Depth of Cure, Surface Characteristics, Hardness, and Brushing Wear of 4 Direct Restorative Materials in Paediatric Dentistry
Abstract
:1. Introduction
2. Materials and Methods
- RivaSilver: SDI Limited, 5-9 Brunsdon Street, Bayswater, Victoria 3153, Australia.
- SDR flow+: Dentsply Sirona, 13320 Ballantyne Corporate Place, Charlotte, NC 28277, USA.
- Vertise Flow: Kerr, 1717 West Collins Avenue, Orange, CA 92867, USA.
- FUJI IX GP FAST: GC EUROPE N.V., Interleuvenlaan 33, 3001 Leuven, Belgium.
2.1. Polymerization Depth
2.2. Hardness
2.3. Wear Resistance
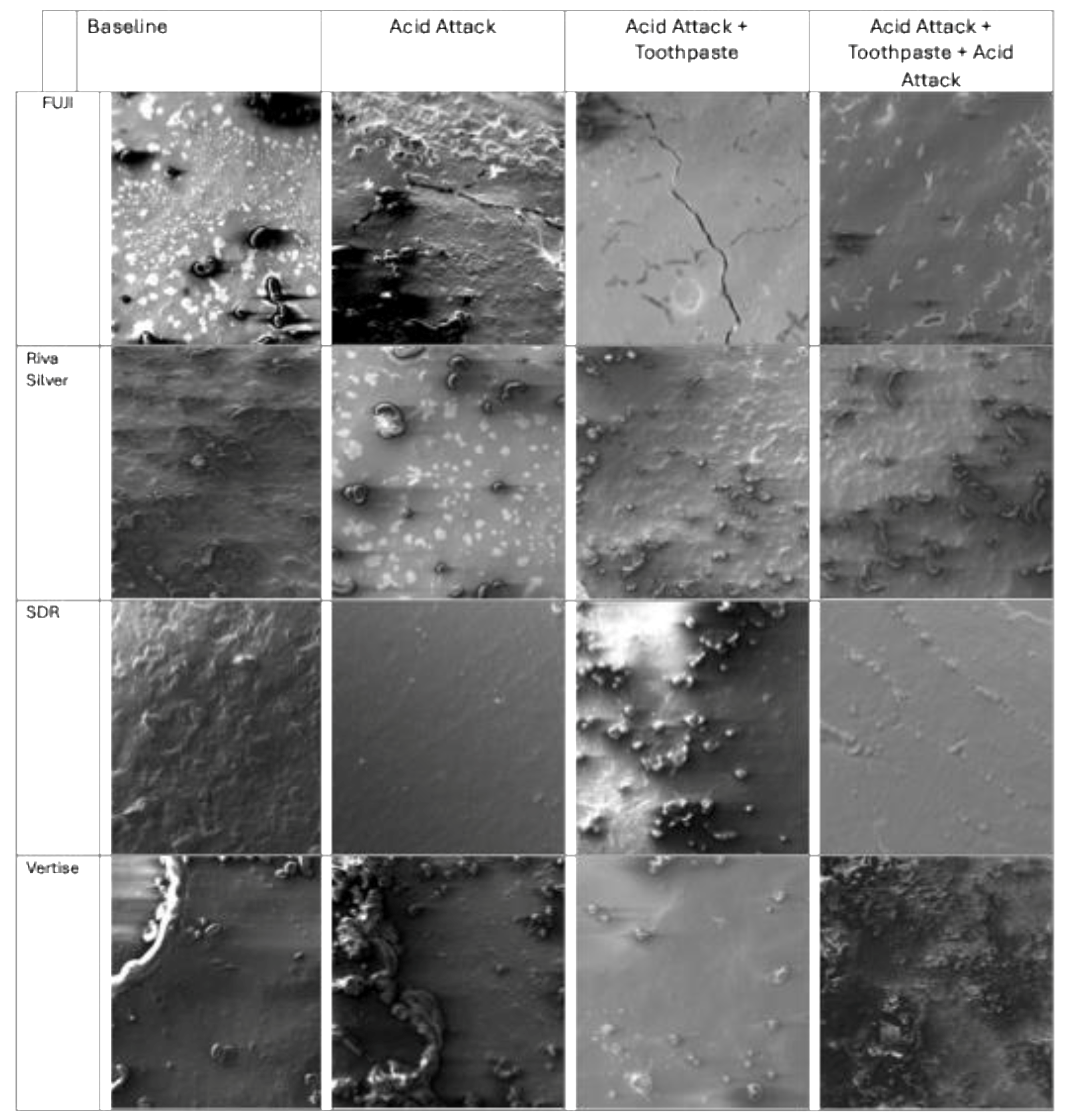
2.4. Acid Resistance
2.5. Surface Roughness
2.6. Scanning Electron Microscopy (SEM)
2.7. Statistical Analysis
3. Results
3.1. Polymerization Depth
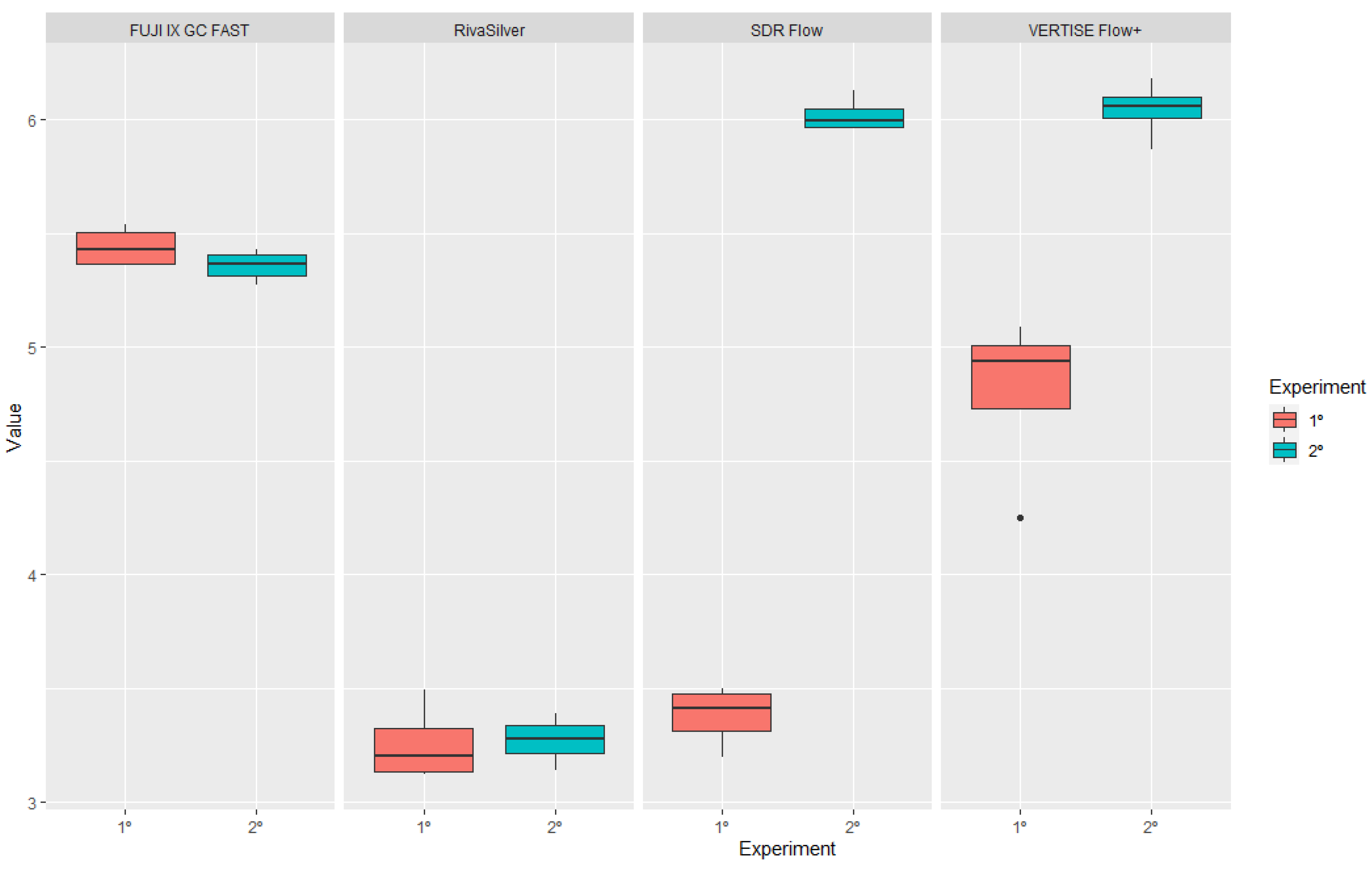
3.2. Hardness
3.3. Surface Roughness after Acid Treatment
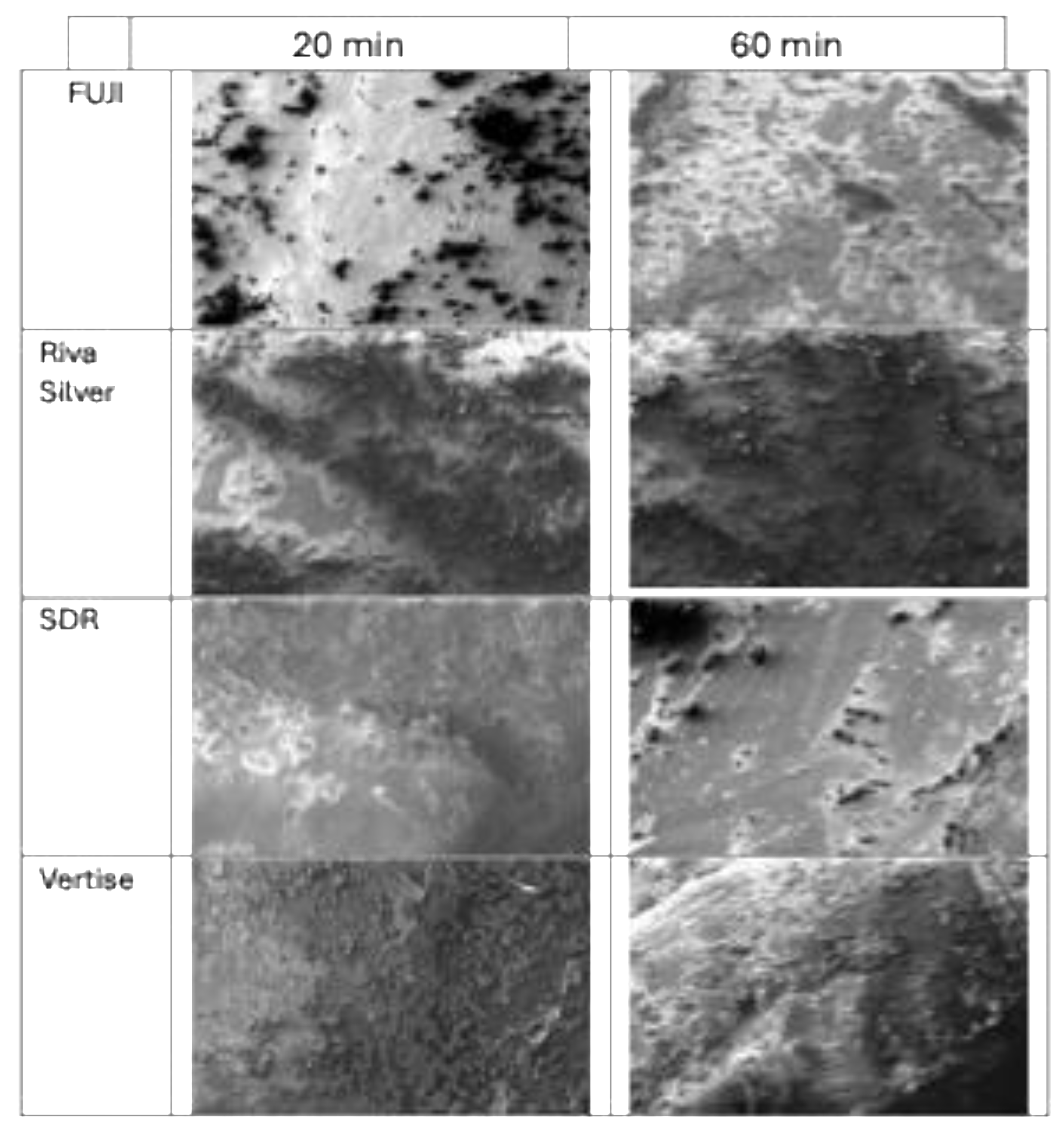
3.4. Brushing Wear Resistance
4. Discussion
5. Limitation of the Study
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Donly, K.J. Restorative dentistry for children. Dent. Clin. N. Am. 2013, 57, 75–82. [Google Scholar] [CrossRef] [PubMed]
- Nowak, A.; Christensen, J.; Mabry, T.; Townsend, J.; Wells, M. Pediatric Dentistry: Infancy through Adolescence, 6th ed.; Elsevier: Philadelphia, PA, USA, 2019; p. 295. [Google Scholar]
- Tortora, G.; Farronato, M.; Gaffuri, F.; Carloni, P.; Occhipinti, C.; Tucci, M.; Cenzato, N.; Maspero, C. Survey of oral hygiene habits and knowledge among school children: A cross-sectional study from Italy. Eur. J. Paediatr. Dent. 2023, 24, 194–200. [Google Scholar] [PubMed]
- Almuhaiza, M. Glass-ionomer cements in restorative dentistry: A critical appraisal. J. Contemp. Dent. Pract. 2016, 17, 331–336. [Google Scholar] [CrossRef] [PubMed]
- Rachmia Riva, Y.; Fauziyah Rahman, S. Dental composite resin: A review. AIP Conf. Proc. 2019, 2193, 020011. [Google Scholar]
- Gupta, R.; Hegde, J.; Prakash, V.; Srirekha, A. Concise Conservative Dentistry and Endodontics; Elsevier: Chennai, India, 2019; pp. 260–268. [Google Scholar]
- Shen, C.; Rawls, H.R.; Esquivel-Upshaw, J.F. Philippe’s Science of Dental Materials; Elsevier: Amsterdam, The Netherlands, 2022; pp. 89–104. [Google Scholar]
- Li, X.; Pongprueksa, P.; Meerbeek, B.V.; De Munck, J. Curing profile of bulk-fill resin-based composites. J. Dent. 2015, 43, 664–672. [Google Scholar] [CrossRef]
- Celik, E.U.; Kucukyilmaz, E.; Savas, S. Effect of different surface pre-treatment methods on the microleakage of two different self-adhesive composites in Class V cavities. Eur. J. Paediatr. Dent. 2015, 16, 33–38. [Google Scholar]
- Ilie, N.; Hickel, R. Resin composite restorative materials. Aust. Dent. J. 2011, 56, 59–66. [Google Scholar] [CrossRef]
- Schneider, L.; Cavalcante, L.; Silikas, N. Shrinkage stresses generated during resin-composite applications: A review. J. Dent. Biomech. 2020, 2020, 131630. [Google Scholar] [CrossRef]
- Riggio, M.; Piazza, M.; Kasal, B.; Tannert, T. Hardness test in situ assessment of structural timber. In RILEM State of the Art Reports; Springer: Dordrecht, The Netherlands, 2012; Volume 7. [Google Scholar]
- Heintze, S.D.; Forjanic, M. Surface roughness of different dental materials before and after simulated toothbrushing in vitro. Oper. Dent. 2005, 5, 30–36. [Google Scholar]
- Gharechahi, M.; Moosavi, H.; Forghani, M. Effect of surface roughness and materials composition. J. Biomater. Nanobiotechnol. 2012, 3, 541–546. [Google Scholar] [CrossRef]
- Ceyhan, D.; Akdik, C.; Kirzioglu, Z. An educational programme designed for the evaluation of effectiveness of two tooth brushing techniques in preschool children. Eur. J. Paediatr. Dent. 2018, 19, 181–186. [Google Scholar]
- Lussi, A.; Schlueter, N.; Rakhmatullina, E.; Ganss, C. Dental erosion: An overview with emphasis on chemical and histopathological aspects. Caries Res. 2011, 45, 2–12. [Google Scholar] [CrossRef]
- Tellefsen, G.; Liljeborg, A.; Johannsen, G. How do dental materials react on tooth brushing? Dentistry 2005, 5, 341–346. [Google Scholar] [CrossRef]
- ISO-Standards ISO 4049; Dentistry Polymer-Based Restorative Materials. International Organization for Standardization: Geneva, Switzerland, 2019; pp. 1–28.
- Zamfirova, G.; Dimitrova, A. Some methodological contributions to the Vickers microhardness technique. Polym. Test. 2000, 19, 533–542. [Google Scholar] [CrossRef]
- Mazzoleni, S.; Gargani, A.; Parcianello, R.G.; Pezzato, L.; Bertolini, R.; Zuccon, A.; Stellini, E.; Ludovichetti, F.S. Protection against dental erosion and the remineralization capacity of non-fluoride toothpaste, fluoride toothpaste and fluoride varnish. Appl. Sci. 2023, 13, 1849. [Google Scholar] [CrossRef]
- ISO 4288:1996; Geometrical Product Specifications (GPS)—Surface Texture: Profile Method—Rules and Procedures for the Assessment of Surface Texture. ISO: Geneva, Switzerland, 1996.
- Ludovichetti, F.S.; Lucchi, P.; Zambon, G.; Pezzato, L.; Bertolini, R.; Zerman, N.; Stellini, E.; Mazzoleni, S. Depth of cure, hardness, roughness and filler dimension of bulk-fill flowable, conventional flowable and high-strength universal injectable composites: An in vitro study. Nanomaterials 2022, 12, 1951. [Google Scholar] [CrossRef]
- Sampaio, C.S.; Chiu, K.J.; Farrokhmanesh, E.; Janal, M.; Puppin-Rontani, R.M.; Giannini, M.; Bonfante, E.A.; Coelho, P.G.; Hirata, R. Microcomputed tomography evaluation of polymerization shrinkage of Class I flowable resin composite restorations. Oper. Dent. 2017, 42, E16–E23. [Google Scholar] [CrossRef]
- Vichi, A.; Margvelashvili, M.; Goracci, C.; Papacchini, F.; Ferrari, M. Bonding and sealing ability of a new self-adhering flowable composite resin in class I restorations. Clin. Oral. Investig. 2013, 17, 1497–1506. [Google Scholar] [CrossRef]
- Garouschi, S.; Vallittu, P.; Shinya, A.; Lassila, L. Influence of increment thickness on light transmission, degree of conversion and micro hardness of bulk-fill composites. Odontology 2016, 104, 291–297. [Google Scholar] [CrossRef]
- Ünal, M.; Candan, M.; İpek, İ.; Küçükoflaz, M.; Özer, A. Evaluation of the microhardness of different resin-based dental restorative materials treated with gastric acid: Scanning electron microscopy–energy dispersive X-ray spectroscopy analysis. Microsc. Res. Tech. 2021, 84, 2140–2148. [Google Scholar] [CrossRef]
- Azizi, F.; Ezoji, F.; Khafri, S.; Esmaeili, B. Surface micro-hardness and wear resistance of a self-adhesive flowable composite in comparison to conventional flowable composites. Front. Dent. 2023, 20, 10. [Google Scholar] [CrossRef]
- Rashidian, A.; Saghiri, M.A.; Bigloo, S.M.; Afsharianzadeh, M. Effect of fluoride gel on microhardness of flowable composites: An in vitro study. J. Dent. Sch. Shahid Beheshti Univ. Med. Sci. 2014, 32, 16–22. [Google Scholar]
- Czasch, P.; Ilie, N. In-vitro comparison of mechanical properties and degree of cure of a self-adhesive and four novel flowable composites. J. Adhes. Dent. 2013, 42, 131–137. [Google Scholar]
- Cabello Malagón, I.; Cánovas Hernández, B.; Martínez Hernández, E.; Serna-Muñoz, C.; Pérez-Silva, A.; Ortiz-Ruiz, A.J. Analysis of the porosity and microhardness of glass ionomer cements. Mater. Sci. 2022, 28, 113–119. [Google Scholar] [CrossRef]
- Yin, I.X.; Zhao, I.S.; Mei, M.L.; Li, Q.; Yu, O.Y.; Chu, C.H. Use of silver nanomaterials for caries prevention: A concise review. Int. J. Nanomed. 2020, 15, 3181–3191. [Google Scholar] [CrossRef]
- Sidhu, S.K.; Nicholson, J.W. A review of glass-ionomer cements. Clin. Dent. J. Funct. Biomater. 2016, 7, 16. [Google Scholar]
- Nair, V.S.; Sainudeen, S.; Padmanabhan, P.; Vijayashankar, L.V.; Sujathan, U.; Pillai, R. Three-dimensional evaluation of surface roughness of resin composites after finishing and polishing. J. Conserv. Dent. 2016, 19, 5–91. [Google Scholar]
- Mulic, A.; Fredriksen, Ø.; Jacobsen, I.D.; Tveit, A.B.; Espelid, I.; Crossner, C.G. Dental erosion: Prevalence and severity among 16-year-old adolescents in Troms, Norway. Eur. J. Paediatr. Dent. 2016, 17, 197–201. [Google Scholar]
- Pini, N.I.; Lima, D.A.; Lovadino, J.R.; Ganss, C.; Schlueter, N. In vitro efficacy of experimental chitosan-containing solutions as anti-erosive agents in enamel. Caries Res. 2016, 50, 337–345. [Google Scholar] [CrossRef]
- Cruz, N.V.; Pessan, J.P.; Manarelli, M.M.; Souza, M.D.; Delbem, A.C. In vitro effect of low-fluoride toothpastes containing sodium trimetaphosphate on enamel erosion. Arch. Oral. Biol. 2015, 60, 1231–1236. [Google Scholar] [CrossRef]
- Kelten, O.S.; Hepdeniz, O.K.; Tuncer, Y.; Kankaya, D.A.; Gurdal, O. Effect of surface characteristic of different restorative materials containing glass ionomer on Streptococcus mutans biofilm. Niger. J. Clin. Pract. 2020, 23, 957–964. [Google Scholar]
- Alijamhan, A.; Habib, S.R.; AlSarhan, M.A.; AlZahrani, B.; AlOtaibi, H.; AlSunaidi, N. Effect of finishing and polishing on the surface roughness of bulk-fill composites. Open Dent. J. 2021, 15, 25–31. [Google Scholar] [CrossRef]
- Marghalani, H.Y. Effect of filler particles on surface roughness of experimental composite series. J. Appl. Oral. Sci. 2010, 18, 59–67. [Google Scholar] [CrossRef]
- Yap, A.U.J.; Teo, J.C.M.; Teoh, S.H. Comparative wear resistance of reinforced glass ionomer restorative materials. Oper. Dent. 2000, 26, 343–348. [Google Scholar]
- Dionysopoulos, D.; Tolidis, K.; Sfeikos, T.; Karanasiou, C.; Parisi, X. Evaluation of surface microhardness and abrasion resistance of two dental glass ionomer cement materials after radiant heat treatment. Adv. Mater. Sci. Eng. 2017, 2017, 1–9. [Google Scholar] [CrossRef]
- Ruivo, M.A.; Pacheco, R.R.; Sebold, M.; Giannini, M. Surface roughness and filler particles characterization of resin-based composites. Microsc. Res. Tech. 2019, 82, 1756–1767. [Google Scholar] [CrossRef]
- Amura, Y.; Kakuta, K.; Ogura, H. Wear and mechanical properties of composite resins consisting of different filler particles. Odontology 2013, 101, 156–169. [Google Scholar]
- O’Neill, C.; Kreplak, L.; Rueggeberg, F.A.; Labrie, D.; Shimokawa, C.A.K.; Price, R.B. Effect of tooth brushing on gloss retention and surface roughness of five bulk-fill resin composites. J. Esthet. Restor. Dent. 2018, 30, 59–69. [Google Scholar] [CrossRef]


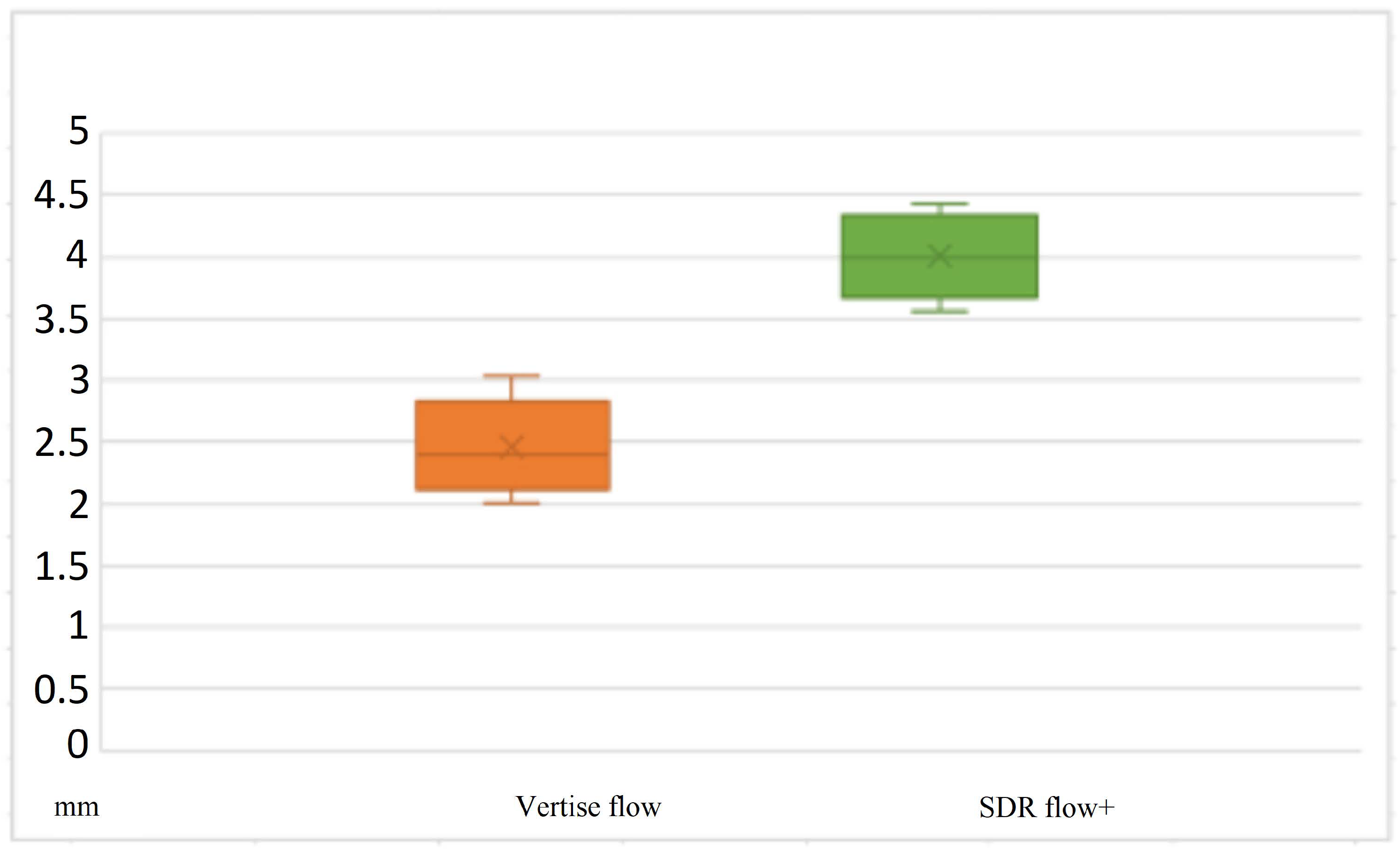

| Vertise Flow | Meas.1 | Meas.2 | Meas.3 | Mean | SDR Flow+ | Meas.1 | Meas.2 | Meas.3 | Mean |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2.49 | 2.45 | 2.38 | 2.44 | 1 | 3.86 | 4.02 | 3.99 | 3.96 |
| 2 | 2.35 | 2.51 | 2.35 | 2.40 | 2 | 4.23 | 4.41 | 4.3 | 4.31 |
| 3 | 2.3 | 2.37 | 2.49 | 2.38 | 3 | 3.53 | 3.56 | 3.61 | 3.56 |
| 4 | 2.12 | 2.2 | 2.10 | 2.14 | 4 | 4.15 | 4.12 | 4.11 | 4.12 |
| 5 | 2.28 | 2.37 | 2.43 | 2.36 | 5 | 3.80 | 3.79 | 3.74 | 3.78 |
| 6 | 2.27 | 2.46 | 2.44 | 2.39 | 6 | 3.99 | 3.86 | 4.01 | 3.94 |
| 7 | 2.65 | 2.56 | 2.22 | 2.48 | 7 | 4.18 | 4.11 | 3.98 | 4.10 |
| 8 | 2.58 | 2.64 | 2.6 | 2.60 | 8 | 3.96 | 4.08 | 4.11 | 4.05 |
| 9 | 2.65 | 2.58 | 2.62 | 2.61 | 9 | 4.47 | 4.49 | 4.30 | 4.42 |
| 10 | 2.77 | 2.76 | 2.68 | 2.74 | 10 | 4.27 | 4.37 | 4.25 | 4.3 |
| 11 | 2.47 | 2.64 | 2.37 | 2.49 | 11 | 3.88 | 3.86 | 3.85 | 3.85 |
| 12 | 3.05 | 3.06 | 2.97 | 3.04 | 12 | 4.51 | 4.39 | 4.4 | 4.43 |
| 13 | 2.29 | 2.25 | 2.29 | 2.27 | 13 | 3.71 | 3.66 | 3.95 | 3.77 |
| 14 | 1.94 | 2.05 | 2.06 | 2.01 | 14 | 3.95 | 3.93 | 3.75 | 3.88 |
| 15 | 2.27 | 2.17 | 2.24 | 2.22 | 15 | 4.09 | 4.13 | 4.1 | 4.10 |
| No Treatment (A) (Mean and Dv. Std.) | 20 min Brushing (B) (Mean and Dv. Std.) | 60 min Brushing (C) (Mean and Dv. Std.) | |
|---|---|---|---|
| RivaSilver | 90 ± 3 | 110 ± 4 | 110 ± 5 |
| SDR Flow+ | 515 ± 10 | 401 ± 12 | 480 ± 15 |
| Vertise Flow | 498 ± 8 | 439 ± 7 | 426 ± 9 |
| FUJI IX GP FAST | 92 ± 2 | 110 ± 3 | 116 ± 14 |
| Experiment Number | Group 1 | Group 2 | p-Value |
|---|---|---|---|
| 1 | FUJI IX GP FAST | RivaSilver | <0.001 |
| 1 | FUJI IX GP FAST | SDR flow+ | <0.001 |
| 1 | RivaSilver | SDR flow+ | <0.001 |
| 1 | FUJI IX GP FAST | Vertise Flow | <0.001 |
| 1 | RivaSilver | Vertise Flow | <0.001 |
| 1 | SDR flow+ | Vertise Flow | <0.001 |
| 2 | FUJI IX GP FAST | RivaSilver | 0.125 |
| 2 | FUJI IX GP FAST | SDR flow+ | <0.001 |
| 2 | RivaSilver | SDR flow+ | <0.001 |
| 2 | FUJI IX GP FAST | Vertise Flow | <0.001 |
| 2 | RivaSilver | Vertise Flow | <0.001 |
| 2 | SDR flow+ | Vertise Flow | <0.001 |
| 3 | FUJI IX GP FAST | RivaSilver | <0.001 |
| 3 | FUJI IX GP FAST | SDR flow+ | <0.001 |
| 3 | RivaSilver | SDR flow+ | <0.001 |
| 3 | FUJI IX GP FAST | Vertise Flow | <0.001 |
| 3 | RivaSilver | Vertise Flow | <0.001 |
| 3 | SDR flow+ | Vertise Flow | <0.001 |
| Variabile | Group 1 | Group 2 | p-Value |
|---|---|---|---|
| FUJI IX GP FAST | 1 | 2 | 0.068 |
| FUJI IX GP FAST | 1 | 3 | 0.246 |
| FUJI IX GP FAST | 1 | 4 | 0.340 |
| FUJI IX GP FAST | 2 | 3 | 0.251 |
| FUJI IX GP FAST | 2 | 4 | 1.000 |
| FUJI IX GP FAST | 3 | 4 | 0.588 |
| RivaSilver | 1 | 2 | 0.007 |
| RivaSilver | 1 | 3 | 1.000 |
| RivaSilver | 1 | 4 | 0.003 |
| RivaSilver | 2 | 3 | 0.022 |
| RivaSilver | 2 | 4 | 0.050 |
| RivaSilver | 3 | 4 | 0.002 |
| SDR flow+ | 1 | 2 | 0.000 |
| SDR flow+ | 1 | 3 | 0.002 |
| SDR flow+ | 1 | 4 | 1.000 |
| SDR flow+ | 2 | 3 | 0.000 |
| SDR flow+ | 2 | 4 | 0.076 |
| SDR flow+ | 3 | 4 | 0.003 |
| Vertise Flow | 1 | 2 | 0.005 |
| Vertise Flow | 1 | 3 | 0.281 |
| Vertise Flow | 1 | 4 | 0.001 |
| Vertise Flow | 2 | 3 | 0.002 |
| Vertise Flow | 2 | 4 | 0.016 |
| Vertise Flow | 3 | 4 | 0.027 |
| Experiment Number | Group 1 | Group 2 | p-Value |
|---|---|---|---|
| 1 | FUJI IX GP FAST | RivaSilver | 0.019 |
| 1 | FUJI IX GP FAST | SDR flow+ | 0.003 |
| 1 | RivaSilver | SDR flow+ | 0.276 |
| 1 | FUJI IX GP FAST | Vertise Flow | 0.226 |
| 1 | RivaSilver | Vertise Flow | 0.261 |
| 1 | SDR flow+ | Vertise Flow | 0.069 |
| 2 | FUJI IX GP FAST | RivaSilver | 0.001 |
| 2 | FUJI IX GP FAST | SDR flow+ | 0.001 |
| 2 | RivaSilver | SDR flow+ | 0.013 |
| 2 | FUJI IX GP FAST | Vertise Flow | 0.001 |
| 2 | RivaSilver | Vertise Flow | 0.211 |
| 2 | SDR flow+ | Vertise Flow | 0.211 |
| 3 | FUJI IX GP FAST | RivaSilver | 0.005 |
| 3 | FUJI IX GP FAST | SDR flow+ | 0.001 |
| 3 | RivaSilver | SDR flow+ | 0.001 |
| 3 | FUJI IX GP FAST | Vertise Flow | 0.043 |
| 3 | RivaSilver | Vertise Flow | 0.000 |
| 3 | SDR flow+ | Vertise Flow | 0.001 |
| 4 | FUJI IX GP FAST | RivaSilver | 0.001 |
| 4 | FUJI IX GP FAST | SDR flow+ | 0.042 |
| 4 | RivaSilver | SDR flow+ | 0.001 |
| 4 | FUJI IX GP FAST | Vertise Flow | 0.339 |
| 4 | RivaSilver | Vertise Flow | 0.001 |
| 4 | SDR flow+ | Vertise Flow | 0.339 |
| Specimen | Riughness Values | Mean | Standard Deviation | |||
|---|---|---|---|---|---|---|
| Ra 1 | Ra 2 | Ra 3 | Ra 4 | |||
| RivaSilver I | 4.42 | 3.58 | 3.021 | 3.619 | 3.660 | 0.576 |
| SDR Flow I | 6.014 | 6.701 | 6.668 | 6.329 | 6.428 | 0.323 |
| VERTISE Flow+ I | 6.546 | 7.074 | 6.861 | 7.254 | 6.934 | 0.304 |
| FUJI IX GP FAST I | 2.756 | 2.948 | 2.356 | 2.167 | 2.557 | 0.358 |
| Rivasilver II | 8.164 | 7.667 | 7.363 | 6.558 | 7.438 | 0.673 |
| SDR Flow+ II | 3.63 | 4.352 | 4.272 | 3.796 | 4.013 | 0.354 |
| Vertise Flow II | 3.553 | 3.301 | 2.561 | 3.218 | 3.158 | 0.423 |
| FUJI IX GP FAST II | 3.574 | 3.38 | 3.276 | 3.307 | 3.384 | 0.134 |
| Rivasilver III | 9.695 | 10.53 | 9.721 | 10.023 | 9.992 | 0.388 |
| SDR Flow+ III | 5.137 | 4.48 | 4.306 | 4.578 | 4.625 | 0.359 |
| Vertise Flow III | 4.591 | 4.3 | 3.486 | 4.316 | 4.173 | 0.477 |
| FUJI IX GP FAST III | 3.174 | 3.574 | 4.391 | 3.798 | 3.734 | 0.508 |
| RivaSilver IV | 3.477 | 3.154 | 3.991 | 3.807 | 3.607 | 0.369 |
| SDR Flow+ IV | 1.253 | 1.263 | 1.369 | 1.132 | 1.254 | 0.097 |
| Vertise Flow IV | 2.801 | 2.681 | 2.503 | 2.423 | 2.602 | 0.171 |
| FUJI IX GP FAST IV | 2.921 | 3.291 | 2.786 | 2.917 | 2.979 | 0.217 |
| Experiment Number | Group 1 | Group 2 | p-Value |
|---|---|---|---|
| 1 | FUJI IX GP FAST | RivaSilver | <0.001 |
| 1 | FUJI IX GP FAST | SDR flow+ | <0.001 |
| 1 | RivaSilver | SDR flow+ | 0.442 |
| 1 | FUJI IX GP FAST | Vertise Flow | 0.0032 |
| 1 | RivaSilver | Vertise Flow | <0.001 |
| 1 | SDR flow+ | Vertise Flow | <0.001 |
| 2 | FUJI IX GP FAST | RivaSilver | <0.001 |
| 2 | FUJI IX GP FAST | SDR flow+ | <0.001 |
| 2 | RivaSilver | SDR flow+ | <0.001 |
| 2 | FUJI IX GP FAST | Vertise Flow | <0.001 |
| 2 | RivaSilver | Vertise Flow | <0.001 |
| 2 | SDR flow+ | Vertise Flow | 0.754 |
| Roughness (μm) | Mean (μm) | Standard Dev. (μm) | ||||
|---|---|---|---|---|---|---|
| Ra 1 | Ra 2 | Ra 3 | Ra 4 | |||
| Riva silver 1 | 3.27 | 3.14 | 3.49 | 3.12 | 3.26 | 0.17 |
| SDR flow 1 | 3.20 | 3.35 | 3.50 | 3.47 | 3.38 | 0.14 |
| Vertise Flow 1 | 4.25 | 4.98 | 5.09 | 4.89 | 4.80 | 0.38 |
| FUJI IX GP FAST 1 | 5.54 | 5.49 | 5.37 | 5.36 | 5.44 | 0.09 |
| Riva silver 2 | 3.24 | 3.39 | 3.14 | 3.32 | 3.27 | 0.11 |
| SDR Flow+ 2 | 6.02 | 5.97 | 6.13 | 5.96 | 6.02 | 0.08 |
| Vertise Flow 2 | 6.07 | 6.05 | 6.18 | 5.87 | 6.04 | 0.13 |
| FUJI IX GP FAST 2 | 5.43 | 5.33 | 5.40 | 5.27 | 5.36 | 0.07 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ludovichetti, F.S.; Guariso, A.; Parcianello, R.G.; Pezzato, L.; Bertolini, R.; Lucchi, P.; Mazzoleni, S. Depth of Cure, Surface Characteristics, Hardness, and Brushing Wear of 4 Direct Restorative Materials in Paediatric Dentistry. Appl. Sci. 2024, 14, 8783. https://doi.org/10.3390/app14198783
Ludovichetti FS, Guariso A, Parcianello RG, Pezzato L, Bertolini R, Lucchi P, Mazzoleni S. Depth of Cure, Surface Characteristics, Hardness, and Brushing Wear of 4 Direct Restorative Materials in Paediatric Dentistry. Applied Sciences. 2024; 14(19):8783. https://doi.org/10.3390/app14198783
Chicago/Turabian StyleLudovichetti, Francesco Saverio, Angela Guariso, Roberta Gaia Parcianello, Luca Pezzato, Rachele Bertolini, Patrizia Lucchi, and Sergio Mazzoleni. 2024. "Depth of Cure, Surface Characteristics, Hardness, and Brushing Wear of 4 Direct Restorative Materials in Paediatric Dentistry" Applied Sciences 14, no. 19: 8783. https://doi.org/10.3390/app14198783







