Abstract
Although malignant melanoma (MM) most frequently tends to metastasize to the regional lymph nodes, liver, lung and brain, several unusual sites of metastasis have been described in the literature. Among these, the metastatic involvement of gallbladder or uterus represents an exceptional event, usually associated with diffuse metastatic disease or observed as an autopsy finding. In this paper, we present two unusual cases of isolated MM metastasis to these anatomic sites, arising in a 71-year-old man and a 54-year-old woman, for whom no information on previous malignancies was known at the time of the histological examination. The clinico-pathologic features are described, emphasizing that MM metastasis must be included in the differential diagnosis when dealing with patients with a previous diagnosis of MM and onset of a novel mass/lesion even at unusual sites.
1. Introduction
Malignant melanoma (MM) is a malignant tumor with an incidence exponentially rising worldwide in the Western and Caucasian populations [1,2]. It is now considered the fifth most common malignancy among men and the sixth among women in the United States [2]. It is generally accepted that this neoplasm originates in melanocytes located at the basal layer of the epidermis [1] in the uveal tract [3], and in the mucosa of the upper respiratory, genitourinary and gastrointestinal tracts. Although many advances have been made in the early diagnosis of this disease, especially if localized on the skin, and the majority of patients exhibit “thin” melanomas and skin-confined disease at the diagnosis, some patients still develop metastases, and, in a smaller portion of them, the disease can arise directly at the metastatic stage [1,2]. Although metastatic MM is known to be able to potentially involve any organ, it most commonly metastasizes to the regional lymph nodes, liver, lung and brain [4]. While cutaneous MM is often clinically evident and may be detected using noninvasive methods, such as dermoscopy or reflectance confocal microscopy, followed by an excisional biopsy with histological examination [5,6,7,8], melanoma metastases are frequently clinically occult and tend to exhibit an asymptomatic course. The metastatic involvement of gallbladder and uterus from cutaneous MM is an unusual finding, generally associated with diffuse metastatic disease or observed during autopsy [9,10].
In this paper, we report two cases of isolated melanoma metastasis located in the gallbladder (case no. 1) and endometrium (case no. 2), respectively.
2. Materials and Methods
Written informed consent was obtained from both patients involved in the study. Tissue samples were fixed in formalin, embedded in paraffin, and stained with hematoxylin and eosin (H&E). Both cases were immunohistochemically tested for anti-S100, Melan-A, HMB45, vimentin, pancytokeratins, LCA, and SOX10 antibodies.
3. Results
3.1. Case no. 1
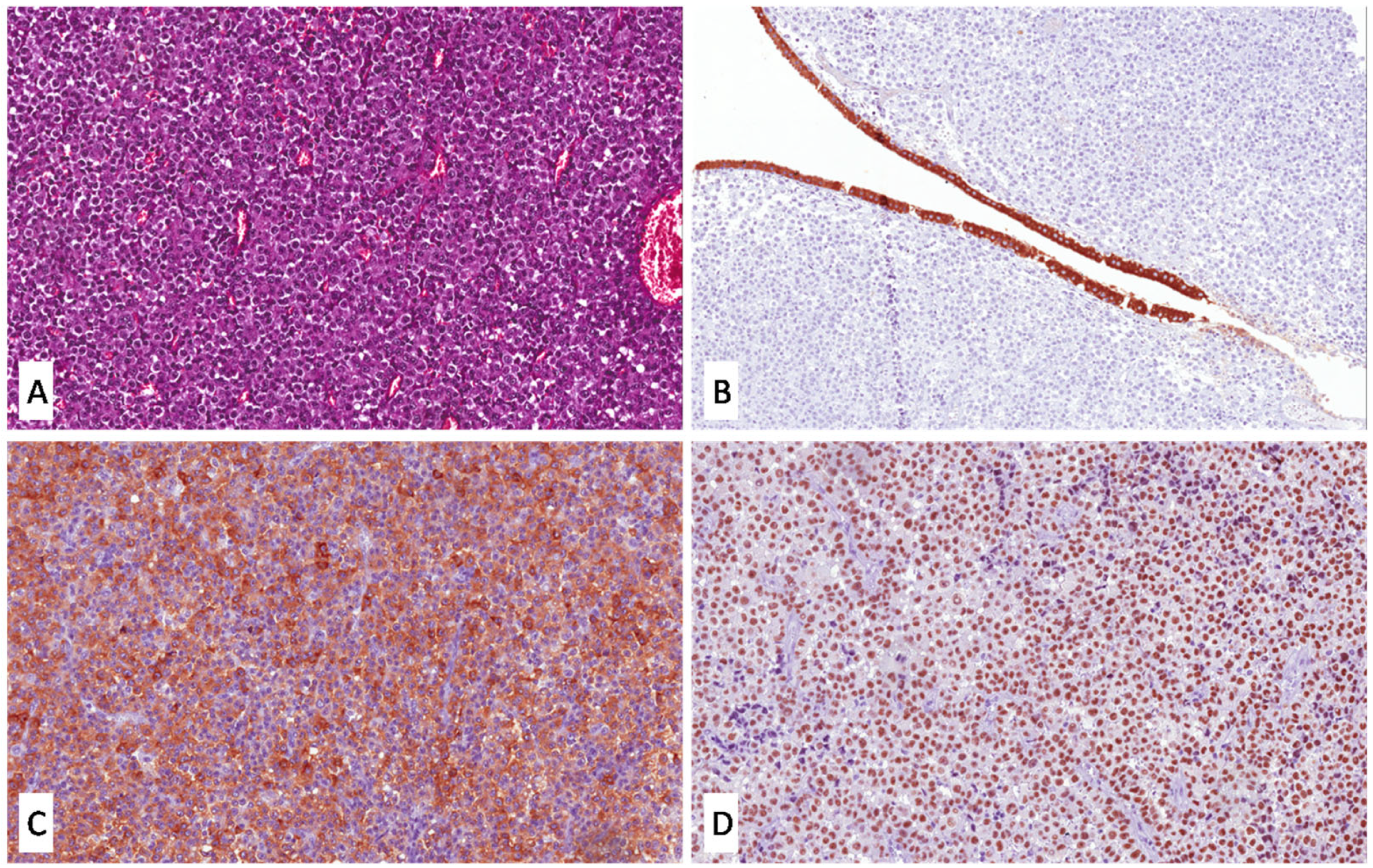
A 71-year-old man was admitted to the hospital with a complaint of upper right abdomen pain. Ultrasound showed gallbladder enlargement and a hypoechoic polypoid lesion located in the fundus. Cholecystectomy was performed. Grossly, the gallbladder exhibited a polypoid lesion of the fundus measuring cm 2.3 in its greatest diameter. Histological examination showed a hypercellular neoplasm exhibiting epithelioid cell morphology (Figure 1A), located at the gallbladder submucosa (Figure 1B) and focally eroding the upper mucosa. The neoplastic cells were large polygonally shaped cells with moderately eosinophilic cytoplasm, hyperchromatic and irregular nuclei, and prominent nucleoli. No melanic pigment was observed.
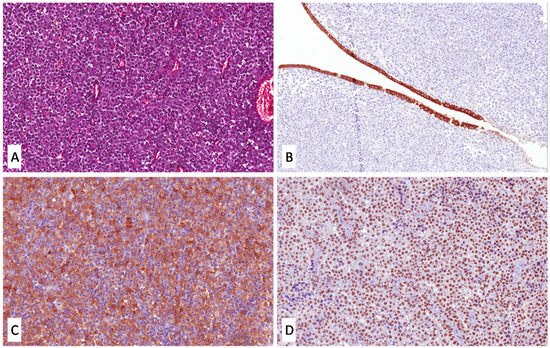
Figure 1.
(A) High magnification shows a hypercellular and slightly pigmented tumor composed of epithelioid cells with large polygonal eosinophilic cytoplasm and vesicular nuclei with prominent nucleoli (H&E; original magnification 200×); (B) a thin flap of overlying atrophic gallbladder mucosa, immunoreactive for pancytokeratins, compressed by the tumor, is seen (immunoperoxidase; original magnification 200×); (C,D) neoplastic cells are diffusely and strongly positive for Melan-A (C) and SOX10 (D) (immunoperoxidase; original magnifications 200×).
The neoplastic cells were diffusely and strongly stained with vimentin, s100, Melan-A (Figure 1C), HBM45, and SOX10 (Figure 1D), while no immunostaining was observed for pancytokeratins and LCA.
The morphological and immunohistochemical features of the tumor were consistent with a diagnosis of metastatic melanoma with epithelioid cell morphology of the gallbladder. While no anamnestic information was known at the time of the histological examination, from discussion with the clinicians we learned that the patient had undergone a previous cutaneous excision with a diagnosis of MM in the right axillary region approximately 15 years earlier. Only the pathology report of the previous MM was available, which exhibited the same epithelioid morphology and lacked both ulceration and regression (Breslow thickness: mm 0.8; Clark level 3). BRAF molecular tests were performed on paraffin tissue samples from the metastatic tumor, and BRAFV600K (1799GT>AA) mutation was found. Unfortunately, no additional patient follow-up and treatment data were available.
3.2. Case no. 2
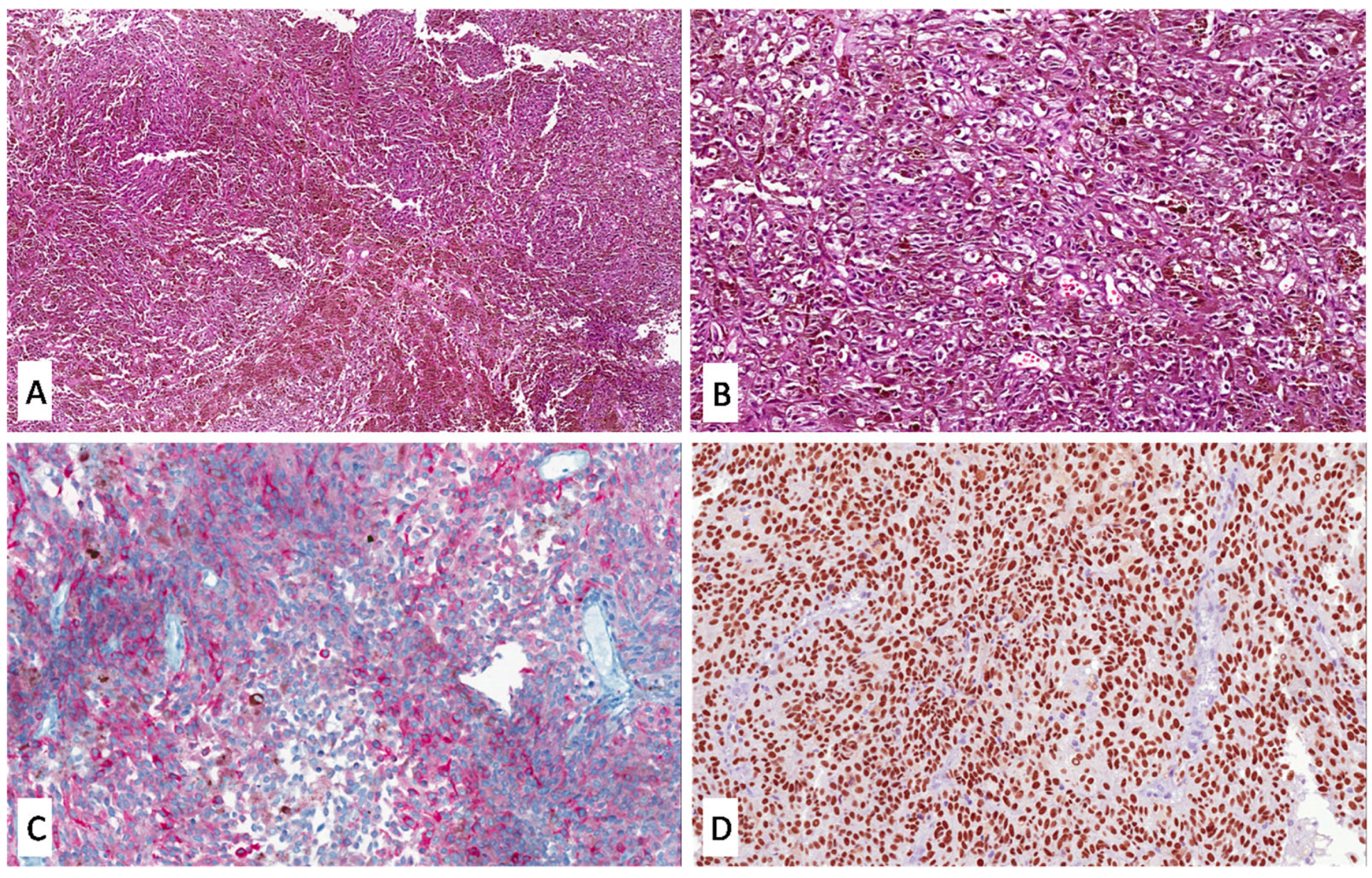
A 54-year-old woman was admitted by a private gynecologist with a complaint of spotting and uterine bleeding not associated with menstruation. Hysteroscopy showed focal endometrium thickening and an intraluminal polypoid lesion of the posterior uterine wall, measuring approximately 1.5 cm in its greatest dimension. A biopsy was performed and submitted for histological examination.
Histologically, a uniformly hypercellular and heavily pigmented malignant tumor was found (Figure 2A). The majority of the lesion was composed of epithelioid cells with large eosinophilic cytoplasm, hyperchromatic nuclei, and prominent nucleoli (Figure 2B). A smaller part of the tumor exhibited spindle cell morphology consisting of elongated cells with eosinophilic cytoplasm and oval nuclei. Neither an endometrial gland nor cytogenous stroma were found. The neoplastic cells were immunoreactive for vimentin, S100, HMB45, Melan-A (Figure 2C), and SOX10 (Figure 2D), while they were consistently negative for pancytokeratins and LCA. Based on both morphological and immunohistochemical features, a diagnosis of metastasis of melanoma with mixed epithelioid and spindled morphology was rendered. As in the previous case, no history of previous malignancies was known when the histological examination was performed and, subsequently, from discussions with the clinicians we learned that the patient had a history of MM of the heel diagnosed in 2018. Unfortunately, neither histological slides nor a pathological report of the primary tumor nor follow-up data were available in this case.
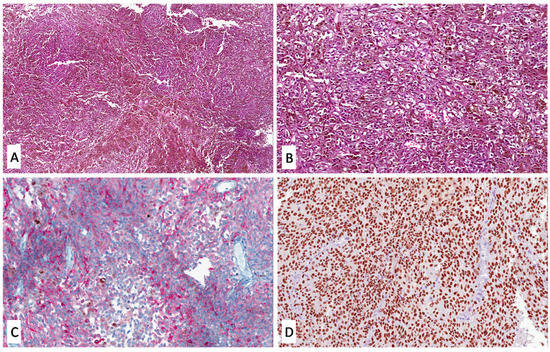
Figure 2.
(A) Low magnification showing a uniformly hypercellular and heavily pigmented tumor (H&E; original magnification 50×); (B) most of the lesion is composed of pigmented epithelioid cells with large eosinophilic cytoplasm and hyperchromatic nuclei (H&E; original magnification 200×); (C,D) tumor cells exhibit heterogeneous, strong and diffuse immunoreactivity for Melan-A (C) and SOX10 (D), respectively (immunoperoxidase; original magnifications 200×).
4. Discussion
Gastrointestinal metastases from malignant melanoma are most commonly located in the small bowel (35–65%), colon and rectum (5–9%), and stomach (5–7%) [9,10]. Isolated gallbladder metastasis from malignant melanoma is exceptionally rare. Gallbladder metastasis may be clinically asymptomatic or present as acute cholecystitis, and is often diagnosed after cholecystectomy or abdominal ultrasound performed for other reasons, accordingly [9,10]. Apparently, due to their asymptomatic course, we are not aware of the real prevalence of gallbladder metastases: autopsy reports show that the prevalence of gallbladder metastases ranges between 15 and 20%, with melanoma alone as the most common metastatic malignancy of the gallbladder (50–67%) [4,11]. Instead, primary malignant melanoma of the gallbladder is extremely rare, with only a few case reports published in the literature [12], being a diagnosis of exclusion when no prior diagnosis of melanoma has been identified. In 1999, some clinicians reported 19 cases of melanoma of the gallbladder registered since 1970, with only 3 of them being isolated metastasis of gallbladder [13]. Since then, quite a few cases have been reported in the literature [4,9,11,13,14,15,16,17,18,19,20,21,22]. Most of them report the same macroscopic and clinical evidence that we encountered in our patient: a polypoid lesion of the mucosa in a patient with acute cholecystitis-like symptoms. The clinical and histopathological differential diagnosis between primary gallbladder and metastatic melanoma can be challenging. Some colleagues [23,24] reported that mucosal and metastatic melanomas have remarkable similarities in terms of pathological findings, size, number and location of lesions, and the presence of extrabiliary lesions. Certainly, the history of primary melanoma located on the skin or at other most commonly affected anatomic sites allows us to suspect the metastatic nature of the lesion. Although, according to some authors, the absence of junctional activity (i.e., the intraepithelial extension to the mucosa overlying the tumor) better fits the diagnosis of metastatic rather than primary disease [25], other clinicians have also described junctional activity in cases of metastatic involvement of the gallbladder, not considering this criterion sufficient to distinguish between primary and metastatic melanoma [26]. The following clinico-pathological criteria have been reported as useful for distinguishing primary gallbladder melanoma from metastatic involvement: (i) the exclusion of previous primary melanoma, (ii) the absence of synchronous involvement of multiple sites, (iii) the presence of a solitary lesion, (iv) its polypoid or papillary shape, and (v) the presence of a junctional melanocytic component. Among these criteria, the first one seems to have more impact on the differential diagnosis since it has been widely demonstrated that metastatic melanoma to gallbladder can have a polypoid/papillary shape (as in our case), that it can represent the only site affected, and can exhibit a junctional component [27]. Moreover, as the clinical/histological evidence of regression in cutaneous melanoma has been associated with long-term metastases, even after a decade from the diagnosis, the possibility of metastasis from a primary melanoma in complete regression must be included in the differential diagnosis of all gallbladder masses with morphology and immunohistochemical profile consistent with those of melanoma [26,28]. In our case, it would have been particularly interesting to test the primary cutaneous tumor for BRAF mutational status to investigate whether it shared the same BRAFV600K (1799GT>AA) mutation with the metastatic lesion, but the paraffin-embedded blocks were not retrievable because they belonged to another institution.
Due to the rarity of the disease, no therapeutic guidelines have yet been standardized. The role of surgery in the treatment of gallbladder metastatic melanoma remains questionable, since the majority of patients have widespread metastatic disease at the time of the diagnosis [22]. Resection of the gallbladder could be a palliative procedure to prevent further dissemination, but the question arising at present is whether it is better to perform a laparoscopic cholecystectomy (LC) or an open surgical cholecystectomy. A recent paper encourages the open surgical approach rather than the laparoscopic one, due to possible local recurrence, and for the detection of other gastrointestinal metastases, fearing the perforation of the gallbladder and intra-abdominal bile leak [22].
The localization of metastatic malignant melanoma in gynecologic organs is exceedingly rare, with the ovaries being a relatively more frequent site. [29]. Some authors have suggested that uterine involvement can be secondary to local retrograde lymphatic spread from existing ovarian metastasis [30]. Pathological studies of the anatomical distribution of metastases within the uterus revealed that they are apparently almost always found in the myometrium (96.2%), whereas the endometrium is involved in approximately one-third of cases [31]. Primary melanoma of the uterine cervix and vagina is relatively more common, accounting for only 3–7% of all cases [32]. In all reported cases of uterine metastatic malignant melanoma, the main complaint is about abnormal uterine bleeding, both in menopausal and non-menopausal women [29,30,32,33,34,35,36,37,38,39,40]. The final diagnosis is often problematic, as the wide spectrum of histological appearances of metastatic melanoma, especially when presenting as unpigmented tumor cells, and due to the polypoid morphology often mimicking a primary endometrial lesion [32,33,34,35,36,37,38,39,40]. Metastatic melanoma of the endometrium generally shows a poor prognosis, with most women having extensive system metastatic disease at the time of diagnosis [32,33,34,35,36,37,38,39,40]. However, for those with metastatic melanoma confined to the uterine corpus and no evidence of other metastatic disease, the prognosis was considerably improved [32,33,34,35,36,37,38,39]. Ulmer et al. described a case with the same site of the primary tumor (heel) as in our case [29]. The diagnosis of acral melanoma for this patient was dated 6 years prior to the discovery of the metastasis, with optimal clinical surveillance following the excision. The main complaint was postmenopausal vaginal bleeding, and hysteroscopy revealed a polypoid lesion with irregular color and appearance [29]. Acral melanoma is a rare (4–7%) melanoma subtype associated with a poor outcome, probably due to the delayed diagnosis and its more aggressive biological behavior. Other cases described in the literature reported previous diagnoses of cutaneous melanoma dated approximately 5–6 years before the discovery of the endometrial metastasis, emphasizing that a thorough anamnesis and clinical examination are crucial.
Patients who had metastatic disease confined to the uterus and who underwent a total abdominal hysteroscopy and bilateral salpingo-oophorectomy had a significantly good prognosis [32,33,34,35,36,37,38,39,40]. It should be kept in mind that abnormal uterine bleeding may be the first sign of metastatic disease in a woman with a history of malignant disease, as in our case, since the endometrium localization is very rare and clinically evident, while the myometrium localization is more common but asymptomatic.
As it is a potentially metastasizing tumor, when dealing with cutaneous MM, pathologists must include in the pathologic report some prognostic and predictive information of survival and metastatic risk [1], including Breslow thickness, Clark levels, dermal mitoses, the presence/absence of microscopic tumor satellitosis, the presence/absence of ulceration and the presence/absence of regression: (i) Breslow thickness represents the most important prognostic factor of cutaneous MM, and is measured from the granular layer of the epidermis to the deepest dermal neoplastic cells. If ulceration is present, the measurement must be made starting from the base of the ulcer; TNM pathological staging of cutaneous MM is based on Breslow thickness and the presence/absence of ulceration. Thicker MMs are predictive of lower survival rates and high metastatic risk. (ii) Clark levels are a description of which skin layers are involved by MM: epidermis (Clark level I), papillary dermis (Clark level II), papillary/reticular dermis interface (Clark level III), reticular dermis (Clark level IV) and subcutaneous fatty tissue (Clark level V). (iii) Dermal mitoses represent the number of mitoses per mm2 found in the dermal tumor component. While the 8th Edition of TNM staging removed them as a pathological stage T1 category criterion, they remain a well-established and reproducible criterion of malignancy, especially in diagnostically challenging lesions. (iv) The definition of microscopic satellitosis is “at least one discontinuous nest of tumor cells > 0.05 mm in greatest dimension, that is distant from the main invasive MM portion at least 0.3 mm with the interposition of unaffected dermis. (v) Regression is defined as the partial or complete replacement of the tumor with fibrovascular tissue, often admixed with melanin-laden histiocytes, and lymphocytic and plasma cell inflammation [41,42].
Due to the epithelioid morphology and the absence of pigmentation of the neoplastic cells, in case no. 1, the pathological differential diagnosis also included undifferentiated metastatic carcinoma and diffuse large B-cell lymphoma/anaplastic large cell lymphoma, which were excluded by the lack of immunostaining for pancytokeratins and LCA, respectively. Conversely, the histologic diagnosis of case no. 2 was more straightforward, as the presence of diffuse pigmentation strongly favored the hypothesis of metastatic MM that was promptly confirmed by immunohistochemistry. In this regard, we would like to emphasize that pathologists must be aware of the possibility of metastatic MM, even at unusual locations, especially when dealing with apparently poorly differentiated neoplasms with epithelioid/spindled morphology and prominent nucleoli, and that MM markers such as S100, Melan-A, HMB45, and SOX10 must be always included in the immunohistochemical panel in this diagnostic context.
In the past decade, metastatic melanoma treatment could rely on targeted therapy with BRAF and MEK inhibitors [43]. BRAF V600E mutation is found in almost half of advanced (unresectable or metastatic) melanomas. As discordances in BRAF mutational status between primary and metastatic lesions are known to be relatively rare [43,44], the common practice is to rely on the BRAF status of the primary tumor, while it is advisable to also test the metastatic lesion only in those patients with no mutation found in the primary neoplasm [44]. Immunohistochemistry (IHC) may be performed as the first mutation screening method, but it is increasingly less used, as molecular analyses are mandatory both to confirm the immunohistochemical results and to detect the V600K- and V600R-mutant cases, not identifiable by IHC, that are candidates for vemurafenib therapy [44]. The first-line systemic treatment for patients with unresectable or metastatic disease includes monotherapy protocols with pembrolizumab or nivolumab (anti-PD1) or a combination protocol with nivolumab associated with ipilimumab (anti-CTLA4).
5. Conclusions
Metastatic MM is one of the most aggressive malignant neoplasms due to its aggressive course and poor prognosis. We have presented these cases in order to emphasize that MM metastasis must be taken into account in the differential diagnosis when dealing with patients with a known history of cutaneous MM and an onset of a novel mass/lesion even at unusual sites. Metastatic MM of the gallbladder and endometrium is considered an exceedingly rare event, whose diagnosis is often challenging because most cases are asymptomatic and/or may mimic benign diseases or primary malignancies due to their nonspecific gross features.
Author Contributions
Conceptualization, G.B. and J.F.; resources, A.P., F.S., M.Z., G.Z. and R.M.; writing—original draft preparation, G.B. and J.F.; writing—review and editing, G.B. and R.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study due to the retrospective description of few cases without identifiable patient data.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
All data presented in this study are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Abbas, O.; Miller, D.D.; Bhawan, J. Cutaneous malignant melanoma: Update on diagnostic and prognostic biomarkers. Am. J. Dermatopathol. 2014, 36, 363–379. [Google Scholar] [CrossRef]
- Pavri, S.N.; Clune, J.; Ariyan, S.; Narayan, D. Malignant Melanoma: Beyond the Basics. Plast. Reconstr. Surg. 2016, 138, 330e–340e. [Google Scholar] [CrossRef] [PubMed]
- Foti, P.V.; Travali, M.; Farina, R.; Palmucci, S.; Spatola, C.; Raffaele, L.; Salamone, V.; Caltabiano, R.; Broggi, G.; Puzzo, L.; et al. Diagnostic methods and therapeutic options of uveal melanoma with emphasis on MR imaging-Part I: MR imaging with pathologic correlation and technical considerations. Insights Imaging 2021, 12, 66. [Google Scholar] [CrossRef]
- Khan, A.; Patel, S.; Zaccarini, D.J.; McGrath, M. Metastatic Melanoma of the Gallbladder in an Asymptomatic Patient. Case Rep. Gastrointest. Med. 2017, 2017, 1767418. [Google Scholar] [CrossRef]
- Bolcato, V.; Michelerio, A. Dermoscopy for Cutaneous Melanoma: Under the Eye of Both the Dermatologist and the Legal Doctor. Dermatol. Pract. Concept 2022, 12, e2022100. [Google Scholar] [CrossRef]
- De Pascalis, A.; Perrot, J.L.; Tognetti, L.; Rubegni, P.; Cinotti, E. Review of Dermoscopy and Reflectance Confocal Microscopy Features of the Mucosal Melanoma. Diagnostics 2021, 11, 91. [Google Scholar] [CrossRef]
- Verzì, A.E.; Lacarrubba, F.; Caltabiano, R.; Broggi, G.; Musumeci, M.L.; Micali, G. Reflectance Confocal Microscopy Features of Plaque Psoriasis Overlap With Horizontal Histopathological Sections: A Case Series. Am. J. Dermatopathol. 2019, 41, 355–357. [Google Scholar] [CrossRef]
- Lacarrubba, F.; Verzì, A.E.; Caltabiano, R.; Broggi, G.; Di Natale, A.; Micali, G. Discoid lupus erythematosus: Reflectance confocal microscopy features correlate with horizontal histopathological sections. Skin Res. Technol. 2019, 25, 242–244. [Google Scholar] [CrossRef] [PubMed]
- D’Urso Vilar, G.G.; Iriarte, F.; Speisky, D.; Bregante, M.L.; Quildrian, S.D. Isolated Gallbladder Metastasis of Melanoma: Case Report. Int. J. Surg. Case Rep. 2020, 71, 311–314. [Google Scholar] [CrossRef] [PubMed]
- Haskaraca, M.F.; Ozsoy, M.; Ozsan, I.; Kurt, K. Primary malignant melanoma of the gallbladder: A case report and review of the literature. Case Rep. Surg. 2012, 2012, 693547. [Google Scholar] [CrossRef]
- Saraswat, N.B.; DeVoe, W.B. Metastatic Melanoma of the Gallbladder Presenting as Polyp in Acute Cholecystitis. J. Surg. Case Rep. 2019, 2019, rjz324. [Google Scholar] [CrossRef]
- Wang, J.K.; Su, F.; Ma, W.J.; Hu, H.J.; Yang, Q.; Liu, F.; Li, Q.S.; Li, F.Y. Primary Malignant Melanoma of the Gallbladder with Multiple Metastases: A Case Report. Medicine 2017, 96, e8793. [Google Scholar] [CrossRef]
- Dong, X.D.; DeMatos, P.; Prieto, V.G.; Seigler, H.F. Melanoma of the gallbladder: A review of cases seen at Duke University Medical Center. Cancer 1999, 85, 32–39. [Google Scholar] [CrossRef]
- Tauziède-Espariat, A.; Raffoul, J.; Sun, S.R.; Monnin, C.; de la Fouchardière, A.; Lassabe, C. Métastase vésiculaire d’un mélanome: Données immunohistochimiques et moléculaires d’un cas et revue de la littérature [Gallbladder Metastasis of Melanoma: Immunohistochemical and Molecular Data of a Case and Review of the Literature]. Ann. Pathol. 2017, 37, 484–487. [Google Scholar] [CrossRef]
- Strick, A.; Busch, H.; Friedhoff, K. Gallenblasenmetastase eines malignen Melanoms [Gallbladder Metastasis of a Malignant Melanoma]. Dtsch. Med. Wochenschr. 2022, 147, 1277–1280. [Google Scholar] [CrossRef]
- Doole, E.L.; Gan, P.; Klein, O. A Rare Case of Solitary Gallbladder Metastasis from an Early Cutaneous Melanoma. Clin. Case Rep. 2021, 9, e04908. [Google Scholar] [CrossRef]
- Hess, G.F.; Glatz, K.; Rothschild, S.I.; Kollmar, O.; Soysal, S.D.; Boll, D.T.; Droeser, R.A.; Mechera, R. Malignant Melanoma Metastasis in the Gallbladder. A Case Report of an Unusual Metastatic Site. Int. J. Surg. Case Rep. 2020, 75, 372–375. [Google Scholar] [CrossRef]
- Di Buono, G.; Maienza, E.; Rinaldi, G.; Buscemi, S.; Romano, G.; Agrusa, A. Malignant Metastatic Melanoma to the Gallbladder: Report of a Peculiar Case. Int. J. Surg. Case Rep. 2020, 77, S37–S39. [Google Scholar] [CrossRef]
- Addeo, P.; Onea, A.; Scrivener, J.N.; Bachellier, P. Gallbladder Metastasis from Melanoma. Dig. Liver Dis. 2020, 52, 679–680. [Google Scholar] [CrossRef]
- Riva, G.; Villanova, M.; Eccher, A.; Luchini, C.; Motta, F.; Bernasconi, R.; Barbareschi, M. Metastatic malignant melanoma to the gallbladder. Case report and review of the literature. Pathologica 2018, 110, 68–71. [Google Scholar]
- Würtz, H.J.; Detlefsen, S.; Ainsworth, A.P. Metastasis from a malignant melanoma presenting as a gall bladder polyp. Ugeskr. Laeger. 2018, 180, V01180034. [Google Scholar] [PubMed]
- Giannini, I.; Cutrignelli, D.A.; Resta, L.; Gentile, A.; Vincenti, L. Metastatic Melanoma of the Gallbladder: Report of Two Cases and a Review of the Literature. Clin. Exp. Med. 2016, 16, 295–300. [Google Scholar] [CrossRef] [PubMed]
- McFadden, P.M.; Krementz, E.T.; McKinnon, W.M.; Pararo, L.L.; Ryan, R.F. Metastatic melanoma of the gallbladder. Cancer 1979, 44, 1802–1808. [Google Scholar] [CrossRef] [PubMed]
- Murphy, M.N.; Lorimer, S.M.; Glennon, P.E. Metastatic melanoma of the gallbladder: A case report and review of the literature. J. Surg. Oncol. 1987, 34, 68–72. [Google Scholar] [CrossRef] [PubMed]
- Marone, U.; Caracò, C.; Losito, S.; Daponte, A.; Chiofalo, M.G.; Mori, S.; Cerra, R.; Pezzullo, L.; Mozzillo, N. Laparoscopic cholecystectomy for melanoma metastatic to the gallbladder: Is it an adequate surgical procedure? Report of a case and review of the literature. World J. Surg. Oncol. 2007, 5, 141. [Google Scholar] [CrossRef]
- Guida, M.; Cramarossa, A.; Gentile, A.; Benvestito, S.; De Fazio, M.; Sanbiasi, D.; Crucitta, E.; De Lena, M. Metastatic malignant melanoma of the gallbladder: A case report and review of the literature. Melanoma Res. 2002, 12, 619–625. [Google Scholar] [CrossRef]
- Ricci, R.; Maggiano, N.; Martini, M.; Mulé, A.M.; Pierconti, F.; Capelli, A.; Larocca, L.M. Primary malignant melanoma of the gallbladder in dysplastic naevus syndrome. Virchows. Arch. 2001, 438, 159–165. [Google Scholar] [CrossRef]
- Langley, R.G.; Bailey, E.M.; Sober, A.J. Acute cholecystitis from metastatic melanoma to the gall-bladder in a patient with a low-risk melanoma. Br. J. Dermatol. 1997, 136, 279–282. [Google Scholar]
- Ulmer, K.; Powers, J.; Alrwashdeh, A.; Hardy-Fairbanks, A. Metastatic malignant melanoma in an endometrial polyp. Dermatol. Online J. 2021, 27, 11. [Google Scholar] [CrossRef]
- Fambrini, M.; Andersson, K.L.; Buccoliero, A.M.; Pieralli, A.; Livi, L.; Marchionni, M. Late Solitary Metastasis of Cutaneous Malignant Melanoma Presenting as Abnormal Uterine Bleeding. J. Obstet. Gynaecol. Res. 2008, 34 Pt 2, 731–734. [Google Scholar] [CrossRef]
- Kumar, N.B.; Hart, W.R. Metastases to the uterine corpus from extragenital cancers. A clinicopathologic study of 63 cases. Cancer 1982, 50, 2163–2169. [Google Scholar] [CrossRef] [PubMed]
- Casey, J.H.; Shapiro, R.F. Metastatic melanoma presenting as primary uterine neoplasm: A case report. Cancer 1974, 33, 729–731. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, M.C.; Shoushtari, A.; Leitao, M.M.; Chui, M.H.; Al-Ahmadie, H.; Petkovska, I. Metastatic Melanoma Concurrent to the Urinary Bladder and Endometrium: Case Report. J. Med. Imaging Radiat. Oncol. 2022, 66, 643–646. [Google Scholar] [CrossRef] [PubMed]
- Song, H.S.; Kim, M.H.; Lee, M.Y.; Jeon, S.J.; Kim, H.S.; Kim, Y.A.; Chun, K.C. Cutaneous Malignant Melanoma Metastatic to Endometrium Manifesting Abnormal Uterine Bleeding in Postmenopausal Woman: A Case Report. J. Obstet. Gynaecol. 2019, 39, 1184–1185. [Google Scholar] [CrossRef]
- Little, J.; Braniff, K. Endometrial Metastasis of Primary Malignant Melanoma of the Brain. BMJ Case Rep. 2018, 2018, bcr2018224435. [Google Scholar] [CrossRef] [PubMed]
- Korolev, A.A.; Golubev, O.A. A rare variant of malignant melanoma progression. Arkh. Patol. 2006, 68, 42. [Google Scholar]
- Berker, B.; Sertcelik, A.; Kaygusuz, G.; Unlu, C.; Ortac, F. Abnormal Uterine Bleeding as a Presenting Sign of Metastasis to the Endometrium in a Patient with a History of Cutaneous Malignant Melanoma. Gynecol. Oncol. 2004, 93, 252–256. [Google Scholar] [CrossRef]
- Heinig, J.; August, C.; Beckmann, V.; Konieczny, A. Endometrial Metastasis of Cutaneous Melanoma—A Case-Report Bearing Diagnostic Difficulties. Zentralbl. Gynakol. 2001, 123, 534–535. [Google Scholar] [CrossRef]
- August, C.; Baba, H.A.; Heinig, J.; Nashan, D.; Höhn, P.; Holzhausen, H.J.; Metze, D.; Böcker, W. Endometrial metastasiertes “Balloon”-Zell-Melanom unter dem Bild einer “xanthomatösen Endometritis” [Endometrial Metastasis of a “Balloon” Cell Melanoma Mimicking a “Xanthomatous Endometritis”]. Pathologe 2001, 22, 145–150. [Google Scholar] [CrossRef]
- Simeone, S.; Laterza, M.M.; Scaravilli, G.; Capuano, S.; Serao, M.; Orabona, P.; Rossi, R.; Balbi, C. Malignant melanoma metastasizing to the uterus in a patient with atypical postmenopause metrorrhagia. A case report. Minerva Ginecol. 2009, 61, 77–80. [Google Scholar]
- Cartron, A.M.; Aldana, P.C.; Khachemoune, A. Reporting regression in primary cutaneous melanoma. Part 1: History, histological criteria and pathogenesis. Clin. Exp. Dermatol. 2021, 46, 28–33. [Google Scholar] [CrossRef] [PubMed]
- Cartron, A.M.; Aldana, P.C.; Khachemoune, A. Reporting regression in primary cutaneous melanoma. Part 2: Prognosis, evaluation and management. Clin. Exp. Dermatol. 2020, 45, 818–823. [Google Scholar] [CrossRef] [PubMed]
- Cheng, L.; Lopez-Beltran, A.; Massari, F.; MacLennan, G.T.; Montironi, R. Molecular testing for BRAF mutations to inform melanoma treatment decisions: A move toward precision medicine. Mod. Pathol. 2018, 31, 24–38. [Google Scholar] [CrossRef] [PubMed]
- Yaman, B.; Kandiloğlu, G.; Akalin, T. BRAF-V600 Mutation Heterogeneity in Primary and Metastatic Melanoma: A Study With Pyrosequencing and Immunohistochemistry. Am. J. Dermatopathol. 2016, 38, 113–120. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).