Abstract
Background: Small-field dosimetry remains an open challenge globally. Thus, it is crucial to consider adequate reference codes of practice for the performance of dosimetry. Furthermore, as part of good clinical practice, the implementation of new codes of practice implies the development of a dosimetry audit program. In this work, a pilot dosimetric audit protocol is established for measuring the absolute dose in water for small fields using micro-TLDs LiF:Mg,Ti dosimeters. Methods: The dosimeters were irradiated with a 6 MV X-ray beam in a linear accelerator. The TLDs were calibrated between 0.5 and 3 Gy for different field sizes. For audit, the TLDs were irradiated at 2 Gy for different circular field sizes. The proposed protocol consists of five TLD dosimeters forming a cross with a marked radiochromic film to identify the position of the central dosimeter during irradiation. Only the dosimeter measurement in the center of the field is used. Results: It was found that the percentage difference between the measured dose and the prescribed dose (2 Gy) for irradiation in circular fields is less than 3%. Conclusions: A pilot dosimetric audit was carried out using the proposed protocol over a linear accelerator using small circular collimator photon beams.
1. Introduction
Nowadays, all physics and technical problems related to the dosimetry of small radiotherapy photon beams and unconventional fields are prominently indicated in the literature [1]. These dosimetric problems are dependent on the size of the field. In the present work, a small field is understood to be one that has one or more of the following characteristics: lack of lateral equilibrium of the charged particle, partial occlusion of the primary source, and beam quality (spectral changes), and when considering the detector, its dimensions compared to the size of the beam. An unconventional field refers to a field in which Bragg Gray conditions can be established, field size of which differs from the standard field size of 10 cm × 10 cm. The above definitions are in line with those established in TRS-483 [2]. The code of practice refers to these unconventional fields as machine-specific reference fields, or “msr.”
There are well-established dosimetry protocols for conventional fields, such as IAEA-TRS-398 [3] and the AAPM-TG-51 [4]. Both protocols are based on standards of dose absorbed to water under reference conditions. It is crucial to consider that the codes of practice used in conventional fields cannot be applied in unconventional fields. The limitations of conventional codes of practice rely on the reference conditions regarding field size and irradiation geometry. Moreover, the relative dosimetry of small static fields is challenging, because the sensitive volumes of the detectors dedicated to these fields are tiny (about 15% relative to the field size); their correct spatial location is essential for achieving correct relative dosimetry. Therefore, the TRS 483 [2] code of practice provides adequate guidelines for reference dosimetry and relative dosimetry in unconventional fields and small static fields, respectively.
The challenges and dosimetric problems related to unconventional and small static fields must be considered in order to be able to perform correct dosimetry. Furthermore, as part of good clinical practice, implementing a new code of practice implies the development of a dosimetry audit program to guarantee that the beam output is within tolerance limits. Therefore, a pilot study of a clinical audit in these fields is necessary and suggested in this article. A clinical audit must be carried out by an expert external to the service to be evaluated. The objective of a comprehensive audit is to review and evaluate the quality of all of the components related to the practice of radiotherapy at an institution, including multidisciplinary professional competence; therefore, a significant part of the audit is patient-oriented (diagnosis, decision to treat, treatment prescription, planning treatment preparation, and delivery and finally follow-up process) [5]. Considering this, it is essential to consider that quality audits can be of various types and levels, ranging from partial processes (reviewing specific critical parts of the radiotherapy process) to comprehensive audits (assessing the whole process) [5,6,7,8,9,10,11,12]
This work focuses on a partial audit, specifically regarding clinical dosimetric analysis, aiming to measure the absorbed dose in water using thermoluminescent dosimeters (TLD) for a small photon beam in a linear accelerator commissioned following the recommendation of Alfonso et al. [13]. TLDs have been widely used for postal audits in conventional fields [14,15,16,17]. Unlike other micro dosimeters such as micro-diamond, TLDs are passive detectors that do not require an electrometer when irradiated; they are cheap and can be deployed in large quantities.
2. Materials and Methods
This work intended to establish a protocol for measuring the dose in water delivered by small fields using TLD-100 micro-cubes. For this work, 1 mm × 1 mm × 1 mm LiF:Mg,Ti (TLD-100) thermoluminescent dosimeters were used, commonly referred to as micro-cubes. The micro-TLDs were characterized by determining their sensitivity and reproducibility factors, as well as their calibration curves (thermoluminescent response as a function of dose), which were measured for four square fields between 0.5 cm × 0.5 cm and 10 cm × 10 cm. During the characterization of the TLDs, the reading conditions necessary to reduce the uncertainty in the measurements were established.
2.1. Commissioning of the Linear Accelerator for Small Static Fields
In this work, a Novalis® Classic linear accelerator with a photon beam with a nominal energy of 6 MV was used to irradiate the dosimeters. The linac’s beam output was measured following the recommendations of code of practice 398 [3]. A Farmer-type ionization chamber was used under the irradiation conditions suggested by TRS 398: a source-to-axis distance (SAD) of 100 cm, a field size of 10 cm × 10 cm, and a depth of 5 cm. With respect to relative dosimetry, this was was performed following the recommendations of Alfonso et al. [13] for the dosimetry of small static fields. A silicon stereotactic diode SFD (IBA-Dosimetry, Germany) and a micro-diamond detector (PTW-60019, PTW-Freiburg, Germany) were used. The measurements were performed in liquid water using an MP3-XS computerized scanning phantom (PTW-Freiburg, Germany). The corresponding output correction factors for each field size were calculated by Monte Carlo simulation to determine the field factors [18]. Finally, the photon beams were collimated using conical collimators with diameters of 4.0 at 20 mm, defined at the isocenter.
2.2. Thermoluminescences Dosimeters
This work used preselected thermoluminescent dosimeters to present micro-cubes with dimensions of 1 × 1 × 1 mm3 of LiF:Mg,Ti (TLD-100) for pilot audit assessment. The initial batch consisted of 200 dosimeters. Before developing this work’s central objective, the micro-TLDs were subjected to pre-irradiation heat treatment. The pre-irradiation consisted of high-temperature annealing to erase signals accumulated during storage and empty the electron and hole traps, and low-temperature annealing to stabilize the low-temperature peaks.
2.2.1. Dosimeter Preparation and Reading
The micro-TLDs were annealed at 400 °C for one hour, followed by rapid cooling and subsequently annealing at 100 °C for two hours before being irradiated. The reading was performed approximately 24 h after irradiation in a Harshaw 3500 reader at a heating rate of 10 °C/s ranging from room temperature to 330 °C, placing the micro-cubes as centrally as possible in the heating system and keeping the nitrogen gas flow as low as possible to avoid any movement of the micro-cube. The TLDs were marked with graphite, so the thermo-stimulated face was always the same, in order to avoid the TL response dependence for differences in the face’s flatness [19].
2.2.2. Experimental Configuration
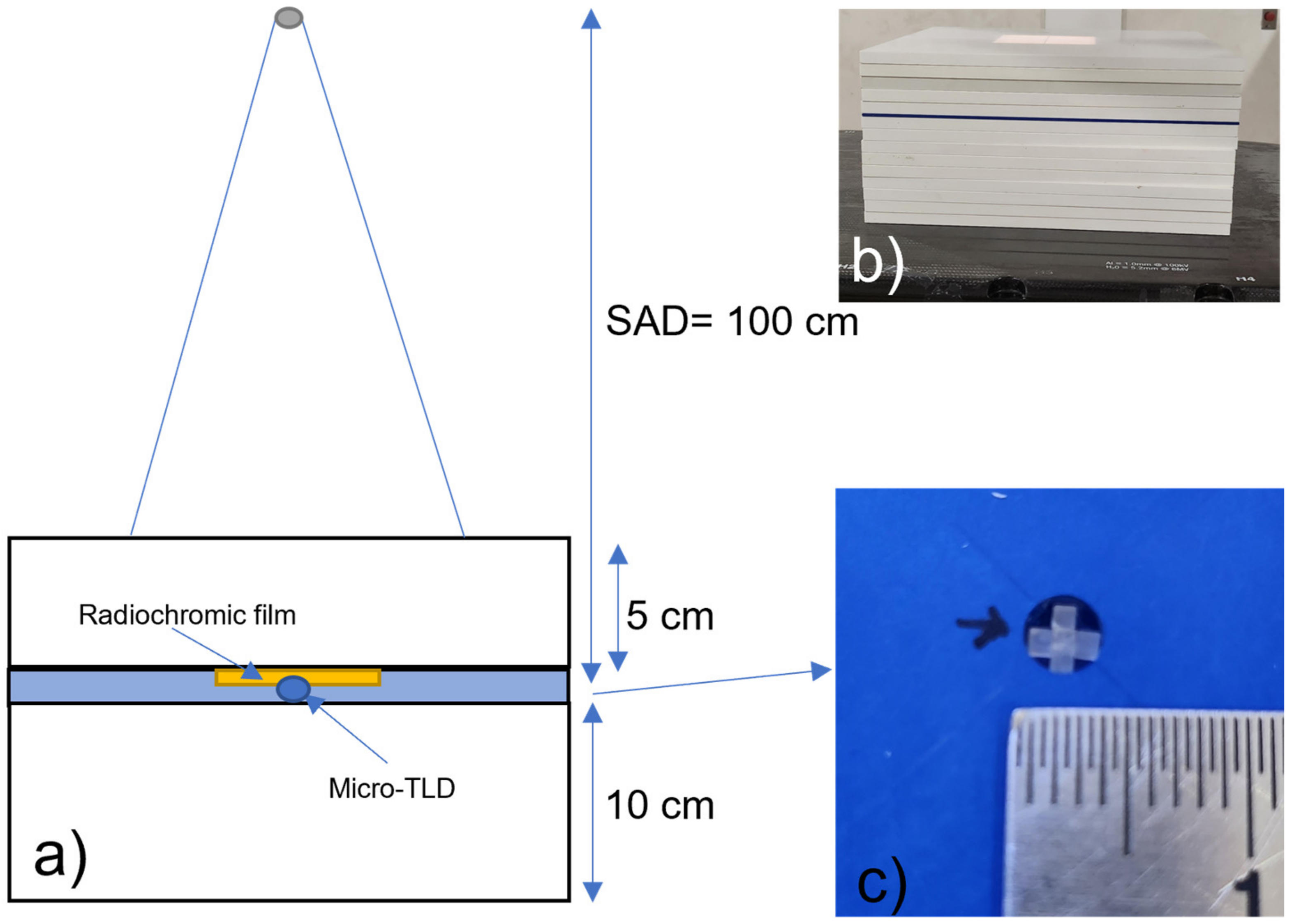
The linear accelerator was calibrated such that 1 cGy per monitor unit (MU) was delivered to a depth of 5 cm with a 10 cm × 10 cm field size and a source-to-axis distance of 100 cm. A water phantom with dimensions of 30 cm × 30 cm × 30 cm (MP3-XS, PTW-Freiburg-Germany) was used for commissioning measurements. Calibration of the TLDs was performed in a solid water phantom with dimensions of 30 cm × 30 cm × 15 cm, designed with a special niche for five micro-TLDs to be placed simultaneously for a single irradiation (Figure 1). The function of the radiochromic films (RF) was to locate the positions of the micro-TLDs relative to the central beam axis. The irradiation field sizes were defined using circular collimators that projected fields at the isocenter that had a diameter of 4.0 at 20 mm, with the jaws set to a field size of 4 cm × 4 cm. The TLD calibration and pilot audit irradiation were performed at a depth of 5 cm and a source-to-axis distance of 100 cm. A piece of radiochromic film was placed over the set of 5 TLDs.
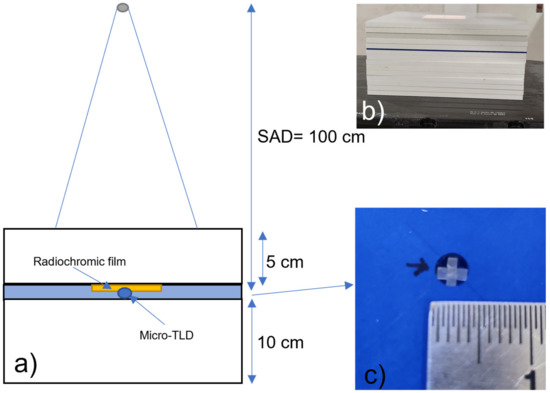
Figure 1.
(a) Experimental irradiation. (b) Solid water phantom showing the slab for micro-TLD placement in blue. (c) Top view of the dosimeters placed in the solid water phantom.
The irradiation conditions used in this work are shown in Table 1, along with the irradiation conditions and the differences between measured and prescribed doses previously reported in the literature.

Table 1.
Conditions under which dose measurement was carried out and the reported percentage differences between the measured and prescribed doses.
2.3. Characterization of TLD Micro-Cubes
2.3.1. Homogeneity and Reproducibility
The response homogeneity and the sensitivity factors of 200 dosimeters were studied in a previous work [24]. In the previous work, the batch was placed in an acrylic holder with 10 cm of acrylic and solid water on and below the sample holder, respectively. An EBT3 radiochromic film was placed between the support and the acrylic thickness to verify that the TLDs had been irradiated at the same dose. The dosimeters were irradiated four times at a dose in the water of 1 Gy, whereby data from the first three irradiations were used to obtain the sensitivity factor (Equation (1)), while those from the fourth were used to evaluate the effect of its application.
The sensitivity factor was defined as [24,25]:
where TLRaverg and TLRi are the average and individual dosimeter thermoluminescent response (TLR), respectively. The TLD response homogeneity of the dosimeters used in this work, before and after correcting for sensitivity, demonstrated a standard deviation of 5.9% and 1.3%, respectively [24].
The average and standard deviation of the individual TLR were obtained to determine the reproducibility of each dosimeter. It was shown that the TLRs presented a standard deviation of 10%. However, after reading the dosimeters by placing the same face of the TLD on the heater pan, the standard deviation of the TLR decreased to 3%. Therefore, dosimeters with a reproducibility of 5% and a sensitivity factor of 1.00 ± 0.05 were selected, thus affording a total of 180 TLDs that met both of the conditions used in the present work [24,26].
2.3.2. Thermoluminescent Response as a Function of Dose
To obtain the thermoluminescent response (TLR) as a function of dose (calibration curve), the dosimeters were separated into five groups so that each group had less than a 2% difference between the dosimeters’ sensitivity factors. Irradiations were performed for field sizes between 10 cm × 10 cm and 0.5 cm × 0.5 cm (see Table 1) at six doses between 0.5 and 3 Gy in water. In a previous work, response functions were obtained for 10 cm × 10 cm and 2 cm × 2 cm [24]. The MUs applied to obtain these doses were calculated using the output factors shown in Table 2, which were measured using a PTW-60019 CVD diamond detector (0.003 mm3 sensitive volume, 1 μm thickness, and 2.1 mm diameter). The five dosimeters were placed in a solid water phantom and irradiated, placing on them a radiochromic film (see Figure 1).

Table 2.
Output factors used to determine the calibration curve.
The average TLD responses of each group of dosimeters was recorded in nC for each field size and dose.
For the 0.5 cm × 0.5 cm field size, a discrepancy was observed between the TLRs of each group, since some were within the field penumbra, a fact that was corroborated with the films. Then, each dosimeter was irradiated individually in a solid water plate with a hole for a micro-cube in the center.
2.4. Dosimetric Audit
For the dosimetric audit, the following circular collimator diameters were used for irradiation: 4.0, 6.0, 7.5, 10.0, 12.5, 15.0, and 20.0 mm. The experimental configuration is presented in Section 2.2.2 and Table 1. For each field size, five TLD dosimeters were irradiated at the prescribed dose of 2 Gy. This is the prescribed dose commonly delivered to tumors in conventional treatment sessions. The MU necessary were determined on the basis of the output factors measured using the PTW-60019 CVD diamond detector for fields with a diameter of 12.5 to 20 mm in diameter, and 10 cm × 10 cm, and with an IBA SFD diode (sensitive volume of 0.017 mm3, thickness 60 μm, diameter 0.6 mm). Afterwards, the output correction factors corresponding to each field size were delivered for circular field sizes ranging from 10 to 4.0 mm while applying the MU shown in Table 3. The reference field was 10 cm × 10 cm.

Table 3.
Field output factors measured with diamond and SFD diodes.
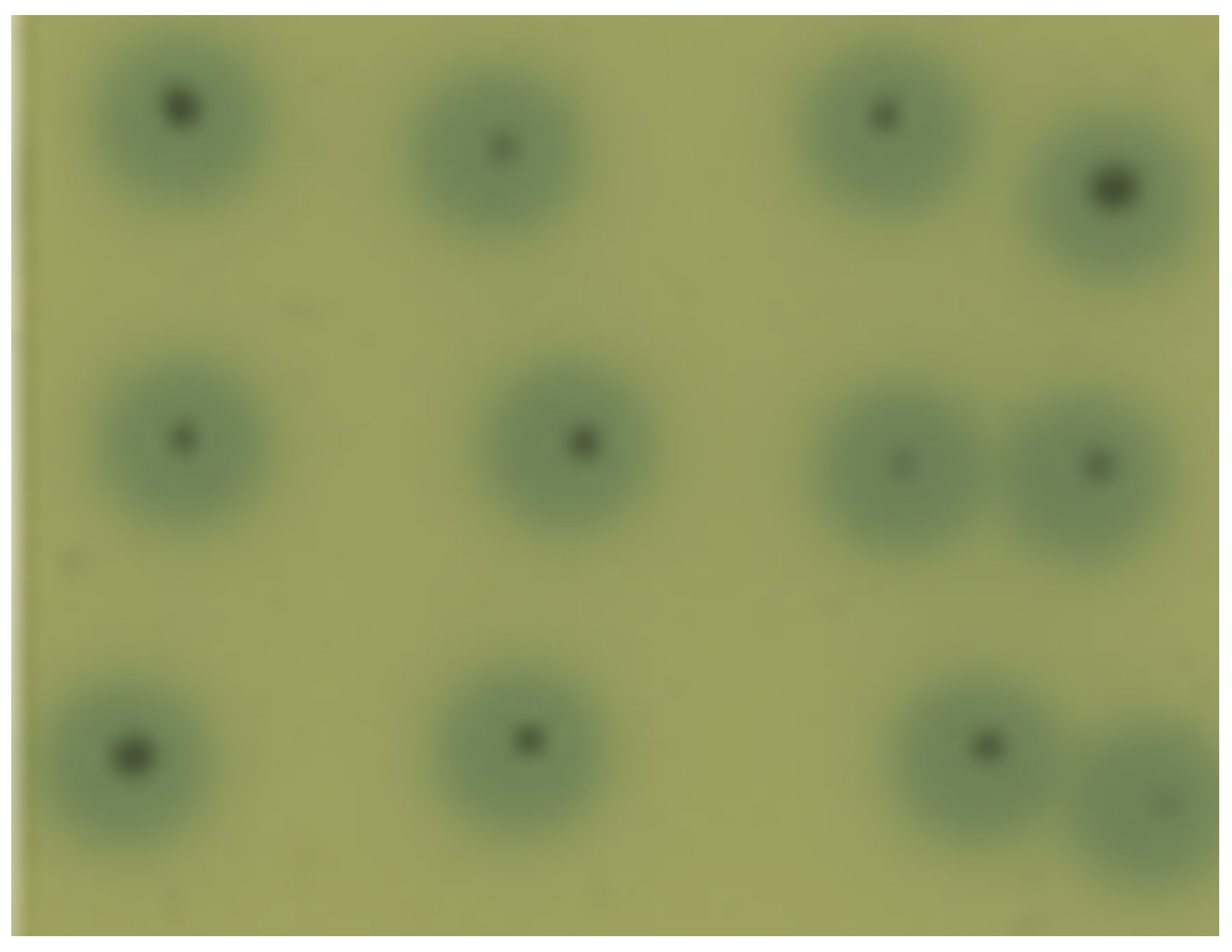
The positions of the micro-TLDs at the center of the radiation field were verified, with the film being marked (black dot) at the position of the central dosimeter (Figure 2). The 12 spots correspond to the 12 independent dosimeter irradiations for a specific field size.
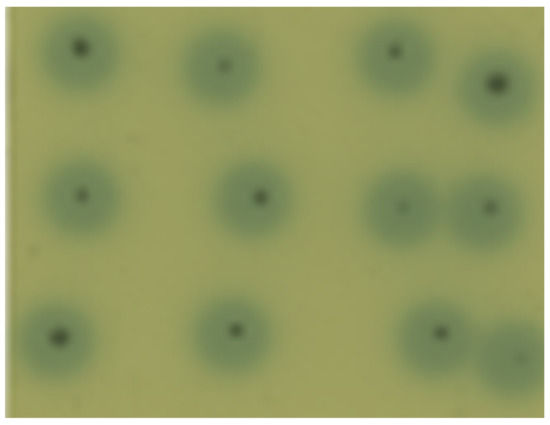
Figure 2.
Image of the RF used to verify the position of the dosimeters in the radiation field.
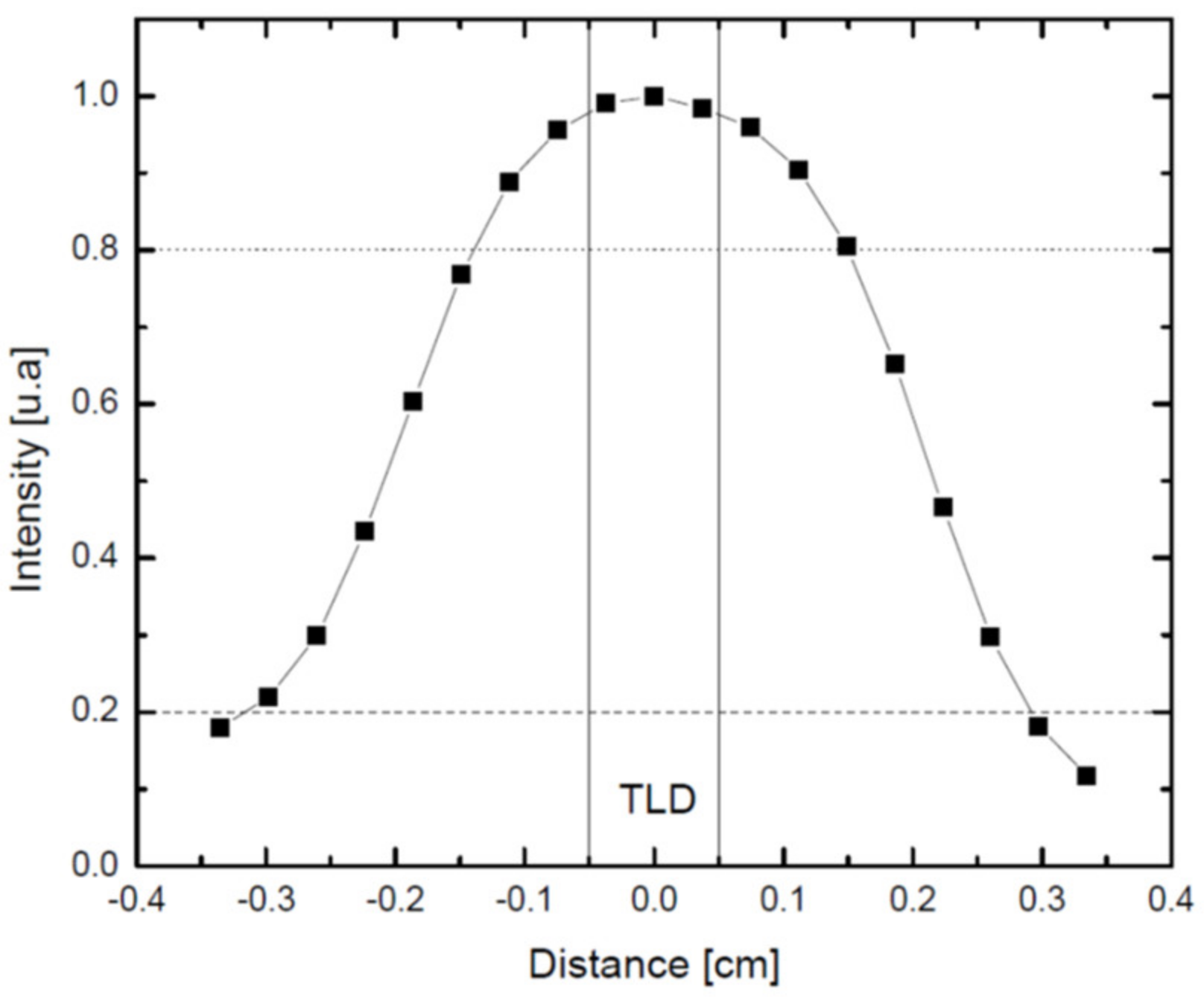
EBT3 radiochromic films were scanned to obtain the intensity profile of the irradiated area that covered the dosimeters, and the percentage standard deviation in 1 mm at the center was obtained. The profile of the field with a diameter of 4 mm is shown in Figure 3, demonstrating that in a circle with a diameter of 1 mm, the field is homogeneous to within 3%.
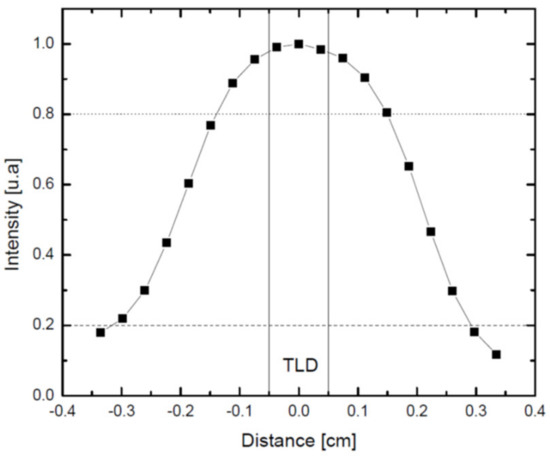
Figure 3.
Profile of a EBT3 radiochromic film irradiated with a circular field with a diameter of 4 mm. The lines represent the width of a TLD-100 micro-cube.
For each field size, 12 irradiations of five dosimeters were performed; the position of the dosimeter closest to the center of the field was determined, and its TL response was measured in order to obtain the average of the 12 measurements used to determine the dose.
3. Results
3.1. Micro-TLD Characterization: Thermoluminescent Response as a Function of Dose
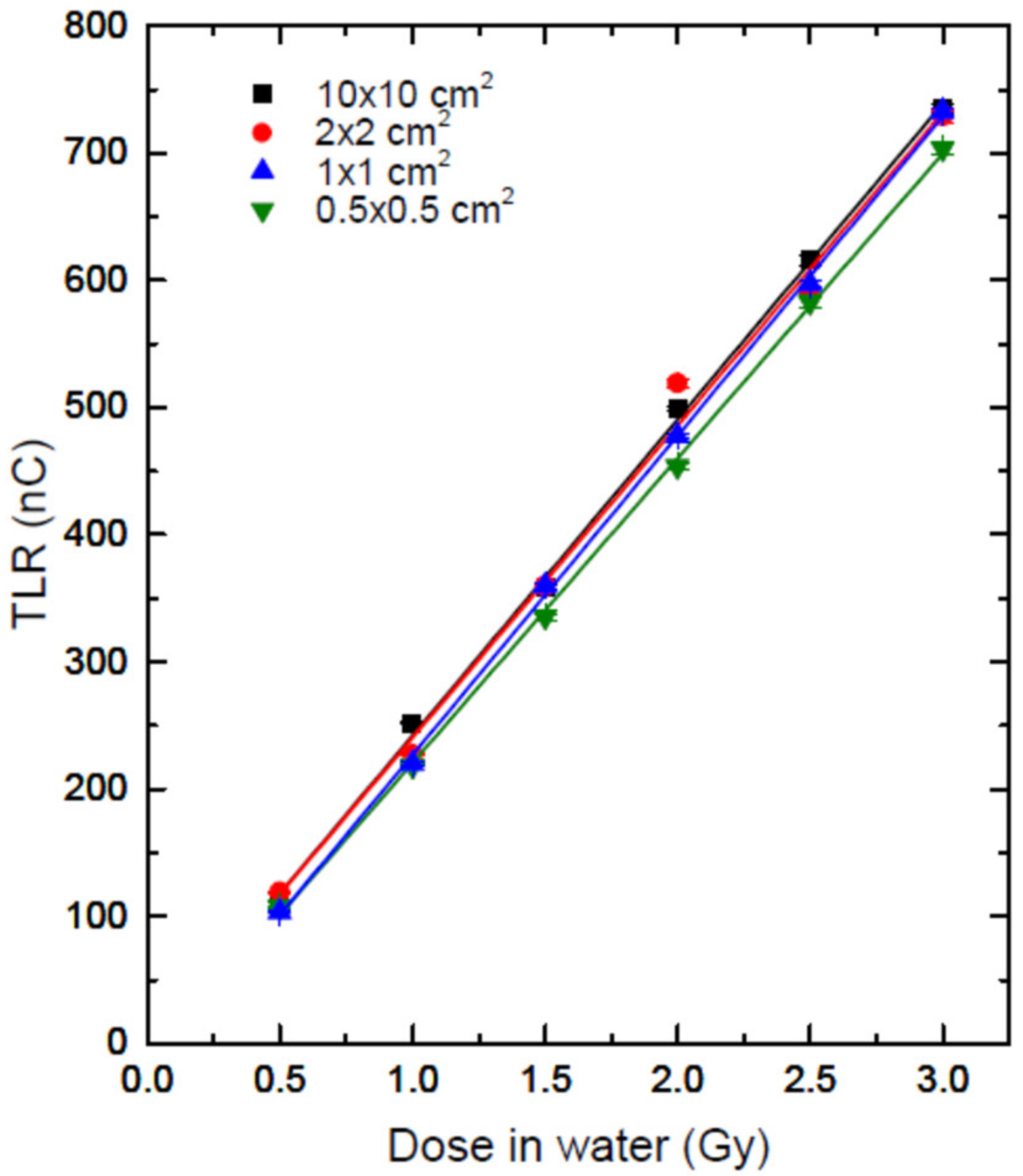
For the four radiation field sizes, the response of the dosimeters was linear within the range of doses studied. Figure 4 shows the thermoluminescent response, corrected for sensitivity, as a function of dose for all field sizes. from the data for the fields with sizes of 10 cm × 10 cm and 2 cm × 2 cm were taken from Peña-Jiménez et al. [24]. The straight lines correspond to linear fits. The values of the slope, y-intercept, and determination coefficient, r2, for each curve are shown in Table 4.
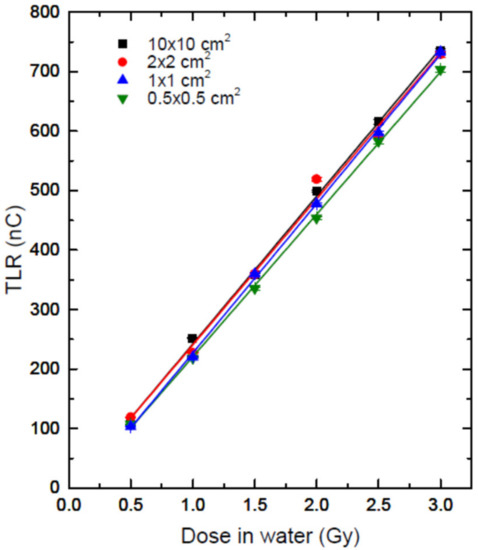
Figure 4.
TL response as a function of dose for each field size. The lines correspond to a linear fit.

Table 4.
Values of the linear fit parameters.
The percentage difference between the slopes and that of the 10 cm ×10 cm field was lower than 1% for the 2 cm × 2 cm and 1 cm × 1 cm fields, and 3.6% for the 0.5 cm × 0.5 cm field.
These differences may be because the relative response of TLD-100s as a function of photon energy for moderately filtered x-ray spectra in the range of 20–250 kVp relative to 60Co gamma rays increases with decreasing energy to a maximum value of about 1.37 at an effective energy of 27 keV, and decreases at lower energies [27], as well as the fact that the fluence of photons of energies lower than 1 MeV decreases with decreasing field size [28]. Additionally, the position of the TLD contributes to this difference. If the micro-cube is moved 0.5 mm from the field center for the smaller field, the TLD response decreases by 2%, because a part of it is in the penumbra (Figure 3).
3.2. Dosimetric Audit
Table 5 shows the field output factors measured using the diode detector, the applied monitor units, and the delivered doses for the small fields studied.

Table 5.
Output factors for estimating the delivered dose and calculating the MU.
The TLD-measured doses were evaluated using the calibration curve of the field with the size closest to that of the studied field.
Table 6 shows the measured doses and their percentage differences with respect to the delivered dose. It can be observed that, for the two largest fields, the percentage difference between the measured dose and the prescribed dose is smaller than the percentage uncertainty of the measured dose. It can be considered that for these fields, there is good agreement between the two doses. However, for the rest of the fields, the percentage differences are greater than the measurement uncertainties, but smaller than 5%. These differences are in accordance with the recommendation by the ICRU that the dose delivered be within 5% of the prescribed dose [29,30].

Table 6.
TLD-measured doses and the percentage difference relative to the prescribed dose.
4. Discussion and Conclusions
This work aimed to establish a protocol for measuring the dose in water delivered by small fields using TLD-100 micro-cubes. The results presented in this work can serve as the basis for such measurements and present a protocol for measuring the dose in water delivered by small fields (with diameters ranging from 4 to 20 mm), for a dose range between 0.5 to 3.0 Gy, using TLD-100 micro-cubes.
The aspects to be highlighted and that must be taken Into account in this methodology are as follows:
- It is necessary for the micro-TLDs of the dosimeters to undergo annealing for one hour at 400 °C and two hours at 100 °C.
- The use of radiochromic films is necessary for the audit in small photon beams to identify the position of the dosimeters during irradiation.
- The use of five dosimeters is suggested, arranged as shown in Figure 1, for each irradiation in order to obtain the calibration curve and conduct the audit.
- One face of the dosimeters should be marked so that the thermally stimulated face is always the same during the reading.
- At the moment of reading, the nitrogen flow should be kept as low as possible in order to avoid movements of the dosimeter.
- The sensitivity factor and the central dosimeter signal should be used to reduce the uncertainty.
- The calibration curve of the square field size closest to the field to be studied should be used.
By following this protocol, a considerable improvement in the reproducibility of the responses can be achieved, with a decrease in uncertainty of up to 7%—from 10 to 3%—when marking the dosimeters and using radiochromic dye film to determine the positions of the dosimeters in the center of the field.
A pilot dosimetric audit was carried out using the proposed protocol over a linear accelerator using small circular collimator photon beams. The results shown in this work are in agreement with those reported in similar audits (as presented in Table 1). Some authors have reported differences of up to 22% between the measured and calculated doses, while differences of 3% have been obtained with standard reference field sizes of 10 cm × 10 cm [22,23]. Budgell et al. [21] reported differences of up to 10% when analyzing cases of intensity-modulated fields. Finally, Espinosa et al. [20] reported differences smaller than 5% for a 1 cm × 1 cm field (the closest to the field sizes audited in this study) in 69% of the audited institutions, and lower than 2.9% in postal audit. In this work, the percentage difference between the delivered and measured doses was smaller than 3%, which is less than or equal to the differences reported in other works.
The methodology used to audit small radiation fields proposed in this work was validated on the basis of the results obtained. In future work, it is intended to carry out various audits in various radiotherapy centers, initially in the same city, for subsequent use nationwide. In the case of expanding this methodology to national postal audits, a development of this work will be considered regarding the fading of the TLD signal.
Author Contributions
Conceptualization, O.A.G.-G. and I.G.-d.; methodology, O.A.G.-G., J.M.L.-G. and I.G.-d.; formal analysis, O.A.G.-G., J.M.L.-G., S.P.-J. and I.G.-d.; investigation, O.A.G.-G., J.M.L.-G., S.P.-J. and I.G.-d.; resources, O.A.G.-G. and I.G.-d.; data curation, S.P.-J. and I.G.-d.; writing—original draft preparation, O.A.G.-G. and I.G.-d.; writing—review and editing, O.A.G.-G., J.M.L.-G. and I.G.-d.; visualization, O.A.G.-G.; supervision, I.G.-d.; project administration, O.A.G.-G. and I.G.-d.; funding acquisition, O.A.G.-G. and I.G.-d. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Health and Social Security Research Sector Fund A3-S-37057 approved by the National Council of Research and Technology (CONACYT).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data is available upon request to the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Das, I.J.; Ding, G.X.; Ahnesjö, A. Small fields: Nonequilibrium radiation dosimetry. Med. Phys. 2007, 35, 206–215. [Google Scholar] [CrossRef] [PubMed]
- International Atomic Energy Agency. Dosimetry of Small Static Fields Used in External Beam Radiotherapy; Technical Reports Series No. 483; IAEA: Vienna, Austria, 2017. [Google Scholar]
- International Atomic Energy Agency. Absorbed Dose Determination in External Beam Radiotherapy; Technical Reports Series No. 398; IAEA: Vienna, Austria, 2000. [Google Scholar]
- Almond, P.R.; Biggs, P.J.; Coursey, B.M.; Hanson, W.F.; Huq, M.S.; Nath, R.; Rogers, D.W.O. AAPM’s TG-51 protocol for clinical reference dosimetry of high-energy photon and electron beams. Med. Phys. 1999, 26, 1847–1870. [Google Scholar] [CrossRef] [PubMed]
- International Atomic Energy Agency. Comprehensive Audits of Radiotherapy Practices: A Tool for Quality Improvement; Non-serial Publications; IAEA: Vienna, Austria, 2007. [Google Scholar]
- Pasler, M.; Hernandez, V.; Jornet, N.; Clark, C.H. Novel methodologies for dosimetry audits: Adapting to advanced radiotherapy techniques. Phys. Imaging Radiat. Oncol. 2018, 5, 76–84. [Google Scholar] [CrossRef] [PubMed]
- Clark, C.H.; Jornet, N.; Muren, L.P. The role of dosimetry audit in achieving high quality radiotherapy. Phys. Imaging Radiat. Oncol. 2018, 5, 85–87. [Google Scholar] [CrossRef]
- Thomas, R.A.; Bolt, M.A.; Bass, G.; Nutbrown, R.; Chen, T.; Nisbet, A.; Clark, C.H. Radiotherapy reference dose audit in the United Kingdom by the National Physical Laboratory: 20 years of consistency and improvements. Phys. Imaging Radiat. Oncol. 2017, 3, 21–27. [Google Scholar] [CrossRef]
- Eaton, D.J.; Bolton, S.; Thomas, R.A.S.; Clark, C. Inter-departmental dosimetry audits—development of methods and lessons learned. J. Med. Phys. 2015, 40, 183–189. [Google Scholar] [CrossRef]
- Maruyama, D.; Yanagisawa, S.; Koba, Y.; Andou, T.; Shinsho, K. Usefulness of Thermoluminescent Slab Dosimeter for Postal Dosimetry Audit of External Radiotherapy Systems. Sens. Mater. 2020, 32, 1461. [Google Scholar] [CrossRef]
- Kry, S.F.; Peterson, C.B.; Howell, R.M.; Izewska, J.; Lye, J.; Clark, C.H.; Nakamura, M.; Hurkmans, C.; Alvarez, P.; Alves, A.; et al. Remote beam output audits: A global assessment of results out of tolerance. Phys. Imaging Radiat. Oncol. 2018, 7, 39–44. [Google Scholar] [CrossRef]
- Dimitriadis, A.; Palmer, A.L.; Thomas, R.A.; Nisbet, A.; Clark, C.H. Adaptation and validation of a commercial head phantom for cranial radiosurgery dosimetry end-to-end audit. Br. J. Radiol. 2017, 90, 20170053. [Google Scholar] [CrossRef]
- Alfonso, R.; Andreo, P.; Capote, R.; Huq, M.S.; Kilby, W.; Kjäll, P.; Mackie, T.R.; Palmans, H.; Rosser, K.; Seuntjens, J.; et al. A new formalism for reference dosimetry of small and nonstandard fields. Med. Phys. 2008, 35, 5179–5186. [Google Scholar] [CrossRef]
- Alvarez, P.; Kry, S.; Stingo, F.; Followill, D. TLD and OSLD dosimetry systems for remote audits of radiotherapy external beam calibration. Radiat. Meas. 2017, 106, 412–415. [Google Scholar] [CrossRef]
- Iżewska, J.; Georg, D.; Bera, P.; Thwaites, D.; Arib, M.; Saravi, M.; Sergieva, K.; Li, K.; Yip, F.G.; Mahant, A.K.; et al. A methodology for TLD postal dosimetry audit of high-energy radiotherapy photon beams in non-reference conditions. Radiother. Oncol. 2007, 84, 67–74. [Google Scholar] [CrossRef]
- Izewska, J.; Andreo, P.; Vatnitsky, S.; Shortt, K.R. The IAEA/WHO TLD postal dose quality audits for radiotherapy: A perspective of dosimetry practices at hospitals in developing countries. Radiother. Oncol. 2003, 69, 91–97. [Google Scholar] [CrossRef]
- Brandon, L. Commissioning of Micro-Cube Thermoluminescent Dosimeters for Small Field Dosimetry Quality Assurance in Radiotherapy. The University of Texas MD Anderson Cancer Center UTHealth Graduate School of Biomedical Sciences Dissertations and Theses (Open Access). 2019, p. 951. Available online: https://digitalcommons.library.tmc.edu/utgsbs_dissertations/951 (accessed on 11 September 2019).
- García-Garduño, O.A.; Rodríguez-Ávila, M.A.; Lárraga-Gutiérrez, J.M. Detector-specific correction factors in radiosurgery beams and their impact on dose distribution calculations. PLoS ONE 2018, 13, e0196393. [Google Scholar] [CrossRef]
- Bassinet, C.; Robbes, I.; Barbier, L.; Baumann, M.; Kernisant, B.; Trompier, F. Characterization of 7LiF:Mg,Ti TLD micro-cubes. Radiat. Meas. 2010, 45, 646–648. [Google Scholar] [CrossRef]
- Espinosa, M.D.M.; Núñez, L.; Muñiz, J.L.; Lagares, J.I.; Embid, M.; Gómez-Ros, J.M. Postal dosimetry audit test for small photon beams. Radiother. Oncol. 2012, 102, 135–141. [Google Scholar] [CrossRef]
- Budgell, G.; Berresford, J.; Trainer, M.; Bradshaw, E.; Sharpe, P.; Williams, P. A national dosimetric audit of IMRT. Radiother. Oncol. 2011, 99, 246–252. [Google Scholar] [CrossRef]
- Hourdakis, C.J.; Boziari, A. Dosimetry quality audit of high energy photon beams in greek radiotherapy centers. Radiother. Oncol. 2008, 87, 132–141. [Google Scholar] [CrossRef]
- da Rosa, L.A.R.; Brito, R.R.A.; Goncalves, M.; de Paiva, E.; Dovales, A.C.M.; Freire, B.L.V.; Giannoni, R.A.; Di Prinzio, R.; Velasco, A.F.; Castelo, L.H.R.; et al. Dosimetric audits of photon beams in radiation therapy centres in Rio de Janeiro, Brazil. Radiat. Prot. Dosim. 2008, 131, 272–275. [Google Scholar] [CrossRef]
- Peña-Jiménez, S.; Lárraga-Gutiérrez, J.M.; Garduño, O.A.G.; Gamboa-Debuen, I. Characterization of TLD-100 micro-cubes for use in small field dosimetry. Radiat. Prot. Dosim. 2014, 1626, 168–170. [Google Scholar] [CrossRef]
- Muniz, J.L.; Delgado, A.; Gómez-Ros, J.M.; Brosed, A. Application of glow curve analysis methods to radiotherapy mailed dosimetry with LiF TLD-100. Phys. Med. Biol. 1995, 40, 253–268. [Google Scholar] [CrossRef] [PubMed]
- Da Rosa, L.A.R.; Regulla, D.F.; Fill, U.A. Reproducibility study of TLD-100 micro-cubes at radiotherapy dose level. Appl. Radiat. Isot. 1999, 50, 573–577. [Google Scholar] [CrossRef] [PubMed]
- Nunn, A.A.; Davis, S.D.; Micka, J.A.; DeWerd, L.A. LiF:Mg,Ti TLD response as a function of photon energy for moderately filtered x-ray spectra in the range of 20-250 kVp relative to C60o. Med. Phys. 2008, 35, 1859–1869. [Google Scholar] [CrossRef] [PubMed]
- García Hernández, D.; Lárraga-Gutiérrez, J.M. Desempeño de Dosímetros de Película Para la Caracterización de Haces de Fotones de Alta Energía Usados en Radiocirugía Estereotáctica. Tesis de Maestría, Posgrado en Ciencias Físicas, UNAM, Mexico City, Mexico, 2012. [Google Scholar]
- ICRU 76. Determination of Absorbed Dose in a Patient Irradiated by Beams of X or Gamma Rays in Radiotherapy Procedures; ICRU Report 24; International Commission on Radiation Units and Measurementss: Bethesda, MD, USA, 1976.
- AAPM Report 54: Stereotactic Radiosurgery Task Group 42; American Association of Physicists in Medicine: New York, NY, USA, 1995. [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).