Prevalence and Characteristics of Radiographic Radiolucencies Associated with Class II Composite Restorations
Abstract
1. Introduction
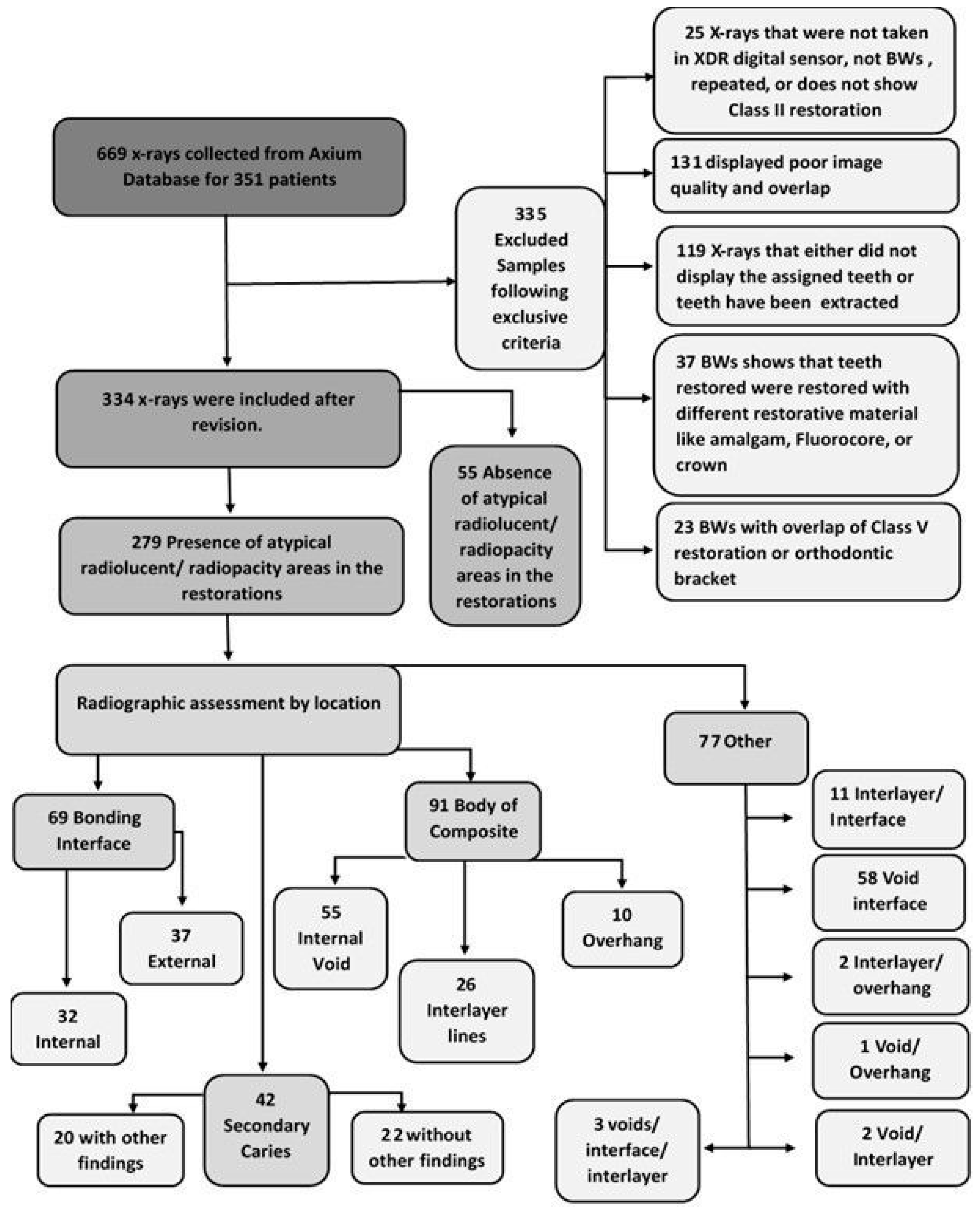
2. Methods and Materials
2.1. Study Design
2.2. Eligibility Criteria
2.3. Radiographic Assessment
2.4. Categorization of the Radiographic Findings
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Wenzel, A. A Review of Dentists’ Use of Digital Radiography and Caries Diagnosis with Digital Systems. Dentomaxillofac. Radiol. 2006, 35, 307–314. [Google Scholar] [CrossRef] [PubMed]
- Akarslan, Z.Z.; Akdevelioğlu, M.; Güngör, K.; Erten, H. A Comparison of the Diagnostic Accuracy of Bitewing, Periapical, Unfiltered and Filtered Digital Panoramic Images for Approximal Caries Detection in Posterior Teeth. Dentomaxillofac. Radiol. 2008, 37, 458–463. [Google Scholar] [CrossRef] [PubMed]
- Atchison, K.A.; White, S.C.; Flack, V.F.; Hewlett, E.R. Assessing the FDA Guidelines for Ordering Dental Radiographs. J. Am. Dent. Assoc. 1995, 126, 1372–1383. [Google Scholar] [CrossRef] [PubMed]
- Haak, R.; Wicht, M.J.; Hellmich, M.; Noack, M.J. Detection of Marginal Defects of Composite Restorations with Conventional and Digital Radiographs. Eur. J. Oral Sci. 2002, 110, 282–286. [Google Scholar] [CrossRef]
- Wenzel, A. Bitewing and Digital Bitewing Radiography for Detection of Caries Lesions. J. Dent. Res. 2004, 83, 72–75. [Google Scholar] [CrossRef]
- Eltahlah, D.; Lynch, C.D.; Chadwick, B.L.; Blum, I.R.; Wilson, N.H.F. An Update on the Reasons for Placement and Replacement of Direct Restorations. J. Dent. 2018, 72, 1–7. [Google Scholar] [CrossRef]
- Fröhlich, T.T.; Nicoloso, G.F.; Lenzi, T.L.; Soares, F.Z.M.; De Oliveira Rocha, R. The Thickness of the Adhesive Layer Increases the Misdiagnosing of the Radiolucent Zones and Restoration Replacement Indication: Thickness of the Adhesive Layer. J. Esthet. Restor. Dent. 2017, 29, 193–200. [Google Scholar] [CrossRef]
- Gordan, V.V.; Garvan, C.W.; Richman, J.S.; Fellows, J.L.; Rindal, D.B.; Qvist, V.; Heft, M.W.; Williams, O.D.; Gilbert, G.H.; for the DPBRN Collaborative Group. How Dentists Diagnose and Treat Defective Restorations: Evidence from The Dental Practice-Based Research Network. Oper. Dent. 2009, 34, 664–673. [Google Scholar] [CrossRef]
- Wilson, N.; Lynch, C.; Brunton, P.; Hickel, R.; Meyer-Lueckel, H.; Gurgan, S.; Pallesen, U.; Shearer, A.; Tarle, Z.; Cotti, E.; et al. Criteria for the Replacement of Restorations: Academy of Operative Dentistry European Section. Oper. Dent. 2016, 41, S48–S57. [Google Scholar] [CrossRef]
- Purk, J.H.; Dusevich, V.; Glaros, A.; Eick, J.D. Adhesive Analysis of Voids in Class II Composite Resin Restorations at the Axial and Gingival Cavity Walls Restored under In Vivo versus In Vitro Conditions. Dent. Mater. 2007, 23, 871–877. [Google Scholar] [CrossRef]
- Chuang, S.F.; Liu, J.K.; Chao, C.C.; Liao, F.P.; Chen, Y.H. Effects of Flowable Composite Lining and Operator Experience on Microleakage and Internal Voids in Class II Composite Restorations. J. Prosthet. Dent. 2001, 85, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Kurşun, Ş.; Dinç, G.; Öztaş, B.; Yüksel, S.; Kamburoğlu, K. The Visibility of Secondary Caries under Bonding Agents with Two Different Imaging Modalities. Dent. Mater. J. 2012, 31, 975–979. [Google Scholar] [CrossRef] [PubMed]
- Pardo Díaz, C.; Shimokawa, C.; Sampaio, C.; Freitas, A.; Turbino, M. Characterization and Comparative Analysis of Voids in Class II Composite Resin Restorations by Optical Coherence Tomography. Oper. Dent. 2020, 45, 71–79. [Google Scholar] [CrossRef]
- Liedke, G.S.; Spin-Neto, R.; da Silveira, H.E.D.; Wenzel, A. Radiographic Diagnosis of Dental Restoration Misfit: A Systematic Review. J. Oral Rehabil. 2014, 41, 957–967. [Google Scholar] [CrossRef] [PubMed]
- Francio, L.A.; Silva, F.E.; Valerio, C.S.; Cardoso, C.A.e.A.; Jansen, W.C.; Manzi, F.R. Accuracy of Various Imaging Methods for Detecting Misfit at the Tooth-Restoration Interface in Posterior Teeth. Imaging Sci. Dent. 2018, 48, 87. [Google Scholar] [CrossRef]
- Soares, C.; Rosatto, C.; Carvalho, V.; Bicalho, A.; Henriques, J.; Faria-e-Silva, A. Radiopacity and Porosity of Bulk-Fill and Conventional Composite Posterior Restorations—Digital X-ray Analysis. Oper. Dent. 2017, 42, 616–625. [Google Scholar] [CrossRef]
- Kirsch, J.; Tchorz, J.; Hellwig, E.; Tauböck, T.T.; Attin, T.; Hannig, C. Decision Criteria for Replacement of Fillings: A Retrospective Study. Clin. Exp. Dent. Res. 2016, 2, 121–128. [Google Scholar] [CrossRef] [PubMed]
- Lynch, C.D.; McConnell, R.J.; Wilson, N.H.F. Teaching the Placement of Posterior Resin-Based Composite Restorations in U.S. Dental Schools. J. Am. Dent. Assoc. 2006, 137, 619–625. [Google Scholar] [CrossRef]
- Hayashi, J.; Shimada, Y.; Tagami, J.; Sumi, Y.; Sadr, A. Real-Time Imaging of Gap Progress during and after Composite Polymerization. J. Dent. Res. 2017, 96, 992–998. [Google Scholar] [CrossRef]
- Sarrett, D. Clinical Challenges and the Relevance of Materials Testing for Posterior Composite Restorations. Dent. Mater. 2005, 21, 9–20. [Google Scholar] [CrossRef]
- Scolavino, S.; Paolone, G.; Orsini, G.; Devoto, W.; Putignano, A. The Simultaneous Modeling Technique: Closing Gaps in Posteriors. Int. J. Esthet. Dent. 2016, 11, 58–81. [Google Scholar] [PubMed]
- Mulder, R.; Mohammed, N.; du Plessis, A.; le Roux, S.G. A Pilot Study Investigating the Presence of Voids in Bulk Fill Flowable Composites. S. Afr. Dent. J. 2017, 72, 462–465. [Google Scholar] [CrossRef]
- Opdam, N.J.M.; Roeters, J.J.M.; Joosten, M.; vd Veeke, O. Porosities and Voids in Class I Restorations Placed by Six Operators Using a Packable or Syringable Composite. Dent. Mater. 2002, 18, 58–63. [Google Scholar] [CrossRef] [PubMed]
- Samet, N.; Kwon, K.-R.; Good, P.; Weber, H.-P. Voids and Interlayer Gaps in Class 1 Posterior Composite Restorations: A Comparison between a Microlayer and a 2-Layer Technique. Quintessence Int. 2006, 37, 803–809. [Google Scholar]
- Reeves, T.E.; Lien, W.; Mah, P. Quality Assurance: Acceptance Testing for Digital Dental Intraoral Sensors. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2020, 129, 388–400. [Google Scholar] [CrossRef]
- Opdam, N.J.M.; Roeters, F.J.M.; Feilzer, A.J.; Smale, I. A Radiographic and Scanning Electron Microscopic Study of Approximal Margins of Class II Resin Composite Restorations Placed In Vivo. J. Dent. 1998, 26, 319–327. [Google Scholar] [CrossRef]
- Jansson, L.; Ehnevid, H.; Lindskog, S.; Blomlöf, L. Proximal Restorations and Periodontal Status. J. Clin. Periodontol. 1994, 21, 577–582. [Google Scholar] [CrossRef] [PubMed]
- Reeves, J. Periodontal Health--Challenges in Restorative Dentistry. Prim. Dent. J. 2014, 3, 73–76. [Google Scholar] [CrossRef] [PubMed]
- Frankenberger, R.; Krämer, N.; Pelka, M.; Petschelt, A. Internal Adaptation and Overhang Formation of Direct Class II Resin Composite Restorations. Clin. Oral Investig. 1999, 3, 208–215. [Google Scholar] [CrossRef]
- Signori, C.; Laske, M.; Mendes, F.M.; Huysmans, M.-C.D.N.J.M.; Cenci, M.S.; Opdam, N.J.M. Decision-Making of General Practitioners on Interventions at Restorations Based on Bitewing Radiographs. J. Dent. 2018, 76, 109–116. [Google Scholar] [CrossRef]
- Araujo, F.O.; Vieira, L.C.C.; Monteiro, S. Influence of Resin Composite Shade and Location of the Gingival Margin on the Microleakage of Posterior Restorations. Oper. Dent. 2006, 31, 556–561. [Google Scholar] [CrossRef] [PubMed]
- Cenci, M.S.; Pereira-Cenci, T.; Cury, J.A.; Ten Cate, J.M. Relationship between Gap Size and Dentine Secondary Caries Formation Assessed in a Microcosm Biofilm Model. Caries Res. 2009, 43, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Turkistani, A.; Nakashima, S.; Shimada, Y.; Tagami, J.; Sadr, A. Microgaps and Demineralization Progress around Composite Restorations. J. Dent. Res. 2015, 94, 1070–1077. [Google Scholar] [CrossRef] [PubMed]
- Hewlett, E.R.; Atchison, K.A.; White, S.C.; Flack, V. Radiographic Secondary Caries Prevalence in Teeth with Clinically Defective Restorations. J. Dent. Res. 1993, 72, 1604–1608. [Google Scholar] [CrossRef]
- Hotta, M.; Yamamoto, K. Comparative Radiopacity of Bonding Agents. J. Adhes. Dent. 2009, 11, 207–212. [Google Scholar] [PubMed]
- Yang, X.; Zhang, D.; Wu, B.; Zhang, K.; Yang, B.; Wang, Z.; Wu, X. Accurate Characterization of the Adhesive Layer Thickness of Ceramic Bonding Structures Using Terahertz Time-Domain Spectroscopy. Materials 2022, 15, 6972. [Google Scholar] [CrossRef] [PubMed]
- Secgin, C.K.; Gulsahi, A.; Arhun, N. Diagnostic Challange: Instances Mimicking a Proximal Carious Lesion Detected by Bitewing Radiography. Oral Health Dent. Manag. 2016, 15, 1–5. [Google Scholar]
- Mua, B.; Barbachan E Silva, B.; Fontanella, V.R.C.; Giongo, F.C.M.D.S.; Maltz, M. Radiolucent Halos beneath Composite Restorations Do Not Justify Restoration Replacement. Am. J. Dent. 2015, 28, 209–213. [Google Scholar]
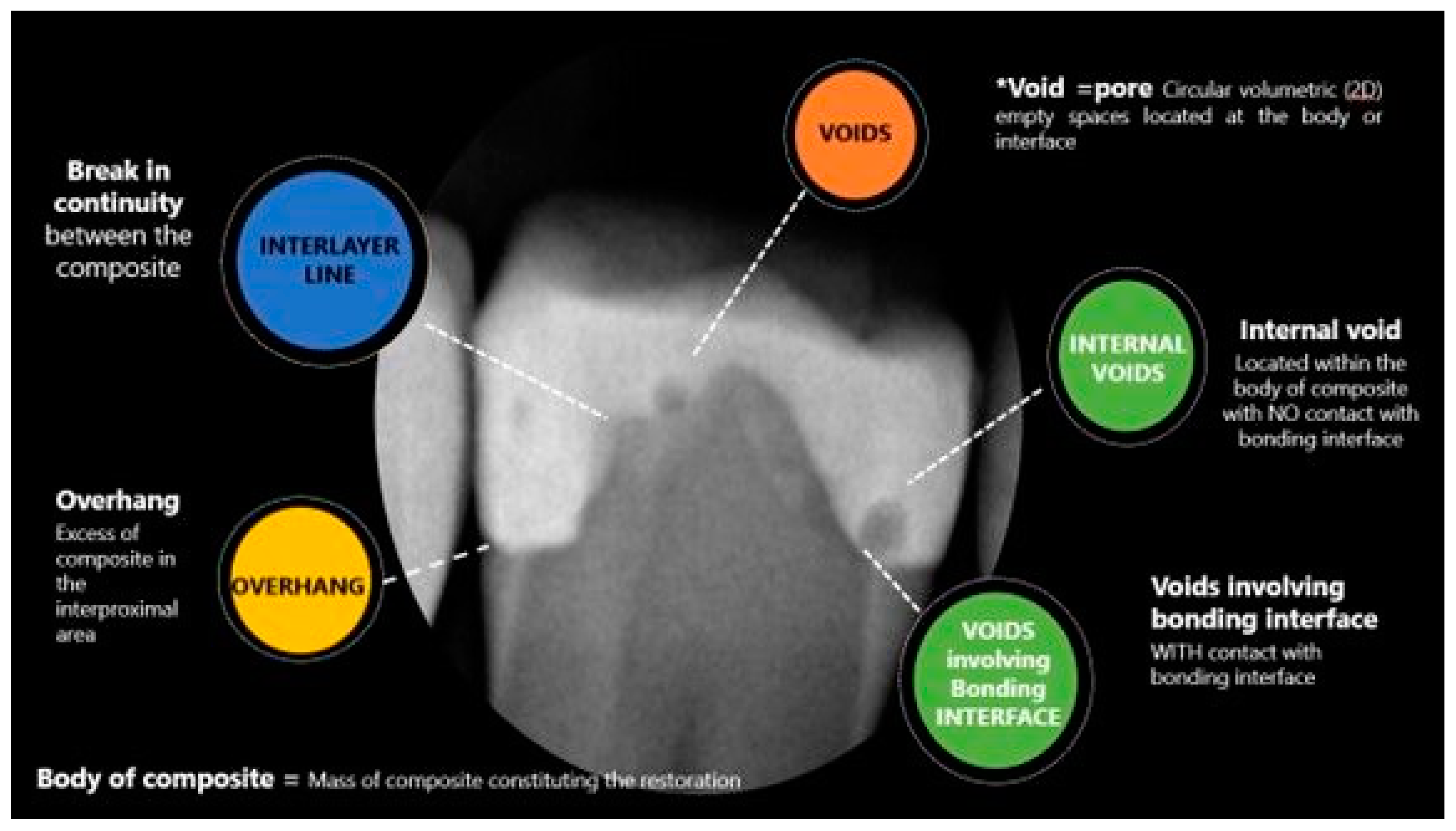

| Location | Category | Description |
|---|---|---|
| No atypical radiographic finding | No radiolucent or radiopaque results suggesting atypical radiographic findings in composite restoration | |
| Body of the restoration Mass of composite constituting the restoration | Internal void/porous | Void = pore Circular volumetric (2D) empty radiolucent spaces located at the body |
| Interlayer line | Lack of continuity between the composite layers characterized by a thin radiolucent line | |
| Overhang | Excess radiopaque composite in the interproximal area | |
| Bonding interface Surface (Line) between tooth and composite | Internal gap–not gingival margin | Lack of continuity, radiolucency between the composite and tooth not involving gingival margins |
| External gap–at the gingival margin | Radiolucency, lack of continuity between the composite and tooth involving gingival margins: usually “notch” shape. | |
| Secondary caries | Presence of radiolucency in dentine indicating recurrent caries | |
| Other | More than one radiographic finding indicating multicategory |
| Radiographic Finding | Frequency/Total | Percentage % |
|---|---|---|
| No atypical findings | 55/334 | 16.5% |
| Atypical findings | 279/334 | 83.5% |
| Bonding interface | 69/334 | 20.7% |
| External bonding interface | 37/334 | 11.1% |
| Internal bonding interface | 32/334 | 9.6% |
| Body of composite | 91/334 | 27.2% |
| Internal Void | 55/334 | 16.5% |
| Interlayer lines | 26/334 | 7.8% |
| Overhang | 10/334 | 3.0% |
| Secondary caries | 42/334 | 12.6% |
| With other radiographic findings | 20/334 | 6.0% |
| Without other findings | 22/334 | 6.6% |
| Other findings | 77/334 | 23.1% |
| Interlayer/interface | 11/334 | 3.3% |
| Void interface | 58/334 | 17.4% |
| Void/overhang | 1/334 | 0.3% |
| Void/interlayer | 2/334 | 0.6% |
| Void/interlayer/interface | 3/334 | 0.9% |
| Interlayer/overhang | 2/334 | 0.6% |
| Radiographic Finding | Gender | Age | Tooth | Restoration Surface | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| F | M | <21 | 21–45 | 46–65 | >65 | PM | M | MO | DO | MOD | ||
| No Voids | freq. | 36/55 | 19/55 | 0/55 | 29/55 | 20/55 | 6/55 | 24/55 | 31/55 | 20/55 | 28/55 | 7/55 |
| perc. | 65.5% | 34.5% | 0.0% | 52.7% | 36.4% | 10.9% | 43.6% | 56.4% | 36.4% | 50.9% | 12.7% | |
| Internal Void | freq. | 37/55 | 18/55 | 2/55 | 29/55 | 22/55 | 2/55 | 38/55 | 17/55 | 11/55 | 36/55 | 8/55 |
| perc. | 67.3% | 32.7% | 3.6% | 52.7% | 40.0% | 3.6% | 69.1% | 30.9% | 20.0% | 65.5% | 14.5% | |
| Interlayer | freq. | 15/26 | 11/26 | 2/26 | 16/26 | 6/26 | 2/26 | 18/26 | 8/26 | 4/26 | 15/26 | 7/26 |
| perc. | 57.7% | 42.3% | 7.7% | 61.5% | 23.1% | 7.7% | 69.2% | 30.8% | 15.4% | 57.7% | 26.9% | |
| Overhang | freq. | 5/10 | 5/10 | 1/10 | 4/10 | 5/10 | 0/10 | 6/10 | 4/10 | 6/10 | 3/10 | 1/10 |
| perc. | 50% | 50% | 10% | 40% | 50% | 0% | 60% | 40% | 60% | 30% | 10% | |
| Interface | freq. | 35/69 | 34/69 | 3/69 | 36/69 | 21/69 | 9/69 | 44/69 | 25/69 | 24/69 | 38/69 | 7/69 |
| perc. | 51% | 49% | 4% | 52% | 30% | 13% | 64% | 36% | 35% | 55% | 10% | |
| Caries | freq. | 23/42 | 19/42 | 3/42 | 16/42 | 19/42 | 4/42 | 30/42 | 12/42 | 13/42 | 19/42 | 10/42 |
| perc. | 55% | 45% | 7% | 38% | 45% | 10% | 71% | 29% | 31% | 45% | 24% | |
| Other | freq. | 58/77 | 19/77 | 2/77 | 43/77 | 26/77 | 6/77 | 65/77 | 12/77 | 11/77 | 53/77 | 13/77 |
| perc. | 75% | 25% | 3% | 56% | 34% | 8% | 84% | 16% | 14% | 69% | 17% | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bazerbashi, J.; Alkhubaizi, Q.; Parsa, A.; Shabayek, M.; Strassler, H.; Melo, M.A.S. Prevalence and Characteristics of Radiographic Radiolucencies Associated with Class II Composite Restorations. Appl. Sci. 2023, 13, 4780. https://doi.org/10.3390/app13084780
Bazerbashi J, Alkhubaizi Q, Parsa A, Shabayek M, Strassler H, Melo MAS. Prevalence and Characteristics of Radiographic Radiolucencies Associated with Class II Composite Restorations. Applied Sciences. 2023; 13(8):4780. https://doi.org/10.3390/app13084780
Chicago/Turabian StyleBazerbashi, Jood, Qoot Alkhubaizi, Azin Parsa, Mohamed Shabayek, Howard Strassler, and Mary Anne S. Melo. 2023. "Prevalence and Characteristics of Radiographic Radiolucencies Associated with Class II Composite Restorations" Applied Sciences 13, no. 8: 4780. https://doi.org/10.3390/app13084780
APA StyleBazerbashi, J., Alkhubaizi, Q., Parsa, A., Shabayek, M., Strassler, H., & Melo, M. A. S. (2023). Prevalence and Characteristics of Radiographic Radiolucencies Associated with Class II Composite Restorations. Applied Sciences, 13(8), 4780. https://doi.org/10.3390/app13084780










