Abstract
The purpose of this study is to evaluate the influence of the matrix system on proximal contact tightness (PCT) of posterior composite resin restorations. Standardized class II cavities on 180 first lower molar dentiform model teeth (Frasaco GmbH, Tettnang, Germany) were prepared. Three groups were formed considering the matrix system: Group-IM: Ivory matrix (Hahnenkratt GmbH, Königsbach-Stein, Germany), Group-OM: Omni matrix (Ultradent, South Jordan, UT, USA), and Group-PM: Palodent V3 sectional matrix (Dentsply, Charlotte, NC, USA). Teeth were restored with resin composite mounted in a manikin head to simulate the clinical environment. Proximal contact tightness (PCT) was measured using a custom-made portable dental pressure meter (PDPM), and the validation of the PCT results was performed with a histogram analysis acquired from bite-wing radiography. All data were statistically analyzed by ANOVA and t-test in SPSS software (v.27.0) (p < 0.05). PM group showed statistically tighter contacts on both mesial (PCTm: 228.28 ± 59.17 N) and distal surfaces (PCTd: 254.91 ± 65.69 N) (p > 0.05). Mesial contacts were found to be significantly tighter than distal contacts among all (p < 0.05). According to the histogram results, only in the PM group, the difference between the mesial and distal areas is significant (p < 0.05). Histogram results confirmed that the tightest contact values were achieved in the PM group, followed by the OM and IM groups, respectively (p < 0.05). The use of sectional matrix systems and separation rings is more effective in creating tighter contact than conventional matrix systems. The use of anatomical wedges will help to create a more natural approximal contour and narrow contact area.
1. Introduction
The general purpose of treatments applied in restorative dentistry is to replace lost tooth tissues in accordance with their anatomical and physiological characteristics [1]. In these treatments, modern dentists have a wide range of direct and indirect restoration techniques to choose from [2]. When resin-based composites (RBC) are chosen as the materials in direct restorations, they have almost unlimited indication options, especially in small and mild lesions [3]. RBCs’ can be applied in most cases, whereas the cavity boundaries change and widen due to caries lesion progression. In addition, they can be applied successfully even in more conservative or minimally invasive treatments with minimum material loss and do not need a standard cavity preparation such as amalgam or ceramic restorations [4,5]. However, the biggest disadvantage of all RBCs’ is polymerization shrinkage, which occurs after the applied RBC is cured with the light device, causing the material to lose its volume [6,7]. Considering that there is a natural gap of 5–20 microns between teeth, this shrinkage can create a significant problem in terms of “contact”, especially in cavities reaching the approximal sides [7]. In addition, in technically critical situations such as cavities with deep margins or excessive tissue loss, the application stages of composite resins make it difficult to give an appropriate “contour” and directly affect the success of the restorations [8]. An inadequate contact or contour will lead to food impaction between the relevant teeth and indirectly to periodontal diseases and secondary caries [9]. For these reasons, it is important to create a suitable contact area between the tooth to be restored and the adjacent tooth to prevent these situations, which are the common cause of patient complaints [10].
In restorative dentistry, circumferential matrices (Tofflemire) and Ivory matrices have been used since the 1950s in the restoration of Class II cavities reaching the approximal surfaces [11,12]. The most common reasons for choosing these matrices are their affordability, ease of application, and firm stability when adapted to the tooth [11]. However, in some cases, this practice results in the tooth’s dimensions being narrower and reduced in length and width than its ideal shape [13]. In addition, as a result of the compression of the matrix bands during fixation, the slope of the bands flattens and their contact with the side teeth decreases. As a result of the fixation process applied to the healthy side, an incorrect separation can occur, and the relevant tooth comes closer to the adjacent tooth in the area to be restored [12,14]. The narrowing of the contact area, combined with the polymerization shrinkage of the RBC, will cause an “open contact” problem in the restoration area.
To overcome these problems, pre-anatomically shaped matrices, defined as “Sectional Matrices”, have been developed [15]. Generally, they are used with a separation ring that separates the teeth and stabilizes the matrix coronally, supporting the formation of a suitable contact area [15,16]. Unlike traditional matrices, these “passively placed” separation rings positioned in the area of the tooth to be restored will not cause a reduction in the size of the tooth. Because this passive placement is sufficient to stabilize the matrix both cervically and coronally, it prevents the formation of an incorrect contour (concave), especially in the buccal and lingual regions [16,17]. In addition, the feet (retainer arms) of the separation ring separate the restoration area from the adjacent tooth, increasing the field of view and essentially making a separation in the right direction [17]. In this way, it is possible to create a tighter contact area between the tooth, which returns to its natural position at the end of the restoration, and the adjacent tooth. The anatomical contour of the tooth, in addition to the contact, prevents food retention and the formation of triangular dead areas [18]. The fact that the matrix bands used in sectional matrices are pre-curved ensures that the contact area in the restorations is not only tight but also reflects the natural contours of the tooth anatomically [18]. This ensures that the restoration in the relevant area is suitable and sufficient in terms of contact and contour.
The oldest method used to measure the tightness of the contact area, both with healthy teeth and in restorations, is to remove a 0.03–0.05 mm thick metal band placed between the teeth by pulling it in the vertical direction and measuring the resulting resistance [19]. Some studies have tested dental floss, strip bands, isolation tapes, and matrices of various sizes [15,18,20].
The aim of this study was to investigate in vitro the tightness of the contact area formed by traditional and sectional matrix systems used in Class II restoration construction with a device designed and manufactured to measure even the smallest voltage differences. The initial hypothesis (h0) of the study was that there would be no difference between the matrix systems in terms of creating a good and tight contact area.
2. Materials and Methods
The steps in this in vitro study consist of cavity preparation, restoration, contact tightness measurement, and radiographic verification. During all these procedures, phantom teeth (Frasaco GmbH, Tettnang, Germany) were fixed to the same brand of phantom jaws as tightly as possible (Max torque: ≈35 N-mm) and in such a way that there were no missing teeth in the jaws. The lower right first molar (no. 46) tooth was selected for the cavities to be prepared.
2.1. Cavity Preparation Phase
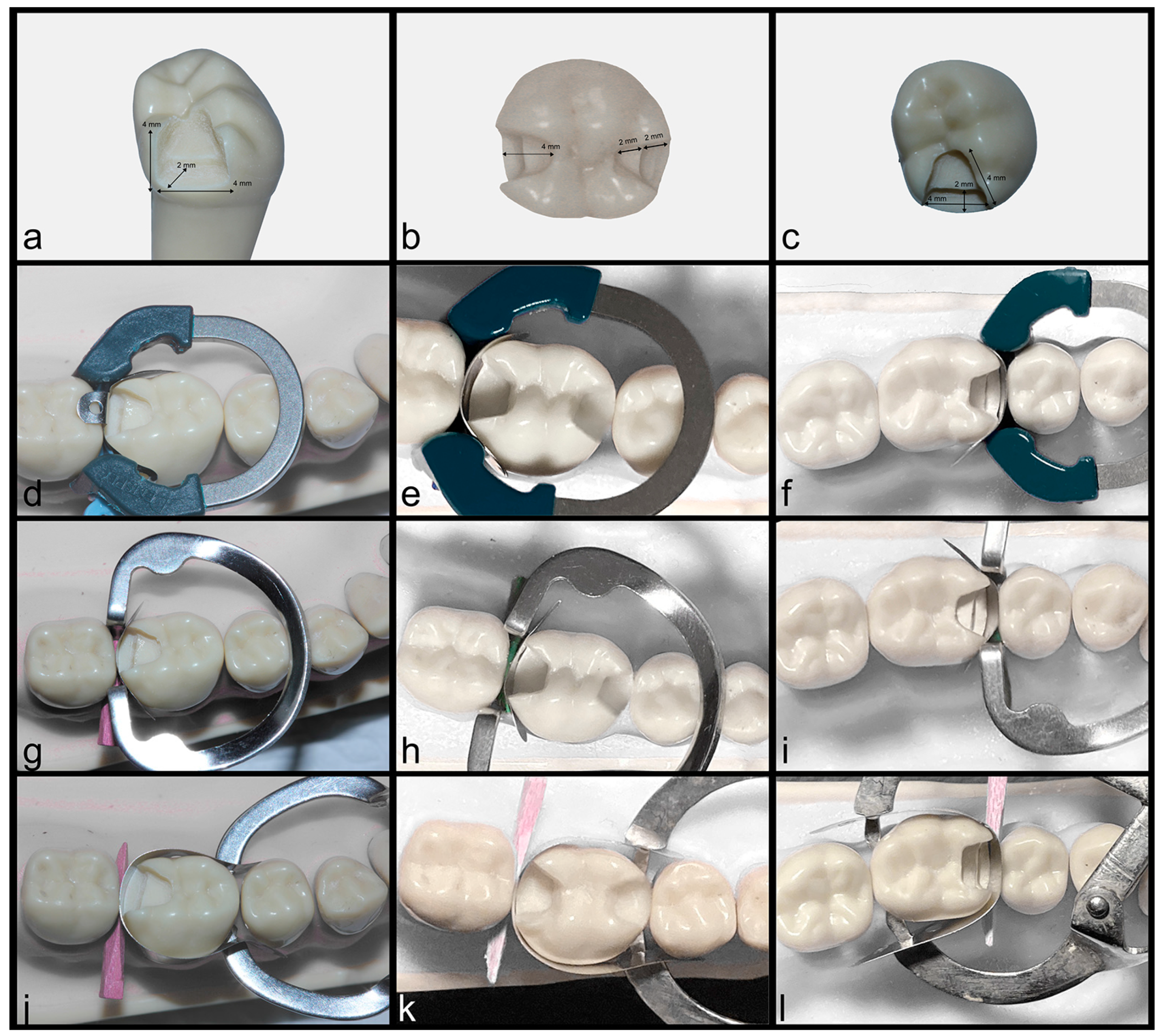
Standardized Class II cavities including occluso-mesial (OM), occluso-distal (OD), and mesio-occluso-distal (MOD) were prepared on phantom teeth for the application of 180 composite resin restorations (n = 20). The cavity dimensions were arranged in the gingival region and the occlusal cavity (4 × 4 × 2 mm) by considering the Black cavity rules (Figure 1). To avoid damaging the neighbor teeth during the preparation of the cavities, a protective wedge and metal band were used in all groups. A high-speed handpiece with diamond burs (Bien Air; Chemin des Grillons, Bienne, Switzerland) was used in cavity preparation phase.
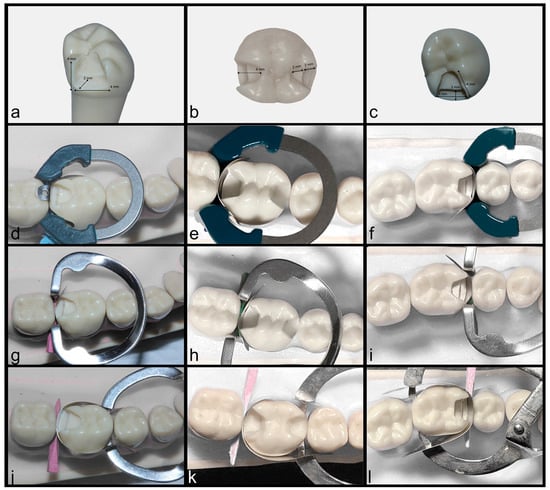
Figure 1.
Pictures of cavity preparation and matrix placement phases: (a) OD cavity design, (b) MOD cavity design, (c) OM cavity design, (d–f) PM group, (g–i) OM group, (j–l) IM group.
2.2. Restoration Phase
During the application of the restorations, 60 teeth were randomly divided into three groups according to the matrix systems used:
- Group-IM: Ivory matrix (Hahnenkratt GmbH, Königsbach-Stein, Germany);
- Group-OM: Omni matrix (Ultradent, South Jordan, UT, USA);
- Group-SM: Palodent Plus V3 sectional matrix (Dentsply, Charlette, NC, USA).
In all groups, the appropriate matrix system was installed on the teeth where the cavities were prepared in accordance with the manufacturer’s instructions (Figure 1). Since no special wedge was produced for the set in the matrix systems in Groups 1 and 2, a traditional wooden wedge (Sycamore No. 2, Kerr Co., Orange County, CA, USA) was used.
Before the RBC application, a self-etch adhesive system (Gluma Bond Universal, Heraus Kulzer, Hanau, Germany) was applied to the cavities and polymerized with an LED light device (Elipar, 3M ESPE, Saint Paul, MN, USA) with a light power of 1200 W for 20 s. The restorations were made using an incremental technique with a nano-hybrid RBC (Charisma Topaz, Heraus Kulzer, Hanau, Germany). After each layer, the RBC was polymerized using the LED light device for 20 s, and after the matrix was removed, final curing was performed for 40 s from both the buccal and lingual sides.
In order to avoid excessive material loss in contact areas during polishing and finishing processes of composites, the finishing and polishing of occlusal surfaces were performed with diamond burs (Acurata, Thurmansbang, Germany) and composite polishing discs (Polishing System 18P, Microdont, São Paulo, Brazil), while for contact areas, only medium and soft interproximal composite strips (PPS, Tor VM, Moscow, Russia) were used for a total of 40 s. To maintain the contact point intact, the polishing process was carried out only with horizontal movements, starting from the areas under the contact. After the polishing process, all composites were polymerized again with the LED light device for 20 s.
2.3. Measuring Contact Tightness
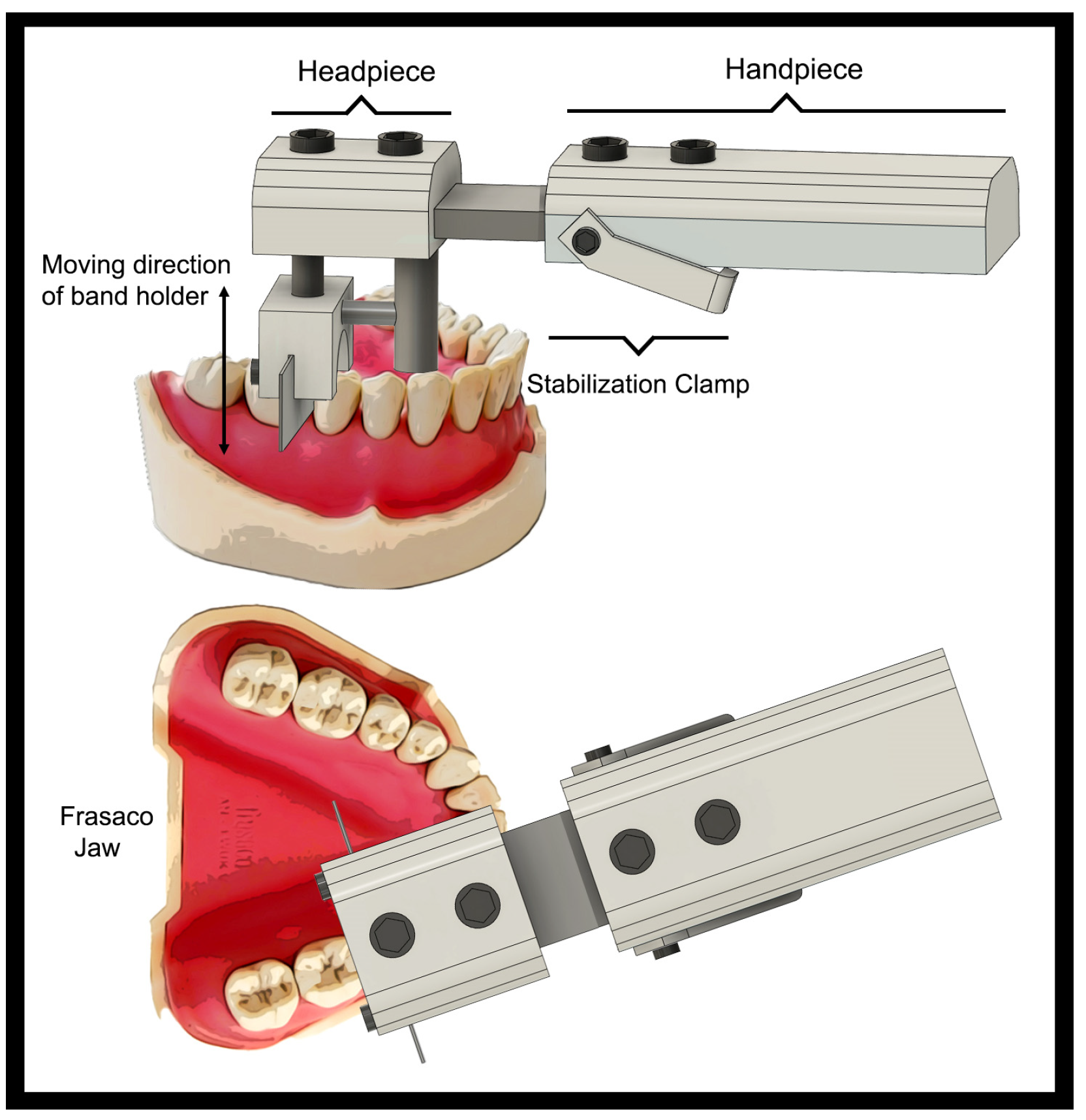
To measure contact tightness, a strain gauge tension (friction force) measuring system called “Portable Dental Pressure Meter (PDPM)” was developed by the faculty of mechanical engineering. The system consists of a “headpiece” part, which contains the metal band holder and a “handpiece” that has a clamp (for stabilization) and elevator (z-axis motor) and contains the mechanical parts (strain gauges, boards, power unit, cables, etc.). A matrix band (Tofflemire Flat Matrix Band, Hahnenkratt GmbH, Königsbach-Stein, Germany) made of 0.03 mm thick stainless steel was cut to a length of 30 mm and fixed to the head of the PDPM. Then, for each sample, the metal band was placed in the interproximal region until it contacted the gum from the restored interface of the relevant tooth through the adjacent tooth interface (Figure 2).
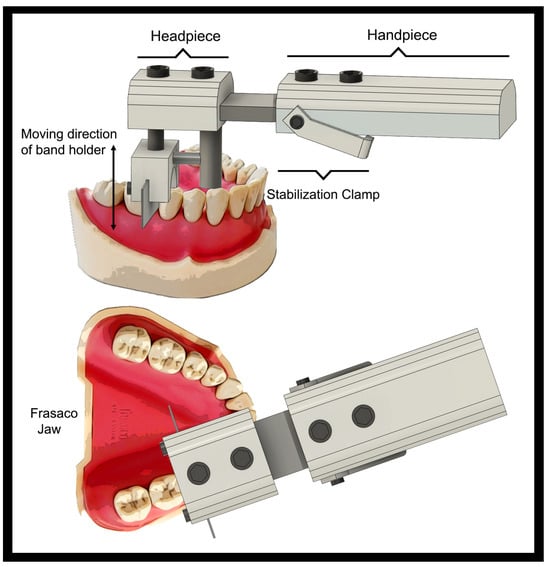
Figure 2.
Schematic image showing the parts, working principle, and positioning of the PDPM device on manikin jaws.
Contact tightness was calculated by recording the minimum, maximum, and average values of the amount of tension obtained when pulling this band upward in the vertical direction. The elevator was responsible for the vertical movement of the system at a constant speed (1 mm/sec) without stalling or wobbling. To obtain a standard measurement of all approximal contact areas, PDPM device, which was modified with the part of a 3D printer (Tronxy P802M, Anet, Longgang District, Shenzhen, China), and a clamp are added to mount the system on phantom jaw models to the premolar region teeth (Figure 2). The strain values were measured depending on the friction resistance between the restored and solid teeth and recorded as Newton [N]. Three measurements were made for each sample, and the average values were recorded to create force–strain diagrams with an algorithm prepared in Excel software (MS Office 2020, Windows, Microsoft, Redmond, WA, USA). For the reliability of the results, measurements were performed using a new and undeformed matrix band with the same dimensions each time.
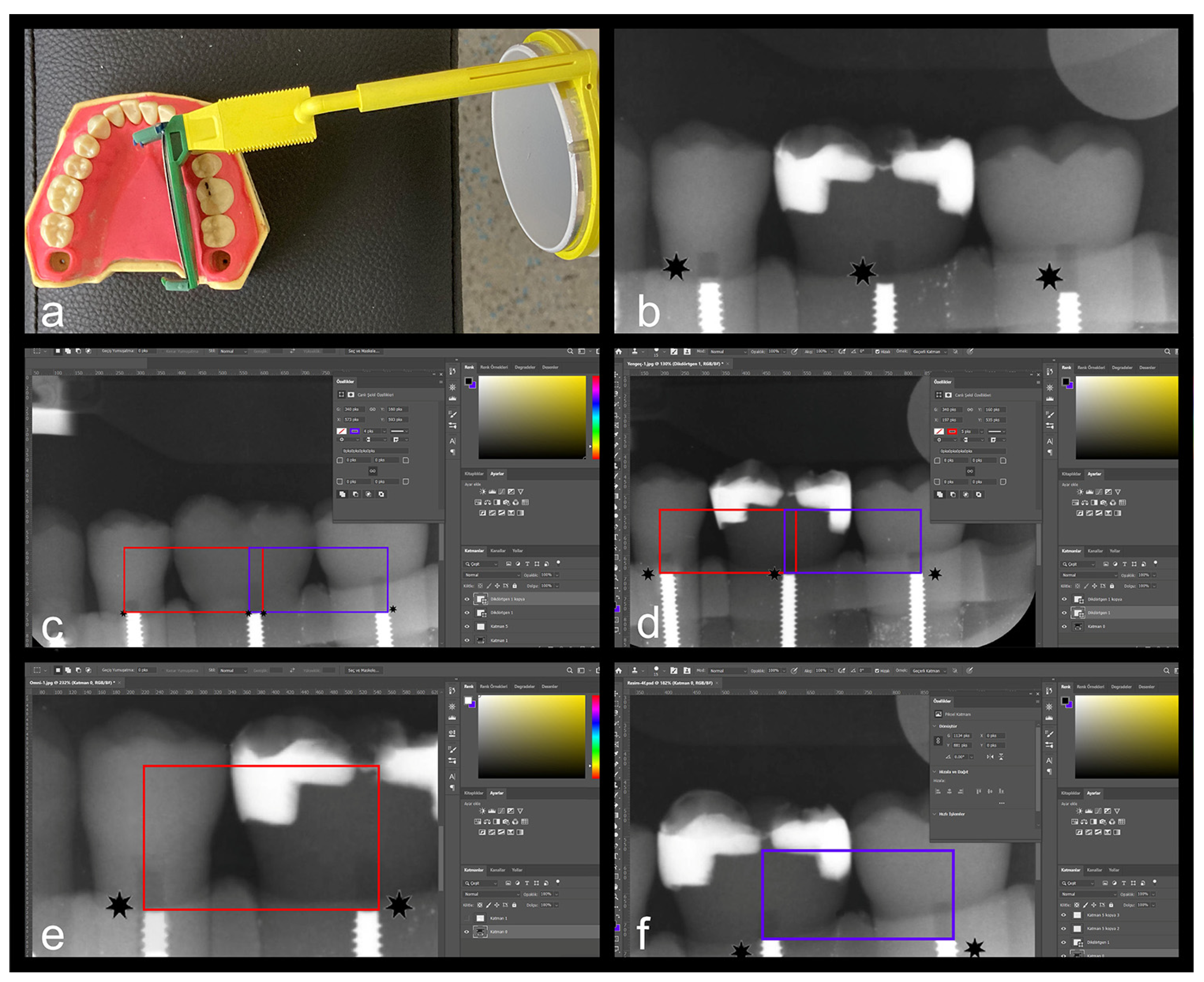
2.4. Radiographic Verification
In order to verify the data obtained in measuring contact tightness, radiography was taken to include the relevant tooth and two adjacent teeth (second premolar and second molar) in each jaw. A radiographic receptor (phosphor plate) was placed on the lingual part of the relevant teeth using a film holder specially prepared for this process (Digora, Optime Scanner, Soredex, Tuusula, Finland): 60 kV, 7 mA and 0.25 s, 100 mm in parameters, irradiated from a distance (Figure 3) (21). A researcher other than the physician performing the restorations took bite-wing films of each restoration at least three times until an acceptable, non-superimposed image of the contact areas was obtained. Also, an X-ray of a sound Frasaco lower right 1st molar tooth (without restoration) has been captured for comparison.
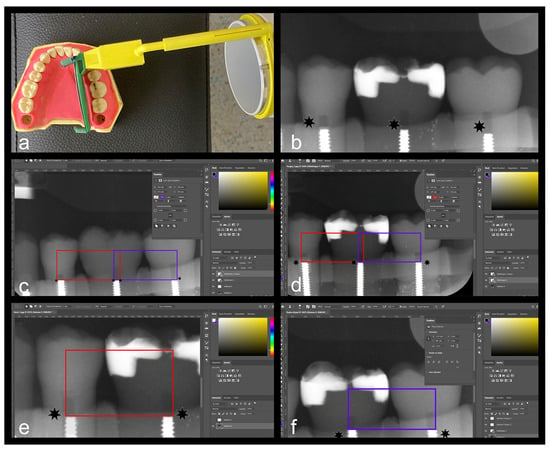
Figure 3.
Radiographic validation of contact tightness in proximal areas with histogram analysis: (a) positioning the beam of X-ray machine, (b) * reference points in radiographic images, (c–f) designated measurement area for histogram analysis and the results of density (black and white).
The data obtained were transferred to the image editing program on the computer (Photoshop PS 2020, Adobe Inc., San Jose, CA, USA), and histogram analysis was performed. In the analysis, the areas where the X-ray light passed directly were observed as dark (black) areas, while the areas where the X-ray was absorbed, depending on the radiopacity of the restoration, were observed as light (white) areas. In histogram analysis, the grey-to-black areas in a selected region are counted as pixels, and the percentage and distribution in this region are determined. To standardize measurements of all teeth, fixed points must be determined, and a standard geometric shape (rectangle) must be selected (Figure 3). The most basic point, which is known to be standard in all Frasaco teeth and can be observed in radiological examination, is the pre-prepared slots for screwing the teeth. Since the positions of these screw slots in the tooth are fixed and the base points are aligned as a result of maximum screwing, the width of the rectangle to be measured was chosen as the distance between these screws. In terms of height, the upper point of the contact areas of the restorations was determined, and histogram measurements were made in rectangles with dimensions of 340 × 160 pixels.
2.5. Statistical Analyses
Since it was a three-group study, to calculate the sample size, a power analysis (G-Power) (V: 3.1, University of Düsseldorf, Düsseldorf, Germany) was performed with alpha (p = 0.05) at 5% and beta (power) scores at 90% after the first 15 measurements. Therefore, an estimated group size of 25 restorations could reach an estimated 90% power. The obtained data were transferred to statistical software (SPSS, IBM Corp., Chicago, IL, USA). Normal distributions were determined using the Kolmogorov–Smirnov test, intra-group differences by t-test, and inter-group differences by one-way analysis of variance (ANOVA) and post hoc Tukey test (p = 0.05).
3. Results
The contact tightness values in N (± obtained from the PDPM system are shown in Table 1, and the values obtained from the histogram analysis are shown in Table 2. The tightest contact area was an average of 254.91 ± 65.69 N in the distal approximal area in the PM group, while an average of 126.96 ± 56.84 N was found in the distal approximal area in the OM group, and 69.01 ± 24.99 N voltage was determined in the distal approximal area in the IM group (Table 1). When the contact tightness in the distal approximal areas of the teeth was examined, the differences between all groups were statistically significant (p < 0.05).

Table 1.
Contact tightness values (N) obtained from the study.

Table 2.
Histogram results from the study (pixel density).
In addition, when the contact tightness in the distal approximal areas of the relevant teeth was examined, higher tension values were obtained in the distal contacts in the PM group, while the tension in the mesial region was higher in the other groups (Table 1). Additionally, the tightest contact area in the mesial region was obtained as an average of 228.26 ± 59.17 N in the PM group, and an average tension of 145.96 ± 40.81 N was detected in the mesial approximal area in the OM group and 74.65 ± 19.18 N in the mesial approximal area in the IM group (Table 1). When the contact tightness in the mesial approximal areas of the teeth was examined, the differences between all groups were statistically significant (p < 0.05).
Class II cavity design contact tightness in Class II (MOD) restorations was found to be lesser when compared to Class II OM and Class II OD restorations (p < 0.05). In addition, for all matrix types and cavity designs, mesial contact tightness was found to be higher than the distal contact tightness values; however, no statistical significance was found for Class II MOD restorations between the mesial and distal surfaces in all groups (p > 0.05). When the values are generalized among all matrix groups in which contact tightness is examined, regardless of the cavity design, the best results are observed in the PM group, followed by OM and IM groups, respectively (p < 0.05).
The histogram exhibited that black pixel (void) density in the IM group was calculated more than any other group except in class II MOD restorations (p < 0.05), which shows that this matrix is inadequate in contour creation compared to other matrix types. Additionally, there was a difference in terms of contour between the mesial and distal areas only in the PM group (p < 0.05), while no significant difference was found among the other groups (p > 0.05). When the groups were compared with each other, it was determined that there was a difference in both the mesial and distal approximal areas in all three groups (p < 0.05). In light of these findings, it was determined that the restorations with the most curvature and the most appropriate anatomical form were made in both the mesial (96.692) and distal (81.142) areas in the PM group.
4. Discussion
In this study, different matrix systems and techniques used to create approximal contacts in Class II posterior RBC restorations were tested. For this purpose, a novel in vitro device was designed to measure the approximal contact tightness of Class II RBC restorations. To ensure the validity of this model, techniques similar to those applied by Loomans et al. in a randomized clinical trial and an in vitro experiment were used [20,21]. Although the tested hypothesis was that the contact tightness obtained would be equal for all groups, in light of the findings, this hypothesis (h0) was rejected because there were statistically significant differences between the groups.
In general, it is known that contour and approximal contact are the most important factors in preventing food impaction, tooth migration, periodontal complications, and caries [14,22]. While pre-shaped (contoured) matrix bands contribute to a better anatomical contour of approximal restorations, it is known that the flat matrix bands used in traditional matrices are insufficient to create contact [18,23]. In this in vitro study, Class II restorations were implanted with a traditional technique (environmental matrix system and wooden wedge), a modified sectional matrix (sectional matrix ring, band, and wooden wedge), and a modern sectional matrix system (separation ring, anatomical band, and wedge). The degree of contact and contact tightness obtained by applying composite resin restorations to Class II approximal cavities were compared. A tighter contact and better histogram results were obtained in the PM matrix with an anatomical matrix band and the OM matrix groups using a traditional wedge compared to the traditional ivory matrix (Group IM). This result is supported by the results of the studies conducted by Loomans et al., Wirsching et al., and Saber et al. [24,25,26].
However, when the effect of fixing the anatomical matrix band with an anatomical wedge or a wooden (traditional) wedge was examined, the contour obtained with the anatomical wedge was found to be closer to the natural form of the dental tissue. In addition, in restorations where an anatomical wedge was used, extrusion and irregularities at the interface occurred less often. In this study, both contact tightness and contour values were better in the sectional matrix group, where anatomical bands and wedges were used, than in the other groups. It can be claimed that when there is less protrusion and irregularity at the interface, smoothing and polishing with sandpaper causes less material loss. Studies in the literature are consistent with the results of this research [27,28,29,30].
There are also studies showing that finishing and polishing processes performed on approximal surfaces with interface sanding may cause changes in the surface of composite restorations and affect the contact and contour [31,32]. In this study, immediately after the RBCs’ were made, dry sanding and polishing were carried out for 40 s with composite interface sandpapers with four different grain thicknesses. Although this stage was kept standard for each group, how much material this sanding process removed from the composite surfaces was not measured.
Studies have shown that sectional matrices have different effects on the separation of the retaining ring in the opening amount and the area where it is positioned [16,33,34]. However, some studies have claimed that separation rings in sectional matrices create similar contacts when used in accordance with the manufacturer’s instructions and that dentists tend to use them in this way [35,36]. However, in some recent studies, it has been shown that Palodent BiTine or similar Composite-Tight Gold separation rings, which are designed to be more anatomical to the contact area of the posterior teeth and produced with a higher percentage of titanium in the metal alloy, provide greater separation [26,37]. This extra titanium ring or ally add-in makes the separation ring more flexible as well as able to apply more force in separation. In addition, if the gripper arms are only flat cylindrical metal in form, are not designed for the interproximal area where the embrasures are located and do not allow the positioning of the wedge, they would cause a tight contact but a weak contour [38]. Since the OM is a sectional matrix system with similar features, it explains the weaker contours in histogram measurement compared to the PM matrix system. Additionally, there are studies in the literature that support our results, the common opinion in all of them is that buccal and lingual embrasures are very effective in creating contact and contour [30].
The measurement and evaluation process of the contact tightness is a challenging procedure where the contact and contour must be compatible together such as in Class II cavities. In cases where there is sufficient contact, if there is an inappropriate contour or vice versa, erroneous measurements will be inevitable. In addition, under clinical conditions, the position of the patient, the stability of the physician, the measurement speed and adequacy of the device, the wetness of the area, which affects the frictional stress caused by teeth and gums, and similar anatomical factors will directly affect the measurement process [34,39]. In a study conducted by Kim et al., it was reported that there were differences in contact tightness measurements depending on the position of the patients as well as the teeth; therefore, it was quite difficult to make objective measurements in the in vivo conditions [34]. Therefore, it is essential that the measuring system has to be fixed to achieve similar results in all conditions to exclude possible effects [40]. Additionally, the polishing stage has a direct effect on the quality and integrity of the contour and strength of the contact point by altering the previous steps and influencing the final results. To maintain the contact point of the restoration solid and tight as the natural morphology of the tooth, it is required to establish a standardized polishing process to minimize the loss of resin composite and to avoid open contacts.
Although this PDPM system is designed and manufactured for clinical use, in vitro test conditions are applied to make standard measurements with this prototype and to reveal the pros and cons of the system, which may cause conflict between the results and incompatibility with the literature. Although reliable and reproducible results are obtained if the system is stabilized in the mouth, the usability of the device in cases of missing anterior abutment/anchor teeth will be challenging under clinical conditions. Additionally, the fact that the manikin model measured in this study remained completely motionless to reflect simulating in vitro conditions is also a misleading advantage. Considering that in clinical conditions, people’s natural movements and even breathing can affect the results, the measurement process must be fast enough to be completed in a very short time.
Due to these difficulties and challenges encountered in the measurement and evaluation of contact tightness, the mounting and measuring processes were standardized optimally to achieve results without a doubt. However, prior to being used in clinical conditions, the system may need to be tested and modified in vivo under different exceptional and extreme conditions, such as partial edentulism or movement disorders. Therefore, the system needs to be developed to ensure precise patient position and device stability.
5. Conclusions
Sectional matrix systems are superior to traditional matrices in restoring approximal walls and contact areas in a more anatomical manner. In the field of restoration, thanks to their separation ability, pre-shaped bands and anatomical wedges enable the construction of an approximal restoration that is both tighter and more contoured to the natural form of the tooth. Traditional wooden wedges, which are commonly used by clinicians instead of the anatomical wedges of sectional matrices, the desired contact in the restoration can be achieved, but the contour may be weaker and partially inadequate, resulting in open or insufficient contact. Radiographical findings suggest that separation ability correlates with the optimal contact of the restoration, while the anatomical bands are largely responsible for creating the contour as desired. Unlike subjective methods used in the measurement of contact tightness in vivo and in vitro, PDPM is promising in terms of providing more objective and reproducible measurements, but more studies and parameters are needed for it to be used safely in clinical conditions.
Author Contributions
Research and investigation, C.P., O.B.G., and M.S.; table and figure preparation, C.P. and E.E.; data curation, O.B.G. and M.T.; writing—review and editing, C.P. and M.T.; All authors have read and agreed to the published version of the manuscript.
Funding
This study is funded by the Ege University Administration of Academical Research Projects Department (Ege-BAP) with a reference number of ID: 21620.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The original contributions presented in the study are included in the article; further inquiries can be directed to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Iandolo, A. Modern Therapeutic strategies in endodontics and restorative dentistry. Medicina 2023, 59, 333–341. [Google Scholar] [CrossRef] [PubMed]
- Azeem, R.A.; Sureshbabu, N.M. Clinical performance of direct versus indirect composite restorations in posterior teeth: A systematic review. J. Conserv. Dent. 2018, 21, 2–9. [Google Scholar]
- Ilie, N.; Hicke, R. Resin composite restorative materials. Aust. Dent. J. 2011, 56, 59–66. [Google Scholar] [CrossRef]
- Worthington, H.V.; Khangura, S.; Seal, K.; Mierzwinski-Urban, M.; Veitz-Keenan, A.; Sahrmann, P.; Schmidlin, P.R.; Davis, D.; Iheozor-Ejiofor, Z.; Rasines Alcaraz, M.G. Direct composite resin fillings versus amalgam fillings for permanent posterior teeth. Cochrane Database Syst. Rev. 2021, 8, 5620–5635. [Google Scholar]
- Dioguardi, M.; Alovisi, M.; Troiano, G.; Caponio, C.V.A.; Baldi, A.; Rocca, G.T.; Comba, A.; Lo Muzio, L.; Scotti, N. Clinical outcome of bonded partial indirect posterior restorations on vital and non-vital teeth: A systematic review and meta-analysis. Clin. Oral. Investig. 2021, 25, 6597–6621. [Google Scholar] [CrossRef] [PubMed]
- Szczesio-Wlodarczyk, A.; Fronczek, M.; Ranoszek-Soliwoda, K.; Sokolowski, J.; Bociong, K. Evaluation of selected artificial aging protocols for dental composites including fatigue and fracture tests. Appl. Sci. 2024, 14, 6964. [Google Scholar] [CrossRef]
- Kaisarly, D.; Gezawi, M.E. Polymerization shrinkage assessment of dental resin composites: A literature review. Odontology 2016, 104, 257–270. [Google Scholar] [CrossRef]
- Brackett, M.G.; Contreras, S.; Contreras, R.; Brackett, W.W. Restoration of proximal contact in direct class II resin composites. Oper. Dent. 2006, 31, 155–160. [Google Scholar] [CrossRef] [PubMed]
- Clark, D. The seven deadly sins of traditional class II restorations. Dent. Today 2017, 36, 119–121. [Google Scholar]
- Sarrett, D.C. Clinical challenges and the relevance of materials testing for posterior composite restorations. Dent. Mater. 2005, 21, 9–20. [Google Scholar] [CrossRef]
- Kampouropoulos, D.; Paximada, C.; Loukidis, M.; Kakaboura, A. The influence of matrix type on the proximal contact in class II resin composite restorations. Oper. Dent. 2010, 35, 454–462. [Google Scholar] [CrossRef] [PubMed]
- Marlynda, A.A. Historical review of dental matrices. Malays. Dent. J. 2011, 33, 2–19. [Google Scholar]
- El-Badrawy, W.A.; Leung, B.W.; El-Mowafy, O.; Rubo, J.H.; Rubo, M.H. Evaluation of proximal contacts of posterior composite restorations with 4 placement techniques. J. Can. Dent. Assoc. 2003, 69, 162–167. [Google Scholar] [PubMed]
- Gilmour, A.S.; James, T.; Bryant, S.; Gardner, A.; Stone, D.; Addy, L.D. An in vitro study on the use of circumferential matrix bands in the placement of class II amalgam restorations. Br. Dent. J. 2008, 205, 221–230. [Google Scholar] [CrossRef]
- Cho, S.D.; Browning, W.D.; Walton, K.S. Clinical use of a sectional matrix and ring. Oper. Dent. 2010, 35, 587–591. [Google Scholar] [CrossRef]
- Bailey, O. Sectional matrix solutions: The distorted truth. Br. Dent. J. 2021, 231, 547–555. [Google Scholar] [CrossRef]
- de la Peña, V.A.; García, R.P.; García, R.P. Sectional matrix: Step-by-step directions for their clinical use. Br. Dent. J. 2016, 220, 11–14. [Google Scholar] [CrossRef]
- Owens, B.M.; Jeffrey, G.P. An evidence-based review of dental matrix systems. Gen. Dent. 2016, 64, 64–70. [Google Scholar]
- Oh, S.H.; Nakano, M.; Bando, E.; Shigemoto, S.; Kori, M. Evaluation of proximal tooth contact tightness at rest and during clenching. J. Oral. Rehab. 2004, 31, 538–545. [Google Scholar] [CrossRef]
- Loomans, B.A.; Opdam, N.J.; Roeters, F.J.; Bronkhorst, E.M.; Burgersdijk, R.C. Comparison of proximal contacts of class 2 resin composite restorations in vitro. Oper. Dent. 2006, 31, 688–693. [Google Scholar] [CrossRef]
- Loomans, B.A.; Roeters, F.J.; Opdam, N.J.; Kuijs, R.H. The effect of proximal contour on marginal ridge fracture of class II composite resin restorations. J. Dent. 2008, 36, 828–832. [Google Scholar] [CrossRef] [PubMed]
- Bhatia, H.P.; Sood, S.; Sharma, N.; Singh, A.; Rajagopal, V. Comparative evaluation of clinical efficiency and patient acceptability toward the use of circumferential matrix and sectional matrix for restoration of class 2 cavities in primary molars. Int. J. Clin. Pediatr. Dent. 2021, 14, 748–751. [Google Scholar] [PubMed]
- Chuang, S.F.; Su, K.C.; Wang, C.H.; Chang, C.H. Morphological analysis of proximal contacts in class II direct restorations with 3D image reconstruction. J. Dent. 2011, 39, 448–456. [Google Scholar] [CrossRef] [PubMed]
- Schropp, L.; Stavropoulos, A.; Spin-Neto, R. Implant image quality in dental radiographs recorded using a customized imaging guide or a standard film holder. Clin. Oral Implants Res. 2012, 23, 55–59. [Google Scholar] [CrossRef]
- Wirsching, E.; Loomans, B.A.; Klaiber, B.; Dörfer, C.E. Influence of matrix systems on proximal contact tightness of 2- and 3-surface posterior composite restorations. J. Dent. 2011, 39, 386–390. [Google Scholar] [CrossRef]
- Saber, M.H.; Loomans, B.A.; El Zohairy, A.; Dörfer, C.E.; El-Badrawy, W. Evaluation of proximal contact tightness of class II resin composite restorations. Oper. Dent. 2010, 35, 37–43. [Google Scholar] [CrossRef]
- Hahn, B.; Haubitz, I.; Krug, R.; Krastl, G.; Soliman, S. Influence of matrix type on marginal gap formation of deep class II bulk-fill composite restorations. Int. J. Environ. Res. Public Health 2022, 19, 4961–4970. [Google Scholar] [CrossRef]
- Dindukurthi, M.K.; Setty, J.V.; Srinivasan, I.; Melwani, A.M.; Manasa Hegde, K.; Radhakrishna, S. Restoration of proximal contacts in decayed primary molars using three different matrix systems in children aged 5–9 years: An in vivo study. Int. J. Clin. Pediatr. Dent. 2021, 14, 70–74. [Google Scholar]
- Gomes, I.A.; Filho, E.M.; Mariz, D.C.; Borges, A.H.; Tonetto, M.R.; Firoozmand, L.M.; Kuga, C.M.; De Jesus, R.R.; Bandéca, M.C. In vivo evaluation of proximal resin composite restorations performed using three different matrix systems. J. Contemp. Dent. Pract. 2015, 16, 643–647. [Google Scholar]
- Loomans, B.A.; Opdam, N.J.; Roeters, F.J.; Huysmans, M.C. Proximal marginal overhang of composite restorations in relation to placement technique of separation ring. Oper. Dent. 2012, 37, 21–27. [Google Scholar] [CrossRef]
- Kaizer, M.R.; de Oliveira-Ogliari, A.; Cenci, M.S.; Opdam, N.J.; Moraes, R.R. Do nanofill or submicron composites show improved smoothness and gloss? A systematic review of in vitro studies. Dent. Mater. 2014, 30, 41–78. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, M.A.G.; Khokhar, N.H.; Razak, A.A.A. Polishing of the composite resin restorations? Literature review. Ann. Dent. Univ. Malaya 2010, 17, 25–34. [Google Scholar] [CrossRef]
- El-Shamy, H.; Sonbul, H.; Alturkestani, N.; Tashkandi, A.; Loomans, B.A.; Dörfer, C.; El-Badrawy, W. Proximal contact tightness of class II bulk-fill composite resin restorations: An in vitro study. Dent. Mater. J. 2019, 38, 96–100. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.H.; Jung, J.H.; Kim, H.J.; Chung, C.H.; Oh, S.H. Evaluation of tightness of proximal tooth contact in permanent dentition. J. Korean Acad. Prosthodont. 2008, 46, 553–560. [Google Scholar] [CrossRef]
- Shaalan, O.O. Evaluation of matrix band systems for posterior proximal restorations among Egyptian dentists: A cross-sectional survey. Acta Stomatol. Croat. 2020, 54, 392–400. [Google Scholar] [CrossRef]
- Ahmad, M.Z.; Sadaf, D.E.; Gaikwad, R.N.; Arjumand, B. Comparison of two different matrix band systems in restoring two surface cavities in posterior teeth done by senior undergraduate students at Qassim University, Saudi Arabia: A randomized controlled clinical trial. Indian. J. Dent. Res. 2018, 29, 459–464. [Google Scholar] [CrossRef]
- Loomans, B.A.; Opdam, N.J.; Roeters, F.J.; Bronkhorst, E.M.; Huysmans, M.C. Restoration techniques and marginal overhang in class II composite resin restorations. J. Dent. 2009, 37, 712–717. [Google Scholar] [CrossRef]
- Raghu, R.; Srinivasan, R. Optimizing tooth form with direct posterior composite restorations. J. Conserv. Dent. 2011, 14, 330–336. [Google Scholar] [CrossRef]
- Vardimon, A.D.; Matsaev, E.; Lieberman, M.; Brosh, T. Tightness of dental contact points in spaced and non-spaced permanent dentitions. Eur. J. Orthod. 2001, 23, 305–314. [Google Scholar] [CrossRef]
- Lima, V.P.; Machado, J.B.; Zhang, Y.; Loomans, B.A.C.; Moraes, R.R. Laboratory methods to simulate the mechanical degradation of resin composite restorations. Dent. Mater. 2022, 38, 214–229. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).