Nutritional Factors Associated with Dental Caries across the Lifespan: A Review
Abstract
:1. Introduction
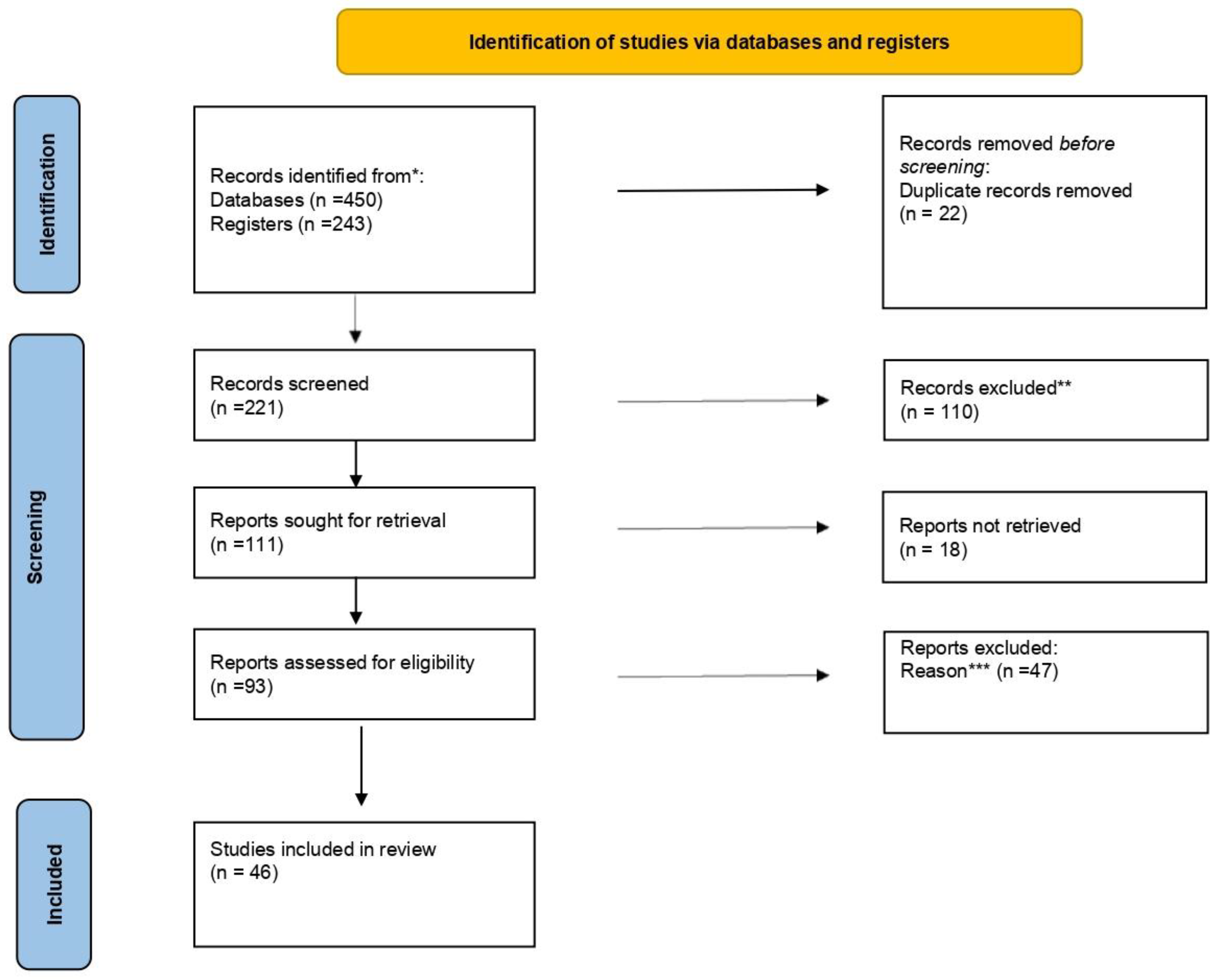
2. Methods
- -
- Population inclusion criteria: Studies involving individuals across all age groups, from infancy through to late adulthood, that had diverse demographic characteristics, such as gender, socioeconomic status, and cultural backgrounds, were used.
- -
- Study design: Rigorous research methodologies, including randomized controlled trials (RCTs), cohort studies, cross-sectional studies, and systematic reviews were also selected. Further exclusion of case reports, editorials, and non-research articles were made to ensure methodological rigor.
- -
- Intervention and exposure variables: Studies evaluating the impact of nutritional interventions on dental caries and exploring dietary factors, including macro- and micronutrient intake, dietary patterns, and specific food items implicated in dental caries etiology, were additionally selected.
- -
- Outcome measures: Studies reporting relevant outcome measures, such as the incidence, prevalence, severity, and progression of dental caries, were incorporated. Among them, only studies employing standardized diagnostic criteria and assessment tools for dental caries evaluation were finally used.
- -
- Temporal considerations: Studies conducted over varying time frames to capture longitudinal perspectives on the relationship between nutrition and dental caries were also selected.
- -
- Publication characteristics: Additionally, we only considered studies published in peer-reviewed journals to uphold scholarly rigor.
- -
- Geographical variation: We also searched for potential variations in nutritional practices and dental health across different geographical regions; thus, we included studies conducted in diverse global settings to enhance generalizability.
- -
- Finally, only articles written in English and published after 2010 were included.
3. Results
4. Effects of Poor Nutrition on Oral Health and Dental Caries
5. Current Food Technology and Its Influence in the Formation of Caries
6. Guidelines and Legislation on Food Intakes to Control Caries
7. The Role of the Dentist in Promoting Healthy Nutrition to Support Oral Health and Prevent Dental Caries
8. Discussion
9. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- World Health Organization (WHO). Global Oral Health Status Report: Towards Universal Health Coverage for Oral Health by 2030; Regional summary of the African Region; World Health Organization: Geneva, Switzerland, 2023. [Google Scholar]
- Fathalla, L.H. Caries Prevention Strategies Practiced In Scandinavia. A literature study. Bachelor’s Thesis, Malmö University, Malmö, Switzerland, 2011. [Google Scholar]
- World Health Organization (WHO). Prevention and Treatment of Dental Caries with Mercury-Free Products and Minimal Intervention: WHO Oral Health Briefing Note Series; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- Chapple, I.L.; Bouchard, P.; Cagetti, M.G.; Campus, G.; Carra, M.C.; Cocco, F.; Nibali, L.; Hujoel, P.; Laine, M.L.; Lingstrom, P.; et al. Interaction of lifestyle, behaviour or systemic diseases with dental caries and periodontal diseases: Consensus report of group 2 of the joint EFP/ORCA workshop on the boundaries between caries and periodontal diseases. J. Clin. Periodontol. 2017, 44, S39–S51. [Google Scholar] [CrossRef]
- Marsh, P.D.; Martin, M.V. Plaque-mediated diseases: Dental caries and periodontal diseases. In Marsh and Martin’s Oral Microbiology, 6th ed.; Marsh, P.D., Lewis, M.A.O., Rogers, H., Williams, D.W., Wilson, M., Eds.; Elsevier Ltd.: Amsterdam, The Netherlands, 2016; pp. 112–129. ISBN 978-070-206-106-6. [Google Scholar]
- Hernández, P.; Sánchez, M.C.; Llama-Palacios, A.; Ciudad, M.J.; Collado, L. Strategies to combat caries by maintaining the integrity of biofilm and homeostasis during the rapid phase of supragingival plaque formation. Antibiotics 2022, 11, 880. [Google Scholar] [CrossRef]
- Beikler, T.; Flemmig, T.F. Oral biofilm-associated diseases: Trends and implications for quality of life, systemic health and expenditures. Periodontol. 2000 2011, 55, 87–103. [Google Scholar] [CrossRef] [PubMed]
- Diamantopoulos, K.; Niakas, D. The Effects of Economic Crisis on the Demand and Supply of the Dental Services in Greece. J. Int. Soc. Prev. Community Dent. 2017, 7, 135–140. [Google Scholar]
- Najihah, L.; Wan Husin, W.Z.; Marhazlinda, J. Multivariable Projections of Caries-Free Prevalence and the Associated Factors from 2019 to 2030 among Schoolchildren Aged 6, 12 and 16-Year-Old in Malaysia. Children 2023, 10, 1125. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Action Plan for Oral Health in South-East Asia 2022–2030: Towards Universal Health Coverage for Oral Health; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- Atkinson, F.S.; Khan, J.H.; Brand-Miller, J.C.; Eberhard, J. The Impact of Carbohydrate Quality on Dental Plaque pH: Does the Glycemic Index of Starchy Foods Matter for Dental Health? Nutrients 2021, 13, 2711. [Google Scholar] [CrossRef]
- Keyes, P.H. Research in dental caries. JADA 1968, 76, 1357–1373. [Google Scholar] [CrossRef] [PubMed]
- Paes Leme, A.F.; Koo, H.; Bellato, C.M.; Bedi, G.; Cury, J.A. The role of sucrose in cariogenic dental biofilm formation–new insight. J. Dent. Res. 2006, 85, 878–887. [Google Scholar] [CrossRef]
- Hancock, S.; Zinn, C.; Schofield, G. The consumption of processed sugar- and starch-containing foods, and dental caries: A systematic review. Eur. J. Oral Sci. 2020, 128, 467–475. [Google Scholar] [CrossRef]
- Suarez-Durall, P.; Mulligan, R.; Enciso, R. Oral health for baby boomers: Past, present, and future. Spec. Care Dent. 2023, 43, 346–358. [Google Scholar] [CrossRef]
- Ates Özcan, B.; Yesilkay, B.; Yaldiz, N.; Pehliva, M. Factors affecting diet quality in adolescents: The effect of sociodemographic characteristics and meal consumption. Progr. Nutr. 2020, 22, e2020094. [Google Scholar]
- Holland, C. Obesity, oral health and the role of the dental profession. Brit. Dent. J. 2022, 233, 712–713. [Google Scholar] [CrossRef]
- World Health Organization. WHO European Regional Obesity Report 2022; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- Tambalis, K.D.; Panagiotakos, D.B.; Psarra, G.; Sidossis, L.S. Current data in Greek children indicate decreasing trends of obesity in the transition from childhood to adolescence; results from the National Action for Children’s Health (EYZHN) program. J. Prev. Med. Hyg. 2018, 59, E36–E47. [Google Scholar] [PubMed]
- Yau, A.; Adams, J.; White, M.; Nicolaou, M. Differences in diet quality and socioeconomic patterning of diet quality across ethnic groups: Cross-sectional data from the HELIUS Dietary Patterns study. Eur. J. Clin. Nutr. 2020, 74, 387–396. [Google Scholar] [CrossRef] [PubMed]
- Muhoozi, G.K.M.; Atukunda, P.; Skaare, A.B.; Willumsen, T.; Diep, L.M.; Westerberg, A.C.; Iversen, P.O. Effects of nutrition and hygiene education on oral health and growth among toddlers in rural Uganda: Follow-up of a cluster-randomised controlled trial. Trop. Med. Int. Health 2018, 23, 391–404. [Google Scholar] [CrossRef]
- Nakai, Y.; Mori-Suzuki, Y. Impact of dietary patterns on plaque acidogenicity and dental caries in early childhood: A retrospective analysis in Japan. Int. J. Environ. Res. Public Health 2022, 19, 7245. [Google Scholar] [CrossRef] [PubMed]
- Zeng, L.; Zeng, Y.; Zhou, Y.; Wen, J.; Wan, L.; Ou, X.; Zhou, X. Diet and lifestyle habits associated with caries in deciduous teeth among 3- to 5-year-old preschool children in Jiangxi province, China. BMC Oral Health 2018, 18, 224. [Google Scholar] [CrossRef]
- Aguiar, B.D.; Fernandes, M.E.F.; de Aguiar, M.H.R.; Torquato, D.S.A.; Peres, E.C.; Teixeira, A.K.M. Nutritional status and dental caries of schoolchildren from Sobral-Ceará. Rev. Gaúch. Odontol. 2019, 67, e20190049. [Google Scholar] [CrossRef]
- Bassa, S.; Workie, S.B.; Kassa, Y.; Tegbaru, D.W. Prevalence of dental caries and relation with nutritional status among school-age children in resource limited setting of southern Ethiopia. BMC Oral Health 2023, 23, 84. [Google Scholar] [CrossRef]
- Rani, V.; Umashankar, G.K.; Benjamin, N.; Rahman, S.A. Association between Nutritional Status and Dental Caries among School Children Attending out Reach Program:-Retrospective Study. SM Prev. Med. Public Health 2019, 3, 1028. [Google Scholar] [CrossRef]
- Lueangpiansamut, J.; Chatrchaiwiwatana, S.; Muktabhant, B.; Inthalohit, W. Relationship between dental caries status, nutritional status, snack foods, and sugar-sweetened beverages consumption among primary schoolchildren grade 4–6 in Nongbua Khamsaen school, Na Klang district, Nongbua Lampoo Province, Thailand. J. Med. Assoc. Thai. 2012, 95, 1090–1097. [Google Scholar]
- da Silva NR, J.; de Camargo MB, J.; Dos Vaz, J.S.; Correa, M.B.; Matijasevich, A.; da Silva dos Santos, I.; Cascaes, A.M. Ultra-processed food consumption and dental caries in adolescents from the 2004 Pelotas Birth Cohort study. Community Dent. Oral Epidemiol. 2023, 51, 1180–1186. [Google Scholar] [CrossRef] [PubMed]
- Hong, J.; Whelton, H.; Douglas, G.; Kang, J. Consumption frequency of added sugars and UK children’s dental caries. Community Dent. Oral Epidemiol. 2018, 46, 457–464. [Google Scholar] [CrossRef]
- Kariya, P.B.; Singh, S. Correlation between nutritional status and dental caries in 3–18-year-old Indian school-going children: A cross-sectional study. World J. Dent. 2022, 13, S189–S193. [Google Scholar]
- van Meijeren-van Lunteren, A.W.; Voortman, T.; Wolvius, E.B.; Kragt, L. Adherence to dietary guidelines and dental caries among children: A longitudinal cohort study. Eur. J. Public Health 2023, 33, 653–658. [Google Scholar] [CrossRef] [PubMed]
- Melissari, A.; Alexopoulos, A.; Mantzourani, I.; Plessas, S.; Voidarou, C.; Tsigalou, C.; Bezirtzoglou, E. Investigating Nutritional Behavior and Oral Health Habits among Adults and Children in Nοrth-Eastern Greece. Oral 2021, 1, 56–74. [Google Scholar] [CrossRef]
- Rosli, T.I.; Chan, Y.M.; Kadir, R.A.; Hamid, T.A.A. Association between oral health-related quality of life and nutritional status among older adults in district of Kuala Pilah, Malaysia. BMC Public Health 2019, 19, 547. [Google Scholar] [CrossRef]
- Wu, L.L.; Cheung, K.Y.; Lam, P.Y.P.; Gao, X.L. Oral health indicators for risk of malnutrition in elders. J. Nutr. Health Aging 2018, 22, 254–261. [Google Scholar] [CrossRef] [PubMed]
- El Hélou, M.; Boulos, C.; Adib, S.M.; Tabbal, N. Relationship between oral health and nutritional status in the elderly: A pilot study in Lebanon. J. Clin. Gerontol. Geriatr. 2014, 5, 91–95. [Google Scholar] [CrossRef]
- Oliveria, S.A.; Ellison, R.C.; Moore, L.L.; Gillman, M.W.; Garrahie, E.J.; Singer, M.R. Parent-child relationships in nutrient intake: The Framingham Children’s Study. Am. J. Clin. Nutr. 1992, 56, 593–598. [Google Scholar] [CrossRef]
- Patterson, T.L.; Rupp, J.W.; Sallis, J.F.; Atkins, C.J.; Nader, P.R. Aggregation of dietary calories, fats, and sodium in Mexican-American and Anglo families. Am. J. Prev. Med. 1988, 4, 75–82. [Google Scholar] [CrossRef]
- Neumark-Sztainer, D.; Story, M.; Resnick, M.D.; Blum, R.W. Lessons learned about adolescent nutrition from the Minnesota Adolescent Health Survey. J. Am. Diet Assoc. 1998, 98, 1449–1456. [Google Scholar] [CrossRef] [PubMed]
- Gibson, E.L.; Wardle, J.; Watts, C.J. Fruit and vegetable consumption, nutritional knowledge and beliefs in mothers and children. Appetite 1998, 31, 205–228. [Google Scholar] [CrossRef] [PubMed]
- Crawley, H.F.; While, D. Parental smoking and the nutrient intake and food choice of British teenagers aged 16–17 years. J. Epidemiol. Community Health 1996, 50, 306–312. [Google Scholar] [CrossRef] [PubMed]
- Davison, K.K.; Birch, L.L. Childhood overweight: A contextual model and recommendations for future research. Obes. Rev. 2001, 2, 159–171. [Google Scholar] [CrossRef] [PubMed]
- Antoniadou, M.; Varzakas, T.M. Breaking the vicious circle of diet, malnutrition and oral health for the independent elderly. Crit. Rev. Food Sci. Nutr. 2021, 61, 3233–3255. [Google Scholar] [CrossRef] [PubMed]
- Dibello, V.; Lobbezoo, F.; Lozupone, M.; Sardone, R.; Ballini, A.; Berardino, G.; Mollica, A.; Coelho-Júnior, H.J.; De Pergola, G.; Stallone, R.; et al. Oral frailty indicators to target major adverse health-related outcomes in older age: A systematic review. Geroscience 2023, 45, 663–706. [Google Scholar] [CrossRef] [PubMed]
- Chan, A.K.Y.; Tsang, Y.C.; Jiang, C.M.; Leung, K.C.M.; Lo, E.C.M.; Chu, C.H. Diet, Nutrition, and Oral Health in Older Adults: A Review of the Literature. Dent. J. 2023, 11, 222. [Google Scholar] [CrossRef]
- Tungare, S.; Paranjpe, A.G. Diet and Nutrition to Prevent Dental Problems; Updated: 10th July, 2023; Tungare, S., Paranjpe, A.G., Eds.; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Kotronia, E.; Brown, H.; Papacosta, A.O.; Lennon, L.T.; Weyant, R.J.; Whincup, P.H.; Wannamethee, S.G.; Ramsay, S.E. Poor oral health and the association with diet quality and intake in older people in two studies in the UK and USA. Br. J. Nutr. 2021, 126, 118–130. [Google Scholar] [CrossRef]
- Murererehe, J.; Uwitonze, A.M.; Nikuze, P.; Patel, J.; Razzaque, M.S. Beneficial Effects of Vitamin C in Maintaining Optimal Oral Health. Front. Nutr. 2021, 8, 805809. [Google Scholar] [CrossRef]
- Moynihan, P.J. The relationship between nutrition and systemic and oral well-being in older people. JADA 2007, 138, 493–497. [Google Scholar] [CrossRef] [PubMed]
- Peponis, M.; Antoniadou, M.; Pappa, E.; Rahiotis, C.; Varzakas, T. Vitamin D and Vitamin D Receptor Polymorphisms Relationship to Risk Level of Dental Caries. Appl. Sci. 2023, 13, 6014. [Google Scholar] [CrossRef]
- Chi, D.L.; Scott, J.M. Added sugar and dental caries in children: A scientific update and future steps. Dent. Clin. N. Am. 2019, 63, 17–33. [Google Scholar] [CrossRef] [PubMed]
- Tonetti, M.S.; Jepsen, S.; Jin, L.; Otomo-Corgel, J. Impact of the global burden of periodontal diseases on health, nutrition and wellbeing of mankind: A call for global action. J. Clin. Periodontol. 2017, 44, 456–462. [Google Scholar] [CrossRef] [PubMed]
- Akram, M.; Munir, N.; Daniyal, M.; Egbuna, C.; Găman, M.-A.; Onyekere, P.F.; Olatunde, A. Vitamins and Minerals: Types, sources and their functions. In Functional Foods and Nutraceuticals: Bioactive Components, Formulations and Innovations; Egbuna, C., Dable-Tupas, G., Eds.; Springer Nature: Cham, Switzerland, 2020; pp. 149–172. [Google Scholar]
- Psoter, W.J.; Reid, B.C.; Katz, R.V. Malnutrition and Dental Caries: A Review of the Literature. Caries Res. 2005, 39, 441–447. [Google Scholar] [CrossRef]
- Hujoel, P.P.; Lingström, P. Nutrition, dental caries and periodontal disease: A narrative review. J. Clin. Periodontol. 2017, 44, S79–S84. [Google Scholar] [CrossRef]
- Soesilawati, P.; Rezkika, Y.F.; Ayunnisa, N.; Syarifina, M.P.; Soffarina, S.; Laturiuw, I.J.; Pertiwi, P.C. Effectivity of Calcium, Phosphate and Vitamin D in Dental Caries Prevention. DENTA 2023, 17, 67–74. [Google Scholar] [CrossRef]
- Nizami, M.Z.I.; Xu, V.W.; Yin, I.X.; Yu, O.Y.; Chu, C.H. Metal and Metal Oxide Nanoparticles in Caries Prevention: A Review. Nanomaterials 2021, 11, 3446. [Google Scholar] [CrossRef]
- Redondo, N.; Gómez-Martínez, S.; Marcos, A. Sensory attributes of soft drinks and their influence on consumers’ preferences. Food Funct. 2014, 5, 1686–1694. [Google Scholar] [CrossRef]
- Rozental, J.M. Tension-Type Headache, Chronic Tension-Type Headache, and Other Chronic Headache Types. In Essentials of Pain Medicine and Regional Anesthesia, 4th ed.; Benzon, H.T., Raja, S.N., Molloy, R.E., Liu, S.S., Fishman, S.M., Eds.; Elsevier Ltd.: Amsterdam, The Netherlands, 2018; pp. 165–168. [Google Scholar]
- Jolly, R. UNICEF (United Nations Children’s Fund): Global Governance That Works, 1st ed.; Routledge: New York, NY, USA, 2014. [Google Scholar]
- Ehizele, A.O.; Ojehanon, P.I.; Akhionbare, O. Nutrition and oral health. Benin J. Postgrad. Med. 2009, 11, 76–82. [Google Scholar] [CrossRef]
- Amargianitakis, M.; Antoniadou, M.; Rahiotis, C.; Varzakas, T. Probiotics, Prebiotics, Synbiotics and Dental Caries. New Perspectives, Suggestions, and Patient Coaching Approach for a Cavity-Free Mouth. Appl. Sci. 2021, 11, 5472. [Google Scholar] [CrossRef]
- Ahmed, S.I.; Sudhir, K.M.; Reddy, V.C.S.; Kumar, R.V.S.K.; Srinivasulu, G. Green Tea in the Prevention of Dental Caries A Systematic Review. Int. Arch. BioMed. Clin. Res. 2017, 3, 1–6. [Google Scholar] [CrossRef]
- Zhang, R.; Cheng, L.; Zhang, T.; Xu, T.; Li, M.; Yin, W.; Jiang, Q.; Yang, Y.; Hu, T. Brick tea consumption is a risk factor for dental caries and dental fluorosis among 12-year-old Tibetan children in Ganzi. Environ. Geochem. Health 2019, 41, 1405–1417. [Google Scholar] [CrossRef]
- Higuchi, T.; Suzuki, N.; Nakaya, S.; Omagari, S.; Yoneda, M.; Hanioka, T.; Hirofuji, T. Effects of Lactobacillus salivarius WB21 combined with green tea catechins on dental caries, periodontitis, and oral malodor. Arch. Oral Biol. 2019, 98, 243–247. [Google Scholar] [CrossRef]
- Chowdhury, J.I.; Hu, Y.; Haltas, I.; Balta-Ozkan, N.; Matthew, G., Jr.; Varga, L. Reducing industrial energy demand in the UK: A review of energy efficiency technologies and energy saving potential in selected sectors. Renew. Sust. Energ. Rev. 2018, 94, 1153–1178. [Google Scholar] [CrossRef]
- Alwaheb, S.A. Dental caries and salivary calcium-phosphate levels among soft drinks factory workers: Exploring the relationship. Int. J. Med. Sci. Dent. Health 2023, 9, 12–15. [Google Scholar]
- Cheng, R.; Yang, H.; Shao, M.Y.; Hu, T.; Zhou, X.D. Dental erosion and severe tooth decay related to soft drinks: A case report and literature review. J. Zhejiang Univ. Sci. B 2009, 10, 395–399. [Google Scholar] [CrossRef] [PubMed]
- Vinson, L.A.; Goodlett, A.K.; Huang, R.; Eckert, G.J.; Gregory, R.L. In vitro effects of sports and energy drinks on Streptococcus mutans biofilm formation and metabolic activity. J. Dent. Chi. 2017, 84, 108–114. [Google Scholar]
- Galanakis, C.M. Innovation Strategies in the Food Industry: Tools for Implementation; Academic Press: Cambridge, MA, USA, 2016. [Google Scholar]
- Oliviero, T.; Fogliano, V. Food design strategies to increase vegetable intake: The case of vegetable enriched pasta. Trends Food Sci. Technol. 2016, 51, 58–64. [Google Scholar] [CrossRef]
- Tortora, P. Global Processes and Local Effects: Food Processing Transnational Corporations in the Developing World. Ph.D. Thesis, London School of Economics and Political Science, London, UK, 2002. [Google Scholar]
- Sharma, R. Nutrition in Infants: Risks and Management. In Nutrition in Infancy; Watson, R.R., Grimble, G., Preedy, V.R., Zibadi, S., Eds.; Humana Totowa: Totowa, NJ, USA, 2013; Volume 1, pp. 17–37. [Google Scholar]
- DiMaggio, D.M.; Du, N.; Scherer, C.; Brodlie, S.; Shabanova, V.; Belamarich, P.; Porto, A.F. Comparison of Imported European and US Infant Formulas: Labeling, Nutrient and Safety Concerns. J. Pediatr. Gastroenterol. Nutr. 2019, 69, 480–486. [Google Scholar] [CrossRef]
- Jiang, Y.; Guo, M.Y. Infant formula product regulation. In Human Milk Biochemistry and Infant Formula Manufacturing Technology, 2nd ed.; Guo, M., Ed.; Elsevier. Ltd: Amsterdam, The Netherlands, 2021; pp. 281–316. [Google Scholar]
- Aceves-Martins, M.; Bates, R.L.; Craig, L.C.A.; Chalmers, N.; Horgan, G.; Boskamp, B.; de Roos, B. Food-Level Analysis to Identify Dietary Choices With the Highest Nutritional Quality and Lowest Greenhouse Gas Emissions and Price. Front. Nutr. 2022, 9, 851826. [Google Scholar] [CrossRef] [PubMed]
- Schifferstein, H.N.J.; de Boer, A.; Lemke, M. Conveying information through food packaging: A literature review comparing legislation with consumer perception. J. Funct. Foods 2021, 86, 104734. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Carbohydrate Intake for Adults and Children: WHO Guideline, in Carbohydrate Intake for Adults and Children: WHO Guideline; World Health Organization: Geneva, Switzerland, 2023. [Google Scholar]
- Voidarou, C.; Antoniadou, M.; Rozos, G.; Alexopoulos, A.; Giorgi, E.; Tzora, A.; Skoufos, I.; Varzakas, T.; Bezirtzoglou, E. An In Vitro Study of Different Types of Greek Honey as Potential Natural Antimicrobials against Dental Caries and Other Oral Pathogenic Microorganisms. Case Study Simulation of Oral Cavity Conditions. Appl. Sci. 2021, 11, 6318. [Google Scholar] [CrossRef]
- Mahdi, S.; Dickerson, A.; Solar, G.I.; Caton, S.J. Timing of energy intake and BMI in children: Differential impacts by age and sex. Br. J. Nutr. 2023, 130, 71–82. [Google Scholar] [CrossRef]
- Suvan, J.E.; Finer, N.; D’Aiuto, F. Periodontal complications with obesity. Periodontology 2000 2018, 78, 98–128. [Google Scholar] [CrossRef] [PubMed]
- Anthamatten, K. A review of potential carcinogenic effects of aspartame. Microrev. Cell Mol. Biol. 2023, 4, 1–3. [Google Scholar]
- EFSA Panel on Food Contact Materials; Enzymes and Processing Aids (CEP); Lambré, C.; Barat Baviera, J.M.; Bolognesi, C.; Cocconcelli, P.S.; Crebelli, R.; Gott, D.M.; Grob, K.; Lampi, E.; et al. Safety evaluation of the food enzyme α-amylase from the non-genetically modified Bacillus licheniformis strain T74. EFSA J. 2023, 21, e08160. [Google Scholar]
- Tenelanda-López, D.; Valdivia-Moral, P.; Castro-Sánchez, M. Eating habits and their relationship to oral health. Nutrients 2020, 12, 2619. [Google Scholar] [CrossRef]
- Couto, F.M.; de Sousa, F.S.O.; Vicente, G.C.; Castro, D.P.F.; Nadanovsky, P.; Dos Santos, A.P.P.; Barja-Fidalgo, F. Recommendations to health professionals on the use of fluoride varnish for caries prevention in preschool children. Int. J. Paediatr. Dent. 2023, 34, 11–25. [Google Scholar] [CrossRef]
- Nyvad, B.; Fejerskov, O. The caries control concept. In Dental Caries: The Disease and Its Clinical Management, 3rd ed.; Fejerskov, O., Nyvad, B., Kidd, E., Eds.; Wiley Blackwell: Hoboken, NJ, USA, 2015; pp. 235–243. [Google Scholar]
- Trumbo, P.; Schlicker, S.; Yates, A.A.; Poos, M.; Food and Nutrition Board of the Institute of Medicine. Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein and amino acids. J. Am. Diet. Assoc. 2002, 102, 1621–1631. [Google Scholar] [CrossRef]
- Stephen, A.M.; Champ, M.M.; Cloran, S.J.; Fleith, M.; Van Lieshout, L.; Mejborn, H.; Burley, V.J. Dietary fibre in Europe: Current state of knowledge on definitions, sources, recommendations, intakes and relationships to health. Nutr. Res. Rev. 2017, 30, 149–190. [Google Scholar] [CrossRef] [PubMed]
- Iizuka, K.; Yabe, D. Dietary and Nutritional Guidelines for People with Diabetes. Nutrients 2023, 15, 4314. [Google Scholar] [CrossRef] [PubMed]
- Kalpe, S.; Mathur, A.; Kharat, P. How fad diets May Jeopardize your oral well-being: The hidden consequences. Hum. Nutr. Metab. 2023, 17, 200214. [Google Scholar] [CrossRef]
- Livne, N. Need for nutrition education in health professional programs: A review of the literature. Internet J. Allied Health Sci. Pract. 2019, 17, 5. [Google Scholar] [CrossRef]
- Lieffers, J.R.L.; Vanzan, A.G.T.; Rover de Mello, J.; Cammer, A. Nutrition Care Practices of Dietitians and Oral Health Professionals for Oral Health Conditions: A Scoping Review. Nutrients 2021, 13, 3588. [Google Scholar] [CrossRef] [PubMed]
- Samdal, G.B.; Eide, G.E.; Barth, T.; Williams, G.; Meland, E. Effective behaviour change techniques for physical activity and healthy eating in overweight and obese adults; systematic review and meta-regression analyses. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 42. [Google Scholar] [CrossRef]
- Spahn, J.M.; Reeves, R.S.; Keim, K.S.; Laquatra, I.; Kellogg, M.; Jortberg, B.; Clark, N.A. State of the evidence regarding behavior change theories and strategies in nutrition counseling to facilitate health and food behavior change. J. Am. Diet. Assoc. 2010, 110, 879–891. [Google Scholar] [CrossRef] [PubMed]
- McCrindle, B.W.; Rowley, A.H.; Newburger, J.W.; Burns, J.C.; Bolger, A.F.; Gewitz, M.; Baker, A.L.; Jackson, M.A.; Takahashi, M.; Shah, P.B.; et al. Diagnosis, treatment, and long-term management of Kawasaki disease: A scientific statement for health professionals from the American Heart Association. Circulation 2017, 135, e927–e999. [Google Scholar] [CrossRef]
- American Diabetes Association. Standards of medical care in diabetes—2022 abridged for primary care providers. Clin. Diabetes 2022, 40, 10–38. [Google Scholar] [CrossRef]
- Antoniadou, M.; Varzakas, T. Diet and Oral Health Coaching Methods and Models for the Independent Elderly. Appl. Sci. 2020, 10, 4021. [Google Scholar] [CrossRef]
- Dart, J.; McCall, L.; Ash, S.; Blair, M.; Twohig, C.; Palermo, C. Toward a global definition of professionalism for nutrition and dietetics education: A systematic review of the literature. J. Acad. Nutr. Diet. 2019, 119, 957–971. [Google Scholar] [CrossRef] [PubMed]
- Sacks, G.S. The shrinking of formalized nutrition education in health professions curricula and postgraduate training. J. Parenter.Enter. Nutr. 2017, 41, 217–225. [Google Scholar] [CrossRef] [PubMed]
- More, F.G.; Sasson, L.M.; Godfrey, E.M.; Sehl, R.B. Collaboration between dietetics and dentistry: Dietetic internship in pediatric dentistry. Top. Clin. Nutr. 2005, 20, 259–268. [Google Scholar] [CrossRef]
- Glanz, K.; Rimer, B.K.; Viswanath, K. Health Behavior and Health Education: Theory, Research, and Practice, 4th ed.; John Wiley & Sons: Hoboken, NJ, USA, 2008. [Google Scholar]
- Schmelzer, L.; Leto, T. Promoting health through engagement in occupations that maximize food resources. Am. J. Occup. Ther. 2018, 72, 7204205020p1–7204205020p9. [Google Scholar] [CrossRef] [PubMed]
- Hickson, M.; Child, J.; Collinson, A. Future dietitian 2025: Informing the development of a workforce strategy for dietetics. J. Hum. Nutr. Diet. 2018, 31, 23–32. [Google Scholar] [CrossRef] [PubMed]
- Pitts, N.B.; Twetman, S.; Fisher, J.; Marsh, P.D. Understanding dental caries as a non-communicable disease. Brit. Dent. J. 2021, 231, 749–753. [Google Scholar] [CrossRef] [PubMed]
- Tinanoff, N.; Palmer, C.A. Dietary determinants of dental caries and dietary recommendations for preschool children. J. Public Health Dent. 2000, 60, 197–206. [Google Scholar] [CrossRef] [PubMed]
- Ritter, A.V.; Sulaiman, T.A.; Altitinchi, A.; Bair, E.; Baratto-Filho, F.; Gonzaga, C.C.; Correr, G.M. Composite-composite adhesion as a function of adhesive-composite material and surface treatment. Oper. Dent. 2019, 44, 348–354. [Google Scholar] [CrossRef]
- Peres, M.A.; Macpherson, L.M.D.; Weyant, R.J.; Daly, B.; Venturelli, R.; Mathur, M.R.; Listl, S.; Celeste, R.K.; Guarnizo-Herreño, C.C.; Kearns, C.; et al. Oral diseases: A global public health challenge. Lancet 2019, 394, 249–260. [Google Scholar] [CrossRef]
- Large, J.F.; O’Keefe, E.; Valentine, C.; Roebuck, E.M. Weight screening in paediatric dentistry: What do families and staff think? Int. J. Paediatr. Dent. 2022, 32, 64–66. [Google Scholar] [CrossRef]
- Parial-Palacio, G. Assessment of School-Age Learners’ Oral Health and Dental Hygiene Practices in Northern Samar: Implications for a Dental Health Education Program. J. Namib. Studies 2023, 34, 2022–2027. [Google Scholar]
- Kierce, E.A.; Boyd, L.D.; Rainchuso, L.; Palmer, C.A.; Rothman, A. Association between Early Childhood Caries, Feeding Practices and an Established Dental Home. J. Dent. Hyg. 2016, 90, 18–27. [Google Scholar] [PubMed]
- Center for Disease Control and Prevention (CDC). Recommendations for Using Fluoride to Prevent and Control Dental Caries in the United States; Center for Disease Control and Prevention (CDC): Atlanta, GA, USA, 2001.
- Presskreischer, R.; Prado, M.A.; Kuraner, S.E.; Arusilor, I.M.; Pike, K. Eating disorders and oral health: A scoping review. J. Eat. Disord. 2023, 11, 55. [Google Scholar] [CrossRef] [PubMed]
- Striegel-Moore, R.H.; Bulik, C.M. Risk factors for eating disorders. Am. Psychol. 2007, 62, 181–198. [Google Scholar] [CrossRef] [PubMed]
- Antoniadou, M.; Varzakas, T. Extra Virgin Olive Oil: Processing, Quality, Safety, Authenticity, Nutritional, Health and Oral Health Aspects. In Proceedings of the 1st International Electronic Conference on Food Science and Functional Foods session Food Safety and Sustainable Development, Online, 10–25 November 2020. [Google Scholar]
- Ke, S.; Guimond, A.J.; Tworoger, S.S.; Huang, T.; Chan, A.T.; Liu, Y.Y.; Kubzansky, L.D. Gut feelings: Associations of emotions and emotion regulation with the gut microbiome in women. Psychol. Med. 2023, 53, 7151–7160. [Google Scholar] [CrossRef]
- Pilozzi, A.; Carro, C.; Huang, X. Roles of β-Endorphin in Stress, Behavior, Neuroinflammation, and Brain Energy Metabolism. Int. J. Mol. Sci. 2020, 22, 338. [Google Scholar] [CrossRef]

| Database | Keywords | MeSH Terms (PubMed) | Initial Articles | Duplicates Removed | Final Articles for Analysis | Contribution to Study | Reason for Inclusion |
|---|---|---|---|---|---|---|---|
| PubMed | #Diet, #Nutrition, #Oral Health, #Dental Caries, #Education, #Dentists, #Sustainability, #Food, #Dentistry | #Dietetics, #Nutrition, #Oral Health, #Dental Caries, #Education, #Dentists, and #Sustainability | 150 | 8 | 142 | Provided a broad understanding of the interplay between nutritional habits, interventions, and dental caries; MeSH terms ensured precision in search. | Widely recognized as a premier biomedical database, often used for systematic reviews in healthcare research. |
| Web of Science | #Diet, #Nutrition, #Oral Health, #Dental Caries, #Education, #Dentists, #Sustainability, #Food, #Dentistry | N/A (Web of Science does not use MeSH terms) | 180 | 6 | 174 | Enhanced the overall coverage of literature related to nutritional habits, interventions, and oral health professionals’ role. | Provides a multidisciplinary approach covering a wide range of scientific disciplines. |
| Cochrane Library | #Diet, #Nutrition, #Oral Health, #Dental Caries, #Education, #Dentists, #Sustainability, #Food, #Dentistry, #Evidence-Based Interventions | #Dietetics, #Nutrition, #Oral Health, #Dental Caries, #Education, #Dentists, #Sustainability, and #Evidence-Based Interventions | 120 | 8 | 112 | Strengthened the evidence base by focusing on articles related to evidence-based interventions; MeSH terms ensured specificity. | Renowned for systematic reviews and emphasis on evidence-based interventions in healthcare research. |
| Author/(Year) | Number of Participants | Age Range | Gender | Methods | Results |
|---|---|---|---|---|---|
| Muhoozi et al. (2018) [21] | 399 | Children 36 months | 211 males and 188 females | Questionnaires, anthropometric measurements and photographs of the upper front teeth. | The educational intervention improved oral hygiene practices and reduced the development and progression of caries as well as extractions in children. |
| Nakai et al. (2022) [22] | 118 | Children 1–4 years | 59 males and 59 females | Data collection, including age, sex, medical history, medication, caries status. and plaque acidogenicity level at the first dental visit. Dietary data were collected from 3-day dietary records. | Altering the frequency and timing of sugar intake may prevent early childhood caries by moderating plaque acidogenicity. |
| Zeng et al. (2018) [23] | 2880 | Children 3–5 years | 1488 males and 1392 females | The questionnaire included demographic characteristics, daily diet, lifestyle factors, and the oral health awareness from the parents. | Caries prevalence increased with age, demonstrating higher rates in rural areas than urban ones, albeit remaining lower than those reported in other developing nations. |
| Aguiar et al. (2019) [24] | 92 | Children 5 years | 41 males and 51 females | The nutritional status * was evaluated using the body mass index (BMI) ** and the nutritional intake with an FFQ ***. The dental health status was evaluated using the decayed, missing, and filling tooth index (DMFT index). | A DMFT index of 1.97 was found, and 39.6% of the children presented to be overweight and having lower prevalence of dental caries compared to the obese ones. Higher prevalence of dental caries was associated with low income, public schools, and less educated parents. |
| Bassa et al. (2023) [25] | 761 | Children 6–12 years | 350 males and 411 females | Face-to-face interview, administered questionnaire, and clinical assessment of dental caries. | Teeth cleaning habit, parental education, sweet food consumption, and milk consumption were associated factors. |
| Rani et al. (2019) [26] | 1231 | Children 5–15 years | 603 males and 628 females | Observational study. Anthropometric measures were performed and oral examination as well. | A notable correlation was identified between dental caries and stunting as well as between dental caries and inadequate hygiene practices. However, no statistically significant association was observed between dental caries and underweight status, notwithstanding the elevated prevalence of dental caries in conjunction with malnutrition. |
| Lueangpiansamut et al. (2012) [27] | 111 | Children 11–12 years | 57 males and 54 females | Questionnaire study. | Malnutrition as well as eating sweets before bedtime were significantly related to dental caries. Family income was a risk factor. |
| De Silva et al. (2023) [28] | 996 | Children 12–13 years | 498 males and 498 females | Questionnaires for schoolchildren were identified by the frequency of ultra processed food consumption. | Negative relationship between ultra processed meats and fats, fast foods, and noodles and dental caries. |
| Hong et al. (2018) [29] | 4950 | Children 12–15 years | 2377 males and 2573 females | FFQ only for foods and drinks with added sugar, tooth-brushing frequency, dental attendance, and water-drinking frequency. | The study highlighted the importance of recognizing dental caries patterns by surface, tooth, and child level amongst adolescents and the value of reporting dental caries distribution by threshold in epidemiological surveys. |
| Kariya et al. (2022) [30] | 829 | Children 3–18 years | 414 males and 415 females | Body mass index was recorded. Dental caries was assessed using decayed, missing, and filled primary teeth (DMFT) and decayed extracted filled teeth (deft) index. A parent-administered questionnaire was used to obtain data on oral hygiene practice, parental education, dental visits, and sugar exposure. | Nutritional status was found to be inversely related to dental caries. Children with lesser BMI were at higher risk of having dental caries and vice versa. |
| Van Meijeren-van Lunteren et al. (2023) [31] | 2911 | Children 8–13 years | 1403 boys and 1508 girls | Longitudinal cohort study. Dietary intake at the age of 8 years was assessed using food frequency questionnaires. Diet quality scores were estimated, reflecting adherence to Dutch dietary guidelines. Dental caries was assessed at the age of 13 years using intraoral photographs. | Better diet quality was associated with a lower occurrence of severe dental caries after adjustments for sociodemographic factors. |
| Melissari et al. (2021) [32] | 576 | 186 children 1–17 years and 389 adults 18 to >50 years | 99 boys and 87 girls and 148 males and 241 females | Questionnaire to assess oral health and FFQ (food frequency questionnaire). Caries prevalence was calculated based on the percentage of positive cases and no decay, missing, and filled teeth (DMFT). | Children and adults were less interested in healthy eating and in preventive and other dental therapies, and they did not adhere to the Mediterranean diet. |
| Rosli et al. (2019) [33] | 446 | Adults 50 years or above | 190 males and 259 females | The General Oral Health Assessment Index (GOHAI) was used to measure OHRQoL, and anthropometric measures took place. | Older adults with poor perception of their oral health were more likely to have unsatisfactory BMI. |
| Wu et al. (2018) [34] | 195 | Elders 65 or above | 98 males and 97 females | General Oral Health Assessment Index (GOHAI), an instrument for assessing oral-health-related quality of life (OHRQoL), was used as a subjective measure of oral health and Mini-Nutritional Assessment (MNA) for nutritional status evaluation. | Elders’ tooth loss and unmet treatment need for dental caries were associated with malnutrition. |
| Helou et al. (2014) [35] | 115 | Elders 70 or above | 56 males and 59 females | The nutritional status was assessed by the Mini-Nutritional Assessment (MNA), and oral health was assessed by the Geriatric Oral Health Assessment Index (GOHAI). | Oral care reduced the risk of malnutrition. |
| Micronutrient | Dental Effect | Nutrition Source | Deficiency | Supplements |
|---|---|---|---|---|
| Vitamin A [46,52,53,54] | Facilitates the stimulation of saliva production, thereby promoting the removal of acids and food particles from teeth, concurrently neutralizing acid and providing protection against dental decay. | Leafy green vegetables (kale, spinach, and broccoli), orange and yellow vegetables (carrots, sweet potatoes, pumpkin, and others), tomatoes, red bell pepper, cantaloupe, mango, beef liver, fish oil, milk, and eggs. | Elevated susceptibility to caries was observed in instances of vitamin A deficiency. A proposed mechanism for this vulnerability postulates that it may be attributed to an increase in enamel solubility. | Deficiency in vitamin A is common in children and pregnant women. Supplements may be suggested in this case. |
| Vitamin B6 [53,55] | Has emerged as a promising contender in safeguarding against dental caries. | Beef liver, tuna, salmon, fortified cereals, chickpeas, poultry, and some vegetables and fruits | The deficiency of vitamin B6 can have implications for dental integrity, disrupting essential processes like enamel formation and increasing the risk of caries development. | Only recommended in case of deficiency of vitamin B6. |
| Vitamin K [53,55] | Has surfaced as a noteworthy prospect for protecting against dental caries. | Spinach, broccoli, iceberg lettuce, and fats and oils | Insufficient levels of vitamin K may compromise dental health by impeding optimal mineralization processes, potentially contributing to enamel hypoplasia and increasing the susceptibility to caries formation. | Only recommended if there is a deficiency of vitamin K. |
| Vitamin C [47,53] | Plays a crucial role in promoting the health of the gingiva and facilitating the healing process. | Citrus (orange, kiwi, lemon, and grapefruit), bell peppers, tomatoes, cruciferous vegetables (broccoli, Brussels sprouts, cabbage, and cauliflower), and white potatoes | Depletion in humans leads to gingival bleeding, regardless of oral hygiene. | Only recommended if there is deficiency of vitamin C. |
| Vitamin D [53,55,56] | Activates a pivotal role in the formation of enamel and dentin during the tooth development process due to its interaction with receptors in ameloblasts and odontoblasts. | Dark-green leafed vegetables, cheese, milk, cod-liver oil, oyster mushrooms, eggs, and certain species of wild salmon | The insufficiency of vitamin D can lead to enamel hypoplasia, a noteworthy factor contributing to early childhood caries. | For strict vegans (those avoiding milk) and elderly, vitamin D supplements could be taken in combination with minerals as either vitamin D alone or minerals alone may not provide systemic benefits. |
| Calcium [53,54,56] | Engages actively in the protection and reconstruction of tooth enamel. | Cheese, milk, plain yogurt, calcium-fortified tofu, leafy greens, and almonds | Enamel hypoplasia, salivary glandular hypofunction, and alterations in saliva composition may represent mechanisms through which an association with caries is established. | Calcium is the most important supplement with vitamin D for elderly and vegetarians for dental health. It may also be recommended for pregnant women and children when they do not consume dairy products daily. |
| Phosphorus [53,56,57] | The equilibrium between enamel demineralization and remineralization is actively influenced by the levels of calcium and phosphorus ions in saliva, and their deficiency markedly alters the morphology of the tooth. | Protein-rich foods like meat, poultry, fish, milk, and eggs | Incorporating amorphous calcium phosphate nanoparticles into orthodontic cement can prevent the occurrence of white spot lesions during orthodontic treatments as these nanoparticles possess the capability to inhibit caries and promote the remineralization of lesions. | Supplementation may be essential in deficiency. |
| Magnesium [53,57] | Demonstrates noteworthy antibacterial and biofilm activity against cariogenic bacteria. | Green leafy vegetables, such as spinach, legumes, nuts, seeds, and whole grains | Has the potential to diminish the progression and development of dental caries by releasing magnesium ions. | Supplementation may be essential in deficiency. |
| Zinc [53,57] | Exhibits the capacity to inhibit S. mutans, diminish plaque formation, and promote remineralization. | Meet, fish, and seafood | Failed to foster antimicrobial activity. | Supplementation may be essential in deficiency. |
| Low (Green) | Medium (Amber) | High (Red) | High Per Portion If More Than 100 g/150 mL (Red) | |
|---|---|---|---|---|
| Sugar in food (per 100 g) | 5 g or less | Between 5 g and 22.5 g | More than 22.5 g | 27 g |
| Sugar in drink (per 100 mL) | 2.5 g or less | Between 2.5 g and 11.25 g | More than 11.25 g | 13.5 g |
| Age Group | Nutritional Lifelong Profile for Oral Health | Nutritionist Interventions | Educational Actions |
|---|---|---|---|
| Infants (0–2) | Breast milk/formula for infants, introduction of solid foods with guidance | Nutrition counseling for breastfeeding/formula feeding | Oral hygiene education for parents, early childhood feeding |
| Children (3–12) | Balanced diet with emphasis on calcium-rich foods, limit sugary snacks | Nutritional guidance for parents and caregivers | School programs on healthy eating, importance of oral care |
| Adolescents | Increased calcium and vitamin D intake, reduced sugar consumption | Individualized dietary plans, addressing peer influences | School-based workshops, promoting healthy food choices |
| Adults (18–50) | Mediterranean balanced diet and focus on fruits, vegetables, and whole grains | Personalized nutrition consultations | Workplace wellness programs, seminars on nutrition and its impact on oral health |
| Older adults | Adequate calcium and vitamin B12, hydration, and soft food options | Nutrition support for age-related oral health challenges | Community seminars on nutrition for seniors, workshops on senior nutrition and oral care |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dimopoulou, M.; Antoniadou, M.; Amargianitakis, M.; Gortzi, O.; Androutsos, O.; Varzakas, T. Nutritional Factors Associated with Dental Caries across the Lifespan: A Review. Appl. Sci. 2023, 13, 13254. https://doi.org/10.3390/app132413254
Dimopoulou M, Antoniadou M, Amargianitakis M, Gortzi O, Androutsos O, Varzakas T. Nutritional Factors Associated with Dental Caries across the Lifespan: A Review. Applied Sciences. 2023; 13(24):13254. https://doi.org/10.3390/app132413254
Chicago/Turabian StyleDimopoulou, Maria, Maria Antoniadou, Markos Amargianitakis, Olga Gortzi, Odysseas Androutsos, and Theodoros Varzakas. 2023. "Nutritional Factors Associated with Dental Caries across the Lifespan: A Review" Applied Sciences 13, no. 24: 13254. https://doi.org/10.3390/app132413254








