Abstract
This case report describes the camouflage treatment of a patient with an anterior open bite, bimaxillary skeletal protrusion with a mild class II skeletal pattern, reduced periodontium with generalized slight bone loss, localized severe bone loss at the maxillary upper incisors, and a tongue thrust habit. Orthodontic treatment included modifying the resting posture of the tongue and sectionally intruding maxillary posterior teeth while controlling the extrusion of mandibular posterior teeth using temporary anchorage devices (TADs), followed by sectional mechanics at the maxillary arch and continuous arch mechanics at the mandibular arch, along with interpromximal reduction at the mandibular teeth and inter-arch elastics from the mandibular teeth to the maxillary TADs to minimize orthodontic force magnitude and duration specifically applied to periodontally compromised maxillary incisors. The patient’s chief complaint was addressed, and treatment objectives were achieved, with good esthetic and occlusal outcomes. Stability was shown over a 56-month follow-up period.
1. Introduction
Adult orthodontic treatment generally involves worn periodontium and dentition necessitating an extensive interdisciplinary approach [1]. The key factors acknowledged to impact tooth position are occlusal traits, oral habits, soft tissue pressures and periodontal tissues [2]. Since adult orthodontic patients typically present with sequelae of periodontal disease, varying degrees of periodontal care are likely to be needed [3]. The concurrence of skeletal and dental malocclusions, deleterious habits and compromised periodontium can complicate a patient’s condition. Appropriate intervention requires knowledge of other disciplines, an understanding of biomechanics and a high level of technical skill to achieve realistic functional and aesthetic improvements [4].
Given its multifactorial etiology and high relapse rate, an anterior open bite (AOB) is considered challenging to correct and stabilize [5]. The use of temporary anchorage devices (TADs) has become an effective treatment strategy for such challenging cases [6]. Nonsurgical treatment of an AOB can be achieved by extrusion of the maxillary anterior teeth and/or intrusion of the posterior teeth with counterclockwise mandibular autorotation [7,8].
This case report describes the nonsurgical non-extraction orthodontic camouflage treatment of a periodontally compromised adult patient with an AOB and tongue thrust habit using lingual spurs, skeletal anchorage, sectional mechanics, interproximal reduction and inter-arch elastics.
2. Case Presentation
2.1. Diagnosis and Etiology
A 33-year-old Hispanic female patient presented to the orthodontic department at the University of Illinois at Chicago with the chief complaint “I have a gap between my front teeth”. Her medical history was unremarkable. The dental history revealed generalized slight bone loss with localized severe bone loss at the maxillary incisors and localized gingivitis on a reduced periodontium. She had received comprehensive periodontal treatment including a periodontal splint at maxillary canines and incisors. She was cleared for orthodontic treatment and scheduled for regular periodontal follow-ups. A tongue thrust habit was observed and reported. The patient had a low socioeconomic status. She presented without private insurance, but she was a beneficiary of the Medicaid program, which is a federal-state medical assistance program that primarily serves low-income individuals. Her orthodontic record met the Medicaid orthodontic requirement criteria and was accepted for orthodontic treatment.
Facial analysis showed a symmetrical face with a slightly convex profile, tipped-up nose with a normal nasiolabial angle, normally positioned upper lip and protrusive lower lip in relation to the esthetic line, lips at rest together but straining (forced competency) and inadequate incisal display upon smiling of ~1 mm at maxillary central incisors (U1s). The maxillary midline coincided with the facial midline (Figure 1).

Figure 1.
Pretreatment facial and intraoral photographs.
Clinical and cast analysis revealed class I canine relationships bilaterally and a right molar relationship, end-on class III left molar relationship, 2.7 mm overjet and −3.9 mm overbite measured at tooth #21, a flat curve of Spee, coincident maxillary and mandibular midlines, mild lower crowding with a small diastema between U1s and ovoid maxillary and mandibular arches. Bolton analysis showed anterior and overall mandibular excesses of 4 mm and 4.6 mm, respectively (Figure 1).
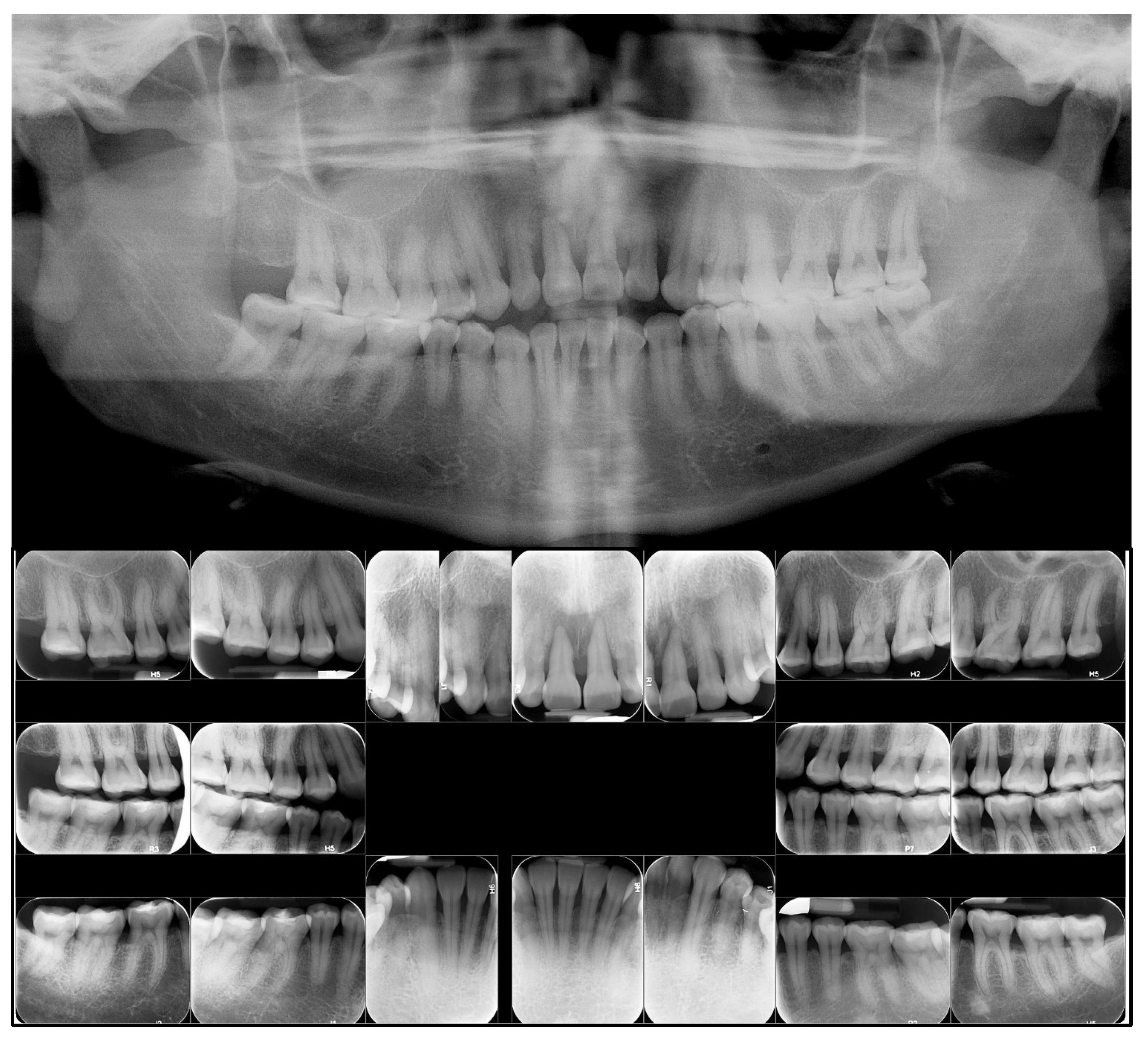
Findings from the panoramic and full-mouth X-rays revealed generalized slight bone loss with localized severe bone loss at the maxillary incisors with blunted roots at teeth #14, #25, #35 and #45 (Figure 2).
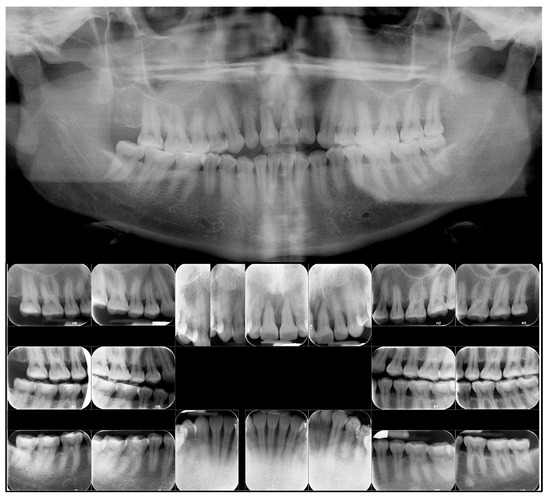
Figure 2.
Pretreatment panoramic and full-mouth radiographs.
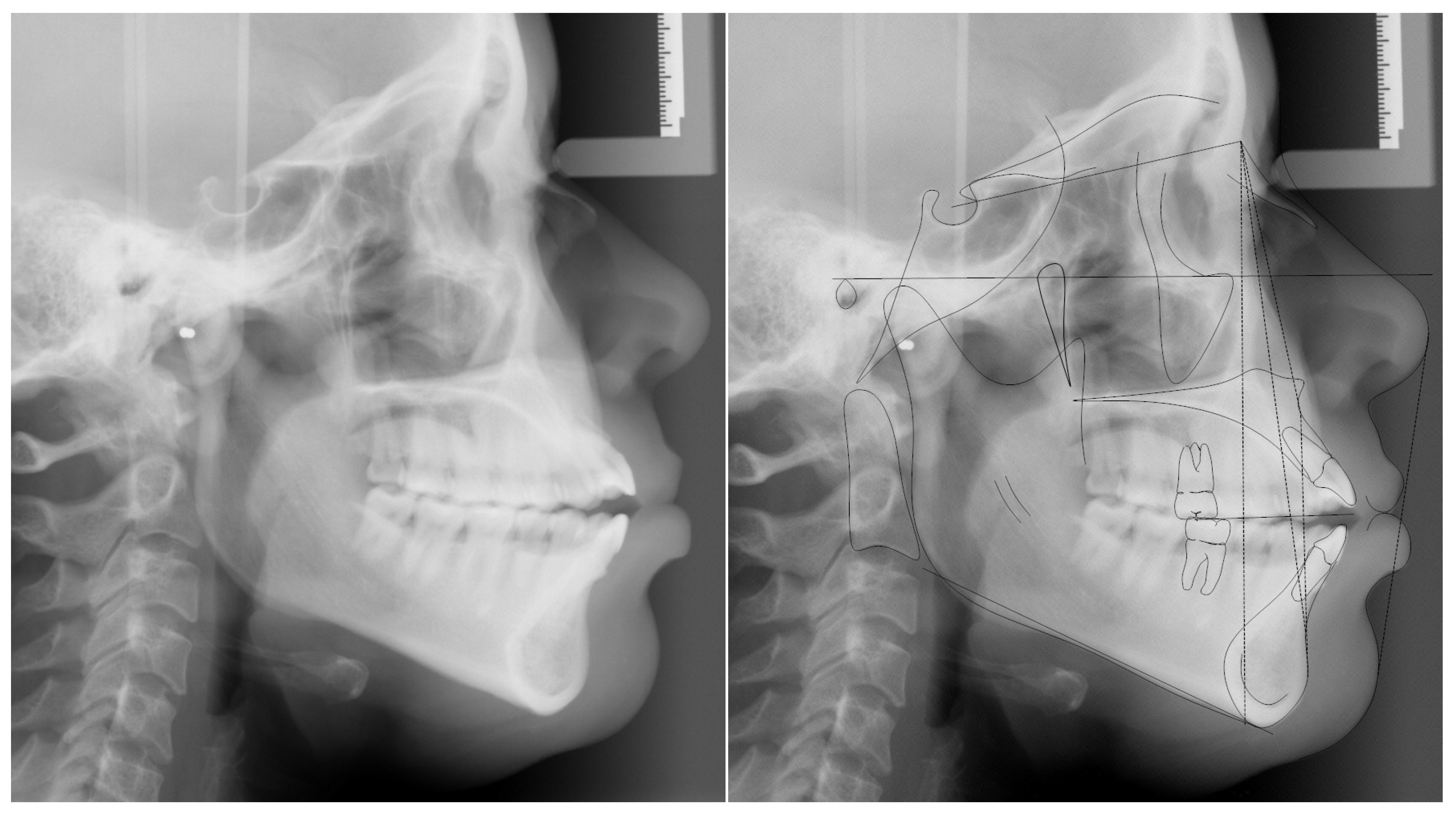
Cephalometric analysis revealed a mild class II skeletal relationship (ANB = 4.9 deg) with protrusive upper and lower jaws (SNA° = 89.6°, SNB° = 84.7°), normal mandibular plane (SNA-MP° and FMA° = 38.7° and 26.3°, respectively), proclined maxillary incisors (U1-SN = 119.6°) and protruded and proclined mandibular incisors (L1-NB = 11 mm, IMPA = 97.7°) (Figure 3 and Table 1).
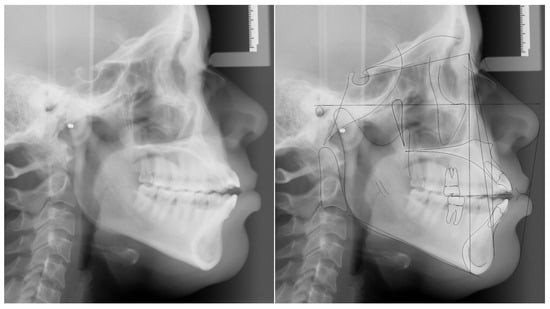
Figure 3.
Pretreatment cephalometric radiograph and tracing.

Table 1.
Cephalometric measurements before and after treatment.
2.2. Treatment Objectives
The treatment objectives were to (1) accept skeletal CL II malocclusion and bimaxillary protrusion, (2) maintain the profile and periodontal condition, (3) modify the resting posture of the tongue, (4) achieve class I molars and canines, (5) improve the inclination of the maxillary and mandibular incisors, along with retraction of the mandibular incisors, and achieve normal overjet, (6) level the compensating curve by intruding molars with relative extrusion of the maxillary incisors to achieve a normal overbite and improve incisal display and (7) accept lower lip protrusion, but improve lip competence.
2.3. Treatment Alternatives
The patient had an AOB and inadequate incisor display upon smiling with the compromised periodontium at the maxillary incisors. The patient needed improvement in the bimaxillary dental proclination, lower incisor protrusion and subsequent lower lip protrusion, along with cessation of the tongue thrusting habit. Therefore, to achieve these treatment goals, the preferred primary treatment options were to reposition the tongue more posteriorly and consider extraction of the mandibular first premolars and, based on the diagnostic set-up, decide on either of the following:
- (1)
- Extraction of U1s and substituting U1s with maxillary lateral incisors (U2s), U2s with maxillary canines (U3s) and U3s with maxillary first premolars (U4s), with future cosmetic restorations and periodontal treatment of the maxillary anterior teeth as needed.
- (2)
- Extraction of U4s and U1s (with forced extrusion of U1s during treatment) where U1s would be replaced with pontics during treatment, if they became significantly mobile, and with final prosthetic restorations (with or without implants) after treatment.
Such options require continuous multidisciplinary collaboration before, during and after treatment to maintain periodontal condition and restore the missing maxillary incisors with pontics and an implant-supported prosthesis or a Maryland bridge. More importantly, it requires the patient’s consent to receive extraction and financial ability to afford prosthodontic treatment. This option (with its subsequent scenarios) was discussed in detail with the patient with direct input from a periodontist and prosthodontist, but the patient refused such scenarios due to financial and psychological constraints. A non-orthodontic treatment was also presented, but the patient declined this option.
To achieve what was mentioned under the treatment objectives section, the selected treatment option was comprehensive nonsurgical non-extraction treatment with interproximal reduction using fixed metal appliances, miniscrews, a transpalatal arch (TPA) and a lower lingual holding arch (LLHA) with soldered lingual spurs. Such an approach was expected to achieve the following: (1) reposition the tongue more posteriorly, (2) intrude the maxillary posterior teeth and relatively extrude the maxillary anterior teeth and (3) maintain the vertical position of mandibular posterior teeth. The treatment was planned for segmental leveling and alignment of the maxillary arch, continuous leveling and alignment and interproximal reduction at the mandibular arch and the use of inter-arch elastics. This patient-centered option was chosen considering several factors, including the patient’s strong desire not to lose a single tooth for as long as possible, compromised periodontium and financial constraints. Before commencing treatment, she fully understood that this option is a camouflage treatment and better (including long-term) esthetic and functional results could be obtained through the previously mentioned options.
2.4. Treatment Progress
After the patient was cleared by her periodontist and signed the treatment consent form, a removable TPA and an LLHA, with soldered tongue spurs, were placed for 3 months. By doing so, we aimed to ensure she will tolerate the appliances before initiating treatment while aiming primarily at modifying the resting position of the tongue (Figure 4A). Afterwards, the maxillary and mandibular second molars were banded, and the premolars were bonded with a pre-adjusted appliance, 0.018″ Synergy brackets, Rickets® prescription, made by Rocky Mountain Orthodontics®, Franklin, IN, USA (USA). Segmental leveling and alignment of the maxillary and mandibular posterior teeth were achieved in 3 months. Afterwards, and on sectional posterior 0.017″ × 0.025″ stainless-steel (SS) archwires, four interradicular miniscrews were placed between the second premolars and first molars. The applied miniscrews were the Aarhus® System made by American Orthodontics, Sheboygan, WI, USA (Ti6I4V titanium alloy, 1.5 mm thread diameter and soft tissue collar length as well as 8 mm thread length). Closed-coil springs were used to intrude the maxillary posterior teeth, while the mandibular posterior teeth were tied to the miniscrews with ligature wires to prevent unwanted extrusion (Figure 4B). The use of miniscrews was aimed at achieving a combination of maxillary posterior teeth intrusion and relative extrusion of the maxillary anterior teeth (i.e., clockwise rotation of the maxillary occlusal plane). Therefore, vertical and sagittal corrections can be achieved with acceptable smile esthetics while minimizing the force duration and magnitude applied on maxillary incisors. After adequate intrusion was achieved in 6 months (Figure 4C), the TPA was removed, and the maxillary and mandibular anterior teeth were bonded. The lower arch was leveled continuously, while the maxillary arch continued to be managed segmentally (i.e., maintained 0.017″ × 0.025″ SS archwires posteriorly with round Nickle Titanium (NiTi) archwires at the maxillary anterior segment, 3M™ Unitek™, Monrovia, CA, USA.). A progress panoramic radiograph was taken 15 months into treatment to assess and adjust root positioning.

Figure 4.
Treatment progress intraoral photographs: (A) 1 month; (B) 7 months; (C) 12 months; and (D) 19 months.
After 17 months of treatment, the LLHA and maxillary 3-3 periodontal splint were removed. A segmental 016″ SS archwire was placed at the maxillary arch with a continuous lower 0.017″ × 0.025″ SS archwire. And IPR was performed at the maxillary and mandibular anterior teeth to improve the black triangles and to resolve the excessive mandibular Bolton discrepancy. Also, buttons were bonded on the lingual surface of mandibular second premolars where cross elastics were used to reduce the buccal overjet at the premolars area. At 19 months into treatment, sectional maxillary 016″ SS archwires were maintained, a continuous mandibular 016″ SS archwire was placed, and class III inter-arch elastics were applied between the maxillary posterior miniscrews and the mandibular canines. Finishing bends were incorporated, along with vertical elastics between the maxillary lateral incisors to the mandibular lateral incisors and canines (Figure 4D). After 22 months of treatment, appliances were removed, and retention was achieved with a Ribbond periodontal splint at the maxillary 3-3, as recommended by her periodontist, and a mandibular fixed 3-3 retainer. In addition, an overlay upper circumferential Hawley retainer, with a small pit lingual to the incisive foramen, was provided to maintain a more posterior resting tongue posture.
3. Treatment Results
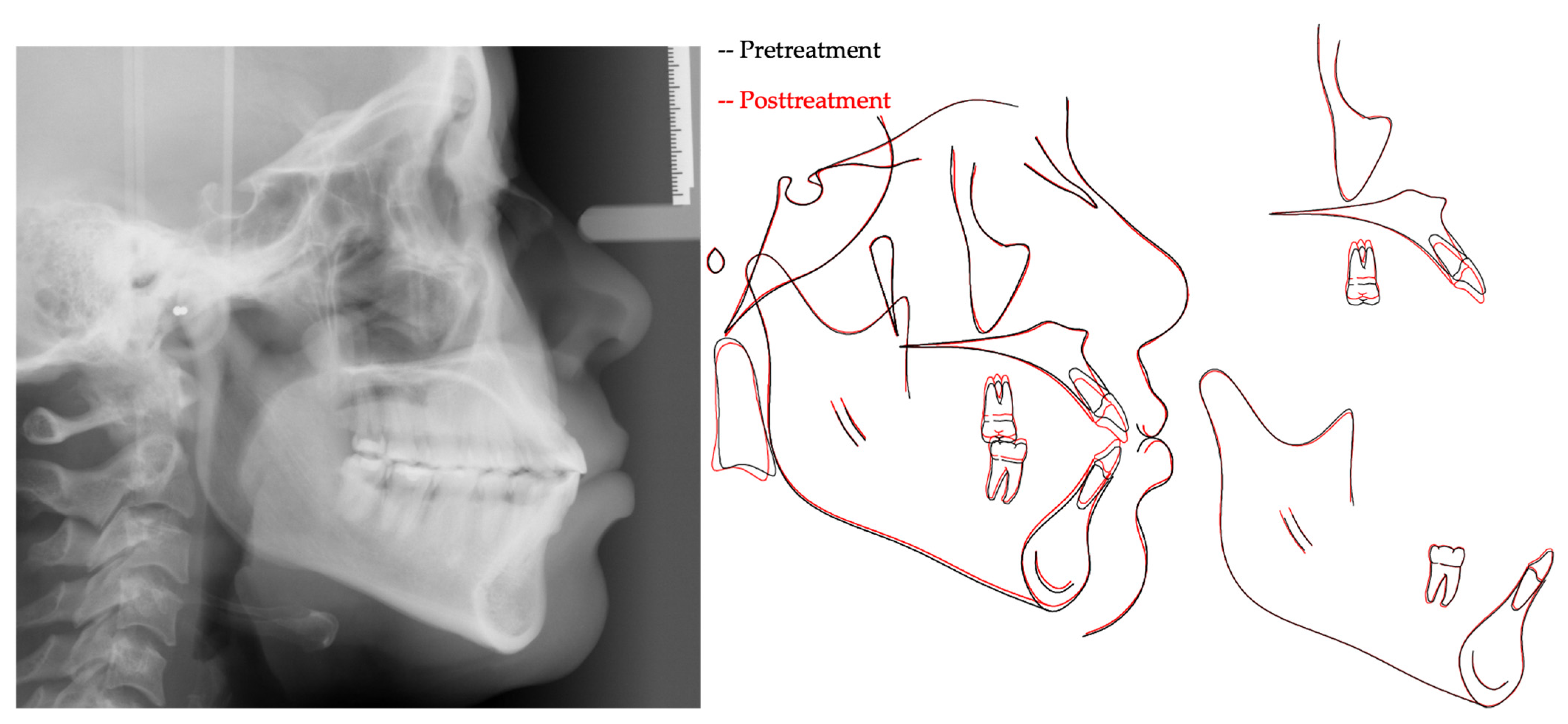
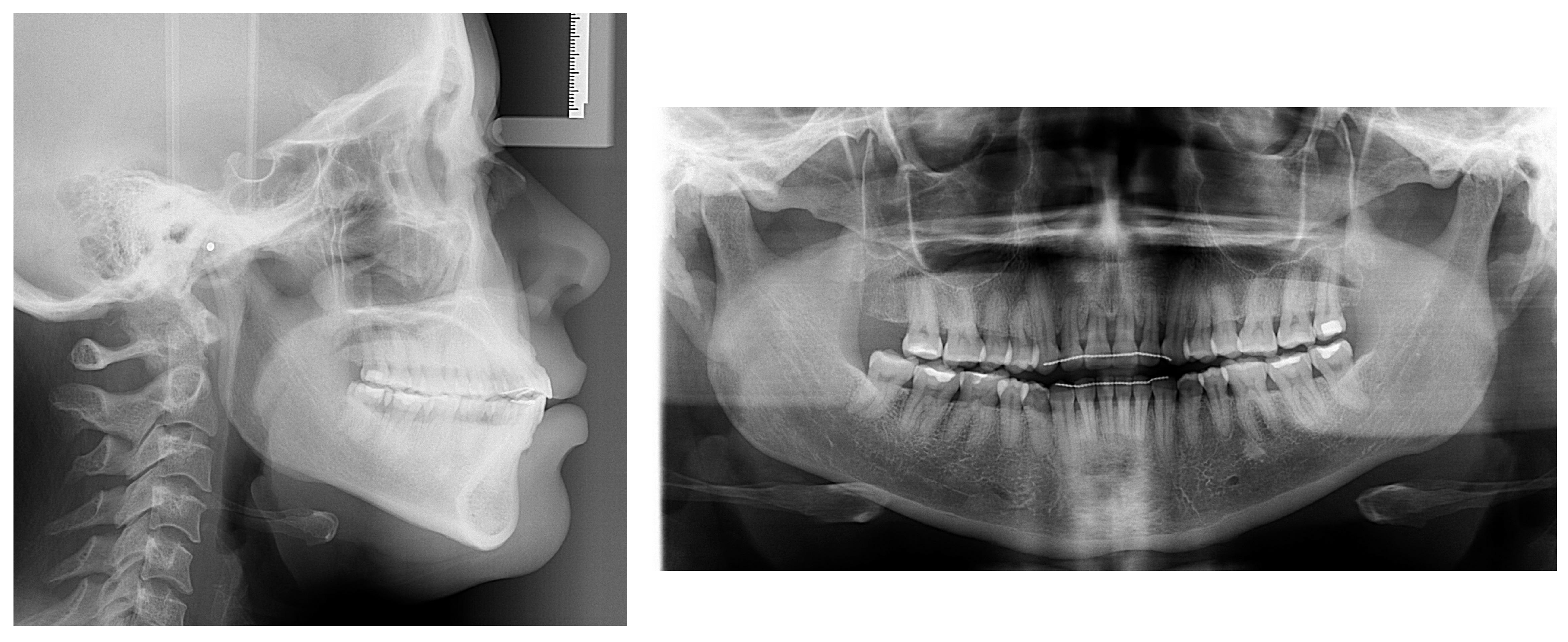
The patient’s chief complaint was addressed, and the patient-centered treatment objectives were achieved, with good esthetic and occlusal outcomes. The post-treatment result shows improvement in lip closure, smile esthetics and overbite (Figure 5). The tongue thrust habit was addressed, and the patient has become genuinely aware of its importance from a stability perspective. Along with the tipping of the occlusal planes, a normal overbite was achieved through a combination of maxillary posterior teeth intrusion, maxillary and mandibular incisors’ relative extrusion, i.e., retroclination and retraction, and mandibular autorotation (Figure 6 and Table 1). Such outcomes were accomplished via the application of miniscrew-assisted sectional mechanics, IPR and inter-arch elastics. The post-treatment panoramic and periapical radiographs showed good root parallelism, without significant root shortening, worsening of the root/crown ratio at the maxillary incisors or development of other pathologies (Figure 7). Follow-up records after 56 months demonstrated a stable occlusion with increased incisal display and an overbite (Figure 8 and Figure 9).

Figure 5.
Post-treatment facial and intraoral photographs.
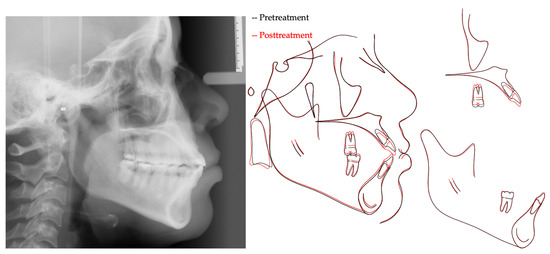
Figure 6.
Post-treatment cephalometric radiograph and pretreatment-to-post-treatment cephalometric superimposition (Black, pretreatment; Red, posttreatment).
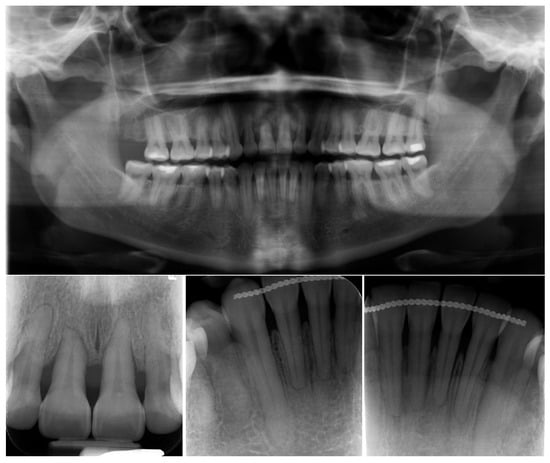
Figure 7.
Post-treatment panoramic and periapical radiographs.

Figure 8.
Facial and intraoral photographs taken 56 months after debonding.
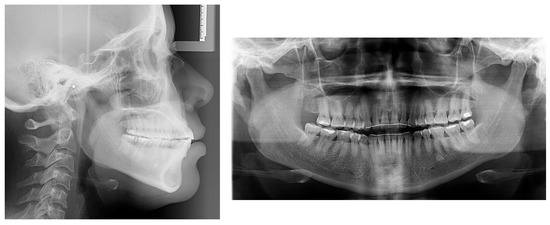
Figure 9.
Cephalometric and panoramic radiographs taken 56 months after debonding.
4. Discussion
This case demonstrates a camouflage-targeted approach in managing a periodontally compromised adult patient with an anterior open bite (AOB) due to dental and habit components. Correction of an AOB is often difficult due to its multifactorial etiology. The patient’s open bite was worsened by the pressure of an anteriorly positioned resting tongue against the lingual of the maxillary anterior teeth [9]. Along with weakened periodontal support, the patient was financially unable to afford complex interdisciplinary treatment and was significantly overwhelmed with its process. She also expressed a strong desire not to receive any extraction. Such patient-related important factors complicated the treatment planning, so a non-extraction treatment had to be planned. We aimed to primarily maintain the bone levels to those of pretreatment while reasonably enhancing the facial esthetics to meet the patient’s expectation. To do so, it was critical to explain the advantages and disadvantages of all available options with direct involvement from other disciplines, so the patient could make an informed decision. The patient was shown animation videos and the results of real cases for the options presented from orthodontic, periodontic and prosthodontic perspectives. In addition, a wax-up based on a three-dimensional (3-D) digital platform was used to simulate the final occlusion, prediction of incisal display and gingival architecture and for the esthetic difference between implant-based crowns and her existing natural incisors.
In AOB cases, the 3-D position of the maxillary incisors should be regarded as a critical factor in deciding the pattern of teeth movement to achieve optimal facial esthetics [8]. During the formulation and execution of the selected treatment, it was critical to balance the esthetic and functional needs. We needed to improve the incisal display without further deterioration at the alveolar bone level. An esthetic and attractive smile includes 2 mm of gingival display with a consonant smile arc [10]. The patient had greater need for incisor “true” extrusion over posterior intrusion. She also presented with significant loss of the alveolar bone at the maxillary incisors. With significant bone loss, the center of resistance becomes more apically positioned, which requires the application of a light, controlled and targeted force system [11]. Therefore, it was more appropriate to select and apply mechanics that would minimize the force duration and magnitude on the maxillary incisors [11]. Throughout treatment, using Synergy low-friction brackets with six tie wings, only round 0.012″ and 0.014″ NiTi and 0.016″ SS archwires were placed segmentally on the maxillary anterior teeth [12,13]. Also, application of anterior vertical elastics was minimized in regard to force and duration.
It is important to consider the 3-D changes associated with intrusion of the maxillary posterior teeth. In the vertical dimension, a combination of intrusion of the maxillary posterior teeth and relative extrusion of the maxillary anterior teeth provided correction of the patient’s AOB with an improved incisal display and smile arc (Figure 5). Although she could have benefited from more incisor extrusion, such “true” extrusion would have deteriorated her periodontal status. Furthermore, it might have worsened her smile esthetics given the presence of notable black triangles (Figure 8). According to Scheffler and colleagues (2014), 2.3 mm of maxillary molar intrusion improves an overbite by 2.2 mm as opposed to the conventionally assumed 4 mm, possibly because of mandibular molar extrusion [14]. In the present case, mandibular molars were maintained, maxillary molars were intruded ~2 mm, maxillary incisors were “relatively” extruded ~3 mm, and mandibular incisors were slightly extruded. The overall change in overbite was about 5.1 mm, from an initial open bite of −3.9 mm to a final overbite of 1.2 mm.
In the anteroposterior dimension, TAD-based maxillary posterior intrusion produces counterclockwise mandibular autorotation that increases the chin projection and improves the facial profile in class II patients [9,14,15]. In our case, the mandibular plane angle became slightly decreased with the mandibular autorotation, which contributed to a more relaxed lower lip closure. We also maintained the vertical position of the mandibular posterior teeth, performed IPR at the mandibular teeth and used CL III elastics from the mandibular teeth to the maxillary TADs. As a result, the mandibular incisors were retracted and retroclined. Such changes in the anteroposterior dimension subsequently impacted the vertical dimension positively, as evident by the rotation of the occlusal planes and OB improvement. In the transverse dimension, buccal crown tipping of the posterior teeth is an adverse side effect that needs to be counteracted using, for example, a TPA or palatal TADs [9,15]. In our case, and despite using stiff rectangular sectional archwires relative to the bracket slot, we encountered such a side effect due to the use of a commercially available removable TPA that lacked proper stiffness. Buccal crown tipping of the posterior teeth in our case was later managed with cross elastics on lighter sectional upper archwires against a larger and stiffer continuous lower archwire.
For a systematic comparison between the present report and previous studies with (dis)similar intervention and retention strategies, it is beneficial to use the Pyramid of Orthodontic-Periodontal Planning described in a previous publication [16]. The pyramid is classified into six sequential steps of customized planning and treatment of periodontally involved patients. The pyramid is used (implicitly) by most studies in the scientific dental literature [3,17,18,19,20,21], and the steps described next are not necessarily ordered according to their importance [16]. The first step includes pre-orthodontic attainment of a stable and healthy periodontium, which includes oral hygiene instructions, scaling and root planning, as well as possible antibiotic prescription and/or flap surgery [20,21]. This is to be followed by a strict periodontal observation period ranging from 2 to 6 months to allow time for the restoration of health, remodeling of periodontal tissue and assessment of the patient’s compliance [3,21]. Others have recommended the need for a pre-orthodontic clearance letter from the periodontist confirming the patient’s readiness for orthodontic treatment [16]. Also, a program of regular periodontal follow-up visits during orthodontic treatment should be scheduled and implemented [1,20]. Our patient was treated by her periodontist with the provision of oral hygiene instructions, scaling and root planning. She was monitored by her periodontist for 4 months before the provision of formal documentation of her readiness for orthodontic movement. For our patient, the observation period extended to the initial phase of active limited orthodontic treatment with the placement of only removable TPAs and LLHAs, with soldered spurs. She also attended a periodontal follow-up every 3 months during orthodontic treatment, which was essential in preventing further alveolar bone loss and providing stable support tissues during and after orthodontic treatment [15,19].
Under an overarching theme of biomechanics, the second, third and fourth steps include planning for anchorage, biomechanics and intrusion movement. The typical presentation of periodontally involved patients includes reduced alveolar support, pathological migration, proclination of maxillary incisors, spacing and supra-eruption, which compromise function and esthetics [1]. Therefore, most studies and case reports in the scientific dental literature investigate and describe intrusion and retraction of extruded and protruded incisors as the most common orthodontic intervention strategy [17,18,22,23,24,25]. In such cases, it is critical to minimize the extrusion and mesial movement of posterior teeth [16]. For appropriate anchorage reinforcement, previous studies have described the use of heathy posterior teeth, headgear, bite blocks, rigid TPAs, Nance buttons and TADs [23,25,26,27,28]. However, such an approach is not applicable to our case given the case findings, etiology and treatment objectives. In their systematic review, Erbe and colleagues (2023) highlighted the scarcity of studies that have investigated extrusive mechanics [29]. They only included one randomized clinical trial that recommended orthodontic extrusion as an effective strategy for patients with infra-bony defects to improve periodontal heath parameters such as probing depth, bleeding index and clinical attachment level [30]. Previous reports have shown predictable treatment outcomes with regenerative periodontal treatment of teeth with significant attachment loss before orthodontists moved the teeth towards an infra-bony defect [31]. However, our patient did not present with infra-bony defects. Others have also shown the benefit of extrusive movement to modify the gingival margin position [32], which was not indicated in our case.
The only comparable study to our case is a case report described by de Barros and colleagues in 2013 [33]. Their adult female patient presented with hopeless maxillary central incisors due to severe bone loss. She was treated by slow forced extrusion for implant site development [33]. Such an approach was presented to our patient as an alternative option, but she rejected it due to psychological and financial constraints, as mentioned previously. Regardless of the type of movement (extrusion or intrusion), there is a clear consensus that orthodontic forces in periodontally compromised patients should be targeted, light, controlled and continuous [29]. Extrusion force should allow movement of ≥2 mm per month [34], and intrusion force should be between 5 and 10 g per tooth [23]. Previous studies also warned against the use of forces with a deleterious effect, such as the use of continuous arch mechanics for intrusion and retraction movements or the application of tooth-born inter-arch elastics for sagittal correction [16]. In line with our approach, previous authors have shown the benefit and applicability of segmental targeted mechanics along with the use of TADs for inter-arch elastics [15,35].
The fifth step includes black triangles and gingival recession. Black triangles, as sites of food debris accumulation, are another complicating factor from esthetic, phonetic and health perspectives [16]. Black triangles can be improved with orthodontic teeth repositioning, especially intrusion movement, interproximal stripping and closure of diastema and other spaces [36]. Despite performing interproximal reduction in our patient, the black triangles were not notably reduced. Such a lack of notable improvement is to be expected given the significant distance between the bone crest and the base of the contact point [16]. Although challenging and unpredictable, one multidisciplinary approach to reconstructing the interdental papilla includes the use of composite resins and/or a subepithelial connective tissue graft [37,38]. Patients with a sensitive receded periodontium could benefit from desensitizing gel and/or a coronal advanced flap with a connective tissue graft, depending on the severity of the problem [39]. Pre-orthodontic periodontal treatment for our patient included the use of desensitizing gel and fluoride application only. In periodontally involved patients, dental expansion and advancement may cause recession and dehiscence and will worsen a preexisting gingival recession, especially in patients with a thin gingival biotype [40]. For such patients, the need for, and timing of, a mucogingival graft with/without phenotype modification need to be assessed by a periodontist [40]. In our case, the planned and executed teeth movement along with her normal gingival biotype did not warrant any surgical periodontal intervention.
The sixth and final step is the retention of the treatment outcome including stable occlusion and a healthy periodontium. Recent systematic reviews and randomized clinical trial have concluded that a combined orthodontic–periodontic approach can improve periodontal health parameters and the prospect of saving and restoring a weakened dentition without a detrimental impact on periodontal health [29,41]. However, the literature still lacks well-controlled studies on long-term periodontal health and maintenance [29,41]. Therefore, guidelines need to be strictly implemented to enhance the possibility of achieving reliable, predictable and stable treatment outcomes. These guidelines include the establishment of periodontal health prior to orthodontic treatment and maintenance of proper periodontal health throughout orthodontic treatment [16,20,40,41]. Orthodontic treatment should be characterized by light, targeted and controlled forces in non-inflammatory conditions [29]. Orthodontic treatment should also identify principal factors of certain malocclusion to ensure stable outcomes [5,6]. For example, soft tissue pressure that contributes to open bite relapse should be eliminated to ensure a stable outcome [4]. The application of lingual spurs, as used in our case, is an effective approach to modifying the tongue position and improving long-term stability [42]. Others advocate for myofunctional therapy to correct resting tongue posture and avoid a relapse [9]. Tavares and colleagues (2013) showed the importance of etiology-based and patient-centered interdisciplinary treatment for a patient with advanced periodontal loss, notable soft tissue problems and skeletal and dental malocclusion [28]. Their therapy included periodontal–endodontic treatment followed by orthodontic and orthognathic surgical correction, and their result remained stable for 11 years [28]. A previous systematic review reported insignificant differences between extraction and non-extraction methods in the long-term stability of a treated open bite [43]. Intrusion of the posterior teeth using TADs is shown to be considerably stable [6], as opposed to the challenges reported in retaining cases that were managed with traditional non-extraction treatment approaches such as bite blocks, multiloop wires and elastics [26,44,45].
In addition to the life-long aging process and general tendency for teeth to return to their original position, adult periodontally involved patients have delayed cell remodeling and mobile teeth, with a tendency for spontaneous migration of teeth [29,31]. There is a consensus regarding the validity and importance of using fixed retainers for the long-term maintenance of orthodontic correction [29]. Bonded retainers need to be flexible to allow the teeth to retain their physiologic mobility [1,3] and need to be positioned correctly to enable good hygiene and intact dynamic occlusion [16]. For patients with severe periodontal bone loss and mobile teeth, conventional removable retainers may not be indicated due to the lack of the force–resistance equilibrium [46]. Nonetheless, patients with light and constant forces from abnormal habits, tongue position or soft tissues have a greater incidence of post-treatment relapse [44], which necessitates the use of overlay removable retainers with a habit breaker modification [43,47].
To conclude, it is apparent that planning for permanent retention for orthodontic stability among periodontally involved patients requires greater consideration without compromising long-term periodontal health. Therefore, patient compliance, as characterized by adherence to meticulous oral hygiene and strict regular follow-up visits to the orthodontist and periodontist, cannot be overstated and needs to be communicated to the patient clearly as an important aspect of informed consent. As simple and basic as it may seem, it is the patient’s best chance to maintain long-term health of the periodontium and stable functioning occlusion. Indeed, this is the most up-to-date evidence-based recommendation for long-term stability and maintenance of periodontal health given the current scarcity of randomized controlled trials with a uniform study design and long-term follow-ups [29,41].
5. Conclusions
Orthodontic camouflage treatment of a periodontally compromised patient with an open bite effectively achieved acceptable dental changes and smile esthetics with the cessation of deleterious oral habit and appropriate biomechanical application of multiple miniscrews, sectional mechanics and inter-arch elastics. The treatment outcomes were acceptable within the limitation of a camouflage treatment and remained stable due to patient compliance, targeted biomechanics, customized retention protocol and continuous monitoring.
Author Contributions
Conceptualization, A.A. and F.A.; writing—original draft preparation, F.A.; writing—review and editing, A.A.; treating the case, A.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Written informed consent was obtained from the patient to publish this paper.
Data Availability Statement
The data presented in this paper are available on request from the corresponding author. The data are not publicly available due to privacy restrictions.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Ong, M.M.; Wang, H.-L. Periodontic and orthodontic treatment in adults. Am. J. Orthod. Dentofac. Orthop. 2002, 122, 420–428. [Google Scholar] [CrossRef] [PubMed]
- Brunsvold, M.A. Pathologic tooth migration. J. Periodontol. 2005, 76, 859–866. [Google Scholar] [CrossRef]
- Gkantidis, N.; Christou, P.; Topouzelis, N. The orthodontic–periodontic interrelationship in integrated treatment challenges: A systematic review. J. Oral Rehabil. 2010, 37, 377–390. [Google Scholar] [CrossRef] [PubMed]
- Proffit, W.R.; Fields, H.W.; Larson, B.; Sarver, D.M. Contemporary Orthodontics-e-Book; Elsevier Health Sciences: Philadelphia, PA, USA, 2018. [Google Scholar]
- Wang, M.; Zhang, B.; Li, L.; Zhai, M.; Wang, Z.; Wei, F. Vertical stability of different orthognathic treatments for correcting skeletal anterior open bite: A systematic review and meta-analysis. Eur. J. Orthod. 2022, 44, 1–10. [Google Scholar] [CrossRef] [PubMed]
- González Espinosa, D.; de Oliveira Moreira, P.E.; da Sousa, A.S.; Flores-Mir, C.; Normando, D. Stability of anterior open bite treatment with molar intrusion using skeletal anchorage: A systematic review and meta-analysis. Prog. Orthod. 2020, 21, 35. [Google Scholar] [CrossRef]
- de Brito Vasconcelos, J.; de Almeida-Pedrin, R.R.; Poleti, T.M.F.F.; Oltramari, P.; de Castro Conti, A.C.F.; Bicheline, M.H.B.; Lindauer, S.J.; de Almeida, M.R. A prospective clinical trial of the effects produced by the extrusion arch in the treatment of anterior open bite. Prog. Orthod. 2020, 21, 39. [Google Scholar] [CrossRef] [PubMed]
- Heo, S.; Park, J.H.; Lee, M.-Y.; Kim, J.-S.; Jung, S.P.; Chae, J.-M. Maxillary incisor position-based orthodontic treatment with miniscrews. Semin. Orthod. 2022, 28, 123–135. [Google Scholar] [CrossRef]
- Miller, J.R. Treatment of a twice-relapsed anterior open bite using temporary anchorage devices, myofunctional therapy, and fixed passive self-ligating appliances. Am. J. Orthod. Dentofac. Orthop. 2020, 157, 832–842. [Google Scholar] [CrossRef]
- Zawawi, K.H.; Malki, G.A.; Al-Zahrani, M.S.; Alkhiary, Y.M. Effect of lip position and gingival display on smile and esthetics as perceived by college students with different educational backgrounds. Clin. Cosmet. Investig. Dent. 2013, 5, 77–80. [Google Scholar] [CrossRef]
- Geramy, A. Alveolar bone resorption and the center of resistance modification (3-D analysis by means of the finite element method). Am. J. Orthod. Dentofac. Orthop. 2000, 117, 399–405. [Google Scholar] [CrossRef]
- Montasser, M.A.; Keilig, L.; Bourauel, C. Archwire diameter effect on tooth alignment with different bracket-archwire combinations. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 76–83. [Google Scholar] [CrossRef]
- Queiroz, G.V.; Rino Neto, J.; De Paiva, J.B.; Rossi, J.L.; Ballester, R.Y. Comparative study of classic friction among different archwire ligation systems. Dent. Press J. Orthod. 2012, 17, 64–70. [Google Scholar] [CrossRef]
- Scheffler, N.R.; Proffit, W.R.; Phillips, C. Outcomes and stability in patients with anterior open bite and long anterior face height treated with temporary anchorage devices and a maxillary intrusion splint. Am. J. Orthod. Dentofac. Orthop. 2014, 146, 594–602. [Google Scholar] [CrossRef]
- Seo, Y.-J.; Park, J.H.; Chang, N.-Y.; Chae, J.-M. Non-Surgical Camouflage Treatment of a Skeletal Class III Patient with Anterior Open Bite and Asymmetry Using Orthodontic Miniscrews and Intermaxillary Elastics. Appl. Sci. 2023, 13, 4535. [Google Scholar] [CrossRef]
- Feu, D. Orthodontic treatment of periodontal patients: Challenges and solutions, from planning to retention. Dent. Press J. Orthod. 2021, 25, 79–116. [Google Scholar] [CrossRef]
- Cardaropoli, D.; Re, S.; Corrente, G.; Abundo, R. Intrusion of migrated incisors with infrabony defects in adult periodontal patients. Am. J. Orthod. Dentofac. Orthop. 2001, 120, 671–675. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.-H.; Kim, Y.-H.; Lee, K.-J.; Hwang, C.-J. Effect of labiolingual inclination of a maxillary central incisor and surrounding alveolar bone loss on periodontal stress: A finite element analysis. Korean J. Orthod. 2016, 46, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Zachrisson, B.U. Clinical implications of recent orthodontic-periodonticresearch findings. Semin. Orthod. 1996, 2, 4–12. [Google Scholar] [CrossRef] [PubMed]
- Zasčiurinskienė, E.; Basevičienė, N.; Lindsten, R.; Slotte, C.; Jansson, H.; Bjerklin, K. Orthodontic treatment simultaneous to or after periodontal cause-related treatment in periodontitis susceptible patients. Part I: Clinical outcome. A randomized clinical trial. J. Clin. Periodontol. 2018, 45, 213–224. [Google Scholar] [CrossRef]
- Zasciurinskiene, E.; Lindsten, R.; Slotte, C.; Bjerklin, K. Orthodontic treatment in periodontitis-susceptible subjects: A systematic literature review. Clin. Exp. Dent. Res. 2016, 2, 162–173. [Google Scholar] [CrossRef]
- Kang, D.-Y.; Choi, S.-H.; Jung, Y.-S.; Hwang, C.-J. Interdisciplinary treatment for an adult patient with anterior open bite, severe periodontitis, and intellectual disability. J. Craniofacial Surg. 2015, 26, e240–e244. [Google Scholar] [CrossRef] [PubMed]
- Melsen, B.; Agerbaek, N.; Markenstam, G. Intrusion of incisors in adult patients with marginal bone loss. Am. J. Orthod. Dentofac. Orthop. 1989, 96, 232–241. [Google Scholar] [CrossRef]
- Rachala, M.R.; Aileni, K.R.; Kumar, P.N.; Soujanya, D.; Prathima, C.R. Orthodontic management of a periodontally compromised patient. Int. J. Orthod. Rehabil. 2017, 8, 78. [Google Scholar]
- Zaveri, P. Orthodontic management of a periodontally compromised dentition. APOS Trends Orthod. 2016, 6, 31. [Google Scholar] [CrossRef]
- Kuster, R.; Ingervall, B. The effect of treatment of skeletal open bite with two types of bite-blocks. Eur. J. Orthod. 1992, 14, 489–499. [Google Scholar] [CrossRef]
- Pinho, T.; Neves, M.; Alves, C. Multidisciplinary management including periodontics, orthodontics, implants, and prosthetics for an adult. Am. J. Orthod. Dentofac. Orthop. 2012, 142, 235–245. [Google Scholar] [CrossRef] [PubMed]
- Tavares, C.A.E.; Allgayer, S.; da Silva Calvete, E.; Polido, W.D. Orthodontic treatment for a patient with advanced periodontal disease: 11-year follow-up. Am. J. Orthod. Dentofac. Orthop. 2013, 144, 455–465. [Google Scholar] [CrossRef]
- Erbe, C.; Heger, S.; Kasaj, A.; Berres, M.; Wehrbein, H. Orthodontic treatment in periodontally compromised patients: A systematic review. Clin. Oral Investig. 2023, 27, 79–89. [Google Scholar] [CrossRef]
- Ogihara, S.; Wang, H.L. Periodontal regeneration with or without limited orthodontics for the treatment of 2- or 3-wall infrabony defects. J. Periodontol. 2010, 81, 1734–1742. [Google Scholar] [CrossRef]
- Roccuzzo, M.; Marchese, S.; Dalmasso, P.; Roccuzzo, A. Periodontal Regeneration and Orthodontic Treatment of Severely Periodontally Compromised Teeth: 10-Year Results of a Prospective Study. Int. J. Periodontics Restor. Dent. 2018, 38, 801–809. [Google Scholar] [CrossRef]
- Pikdoken, L.; Erkan, M.; Usumez, S. Editor’s summary, Q & A, reviewer’s critique: Gingival response to mandibular incisor extrusion. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 432.e1–432.e6. [Google Scholar]
- de Barros, L.A.B.; de Almeida Cardoso, M.; De Avila, É.D.; De Molon, R.S.; Siqueira, D.F.; de Assis Mollo-Junior, F.; Capelloza Filho, L. Six-year follow-up of maxillary anterior rehabilitation with forced orthodontic extrusion: Achieving esthetic excellence with a multidisciplinary approach. Am. J. Orthod. Dentofac. Orthop. 2013, 144, 607–615. [Google Scholar] [CrossRef]
- Korayem, M.; Flores-Mir, C.; Nassar, U.; Olfert, K. Implant site development by orthodontic extrusion: A systematic review. Angle Orthod. 2008, 78, 752–760. [Google Scholar] [CrossRef] [PubMed]
- Musilli, M.; Iuorio, M.T.; Vaia, E.; Vaia, E.; Ramaglia, L.; D’Antò, V. Biomechanically and Periodontally-Based Orthodontic Treatment of a Patient with Upper Canine Affected by External Cervical Resorption (ECR): A Case Report. Dent. J. 2023, 11, 278. [Google Scholar] [CrossRef] [PubMed]
- Rashid, Z.J.; Gul, S.S.; Shaikh, M.S.; Abdulkareem, A.A.; Zafar, M.S. Incidence of gingival black triangles following treatment with fixed orthodontic appliance: A systematic review. Healthcare 2022, 10, 1373. [Google Scholar] [CrossRef]
- Hussien, A.O.T.; Ibrahim, S.H.; Essa, M.E.S.; Hafez, R.M. Restoring black triangle with bioclear matrix versus conventional celluloid matrix method: A randomized clinical trial. BMC Oral Health 2023, 23, 402. [Google Scholar] [CrossRef]
- Yi, Z.; Miao, X.; Wang, L.; Zhang, G.; Wu, Y. A customized subepithelial connective tissue graft for interdental papilla reconstruction and soft tissue augmentation. J. Esthet. Restor. Dent. 2022, 34, 451–460. [Google Scholar] [CrossRef]
- Erpenstein, H.; Borchard, R. Criteria for the selection of root coverage procedures. Part 1: Intention, indication, methods. Periodontal Pract. Today 2006, 3, 139. [Google Scholar]
- Cadenas de Llano-Pérula, M.; Castro, A.B.; Danneels, M.; Schelfhout, A.; Teughels, W.; Willems, G. Risk factors for gingival recessions after orthodontic treatment: A systematic review. Eur. J. Orthod. 2023, 45, 528–544. [Google Scholar] [CrossRef]
- Gehlot, M.; Sharma, R.; Tewari, S.; Kumar, D.; Gupta, A. Effect of orthodontic treatment on periodontal health of periodontally compromised patients: A randomized controlled clinical trial. Angle Orthod. 2022, 92, 324–332. [Google Scholar] [CrossRef] [PubMed]
- Canuto, L.F.G.; Janson, G.; de Lima, N.S.; de Almeida, R.R.; Cançado, R.H. Anterior open-bite treatment with bonded vs conventional lingual spurs: A comparative study. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 847–855. [Google Scholar] [CrossRef] [PubMed]
- Al-Thomali, Y.; Basha, S.; Mohamed, R.N. The factors affecting long-term stability in anterior open-bite correction-a systematic review. Turk. J. Orthod. 2017, 30, 21. [Google Scholar] [CrossRef]
- Kim, Y.H.; Han, U.K.; Lim, D.D.; Serraon, M.L.P. Stability of anterior openbite correction with multiloop edgewise archwire therapy: A cephalometric follow-up study. Am. J. Orthod. Dentofac. Orthop. 2000, 118, 43–54. [Google Scholar] [CrossRef] [PubMed]
- Küçükkeles, N.; Acar, A.; Demirkaya, A.A.; Evrenol, B.; Enacar, A. Cephalometric evaluation of open bite treatment with NiTi arch wires and anterior elastics. Am. J. Orthod. Dentofac. Orthop. 1999, 116, 555–562. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Sidhu, M.S.; Prabhakar, M.; Nindra, J. Orthodontic Limitations in Adults: A Review. J. Clin. Diagn. Res. 2022, 16, ZE1–ZE5. [Google Scholar] [CrossRef]
- Chhabra, N.; Chhabra, A. Evaluation of the efficacy of the modified bluegrass appliance in cessation of thumb-sucking habit: An in vivo study with 12 months follow-up. Med. Pharm. Rep. 2020, 93, 190. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).