e30147. [Google Scholar] [CrossRef]
- Kankam, H.K.N.; Gupta, H.; Sawh-Martinez, R.; Steinbacher, D.M. Segmental Multiple-Jaw Surgery without Orthodontia: Clear Aligners Alone. Plast. Reconstr. Surg. 2018, 142, 181–184. [Google Scholar] [CrossRef]
- Guntaka, P.K.; Kiang, K.; Caprio, R.; Parry, G.J.; Padwa, B.L.; Resnick, C.M. Do patients treated with Invisalign have less swelling after orthognathic surgery than those with fixed orthodontic appliances? Am. J. Orthod. Dentofacial. Orthop. 2023, 163, 243–251. [Google Scholar] [CrossRef]
- Liou, Y.J.; Chen, P.R.; Tsai, T.Y.; Lin, S.; Chou, P.Y.; Lo, C.M.; Chen, Y.R. Comparative assessment of orthodontic and aesthetic outcomes after orthognathic surgery with clear aligner or fixed appliance therapy. Plast. Reconstr. Surg. 2023. [Google Scholar] [CrossRef] [PubMed]
- Kankam, H.; Madari, S.; Sawh-Martinez, R.; Bruckman, K.C.; Steinbacher, D.M. Comparing Outcomes in Orthognathic Surgery Using Clear Aligners Versus Conventional Fixed Appliances. J. Craniofac. Surg. 2019, 30, 1488–1491. [Google Scholar] [CrossRef] [PubMed]
- Robitaille, P. Duration and Outcomes of Combined Orthodontic-Surgical Treatment with Invisalign®. 2016. Available online: https://papyrus.bib.umontreal.ca/xmlui/handle/1866/16432 (accessed on 25 September 2023).
- Papageorgiou, S.N.; Koletsi, D.; Iliadi, A.; Peltomaki, T.; Eliades, T. Treatment outcome with orthodontic aligners and fixed appliances: A systematic review with meta-analyses. Eur. J. Orthod. 2020, 42, 331–343. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Hinneburg, I. ROBINS-1: A tool for asssessing risk of bias in non-randomised studies of interventions. Med. Monatsschr. Pharm. 2017, 40, 175–177. [Google Scholar] [PubMed]
- Guyatt, G.H.; Oxman, A.D.; Vist, G.E.; Kunz, R.; Falck-Ytter, Y.; Alonso-Coello, P.; Schünemann, H.J. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008, 336, 924–926. [Google Scholar] [CrossRef]
- Varghese, L.; Agarwal, P.; Rupa, V. Unusual complication of dental extraction: Lingual abscess. Indian J. Dent. Res. 2013, 24, 772–774. [Google Scholar] [CrossRef]
- Delucchi, K.L. Sample size estimation in research with dependent measures and dichotomous outcomes. Am. J. Public Health 2004, 94, 372–377. [Google Scholar] [CrossRef]
- Kang, H. Sample size determination and power analysis using the G*Power software. J. Educ. Eval. Health Prof. 2021, 18, 17. [Google Scholar] [CrossRef]
- Lin, L.; Chu, H. Quantifying publication bias in meta-analysis. Biometrics 2018, 74, 785–794. [Google Scholar] [CrossRef]
- Olson, C.M. Publication bias. Acad. Emerg Med. 1994, 1, 207–209. [Google Scholar] [CrossRef] [PubMed]
- Grimes, D.A.; Schulz, K.F. Bias and causal associations in observational research. Lancet 2002, 359, 248–252. [Google Scholar] [CrossRef] [PubMed]
- Julious, S.A. Sample sizes for clinical trials with normal data. Stat. Med. 2004, 23, 1921–1986. [Google Scholar] [CrossRef] [PubMed]
- Vandenbroucke, J.P. Observational research, randomised trials, and two views of medical science. PLoS Med. 2008, 5, e67. [Google Scholar] [CrossRef]
- Flegal, K.M. Body-mass index and all-cause mortality. Lancet 2017, 389, 2284–2285. [Google Scholar] [CrossRef]
- van der Vlis, M.; Dentino, K.M.; Vervloet, B.; Padwa, B.L. Postoperative swelling after orthognathic surgery: A prospective volumetric analysis. J. Oral. Maxillofac. Surg. 2014, 72, 2241–2247. [Google Scholar] [CrossRef] [PubMed]
- Sortino, F.; Cicciù, M. Strategies used to inhibit postoperative swelling following removal of impacted lower third molar. Dent. Res. J. 2011, 8, 162–171. [Google Scholar] [CrossRef]
- Cong, A.; Ruellas, A.C.O.; Tai, S.K.; Loh, C.T.; Barkley, M.; Yatabe, M.; Caminiti, M.; Massaro, C.; Bianchi, J.; Deleat-Besson, R.; et al. Presurgical orthodontic decompensation with clear aligners. Am. J. Orthod. Dentofacial. Orthop. 2022, 162, 538–553. [Google Scholar] [CrossRef]
- Jaber, S.T.; Hajeer, M.Y.; Sultan, K. Treatment Effectiveness of Clear Aligners in Correcting Complicated and Severe Malocclusion Cases Compared to Fixed Orthodontic Appliances: A Systematic Review. Cureus 2023, 15, e38311. [Google Scholar] [CrossRef]
- Moshiri, M. Considerations for treatment of patients undergoing orthognathic surgery using clear aligners. Am. J. Orthod. Dentofac. Orthop. Clin. Companion 2022, 2, 229–239. [Google Scholar] [CrossRef]
- Moon, C.; Sándor, G.K.; Ko, E.C.; Kim, Y.-D. Postoperative Stability of Patients Undergoing Orthognathic Surgery with Orthodontic Treatment Using Clear Aligners: A Preliminary Study. Appl. Sci. 2021, 11, 11216. [Google Scholar] [CrossRef]
- Mangat, H. A Comparative Analysis of Orthognathic Surgical Stability between Fixed Appliances and Clear Aligner Orthodontic Therapy. J. Oral Maxillofac. Surg. 2021, 79, e83–e84. [Google Scholar] [CrossRef]
- de Leyva, P.; Eslava, J.M.; Hernandez-Alfaro, F.; Acero, J. Orthognathic surgery and aligners. A comparative assessment of periodontal health and quality of life in postsurgical orthodontic treatment with aligners versus traditional fixed appliances: A randomized controlled trial. Med. Oral. Patol. Oral. Cir. Bucal. 2023, 28, e208–e216. [Google Scholar] [CrossRef] [PubMed]
- Jaber, S.T.; Hajeer, M.Y.; Burhan, A.S.; Latifeh, Y. The Effect of Treatment With Clear Aligners Versus Fixed Appliances on Oral Health-Related Quality of Life in Patients With Severe Crowding: A One-Year Follow-Up Randomized Controlled Clinical Trial. Cureus 2022, 14, e25472. [Google Scholar] [CrossRef] [PubMed]
- Karkhanechi, M.; Chow, D.; Sipkin, J.; Sherman, D.; Boylan, R.J.; Norman, R.G.; Craig, R.G.; Cisneros, G.J. Periodontal status of adult patients treated with fixed buccal appliances and removable aligners over one year of active orthodontic therapy. Angle Orthod 2013, 83, 146–151. [Google Scholar] [CrossRef]
- Azaripour, A.; Weusmann, J.; Mahmoodi, B.; Peppas, D.; Gerhold-Ay, A.; Van Noorden, C.J.F.; Willershausen, B. Braces versus Invisalign®: Gingival parameters and patients’ satisfaction during treatment: A cross-sectional study. BMC Oral. Health 2015, 15, 69. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).