Imaging and 3D Analysis Based on Two or More Three-Dimensional CBCT Recordings before and after Orthodontic Treatment and Maxillofacial Therapy
Abstract
1. Introduction
2. Materials and Methods
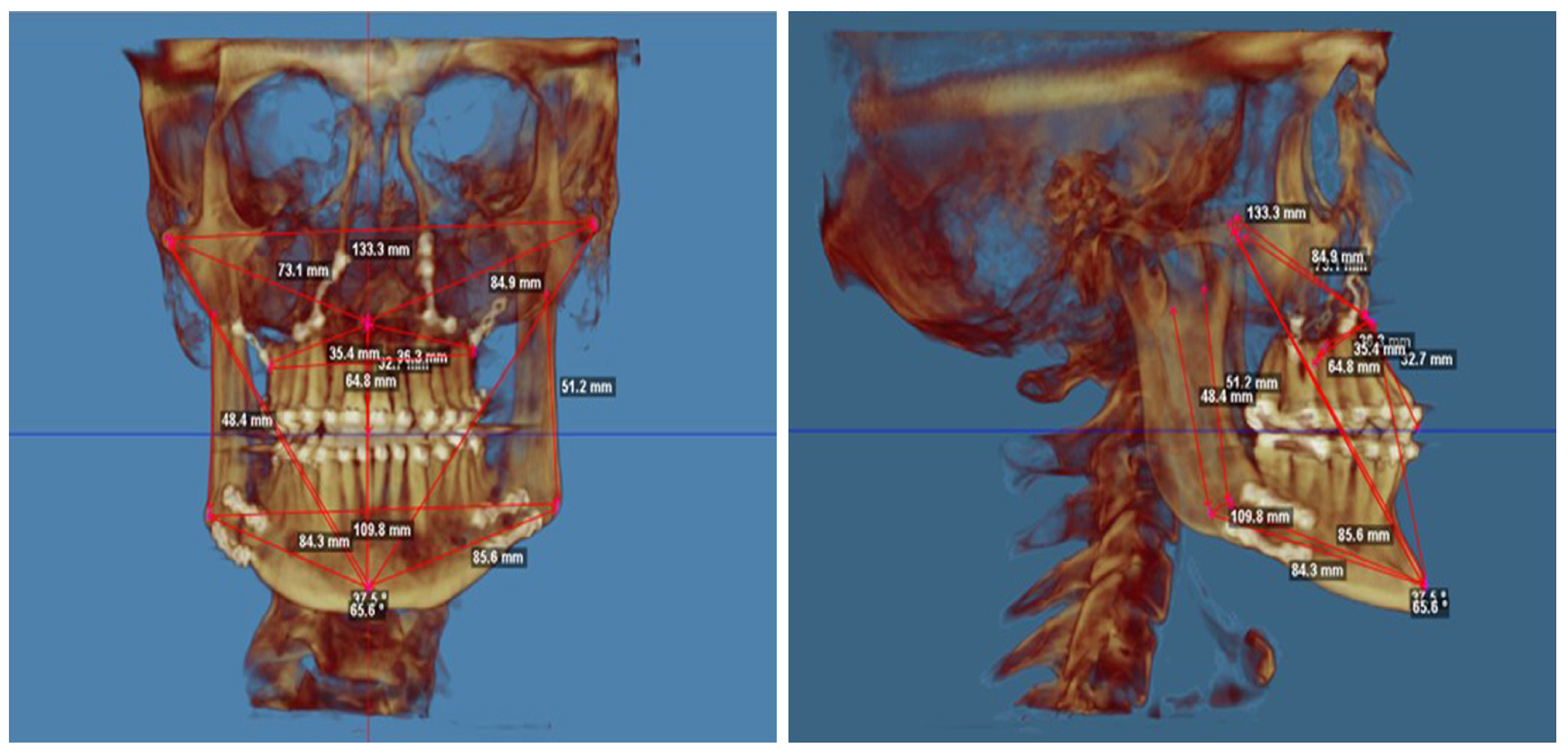
- taking cranial measurements on 3D cranial models,
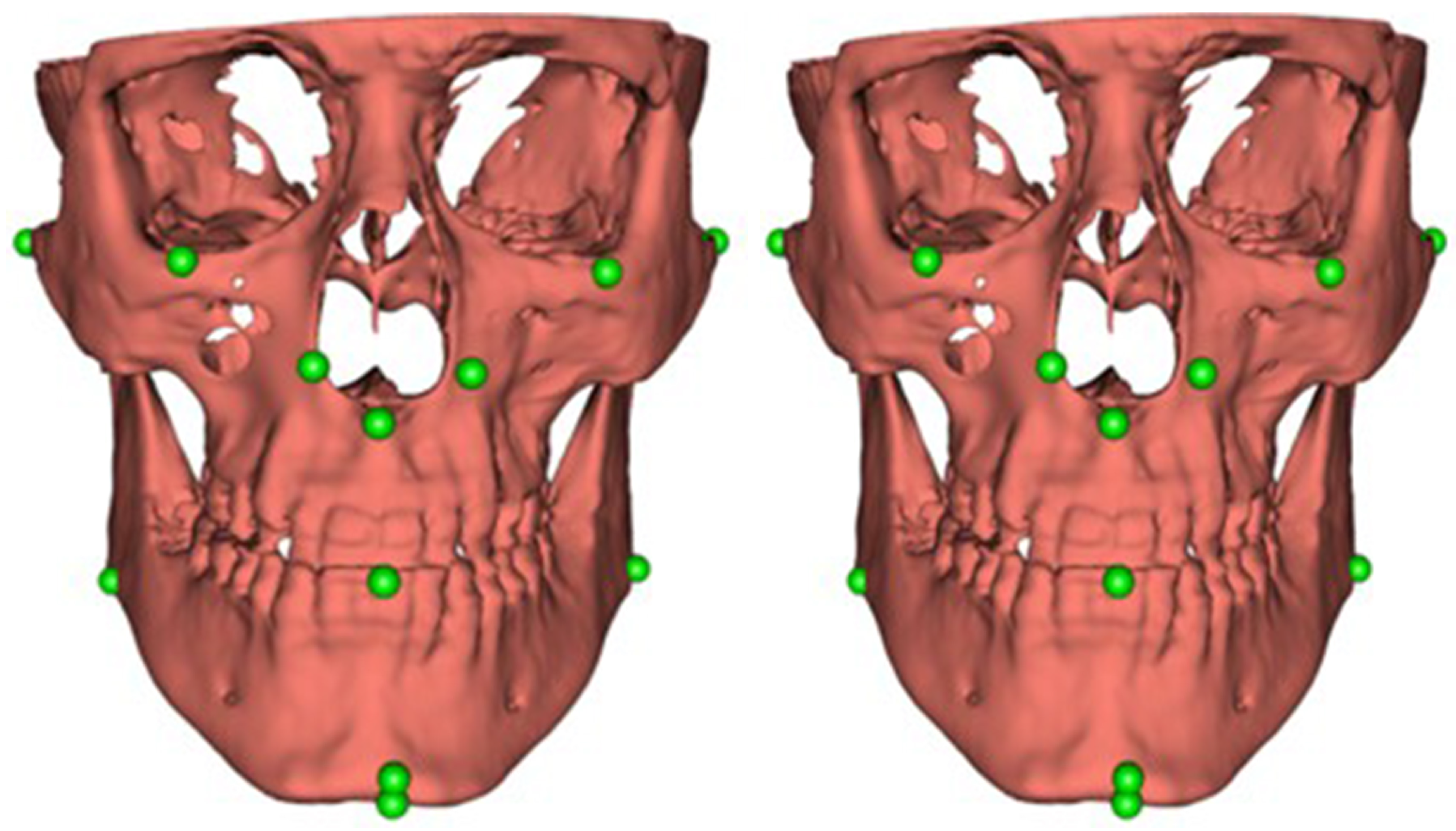
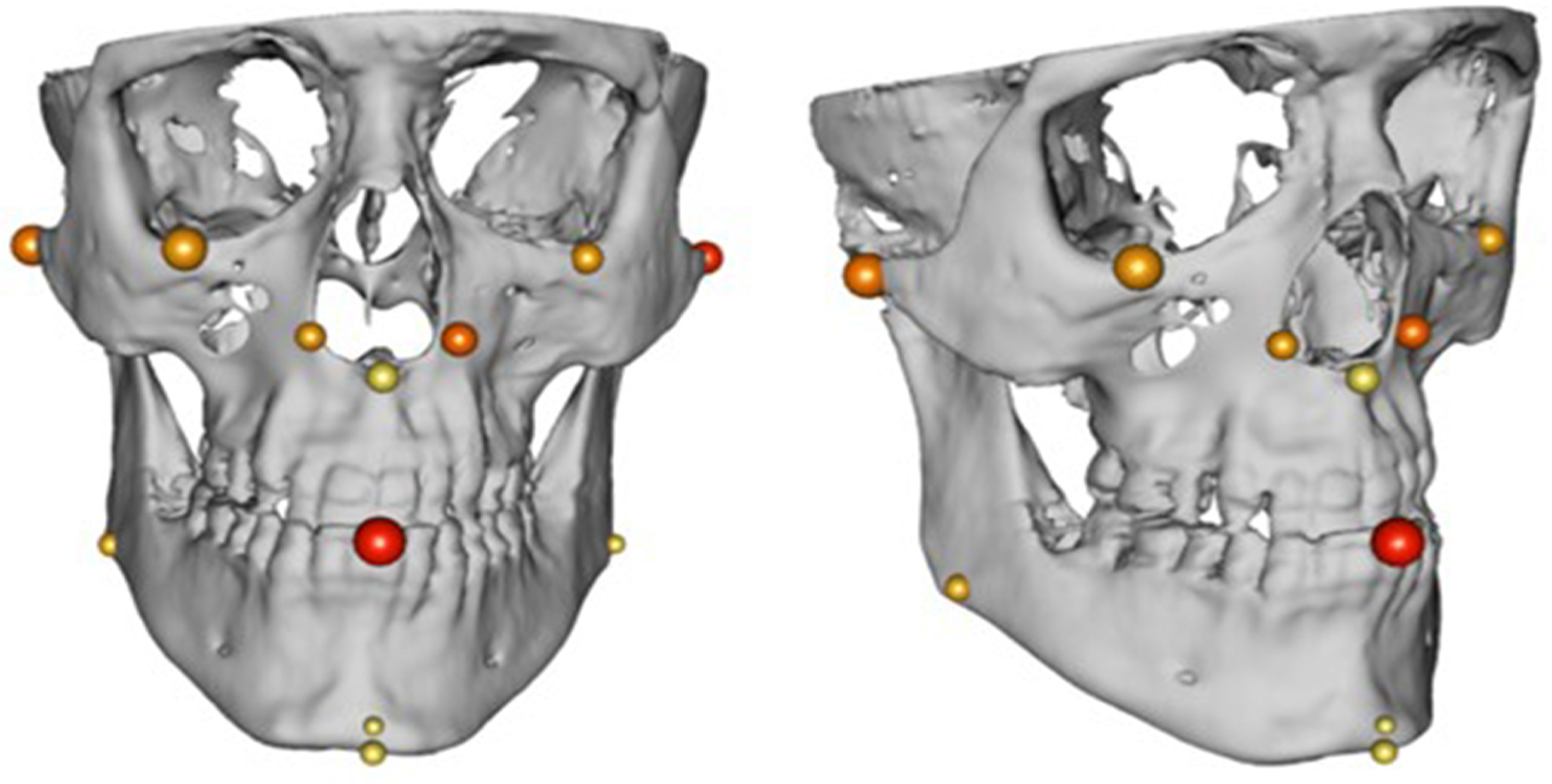
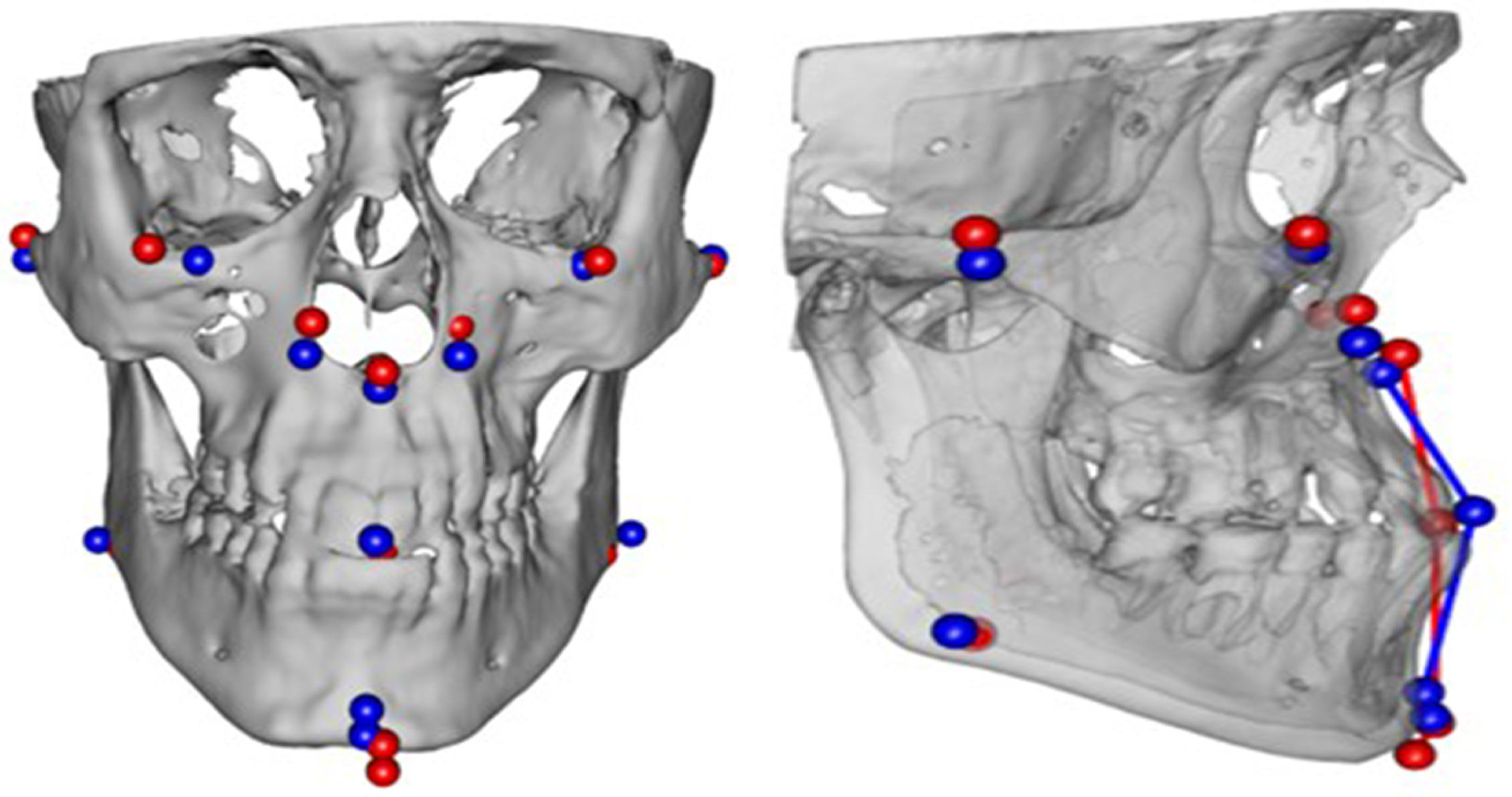
- collecting discrete feature points on 3D cranial models,
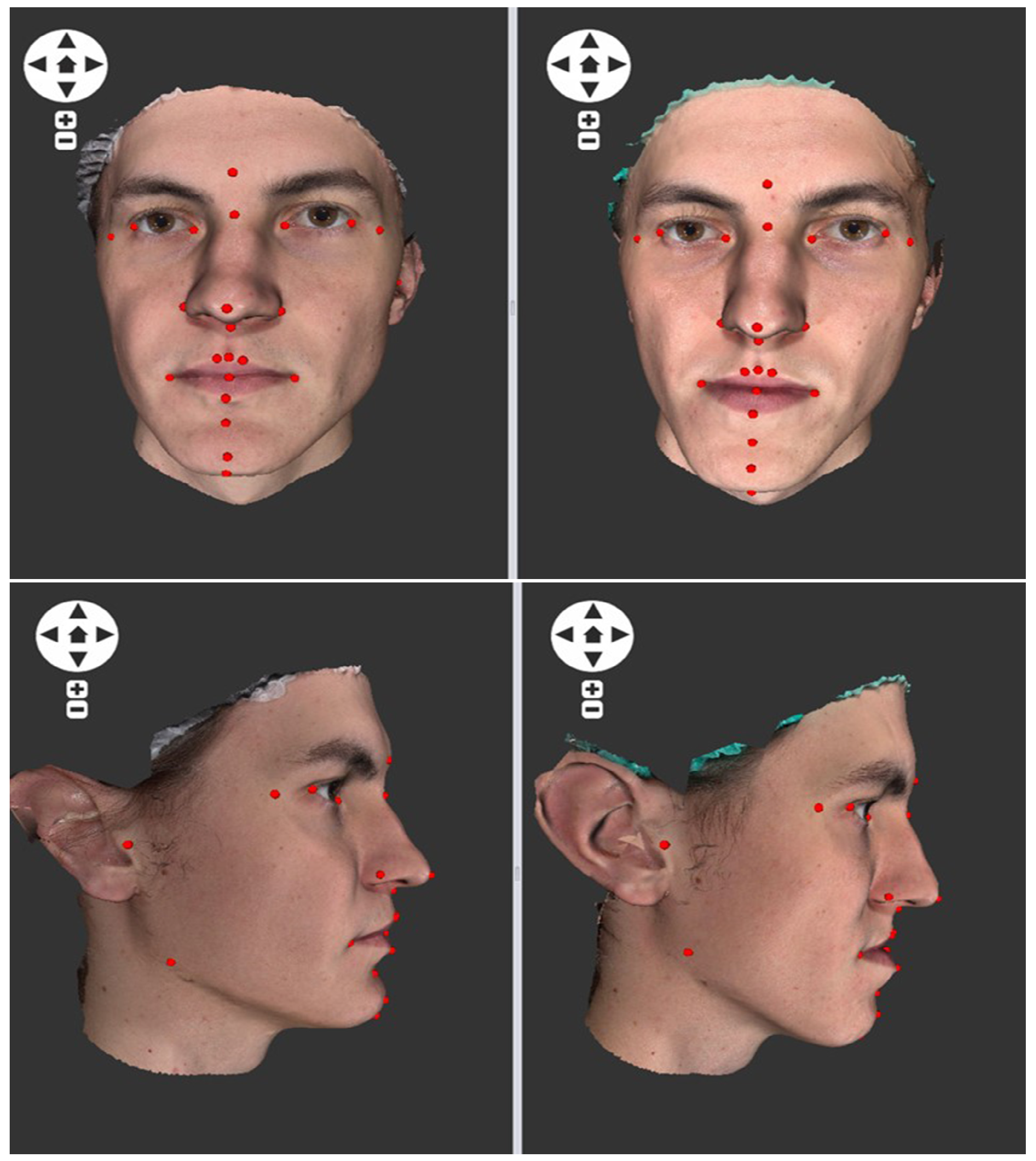
- using surface face models and discrete feature points collected on 3D face models.
3. Results
3.1. Cranial Metrics Altered by Surgery
3.2. Landmark-Based Hard Tissue Comparison
3.3. Surface and Landmark-Based Soft Tissue Comparison
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Scarfe, W.; Azevedo, B.; Toghyani, S.; Farman, A. Cone Beam Computed Tomographic Imaging in Orthodontics. Aust. Dent. J. 2017, 62, 33–50. [Google Scholar] [CrossRef] [PubMed]
- Kapila, S.; Nervina, J. CBCT in orthodontics: Assessment of treatment outcomes and indications for its use. Dentomaxillofac. Radiol. 2015, 44, 20140282. [Google Scholar] [CrossRef]
- Flugge, T.; Derksen, W.; Te Poel, J.; Hassan, B.; Nelson, K.; Wismeijer, D. Registration of cone beam computed tomography data and intraoral surface scans—A prerequisite for guided implant surgery with CAD/CAM drilling guides. Clin. Oral Implants Res. 2017, 28, 1113–1118. [Google Scholar] [CrossRef]
- Nur, R.; Derya Germec Cakan, D.; Arun, T. Cone Beam Computed Tomography in Oral and Maxillofacial Surgery: An Evidence-Based Review. Am. J. Orthod. 2016, 149, 225–237. [Google Scholar] [CrossRef]
- Gráfová, L.; Kašparová, M.; Kakawand, S.; Procházka, A.; Dostálová, T. Study of Edge Detection Task in Dental Panoramic X-ray Images. Dentomaxillofac. Radiol. 2013, 42, 20120391. [Google Scholar] [CrossRef] [PubMed]
- Heinz, J.; Stewart, K.; Ghoneima, A. Evaluation of two-dimensional lateral cephalogram and three-dimensional cone beam computed tomography superimpositions: A comparative study. Int. J. Oral Maxillofac. Surg. 2018, 48, 519–529. [Google Scholar] [CrossRef]
- Kim, D.; Lagravere, M. Assessing the Correlation between Skeletal and Corresponding Soft-Tissue Equivalents to Determine the Relationship between CBCT Skeletal/Dental Dimensions and 3D Radiographic Soft-Tissue Equivalents. Int. J. Dent. 2018, 2018, 8926314. [Google Scholar] [CrossRef] [PubMed]
- Eliášová, H.; Dostálová, T.; Procházka, A.; Šedivá, E.; Horáček, M.; Urbanová, P.; Hlinakova, P. Comparison of 2D OPG Image versus Orthopantomogram from 3D CBCT from the Forensic Point of View. Leg. Med. 2021, 48, 101802. [Google Scholar] [CrossRef]
- Plooij, J.; Maal, T.; Haers, P.; Borstlap, W.; Kuijpers-Jagtman, A.; Berge, S. Digital three-dimensional image fusion processes for planning and evaluating orthodontics and orthognathic surgery: A systematic review. Int. J. Oral Maxillofac. Surg. 2011, 40, 341–352. [Google Scholar] [CrossRef]
- Jarnstedt, J.; Sahlsten, J.; Jaskari, J.; Kaski, K.; Mehtonen, H.; Hietanen, A.; Sundqvist, O.; Varjonen, V.; Mattila, V.; Prapayasatok, S.; et al. Reproducibility analysis of automated deep learning based localisation of mandibular canals on a temporal CBCT dataset. Sci. Rep. 2023, 13, 14159. [Google Scholar] [CrossRef]
- Baan, F.; de Waard, O.; Bruggink, R.; Xi, T.; Ongkosuwito, E.; Maal, T. Virtual setup in orthodontics: Planning and evaluation. Clin. Oral Investig. 2020, 24, 2385–2393. [Google Scholar] [CrossRef] [PubMed]
- Verykokou, S.; Ioannidis, C.; Angelopoulos, C. Evaluation of 3D Modeling Workflows Using Dental CBCT Data for Periodontal Regenerative Treatment. Pers. Med. 2022, 12, 1355. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.; Kharbanda, O.; Balachandran, R.; Sardana, V.; Kalra, S.; Chaurasia, S.; Sardana, H. Precision of manual landmark identification between as-received and oriented volume-rendered cone-beam computed tomography images. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 118–131. [Google Scholar] [CrossRef] [PubMed]
- Weiss, R.; Read-Fuller, A. Cone Beam Computed Tomography in Oral and Maxillofacial Surgery: An Evidence-Based Review. Dent. J. 2019, 7, 52. [Google Scholar] [CrossRef] [PubMed]
- Bookstein, F. Foundations of morphometrics. Annu. Rev. Ecol. Syst. 1982, 13, 451–470. [Google Scholar] [CrossRef]
- Li, J.; Wu, S.; Mei, L.; Wen, J.; Marra, J.; Lei, L.; Li, H. Facial asymmetry of the hard and soft tissues in skeletal Class I, II, and III patients. Sci. Rep. 2024, 14, 4966. [Google Scholar] [CrossRef] [PubMed]
- Nahm, K.; Kim, Y.; Choi, Y.; Lee, J.; Kim, S.; Nelson, G. Accurate registration of cone-beam computed tomography scans to 3-dimensional facial photographs. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 256–264. [Google Scholar] [CrossRef]
- Resnick, C.; Dang, R.; Glick, S.J. Padwa, B. Accuracy of three-dimensional soft tissue prediction for Le Fort I osteotomy using Dolphin 3D software: A pilot study. Int. J. Oral Maxillofac. Surg. 2017, 46, 289–295. [Google Scholar] [CrossRef] [PubMed]
- Ross, A.; Williams, S. Testing repeatability and error of coordinate cranial landmark data acquired from skulls. J. Forensic Sci. 2008, 53, 782–785. [Google Scholar] [CrossRef]
- Mukhia, N.; Birur, N.; Shubhasini, A.; Shubha, G.; Keerthi, G. Dimensional measurement accuracy of 3-dimensional models from cone beam computed tomography using different voxel sizes. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2021, 132, 361–369. [Google Scholar] [CrossRef]
- Tanna, N.; AlMuzaini, A.; Mupparapu, M. Imaging in Orthodontics. Dent. Clin. N. Am. 2021, 65, 623–641. [Google Scholar] [CrossRef] [PubMed]
- Elshebiny, T.; Bous, R.; Withana, T.; Morcos, S.; Valiathan, M. Accuracy of Three-Dimensional Upper Airway Prediction in Orthognathic Patients Using Dolphin Three-Dimensional Software. J. Craniofac. Surg. 2020, 31, 1098–1100. [Google Scholar] [CrossRef] [PubMed]
- Dahiya, N.; Alam, S.; Zhang, P.; Zhang, S.; Li, T.; Yezzi, A.; Nadeem, S. Multitask 3D CBCT-to-CT translation and organs-at-risk segmentation using physics-based data augmentation. Med Phys. 2021, 48, 5130–5141. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Lee, G.; Moon, D.; Yun, K.; Kim, J.; Lee, K. Creation of Digital Virtual Patient by Integrating CBCT, Intraoral Scan, 3D Facial Scan: An Approach to Methodology for Integration Accuracy. J. Craniofacial Surg. 2022, 33, e396–e398. [Google Scholar] [CrossRef] [PubMed]
- Procházka, A.; Vyšata, O.; Mařík, V. Integrating the Role of Computational Intelligence and Digital Signal Processing in Education. IEEE Signal Process. Mag. 2021, 38, 154–162. [Google Scholar] [CrossRef]
- Bora, P.; Agrawal, P.; Bagga, D.; Tiwari, S.; Singh, A. Applications of Cone Beam Computed Tomography in Orthodontics: An Overview. Biosci. Biotechnol. Res. Comm. 2021, 13, 168–172. [Google Scholar] [CrossRef]
- van Bakelen, N.; van der Graaf, J.; Kraeima, J.; Spijkervet, F. Reproducibility of 2D and 3D Ramus Height Measurements in Facial Asymmetry. J. Pers. Med. 2022, 12, 1181. [Google Scholar] [CrossRef] [PubMed]
- Balaji, S. Maxillofacial Surgery and Artificial Intelligence. Ann. Maxillofac. Surg. 2023, 13, 1–2. [Google Scholar] [CrossRef]
- Rasteau, S.; Ernenwein, D.; Savoldelli, C.; Bouletreau, P. Artificial intelligence for oral and maxillo-facial surgery: A narrative review. J. Stomatol. Oral Maxillofac. Surg. 2022, 123, 276–282. [Google Scholar] [CrossRef]


| Measurement | Dataset | N | MEAN | STD | MIN | MAX | t | p-Value | ||
|---|---|---|---|---|---|---|---|---|---|---|
| MEAN | Females | Males | ||||||||
| zy dx-sin | pre | 43 | 6.806 | 6.806 | 105.6 | 135.6 | ||||
| zy dx-sin | post | 43 | 124.630 | 6.339 | 107 | 134.7 | −0.800 | 0.429 | 0.202 | 0.734 |
| mx dx-mx sin | pre | 43 | 60.370 | 4.309 | 49 | 69.4 | ||||
| mx dx-mx sin | post | 44 | 60.602 | 4.946 | 50.2 | 74.6 | −0.484 | 0.631 | 0.903 | 0.443 |
| go dx-go sin | pre | 44 | 95.384 | 6.913 | 84.5 | 109.8 | ||||
| go dx-go sin | post | 44 | 97.311 | 7.215 | 79.1 | 112.1 | −3.935 | 0.001 | 0.033 | 0.004 |
| zy dx-subsp | pre | 3 | 81.551 | 5.591 | 70.1 | 92.8 | ||||
| zy dx-subsp | post | 43 | 82.535 | 5.290 | 68.8 | 90.8 | −1.223 | 0.228 | 0.351 | 0.447 |
| zy sin-subsp | pre | 43 | 80.340 | 6.983 | 59.4 | 92.1 | ||||
| zy sin-subsp | post | 43 | 82.184 | 5.453 | 69.1 | 92.8 | −2.130 | 0.039 | 0.287 | 0.083 |
| mx dx-subsp | pre | 43 | 38.260 | 3.344 | 31.7 | 44.4 | ||||
| mx dx-subsp | post | 44 | 37.814 | 4.367 | 30.3 | 48.4 | 0.847 | 0.402 | 0.306 | 0.809 |
| mx sin-subsp | pre | 43 | 38.793 | 4.099 | 30.2 | 46.2 | ||||
| mx sin-subsp | post | 44 | 38.200 | 3.516 | 31.1 | 45.8 | 1.210 | 0.233 | 0.822 | 0.202 |
| go dx-pog | pre | 44 | 78.445 | 7.550 | 61.3 | 92.9 | ||||
| go dx-pog | post | 43 | 78.942 | 7.355 | 62 | 92.9 | −0.524 | 0.603 | 0.339 | 0.915 |
| go sin-pog | pre | 44 | 78.532 | 7.818 | 58.8 | 92.9 | ||||
| go sin-pog | post | 43 | 79.574 | 7.344 | 60.9 | 90.9 | −1.555 | 0.127 | 0.424 | 0.203 |
| inc dx-go dx | pre | 44 | 43.080 | 6.620 | 32 | 65.1 | ||||
| inc dx-go dx | post | 44 | 42.627 | 4.917 | 36.1 | 53.7 | 0.671 | 0.506 | 0.637 | 0.197 |
| inc sin-go sin | pre | 44 | 41.509 | 5.880 | 34 | 61.4 | ||||
| inc sin-go sin | post | 44 | 41.041 | 4.484 | 34.4 | 49.6 | 0.768 | 0.447 | 0.455 | 0.169 |
| subsp-pog | pre | 29 | 66.907 | 5.609 | 57.2 | 75.3 | ||||
| subsp-pog | post | 27 | 65.300 | 7.866 | 39.6 | 77.3 | 1.271 | 0.215 | 0.622 | 0.266 |
| sto-pog | pre | 29 | 42.790 | 16.587 | 33.7 | 102 | ||||
| sto-pog | post | 27 | 37.648 | 4.557 | 22.5 | 46.8 | 1.742 | 0.093 | 0.43 | 0.085 |
| B-pog | pre | 28 | 20.929 | 2.544 | 13.6 | 25.6 | ||||
| B-pog | post | 25 | 20.616 | 2.828 | 15.7 | 25.3 | 0.486 | 0.631 | 0.927 | 0.297 |
| N | MEAN | STD | t | p | p-pre | p-post | p-female | p-male | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| pre | post | pre | post | |||||||||
| zy dx-subsp | 81.891 | 5.464 | ||||||||||
| zy sin-subsp | 88 | 81.136 | 6.280 | 1.497 | 0.138 | 0.646 | 0.124 | 0.057 | 0.082 | 0.713 | 0.436 | |
| mx dx-subsp | 38.019 | 3.836 | ||||||||||
| mx sin-subsp | 89 | 38.458 | 3.769 | −0.983 | 0.328 | 0.594 | 0.396 | 0.249 | 0.627 | 0.035 | 0.244 | |
| go dx-pog | 78.653 | 7.337 | ||||||||||
| go sin-pog | 89 | 79.022 | 7.478 | −0.639 | 0.525 | 0.479 | 0.928 | 0.462 | 0.468 | 0.398 | 0.108 | |
| inc dx-go dx | 42.650 | 5.897 | ||||||||||
| inc sin-go sin | 90 | 41.070 | 5.330 | 4.442 | 0.000 | 0.001 | 0.006 | 0.135 | 0.014 | 0.022 | 0.020 | |
| Signed Post-to-Preoperative Differences | Absolute Post-to-Pre Operative Differences | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| MEAN | Sth | Z | p -Value | MEAN | Sth | Z | p -Value | ||
| zy dx-sin | 0.256 | 2.042 | 0.871 | 0.384 | 1.364 | 1.528 | −0.794 | 0.427 | |
| mx dx-sin | 0.164 | 3.148 | −0.800 | 0.424 | 2.148 | 2.284 | 0.062 | 0.951 | |
| go dx-go sin | 1.983 | 3.394 | −0.310 | 0.756 | 3.079 | 2.417 | −0.286 | 0.775 | |
| zy dx-subsp | 0.892 | 4.752 | 0.000 | 1.000 | 3.545 | 3.244 | 0.077 | 0.939 | |
| zy sin-subsp | 2.275 | 6.797 | 0.179 | 0.858 | 5.313 | 4.753 | 1.717 | 0.086 * | |
| mx dx-subsp | −1.492 | 9.475 | −0.935 | 0.350 | 7.020 | 6.449 | −0.148 | 0.883 | |
| mx sin-subsp | −1.581 | 9.241 | 0.972 | 0.331 | 7.557 | 5.430 | 0.406 | 0.685 | |
| go dx-pog | 0.530 | 6.275 | 1.006 | 0.314 | 4.424 | 4.429 | 1.180 | 0.238 | |
| go sin-pog | 1.370 | 5.919 | 0.708 | 0.479 | 4.083 | 4.459 | 1.925 | 0.054 * | |
| inc dx-go dx | −0.590 | 9.572 | 1.611 | 0.107 | 6.660 | 6.825 | −1.540 | 0.124 | |
| inc sin-go sin | −0.792 | 9.299 | 0.991 | 0.322 | 6.731 | 6.384 | −0.465 | 0.642 | |
| subsp-pog | −3.006 | 12.271 | 0.370 | 0.711 | 5.523 | 11.326 | 0.025 | 0.980 | |
| sto-pog | −2.986 | 11.218 | 1.702 | 0.089 * | 5.515 | 10.175 | −1.850 | 0.064 * | |
| B-pog | −1.053 | 9.678 | 0.139 | 0.890 | 7.649 | 5.821 | 2.746 | 0.006 ** | |
| PD | Total | Females | Males |
|---|---|---|---|
| Min | 0.022 | 0.022 | 0.049 |
| Max | 0.168 | 0.154 | 0.168 |
| Mean | 0.093 | 0.094 | 0.092 |
| SD | 0.034 | 0.037 | 0.033 |
| Median | 0.090 | 0.101 | 0.084 |
| Minimum | Mean | SD | Maximum | |
|---|---|---|---|---|
| or dx | 0.765 | 5.263 | 3.406 | 14.082 |
| or sin | 0.847 | 4.505 | 3.342 | 14.580 |
| zy dx | 0.412 | 5.336 | 3.833 | 16.187 |
| zy sin | 0.370 | 4.824 | 4.603 | 20.705 |
| go dx | 0.865 | 4.217 | 3.054 | 16.695 |
| go sin | 0.260 | 3.762 | 2.596 | 10.476 |
| al dx | 0.796 | 4.279 | 3.358 | 15.177 |
| al sin | 0.332 | 4.672 | 4.029 | 17.483 |
| ns | 0.824 | 4.408 | 2.413 | 10.336 |
| inc | 0.908 | 5.466 | 4.784 | 25.609 |
| pg | 0.347 | 3.456 | 2.272 | 10.589 |
| gn | 0.487 | 3.930 | 2.467 | 11.830 |
| Males | Females | Total | ||
|---|---|---|---|---|
| RMS | means | 2.090 | 1.582 | 1.813 |
| SD | 0.367 | 0.220 | 0.385 | |
| min | 1.719 | 1.293 | 1.293 | |
| max | 2.610 | 1.959 | 2.610 | |
| PERC75 | means | 2.137 | 1.767 | 1.935 |
| SD | 0.251 | 0.239 | 0.302 | |
| min | 1.950 | 1.457 | 1.457 | |
| max | 2.533 | 2.184 | 2.533 | |
| PDs | means | 18.859 | 15.225 | 17.987 |
| SD | 0.933 | 1.085 | 0.810 | |
| min | 14.086 | 10.929 | 10.929 | |
| max | 26.869 | 18.697 | 26.869 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dostalova, T.; Eliasova, H.; Prochazka, A.; Nocar, A.; Urbanova, P. Imaging and 3D Analysis Based on Two or More Three-Dimensional CBCT Recordings before and after Orthodontic Treatment and Maxillofacial Therapy. Appl. Sci. 2024, 14, 4829. https://doi.org/10.3390/app14114829
Dostalova T, Eliasova H, Prochazka A, Nocar A, Urbanova P. Imaging and 3D Analysis Based on Two or More Three-Dimensional CBCT Recordings before and after Orthodontic Treatment and Maxillofacial Therapy. Applied Sciences. 2024; 14(11):4829. https://doi.org/10.3390/app14114829
Chicago/Turabian StyleDostalova, Tatjana, Hana Eliasova, Ales Prochazka, Adam Nocar, and Petra Urbanova. 2024. "Imaging and 3D Analysis Based on Two or More Three-Dimensional CBCT Recordings before and after Orthodontic Treatment and Maxillofacial Therapy" Applied Sciences 14, no. 11: 4829. https://doi.org/10.3390/app14114829
APA StyleDostalova, T., Eliasova, H., Prochazka, A., Nocar, A., & Urbanova, P. (2024). Imaging and 3D Analysis Based on Two or More Three-Dimensional CBCT Recordings before and after Orthodontic Treatment and Maxillofacial Therapy. Applied Sciences, 14(11), 4829. https://doi.org/10.3390/app14114829








