Abstract
Objective: The objective was to compare the shear bond strength (SBS) and the adhesive remnant index (ARI) amongst six orthodontic bracket groups. Materials and Methods: Three-dimensional printed polycrystalline alumina brackets (3DBs), ceramic brackets (CBs), and metal brackets (MBs), divided into six groups, were bonded to bovine incisors using different bonding procedures. The SBSs were obtained using a universal testing machine, and the ARIs were assessed with a stereomicroscope. The statistical analyses included one-way analysis of variance (ANOVA) for SBS differences and Fisher’s exact test to show ARI differences amongst the groups (p < 0.05). Results: No significant differences (p > 0.05) were measured amongst the SBSs of the 3DB groups (12.3 MPa, 12.6 MPa, 12.3 MPa, 11.0 MPa, respectively). The latter four groups generally had significantly lower SBSs (p < 0.001) than the conventional bracket groups, CB and MB (16.9 MPa and 19.3 MPa, respectively). Also, there was no significant difference in SBSs for the CB and MB groups (p > 0.05). A high ARI for CBs and MBs (2) indicated that more than 50% of the adhesive remained on the enamel surface. The four 3DB groups had no residual adhesive or less than 50% adhesive on the enamel surface after debonding (ARI scores 0 and 1). A significant difference in ARI levels existed across the types of brackets (p < 0.05). Conclusion: Three-dimensional printed polycrystalline alumina brackets exhibited adequate SBS values for successful bonding. However, the values were lower compared to those for conventional ceramic and metal brackets. The majority of the adhesive remnant for the 3D-printed brackets was mainly located on the bracket base.
1. Introduction
The orthodontic bracket’s bonding to enamel using resin–composite adhesives should provide high enough bond strengths to withstand unintentional failure [1,2]; moreover, debonding after treatment must also produce no enamel damage [1,3]. The design of the orthodontic bracket base is vital in obtaining a clinically adequate strong bond to the tooth enamel [4,5,6]. The strength of the bracket’s bond to the enamel has been extensively investigated resulting in the establishment of various factors influencing the bond strength, including conditioning procedures of the enamel, masticatory strengths, adherent procedures, and bracket-correlating factors (such as the size of the brackets, bracket base design, and material of the bracket base) [2,4,5,6,7,8]. Earlier studies showed that the failure of the bracket bond usually happens at the adhesive/bracket base interface [1,6]. The differences in metal bracket base design have improved the bracket base interface’s micro-interlocking mechanism, enabling successful adhesive retention to the base. Moreover, the combination with adhesive penetrance properties to etched enamel ensures a clinically good bond strength [1,6,9]. In addition, different mechanical retentive and chemical treatments have been applied to the bracket base in an effort to enhance the adhesive retention to the base [1,10,11].
Bonding systems for ceramic brackets rely on mechanical retention rather than chemical retention. The latter method has resulted in excessively high bond strengths, resulting in enamel surface fracture during the debonding procedure [12,13,14,15]. Subsequently, manufacturers favored mechanical retention mechanisms for orthodontic attachments. This evolution in ceramic bracket design enabled adequate adhesion to the resin/composite interface and, thus, to the enamel, subsequently leading to safe debonding [12,13,14]. Ceramic brackets are composed of monocrystalline or polycrystalline materials [12]. These aesthetically acceptable tooth-colored brackets are safe for magnetic resonance imaging (MRI) and exhibit superior biocompatibility. These brackets have been utilized successfully for over 30 years [12,13].
Contemporary orthodontics is experiencing significant growth due to the development of digital technologies such as cone-beam computed tomography (CBCT), intraoral scanning, three-dimensional (3D) photography, computer-aided design, and computer-aided manufacturing (CAD/CAM), affecting diagnosis, treatment planning, and orthodontic treatment process [12,13,14]. Additive manufacturing (3D printing) is a new technique that permits the fabrication of metallic and nonmetallic parts directly from the CAD file. In this technique, the CAD file is sliced into thin sheets, and each sheet is built on top of the previous sheet until the final part is produced [12,16]. For example, 3D-printed brackets are now designed and fabricated using CAD and 3D printing technology [16]. Customized bracket design and fabrication provide specific and individualized bracket base characteristics, which in turn ensure an improved match to the tooth surfaces. This characteristic in itself promotes good adhesion properties [17]. The 3D-printed bracket thus has the appearance and morphology to meet the specific clinical requirements [16]. There is a continual search to embrace effective and efficient orthodontic treatment. One such development is 3D printing technology, which is considered a likely approach to grant higher-quality orthodontic treatment by diminishing chair time, treatment time, and discomfort and achieving better treatment outcomes [16,18].
Yang, L. et al. [16] compared the shear bond strength (SBS) and the adhesive remnant index (ARI) amongst 3D custom-printed lithium disilicate orthodontic brackets, stainless-steel orthodontic brackets, and three types of clear ceramic orthodontic brackets, and found no significant differences in SBS values amongst the groups. Moreover, in a recent study, Hodecker et al. [19] compared the SBSs and ARIs amongst 3D custom-printed resin brackets with different retention but all the same base size, a micro-retentive group and a macro-retentive group and a conventional metal bracket group, and a 3D-printed bracket group with a larger base size. They reported a higher shear bond strength value for the metal bracket group than for the other groups, and there were significant differences between the 3D-printed bracket groups. Also, regarding the ARI score, there were significant differences in the micro-retentive group compared to the other groups.
New and unique 3D custom-printed polycrystalline alumina brackets (Lightforce®, Cambridge, MA, USA) were recently introduced to orthodontic practice. Adequate SBS and ARI studies for this bracket have not been performed. Thus, the present study pursued this evidence to assist clinicians in bonding decision-making.
Purpose:
- To determine and compare the SBSs [20] amongst 3D custom-printed polycrystalline alumina brackets (3DBs), ceramic brackets (CBs), and metal brackets (MBs).
- To determine the ARI [21] as an assessment of failure at the adhesive–bracket interface amongst the three noted bracket types.
Hypotheses:
Hypothesis 1.
Primary null hypothesis: no significant difference exists in SBSs among the 3DB, CB, and MB groups.
Hypothesis 2.
Secondary null hypothesis: no significant difference exists in the ARI amongst the 3DB, CB, and MB groups.
2. Materials and Methods
2.1. The Design and the Sample of This Study
A bovine tooth model was used for this experimental in vitro study. The brackets were obtained and divided according to the bracket material type into three groups. The bracket base configurations were determined through the manufacturer’s fabrication process and used as provided by the manufacturer. The bracket types are outlined in Table 1. A different bonding procedure for each of the six groups entailed the use of composite (Transbond™ plus adhesive, 3M, Unitek, CA, USA) or flowable resin (Flow Tain, Itasca, IL, USA) with or without Assure Plus bonding enhancer (Reliance, Reliance Orthodontic Products 1540 West Thorndale Ave, Itasca, IL, USA) in 3DB, while the CB and MB bonding procedures used only the composite resin without the Assure Plus bonding enhancer as portrayed in Table 2.

Table 1.
Bracket type, material, and base size of the brackets.

Table 2.
The experimental protocol of the 6 subgroups.
2.2. Teeth and Bonding Procedures
Bovine permanent incisor teeth [22] were harvested with inclusion criteria dictating an intact labial surface, no enamel defects, no cracks, and no dental caries. The teeth were examined with a magnifier (×10) to determine eligibility. The teeth were cleaned and polished with pumice paste (Reliance, Houston, TX, USA) at low speed for 10 s, rinsed with distilled water for 10 s, and stored in a 0.1% (wt/vol) thymol solution at 37 °C to avoid any bacterial growth [1,20].
The enamel surfaces of the bovine teeth were scanned with an intraoral scanner (CS 3600, Carestream Dental, Atlanta, GA, USA) and analyzed with CS Mesh Viewer™ software (version; 1.0.0.13.568) (Carestream Dental, Atlanta, GA, USA). The scanned STL files were sent to the Lightforce Company (Lightforce, Cambridge, MA, USA) to generate the 3D custom-printed brackets according to the enamel surface of the teeth.
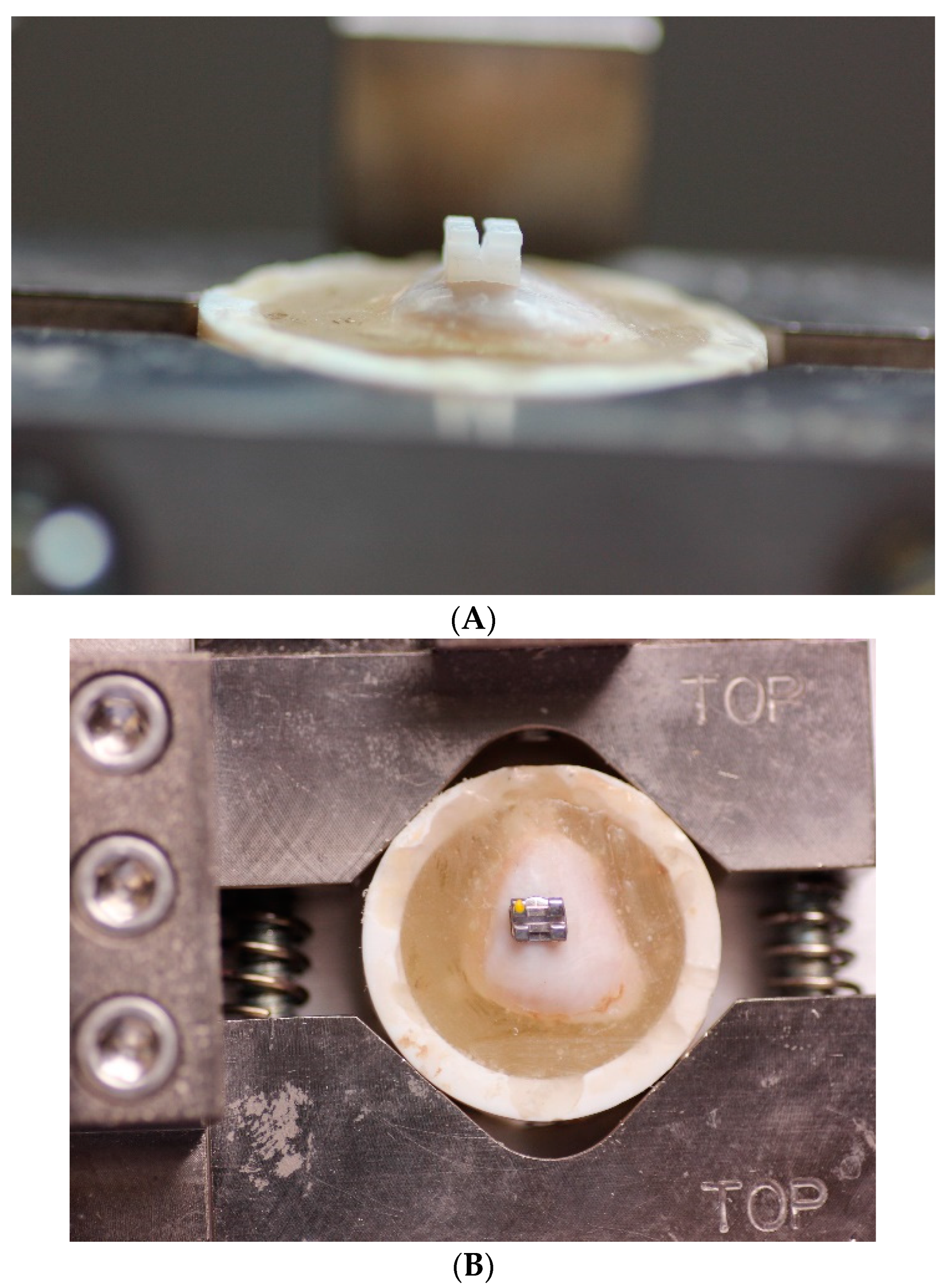
The teeth were secured into polyvinyl chloride (PVC) cylinders with self-cure acrylic resin (Alumilite, Amazing clear cast, Kalamazoo, MI, USA ) (Figure 1A,B). The enamel surface was prepared with Transbond™ plus self-etching primer (3M, Unitek, CA, USA) for 5 s, and then, a gentle stream of oil-free air was delivered for 1–2 s on all the teeth. The ceramic and metal brackets were bonded with a light-cure composite resin (Transbond™ plus adhesive, 3M, Unitek, CA, USA). The 3DBs were bonded using either composite resin (Transbond™ plus adhesive, 3M, Unitek, CA, USA) or a more flowable resin (Flow Tain, Itasca, IL, USA). Finally, the Assure Plus bonding enhancer (Reliance Orthodontic Products, Itasca, IL, USA) was placed after the self-etching primer in some groups as proposed by the 3DB manufacturer (Lightforce, Cambridge, MA, USA).
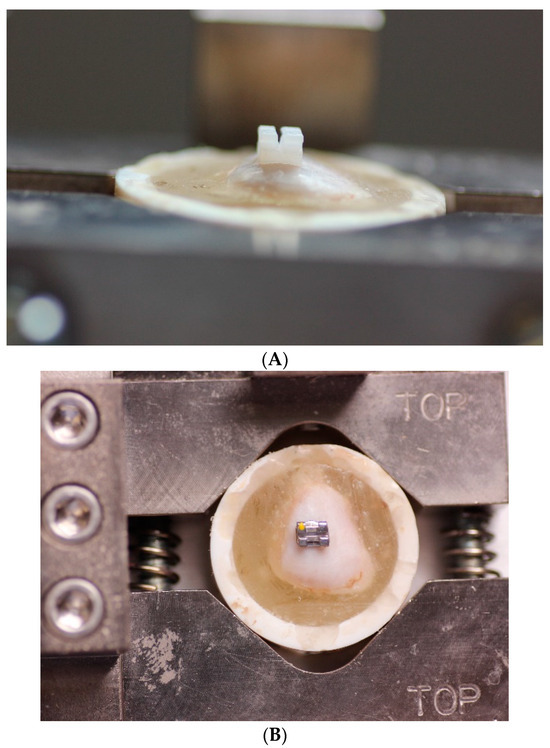
Figure 1.
(A) Imbedded tooth (polyvinyl chloride (PVC) cylinders filled with self-cure acrylic resin). (B) Prepared bracket insert into universal test machine.
It is essential to have a standardized bonding methodology when studying the bond strengths of orthodontic brackets or attachments to the enamel surface of teeth. Thus, a 1.5-inch Push–Pull Gauge (The Jonard Tools, Elmsford, NY, USA), applying a 300 gf compression, was utilized to set the brackets on all teeth with a standard force prior to the initiation of the curing process of the resin. Before curing, the resin excess was removed from the edge of the brackets with a dental explorer [1,20]. An LED curing light (Acteon LED, American Orthodontics, Sheboygan, WI, USA) ensured that appropriate polymerization of the resin occurred, resulting in a harder, tougher, and more stable adhesive/resin bond. This procedure was performed on each side of the bracket base for 10 s, with an intensity of 1200 mW/cm2 [1,20]. The specimens were stored in a water bath at 37 °C for 24 h to prevent dehydration after bonding. These processes were achieved for all samples [1]. A universal test machine (New Day Research, West Chicago, IL, USA) was operated to obtain the SBS value (Figure 2A). Each specimen was exposed to a force on its labial surface parallel to the force (Figure 2B). A sharpened chisel blade was placed at the bracket base–enamel interface and using a 1 kilonewton load cell with a crosshead speed of 0.5 mm/min, and the bracket was shear tested to bond failure (Figure 2B and Figure 3).
The force that produced failure was recorded in newtons and converted into force per unit area megapascals (MPa) by dividing the measured force values by the mean surface area of the brackets [4]. Bond strengths between 6 and 8 MPa were reported as clinically acceptable [16,23]. Moreover, Sperber et al. [24] (mean 10.76 MPa) and Sharma-Sayal et al. [4] (mean > 9.73 MPa) also concurred with their SBS control values.
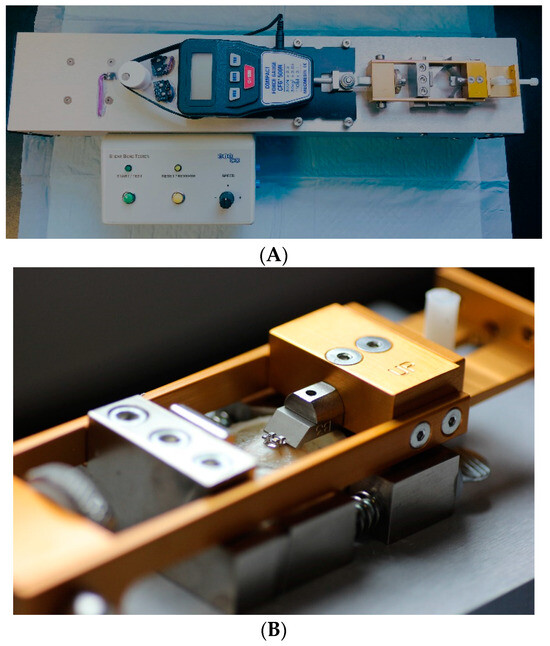
Figure 2.
(A) Universal test machine (New Day Research, West Chicago, IL, USA) and (B) closeup of the blade and bracket in the test machine ready for debonding.
Figure 2.
(A) Universal test machine (New Day Research, West Chicago, IL, USA) and (B) closeup of the blade and bracket in the test machine ready for debonding.
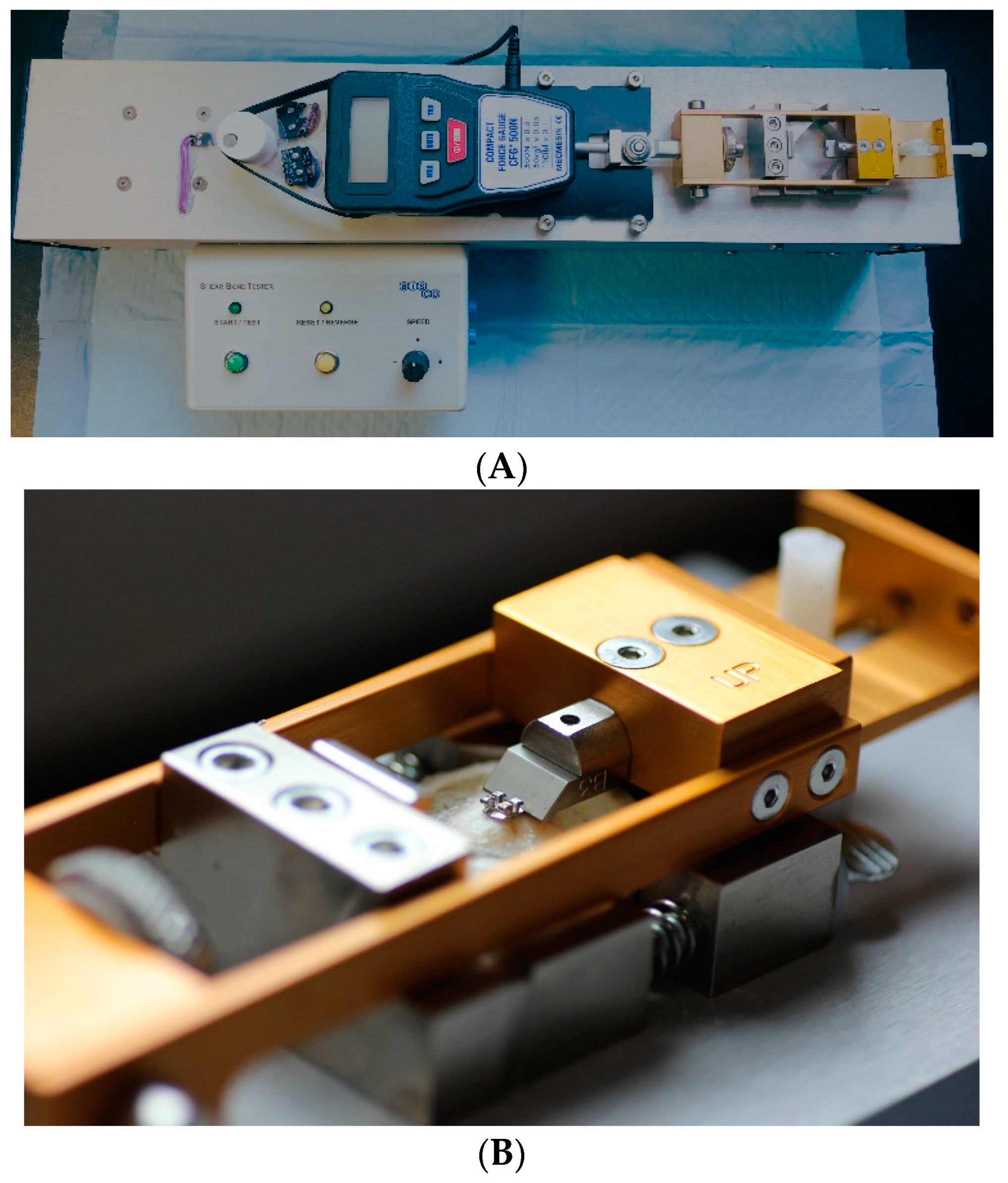
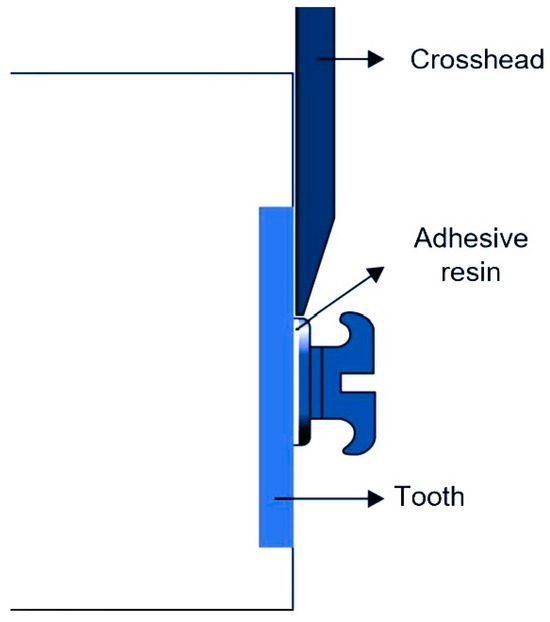
Figure 3.
Diagram of shear bond strength (SBS) setup for testing.
Figure 3.
Diagram of shear bond strength (SBS) setup for testing.
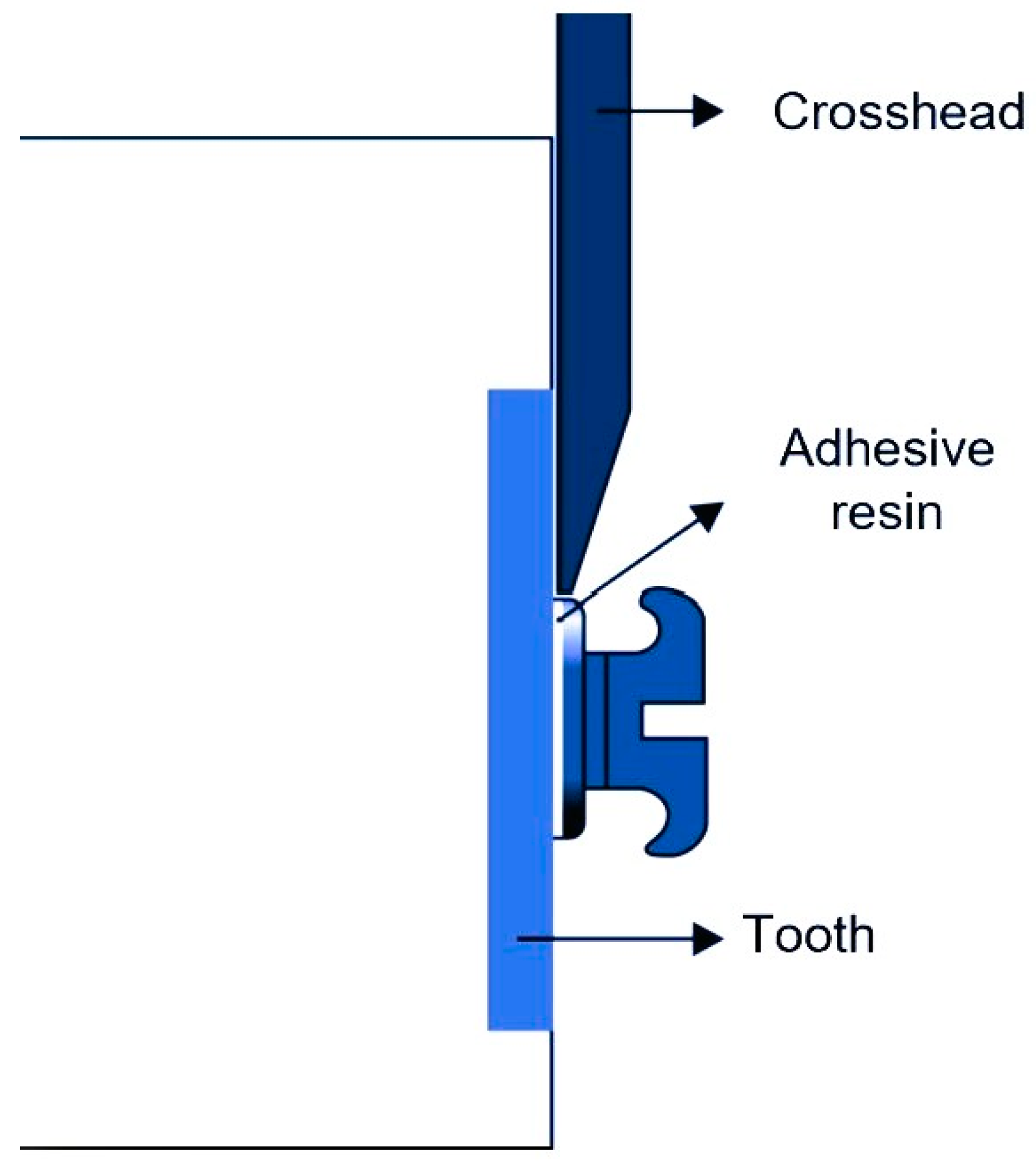
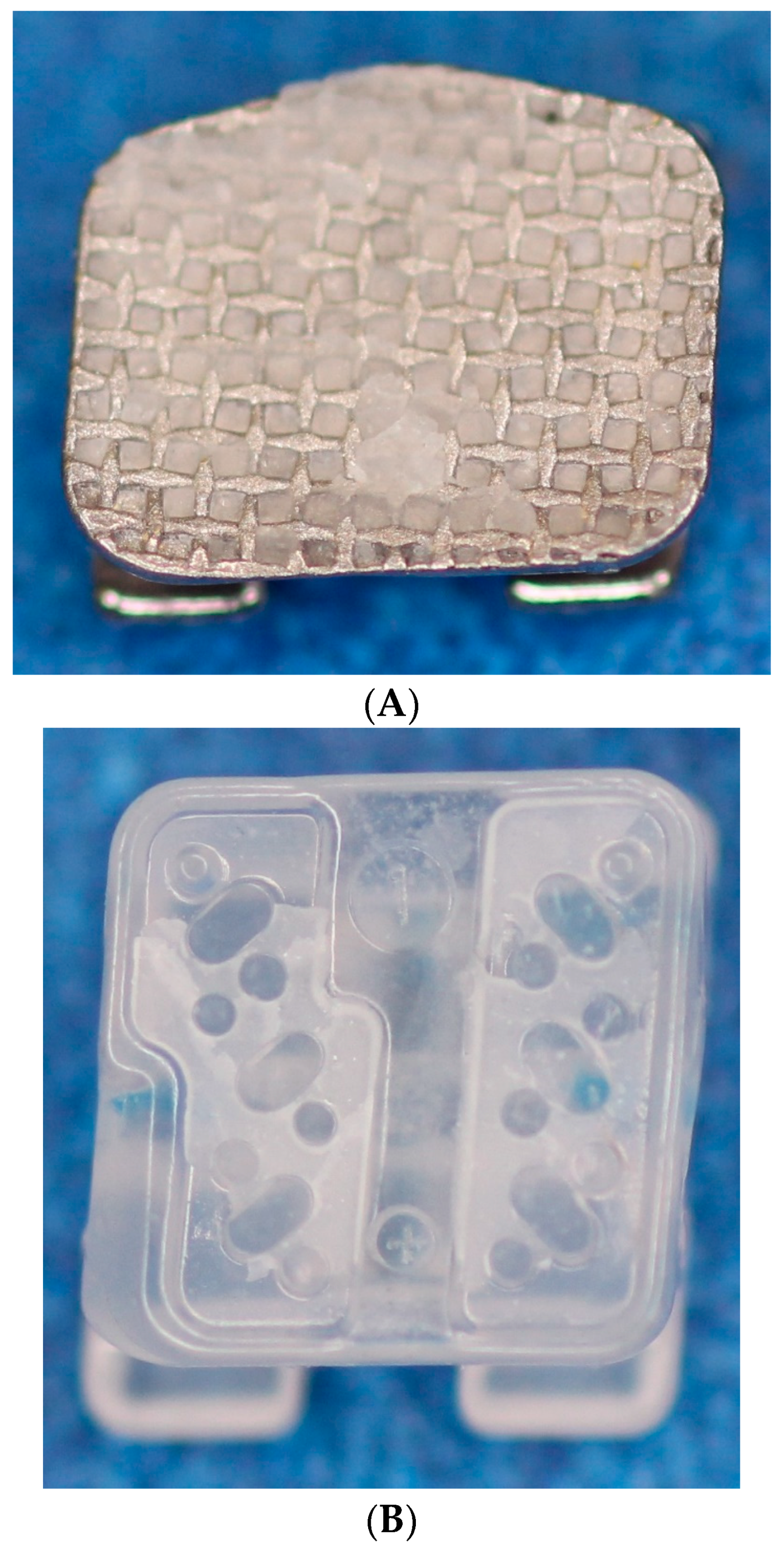
A stereomicroscope (Leica MZ95, Wetzlar, Germany) was used to determine the ARI for each specimen at 0.63× magnification. The ARI represents the residual amount of composite following debonding on the bracket and enamel surface (Figure 4). ARI 0 = no composite left on the bracket or enamel surface; ARI 1 = less than half of the composite left on the bracket or enamel surface; ARI 2 = more than half of the composite left on the bracket or enamel surface; and ARI 3 = all composites left on the bracket or enamel surface [21].
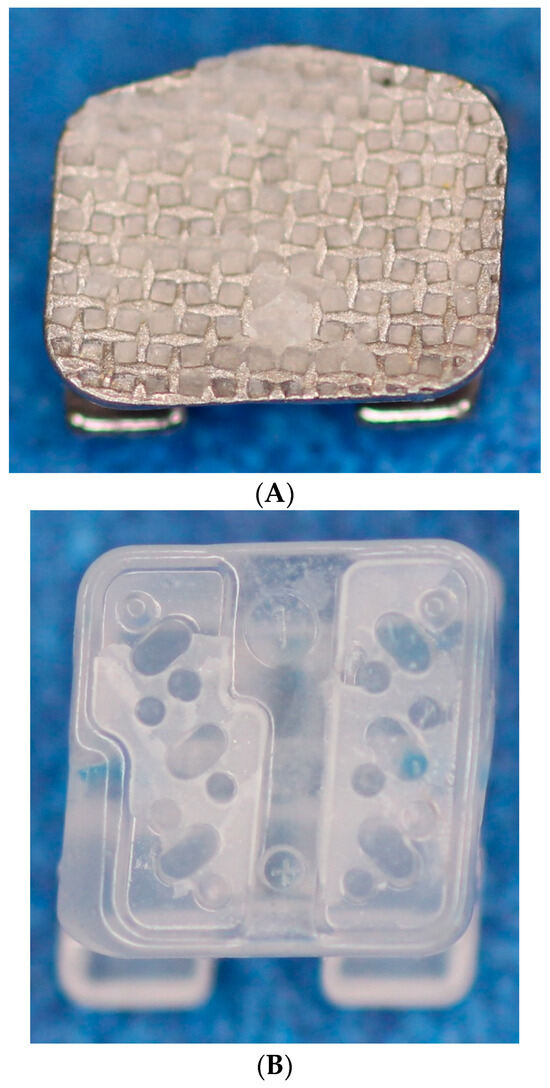

Figure 4.
Top view of the residual amount of composite on the bracket base. (A) Metal base surface, (B) ceramic base surface, and (C) 3D-printed base surface.
2.3. Statistical Analysis
The mean SBSs and standard deviations of the samples were calculated using IBM SPSS™ statistics (version 23 for Windows, SPSS, Armonk, NY, USA). The differences in the SBSs were determined using the one-way analysis of variance (ANOVA) and Tukey tests to show any statistical significance. In addition, Fisher’s exact test indicated differences among the ARI scores of the groups. Statistical significance was determined at p < 0.05.
The sample size of this study was not calculated a priori due to the lack of previous data in the literature. Based on the sample size, mean, and standard deviation of the six groups, for an effect size of f = 0.83, this study had a power of 0.998.
3. Results
3.1. Shear Bond Strength
The 3DBC, 3DBCA, 3DBF, and 3DBFA groups (12.3 MPa, 12.6 MPa, 12.3 MPa, and 11.0 MPa, respectively) were not statistically significantly different (p > 0.05); however, they had significantly lower SBSs (p < 0.001) than the CBC and MBC groups (16.9 MPa, and 19.3 MPa, respectively). Moreover, there were no significant differences in SBSs between the CBC and MBC groups (p > 0.05) (Table 3).

Table 3.
Descriptive statistics and statistical comparisons for SBS (MPa) amongst six groups.
3.2. Adhesive Remnant Index (ARI)
A high ARI score of 2 was observed for the CB and MB groups. Thus, more than 50% of the adhesive remained on the enamel surface. In contrast, in the 3DB groups, no residual adhesive or less than 50% of the adhesive remained on the enamel surface (ARI scores 0 and 1). A significant difference was determined amongst the ARIs across the three types of brackets (p < 0.05) (Table 4).

Table 4.
Frequency distribution and the result of Fisher’s exact test of the adhesive remnant index.
4. Discussion
The in vitro testing of the SBS is of translational clinical importance and allows the selection of an ideal combination of materials for effective orthodontic bonding. Clinicians seek to perform the most reliable and stable bonding procedures without inducing any harm to the tooth during intentional debonding at the completion of active treatment [16].
The SBS of orthodontic brackets is impacted by the bracket base design [4]. Moreover, MBs and CBs mostly have mechanical surface roughening or etching to enhance the mechanical retention of the composite to the bracket base. Three-dimensional (3D) printing is a new technique used to fabricate 3D-printed custom brackets [16]. This system delivers precise and individualized bracket base characteristics, assuring an excellent match to the tooth surface through the form-fit properties between the custom bracket base and the tooth surface [16]. The curvature of the bracket base should seamlessly fit the surface of the tooth, leaving a thin layer of resin between the bracket base and the tooth enamel. Any discrepancy in this fit will impact the innate mechanical properties of the resin and, thus, could lead to a fragile interface with a resultant inadequate bond strength [7,17]. Thus, it is pertinent to evaluate the SBS values of 3D-printed resin brackets and to compare them with those of conventional CB and MB groups.
In the present study, the SBS for the 3DBs with various bonding variables was significantly lower (p < 0.001) than that for the CB and MB groups. All the SBSs were above the minimal force levels recommended in the published literature for a successful clinical debonding procedure [16,23,24]. Orthodontic brackets need to remain bonded to the enamel during the extent of the orthodontic treatment. A very low bond strength will lead to inefficient bonding with resultant debonding. On the contrary, a very high bond strength will likely lead to enamel fracture during debonding. Moreover, a clearly noticeable high bond strength may not be clinically appropriate because of the significant risk of enamel damage during the debonding procedure [25]. Retief et al. [26] reported enamel fracture incidents with bond strength measurements as low as 9.7 MPa in samples during in vitro bond testing.
Even though the enamel can often resist greater forces compared to the force level reported, it is desirable to follow the instructions for debonding as instructed by the manufacturer to avoid enamel damage [25]. Although all the 3D-printed brackets’ mean SBS value in the present study was higher than the ideal mean SBS value suggested by Retief et al. [26] (9.7 MPa) and that of Sperber et al. [24] (10.76 MPa), there were only two incidences of damage to the tooth enamel during the debonding procedure from each group represented.
Moreover, the SBSs of all the 3DB groups were significantly lower than the SBSs of the MB and CB groups, which suggests a lower risk of enamel damage during bracket debonding. The lower SBSs could result from the flexible resin of the 3DB compared to the more rigid MBs and CBs, which will require slightly more force to engender a composite fracture. In addition, no significant difference existed in SBSs between the MB and CB groups, which has also been supported by other studies [27,28].
The ARI provides information on the efficiency of debonding, that is, the potential for enamel fracture or enamel damage when debonding occurs [29]. ARI scores are impacted by the type of bracket, the debonding procedure, the adhesive type, and the bonding procedure used [25]. Composite resin remaining after the debonding procedure mandates additional cleaning, which may include superficial enamel removal; however, carefully removing the residual resin is likely less risky than damage during the debonding procedure [27,30,31].
In the present study, in all the 3DB groups debonded, less than 50% composite remained, which may be due to the lower SBSs for the 3DB compared to the MB and CB groups. Less removal of the remaining adhesive with the 3DB ensures less chair time and may decrease the risk of enamel damage. The perfect fit of the 3DB also ensures that only a skinny layer of resin is needed for a successful bond.
Concerning the different bonding protocols used for the 3D-printed brackets, there is a lack of sufficient evidence regarding the bonding strength and characteristics of 3D-printed brackets, as well as a lack of evidence regarding the optimal bonding protocol with these types of brackets. Therefore, we tested various potentially useful bonding protocols to determine effectiveness and appropriateness for potential clinical use.
On the other hand, there are multiple studies [1,4,12,32] examining the bonding characteristics and bonding protocols of MBs and CBs; thus, the conventional bonding protocols were adopted for the control groups.
The use of bovine incisors was encouraged in the present study due to the challenges associated with obtaining an adequate number of intact human teeth. Moreover, bovine teeth are inexpensive and widely available and have been used in multiple in vitro studies [33,34,35]. Yassen et al. [36] have indicated that the differences in chemical composition and mineralization degree between bovine and human teeth are minor. However, bovine teeth differ histologically from human teeth [35,37]. Furthermore, according to Pickett et al. [38], SBS is lower in vivo on human teeth despite their similar structures than in vitro on bovine teeth. This is due to the histological differences in structure and the influence of intraoral factors (e.g., saliva, acid, mastication) on the cohesion of a tooth–adhesive–bracket complex [35,39]. Hence, any results obtained in in vitro studies guide the efficacy of bonding or debonding. Standardization, in order to make the present results useful, is important; thus, the reason for the use of similar teeth is mostly published in studies of this kind. It thus acknowledges the results of other studies performed on bovine teeth and again emphasizes the standardization among studies [35]. Moreover, it is pertinent to mention that teeth stored in 0.1% (wt/vol) thymol solution are much drier than vital teeth and exhibit a higher risk of enamel damage [12,25]. Further, the debonding plier may present a variety of debonding forces, e.g., shear, tensile, and peel forces in in vivo tests (clinical scenarios), while the universal test machine is a rigid and stable machine qualified to create pure shear debonding forces in in vitro tests [38]. In addition, the debonding plier is not stable regarding the rate of loading because of its clinical application, whereas the universal testing machine is steady regarding the speed of loading [38]. Furthermore, when compared to the debonding plier, the universal test machine debonding is exceptionally harsh, sharp, and unilateral [12,25]. Also, 3D printers are becoming more affordable and play significant roles in dentistry. However, the materials and maintenance, the cost of operating, and the demand for experienced workers must be evaluated, as well as the requirement for postprocessing and commitment to exact safety and health protocols [40].
The SBSs obtained for the 3D-printed brackets, considering the noted in vitro variables, thus have shown the useful application of the bonding and debonding process in the absence of enamel fractures, which enhances its clinical acceptance.
5. Conclusions
- All the 3DB groups exhibited adequate SBSs that were lower compared to those for the conventional MB and CB groups.
- The majority of adhesive remnants for the 3DB groups remained on the bracket base, whereas, for conventional brackets, the majority remained on the enamel surfaces.
- The cleaning process following debonding appeared to be more efficient with 3D-printed brackets.
Author Contributions
Conceptualization: P.E.R., T.T.W. and L.J.; Methodology: P.E.R., D.M. and L.J.; Validation: P.E.R., A.B.B. and L.J.; Formal analysis: P.E.R., L.J. and A.B.B.; Investigation, L.J. and P.E.R.; Resources: P.E.R. and T.T.W.; Data curation, P.E.R. and L.J.; Writing—original draft preparation: P.E.R., L.J. and A.B.B.; Writing—review and editing, P.E.R., D.M., S.M., L.J., T.T.W. and A.B.B.; Supervision: P.E.R., D.M., S.M. and A.B.B.; Project administration: P.E.R. and L.J. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available in the manuscript.
Acknowledgments
Chris Bonebreak Jackson. Review bonding protocol in respect to composite resin application to the base of the Lightforce 3D printed bracket.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Moreira, F.C.; Jacob, H.B.; Vaz, L.G.; Guastaldi, A.C. Effect of Yd: YAG laser irradiation on the shear bond strength of orthodontic metal brackets. Dent. Press J. Orthasod. 2020, 25, 28–35. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.L.; Huang, S.F.; Tsai, H.C.; Chang, W.J. Finite element sub-modeling analyses of damage to enamel at the incisor enamel/adhesive interface upon de-bonding for different orthodontic bracket bases. J. Biomech. 2011, 44, 134–142. [Google Scholar] [CrossRef]
- Kechagia, A.; Zinelis, S.; Pandis, N.; Athanasiou, A.E.; Eliades, T. The effect of orthodontic adhesive and bracket-base design in adhesive remnant index on enamel. J. World Fed. Orthod. 2015, 4, 18–22. [Google Scholar] [CrossRef]
- Sharma-Sayal, S.K.; Rossouw, P.E.; Kulkarni, G.V.; Titley, K.C. The influence of orthodontic bracket base design on shear bond strength. Am. J. Orthod. Dentofacial. Orthop. 2003, 124, 74–82. [Google Scholar] [CrossRef]
- Cozza, P.; Martucci, L.; De Toffol, L.; Penco, S.I. Shear bond strength of metal brackets on enamel. Angle Orthod. 2006, 76, 851–856. [Google Scholar] [PubMed]
- Sorel, O.; El Alam, R.; Chagneau, F.; Cathelineau, G. Comparison of bond strength between simple foil mesh and laser-structured base retention brackets. Am. J. Orthod. Dentofac. Orthop. 2002, 122, 260–266. [Google Scholar] [CrossRef]
- Altmann, A.S.; Degrazia, F.W.; Celeste, R.K.; Leitune, V.C.; Samuel, S.M.; Collares, F.M. Orthodontic bracket bonding without previous adhesive priming: A meta-regression analysis. Angle Orthod. 2016, 86, 391–398. [Google Scholar] [CrossRef] [PubMed]
- Rajesh, R.N.; Girish, K.S.; Sanjay, N.; Scindhia, R.D.; Kumar, S.G.; Rajesh, S. Comparison of Bond Strength of Brackets with Foil Mesh and Laser Structure Base using Light Cure Composite Resin: An in vitro Study. J. Contemp. Dent. Pract. 2015, 16, 963–970. [Google Scholar]
- Smith, D.C.; Maijer, R. Improvements in bracket base design. Am. J. Orthod. 1983, 83, 277–281. [Google Scholar] [CrossRef]
- Algera, T.J.; Kleverlaan, C.J.; Prahl-Andersen, B.; Feilzer, A.J. The influence of different bracket base surfaces on tensile and shear bond strength. Eur. J. Orthod. 2008, 30, 490–494. [Google Scholar] [CrossRef]
- Bishara, S.E.; Soliman, M.M.; Oonsombat, C.; Laffoon, J.F.; Ajlouni, R. The effect of variation in mesh-base design on the shear bond strength of orthodontic brackets. Angle Orthod. 2004, 74, 400–404. [Google Scholar] [PubMed]
- Elekdag-Türk, S. In vitro evaluation of a ceramic bracket with a laser-structured base. BMC Oral Health 2020, 20, 17. [Google Scholar] [CrossRef] [PubMed]
- Poorsattar-Bejeh Mir, A.; Rahmati-Kamel, M. Should the orthodontic brackets always be removed prior to magnetic resonance imaging (MRI)? J. Oral Biol. Craniofac. Res. 2016, 6, 142–152. [Google Scholar] [CrossRef]
- Russell, J.S. Aesthetic orthodontic brackets. J. Orthod. 2005, 32, 146–163. [Google Scholar] [CrossRef] [PubMed]
- Abend, R.; Dan, O.; Maoz, K.; Raz, S.; Bar-Haim, Y. Reliability, validity and sensitivity of a computerized visual analog scale measuring state anxiety. J. Behav. Ther. Exp. Psychiatry 2014, 45, 447–453. [Google Scholar] [CrossRef]
- Yang, L.; Yin, G.; Liao, X.; Yin, X.; Ye, N. A novel customized ceramic bracket for esthetic orthodontics: In vitro study. Prog. Orthod. 2019, 20, 39. [Google Scholar] [CrossRef] [PubMed]
- Rossouw, P.E. A historical overview of the development of the acid-etch bonding system in orthodontics. In Seminars in Orthodontics; Elsevier: Amsterdam, The Netherlands, 2010; pp. 2–23. [Google Scholar]
- Wiechmann, D.; Rummel, V.; Thalheim, A.; Simon, J.S.; Wiechmann, L. Customized brackets and archwires for lingual orthodontic treatment. Am. J. Orthod. Dentofac. Orthop. 2003, 124, 593–599. [Google Scholar] [CrossRef]
- Hodecker, L.D.; Scheurer, M.; Scharf, S.; Roser, C.J.; Fouda, A.M.; Bourauel, C.; Lux, C.J.; Bauer, C.A. Influence of Individual Bracket Base Design on the Shear Bond Strength of In-Office 3D Printed Brackets—An In Vitro Study. J. Funct. Biomater. 2023, 14, 289. [Google Scholar] [CrossRef]
- Bishara, S.E.; Soliman, M.; Laffoon, J.; Warren, J.J. Effect of changing a test parameter on the shear bond strength of orthodontic brackets. Angle Orthod. 2005, 75, 832–835. [Google Scholar]
- Artun, J.; Bergland, S. Clinical trials with crystal growth conditioning as an alternative to acid-etch enamel pretreatment. Am. J. Orthod. 1984, 85, 333–340. [Google Scholar] [CrossRef]
- Soares, F.Z.; Follak, A.; da Rosa, L.S.; Montagner, A.F.; Lenzi, T.L.; Rocha, R.O. Bovine tooth is a substitute for human tooth on bond strength studies: A systematic review and meta-analysis of in vitro studies. Dent. Mater. 2016, 32, 1385–1393. [Google Scholar] [CrossRef]
- Reynolds, I. A review of direct orthodontic bonding. Br. J. Orthod. 1975, 2, 171–178. [Google Scholar] [CrossRef]
- Sperber, R.L.; Watson, P.A.; Rossouw, P.E.; Sectakof, P.A. Adhesion of bonded orthodontic attachments to dental amalgam: In vitro study. Am. J. Orthod. Dentofac. Orthop. 1999, 116, 506–513. [Google Scholar] [CrossRef] [PubMed]
- Mundstock, K.S.; Sadowsky, P.L.; Lacefield, W.; Bae, S. An in vitro evaluation of a metal reinforced orthodontic ceramic bracket. Am. J. Orthod. Dentofac. Orthop. 1999, 116, 635–641. [Google Scholar] [CrossRef] [PubMed]
- Retief, D.H. Failure at the dental adhesive-etched enamel interface. J. Oral Rehabil. 1974, 1, 265–284. [Google Scholar] [CrossRef] [PubMed]
- Arash, V.; Naghipour, F.; Ravadgar, M.; Karkhah, A.; Barati, M.S. Shear bond strength of ceramic and metallic orthodontic brackets bonded with self-etching primer and conventional bonding adhesives. Electron. Physician 2017, 9, 3584–3591. [Google Scholar] [CrossRef] [PubMed]
- Mirzakouchaki, B.; Shirazi, S.; Sharghi, R.; Shirazi, S.; Moghimi, M.; Shahrbaf, S. Shear bond strength and debonding characteristics of metal and ceramic brackets bonded with conventional acid-etch and self-etch primer systems: An in-vivo study. J. Clin. Exp. Dent. 2016, 8, e38–e43. [Google Scholar] [CrossRef]
- Mirzakouchaki, B.; Kimyai, S.; Hydari, M.; Shahrbaf, S.; Mirzakouchaki-Boroujeni, P. Effect of self-etching primer/adhesive and conventional bonding on the shear bond strength in metallic and ceramic brackets. Med. Oral Patol. Oral Cir. Bucal 2012, 17, e164–e170. [Google Scholar] [CrossRef][Green Version]
- Eminkahyagil, N.; Arman, A.; Cetinşahin, A.; Karabulut, E. Effect of resin-removal methods on enamel and shear bond strength of rebonded brackets. Angle Orthod. 2006, 76, 314–321. [Google Scholar]
- Tecco, S.; Traini, T.; Caputi, S.; Festa, F.; de Luca, V.; D’Attilio, M. A new one-step dental flowable composite for orthodontic use: An in vitro bond strength study. Angle Orthod. 2005, 75, 672–677. [Google Scholar]
- Gittner, R.; Müller-Hartwich, R.; Engel, S.; Jost-Brinkmann, P.-G. Shear bond strength and enamel fracture behavior of ceramic brackets Fascination® and Fascination®2. J. Orofac. Orthop. Fortschritte Kieferorthopadie 2012, 73, 49–57. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.T.; Miller, A.; Orellana, M.F. Characterization of the porosity of human dental enamel and shear bond strength in vitro after variable etch times: Initial findings using the BET method. Angle Orthod. 2011, 81, 707–715. [Google Scholar] [CrossRef] [PubMed]
- Oesterle, L.J.; Shellhart, W.C.; Belanger, G.K. The use of bovine enamel in bonding studies. Am. J. Orthod. Dentofac. Orthop. 1998, 114, 514–519. [Google Scholar] [CrossRef] [PubMed]
- Hofmann, E.; Elsner, L.; Hirschfelder, U.; Ebert, T.; Hanke, S. Effects of enamel sealing on shear bond strength and the adhesive remnant index: Study of three fluoride-releasing adhesives in combination with metal and ceramic brackets. J. Orofac. Orthop. 2017, 78, 1–10. [Google Scholar] [CrossRef]
- Yassen, G.H.; Platt, J.A.; Hara, A.T. Bovine teeth as substitute for human teeth in dental research: A review of literature. J. Oral Sci. 2011, 53, 273–282. [Google Scholar] [CrossRef]
- Nakamichi, I.; Iwaku, M.; Fusayama, T. Bovine teeth as possible substitutes in the adhesion test. J. Dent. Res. 1983, 62, 1076–1081. [Google Scholar] [CrossRef]
- Pickett, K.L.; Sadowsky, P.L.; Jacobson, A.; Lacefield, W. Orthodontic in vivo bond strength: Comparison with in vitro results. Angle Orthod. 2001, 71, 141–148. [Google Scholar]
- Reimann, S.; Mezey, J.; Daratsianos, N.; Jäger, A.; Bourauel, C. The influence of adhesives and the base structure of metal brackets on shear bond strength. J. Orofac. Orthop. 2012, 73, 184–193. [Google Scholar] [CrossRef]
- Dawood, A.; Marti, B.M.; Sauret-Jackson, V.; Darwood, A. 3D printing in dentistry. Br. Dent. J. 2015, 219, 521–529. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).