Virtual Reality Training Affects Center of Pressure (COP)-Based Balance Parameters in Older Individuals
Abstract
:1. Introduction
2. Materials and Methods
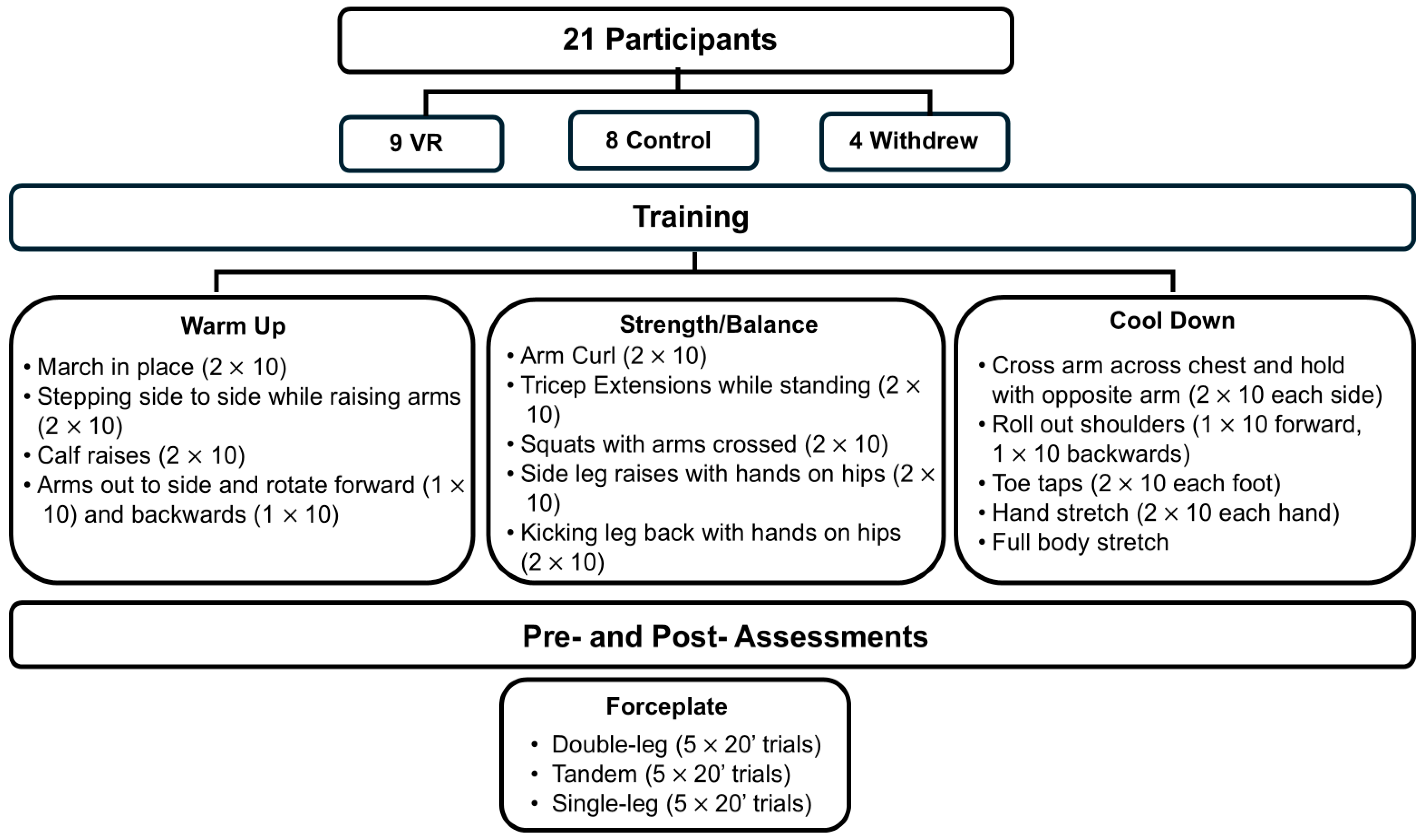
2.1. Study Overview
2.1.1. Participants
2.1.2. Training
2.1.3. Pre- and Post-Training Assessments
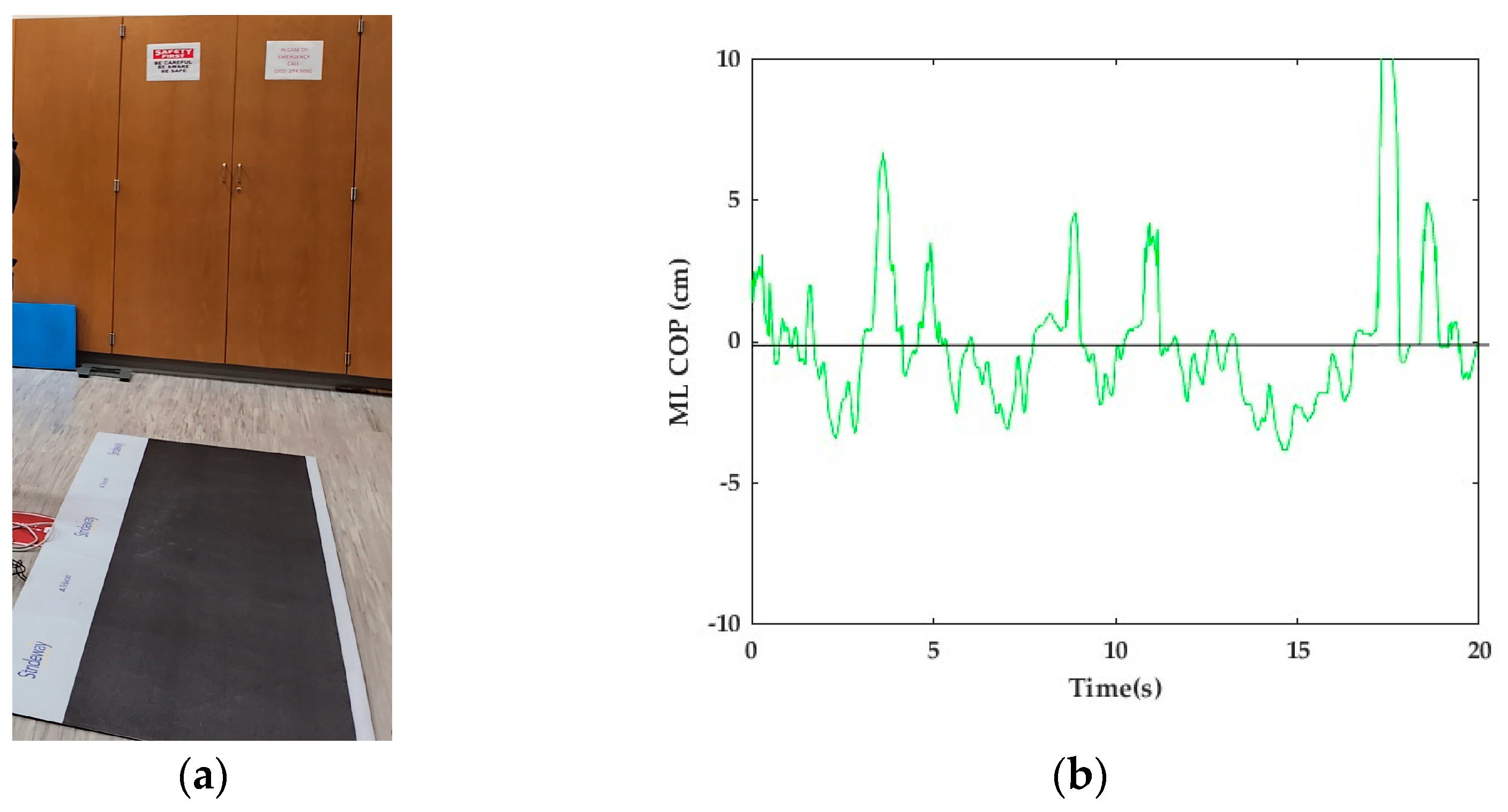
2.2. Analysis
2.2.1. COP Parameters
2.2.2. Statistical Analysis
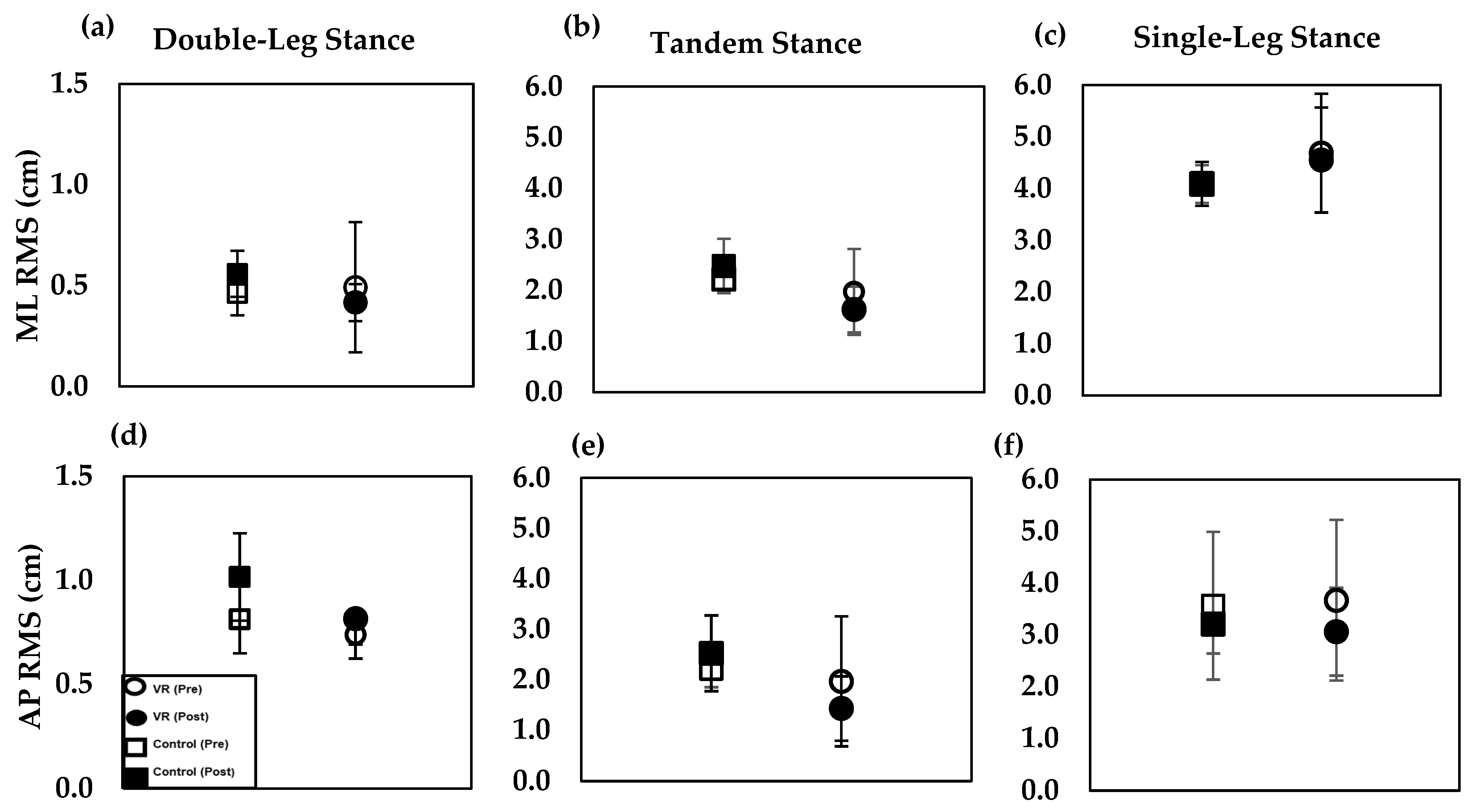
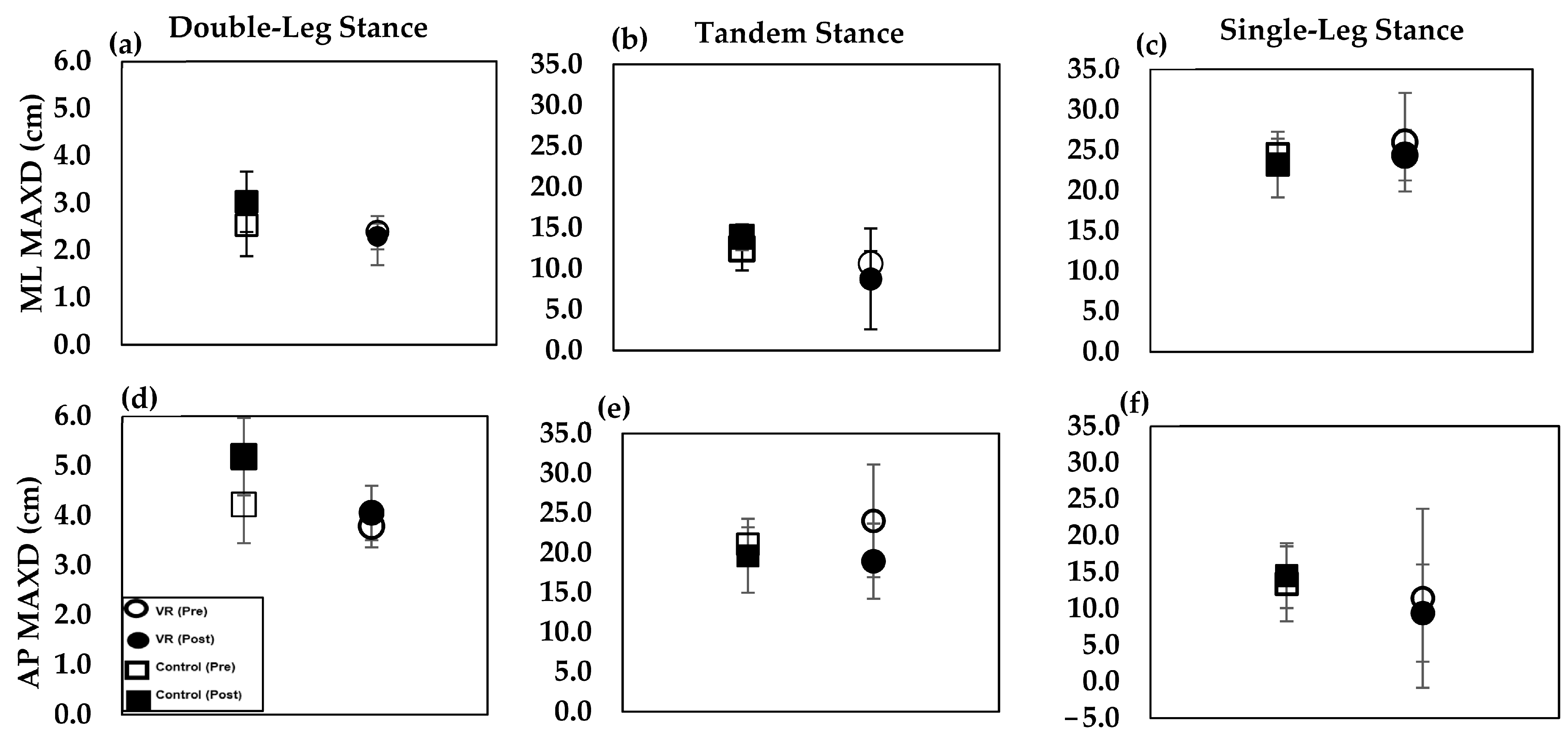
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bergen, G.; Stevens, M.R.; Burns, E.R. Falls and Fall Injuries among Adults Aged ≥ 65 Years—United States, 2014. MMWR Morb. Mortal. Wkly. Rep. 2019, 65, 993–998. [Google Scholar] [CrossRef]
- Soomar, S.M.; Dhalla, Z. Injuries and Outcomes Resulting Due to Falls in Elderly Patients Presenting to the Emergency Department of a Tertiary Care Hospital—A Cohort Study. BMC Emerg. Med. 2023, 23, 14. [Google Scholar]
- Liu, S.W.; Obermeyer, Z.; Chang, Y.; Shankar, K.N. Frequency of ED Revisits and Death among Older Adults after a Fall. Am. J. Emerg. Med. 2015, 33, 1012–1018. [Google Scholar] [CrossRef] [PubMed]
- Sterling, D.A.; O’Connor, J.A.; Bonadies, J. Geriatric Falls: Injury Severity Is High and Disproportionate to Mechanisn. J. Trauma Acute Care Surg. 2001, 50, 116–119. [Google Scholar] [CrossRef]
- Stel, V.S.; Smit, J.H.; Pluijm, S.M.F.; Lips, P. Balance and Mobility Performance as Treatable Risk Factors for Recurrent Falling in Older Persons. J. Clin. Epidemiol. 2003, 56, 659–668. [Google Scholar] [CrossRef] [PubMed]
- Gillespie, L.D.; Robertson, M.C.; Gillespie, W.J.; Sherrington, C.; Gates, S.; Clemson, L.M.; Lamb, S.E. Interventions for Preventing Falls in Older People Living in the Community. Cochrane Database Syst. Rev. 2012, 2012, CD007146. [Google Scholar] [PubMed]
- Overstall, P.W.; Exton-Smith, A.N.; Imms, F.J.; Johnson, A.L. Falls in the elderly related to postural imbalance. Br. Med. J. 1977, 1, 261–264. [Google Scholar] [CrossRef] [PubMed]
- Judge, J.O.; Lindsey, C.; Underwood, M.; Winsemius, D.; Keshner, E.A. Balance Improvements in Older Women: Effects of Exercise Training. Phys. Ther. 1993, 73, 254–265. [Google Scholar] [CrossRef]
- Barnett, A.; Smith, B.; Lord, S.R.; Williams, M.; Baumand, A. Community-Based Group Exercise Improves Balance and Reduces Falls in at-Risk Older People: A Randomised Controlled Trial. Age Aging 2003, 32, 407–414. [Google Scholar] [CrossRef]
- Crilly, R.G.; Willems, D.A.; Trenholm, K.J.; Hayes, K.C.; Delaquerriere-Richardson, L.F.O. Effect of Exercise on Postural Sway in the Elderly. Gerontology 1989, 35, 137–143. [Google Scholar] [CrossRef]
- Phu, S.; Vogrin, S.; Al Saedi, A.; Duque, G. Balance Training Using Virtual Reality Improves Balance and Physical Performance in Older Adults at High Risk of Falls. Clin. Interv. Aging 2019, 14, 1567–1577. [Google Scholar] [CrossRef] [PubMed]
- Hornbrook, M.C.; Stevens, V.J.; Wingfield, D.J.; Hollis, J.F.; Greenlick, M.R.; Ory, M.G. Preventing Falls Among Community-Dwelling Older Persons: Results From a Randomized Trial. Gerontologist 1994, 34, 16–23. [Google Scholar] [CrossRef] [PubMed]
- Wilson, O.; Arnold, N.; Thompson, L.A. Investigating the Effects of Virtual Reality-Based Training on Balance Ability and Balance Confidence in Older Individuals. Appl. Sci. 2024, 14, 4581. [Google Scholar] [CrossRef]
- Lee, Y.; Choi, W.; Lee, K.; Song, C.; Lee, S. Virtual Reality Training With Three-Dimensional Video Games Improves Postural Balance and Lower Extremity Strength in Community-Dwelling Older Adults. J. Aging Phys. Ther. 2015, 25, 621–627. [Google Scholar] [CrossRef]
- Rebêlo, F.L.; de Souza Silva, L.F.; Doná, F.; Barreto, A.S.; Quintans, J.D.S.S. Immersive Virtual Reality Is Effective in the Rehabilitation of Older Adults with Balance Disorders: A Randomized Clinical Trial. Exp. Gerontol. 2021, 149, 111308. [Google Scholar] [CrossRef]
- Kamińska, M.S.; Miller, A.; Rotter, I.; Szylińska, A.; Grochans, E. The Effectiveness of Virtual Reality Training in Reducing the Risk of Falls among Elderly People. Clin. Interv. Aging 2018, 13, 2329–2338. [Google Scholar] [CrossRef] [PubMed]
- Duque, G.; Boersma, D.; Loza-Diaz, G.; Hassan, S.; Suarez, H.; Geisinger, D.; Suriyaarachchi, P.; Sharma, A.; Demontiero, O. Effects of Balance Training Using a Virtual-Reality System in Older Fallers. Clin. Interv. Aging 2013, 8, 257–263. [Google Scholar] [CrossRef] [PubMed]
- Prieto, T.E.; Myklebust, J.B.; Hoffmann, R.G.; Lovett, E.G.; Myklebust, B.M. Measures of Postural Steadiness: Differences between Healthy Young and Elderly Adults. IEEE Trans. Biomed. Eng. 1996, 43, 956–966. [Google Scholar] [CrossRef]
- Podsiadlo, D.; Richardson, S. The Timed ‘Up & Go’: A Test of Basic Functional Mobility for Frail Elderly Persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Almagro, D.; Achalandabaso-Ochoa, A.; Ibáñez-Vera, A.J.; Góngora-Rodríguez, J.; Rodríguez-Huguet, M. Effectiveness of Virtual Reality Therapy on Balance and Gait in the Elderly: A Systematic Review. Healthcare 2024, 12, 158. [Google Scholar] [CrossRef]
- Yesilyaprak, S.; Yildirim, M.; Tomruk, M.; Ertekin, O.; Algun, Z. Comparison of the Effects of Virtual Reality-Based Balance Exercises and Conventional Exercises on Balance and Fall Risk in Older Adults Living in Nursing Homes in Turkey. Physiother. Theory Pract. 2016, 32, 191–201. [Google Scholar] [CrossRef] [PubMed]
- YouTube. National Institutes on Aging, 2016. 15-Minute Workout for Older Adults. 2016. Available online: https://www.youtube.com/watch?v=Ev6yE55kYGw (accessed on 24 July 2024).
- Balance Error Scoring System (BESS). APTA [Online]. Available online: https://www.apta.org/patient-care/evidence-based-practice-resources/test-measures/balance-error-scoring-system-bess (accessed on 3 May 2024).
- Moiz, J.A.; Bansal, V.; Noohu, M.M.; Gaur, S.N.; Hussain, M.E.; Anwer, S.; Alghadir, A. Activities-Specific Balance Confidence Scale for Predicting Future Falls in Indian Older Adults. Clin. Interv. Aging 2017, 12, 645–651. [Google Scholar] [CrossRef] [PubMed]
- Köpke, S.; Meyer, G. The Tinetti Test: Babylon in Geriatric Assessment. Z. Gerontol. Geriatr. 2006, 39, 288–291. [Google Scholar] [CrossRef] [PubMed]
- Yesavage, J.A. Geriatric Depression Scale. Psychopharmacol. Bull. 1988, 24, 709–710. [Google Scholar] [PubMed]
- Lakens, D. Calculating and Reporting Effect Sizes to Facilitate Cumulative Science: A Practical Primer for t-Tests and ANOVAs. Front. Psychol. 2013, 4, 863. [Google Scholar] [CrossRef] [PubMed]
- Lee, K. Virtual Reality Gait Training to Promote Balance and Gait among Older People: A Randomized Clinical Trial. Geriatrics 2021, 6, 1. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H.; Cho, S.H. Benefits of Virtual Reality Program and Motor Imagery Training on Balance and Fall Efficacy in Isolated Older Adults: A Randomized Controlled Trial. Medicina 2022, 58, 1545. [Google Scholar] [CrossRef] [PubMed]
- Babadi, S.Y.; Daneshmandi, H. Effects of Virtual Reality versus Conventional Balance Training on Balance of the Elderly. Exp. Gerontol. 2021, 153, 111498. [Google Scholar] [CrossRef]
- Ren, Y.; Lin, C.; Zhou, Q.; Yingyuan, Z.; Wang, G.; Lu, A. Effectiveness of Virtual Reality Games in Improving Physical Function, Balance and Reducing Falls in Balance-Impaired Older Adults: A Systematic Review and Meta-Analysis. Arch. Gerontol. Geriatr. 2023, 108, 104924. [Google Scholar] [CrossRef]

| Medical Conditions | Physical Abilities | Visual Abilities | |||||||||||
| Subject | Age | Gender | Ethnicity | Traumatic Brain Injury | Dizziness/ Vertigo | Other | Previous Falls | Meds Cause Dizziness/Loss of Balance | Exercise | Physical Limitations | Perceived Fitness Level (10 = most, 1 = least) | Glasses | Vision Loss |
| VR1 | 73 | M | Caucasian | No | No | LTKR, lumbar spinal fusion | No | Yes | Yes (bike, swim, weights, stretch) | No | 10 | Yes | No |
| VR2 | 82 | F | Caucasian | No | No | No | No | Y (Lunesta) | Yes (4/wk, walk, yoga, weights) | No | 10 | No | No |
| VR3 | 78 | F | Caucasian | No | No | Arthritis (hips/back) | No | No | NA | NA | NA | NA | NA |
| VR4 | 76 | F | Caucasian | No | No | No | No | No | Yes (walk, weights, stretch) | No | 6 | Yes | No |
| VH5 | 77 | F | Caucasian | No | No | No | No | No | Yes(walking) | Left shoulder issues | 7 | Yes | No |
| VR6 | 72 | F | Black/African American | No | No | No | Yes (trip and fall of step) | No | Yes (Bike 6/wk, strength and stretch 2) | No | 6 | Yes | No |
| VR7 | NA | F | Caucasian | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| VR8 | 78 | F | Caucasian | No | No | Mid-low back if sit too long | No | No | Yes (walk, 10 k steps/day, sometimes bike) | No | 6 | Yes | No |
| VR9 | 71 | M | Caucasian | No | No | No | No | Yes (metformin, metoprolol) | Yes (6–7 days/wk of walking) | No | 7 | No | No |
| C1 | 78 | F | Caucasian | No | No | No | No | No | Yes (walk several/wk) | No | 6 | Yes | No |
| Medical Conditions | Physical Abilities | Visual Abilities | |||||||||||
| Subject | Age | Gender | Ethnicity | Traumatic Brain Injury | Dizziness/ Vertigo | Other | Previous Falls | Meds Cause Dizziness/Loss of Balance | Exercise | Physical Limitations | Perceived Fitness Level (10 = most, 1 = least) | Glasses | Vision Loss |
| C2 | 79 | F | Caucasian | No | No | Osteo porosis | Yes (once 2 month ago) | No | Yes (2/wk) | NA | 6 | Yes (post-cataract surgery) | No |
| C3 | 82 | F | Caucasian | No | No | No | Yes (on ice 3 years ago) | No | Yes (bike, walk, weights) | No | 9 | Yes (post-cataract surgery) | No |
| C4 | 80 | F | Caucasian | No | No | No | Yes (trip and fall while walking) | No | Yes (walk, weights, bike) | No | 10 | No (cataract surgery 5 years ago | No |
| C5 | 78 | F | Caucasian | No | No | No | No | No | (Yes, walking, bike) | No | 6 | Yes | No |
| C6 | 62 | F | Black/African American | No | Yes | Osteoarthritis | No | No | Yes (5 + days, pool/other) | No | 7 | Yes | No |
| C7 | 73 | F | Black/African American | No | No | No | No | No | Yes(5/wk) | NA | 6 | NA | No |
| C8 | 69 | F | Caucasian | No | No | No | No | No | Yes (4–5 days/wk, boxing, swimming, gym workout) | No | 9 | Yes | No |
| W | 78 | F | Moroccan | NA | No | No | No | No | Yes (walking) | NA | NA | Yes | No |
| W | 72 | F | Caucasian | No | No | No | Yes (trip and fall off step) | No | Yes (Bike 6/wk, strength and stretch 2/wk) | No | 6 | Yes | No |
| W | NA | F | Black/African American | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| W | 83 | M | Caucasian | No | No | NA | Yes (trip, broke nose, 1 month ago) | No | No (last time 2 years ago) | No | 4 | Yes | No |
| Control | VR | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | ||||||||||
| Double | Tandem | Single | Double | Tandem | Single | Double | Tandem | Single | Double | Tandem | Single | ||
| RMS (cm) | ML | 0.46(0.11) | 2.22(0.27) | 4.09(0.37) | 0.56(0.11) | 2.48(0.52) | 4.09(0.42) | 0.49(0.32) | 1.97(0.84) | 4.68(1.1) | 0.42(0.09) | 1.62(0.44) | 4.55(1.0) |
| AP | 0.81(0.17) | 2.22(0.37) | 3.56(1.4) | 1.02(0.21) | 2.53(0.69) | 3.21(0.57) | 0.74(0.11) | 1.97(1.3) | 3.67(1.5) | 0.82(0.11) | 1.43(0.63) | 3.06(0.85) | |
| MAXD (cm) | ML | 2.53(0.65) | 12.4(1.9) | 24.5(2.6) | 3.03(0.64) | 13.9(4.0) | 23.2(1.6) | 2.40(0.33) | 10.6(6.1) | 26.0(6.0) | 2.29(0.67) | 8.74(3.0) | 24.3(6.0) |
| AP | 4.22(0.78) | 13.4(2.1) | 21.1(5.1) | 5.19(0.78) | 14.5(4.7) | 19.6(4.5) | 3.79(0.42) | 11.4(7.1) | 24.0(11) | 5.31(6.2) | 9.38(4.6) | 18.9(6.4) | |
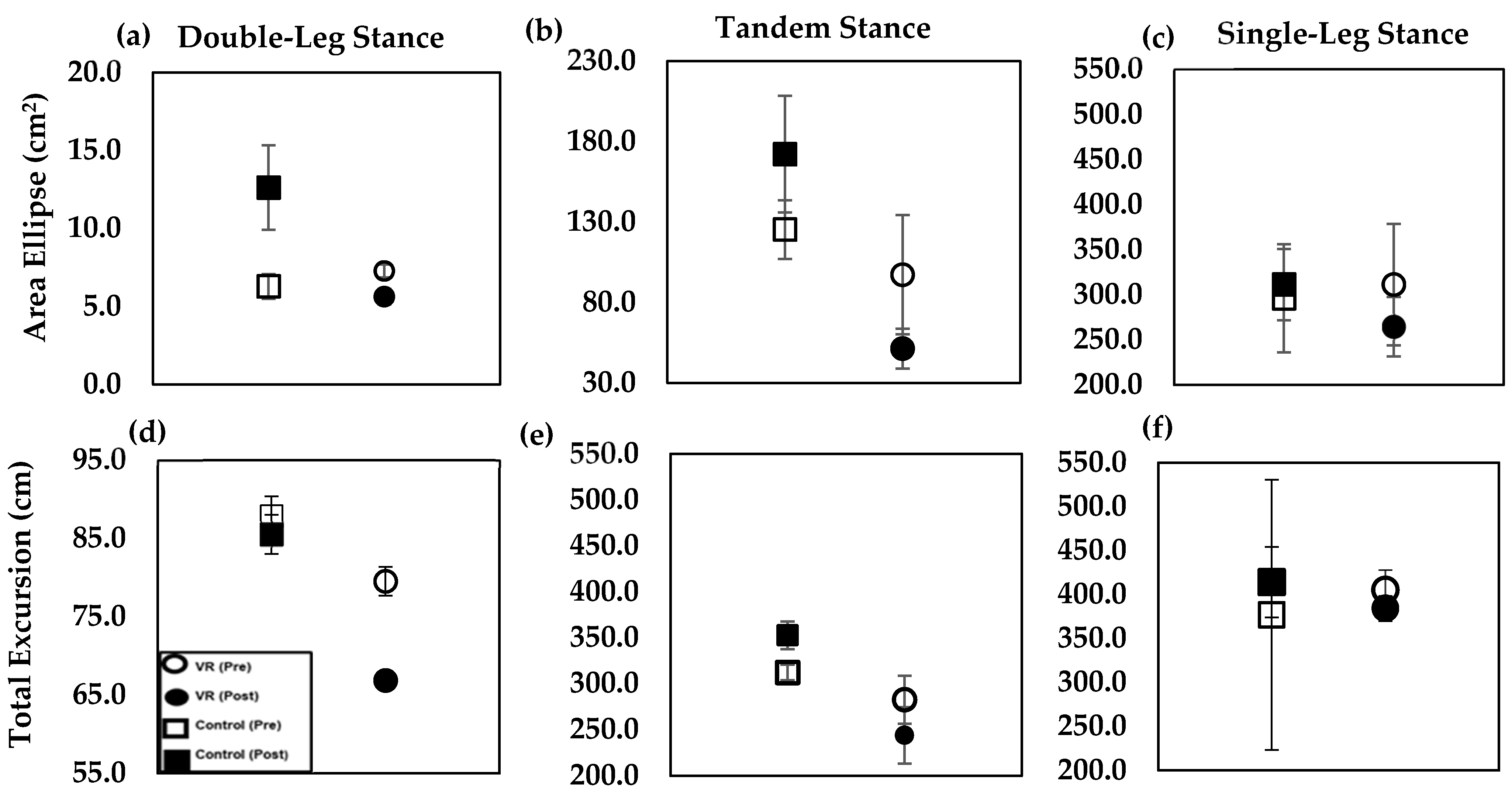
| AE (cm2) | 6.30(2.3) | 125(51) | 296(170) | 12.6(6.4) | 172(102) | 265(84) | 5.51(1.2) | 97.2(107) | 311(165) | 5.62(1.4) | 51.4(35) | 238(93) | |
| TE (cm) | 87.8(7.3) | 312(24) | 377(18) | 85.5(5.8) | 353(43) | 414(51) | 79.5(5.8) | 283(75) | 405(65) | 66.8(3.4) | 244(40) | 384(40) | |
| Control | VR | ||||||
|---|---|---|---|---|---|---|---|
| Cohen’s d | Cohen’s d | ||||||
| Double | Tandem | Single | Double | Tandem | Single | ||
| RMS (cm) | ML | 0.51 | 0.16 | −0.19 | 0.32 | −0.46 | −0.64 |
| AP | 0.53 | 0.16 | −0.04 | −0.41 | −0.42 | −0.07 | |
| MAXD (cm) | ML | 0.29 | 0.11 | −0.09 | 0.26 | −0.31 | −0.62 |
| AP | 0.44 | 0.14 | −0.13 | −0.13 | −0.37 | −0.40 | |
| AE (cm2) | 0.79 | 0.19 | −0.14 | 0.04 | −0.63 | −0.73 | |
| TE (cm) | −0.08 | 0.20 | −0.06 | −0.77 | −0.29 | 0.20 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arnold, N.; Wilson, O.; Thompson, L. Virtual Reality Training Affects Center of Pressure (COP)-Based Balance Parameters in Older Individuals. Appl. Sci. 2024, 14, 7182. https://doi.org/10.3390/app14167182
Arnold N, Wilson O, Thompson L. Virtual Reality Training Affects Center of Pressure (COP)-Based Balance Parameters in Older Individuals. Applied Sciences. 2024; 14(16):7182. https://doi.org/10.3390/app14167182
Chicago/Turabian StyleArnold, Nicole, Oshin Wilson, and Lara Thompson. 2024. "Virtual Reality Training Affects Center of Pressure (COP)-Based Balance Parameters in Older Individuals" Applied Sciences 14, no. 16: 7182. https://doi.org/10.3390/app14167182






