Smart Healthcare Applications over 5G Networks: A Systematic Review
Abstract
:1. Introduction
- Latif et al. [8], in 2017, presented the challenges and difficulties that could hinder 5G development in the health sector. The authors mentioned the fact that 5G, in conjunction with IoT devices, big data, artificial intelligence (AI), and machine learning (ML), has the potential to transform health systems globally. They also performed a comparison of latency and performance between 2G, 3G, 4G, and 5G technologies. They emphasized that coverage and reliability are key to enabling electronic health applications, such as home health monitoring.
- In 2019, Selem et al. [9] reported the state of the art in e-health applications that use 5G, in which various medical scenarios, such as robotic surgery and remote monitoring, are presented, highlighting the benefits of implementing 5G. In addition, they indicate the use of a wireless body sensor network (WBSN) in real-time monitoring applications, data transmission, emergency situations, and patient location. The emphasized that WBSN will be the backbone for the development of health applications with 5G.
- In 2020, Contreras et al. [10] contributed through a study on the use of telemedicine in the context of the pandemic caused by COVID-19. Through an analysis, they indicated that telemedicine can be enhanced later, after the health system was violated as a result of the pandemic. This review shows a descriptive approach and not a systematic analysis, since the selection of previously published articles was not performed. In the same year, Zhang Chunming et al. [11] also highlighted 5G use in smart healthcare in the control and management of the pandemic caused by COVID-19. The implementation of one of the methods consists of a teleconsultation system to attend two critical cases. The “West China Hospital” of Sichuan University was the developer of this implementation. Kim et al. [12] discussed the use of 5G technology in pre-hospital emergencies. They mentioned that it can support paramedics when assisting patients in emergency. Mainly, they highlighted the use of a remote connection to provide real-time information to external doctors and hospitals. In addition, they emphasized several challenges to which it is exposed, such as security, privacy, patient information sharing, and lack of access in rural areas. Siriwardhana et al. [13] presented the opportunities and challenges of 5G use in the health area. The solutions it can provide for the fight against the COVID-19 pandemic are detailed. The authors emphasize 5G use in telemedicine systems, telesurgery, remote monitoring, and drug delivery. Furthermore, they describe the technical requirements expected for different telehealth applications, such as telemedicine, telenursing, telesurgery, and telepharmacy. Finally, Ahad et al. [14], through a literature review, highlighted the solutions that 5G can provide in the medicine area. The authors presented a categorization of smart healthcare based on communication technologies, services, applications, and requirements that are key to the development of these systems.
- In 2021, Penn et al. [15] provided a narrative review of 5G opportunities in neurosurgery, in which they refer to the enhanced features of 5G such as ultra-reliable low-latency communication (URLLC), massive machine-type communication (mMTC), and enhanced mobile broadband (eMBB). They mentioned that these features could promote the development of neurosurgery by eliminating geographical barriers. They consider that 5G facilitates neurosurgeons’ real-time remote connection in pre-hospital emergencies. In addition, they revealed that in 2019, the China Daily newspaper announced a first neurosurgical case developed with 5G.
2. Method
- RQ1: What are the healthcare applications that can be developed with the 5G implementation in smart health systems?Through this question, we intended to know the different health systems developed with the use of 5G technology, its benefits, and marked trends in terms of the deployment of new supports.
- RQ2: What is the type of technology used, and what technical requirements does an intelligent health system demand through the use of 5G?This question was aimed at identifying the devices, tools, and technical characteristics that enable the development and operation of smart healthcare systems. It also aims to detect the technical characteristics that developers consider essential in the generation of applications.
- RQ3: What are the security mechanisms or protocols required by smart health systems based on 5G?This question was aimed at finding out what security measures are used in smart health systems based on 5G, related to security architectures and encryption protocols in the information transmission.
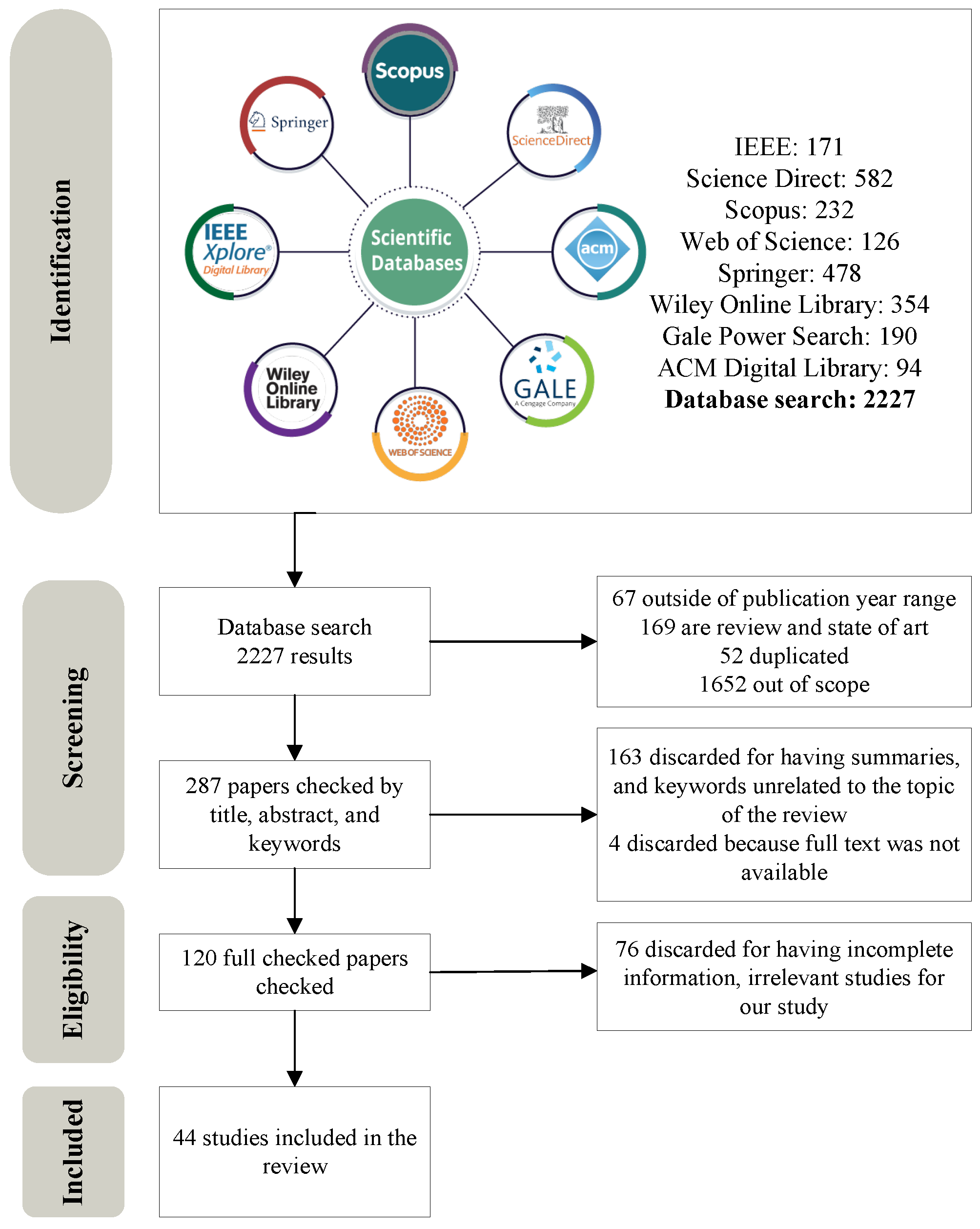
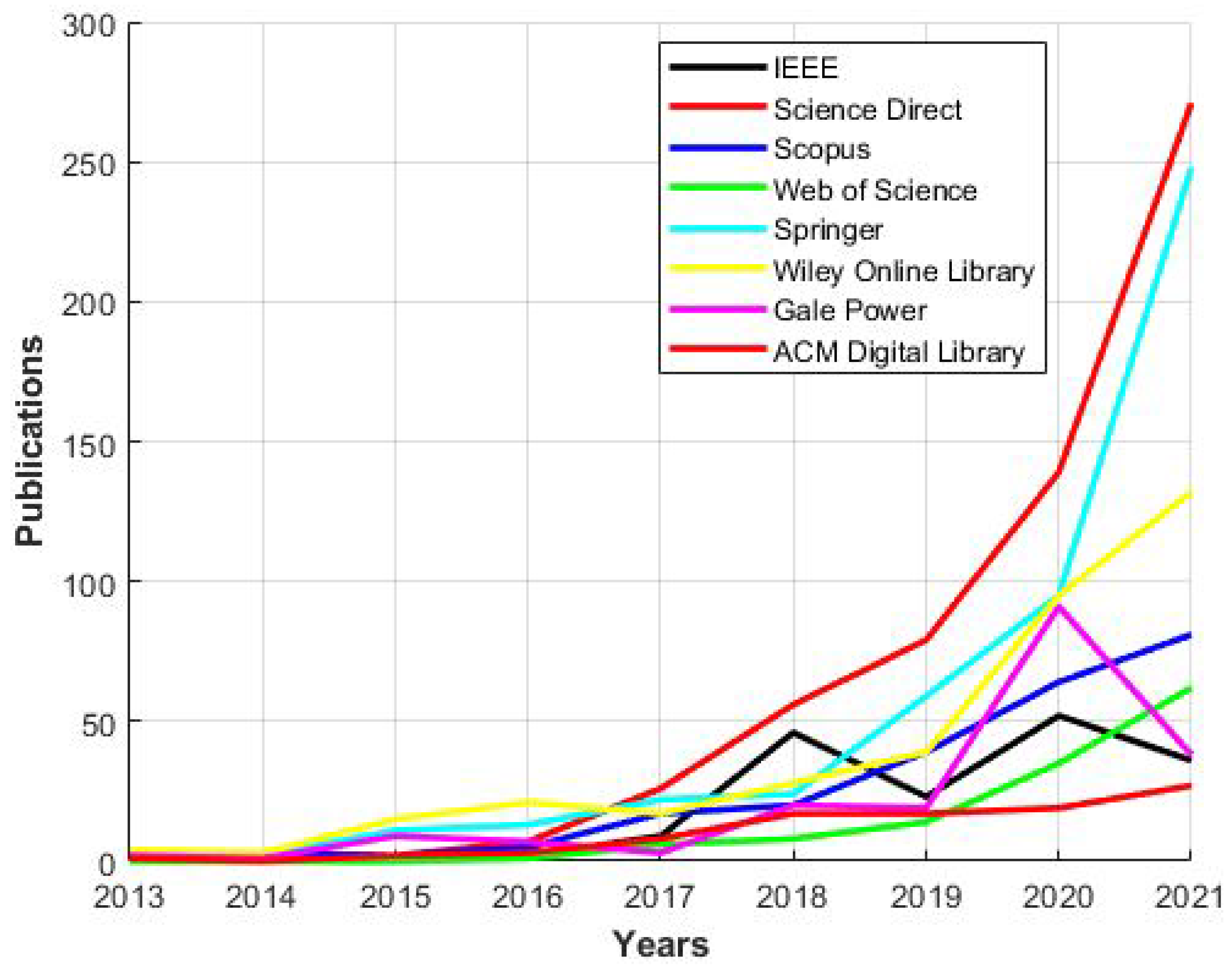
- In stage 1 (identification), the metadata were extracted from the retrieved articles, and the inclusion and exclusion criteria were used, starting with the publication year. As shown in Figure 2, since 2016 there has been an increase in the number of publications produced. With this background, we decided to review the documents published from 2016 to 2021. Within this framework, we also eliminated systematic reviews and state-of-the-art studies that were not based on a technological foundation and showed previous analyses that were inappropriate to the objective of this research.
- In stage 2 (screening), we reviewed the articles according to title, abstract, and keywords. Articles unrelated to our topic and brief, non-relevant articles were removed. Articles that could not be accessed were also discarded.
- In stage 3 (eligibility), we reviewed each article in depth, including for review those that clearly expressed and detailed their applications.
3. Results and Discussion
- Application area.
- Healthcare benefits.
- IoMT devices.
- Communication protocols.
- Networking technologies.
- Network technical requirements.
- Security mechanisms or protocols.
3.1. RQ1: What Are the Healthcare Applications That Can Be Developed with the Implementation of 5G in Smart Health Systems?
3.1.1. Remote Care: Surgery and Diagnosis
3.1.2. Real-Time Continuous Monitoring
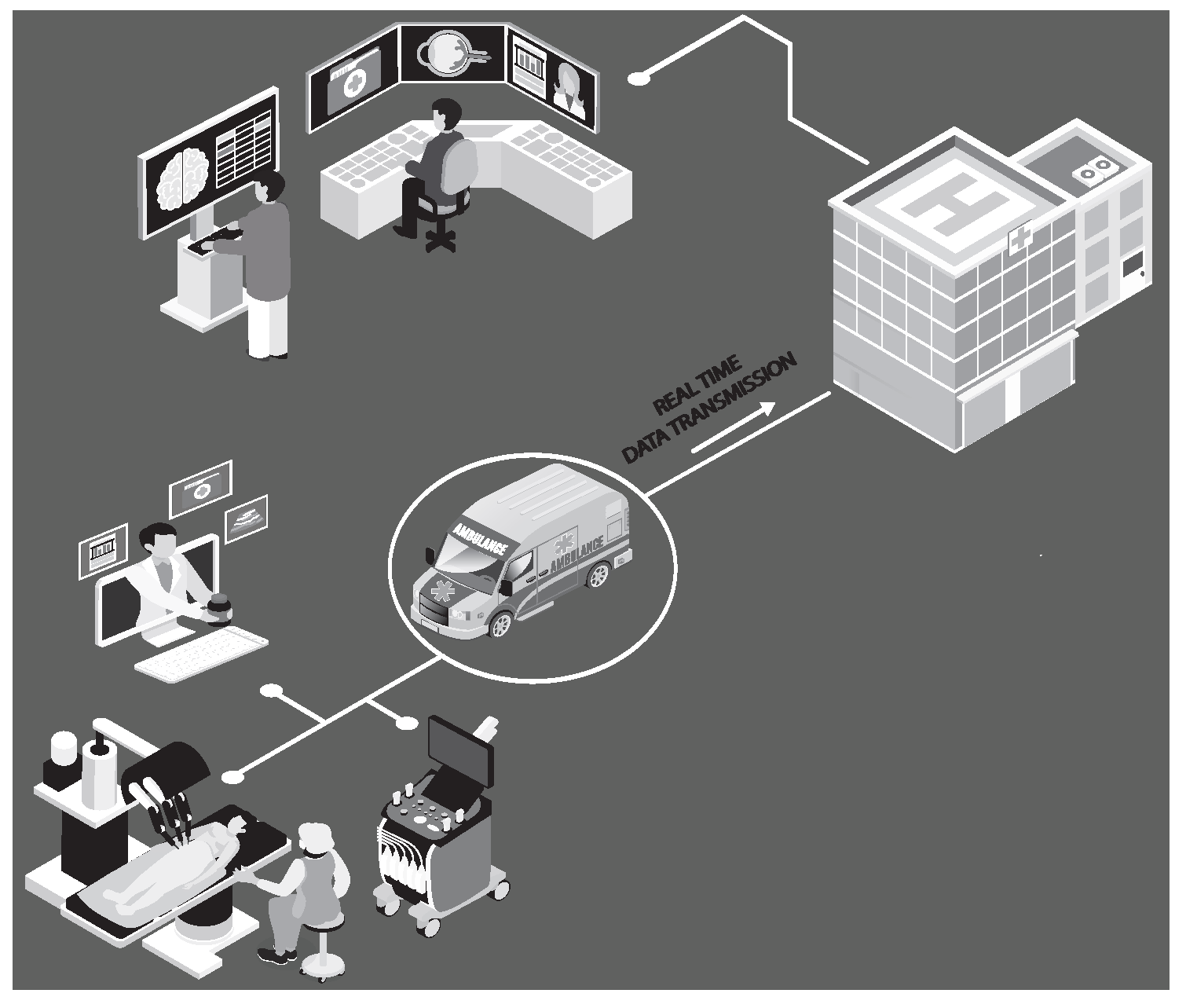
3.1.3. Data Transmission: Smart Ambulances
Healthcare Benefits
3.2. RQ2: What Is the Type of Technology Used, and What Technical Requirements Does an Intelligent Health System Demand through the Use of 5G?
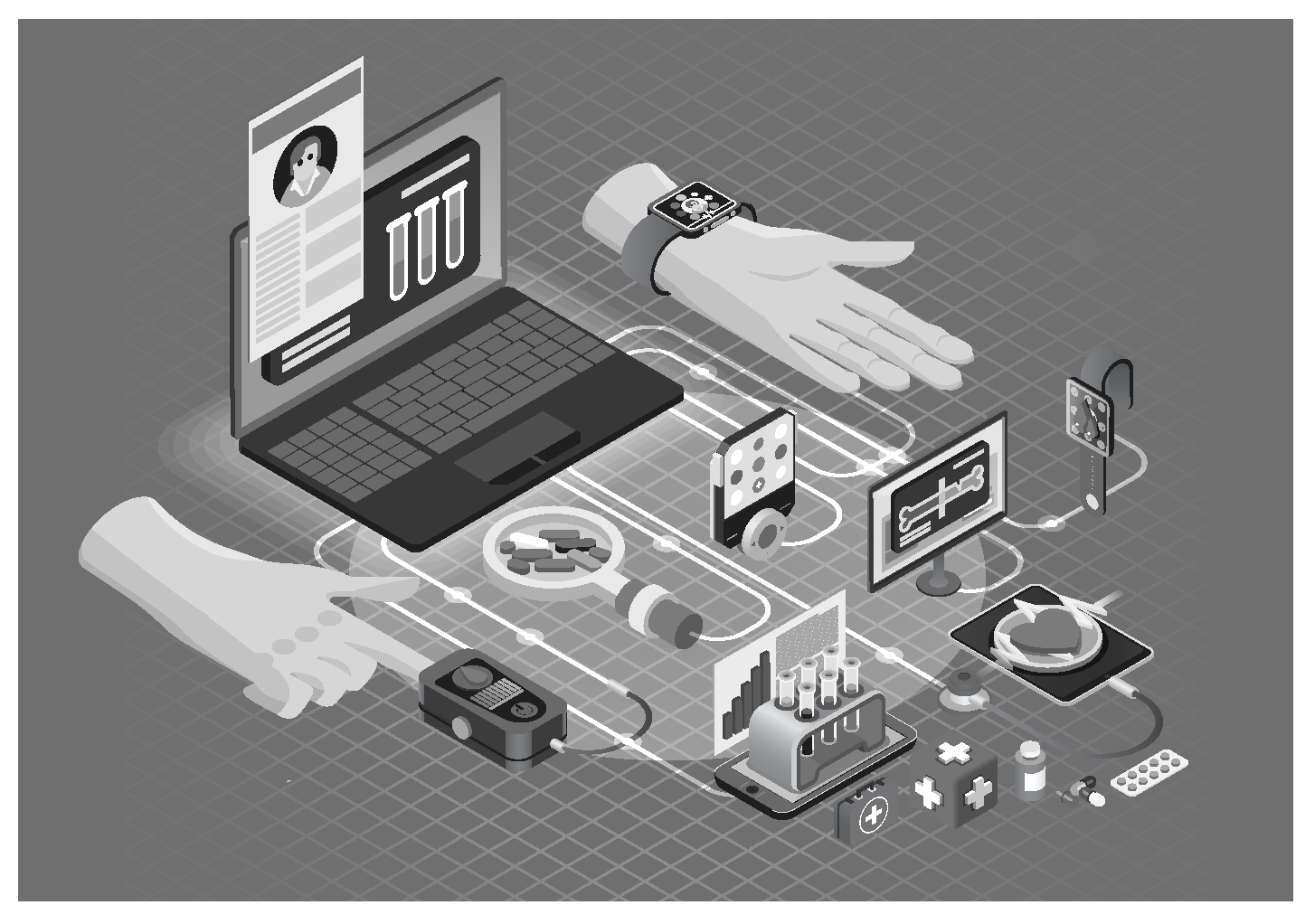
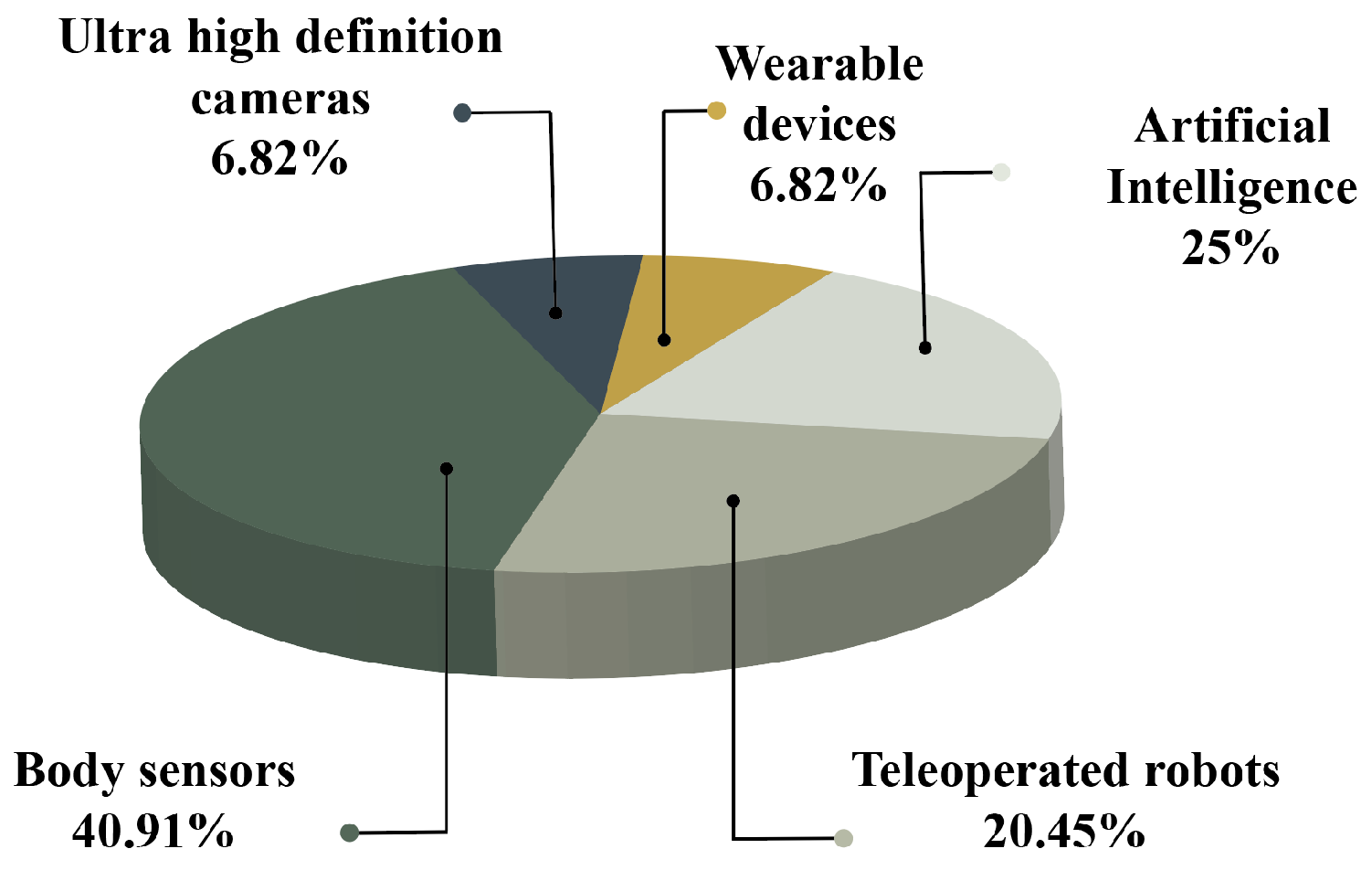
3.2.1. IoMT Devices
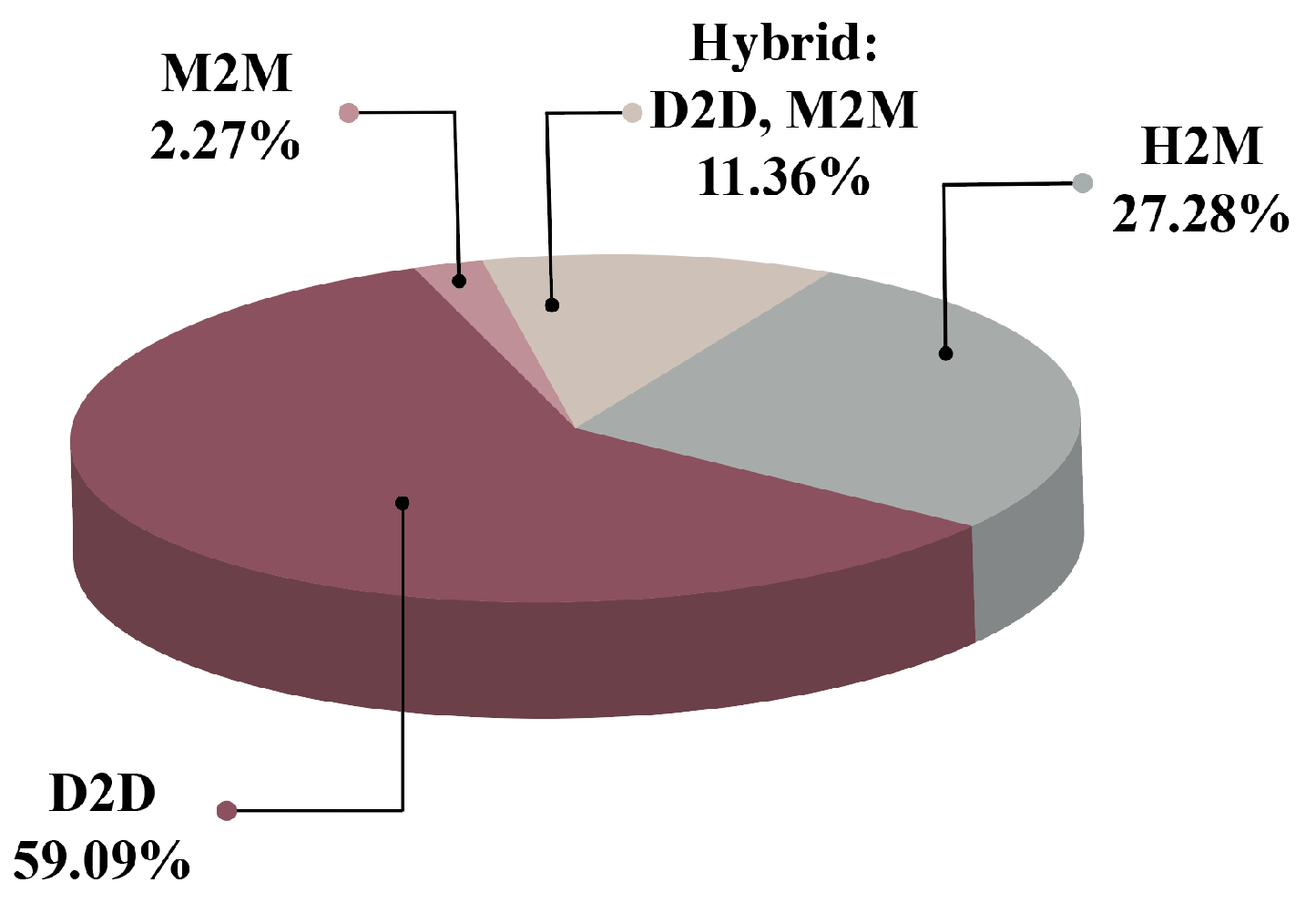
3.2.2. Communication Protocols
3.2.3. Networking Technologies
3.2.4. Network Technical Requirements
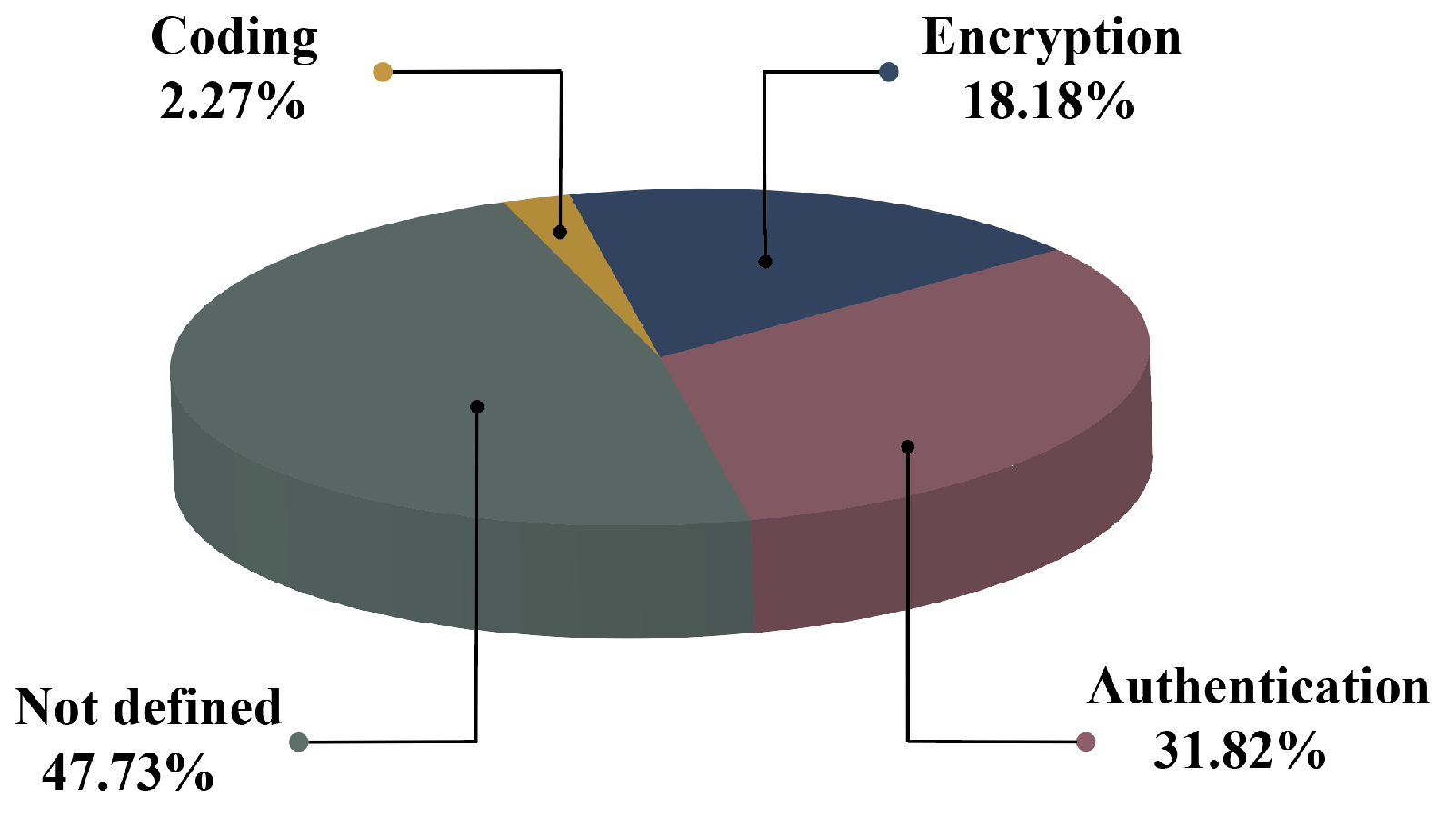
3.3. RQ3: What Are the Security Mechanisms or Protocols Required by Smart Health Systems Based on 5G?
3.3.1. Authentication
3.3.2. Encryption
3.3.3. Coding
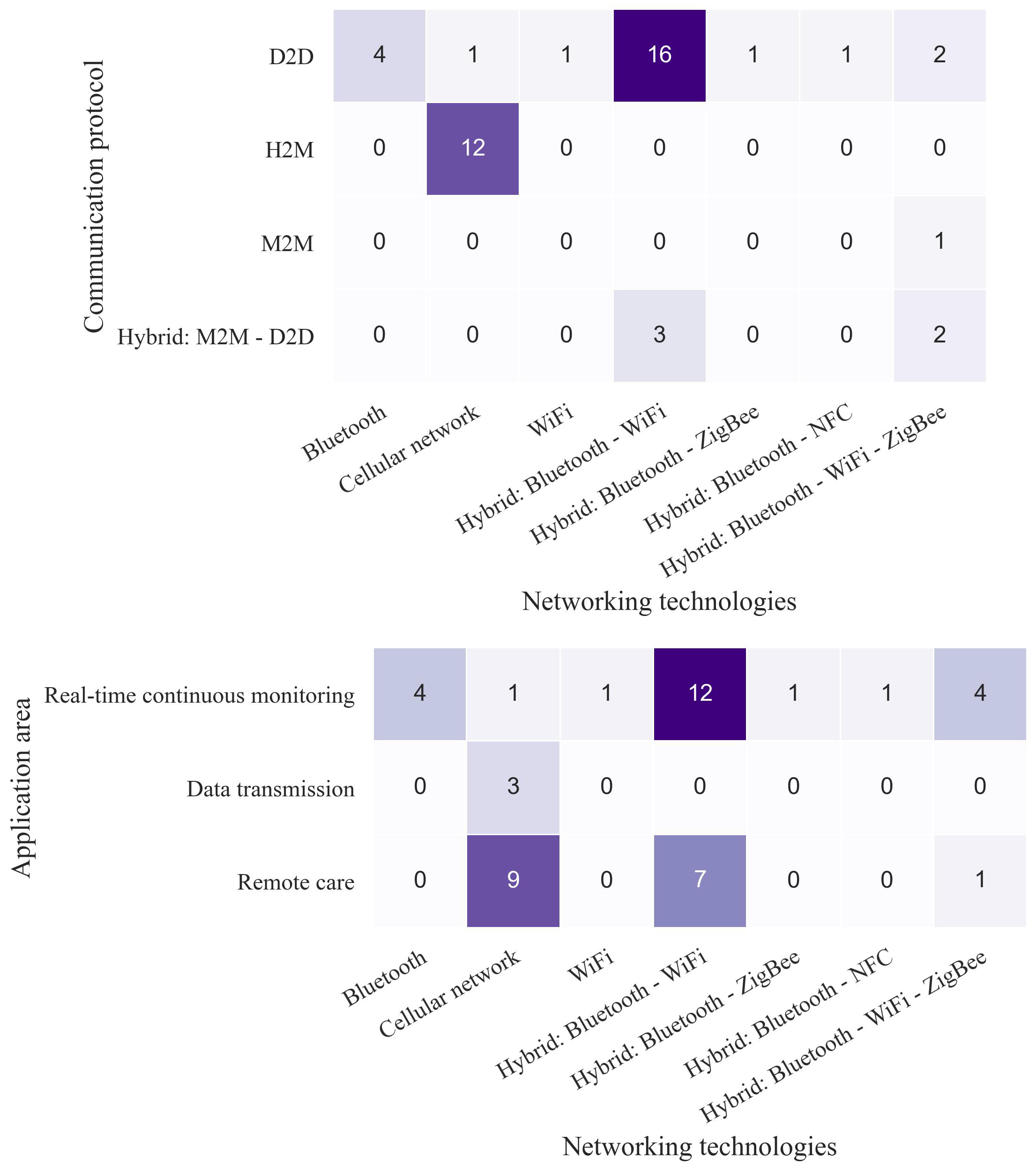
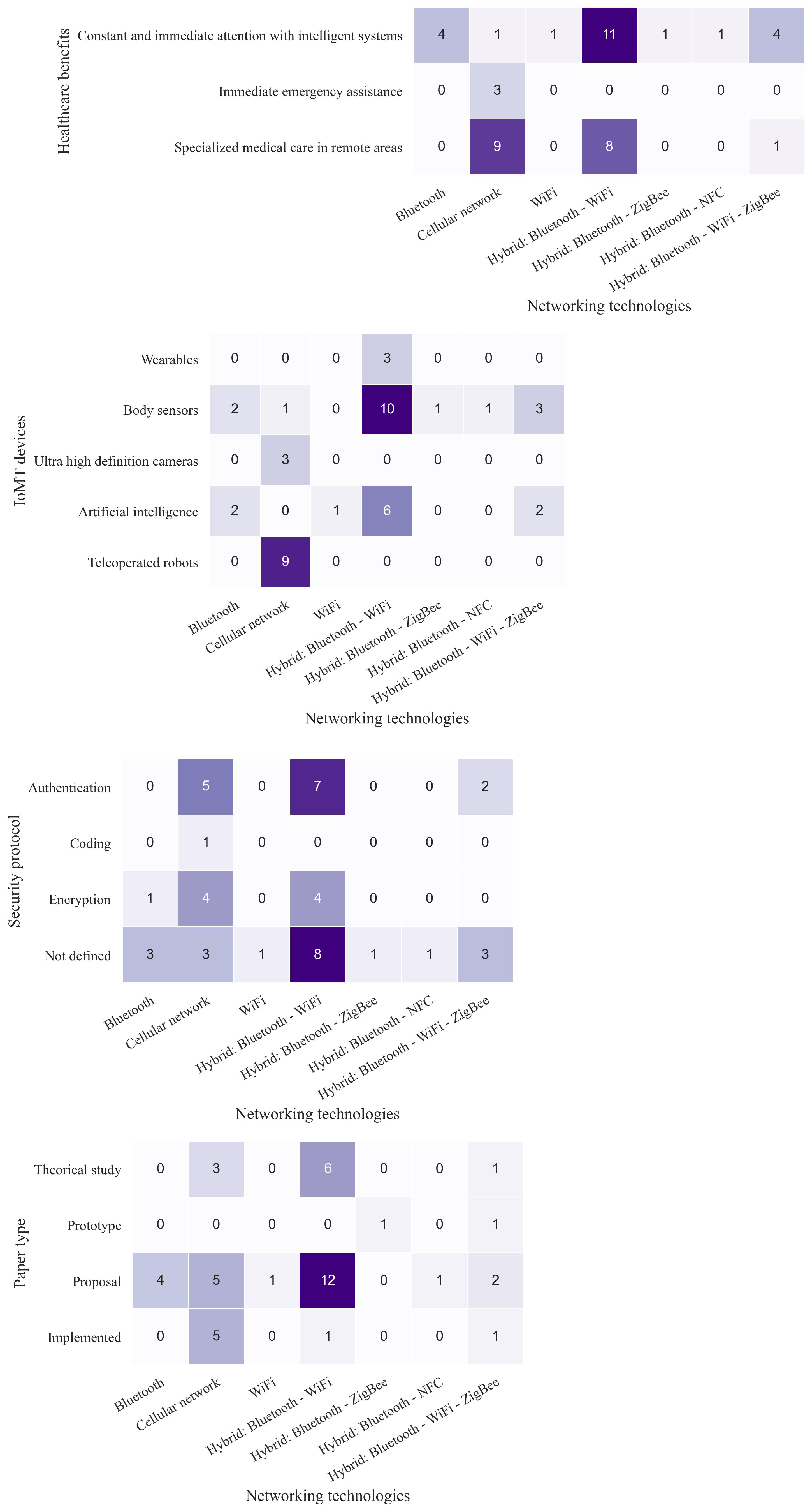
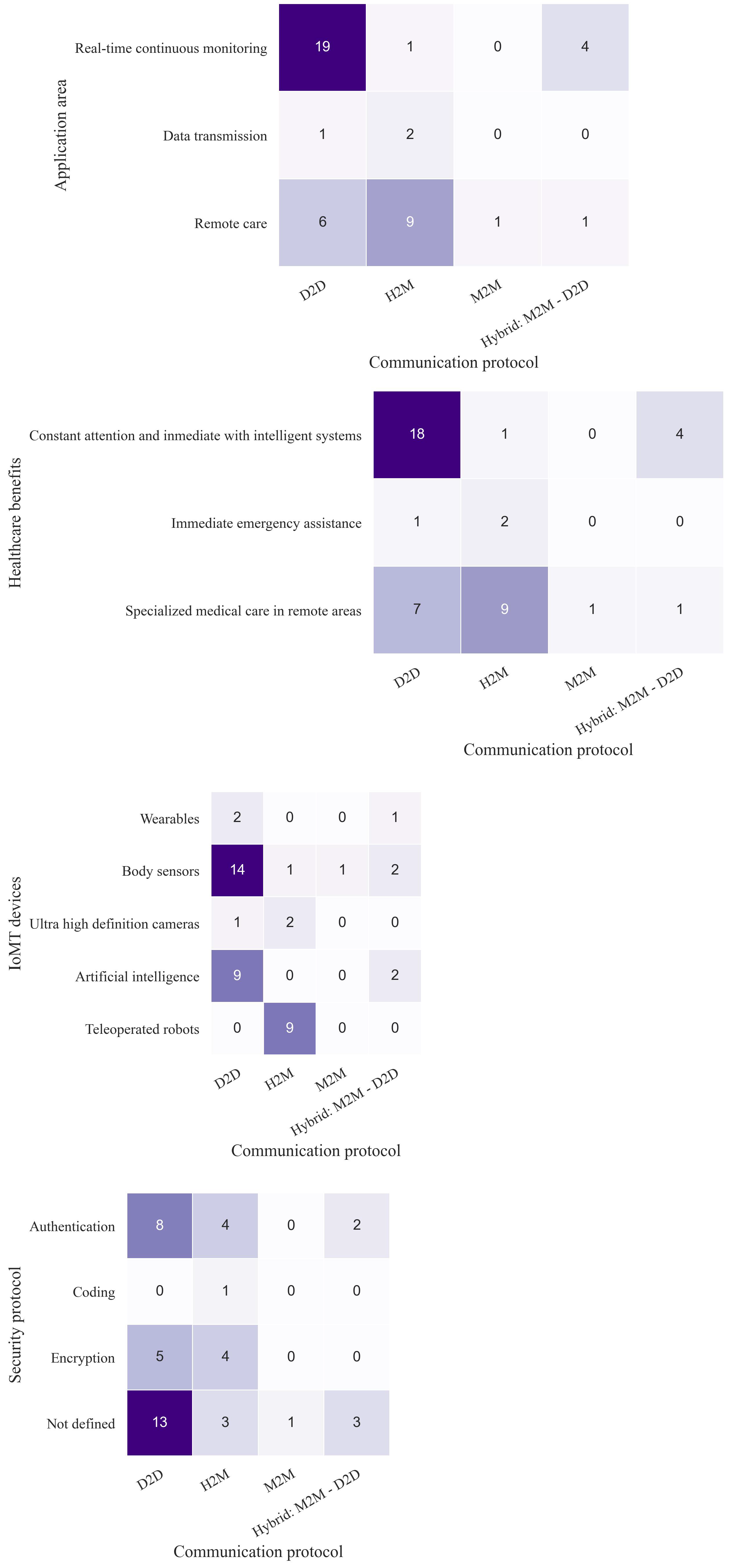
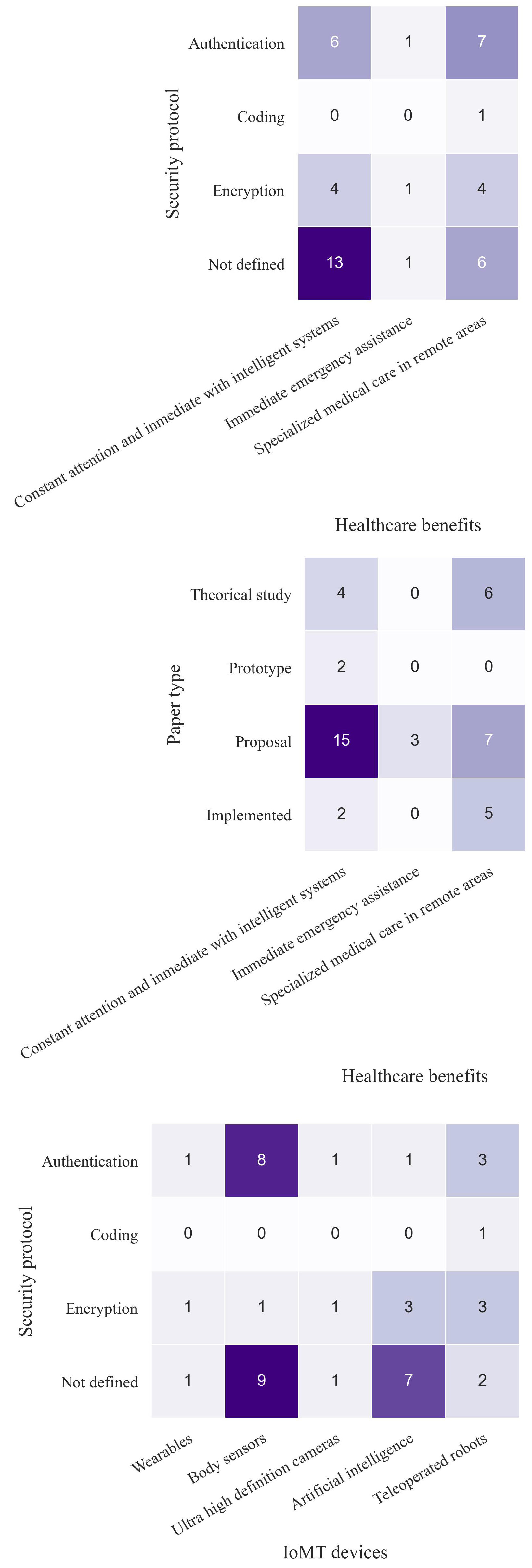
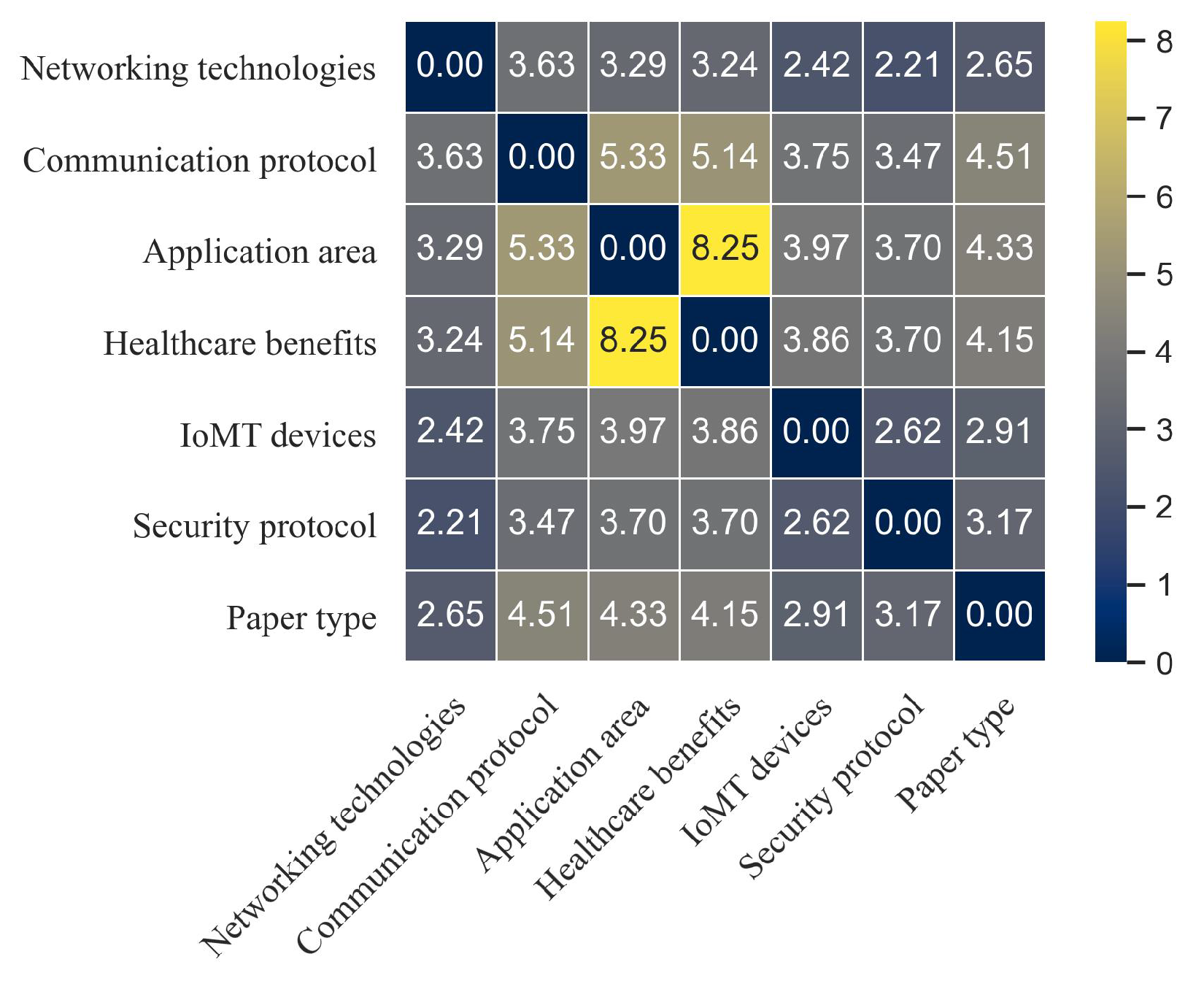
3.4. Correlation Analysis
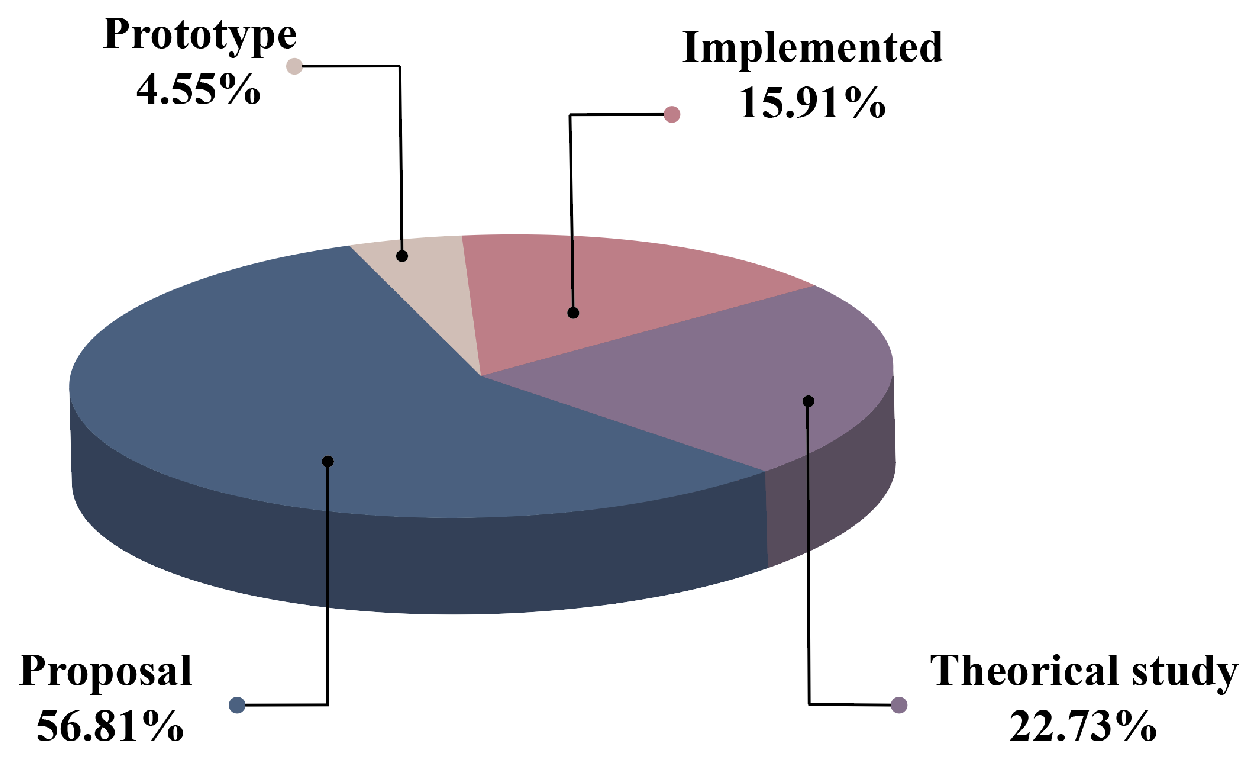
- Paper type: theoretical study; proposal; implementation; prototype.
- Application area: remote care: surgery and diagnosis; real-time continuous monitoring; data transmission: smart ambulances.
- Healthcare benefits: constant and immediate attention with intelligent systems; specialized medical care in remote areas; immediate emergency assistance.
- IoMT devices: body sensors; teleoperated robots; artificial intelligence; wearable devices; ultra high definition cameras.
- Communication protocols: D2D; M2M; H2M; hybrid: D2D–M2M.
- Networking technologies: WiFi; Bluetooth; cellular network; hybrid: Bluetooth–NFC; hybrid: Bluetooth–ZigBee; hybrid: Bluetooth–WiFi; hybrid: WiFi–ZigBee–Bluetooth.
- Security protocol: authentication; encryption; coding; not defined.
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| 4G | Fourth Generation |
| IoMT | Internet of Medical Things |
| 5G | Fifth Generation |
| IoT | Internet of Things |
| AI | Artificial Intelligence |
| 2G | Second Generation |
| 3G | Third Generation |
| WBSN | Wireless Body Sensor Network |
| URLLC | Ultra-Reliable Low Latency Communications |
| mMTC | Massive Machine Type Communication |
| eMBB | Enhanced Mobile Broadband |
| US | Ultrasound |
| ICU | Intensive Care Unit |
| SVM | Support Vector Machine |
| ANN | Artificial Neural Network |
| HSI | Human System Interface |
| DBN | Deep Belief Network |
| DP | Deep Learning |
| NFC | Near Field Communication |
| LBP | Local Binary Pattern |
| IDP | Interlaced Derivative Pattern |
| ERHs | Electronic Health reports |
| VR | Virtual Reality |
| ML | Machine Learning |
| D2D | Device to Device |
| H2M | Human to Machine |
| M2M | Machine to Machine |
| QoS | Quality of Service |
| IdM | Identity Management |
| EAP-TLS | Extensible Authentication Protocol- Transport Layer Security |
| FAIDM | Federated Anonymous Identity Management |
| UCSSO | User Controlled Single Sign On |
| VPN | Virtual Private Network |
| WHO | World Health Organization |
Appendix A. Pairwise Article Counts



References
- Neha, G.; Juneja, P.K.; Sharma, S.; Garg, U. Future Aspect of 5G-IoT Architecture in Smart Healthcare System. In Proceedings of the 2021 5th International Conference on Intelligent Computing and Control Systems (ICICCS), Madurai, India, 6–8 May 2021; pp. 406–411. [Google Scholar] [CrossRef]
- Magsi, H.; Sodhro, A.H.; Chachar, F.A.; Abro, S.A.K.; Sodhro, G.H.; Pirbhulal, S. Evolution of 5G in Internet of medical things. In Proceedings of the 2018 International Conference on Computing, Mathematics and Engineering Technologies (iCoMET), Sukkur, Pakistan, 3–4 March 2018; pp. 1–7. [Google Scholar] [CrossRef]
- Kapassa, E.; Touloupou, M.; Mavrogiorgou, A.; Kiourtis, A.; Giannouli, D.; Katsigianni, K.; Kyriazis, D. An Innovative eHealth System Powered By 5G Network Slicing. In Proceedings of the 2019 Sixth International Conference on Internet of Things: Systems, Management and Security (IOTSMS), Granada, Spain, 22–25 October 2019; pp. 7–12. [Google Scholar] [CrossRef]
- Dananjayan, S.; Raj, G.M. 5G in healthcare: How fast will be the transformation? Ir. J. Med Sci. (1971-) 2021, 190, 497–501. [Google Scholar] [CrossRef] [PubMed]
- Vergütz, A.; Prates, N.G.; Henrique Schwengber, B.; Santos, A.; Nogueira, M. An Architecture for the Performance Management of Smart Healthcare Applications. Sensors 2020, 20, 5566. [Google Scholar] [CrossRef]
- Le, T.V.; Hsu, C.L. An Anonymous Key Distribution Scheme for Group Healthcare Services in 5G-Enabled Multi-Server Environments. IEEE Access 2021, 9, 53408–53422. [Google Scholar] [CrossRef]
- Soldani, D.; Fadini, F.; Rasanen, H.; Duran, J.; Niemela, T.; Chandramouli, D.; Hoglund, T.; Doppler, K.; Himanen, T.; Laiho, J.; et al. 5G Mobile Systems for Healthcare. In Proceedings of the 2017 IEEE 85th Vehicular Technology Conference (VTC Spring), Sydney, Australia, 4–7 June 2017; pp. 1–5. [Google Scholar] [CrossRef]
- Latif, S.; Qadir, J.; Farooq, S.; Imran, M.A. How 5g wireless (and concomitant technologies) will revolutionize healthcare? Future Internet 2017, 9, 93. [Google Scholar] [CrossRef] [Green Version]
- Selem, E.; Fatehy, M.; El-Kader, S.M.A. E-Health applications over 5G networks: Challenges and state of the art. In Proceedings of the 2019 6th International Conference on Advanced Control Circuits and Systems (ACCS) 2019 5th International Conference on New Paradigms in Electronics information Technology (PEIT), Hurghada, Egypt, 17–20 November 2019; pp. 111–118. [Google Scholar] [CrossRef]
- Contreras, C.M.; Metzger, G.A.; Beane, J.D.; Dedhia, P.H.; Ejaz, A.; Pawlik, T.M. Telemedicine: Patient-Provider Clinical Engagement During the COVID-19 Pandemic and Beyond. J. Gastrointest. Surg. 2020, 24, 1692–1697. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C. 5G Aplications Help and China Fight against COVID-19. Available online: http://www.caict.ac.cn/english/research/covid19/study/202004/t20200426_280331.html (accessed on 13 October 2021).
- Kim, H.; Kim, S.W.; Park, E.; Kim, J.; Chang, H. The role of fifth-generation mobile technology in prehospital emergency care: An opportunity to support paramedics. Health Policy Technol. 2020, 9, 109–114. [Google Scholar] [CrossRef]
- Siriwardhana, Y.; Gür, G.; Ylianttila, M.; Liyanage, M. The role of 5G for digital healthcare against COVID-19 pandemic: Opportunities and challenges. ICT Express 2021, 7, 244–252. [Google Scholar] [CrossRef]
- Ahad, A.; Tahir, M.; Aman Sheikh, M.; Ahmed, K.I.; Mughees, A.; Numani, A. Technologies Trend towards 5G Network for Smart Health-Care Using IoT: A Review. Sensors 2020, 20, 4047. [Google Scholar] [CrossRef]
- Penn, J.; Marcus, H.; Uff, C. Fifth Generation Cellular Networks and Neurosurgery: A Narrative Review. World Neurosurg. 2021, 156, 96–102. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef] [Green Version]
- Mattos, W.D.; Gondim, P.R. M-Health Solutions Using 5G Networks and M2M Communications. IT Prof. 2016, 18, 24–29. [Google Scholar] [CrossRef]
- Jusak, J.; Pratikno, H.; Putra, V.H. Internet of Medical Things for cardiac monitoring: Paving the way to 5G mobile networks. In Proceedings of the 2016 IEEE International Conference on Communication, Networks and Satellite (COMNETSAT), Surabaya, Indonesia, 8–10 December 2016; pp. 75–79. [Google Scholar] [CrossRef]
- Philip, N.Y.; Rehman, I.U. Towards 5G Health for Medical Video Streaming over Small Cells. In Proceedings of the XIV Mediterranean Conference on Medical and Biological Engineering and Computing 2016, Paphos, Cyprus, 31 March–2 April 2016; Kyriacou, E., Christofides, S., Pattichis, C.S., Eds.; Springer International Publishing: Berlin/Heidelberg, Germany; pp. 1093–1098. [Google Scholar]
- Nasri, F.; Mtibaa, A. Smart Mobile Healthcare System based on WBSN and 5G. Int. J. Adv. Comput. Sci. Appl. 2017, 8, 147–156. [Google Scholar] [CrossRef]
- Lloret, J.; Parra, L.; Taha, M.; Tomas, J. An architecture and protocol for smart continuous eHealth monitoring using 5G. Comput. Netw. 2017, 129, 340–351. [Google Scholar] [CrossRef]
- Hossain, M.S.; Muhammad, G. Emotion-Aware Connected Healthcare Big Data Towards 5G. IEEE Internet Things J. 2018, 5, 2399–2406. [Google Scholar] [CrossRef]
- Guo, J. Smartphone-Powered Electrochemical Biosensing Dongle for Emerging Medical IoTs Application. IEEE Trans. Ind. Inform. 2018, 14, 2592–2597. [Google Scholar] [CrossRef]
- Fang, D.; Ye, F. Identity Management Framework for E-Health Systems over 5G Networks. In Proceedings of the 2018 IEEE International Conference on Communications (ICC), Kansas City, MO, USA, 20–24 May 2018; pp. 1–6. [Google Scholar] [CrossRef]
- Dhaya, R.; Suganth Maharaja, S.; Sowmya, J.; Kanthavel, R. Advanced LTE (5G) in Medical IOT-Research, Future and Scope. In Proceedings of the Smart Trends in Information Technology and Computer Communications, Pune, India, 18–19 August 2017; Deshpande, A., Unal, A., Passi, K., Singh, D., Nayak, M., Patel, B., Pathan, S., Eds.; Springer: Singapore, 2017; pp. 192–200. [Google Scholar]
- Mohanta, B.; Das, P.; Patnaik, S. Healthcare 5.0: A Paradigm Shift in Digital Healthcare System Using Artificial Intelligence, IOT and 5G Communication. In Proceedings of the 2019 International Conference on Applied Machine Learning (ICAML), Bhubaneswar, India, 27–28 September 2019; pp. 191–196. [Google Scholar] [CrossRef]
- Zhang, D.; Zhang, T.; Zhai, Y.; Rodrigues, J.J.P.C.; Zhang, D.; Wen, Z.; Yu, K.; Sato, T. 5G-Enabled Health Systems: Solutions, Challenges and Future Research Trends. In Proceedings of the 2019 ITU Kaleidoscope: ICT for Health: Networks, Standards and Innovation (ITU K), Atlanta, GA, USA, 4–6 December 2019; pp. 1–8. [Google Scholar] [CrossRef]
- Mamun, M.I.; Rahman, A.; Khaleque, M.A.; Hamid, M.A.; Mridha, M.F. AutiLife: A Healthcare Monitoring System for Autism Center in 5G Cellular Network using Machine Learning Approach. In Proceedings of the 2019 IEEE 17th International Conference on Industrial Informatics (INDIN), Helsinki-Espoo, Finland, 22–25 July 2019; Volume 1, pp. 1501–1506. [Google Scholar] [CrossRef]
- Gupta, R.; Tanwar, S.; Tyagi, S.; Kumar, N. Tactile-Internet-Based Telesurgery System for Healthcare 4.0: An Architecture, Research Challenges, and Future Directions. IEEE Netw. 2019, 33, 22–29. [Google Scholar] [CrossRef]
- Imran, M.A.; Sambo, Y.A.; Abbasi, Q.H. 5G Communication Systems and Connected Healthcare. In Enabling 5G Communication Systems to Support Vertical Industries; Wiley: Hoboken, NJ, USA, 2019; pp. 149–177. [Google Scholar] [CrossRef]
- Usman, M.; Philip, N.; Politis, C. 5G enabled mobile healthcare for ambulances. In Proceedings of the 2019 IEEE Globecom Workshops (GC Wkshps), Waikoloa, HI, USA, 9–13 December 2019. [Google Scholar] [CrossRef]
- Haider, D.; Yang, X.; Abbasi, Q.H. Post-surgical fall detection by exploiting the 5 G C-Band technology for eHealth paradigm. Appl. Soft Comput. 2019, 81, 105537. [Google Scholar] [CrossRef]
- Morosi, S.; Jayousi, S.; Mucchi, L.; Peinetti, F.; Mastrantonio, L.; Fioravanti, G.; Giacomini, A.; Fratini, A.; Padiglione, F.; De Lucia, F. Medical Tele-Monitoring and Tele-Assistance for Diabetics Patients by Means of 5G Cellular Networks. In Proceedings of the EAI International Conference on Body Area Networks, Florence, Italy, 2–3 October 2019; Springer: Berlin/Heidelberg, Germany, 2019; pp. 79–88. [Google Scholar]
- Padmashree, T.; Nayak, S.S. 5G Technology for E-Health. In Proceedings of the 2020 Fourth International Conference on I-SMAC (IoT in Social, Mobile, Analytics and Cloud) (I-SMAC), Palladam, India, 7–9 October 2020; pp. 211–216. [Google Scholar] [CrossRef]
- Tsoulchas, V.; Tsolis, N.; Zoumi, E.; Skondras, E.; Vergados, D.D. Health Monitoring of People with Diabetes using IoT and 5G Wireless Network Infrastructures. In Proceedings of the 2020 11th International Conference on Information, Intelligence, Systems and Applications (IISA), Piraeus, Greece, 15–17 July 2020; pp. 1–6. [Google Scholar] [CrossRef]
- Meshram, D.A.; Patil, D.D. 5G Enabled Tactile Internet for Tele-Robotic Surgery. Procedia Comput. Sci. 2020, 171, 2618–2625. [Google Scholar] [CrossRef]
- Kumar, A.; Albreem, M.; Gupta, M.; Alsharif, M.; Kim, S. Future 5g network based smart hospitals: Hybrid detection technique for latency improvement. IEEE Access 2020, 8, 153240–153249. [Google Scholar] [CrossRef]
- Zheng, J.; Wang, Y.; Zhang, J.; Guo, W.; Yang, X.; Luo, L.; Jiao, W.; Hu, X.; Yu, Z.; Wang, C.; et al. 5G ultra-remote robot-assisted laparoscopic surgery in China. Surg. Endosc. Other Interv. Tech. 2020, 34, 5172–5180. [Google Scholar] [CrossRef]
- Ye, J. The Role of Health Technology and Informatics in a Global Public Health Emergency: Practices and Implications From the COVID-19 Pandemic. JMIR Med. Inform. 2020, 8, e19866. [Google Scholar] [CrossRef] [PubMed]
- Khorashadizadeh, S.; Ikuesan, A.R.; Kebande, V.R. Generic 5g infrastructure for iot ecosystem. In Proceedings of the International Conference of Reliable Information and Communication Technology, Johor, Malaysia, 22–23 September 2019; Springer: Berlin/Heidelberg, Germany, 2020; pp. 451–462. [Google Scholar]
- Chen, B.; Qiao, S.; Zhao, J.; Liu, D.; Shi, X.; Lyu, M.; Chen, H.; Lu, H.; Zhai, Y. A Security Awareness and Protection System for 5G Smart Healthcare Based on Zero-Trust Architecture. IEEE Internet Things J. 2021, 8, 10248–10263. [Google Scholar] [CrossRef] [PubMed]
- Angelucci, A.; Kuller, D.; Aliverti, A. A Home Telemedicine System for Continuous Respiratory Monitoring. IEEE J. Biomed. Health Inform. 2021, 25, 1247–1256. [Google Scholar] [CrossRef]
- Zhai, Y.; Xu, X.; Chen, B.; Lu, H.; Wang, Y.; Li, S.; Shi, X.; Wang, W.; Shang, L.; Zhao, J. 5G-Network-Enabled Smart Ambulance: Architecture, Application, and Evaluation. IEEE Netw. 2021, 35, 190–196. [Google Scholar] [CrossRef]
- Zhan, K. Sports and health big data system based on 5G network and Internet of Things system. Microprocess. Microsyst. 2021, 80, 103363. [Google Scholar] [CrossRef]
- Pustokhin, D.A.; Pustokhina, I.V.; Rani, P.; Kansal, V.; Elhoseny, M.; Joshi, G.P.; Shankar, K. Optimal deep learning approaches and healthcare big data analytics for mobile networks toward 5G. Comput. Electr. Eng. 2021, 95, 107376. [Google Scholar] [CrossRef]
- Braeken, A.; Liyanage, M. Highly efficient key agreement for remote patient monitoring in MEC-enabled 5G networks. J. Supercomput. 2021, 77, 5562–5585. [Google Scholar] [CrossRef]
- Zhang, Y.; Wang, X.; Han, N.; Zhao, R. Ensemble Learning Based Postpartum Hemorrhage Diagnosis for 5G Remote Healthcare. IEEE Access 2021, 9, 18538–18548. [Google Scholar] [CrossRef]
- Zhang, D.; Rodrigues, J.; Zhai, Y.; Sato, T. Design and Implementation of 5G e-Health Systems: Technologies, Use Cases, and Future Challenges. IEEE Commun. Mag. 2021, 59, 80–85. [Google Scholar] [CrossRef]
- Lin, T.W.; Hsu, C.L. FAIDM for Medical Privacy Protection in 5G Telemedicine Systems. Appl. Sci. 2021, 11, 1155. [Google Scholar] [CrossRef]
- Hameed, K.; Bajwa, I.S.; Sarwar, N.; Anwar, W.; Mushtaq, Z.; Rashid, T. Integration of 5G and Block-Chain Technologies in Smart Telemedicine Using IoT. J. Healthc. Eng. 2021, 2021, 8814364. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Pan, X.; Yang, J.; Fan, J.; Qin, M.; Sun, H.; Liu, J.; Li, N.; Ting, D.S.W.; Chen, Y. Application of 5G Technology to Conduct Real-Time Teleretinal Laser Photocoagulation for the Treatment of Diabetic Retinopathy. JAMA Ophthalmol. 2021, 139, 975–982. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Chen, S.; Tian, S.; Liu, K.; Ni, J.; Zhao, M.; Kang, Y.; Ma, X.; Guo, J. 5G-enabled ultra-sensitive fluorescence sensor for proactive prognosis of COVID-19. Biosens. Bioelectron. 2021, 181, 113160. [Google Scholar] [CrossRef] [PubMed]
- Lin, T.W.; Hsu, C.L.; Le, T.V.; Lu, C.F.; Huang, B.Y. A Smartcard-Based User-Controlled Single Sign-On for Privacy Preservation in 5G-IoT Telemedicine Systems. Sensors 2021, 21, 2880. [Google Scholar] [CrossRef] [PubMed]
- Minahil; Ayub, M.F.; Mahmood, K.; Kumari, S.; Sangaiah, A.K. Lightweight authentication protocol for e-health clouds in IoT-based applications through 5G technology. Digit. Commun. Netw. 2021, 7, 235–244. [Google Scholar] [CrossRef]
- Tang, Z.; Hu, H.; Xu, C.; Zhao, K. Exploring an Efficient Remote Biomedical Signal Monitoring Framework for Personal Health in the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 9037. [Google Scholar] [CrossRef]
- Ying, S.; Yu, W. Application of 5G Technology in the Construction of Intelligent Health Management System. In Proceedings of the International Conference on Human–Computer Interaction, Virtual Event, 24–29 July 2021; Springer: Berlin/Heidelberg, Germany, 2021; pp. 408–413. [Google Scholar]
- Mishra, L.; Vikash; Varma, S. Seamless Health Monitoring Using 5G NR for Internet of Medical Things. Wirel. Pers. Commun. 2021, 120, 2259–2289. [Google Scholar] [CrossRef]
- Wang, J.; Peng, C.; Zhao, Y.; Ye, R.; Hong, J.; Huang, H.; Chen, L. Application of a Robotic Tele-Echography System for COVID-19 Pneumonia. J. Ultrasound Med. 2021, 40, 385–390. [Google Scholar] [CrossRef]
- Duan, S.; Liu, L.; Chen, Y.; Yang, L.; Zhang, Y.; Wang, S.; Hao, L.; Zhang, L. A 5G-powered robot-assisted teleultrasound diagnostic system in an intensive care unit. Crit. Care 2021, 25, 134. [Google Scholar] [CrossRef]
- Talukder, A.; Haas, R. AIoT: AI meets IoT and Web in Smart Healthcare. In Proceedings of the 13th ACM Web Science Conference 2021, Virtual Event, UK, 21–25 June 2021; ACM: New York, NY, USA, 2021; pp. 92–98. [Google Scholar] [CrossRef]
- Haghi Kashani, M.; Madanipour, M.; Nikravan, M.; Asghari, P.; Mahdipour, E. A systematic review of IoT in healthcare: Applications, techniques, and trends. J. Netw. Comput. Appl. 2021, 192, 103164. [Google Scholar] [CrossRef]
- Guerrero-Vásquez, L.F.; López-Nores, M.; Pazos-Arias, J.J.; Robles-Bykbaev, V.E.; Bustamante-Cacao, K.C.; Jara-Quito, H.J.; Bravo-Torres, J.F.; Campoverde-Jara, P.X. Systematic Review of Technological Aids to Social Interaction in Autistic Spectrum Disorders from Transversal Perspectives: Psychology, Technology and Therapy. In Review Journal of Autism and Developmental Disorders; Springer: Berlin/Heidelberg, Germany, 2022; pp. 1–30. [Google Scholar]
- Rocha, N.P.; Dias, A.; Santinha, G.; Rodrigues, M.; Queirós, A.; Rodrigues, C. Smart cities and public health: A systematic review. Procedia Comput. Sci. 2019, 164, 516–523. [Google Scholar] [CrossRef]
- Pacheco Rocha, N.; Dias, A.; Santinha, G.; Rodrigues, M.; Queirós, A.; Rodrigues, C. Smart Cities and Healthcare: A Systematic Review. Technologies 2019, 7, 58. [Google Scholar] [CrossRef] [Green Version]
- Rocha, N.P.; Bastardo, R.; Pavão, J.; Santinha, G.; Rodrigues, M.; Rodrigues, C.; Queirós, A.; Dias, A. Smart Cities’ Applications to Facilitate the Mobility of Older Adults: A Systematic Review of the Literature. Appl. Sci. 2021, 11, 6395. [Google Scholar] [CrossRef]
- Cortés. Tendencias de Salud Digital 2022. Available online: https://www.conexiones365.com/nota/expo-med/innovacion/tendencias-salud-digital-2022 (accessed on 9 December 2021).
- WHO. La Oms Publica El Primer Informe Mundial Sobre Inteligencia Artificial (IA) Aplicada a la Salud y Seis Principios Rectores Relativos a su Concepción Y Utilización. Available online: https://www.who.int/es/news/item/28-06-2021-who-issues-first-global-report-on-ai-in-health-and-six-guiding-principles-for-its-design-and-use (accessed on 10 December 2021).




| Ref. | Author | Source | Year | Country |
|---|---|---|---|---|
| [17] | Mattos and Gondim | IEEE | 2016 | Brasil |
| [18] | Jusak et al. | IEEE | 2016 | Indonesia |
| [19] | Philip and Rehman | Springer | 2016 | United Kingdom |
| [20] | Nasri and Mtibaa | Web of Science | 2017 | Tunisia |
| [21] | Lloret et al. | Web of Science | 2017 | Spain |
| [22] | Nasri and Mtibaa | IEEE | 2018 | Saudi Arabia |
| [23] | Guo | IEEE | 2018 | China |
| [24] | Fang and Ye | IEEE | 2018 | USA |
| [25] | Dhaya et al. | Springer | 2018 | India |
| [26] | Mohanta et al. | IEEE | 2019 | India |
| [27] | Zhang et al. | IEEE | 2019 | Japan |
| [28] | Mamun et al. | IEEE | 2019 | Bangladesh |
| [29] | Gupta et al. | IEEE | 2019 | India |
| [30] | Imran et al. | IEEE | 2019 | India |
| [31] | Usman et al. | Scopus | 2019 | United Kingdom |
| [32] | Haider et al. | Web of Science | 2019 | China |
| [33] | Morosi et al. | Springer | 2019 | Italy |
| [34] | Padmashree and Nayak | IEEE | 2020 | India |
| [35] | Tsoulchas et al. | IEEE | 2020 | Greece |
| [36] | Meshram and Patil | Science Direct | 2020 | India |
| [37] | Kumar et al. | Scopus | 2020 | India |
| [38] | Zheng et al. | Web of Science | 2020 | China |
| [39] | Ye | Web of Science | 2020 | USA |
| [40] | Khorashadizadeh et al. | Springer | 2020 | Malaysia |
| [41] | Chen et al. | IEEE | 2021 | China |
| [42] | Angelucci et al. | IEEE | 2021 | USA |
| [43] | Zhai et al. | IEEE | 2021 | China |
| [44] | Zhan | Science Direct | 2021 | China |
| [45] | Pustokin et al. | Science Direct | 2021 | Spain |
| [46] | Braeken and Liyanage | Scopus | 2021 | Finland |
| [47] | Zhang et al. | Scopus | 2021 | China |
| [48] | Zhang et al. | Scopus | 2021 | China |
| [49] | Lin and Hsu | Web of Science | 2021 | Taiwán |
| [50] | Hameed et al. | Web of Science | 2021 | Pakistan |
| [51] | Chen et al. | Web of Science | 2021 | China |
| [52] | Guo et al. | Web of Science | 2021 | China |
| [53] | Lin et al. | Web of Science | 2021 | Taiwan |
| [54] | Minahil et al. | Web of Science | 2021 | Pakistan |
| [55] | Tang et al. | Web of Science | 2021 | China |
| [56] | Ying and Yu | Springer | 2021 | China |
| [57] | Mishra et al. | Springer | 2021 | India |
| [58] | Wang et al. | Wiley Online Library | 2021 | China |
| [59] | Duan et al. | Gale Power Search | 2021 | China |
| [60] | Talukder and Haas | ACM Digital Library | 2021 | India |
| Application Area | Article |
|---|---|
| Remote care: surgery and diagnosis | [26,27,29,30,34,36,37,38,39,40,41,45,47,51,53,54,58,59,60] |
| Real-time continuous monitoring | [17,18,20,21,22,23,24,25,28,32,33,35,42,44,46,48,49,50,52,55,56,57] |
| Data transmission: smart ambulance | [19,31,43] |
| Healthcare Benefits | Article |
|---|---|
| Constant attention and inmediate with intelligent systems | [17,18,20,21,22,23,24,25,26,28,32,33,35,42,44,48,49,50,52,55,56,57,60] |
| Specialized medical care in remote areas | [27,29,30,34,36,37,38,39,40,41,45,46,47,53,54,56,58,59] |
| Immediate emergency assistance | [19,31,43] |
| Ref. | Capacity | Latency |
|---|---|---|
| [17] | Peak data rate 10 Gbps | ≤1 ms |
| [19] | Peak data rate 10 Gbps | ≤1 ms |
| [21] | Bandwidth 1000 MbpsMbps | 1–5 ms |
| [25] | Bandwidth 1 Gbps | - |
| [26] | Data rate 137 MbpsMbps-1.6 Gbps | - |
| [27] | Downlink peak speed 1 Gb/s, Uplink peak speed 100 MbpsMb/s | 7.6 ms |
| [29] | - | <1 ms |
| [30] | - | 100 ms, 10 ms y 1 ms |
| [31] | Data rate 10 Gbps | 1–4 ms |
| [33] | 200 MbpsMbps | - |
| [34] | Bandwidth > 1 Gbps average speed 200–400 MbpsMbps | <10 ms |
| [36] | Ultra high data rate > 1 Gbps | <5 ms |
| [37] | Data rate of 10 Gbps | <1 ms |
| [38] | Bandwidth Gb/s | 264 ms |
| [39] | Peak data rate 10 Gb/s | 1 ms |
| [40] | Data rate > 1 Gb/ss | ≤ 1 ms |
| [43] | Data rate 10–20 Gbps | 12.88 ms |
| [48] | Uplink transmission speed 100 MbpsMbps | 10 ms |
| [51] | Upload speed 88.45 MbpsMb/s and Download speed 853.63 MbpsMb/s | 20 ms |
| [57] | 20 Gbps for downloading and 10 Gbpsfor uplink | 1 ms |
| [58] | Transmission rates 930/132 MbpsMbps audio/video | 1 ms |
| [59] | Download speed 580 MbpsMbps upload speed 92 MbpsMbps | - |
| [60] | Download speed 20 Gbps | 1 ms |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Peralta-Ochoa, A.M.; Chaca-Asmal, P.A.; Guerrero-Vásquez, L.F.; Ordoñez-Ordoñez, J.O.; Coronel-González, E.J. Smart Healthcare Applications over 5G Networks: A Systematic Review. Appl. Sci. 2023, 13, 1469. https://doi.org/10.3390/app13031469
Peralta-Ochoa AM, Chaca-Asmal PA, Guerrero-Vásquez LF, Ordoñez-Ordoñez JO, Coronel-González EJ. Smart Healthcare Applications over 5G Networks: A Systematic Review. Applied Sciences. 2023; 13(3):1469. https://doi.org/10.3390/app13031469
Chicago/Turabian StylePeralta-Ochoa, Angélica M., Pedro A. Chaca-Asmal, Luis F. Guerrero-Vásquez, Jorge O. Ordoñez-Ordoñez, and Edwin J. Coronel-González. 2023. "Smart Healthcare Applications over 5G Networks: A Systematic Review" Applied Sciences 13, no. 3: 1469. https://doi.org/10.3390/app13031469
APA StylePeralta-Ochoa, A. M., Chaca-Asmal, P. A., Guerrero-Vásquez, L. F., Ordoñez-Ordoñez, J. O., & Coronel-González, E. J. (2023). Smart Healthcare Applications over 5G Networks: A Systematic Review. Applied Sciences, 13(3), 1469. https://doi.org/10.3390/app13031469








