Technological Aspects and Performance of High Entropy Alloys with Potential Application in Dental Restorations and Reducing Implant Failure
Abstract
:1. Introduction
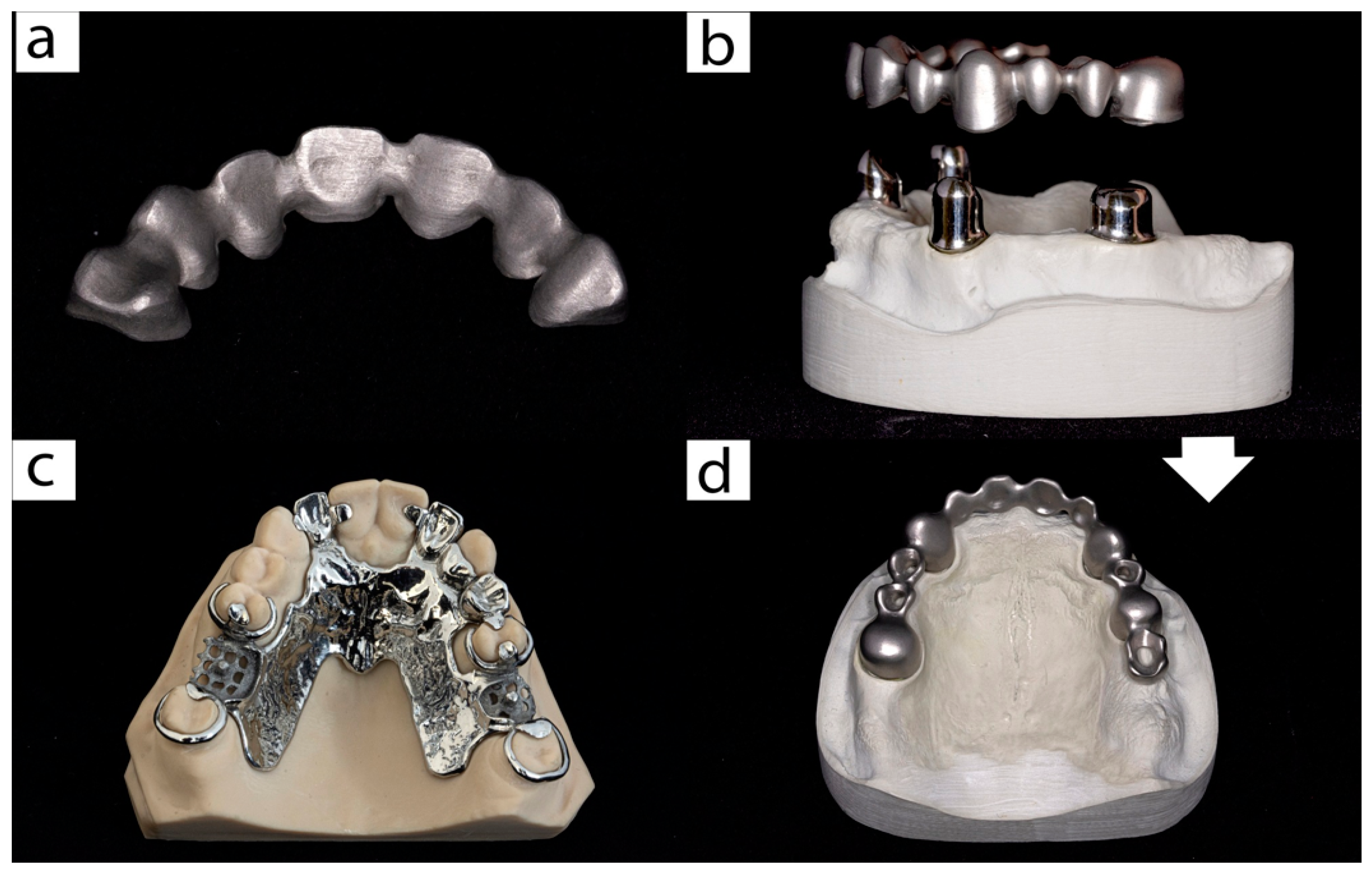
2. Data Sources and Search Strategy
3. The Oral Cavity Relationship with Prosthodontics and Implant Dentistry
4. BioHEAs
4.1. Bulk
4.2. Coatings
5. In Vitro Biological Performance of HEA
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Tharani Kumar, S.; Prasanna Devi, S.; Krithika, C.; Raghavan, R. Review of metallic biomaterials in dental applications. J. Pharm. Bioallied Sci. 2020, 12, 14. [Google Scholar] [CrossRef] [PubMed]
- Han, X.; Sawada, T.; Schille, C.; Schweizer, E.; Scheideler, L.; Geis-Gerstorfer, J.; Rupp, F.; Spintzyk, S. Comparative Analysis of Mechanical Properties and Metal-Ceramic Bond Strength of Co-Cr Dental Alloy Fabricated by Different Manufacturing Processes. Materials 2018, 11, 1801. [Google Scholar] [CrossRef] [PubMed]
- Messer, R.; Wataha, J. Dental Materials: Biocompatibility. In Encyclopedia of Materials: Science and Technology; Elsevier: Amsterdam, The Netherlands, 2002; pp. 1–10. [Google Scholar]
- de Matos, J.D.M.; Dos-Santos, A.C.M.; Nakano, L.J.N.; De-Vasconcelos, J.E.L.; Andrade, V.C.; Nishioka, R.S.; Bottino, M.A.; da Rocha Scalzer Lopes, G. Metal Alloys in Dentistry: An Outdated Material or Required for Oral Rehabilitation? Int. J. Odontostomatol. 2021, 15, 702–711. [Google Scholar] [CrossRef]
- Reclaru, L.; Lüthy, H.; Eschler, P.-Y.; Blatter, A.; Susz, C. Corrosion behaviour of cobalt–chromium dental alloys doped with precious metals. Biomaterials 2005, 26, 4358–4365. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Jang, S.H.; Kim, Y.; Son, J.; Min, B.; Kim, K.H.; Kwon, T.Y. Microstructures and Mechanical Properties of Co-Cr Dental Alloys Fabricated by Three CAD/CAM-Based Processing Techniques. Materials 2016, 9, 596. [Google Scholar] [CrossRef]
- Cabrita, J.; Mendes, T.; Martins, J.; Lopes, L. Removable partial denture metal framework manufactured by selective laser melting technology—A clinical report. Rev. Port. Estomatol. Med. Dentária Cir. Maxilofac. 2021, 62, 109–113. [Google Scholar] [CrossRef]
- Venkatesh, K.V.; Nandini, V.V. Direct Metal Laser Sintering: A Digitised Metal Casting Technology. J. Indian Prosthodont. Soc. 2013, 13, 389–392. [Google Scholar] [CrossRef]
- Romonti, D.E.; Gomez Sanchez, A.V.; Milošev, I.; Demetrescu, I.; Ceré, S. Effect of anodization on the surface characteristics and electrochemical behaviour of zirconium in artificial saliva. Mater. Sci. Eng. C 2016, 62, 458–466. [Google Scholar] [CrossRef]
- Davis, R.; Singh, A.; Jackson, M.J.; Coelho, R.T.; Prakash, D.; Charalambous, C.P.; Ahmed, W.; da Silva, L.R.R.; Lawrence, A.A. A comprehensive review on metallic implant biomaterials and their subtractive manufacturing. Int. J. Adv. Manuf. Technol. 2022, 120, 1473–1530. [Google Scholar] [CrossRef]
- Gueye, M.; Ammar-Merah, S.; Nowak, S.; Decorse, P.; Chevillot-Biraud, A.; Perrière, L.; Couzinie, J.P.; Guillot, I.; Dirras, G. Study of the stability under in vitro physiological conditions of surface silanized equimolar HfNbTaTiZr high-entropy alloy: A first step toward bio-implant applications. Surf. Coat. Technol. 2020, 385, 125374. [Google Scholar] [CrossRef]
- Gurel, S.; Nazarahari, A.; Canadinc, D.; Cabuk, H.; Bal, B. Assessment of biocompatibility of novel TiTaHf-based high entropy alloys for utility in orthopedic implants. Mater. Chem. Phys. 2021, 266, 124573. [Google Scholar] [CrossRef]
- Giesen, E.B.W.; Van Eijden, T.M.G.J. The Three-dimensional Cancellous Bone Architecture of the Human Mandibular Condyle. J. Dent. Res. 2000, 79, 957–963. [Google Scholar] [CrossRef] [PubMed]
- Liu, R.; Li, X.; Hu, X.; Dong, H. Surface modification of a medical grade Co-Cr-Mo alloy by low-temperature plasma surface alloying with nitrogen and carbon. Surf. Coat. Technol. 2013, 232, 906–911. [Google Scholar] [CrossRef]
- Gurel, S.; Nazarahari, A.; Canadinc, D.; Gerstein, G.; Maier, H.J.; Cabuk, H.; Bukulmez, T.; Cananoglu, M.; Yagci, M.B.; Toker, S.M.; et al. From corrosion behavior to radiation response: A comprehensive biocompatibility assessment of a CoCrMo medium entropy alloy for utility in orthopedic and dental implants. Intermetallics 2022, 149, 107680. [Google Scholar] [CrossRef]
- Ionita, D.; Man, I.; Demetrescu, I. The Behaviour of Electrochemical Deposition of Phosphate Coating on CoCr Bio Alloys. Key Eng. Mater. 2007, 330–332, 545–548. [Google Scholar] [CrossRef]
- Feng, J.; Tang, Y.; Liu, J.; Zhang, P.; Liu, C.; Wang, L. Bio-high entropy alloys: Progress, challenges, and opportunities. Front. Bioeng. Biotechnol. 2022, 10, 977282. [Google Scholar] [CrossRef]
- Motallebzadeh, A. Evaluation of mechanical properties and in vitro biocompatibility of TiZrTaNbHf refractory high-entropy alloy film as an alternative coating for TiO2 layer on NiTi alloy. Surf. Coat. Technol. 2022, 448, 128918. [Google Scholar] [CrossRef]
- Aksoy, C.B.; Canadinc, D.; Yagci, M.B. Assessment of Ni ion release from TiTaHfNbZr high entropy alloy coated NiTi shape memory substrates in artificial saliva and gastric fluid. Mater. Chem. Phys. 2019, 236, 121802. [Google Scholar] [CrossRef]
- Olms, C.; Yahiaoui-Doktor, M.; Remmerbach, T.W. Contact allergies to dental materials. Swiss Dent. J. 2019, 129, 571–579. [Google Scholar]
- Al-Imam, H.; Benetti, A.R.; Özhayat, E.B.; Pedersen, A.M.L.; Johansen, J.D.; Thyssen, J.P.; Jellesen, M.S.; Gotfredsen, K. Cobalt release and complications resulting from the use of dental prostheses. Contact Dermat. 2016, 75, 377–383. [Google Scholar] [CrossRef]
- Zigante, M.; Rincic Mlinaric, M.; Kastelan, M.; Perkovic, V.; Trinajstic Zrinski, M.; Spalj, S. Symptoms of titanium and nickel allergic sensitization in orthodontic treatment. Prog. Orthod. 2020, 21, 17. [Google Scholar] [CrossRef] [PubMed]
- Hostýnek, J.J.; Reagan, K.E.; Maibach, H.I. Nickel Allergic Hypersensitivity: Prevalence and Incidence by Country, Gender, Age, and Occupation. In Nickel and the Skin; CRC Press: Boca Raton, FL, USA, 2002; pp. 39–82. [Google Scholar]
- Regulation (EU) 2017/745 of the European Parliament and of the Council of 5 April 2017 on Medical Devices. Available online: https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=CELEX%3A32017R0745 (accessed on 14 April 2023).
- Grosgogeat, B.; Vaicelyte, A.; Gauthier, R.; Janssen, C.; Le Borgne, M. Toxicological Risks of the Cobalt–Chromium Alloys in Dentistry: A Systematic Review. Materials 2022, 15, 5801. [Google Scholar] [CrossRef]
- Peighambardoust, N.S.; Alamdari, A.A.; Unal, U.; Motallebzadeh, A. In vitro biocompatibility evaluation of Ti1.5ZrTa0.5Nb0.5Hf0.5 refractory high-entropy alloy film for orthopedic implants: Microstructural, mechanical properties and corrosion behavior. J. Alloys Compd. 2021, 883, 160786. [Google Scholar] [CrossRef]
- Wang, H.; Liu, P.; Chen, X.; Lu, Q.; Zhou, H. Mechanical properties and corrosion resistance characterization of a novel Co36Fe36Cr18Ni10 high-entropy alloy for bioimplants compared to 316L alloy. J. Alloys Compd. 2022, 906, 163947. [Google Scholar] [CrossRef]
- George, E.P.; Raabe, D.; Ritchie, R.O. High-entropy alloys. Nat. Rev. Mater. 2019, 4, 515–534. [Google Scholar] [CrossRef]
- Miracle, D.B.; Senkov, O.N. A critical review of high entropy alloys and related concepts. Acta Mater. 2017, 122, 448–511. [Google Scholar] [CrossRef]
- Miracle, D.B. High entropy alloys as a bold step forward in alloy development. Nat. Commun. 2019, 10, 1805. [Google Scholar] [CrossRef]
- Normand, J.; Moriche, R.; García-Garrido, C.; Sepúlveda Ferrer, R.E.; Chicardi, E. Development of a TiNbTaMoZr-Based High Entropy Alloy with Low Young’s Modulus by Mechanical Alloying Route. Metals 2020, 10, 1463. [Google Scholar] [CrossRef]
- Nguyen, V.T.; Qian, M.; Shi, Z.; Tran, X.Q.; Fabijanic, D.M.; Joseph, J.; Qu, D.D.; Matsumura, S.; Zhang, C.; Zhang, F.; et al. Cuboid-like nanostructure strengthened equiatomic Ti–Zr–Nb–Ta medium entropy alloy. Mater. Sci. Eng. A 2020, 798, 140169. [Google Scholar] [CrossRef]
- Hua, N.; Wang, W.; Wang, Q.; Ye, Y.; Lin, S.; Zhang, L.; Guo, Q.; Brechtl, J.; Liaw, P.K. Mechanical, corrosion, and wear properties of biomedical Ti–Zr–Nb–Ta–Mo high entropy alloys. J. Alloys Compd. 2021, 861, 157997. [Google Scholar] [CrossRef]
- Elshahawy, W.; Watanabe, I. Biocompatibility of dental alloys used in dental fixed prosthodontics. Tanta Dent. J. 2014, 11, 150–159. [Google Scholar] [CrossRef]
- Haugli, K.H.; Syverud, M.; Samuelsen, J.T. Ion release from three different dental alloys—Effect of dynamic loading and toxicity of released elements. Biomater. Investig. Dent. 2020, 7, 71–79. [Google Scholar] [CrossRef] [PubMed]
- Heitz-Mayfield, L.J.A.; Salvi, G.E. Peri-implant mucositis. J. Clin. Periodontol. 2018, 45, S237–S245. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, F.; Derks, J.; Monje, A.; Wang, H.-L. Peri-implantitis. J. Clin. Periodontol. 2018, 45, S246–S266. [Google Scholar] [CrossRef] [PubMed]
- Andrei, M.; Dinischiotu, A.; Didilescu, A.C.; Ionita, D.; Demetrescu, I. Periodontal materials and cell biology for guided tissue and bone regeneration. Ann. Anat. Anat. Anz. 2018, 216, 164–169. [Google Scholar] [CrossRef]
- Ishimoto, T.; Ozasa, R.; Nakano, K.; Weinmann, M.; Schnitter, C.; Stenzel, M.; Matsugaki, A.; Nagase, T.; Matsuzaka, T.; Todai, M.; et al. Development of TiNbTaZrMo bio-high entropy alloy (BioHEA) super-solid solution by selective laser melting, and its improved mechanical property and biocompatibility. Scr. Mater. 2021, 194, 113658. [Google Scholar] [CrossRef]
- Rashidy Ahmady, A.; Ekhlasi, A.; Nouri, A.; Haghbin Nazarpak, M.; Gong, P.; Solouk, A. High entropy alloy coatings for biomedical applications: A review. Smart Mater. Manuf. 2023, 1, 100009. [Google Scholar] [CrossRef]
- Ozerov, M.; Sokolovsky, V.; Nadezhdin, S.; Zubareva, E.; Zherebtsova, N.; Stepanov, N.; Huang, L.; Zherebtsov, S. Microstructure and mechanical properties of medium-entropy TiNbZr alloy-based composites, reinforced with boride particles. J. Alloys Compd. 2023, 938, 168512. [Google Scholar] [CrossRef]
- Nartita, R.; Ionita, D.; Demetrescu, I.; Enachescu, M. A fresh perspective on medium entropy alloys applications as coating and coating substrate. Ann. Acad. Rom. Sci. Ser. Phys. Chem. 2022, 7, 34–46. [Google Scholar] [CrossRef]
- Sharma, A. High Entropy Alloy Coatings and Technology. Coatings 2021, 11, 372. [Google Scholar] [CrossRef]
- Dobbelstein, H.; Gurevich, E.L.; George, E.P.; Ostendorf, A.; Laplanche, G. Laser metal deposition of compositionally graded TiZrNbTa refractory high-entropy alloys using elemental powder blends. Addit. Manuf. 2019, 25, 252–262. [Google Scholar] [CrossRef]
- Zhou, E.; Qiao, D.; Yang, Y.; Xu, D.; Lu, Y.; Wang, J.; Smith, J.A.; Li, H.; Zhao, H.; Liaw, P.K.; et al. A novel Cu-bearing high-entropy alloy with significant antibacterial behavior against corrosive marine biofilms. J. Mater. Sci. Technol. 2020, 46, 201–210. [Google Scholar] [CrossRef]
- Prodana, M.; Ionita, D.; Stoian, A.B.; Demetrescu, I.; Mihai, G.V.; Enăchescu, M. The Design and Characterization of New Chitosan, Bioglass and ZnO-Based Coatings on Ti-Zr-Ta-Ag. Coatings 2023, 13, 493. [Google Scholar] [CrossRef]
- Isola, G. Interface between Periodontal Tissues and Dental Materials: Dynamic Changes and Challenges. Coatings 2021, 11, 485. [Google Scholar] [CrossRef]
- Kuralt, M.; Selmani Bukleta, M.; Kuhar, M.; Fidler, A. Bone and soft tissue changes associated with a removable partial denture. A novel method with a fusion of CBCT and optical 3D images. Comput. Biol. Med. 2019, 108, 78–84. [Google Scholar] [CrossRef]
- Etman, M.K.; Bikey, D. Clinical performance of removable partial dentures: A retrospective clinical study. Open J. Stomatol. 2012, 02, 173–181. [Google Scholar] [CrossRef]
- Greenstein, G.; Cavallaro, J.; Tarnow, D. Practical Application of Anatomy for the Dental Implant Surgeon. J. Periodontol. 2008, 79, 1833–1846. [Google Scholar] [CrossRef]
- Yu, J.-M.; Kang, S.-Y.; Lee, J.-S.; Jeong, H.-S.; Lee, S.-Y. Mechanical Properties of Dental Alloys according to Manufacturing Process. Materials 2021, 14, 3367. [Google Scholar] [CrossRef]
- Zhang, W.; Liaw, P.K.; Zhang, Y. Science and technology in high-entropy alloys. Sci. China Mater. 2018, 61, 2–22. [Google Scholar] [CrossRef]
- Zhao, Y.; Zhao, P.; Li, W.; Kou, S.; Jiang, J.; Mao, X.; Yang, Z. The microalloying effect of ce on the mechanical properties of medium entropy bulk metallic glass composites. Crystals 2019, 9, 483. [Google Scholar] [CrossRef]
- Perumal, G.; Grewal, H.S.; Pole, M.; Reddy, L.V.K.; Mukherjee, S.; Singh, H.; Manivasagam, G.; Arora, H.S. Enhanced Biocorrosion Resistance and Cellular Response of a Dual-Phase High Entropy Alloy through Reduced Elemental Heterogeneity. ACS Appl. Bio Mater. 2020, 3, 1233–1244. [Google Scholar] [CrossRef]
- Castro, D.; Jaeger, P.; Baptista, A.C.; Oliveira, J.P. An Overview of High-Entropy Alloys as Biomaterials. Metals 2021, 11, 648. [Google Scholar] [CrossRef]
- Cemin, F.; Luís Artico, L.; Piroli, V.; Andrés Yunes, J.; Alejandro Figueroa, C.; Alvarez, F. Superior in vitro biocompatibility in NbTaTiVZr(O) high-entropy metallic glass coatings for biomedical applications. Appl. Surf. Sci. 2022, 596, 153615. [Google Scholar] [CrossRef]
- Ma, N.; Liu, S.; Liu, W.; Xie, L.; Wei, D.; Wang, L.; Li, L.; Zhao, B.; Wang, Y. Research Progress of Titanium-Based High Entropy Alloy: Methods, Properties, and Applications. Front. Bioeng. Biotechnol. 2020, 8, 603522. [Google Scholar] [CrossRef] [PubMed]
- Edalati, P.; Floriano, R.; Tang, Y.; Mohammadi, A.; Pereira, K.D.; Luchessi, A.D.; Edalati, K. Ultrahigh hardness and biocompatibility of high-entropy alloy TiAlFeCoNi processed by high-pressure torsion. Mater. Sci. Eng. C 2020, 112, 110908. [Google Scholar] [CrossRef] [PubMed]
- Geanta, V.; Voiculescu, I.; Vizureanu, P.; Victor Sandu, A. High Entropy Alloys for Medical Applications. In Engineering Steels and High Entropy-Alloys; IntechOpen: London, UK, 2020. [Google Scholar]
- Drob, S.I.; Vasilescu, C.; Andrei, M.; Calderon Moreno, J.M.; Demetrescu, I.; Vasilescu, E. Microstructural, mechanical and anticorrosion characterisation of new CoCrNbMoZr alloy. Mater. Corros. 2016, 67, 739–747. [Google Scholar] [CrossRef]
- Yang, W.; Liu, Y.; Pang, S.; Liaw, P.K.; Zhang, T. Bio-corrosion behavior and in vitro biocompatibility of equimolar TiZrHfNbTa high-entropy alloy. Intermetallics 2020, 124, 106845. [Google Scholar] [CrossRef]
- Zhang, G.; Khanlari, K.; Huang, S.; Li, X.; Zhao, D.; Wu, H.; Cao, Y.; Liu, B.; Huang, Q. Dual-structured oxide coatings with enhanced wear and corrosion resistance prepared by plasma electrolytic oxidation on Ti-Nb-Ta-Zr-Hf high-entropy alloy. Surf. Coat. Technol. 2023, 456, 129254. [Google Scholar] [CrossRef]
- Mazare, A.; Totea, G.; Burnei, C.; Schmuki, P.; Demetrescu, I.; Ionita, D. Corrosion, antibacterial activity and haemocompatibility of TiO2 nanotubes as a function of their annealing temperature. Corros. Sci. 2016, 103, 215–222. [Google Scholar] [CrossRef]
- Prodana, M.; Duta, M.; Ionita, D.; Bojin, D.; Stan, M.S.; Dinischiotu, A.; Demetrescu, I. A new complex ceramic coating with carbon nanotubes, hydroxyapatite and TiO2 nanotubes on Ti surface for biomedical applications. Ceram. Int. 2015, 41, 6318–6325. [Google Scholar] [CrossRef]
- Grigorescu, S.; Ungureanu, C.; Kirchgeorg, R.; Schmuki, P.; Demetrescu, I. Various sized nanotubes on TiZr for antibacterial surfaces. Appl. Surf. Sci. 2013, 270, 190–196. [Google Scholar] [CrossRef]
- Berger, J.E.; Jorge, A.M.; Asato, G.H.; Roche, V. Formation of self-ordered oxide nanotubes layer on the equiatomic TiNbZrHfTa high entropy alloy and bioactivation procedure. J. Alloys Compd. 2021, 865, 158837. [Google Scholar] [CrossRef]
- Yang, W.; Pang, S.; Liu, Y.; Wang, Q.; Liaw, P.K.; Zhang, T. Design and properties of novel Ti–Zr–Hf–Nb–Ta high-entropy alloys for biomedical applications. Intermetallics 2022, 141, 107421. [Google Scholar] [CrossRef]
- Wang, S.; Wu, D.; She, H.; Wu, M.; Shu, D.; Dong, A.; Lai, H.; Sun, B. Design of high-ductile medium entropy alloys for dental implants. Mater. Sci. Eng. C 2020, 113, 110959. [Google Scholar] [CrossRef]
- Iijima, Y.; Nagase, T.; Matsugaki, A.; Wang, P.; Ameyama, K.; Nakano, T. Design and development of Ti–Zr–Hf–Nb–Ta–Mo high-entropy alloys for metallic biomaterials. Mater. Des. 2021, 202, 109548. [Google Scholar] [CrossRef]
- Nagase, T.; Iijima, Y.; Matsugaki, A.; Ameyama, K.; Nakano, T. Design and fabrication of Ti–Zr-Hf-Cr-Mo and Ti–Zr-Hf-Co-Cr-Mo high-entropy alloys as metallic biomaterials. Mater. Sci. Eng. C 2020, 107, 110322. [Google Scholar] [CrossRef]
- Hashimoto, N.; Al-Zain, Y.; Yamamoto, A.; Koyano, T.; Kim, H.Y.; Miyazaki, S. Novel beta-type high entropy shape memory alloys with low magnetic susceptibility and high biocompatibility. Mater. Lett. 2021, 287, 129286. [Google Scholar] [CrossRef]
- Wang, W.; Yang, K.; Wang, Q.; Dai, P.; Fang, H.; Wu, F.; Guo, Q.; Liaw, P.K.; Hua, N. Novel Ti-Zr-Hf-Nb-Fe refractory high-entropy alloys for potential biomedical applications. J. Alloys Compd. 2022, 906, 164383. [Google Scholar] [CrossRef]
- Gurel, S.; Yagci, M.B.; Bal, B.; Canadinc, D. Corrosion behavior of novel Titanium-based high entropy alloys designed for medical implants. Mater. Chem. Phys. 2020, 254, 123377. [Google Scholar] [CrossRef]
- Tüten, N.; Canadinc, D.; Motallebzadeh, A.; Bal, B. Microstructure and tribological properties of TiTaHfNbZr high entropy alloy coatings deposited on Ti–6Al–4V substrates. Intermetallics 2019, 105, 99–106. [Google Scholar] [CrossRef]
- Hori, T.; Nagase, T.; Todai, M.; Matsugaki, A.; Nakano, T. Development of non-equiatomic Ti-Nb-Ta-Zr-Mo high-entropy alloys for metallic biomaterials. Scr. Mater. 2019, 172, 83–87. [Google Scholar] [CrossRef]
- Shittu, J.; Pole, M.; Cockerill, I.; Sadeghilaridjani, M.; Reddy, L.V.K.; Manivasagam, G.; Singh, H.; Grewal, H.S.; Arora, H.S.; Mukherjee, S. Biocompatible High Entropy Alloys with Excellent Degradation Resistance in a Simulated Physiological Environment. ACS Appl. Bio Mater. 2020, 3, 8890–8900. [Google Scholar] [CrossRef] [PubMed]
- Yu, B.; Juma, T.; Wang, H.; Bao, X.; Cao, X.; Wang, Z.; Wang, R.; Yang, X.; Ning, T.; Liang, G.; et al. Development of new Ti50Zr25Nb20Cu5–Ag high-entropy alloys with excellent antibacterial property, osteo-conductivity and biocompatibility in vitro and in vivo. J. Mater. Sci. Technol. 2023, 141, 209–220. [Google Scholar] [CrossRef]
- Todai, M.; Nagase, T.; Hori, T.; Matsugaki, A.; Sekita, A.; Nakano, T. Novel TiNbTaZrMo high-entropy alloys for metallic biomaterials. Scr. Mater. 2017, 129, 65–68. [Google Scholar] [CrossRef]
- Riivari, S.; Närvä, E.; Kangasniemi, I.; Willberg, J.; Närhi, T. Focal adhesion formation of primary human gingival fibroblast on hydrothermally and in-sol-made TiO2-coated titanium. Clin. Implant. Dent. Relat. Res. 2023, 25, 583–591. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Wang, X.; Wang, Y.; Hu, X.; Kawazoe, N.; Yang, Y.; Chen, G. Influence of Cell Spreading Area on the Osteogenic Commitment and Phenotype Maintenance of Mesenchymal Stem Cells. Sci. Rep. 2019, 9, 6891. [Google Scholar] [CrossRef]
- Akmal, M.; Hussain, A.; Afzal, M.; Lee, Y.I.; Ryu, H.J. Systematic study of (MoTa) NbTiZr medium- and high-entropy alloys for biomedical implants—In vivo biocompatibility examination. J. Mater. Sci. Technol. 2021, 78, 183–191. [Google Scholar] [CrossRef]



| Alloy Studied | Microstructure | Mechanical Properties | Resistance to Corrosion | Reference |
|---|---|---|---|---|
| TiZrHfNbTa | BCC structure | n/a | Corrosion rate–5.6 × 10−4 mm/year (Hank’s solution) Ion concentration after 28 days of immersion in Hank’s solution: Ti—19.8 ppb Zr—1.4 ppb Hf—0.76 ppb Nb—8.4 ppb Ta—9.8 pbb | [61] |
| Ti28.33Zr28.33Hf 28.33Nb6.74Ta6.74Mo1.55 | BCC structure | Higher mechanical strength than CP-Ti observed through the stress–strain curve | n/a | [69] |
| TiZrHfCr0.2Mo | BCC dendritic structure with minor interdendritic phases | HV—531 | [70] | |
| TiZrHfCo0.07Cr0.07Mo | HV–532 | |||
| Ti40Zr20Hf10Nb20Ta10 | BCC structure | HV—294 E—86.4 GPa | The polarization behavior in 3.5% NaCl indicates significantly higher corrosion resistance compared with CP-Ti | [68] |
| Ti20Zr20Hf20Nb20Ta20 | Single BCC solid solution | HV—320 E—79 GPa | Corrosion rate—5.5 × 10−4 mm/year (Hank’s solution) | [67] |
| Ti25Zr25Hf25Nb12.5Ta12.5 | HV—293 E—68 GPa | Corrosion rate—8.8 × 10−4mm/year (Hank’s solution) | ||
| Ti27.78Zr27.78Hf27.78Nb8.33Ta8.33 | HV—287 E—56 GPa | Corrosion rate—9.3 × 10−4mm/year (Hank’s solution) | ||
| CoCrNbMoZr | bi-phase of two hexagonally Co-based phases | E—107.88 GPa | Rp—251.9 kΩcm2 (saliva pH = 3.83) Rp—751.4 kΩcm2 (saliva pH = 7.84) Rp—163.3 kΩcm2 (saliva pH = 9.11) Rp—206.5 kΩcm2 (saliva + 0.05 M NaF pH = 8.21) | [60] |
| TiTaHfNb | BCC structure | n/a | Ion concentration after 28 days immersion in fetal bovine serum (FBS): Ti—309.32 ppb Ta—1.14 ppb Nb—0.87 ppb Total ion concentration after 28 days of immersion in: —artificial saliva (AS): approx. 70 ppb —in simulated body fluid (SBF): approx. 20 ppb | [12,73] |
| TiTaHfNbZr | Ion concentration after 28 days of immersion in FBS: Ti—347.24 ppb Ta—9.34 ppb Nb—29.86 ppb Zr—10.76 ppb Total ion concentration after 28 days of immersion in: —AS: approx. 70 ppb —SBF: approx. 15 ppb | |||
| TiTaHfMoZr | Ion concentration after 28 days of immersion in FBS: Ti—309.32 ppb Ta—9.45 ppb Mo—162.49 ppb Zr—4.39 ppb Total ion concentration after 28 days of immersion in: —AS: approx. 200 ppb —SBF: approx. 70 ppb | |||
| Ti1.4Nb0.6Ta0.6Zr1.4Mo0.6 | BCC solid solution | E—140 GPa | n/a | [39] |
| Coating Studied | Substrate Used | Microstructure | Mechanical Properties | Resistance to Corrosion | Reference |
|---|---|---|---|---|---|
| Ti1.5ZrTa0.5Nb0.5Hf0.5 | 316L | Amorphous structure Roughness—2.05 nm | H—11.43 GPa E—180 GPa Critical load—190 mN | Rp (Tafel)—78.2 × 104 Ωcm2 (PBS) Rfilm (EIS)—5.10 × 104 Ωcm2 (PBS) Rct (EIS)—4.25 × 106 Ωcm2 (PBS) | [26] |
| CoCrMo | Amorphous structure Roughness—2.11 nm | H—11.49 GPa E—185 GPa Critical load—280 mN | Rp (Tafel)—81.8 × 104 Ωcm2 (PBS) Rfilm (EIS)—6.10 × 104 Ωcm2 (PBS) Rct (EIS)—6.95 × 106 Ωcm2 (PBS) | ||
| Ti6Al4V | Amorphous structure Roughness—2.27 nm | H—11.49 GPa E—183 GPa Critical load—>400 mN | Rp (Tafel)—83.0 × 104 Ωcm2 (PBS) Rfilm (EIS)—8.43 × 104 Ωcm2 (PBS) Rct (EIS)—1.54 × 107 Ωcm2 (PBS) | ||
| TiTaHfNbZr | Ti6Al4V | Amorphous structure Roughness—2.78 nm | H—12.51 GPa E—181.3 GPa | n/a | [74] |
| TiTaHfNbZr | NiTi | Amorphous structure | HV—1285 E—183.2 GPa | Lower Ni ion concentration after 28 days of immersion both in artificial saliva (pH = 2.3) and gastric fluid (pH = 2) for the coated samples | [19] |
| TiTaHfNbZr | NiTi | 750 nm coating thickness Roughness—4.35 nm | H—12.44 GPa E—182.8 GPa Critical load—158 mN | 1.88 ppb Ni after 28 days immersion in SBF compared to 265.55 ppb Ni for uncoated alloy | [18] |
| 1500 nm coating thickness Roughness—4.35 nm | H—11.82 GPa E—175.1 GPa Critical load—204 mN | n/a |
| BioHEA Studied | Investigated Cell Type | In Vitro Biological Performance | Quantitative Assessments | Reference |
|---|---|---|---|---|
| Non-equiatomic BioHEAs (Ti1.4Zr1.4Nb0.6Ta0.6Mo0.6) | Human osteoblasts | Cell morphology and density are similar to CP-Ti and equiatomic TiNbTaZrMo but higher than on SUS-316L surface. More mature focal adhesions than on SUS-316L. | Size regulation of fibrillar adhesions: 810/mm2 | [75] |
| As-cast and SLM-built Ti1.4Nb0.6Ta 0.6Zr1.4Mo0.6 BioHEAs | Mouse primary neonatal calvarial osteoblasts | Comparable biological performance to CP-Ti but superior to SS316L in terms of cell density, morphology and spreading as well as osteogenic differentiation. The SLM process showed the most promising potential. | Cell density: >8000 cells/cm2 | [39] |
| Ti28.33Zr28.33Hf28.33Nb6.74Ta6.74Mo1.55 (at.%) (TZHNTM-3) | Mouse primary neonatal calvarial osteoblasts | Similar biological performance to CP-Ti but superior to SUS316L and Co-Cr-Mo in terms of osteoblast cytomorphology, adhesion and spreading, as well as cytoskeleton organization | Cell density: ~8000 cells/cm2 | [69] |
| TiZrHfCr0.2Mo TiZrHfCo0.07Cr0.07Mo | Mouse primary neonatal calvarial osteoblasts | Superior in vitro biocompatibility (enhanced cell adhesion, widespread morphology, mature focal adhesions) comparable to that of CP-Ti and higher than that exhibited by SUS316 and Co-Cr-Mo commercial alloys. | Cell density: ~9000 cells/cm2 | [70] |
| Ti20Zr20Hf20Nb20Ta20 | MC3T3-E1 mouse pre-osteoblast cell line | In vitro cellular response comparable to Ti6Al4V alloy (morphology characteristic to healthy cells, enhanced pre-osteoblast adhesion, high levels of cell viability and proliferation) | Cell viability after 7 days incubation: ~100% | [61] |
| Ti20Zr20Hf20Nb20Ta20 Ti25Zr25Hf25Nb12.5Ta12.5 (Alloy-II) Ti27.78Zr27.78Hf27.78Nb8.33Ta8.33 (Alloy-III) | MC3T3-E1 mouse pre-osteoblast cell line | Good cell adhesion, high cell viability and proliferation, which were equivalent to those exhibited by the Ti6Al4V alloy | Cell numbers attached: 95–105% * | [67] |
| MoNbTaTiZr | HW-MSCs; MC3T3-E1 pre-osteoblast cell line | Improved in vitro biocompatibility in terms of cell adhesion and survival rate, migratory potential and osteogenic commitment when compared to SS304 alloy | Cell viability: 89.31% | [76] |
| Dual-phase MoNbTaTiZr (HEA); HEA-FSP, HEA-SFP | HW-MSCs | Conditioned media collected by incubation of the processed samples showed better cell viability and proliferation than that exhibited by the extraction media of SS316L and Ti6Al4V materials. HEA-SFP displayed the highest biological performance | Cell viability: 90–95% | [54] |
| Ti40Zr20Hf10Nb20Ta10 | Human primary gingival fibroblasts (HGF) | Greater biological performance in terms of HGF adhesion (cell attachment, spreading and gene expression of some cell adhesion factors), viability and proliferation than TiZrHf and, especially, CP-Ti | Quantitative real-time PCR assay: enhanced expression of VEGFA, COL1a, COL5a, FN1 and MMP9 | [68] |
| Ti50Zr25Nb20Cu2.5Ag2.5 HEA | MC3T3-E1 pre-osteoblast cell line | Higher capacity to induce the osteogenic differentiation of MC3T3-E1 pre-osteoblasts than Ti4Al6V by increasing the expression of osteogenesis-related genes and alkaline phosphatase activity | Antibacterial rate: 99% | [77] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Demetrescu, I.; Nartita, R.; Andrei, M.; Didilescu, A.C.; Cimpean, A.; Ionita, D. Technological Aspects and Performance of High Entropy Alloys with Potential Application in Dental Restorations and Reducing Implant Failure. Appl. Sci. 2023, 13, 12000. https://doi.org/10.3390/app132112000
Demetrescu I, Nartita R, Andrei M, Didilescu AC, Cimpean A, Ionita D. Technological Aspects and Performance of High Entropy Alloys with Potential Application in Dental Restorations and Reducing Implant Failure. Applied Sciences. 2023; 13(21):12000. https://doi.org/10.3390/app132112000
Chicago/Turabian StyleDemetrescu, Ioana, Radu Nartita, Mihai Andrei, Andreea Cristiana Didilescu, Anisoara Cimpean, and Daniela Ionita. 2023. "Technological Aspects and Performance of High Entropy Alloys with Potential Application in Dental Restorations and Reducing Implant Failure" Applied Sciences 13, no. 21: 12000. https://doi.org/10.3390/app132112000
APA StyleDemetrescu, I., Nartita, R., Andrei, M., Didilescu, A. C., Cimpean, A., & Ionita, D. (2023). Technological Aspects and Performance of High Entropy Alloys with Potential Application in Dental Restorations and Reducing Implant Failure. Applied Sciences, 13(21), 12000. https://doi.org/10.3390/app132112000












