Mechanical Assessment of CAD/CAM Fabricated Hybrid Ceramics: An In Vitro Study
Abstract
:1. Introduction
2. Literature Review
3. Materials and Methods
3.1. Sample Size Calculation
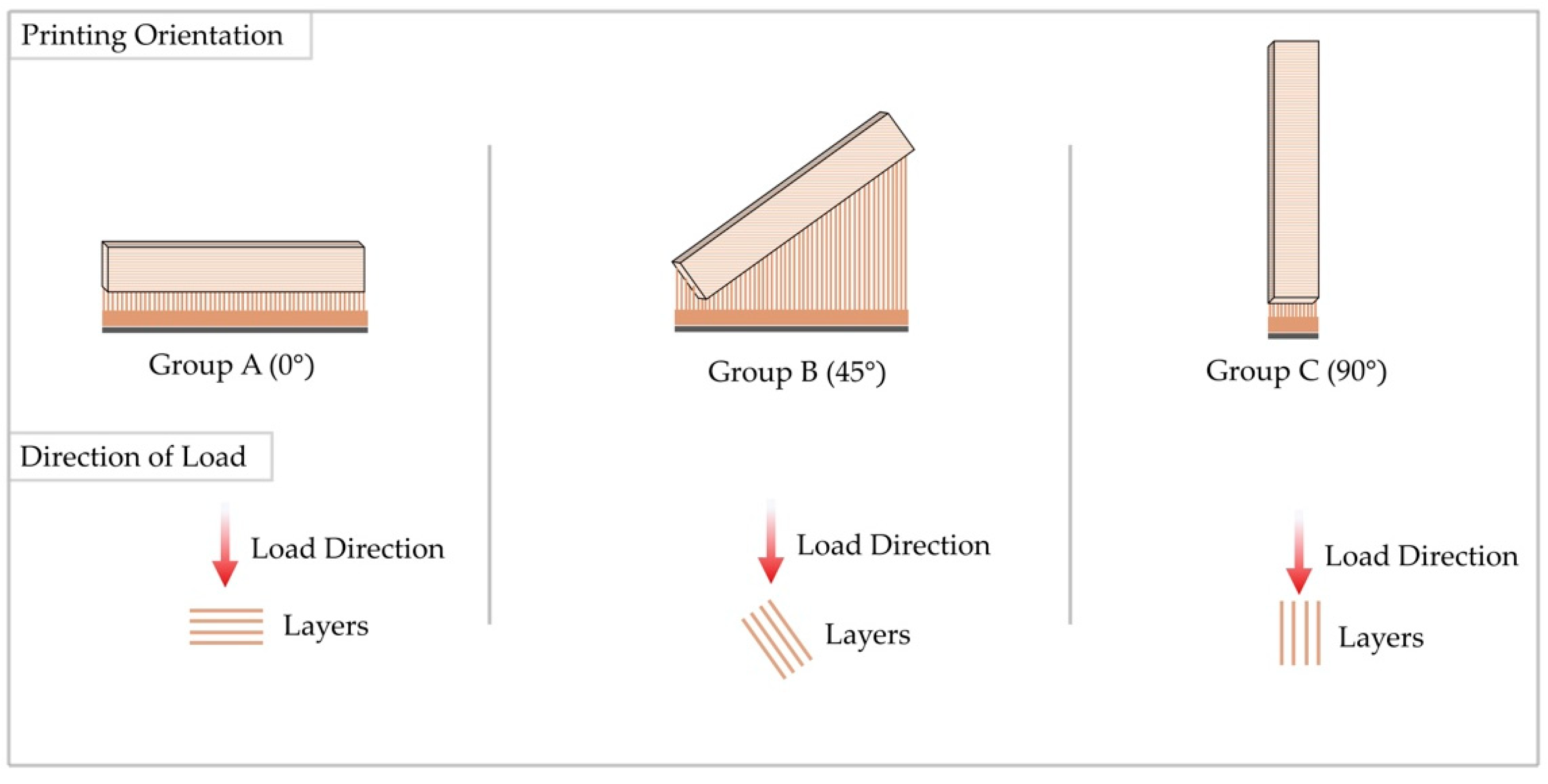
3.2. Study Design
3.3. Samples Preparation
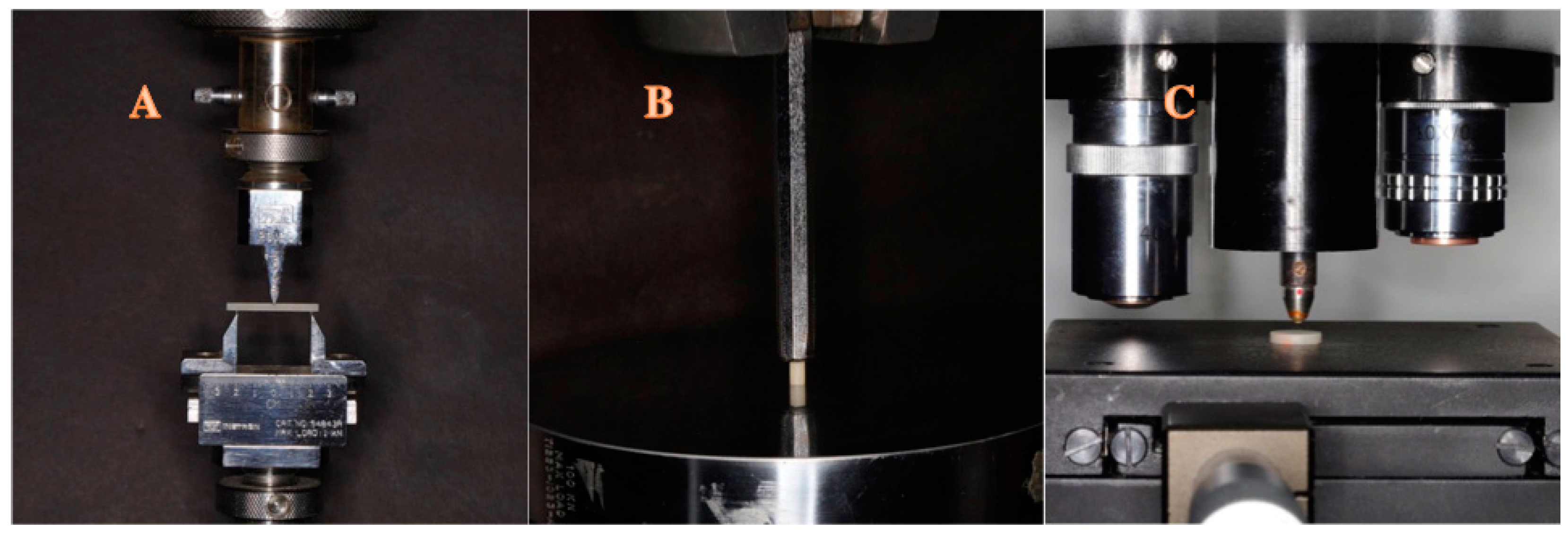
3.4. Samples Testing
3.5. Statistical Analysis
4. Results
4.1. Flexural Strength Test
4.2. Compressive Strength Test
4.3. Vickers Hardness Test
5. Discussion
6. Conclusions
- The subtractive group achieved ISO specifications in terms of flexural strength. This group was superior to additive groups in hardness while exhibiting lower performance in compressive strength;
- Printing orientation had a significant influence on the performance of additive groups. Flexural strength and hardness were improved when the printing orientation was in alignment with the direction of load (90°), while compressive strength was improved when the printing orientation was perpendicular to the direction of load (0°);
- Polishing did not significantly improve the hardness values of the subtractive group;
- Additive groups’ hardness values were significantly improved post-polishing, highlighting its importance for 3D-printed restorations.
7. Clinical Significance
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dawood, A.; Marti, B.M.; Sauret-Jackson, V.; Darwood, A. 3D printing in dentistry. Bri. Dent. J. 2015, 219, 521–529. [Google Scholar]
- Abduo, J.; Lyons, K.; Bennamoun, M. Trends in computer-aided manufacturing in prosthodontics: A review of the available streams. Int. J. Dent. 2014, 2014, 783948. [Google Scholar] [CrossRef] [PubMed]
- Moon, W.; Kim, S.; Lim, B.-S.; Park, Y.-S.; Kim, R.J.-Y.; Chung, S.H. Dimensional accuracy evaluation of temporary dental restorations with different 3D printing systems. Materials 2021, 14, 1487. [Google Scholar] [CrossRef]
- Kantaros, A.; Ganetsos, T.; Piromalis, D. 3D and 4D printing as integrated manufacturing methods of industry 4.0. Am. J. Appl. Sci. 2023, 16, 12–22. [Google Scholar] [CrossRef]
- Stawarczyk, B.; Liebermann, A.; Eichberger, M.; Güth, J.-F. Evaluation of mechanical and optical behavior of current esthetic dental restorative CAD/CAM composites. J. Mech. Behav. Biomed. Mater. 2016, 55, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Oouchi, H.; Takamizawa, T.; Tamura, T.; Ishii, R.; Tsujimoto, A.; Miyazaki, M.; Kitahara, N. Flexural properties and wear behavior of computer-aided design/computer-aided manufacturing resin blocks. Dent. Mater. J. 2021, 40, 979–985. [Google Scholar] [CrossRef]
- Alharbi, A.; Ardu, S.; Bortolotto, T.; Krejci, I. Stain susceptibility of composite and ceramic CAD/CAM blocks versus direct resin composites with different resinous matrices. Odontology 2017, 105, 162–169. [Google Scholar] [CrossRef]
- He, L.-H.; Purton, D.; Swain, M. A novel polymer infiltrated ceramic for dental simulation. J. Mater. Sci. Mater. Med. 2011, 22, 1639–1643. [Google Scholar] [CrossRef]
- Zimmermann, M.; Mehl, A.; Reich, S. New CAD/CAM materials and blocks for chairside procedures. Int. J. Comput. Dent. 2013, 16, 173–181. [Google Scholar]
- Kessler, A.; Reymus, M.; Hickel, R.; Kunzelmann, K.-H. Three-body wear of 3D printed temporary materials. Dent. Mater. 2019, 35, 1805–1812. [Google Scholar] [CrossRef]
- Kihara, H.; Sugawara, S.; Yokota, J.; Takafuji, K.; Fukazawa, S.; Tamada, A.; Hatakeyama, W.; Kondo, H. Applications of three-dimensional printers in prosthetic dentistry. J. Oral Sci. 2021, 63, 212–216. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, M.; Ender, A.; Egli, G.; Özcan, M.; Mehl, A. Fracture load of CAD/CAM-fabricated and 3D-printed composite crowns as a function of material thickness. Clin. Oral Investig. 2019, 23, 2777–2784. [Google Scholar] [CrossRef]
- Zimmermann, M.; Ender, A.; Attin, T.; Mehl, A. Fracture load of three-unit full-contour fixed dental prostheses fabricated with subtractive and additive CAD/CAM technology. Clin. Oral Investig. 2020, 24, 1035–1042. [Google Scholar] [CrossRef]
- Zimmermann, M.; Egli, G.; Zaruba, M.; Mehl, A. Influence of material thickness on fractural strength of CAD/CAM fabricated ceramic crowns. Dent. Mater. J. 2017, 36, 778–783. [Google Scholar] [CrossRef] [PubMed]
- Della Bona, A.; Cantelli, V.; Britto, V.T.; Collares, K.F.; Stansbury, J.W. 3D printing restorative materials using a stereolithographic technique: A systematic review. Dent. Mater. 2021, 37, 336–350. [Google Scholar] [CrossRef]
- Dimitrov, D.; Schreve, K.; de Beer, N. Advances in three dimensional printing–state of the art and future perspectives. Prototyp. J. 2006, 12, 136–147. [Google Scholar] [CrossRef]
- Alharbi, N.; Osman, R.; Wismeijer, D. Effects of build direction on the mechanical properties of 3D-printed complete coverage interim dental restorations. J. Prosthet. Dent. 2016, 115, 760–767. [Google Scholar] [CrossRef]
- Mueller, J.; Shea, K. The effect of build orientation on the mechanical properties in inkjet 3D printing. UT. Austin 2015. Available online: https://hdl.handle.net/2152/89394 (accessed on 29 July 2024).
- Keßler, A.; Hickel, R.; Ilie, N. In vitro investigation of the influence of printing direction on the flexural strength, flexural modulus and fractographic analysis of 3D-printed temporary materials. Dent. Mater. J. 2021, 40, 641–649. [Google Scholar] [CrossRef]
- Cazzaniga, G.; Ottobelli, M.; Ionescu, A.C.; Paolone, G.; Gherlone, E.; Ferracane, J.L.; Brambilla, E. In vitro biofilm formation on resin-based composites after different finishing and polishing procedures. J. Dent. 2017, 67, 43–52. [Google Scholar] [CrossRef]
- Ruse, N.; Sadoun, M. Resin-composite blocks for dental CAD/CAM applications. J. Dent. Res. 2014, 93, 1232–1234. [Google Scholar] [CrossRef]
- Block, P.M. Technical Product Profile; 3M ESPE: St. Paul, MN, USA, 2000. [Google Scholar]
- Lava Ultimate, C. CAM Restorative Technical Product Profile; 3M ESPE: St. Paul, MN, USA, 2011. [Google Scholar]
- Ling, L.; Ma, Y.; Malyala, R. A novel CAD/CAM resin composite block with high mechanical properties. Dent. Mater. 2021, 37, 1150–1155. [Google Scholar] [CrossRef] [PubMed]
- Della Bona, A.; Corazza, P.H.; Zhang, Y. Characterization of a polymer-infiltrated ceramic-network material. Dent. Mater. 2014, 30, 564–569. [Google Scholar] [CrossRef] [PubMed]
- Zahnfabrik, V. VITA ENAMIC Technical and Scientific Documentation; VITA Zahnfabrik: Bad Sackingen, Germany, 2019. [Google Scholar]
- Kantaros, A.; Petrescu, F.I.T.; Abdoli, H.; Diegel, O.; Chan, S.; Iliescu, M.; Ganetsos, T.; Munteanu, I.S.; Ungureanu, L.M. Additive Manufacturing for Surgical Planning and Education: A Review. Appl. Sci. 2024, 14, 2550. [Google Scholar] [CrossRef]
- Kantaros, A.; Soulis, E.; Ganetsos, T.; Petrescu, F.I.T. Applying a combination of cutting-edge industry 4.0 processes towards fabricating a customized component. Processes 2023, 11, 1385. [Google Scholar] [CrossRef]
- Strub, J.R.; Rekow, E.D.; Witkowski, S. Computer-aided design and fabrication of dental restorations: Current systems and future possibilities. J. Am. Dent. Assoc. 2006, 137, 1289–1296. [Google Scholar] [CrossRef]
- Salmi, M.; Paloheimo, K.-S.; Tuomi, J.; Ingman, T.; Mäkitie, A. A digital process for additive manufacturing of occlusal splints: A clinical pilot study. J. R. Soc. Interface 2013, 10, 20130203. [Google Scholar] [CrossRef]
- Martorelli, M.; Gerbino, S.; Giudice, M.; Ausiello, P. A comparison between customized clear and removable orthodontic appliances manufactured using RP and CNC techniques. Dent. Mater. 2013, 29, e1–e10. [Google Scholar] [CrossRef]
- Kantaros, A.; Ganetsos, T.; Petrescu, F.I.T. Transforming object design and creation: Biomaterials and contemporary manufacturing leading the way. Biomimetics 2024, 9, 48. [Google Scholar] [CrossRef]
- Chaysuwan, D.; Sirinukunwattana, K.; Kanchanatawewat, K.; Heness, G.; Yamashita, K. Machinable glass-ceramics forming as a restorative dental material. Dent. Mater. J. 2011, 30, 358–367. [Google Scholar] [CrossRef]
- ISO 4049; Dentistry–Polymer–Based Restorative Materials. International Organization for Standardization: Geneva Switzerland, 2009.
- ADA Council on Scientific Affairs. American National Standard/American Dental Association Specification No. 32 for Orthodontic Wires; ADA Council on Scientific Affairs: Chicago, IL, USA, 2000. [Google Scholar]
- Temizci, T.; Bozoğulları, H.N. Effect of thermocycling on the mechanical properties of permanent composite-based CAD-CAM restorative materials produced by additive and subtractive manufacturing techniques. BMC Oral Health 2024, 24, 334. [Google Scholar] [CrossRef]
- Sahin, Z.; Ozer, N.; Kιlιçarslan, M. Mechanical characteristics of composite resins produced by additive and subtractive manufacturing. Eur. J. Prosthodont. Restor. Dent. 2023, 31, 278–285. [Google Scholar]
- Prpić, V.; Schauperl, Z.; Ćatić, A.; Dulčić, N.; Čimić, S. Comparison of mechanical properties of 3D-printed, CAD/CAM, and conventional denture base materials. J. Prosthod. 2020, 29, 524–528. [Google Scholar] [CrossRef]
- Pantea, M.; Ciocoiu, R.C.; Greabu, M.; Ripszky Totan, A.; Imre, M.; Țâncu, A.M.C.; Sfeatcu, R.; Spînu, T.C.; Ilinca, R.; Petre, A.E. Compressive and flexural strength of 3D-printed and conventional resins designated for interim fixed dental prostheses: An in vitro comparison. Materials 2022, 15, 3075. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Bonilla, M.; Berrendero, S.; Moron-Conejo, B.; Martinez-Rus, F.; Salido, M.P. Clinical evaluation of posterior zirconia-based and porcelain-fused-to-metal crowns with a vertical preparation technique: An up to 5-year retrospective cohort study. J. Dent. 2024, 28, 104953. [Google Scholar] [CrossRef]
- Abrisham, S.M.; Tafti, A.F.; Kheirkhah, S.; Tavakkoli, M.A. Shear bond strength of porcelain to a base-metal compared to zirconia core. J. Dent. Biomater. 2017, 4, 367. [Google Scholar]
- Chun, K.J.; Choi, H.H.; Lee, J.Y. Comparison of mechanical property and role between enamel and dentin in the human teeth. J. Dent. Biomech. 2014, 5, 1758736014520809. [Google Scholar] [CrossRef] [PubMed]
- Farkas, A.Z.; Galatanu, S.V.; Nagib, R. The influence of printing layer thickness and orientation on the mechanical properties of DLP 3D-printed dental resin. Polymers 2023, 15, 1113. [Google Scholar] [CrossRef] [PubMed]
- Amend, S.; Seremidi, K.; Kloukos, D.; Bekes, K.; Frankenberger, R.; Gizani, S.; Kraemer, N. Clinical effectiveness of restorative materials for the restoration of carious primary teeth: An umbrella review. J Clin. Med. 2022, 11, 3490. [Google Scholar] [CrossRef]
- Robaian, A.; Alotaibi, N.M.; Allaboon, A.K.; AlTuwaijri, D.S.; Aljarallah, A.F.; Alshehri, R.S.; Alabsi, A.A.; Mirza, M.B.; Al Moaleem, M.M. Factors Influencing Dentists’ Choice of Restorative Materials for Single-Tooth Crowns: A Survey Among Saudi Practitioners. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2024, 30, e942723-1. [Google Scholar] [CrossRef]
| Material | Description | Composition | Polishing Protocol | Manufacturer | Batch Number |
|---|---|---|---|---|---|
| Shofu Disc HC | CAD/CAM hybrid ceramic disc | Urethane dimethacrylate, triethylene glycol dimethacrylate, silica powder, fine particulate silica, zirconium silicate, colorant | SHOFU Inc., Kyoto, Japan | 416581 | |
| Saremco print CROWNTEC | 3D printing resin | bisphenol A diglycidyl methacrylate ethoxylated, trimethylbenzoyldiphenylphosphine oxide | I. Trimming with dark grey coarse grit polisher (No. 0426) for 1 min II. Finishing with brown medium grit polisher (No. 0427) for 1 min III. Polishing with light grey fine grit polisher (No. 0428) for 1 min | Saremco Dental AG, Rebstein, Switzerland | E394 |
| Nextdent C&B MFH | 3D printing resin | Methacrylic oligomers, methacrylate monomer, inorganic filler, phosphine oxides, pigment | NextDent, Soesterberg, The Netherlands | WX131N54 |
| Variables (n = 12) | Mean | SD | p |
|---|---|---|---|
| Milled | 105.79 | 5.67 | 0.0001 * |
| 3D-printed (0°) | 32.43 | 1.27 | |
| 3D-printed (45°) | 26.16 | 1.37 | |
| 3D-printed (90°) | 41.73 | 1.07 |
| Variables | MD | CI | p | |
|---|---|---|---|---|
| Lower | Upper | |||
| Milled vs. 3D-printed (0°) | 73.37 | 70.06 | 76.67 | 0.0001 * |
| Milled vs. 3D-printed (45°) | 79.63 | 76.33 | 82.93 | 0.0001 * |
| Milled vs. 3D-printed (90°) | 64.06 | 60.76 | 67.37 | 0.0001 * |
| 3D-printed (0°) vs. 3D-printed (45°) | 6.26 | 2.96 | 9.57 | 0.0001 * |
| 3D-printed (0°) vs. 3D-printed (90°) | −9.30 | −12.61 | −5.99 | 0.0001 * |
| 3D-printed (45°) vs. 3D-printed (90°) | −15.57 | −18.87 | −12.26 | 0.0001 * |
| Variables (n = 12) | Mean | SD | p |
|---|---|---|---|
| Milled | 319.97 | 3.67 | 0.0001 * |
| 3D-printed (0°) | 375.54 | 4.28 | |
| 3D-printed (45°) | 330.11 | 3.19 | |
| 3D-printed (90°) | 353.09 | 4.12 |
| Variables | MD | CI | p | |
|---|---|---|---|---|
| Lower | Upper | |||
| Milled vs. 3D-printed (0°) | −55.56 | −59.75 | −51.38 | 0.0001 * |
| Milled vs. 3D-printed (45°) | −10.14 | −14.32 | −5.95 | 0.0001 * |
| Milled vs. 3D-printed (90°) | −33.12 | −37.31 | −28.93 | 0.0001 * |
| 3D-printed (0°) vs. 3D-printed (45°) | 45.42 | 41.24 | 49.61 | 0.0001 * |
| 3D-printed (0°) vs. 3D-printed (90°) | 22.44 | 18.25 | 26.63 | 0.0001 * |
| 3D-printed (45°) vs. 3D-printed (90°) | −22.98 | −27.17 | −18.79 | 0.0001 * |
| Variables (n = 15) | Mean | SD |
|---|---|---|
| Milled unpolish | 84.7933 | 1.78064 |
| Milled polish | 85.0333 | 1.14434 |
| 3D (0°) unpolish | 3.5267 | 0.18696 |
| 3D (0°) polish | 6.680 | 0.08619 |
| 3D (45°) unpolish | 3.6600 | 0.14541 |
| 3D (45°) polish | 8.4733 | 0.24339 |
| 3D (90°) unpolish | 7.4133 | 0.28502 |
| 3D (90°) polish | 12.4333 | 0.37544 |
| Variables (Polished vs. Unpolished) | Mean | SD | CI | p | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Milled | −0.24 | 2.21 | −1.46 | 0.98 | 0.681 |
| 3D-printed (0°) | −3.15 | 0.25 | −3.02 | −3.02 | 0.0001 * |
| 3D-printed (45°) | −4.81 | 0.25 | −4.95 | −4.67 | 0.0001 * |
| 3D-printed (90°) | −5.02 | 0.53 | −5.32 | −4.72 | 0.0001 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alanazi, K.K.; Alzaid, A.A.; Elkaffas, A.A.; Bukhari, S.A.; Althubaitiy, R.O.; Alfaifi, K.A.; Alfahdi, I.M.; Alqahtani, H.A. Mechanical Assessment of CAD/CAM Fabricated Hybrid Ceramics: An In Vitro Study. Appl. Sci. 2024, 14, 7939. https://doi.org/10.3390/app14177939
Alanazi KK, Alzaid AA, Elkaffas AA, Bukhari SA, Althubaitiy RO, Alfaifi KA, Alfahdi IM, Alqahtani HA. Mechanical Assessment of CAD/CAM Fabricated Hybrid Ceramics: An In Vitro Study. Applied Sciences. 2024; 14(17):7939. https://doi.org/10.3390/app14177939
Chicago/Turabian StyleAlanazi, Khalid K., Abdulaziz A. Alzaid, Ali A. Elkaffas, Sarah A. Bukhari, Ramzi O. Althubaitiy, Khalid A. Alfaifi, Ibrahim M. Alfahdi, and Hussain A. Alqahtani. 2024. "Mechanical Assessment of CAD/CAM Fabricated Hybrid Ceramics: An In Vitro Study" Applied Sciences 14, no. 17: 7939. https://doi.org/10.3390/app14177939






