Abutment Tooth Formation Simulator for Naked-Eye Stereoscopy
Abstract
:1. Introduction
2. Materials and Methods
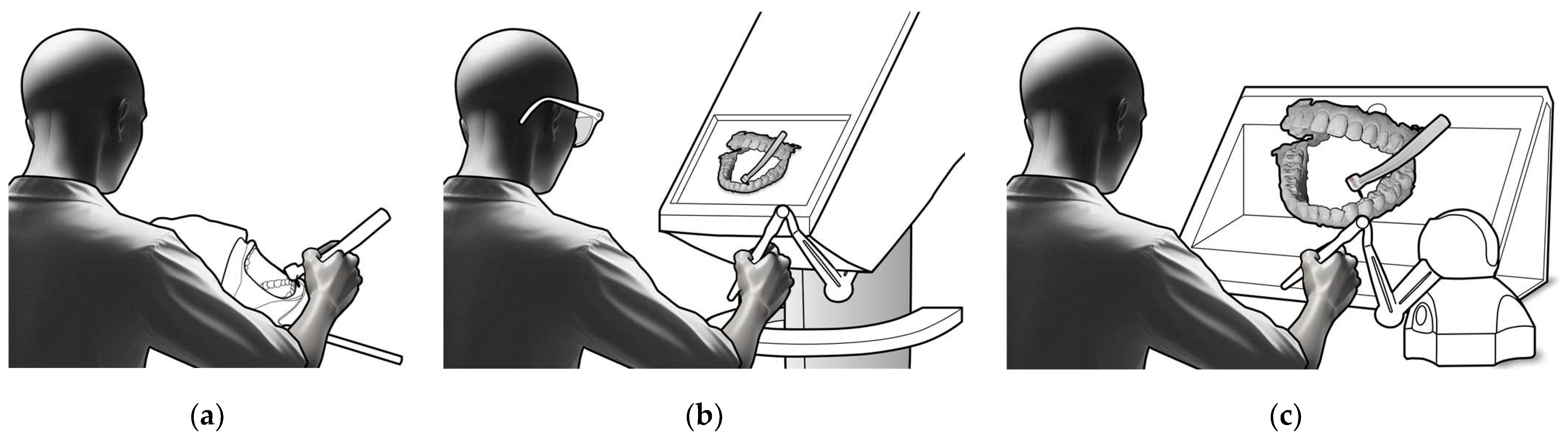
2.1. Machinery and Tools
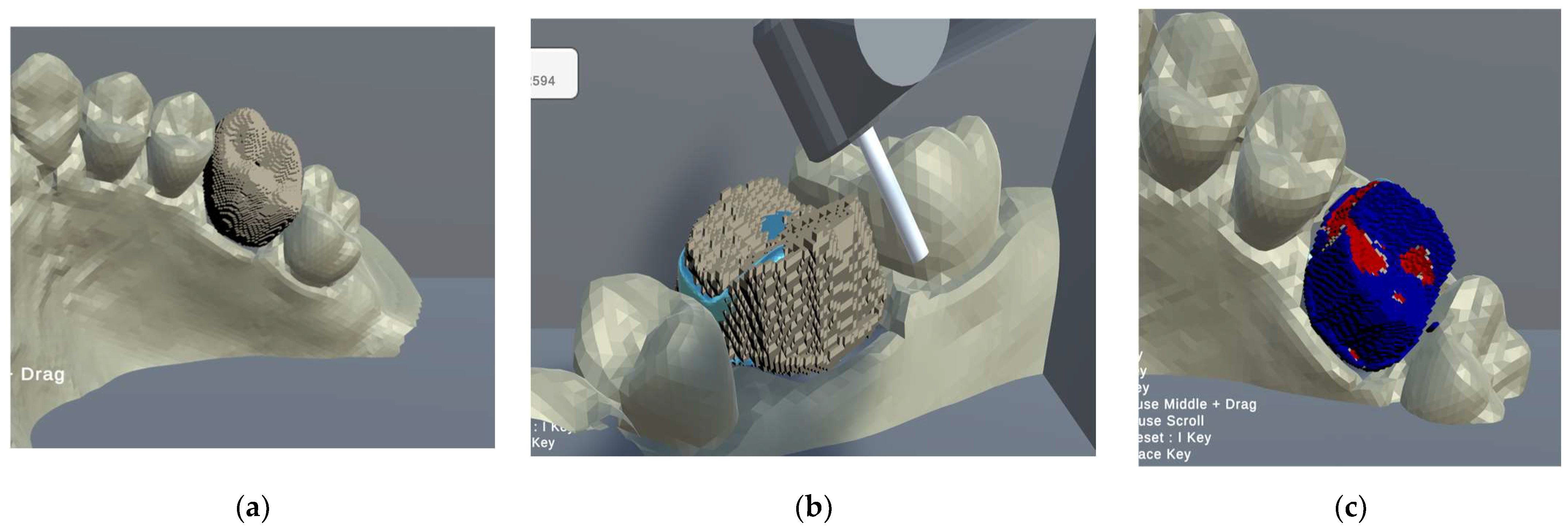
2.1.1. Software
- A function to display the tooth model obtained through the intraoral scanner on the SRD and allows observing the 3D-CG tooth model from various angles via rotation.
- A function that allows observing the morphology of an abutment tooth model by ooking through a 3D-CG tooth model.
- 3.
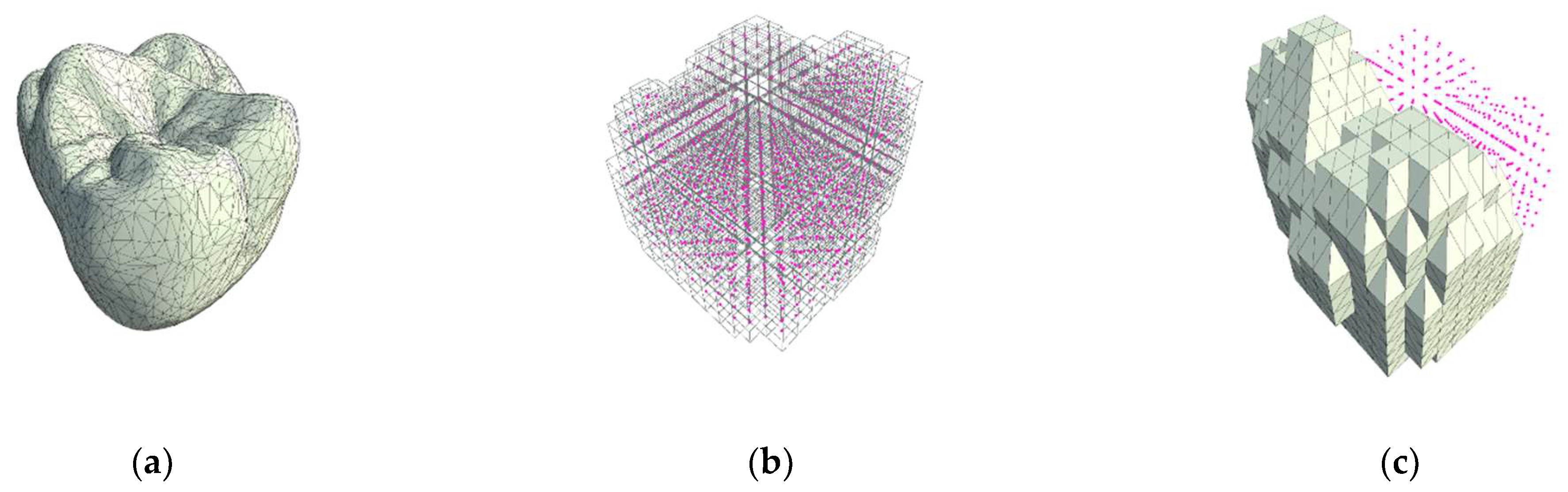
- Function to convert standard tessellation language (STL) data to morphologically deformable data.
- 4.
- The real-time formation of 3D-CG tooth models and their reproduction using haptic technology.
- 5.
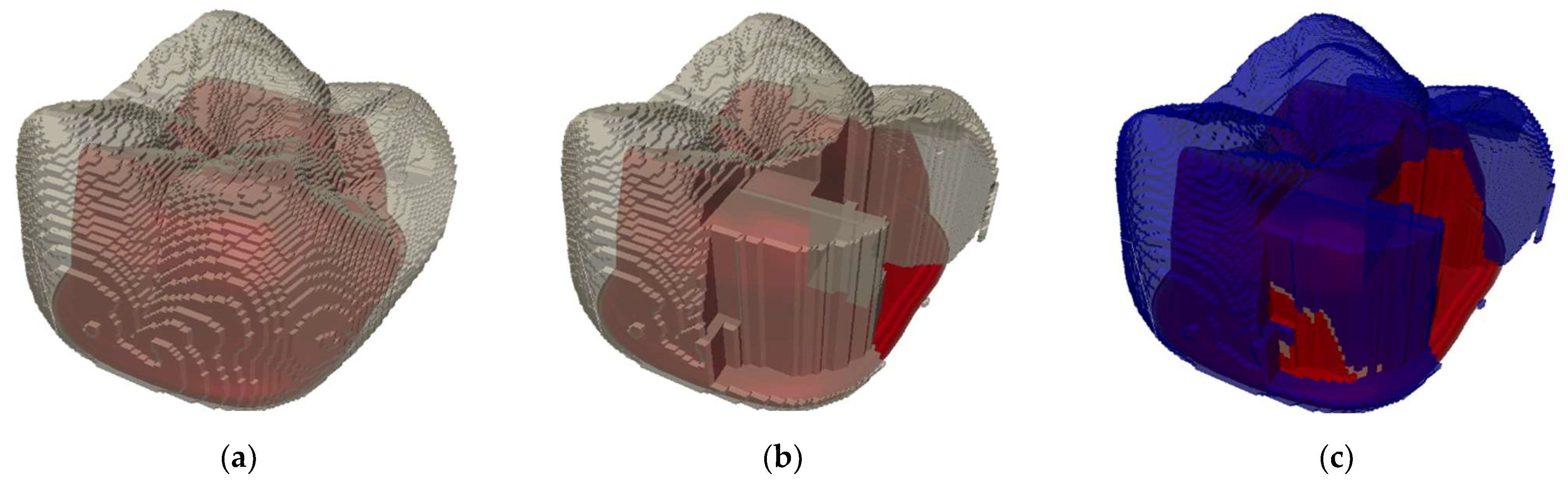
- Automatic objective evaluation after formation.
2.1.2. Tooth Models
2.2. Evaluations by Dentists
2.3. Statistical Processing
3. Results
3.1. Objective Evaluations
3.2. Subjective Evaluations
3.3. Correlation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kramer, G.; Albino, J.; Andrieu, S.; Hendricson, W.; Henson, L.; Horn, B.; Neumann, L.; Young, S. Dental Student Assessment Toolbox. J. Dent. Educ. 2009, 73, 12–35. [Google Scholar] [CrossRef] [PubMed]
- Commission on Dental Accreditation. Accreditation Standards for Dental Education Programs 2023. Available online: https://coda.ada.org/-/media/project/ada-organization/ada/coda/files/predoc_standards.pdf (accessed on 10 September 2024).
- McGivney, G.P. Advanced Education in Prosthodontics. J. Prosthet. Dent. 1990, 64, 334–341. [Google Scholar] [CrossRef] [PubMed]
- Olley, R.C.; Frost Bem, P.M. Clinical and Academic Recommendations for Primary Dental Care Prosthodontics. Br. Dent. J. 2019, 227, 451–455. [Google Scholar] [CrossRef]
- Henzi, D.; Davis, E.; Jasinevicius, R.; Hendricson, W. In the Students’ Own Words: What Are the Strengths and Weaknesses of the Dental School Curriculum? J. Dent. Educ. 2007, 71, 632–645. [Google Scholar] [CrossRef]
- Divaris, K.; Barlow, P.J.; Chendea, S.A.; Cheong, W.S.; Dounis, A.; Dragan, I.F.; Hamlin, J.; Hosseinzadeh, L.; Kuin, D.; Mitrirattanakul, S.; et al. The Academic Environment: The Students’ Perspective. Eur. J. Dent. Educ. 2008, 12 (Suppl. 1), 120–130. [Google Scholar] [CrossRef]
- Uoshima, K.; Akiba, N.; Nagasawa, M. Technical Skill Training and Assessment in Dental Education. Jpn. Dent. Sci. Rev. 2021, 57, 160–163. [Google Scholar] [CrossRef] [PubMed]
- Eliyas, S.; Holsgrove, G.; Gallagher, J.E. Education and Training in Craft Skills Dentistry. Br. Dent. J. 2019, 226, 795–800. [Google Scholar] [CrossRef]
- Pottle, J. Virtual Reality and the Transformation of Medical Education. Future Healthc. J. 2019, 6, 181–185. [Google Scholar] [CrossRef]
- Anglin, J.M.; Sugiyama, T.; Liew, S.-L. Visuomotor Adaptation in Head-Mounted Virtual Reality versus Conventional Training. Sci. Rep. 2017, 7, 45469. [Google Scholar] [CrossRef]
- Muhanna, M.A. Virtual Reality and the CAVE: Taxonomy, Interaction Challenges and Research Directions. J. King Saud Univ. Comput. Inf. Sci. 2015, 27, 344–361. [Google Scholar] [CrossRef]
- Juliano, J.M.; Liew, S.-L. Transfer of Motor Skill between Virtual Reality Viewed Using a Head-Mounted Display and Conventional Screen Environments. J. Neuroeng. Rehabil. 2020, 17, 48. [Google Scholar] [CrossRef] [PubMed]
- Makri, A.; Vlachopoulos, D.; Martina, R.A. Digital Escape Rooms as Innovative Pedagogical Tools in Education: A Systematic Literature Review. Sustainability 2021, 13, 4587. [Google Scholar] [CrossRef]
- Peney, T.; Skarratt, P.A. Increasing the Immersivity of 360° Videos Facilitates Learning and Memory: Implications for Theory and Practice. Educ. Technol. Res. Dev. 2024. [Google Scholar] [CrossRef]
- Barteit, S.; Lanfermann, L.; Bärnighausen, T.; Neuhann, F.; Beiersmann, C. Augmented, Mixed, and Virtual Reality-Based Head-Mounted Devices for Medical Education: Systematic Review. JMIR Serious Games 2021, 9, e29080. [Google Scholar] [CrossRef] [PubMed]
- Tursø-Finnich, T.; Jensen, R.O.; Jensen, L.X.; Konge, L.; Thinggaard, E. Virtual Reality Head-Mounted Displays in Medical Education: A Systematic Review. Simul. Healthc. J. Soc. Simul. Healthc. 2023, 18, 42–50. [Google Scholar] [CrossRef]
- Berthold, D.P.; Muench, L.N.; Rupp, M.-C.; Siebenlist, S.; Cote, M.P.; Mazzocca, A.D.; Quindlen, K. Head-Mounted Display Virtual Reality Is Effective in Orthopaedic Training: A Systematic Review. Arthrosc. Sports Med. Rehabil. 2022, 4, e1843–e1849. [Google Scholar] [CrossRef]
- Lareyre, F.; Chaudhuri, A.; Adam, C.; Carrier, M.; Mialhe, C.; Raffort, J. Applications of Head-Mounted Displays and Smart Glasses in Vascular Surgery. Ann. Vasc. Surg. 2021, 75, 497–512. [Google Scholar] [CrossRef]
- Chen, S.; Zhu, J.; Cheng, C.; Pan, Z.; Liu, L.; Du, J.; Shen, X.; Shen, Z.; Zhu, H.; Liu, J.; et al. Can Virtual Reality Improve Traditional Anatomy Education Programmes? A Mixed-Methods Study on the Use of a 3D Skull Model. BMC Med. Educ. 2020, 20, 395. [Google Scholar] [CrossRef]
- Zitzmann, N.U.; Matthisson, L.; Ohla, H.; Joda, T. Digital Undergraduate Education in Dentistry: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 3269. [Google Scholar] [CrossRef]
- Cayo, C.F.; Cervantes, L.A.; Agramonte, R. VR Systems in Dental Education. Br. Dent. J. 2020, 228, 738. [Google Scholar] [CrossRef]
- Erdilek, D.; Gümüştaş, B.; Güray Efes, B. Digitalization Era of Dental Education: A Systematic Review. Dent. Med. Probl. 2023, 60, 513–525. [Google Scholar] [CrossRef] [PubMed]
- Dzyuba, N.; Jandu, J.; Yates, J.; Kushnerev, E. Virtual and Augmented Reality in Dental Education: The Good, the Bad and the Better. Eur. J. Dent. Educ. 2022; online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Huang, T.-K.; Yang, C.-H.; Hsieh, Y.-H.; Wang, J.-C.; Hung, C.-C. Augmented Reality (AR) and Virtual Reality (VR) Applied in Dentistry. Kaohsiung J. Med. Sci. 2018, 34, 243–248. [Google Scholar] [CrossRef] [PubMed]
- Hadjichristou, C.; Kokoti, M.; Bakopoulou, A. Haptics in Fixed Prosthodontics and Their Role in Dental Education: A Literature Review. J. Dent. Educ. 2024, 88, 1020–1028. [Google Scholar] [CrossRef] [PubMed]
- McAlpin, E.; Levine, M.; Brenner, C.; Opazo, C.; Bathini, S.; Choi, S.J.V.; Louisville, M.; Grandhi, U. Evaluating the Effectiveness of a Virtual Reality Simulation for Preclinical Local Anaesthesia Dental Education. Eur. J. Dent. Educ. 2022; online ahead of print. [Google Scholar] [CrossRef]
- Vincent, M.; Joseph, D.; Amory, C.; Paoli, N.; Ambrosini, P.; Mortier, É.; Tran, N. Contribution of Haptic Simulation to Analogic Training Environment in Restorative Dentistry. J. Dent. Educ. 2020, 84, 367–376. [Google Scholar] [CrossRef]
- Perry, S.; Bridges, S.M.; Burrow, M.F. A Review of the Use of Simulation in Dental Education. Simul. Healthc. J. Soc. Simul. Healthc. 2015, 10, 31–37. [Google Scholar] [CrossRef]
- Felszeghy, S.; Huhtela, O.; Manninen, K.; Mäenpää, M.; Banafa, A.; Liukkonen, M.; Mutluay, M. VR-Haptic and Phantom Head Dental Training: Does the Order Matter? A Comparative Study from a Preclinical Fixed Prostho-Dontics Course. Int. J. Comput. Dent. 2023; online ahead of print. [Google Scholar] [CrossRef]
- Patil, S.; Bhandi, S.; Awan, K.H.; Licari, F.W.; Di Blasio, M.; Ronsivalle, V.; Cicciù, M.; Minervini, G. Effectiveness of Haptic Feedback Devices in Preclinical Training of Dental Students—A Systematic Review. BMC Oral Health 2023, 23, 739. [Google Scholar] [CrossRef]
- Li, Y.; Ye, H.; Wu, S.; Zhao, X.; Liu, Y.; Lv, L.; Zhang, P.; Zhang, X.; Zhou, Y. Mixed Reality and Haptic-Based Dental Simulator for Tooth Preparation: Research, Development, and Preliminary Evaluation. JMIR Serious Games 2022, 10, e30653. [Google Scholar] [CrossRef]
- Moro, C.; Štromberga, Z.; Raikos, A.; Stirling, A. The Effectiveness of Virtual and Augmented Reality in Health Sciences and Medical Anatomy. Anat. Sci. Educ. 2017, 10, 549–559. [Google Scholar] [CrossRef]
- Chang, E.; Kim, H.T.; Yoo, B. Virtual Reality Sickness: A Review of Causes and Measurements. Int. J. Human Computer Interact. 2020, 36, 1658–1682. [Google Scholar] [CrossRef]
- Trinidad-Fernández, M.; Bossavit, B.; Salgado-Fernández, J.; Abbate-Chica, S.; Fernández-Leiva, A.J.; Cuesta-Vargas, A.I. Head-Mounted Display for Clinical Evaluation of Neck Movement Validation with Meta Quest 2. Sensors 2023, 23, 3077. [Google Scholar] [CrossRef] [PubMed]
- Kaluschke, M.; Yin, M.S.; Haddawy, P.; Suebnukarn, S.; Zachmann, G. The Effect of 3D Stereopsis and Hand-Tool Alignment on Learning Effectiveness and Skill Transfer of a VR-Based Simulator for Dental Training. PLoS ONE 2023, 18, e0291389. [Google Scholar] [CrossRef] [PubMed]
- Waller, D.; Richardson, A.R. Correcting Distance Estimates by Interacting with Immersive Virtual Environments: Effects of Task and Available Sensory Information. J. Exp. Psychol. Appl. 2008, 14, 61–72. [Google Scholar] [CrossRef] [PubMed]
- Guzsvinecz, T.; Perge, E.; Szűcs, J. Examining the Results of Virtual Reality-Based Egocentric Distance Estimation Tests Based on Immersion Level. Sensors 2023, 23, 3138. [Google Scholar] [CrossRef]
- Naceri, A.; Chellali, R.; Hoinville, T. Depth Perception Within Peripersonal Space Using Head-Mounted Display. Presence Teleoper. Virtual Environ. 2011, 20, 254–272. [Google Scholar] [CrossRef]
- Itamiya, T.; To, M.; Oguchi, T.; Fuchida, S.; Matsuo, M.; Hasegawa, I.; Kawana, H.; Kimoto, K. A Novel Anatomy Education Method Using a Spatial Reality Display Capable of Stereoscopic Imaging with the Naked Eye. Appl. Sci. 2021, 11, 7323. [Google Scholar] [CrossRef]
- Tsukuda, T.; Mutoh, N.; Nakano, A.; Itamiya, T.; Tani-Ishii, N. Study of Root Canal Length Estimations by 3D Spatial Reproduction with Stereoscopic Vision. Appl. Sci. 2023, 13, 8651. [Google Scholar] [CrossRef]
- Unity. Available online: https://unity.com (accessed on 10 September 2024).
- 3D System Touch. Available online: https://www.3dsystems.com/haptics-devices/touch (accessed on 10 September 2024).
- 3shape TRIOS 3 WIRED. Available online: https://www.3shape.com/scanners/trios-3 (accessed on 10 September 2024).
- Blender. Available online: https://www.blender.org (accessed on 10 September 2024).
- R-Project. Available online: https://www.r-project.org (accessed on 10 September 2024).
- Ariwa, M.; Itamiya, T.; Koizumi, S.; Yamaguchi, T. Comparison of the Observation Errors of Augmented and Spatial Reality Systems. Appl. Sci. 2021, 11, 12076. [Google Scholar] [CrossRef]
- Guyer, S.E. Multiple Preparations for Fixed Prosthodontics. J. Prosthet. Dent. 1970, 23, 529–553. [Google Scholar] [CrossRef] [PubMed]
- Jørgensen, K.D. The Relationship between Retention and Convergence Angle in Cemented Veneer Crowns. Acta Odontol. Scand. 1955, 13, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Goodacre, C.J. Designing Tooth Preparations for Optimal Success. Dent. Clin. N. Am. 2004, 48, 359–385. [Google Scholar] [CrossRef] [PubMed]
- Selvakumar, H.; Kavitha, S.; Vijayakumar, R.; Eapen, T.; Bharathan, R. Study of Pulp Chamber Morphology of Primary Mandibular Molars Using Spiral Computed Tomography. J. Contemp. Dent. Pract. 2014, 15, 726–729. [Google Scholar] [CrossRef]
- Velmurugan, N.; Venkateshbabu, N.; Abarajithan, M.; Kandaswamy, D. Evaluation of the Pulp Chamber Size of Human Maxillary First Molars: An Institution Based in Vitro Study. Indian J. Dent. Res. 2008, 19, 92–94. [Google Scholar] [CrossRef]
- Sadid-Zadeh, R.; Farsaii, A.; Goodarzi, A.; Davis, E.L. Loss of Tooth Structure Associated with Preparation for Two Monolithic CAD-CAM Complete Coverage Restorations. J. Prosthet. Dent. 2018, 120, 403–408. [Google Scholar] [CrossRef]



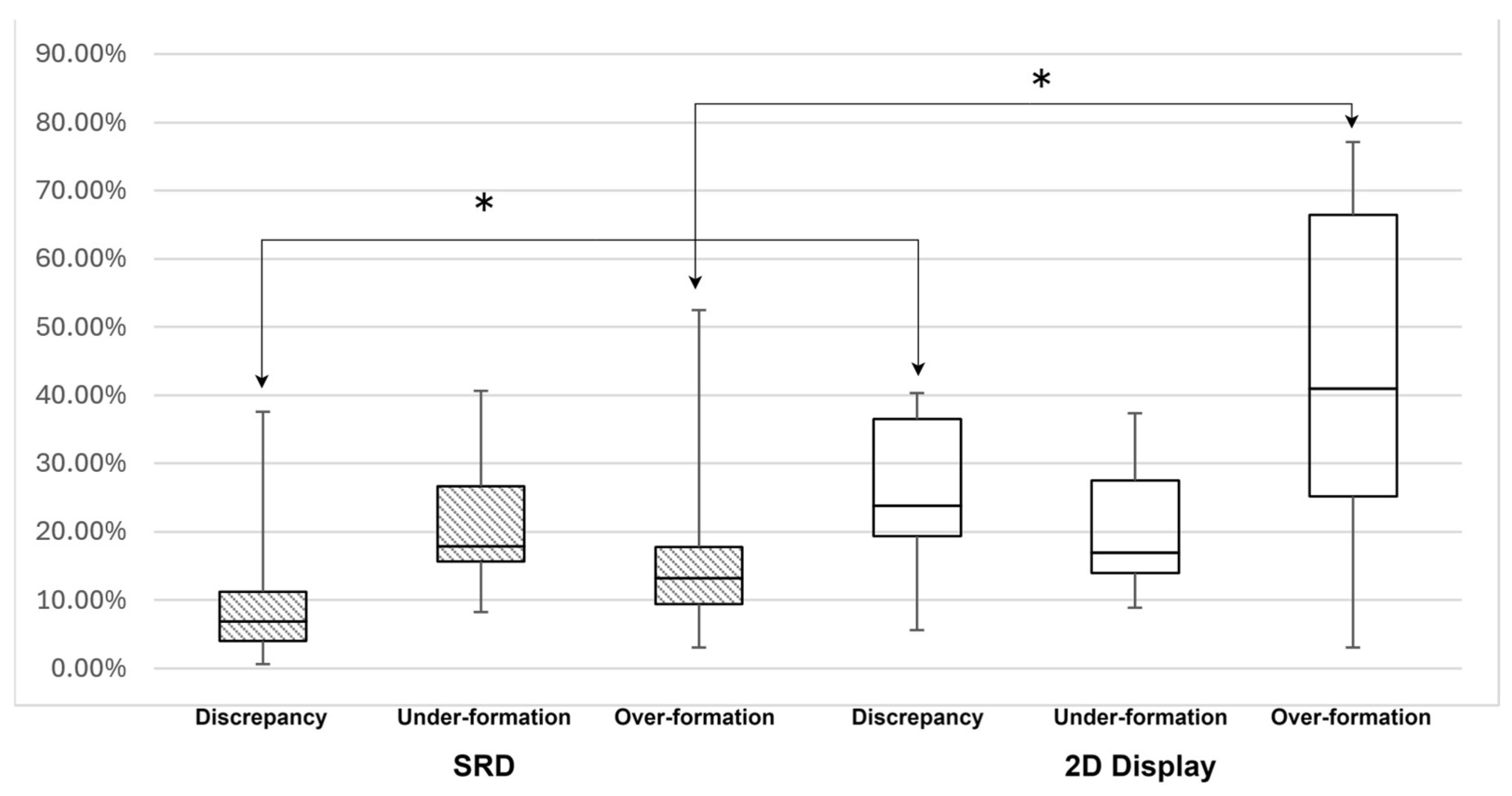
| Device | Evaluation Items | Between the Number of Voxels of the Exemplar Abutment Tooth and Those Created by the Participants | |||
|---|---|---|---|---|---|
| Average | (SD) | Min | Max | ||
| SRD | Discrepancy | 10.49% | 9.98% | 0.61% | 37.57% |
| Under-formation | 21.30% | 8.26% | 8.30% | 40.65% | |
| Over-formation | 17.49% | 12.80% | 3.13% | 52.43% | |
| 2D Display | Discrepancy | 24.89% | 10.92% | 5.61% | 40.27% |
| Under-formation | 20.55% | 9.07% | 8.96% | 37.32% | |
| Over-formation | 41.98% | 23.30% | 3.14% | 77.15% | |
| Category | Average | (SD) | Min | Max |
|---|---|---|---|---|
| Application | 4.37 | 0.23 | 4.00 | 4.90 |
| SRD | 4.28 | 0.31 | 3.75 | 4.75 |
| Physical harm | 1.80 | 0.81 | 1.00 | 3.00 |
| Academic improvement | 4.37 | 0.27 | 4.00 | 4.87 |
| Correlation Coefficient | p-Value | ||
|---|---|---|---|
| SRD | Over-formation | −0.183 | 0.440 |
| Under-formation | 0.475 | 0.034 | |
| Discrepancy | 0.505 | 0.023 | |
| 2D Display | Over-formation | −0.388 | 0.090 |
| Under-formation | 0.598 | 0.005 | |
| Discrepancy | −0.221 | 0.349 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tomita, R.; Nakano, A.; Kawanishi, N.; Hoshi, N.; Itamiya, T.; Kimoto, K. Abutment Tooth Formation Simulator for Naked-Eye Stereoscopy. Appl. Sci. 2024, 14, 8367. https://doi.org/10.3390/app14188367
Tomita R, Nakano A, Kawanishi N, Hoshi N, Itamiya T, Kimoto K. Abutment Tooth Formation Simulator for Naked-Eye Stereoscopy. Applied Sciences. 2024; 14(18):8367. https://doi.org/10.3390/app14188367
Chicago/Turabian StyleTomita, Rintaro, Akito Nakano, Norishige Kawanishi, Noriyuki Hoshi, Tomoki Itamiya, and Katsuhiko Kimoto. 2024. "Abutment Tooth Formation Simulator for Naked-Eye Stereoscopy" Applied Sciences 14, no. 18: 8367. https://doi.org/10.3390/app14188367
APA StyleTomita, R., Nakano, A., Kawanishi, N., Hoshi, N., Itamiya, T., & Kimoto, K. (2024). Abutment Tooth Formation Simulator for Naked-Eye Stereoscopy. Applied Sciences, 14(18), 8367. https://doi.org/10.3390/app14188367






