Fall Risk Classification Using Trunk Movement Patterns from Inertial Measurement Units and Mini-BESTest in Community-Dwelling Older Adults: A Deep Learning Approach
Abstract
:1. Introduction
1.1. Frailty Syndrome
1.2. Risk Factors
2. Related Work
2.1. Clinical Tools for Fall Risk Assessment
2.2. Sensor-Based Fall Risk Assessment
2.3. Current Methodologies for Predicting Fall Risk
2.4. Classification Models for Fall Risk Prediction
2.5. Advances in Deep Learning for Fall Risk Prediction
3. Materials and Methods
3.1. Dataset
3.2. Data Augmentation and Segmentation
- Jittering: Adding random noise to simulate natural variability. This technique is commonly employed in time series data augmentation to enhance model robustness by introducing minor variations in the input data [67].
- Scaling: Applying small, constant variations to the time series. Scaling has been shown to improve model performance by generating variability in the amplitude of the input data [68].
- Time warping: Non-linear stretching or compressing of the time axis. Time warping is especially useful in time series classification tasks, as it allows the model to handle variations in the speed of events [68].
- Window slicing: Extracting different segments from the time series to create new, slightly shifted samples. This technique helps create additional data points by slicing the data into overlapping windows, increasing the effective size of the dataset [69].
- Interpolation: Generating new, smoothed samples by interpolating between existing data points. Interpolation techniques are widely used in augmenting time series data to create smoothed transitions between samples [68].
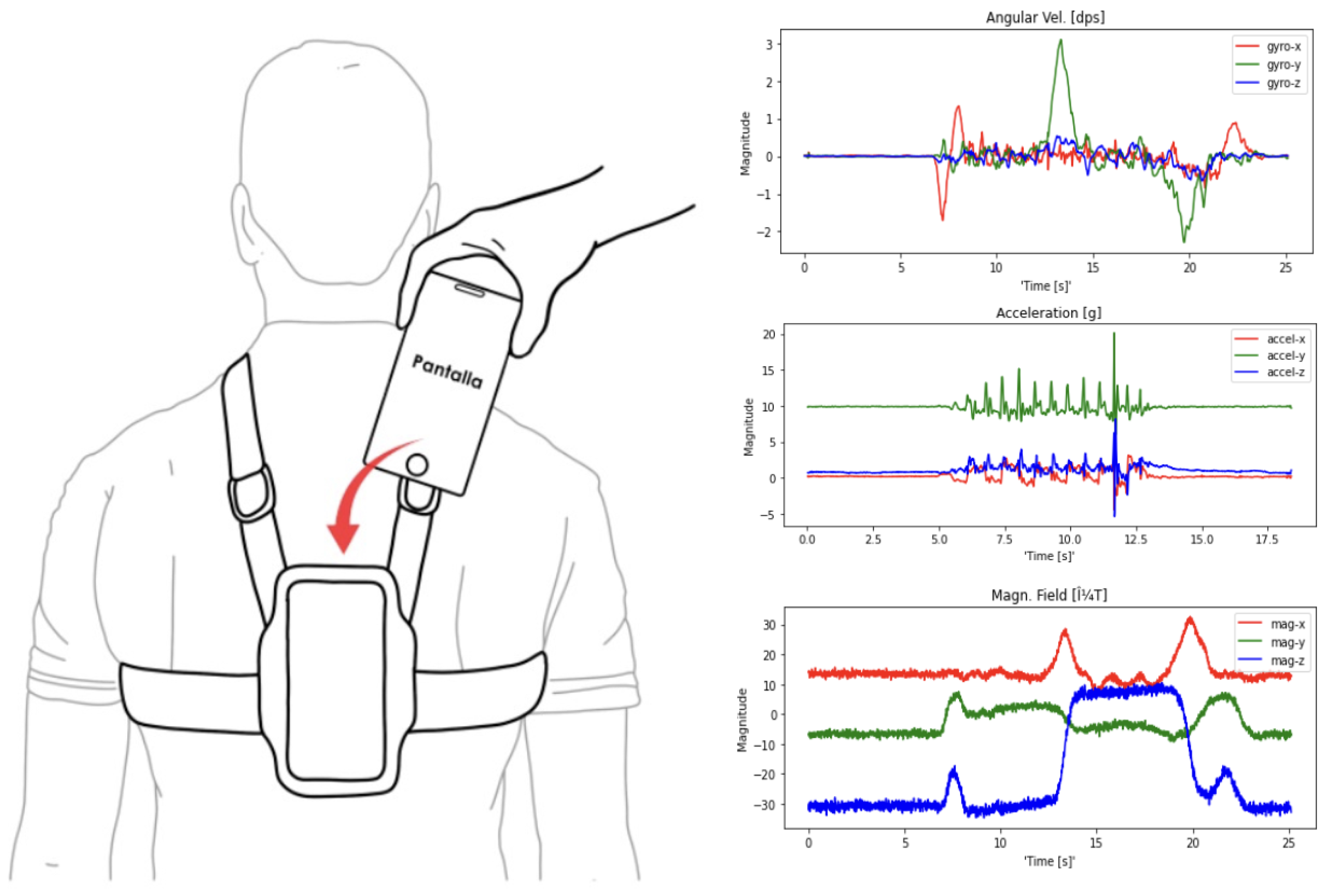
3.3. Smartphones for Monitoring System
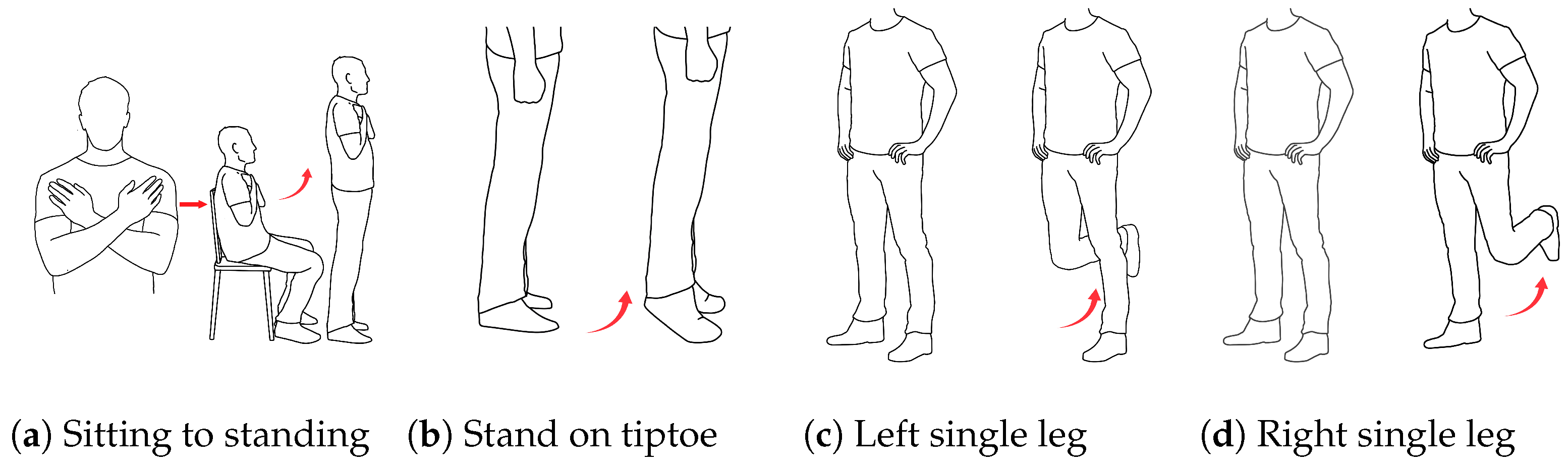
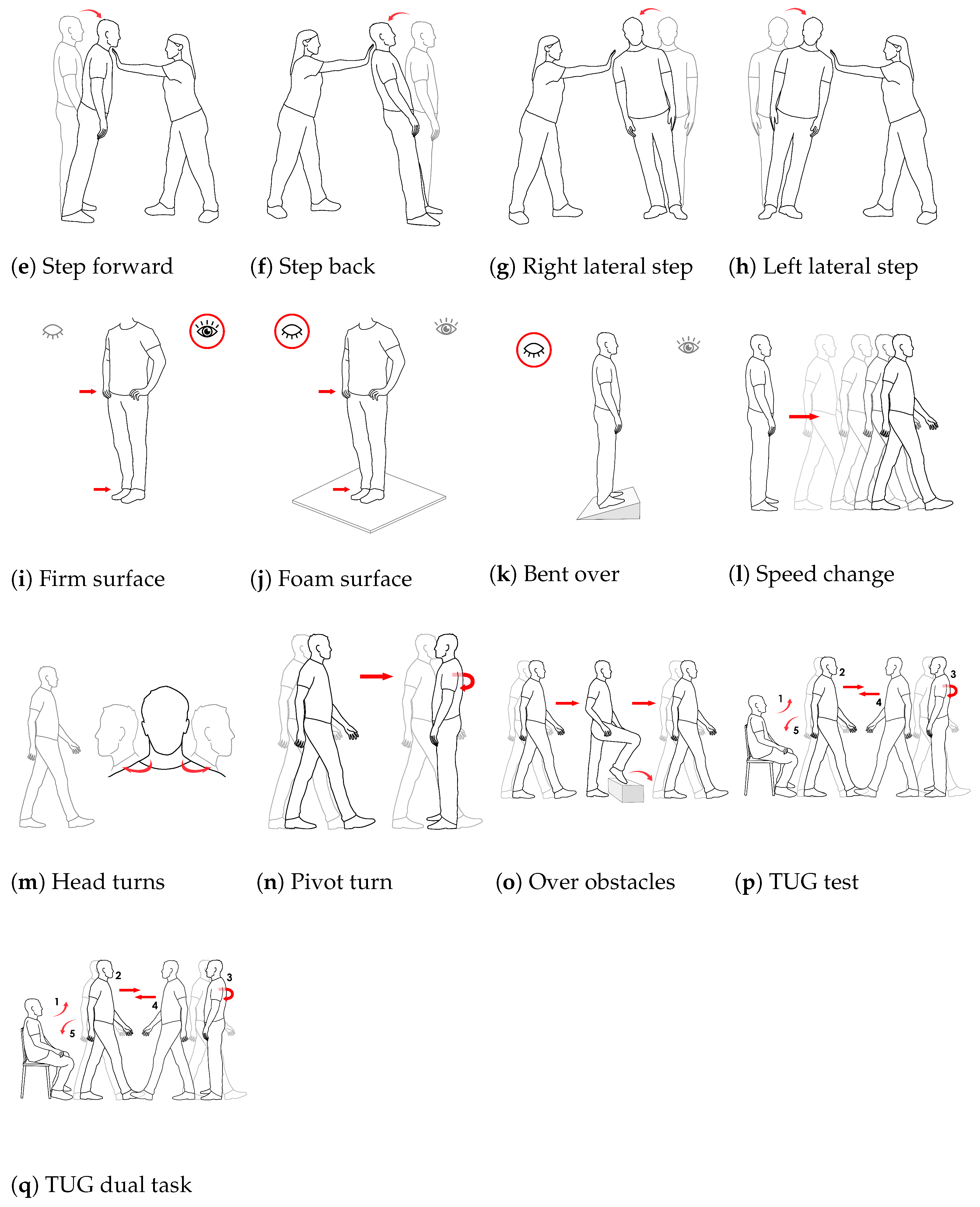
3.4. Assessment of Postural Control
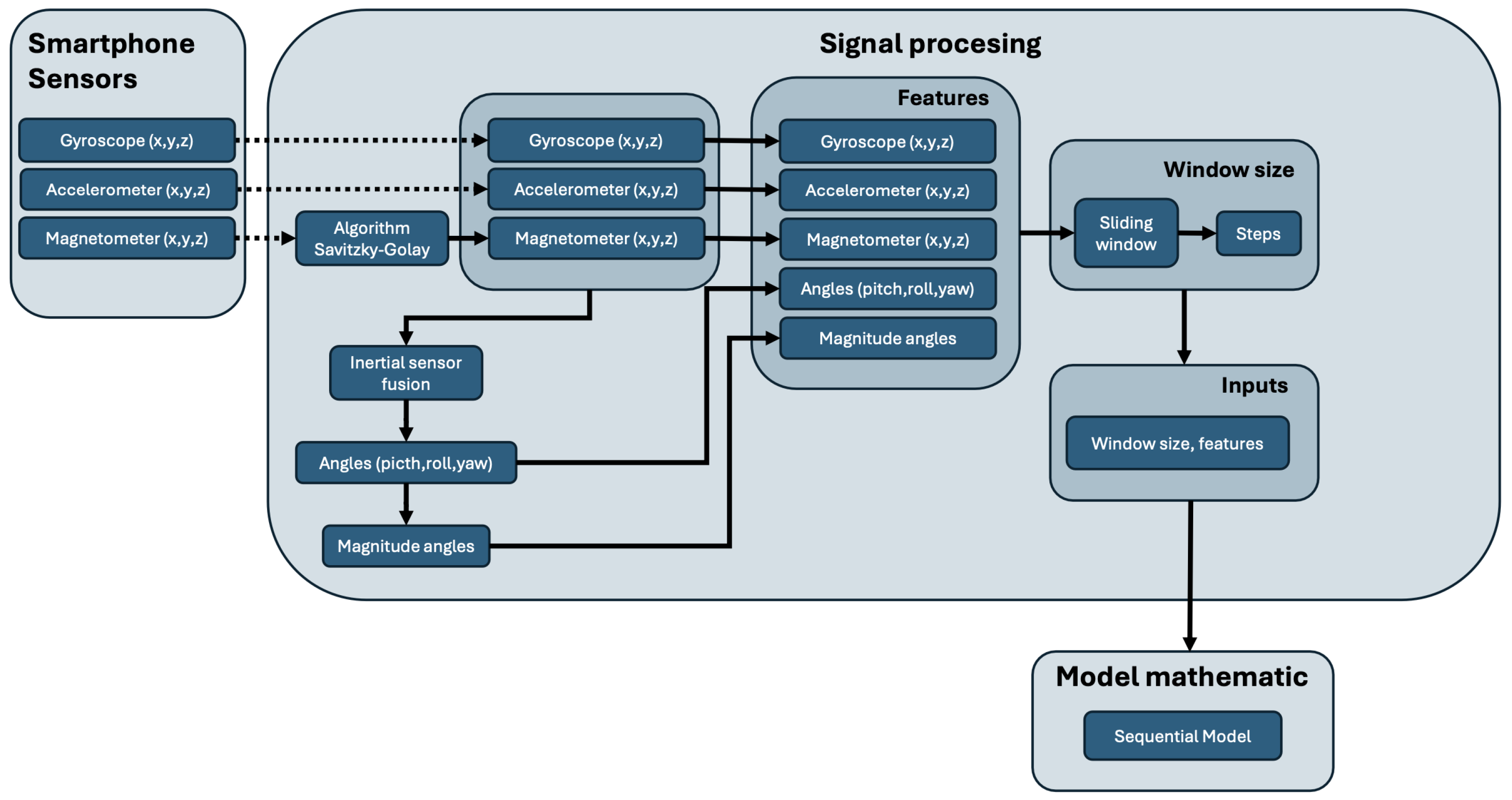
3.5. Signal Processing
3.6. Neural Network Model
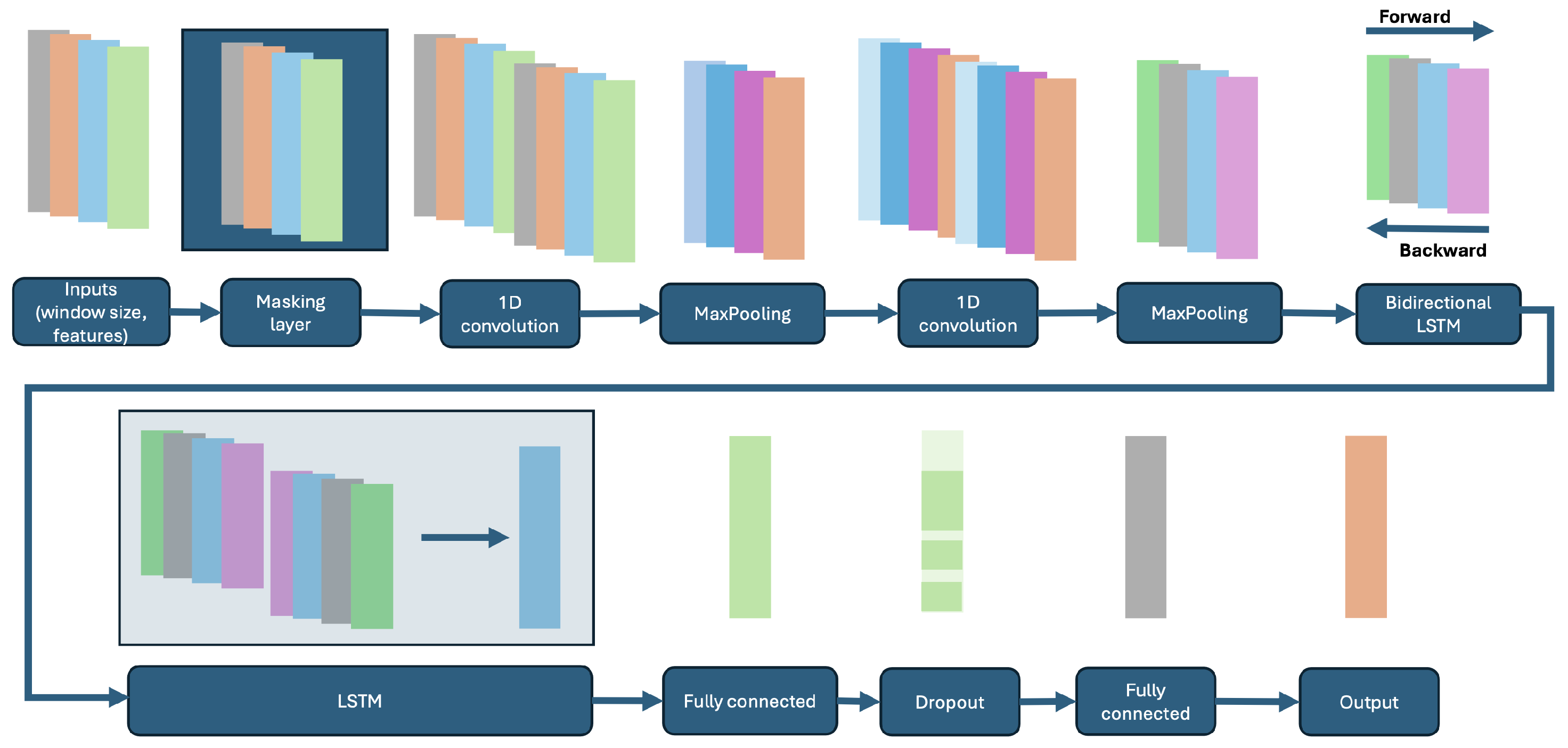
3.6.1. Architecture
- Masking Layer: A masking layer was used to ignore padded values in the input sequences, ensuring that padding does not influence the learning process [75].
- Convolutional Layers: Two convolutional layers (CNN) with ReLU activation functions were applied, followed by max pooling layers. These layers extracted temporal features from the input signals, enabling the network to learn spatial hierarchies and reduce the dimensionality of the data [76].
- Bidirectional LSTM Layer: A bidirectional LSTM (Long Short-Term Memory) layer was implemented to capture temporal dependencies in both forward and backward directions. This allowed the model to preserve information from both past and future time steps, crucial for processing time-series data related to human movement [75].
- Standard LSTM Layer: Following the bidirectional LSTM, a standard unidirectional LSTM layer with 256 units was employed to further process the temporal dependencies identified by the previous layer [75].
- Dense Layer: A fully connected dense layer with 256 units was included to process the output of the LSTM layers, providing the model with the capacity to learn complex representations of temporal features [77].
- Output Layer: The final output layer was a fully connected dense layer with a sigmoid activation function. This layer was responsible for binary classification, differentiating between individuals with a history of falls and those without [77].
3.6.2. Loss Function, Metrics, and Optimization
- Loss Function: The binary cross-entropy loss function was used to optimize the model. This function is suitable for binary classification tasks, as it quantifies the difference between the predicted probability and the actual class label [78].
- Evaluation Metric: The model was evaluated using the F1 score, which is a harmonic mean of precision and recall. This metric is especially useful in imbalanced datasets where both false positives and false negatives need to be carefully accounted for [79].
- Optimizer: The ADAM (Adaptive Moment Estimation) optimizer was employed to update the network weights. ADAM is well-suited for deep learning models as it adapts the learning rate during training and efficiently handles sparse gradients [79].
3.6.3. Training and Callbacks
- EarlyStopping: This callback monitors the validation loss during training and stops the process if no improvements are observed over a set number of epochs. This prevents the model from overfitting by terminating the training when further learning yields diminishing returns [80].
3.7. Data Split
3.8. Data Analysis
- Accuracy: Accuracy is the ratio of correctly predicted observations to the total observations. It is a measure of how well the model predicts both fallers and non-fallers. The formula for accuracy iswhere TP represents true positives, true negatives, false positives, and false negatives [82].
- Precision: Also known as positive predictive value, precision is the ratio of correctly predicted fallers (true positives) to all the instances classified as fallers (true positives and false positives). Precision is crucial when the cost of false positives is high [83]:
- Recall (Sensitivity): Recall, or sensitivity, measures the model’s ability to correctly identify all the fallers (true positives). A high recall indicates that the model successfully detects most of the actual fallers [84]:
- Specificity: Specificity, or true negative rate, refers to the ability of the model to correctly identify non-fallers, i.e., the proportion of true negatives among all the actual non-fallers [84]:
- Score: The score is the harmonic mean of precision and recall, providing a single metric that balances both:This metric is especially useful when dealing with imbalanced datasets, as it accounts for both false positives and false negatives [85].
- Balanced Accuracy: Balanced accuracy is the average of recall and specificity. It is used to handle imbalanced datasets by considering both fallers and non-fallers equally [86]:
Operational Definitions of Performance Thresholds
3.9. Variability Measurement
4. Results
4.1. Model Training and Evaluation Process
4.2. Postural Control Tasks
- -
- Sitting to Standing showed a moderate accuracy of 0.6503, but stood out with a high recall of 0.9610, indicating that the model was very effective in identifying positive cases (individuals with the condition being evaluated). However, the low specificity (0.2672) suggested that the model struggled to correctly identify negative cases. This could indicate that the model tended to over-predict risk.
- -
- Stand on Tiptoe showed perfect accuracy (1.0000) and specificity, meaning that the model had no false positives for this task. However, its recall of 0.5290 indicated that almost half of the positive cases were not correctly identified. This suggested that while the model is accurate, it struggled to detect all possible falls.
- -
- Left-leg and right-leg support tasks presented more homogeneous results, with balanced accuracies of 0.8278 and 0.7386, respectively. Both had a good combination of precision and recall, indicating reasonable performance in correctly identifying positive and negative cases.
4.3. Reactive Control Tasks (Compensatory Corrections)
- -
- Correction with a Step Forward: The precision and recall values were close to 0.81, indicating task consistency and ability to handle both positive and negative cases well. This was reflected in a balanced precision of 0.8097.
- -
- Correction with a Step Back: This stood out for its high F1 score of 0.8917 and good specificity (0.9371), indicating a strong overall performance. It is one of the best tasks for predicting falls, with a solid balance between sensitivity and specificity.
- -
- Corrections with Left and Right Lateral Steps: This demonstrated lower balanced accuracies (0.6696 and 0.7220), which indicated that the model had difficulty correctly differentiating between positive and negative cases under these lateral corrections.
4.4. Sensory Orientation Tasks
- -
- Standing, Eyes Open, Firm Surface: Perfect recall (1.0000) was observed, meaning the model detected all positive cases, but its low specificity (0.3220) suggestsa high number of false positives. The model tended to be very conservative, misclassifying negative cases as positive.
- -
- Standing, Eyes Open, Foam Surface: This demonstrated a more balanced performance, with a balanced accuracy of 0.7816, indicating a better ability to distinguish between positive and negative cases.
- -
- Bent Over, Eyes Closed: This showed excellent precision (0.9986) and specificity (0.9987), meaning almost no false positives are predicted. However, the relatively low recall (0.6207) indicated that it failed to detect some positive cases, which could be concerning in fall prediction contexts.
4.5. Dynamic Gait Tasks
- -
- Gait Speed Change and Walking with a Pivot Turn: These exhibited strong balanced accuracies (0.8487 and 0.8729), with good values for both precision and recall. This suggested that the model performed effectively in predicting falls based on changes in gait speed and pivot turns during walking.
- -
- Walking Over Obstacles: This had an excellent recall of 0.9922, meaning the model detected almost all positive cases. However, lower specificity (0.6725) may result in some false positives.
- -
- Timed Up and Go (TUG) Test: These showed high recall (0.9670), suggesting it was effective in identifying those at risk, although a specificity of 0.5918 suggested some false positives.
- -
- Dual Task over Three Meters: This had the lowest balanced accuracy (0.6077), indicating that the model struggled to make accurate predictions on this task, with less effectiveness in distinguishing between positive and negative cases.
4.6. Performance Analysis with Combined Signals
- -
- Accuracy: The model achieved an accuracy of 0.8855, which was higher than most of the individual tasks, except for a few tasks such as “Walking over obstacles” and “One-step back correction”, which also demonstrated high accuracy. Combining all the signals improved the model’s ability to generalize between fallers and non-fallers, resulting in better overall performance.
- -
- Precision: An accuracy of 0.9014 was remarkably high, which indicated that the model was very effective in correctly predicting positive cases (fallers) while minimizing false positives when all signals were used together.
- -
- Recall: The recall of 0.8793 was also high, suggesting that the model was effective in identifying most positive cases (fallers), which is crucial in fall prevention contexts.
- -
- F1 Score: With an F1 score of 0.8902, the model demonstrated a good balance between precision and recall, which is critical in classification tasks like fall risk, where both correct detection and reduction of false positives are essential.
- -
- Specificity: The specificity of 0.8924 indicated that the model was also very effective at correctly identifying negative cases (non-fallers), reducing the number of false positives.
- -
- Balanced Accuracy: With a balanced accuracy of 0.8859, the overall model performance was significantly improved compared to individual tasks. This suggested that combining all signals provided a more complete and robust assessment of fall risk by integrating various aspects of postural control, sensory orientation, and dynamic gait.
4.7. Comparison with Individual Task Results
- -
- Overall Improved Performance: When combining all signals, the model showed better precision, recall and F1 score metrics compared to most individual tasks. This suggested that signals from multiple tasks contributed complementarily to improving classification between fallers and non-fallers.
- -
- Reduced Variability in Metrics: The results for individual tasks showed more variability in metrics, with some tasks showing high precision but low recall or low specificity. By combining all signals, these discrepancies appeared to be reduced, suggesting that using all signals together provided a more balanced and stable model.
- -
- Higher Specificity and Recall Together: Individual tasks showed challenges with either specificity or recall in several cases. For example, “Sitting to Standing” had a high recall (0.9610) but low specificity (0.2672), while “Correction with a Step Back” had a recall of 0.8248 and excellent specificity of 0.9371. By combining all signals, the model achieved high specificity (0.8924) and recall (0.8793) simultaneously, which was a significant improvement in overall performance.
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| EP | Elderly People |
| CoM | Center of Mass |
| LSTM | Long Short-Term Memory |
| CNN | Convolutional Layers |
| Bidir-LSTM | Bidirectional Residual Deep Short-Term Memory |
| BiLSTM | Bidirectional Long Short-Term Memory Network |
| HAR | Human Activity Recognition |
References
- Ganz, D.; Latham, N. Prevention of falls in community-dwelling older adults. N. Engl. J. Med. 2020, 382, 734–743. [Google Scholar] [CrossRef] [PubMed]
- James, S.; Lucchesi, L.; Bisignano, C.; Castle, C.; Dingels, Z.; Fox, J.; Hamilton, E.; Henry, N.; Krohn, K.; Liu, Z.; et al. The global burden of falls: Global, regional and national estimates of morbidity and mortality from the Global Burden of Disease Study 2017. Inj. Prev. 2020, 26, i3–i11. [Google Scholar] [CrossRef] [PubMed]
- Montero-Odasso, M.; Van Der Velde, N.; Martin, F.; Petrovic, M.; Tan, M.; Ryg, J.; Aguilar-Navarro, S.; Alexander, N.; Becker, C.; Blain, H.; et al. World guidelines for falls prevention and management for older adults: A global initiative. Age Ageing 2022, 51, afac205. [Google Scholar] [CrossRef] [PubMed]
- Salari, N.; Darvishi, N.; Ahmadipanah, M.; Shohaimi, S.; Mohammadi, M. Global prevalence of falls in the older adults: A comprehensive systematic review and meta-analysis. J. Orthop. Surg. Res. 2022, 17, 334. [Google Scholar] [CrossRef]
- Plaut, P.; Shach-Pinsly, D.; Schreuer, N.; Kizony, R. The reflection of the fear of falls and risk of falling in walking activity spaces of older adults in various urban environments. J. Transp. Geogr. 2021, 95, 103152. [Google Scholar] [CrossRef]
- Reider, L.; Falvey, J.; Okoye, S.; Wolff, J.; Levy, J. Cost of US emergency department and inpatient visits for fall injuries in older adults. Injury 2024, 55, 111199. [Google Scholar] [CrossRef]
- Wu, J.; Mu, Z.; Jiang, S.; Miao, Y.; Tang, Y.; Wang, J.; Wang, S.; Zhao, Y. Trends in all-cause mortality and leading causes of death from 2009 to 2019 among older adults in China. BMC Geriatr. 2023, 23, 645. [Google Scholar] [CrossRef]
- World Health Organization. Step Safely: Strategies for Preventing and Managing Falls Across the Life-Course; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Bouvard, B.; Annweiler, C.; Legr, E. Osteoporosis in older adults. Jt. Bone Spine 2021, 88, 105135. [Google Scholar] [CrossRef]
- Meng, S.; Tong, M.; Yu, Y.; Cao, Y.; Tang, B.; Shi, X.; Liu, K. The prevalence of osteoporotic fractures in the elderly in China: A systematic review and meta-analysis. J. Orthop. Surg. Res. 2023, 18, 536. [Google Scholar] [CrossRef]
- Rath, R.; Wade, M. The two faces of postural control in older adults: Stability and function. EBioMedicine 2017, 21, 5–6. [Google Scholar] [CrossRef]
- Kanekar, N.; Aruin, A. Aging and balance control in response to external perturbations: Role of anticipatory and compensatory postural mechanisms. Age 2014, 36, 1067–1077. [Google Scholar] [CrossRef] [PubMed]
- Martinikorena, I.; Martínez-Ramírez, A.; Gómez, M.; Lecumberri, P.; Casas-Herrero, A.; Cadore, E.L.; Millor, N.; Zambom-Ferraresi, F.; Idoate, F.; Izquierdo, M. Gait variability related to muscle quality and muscle power output in frail nonagenarian older adults. J. Am. Med. Dir. Assoc. 2016, 17, 162–167. [Google Scholar] [CrossRef]
- Michalska, J.; Kamieniarz, A.; Sobota, G.; Stania, M.; Juras, G.; Słomka, K. Age-related changes in postural control in older women: Transitional tasks in step initiation. BMC Geriatr. 2021, 21, 17. [Google Scholar] [CrossRef] [PubMed]
- Van Humbeeck, N.; Kliegl, R.; Krampe, R. Lifespan changes in postural control. Sci. Rep. 2023, 13, 541. [Google Scholar] [CrossRef] [PubMed]
- Wleklik, M.; Uchmanowicz, I.; Jankowska, E.; Vitale, C.; Lisiak, M.; Drozd, M.; Pobrotyn, P.; Tkaczyszyn, M.; Lee, C. Multidimensional approach to frailty. Front. Psychol. 2020, 11, 564. [Google Scholar] [CrossRef]
- Fried, L.; Cohen, A.; Xue, Q.; Walston, J.; Bandeen-Roche, K.; Varadhan, R. The physical frailty syndrome as a transition from homeostatic symphony to cacophony. Nat. Aging 2021, 1, 36–46. [Google Scholar] [CrossRef]
- Dlima, S.; Hall, A.; Aminu, A.; Akpan, A.; Todd, C.; Vardy, E. Frailty: A global health challenge in need of local action. BMJ Glob. Health 2024, 9, e015173. [Google Scholar] [CrossRef]
- Guo, X.; Pei, J.; Ma, Y.; Cui, Y.; Guo, J.; Wei, Y.; Han, L. Cognitive frailty as a predictor of future falls in older adults: A systematic review and meta-analysis. J. Am. Med. Dir. Assoc. 2023, 24, 38–47. [Google Scholar] [CrossRef]
- Porta, M. A Dictionary of Epidemiology; Oxford University Press: Oxford, UK, 2014. [Google Scholar]
- Ríos-Fraustro, C.; Galván-Plata, M.E.; Gómez-Galicia, D.L.; Giraldo-Rodríguez, L.; Agudelo-Botero, M.; Mino-León, D. Intrinsic and extrinsic factors associated with falls in older adults: A case-control study in Mexico. Gac Med Mex. 2021, 157, 127–132. [Google Scholar] [CrossRef]
- Nugraha, S.; Sabarinah, S.; Susilowati, I.; Rahardjo, T. Intrinsic and extrinsic risk factor for fall among community dwelling Indonesian elderly. Open Access Maced. J. Med. Sci. 2022, 10, 619–624. [Google Scholar] [CrossRef]
- Ambrose, A.; Paul, G.; Hausdorff, J. Risk factors for falls among older adults: A review of the literature. Maturitas 2013, 75, 51–61. [Google Scholar] [CrossRef] [PubMed]
- Yingyongyudha, A.; Saengsirisuwan, V.; Panichaporn, W.; Boonsinsukh, R. The Mini-Balance Evaluation Systems Test (Mini-BESTest) demonstrates higher accuracy in identifying older adult participants with history of falls than do the BESTest, Berg Balance Scale, or Timed Up and Go Test. J. Geriatr. Phys. Ther. 2016, 39, 64–70. [Google Scholar] [CrossRef]
- Magnani, P.; Genovez, M.; Porto, J.; Zanellato, N.; Alvarenga, I.; Freire, R., Jr.; Abreu, D. Use of the BESTest and the Mini-BESTest for fall risk prediction in community-dwelling older adults between 60 and 102 years of age. J. Geriatr. Phys. Ther. 2020, 43, 179–184. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, M.; Booth, J. Preventing falls in older adults: A multifactorial approach. Home Health Care Manag. Pract. 2006, 19, 45–50. [Google Scholar] [CrossRef]
- Kim, T.; Park, J.; Heo, S.; Sung, K.; Park, J. Characterizing dynamic walking patterns and detecting falls with wearable sensors using Gaussian process methods. Sensors 2017, 17, 1172. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.; Xiong, S. Comparison of seven fall risk assessment tools in community-dwelling Korean older women. Ergonomics 2017, 60, 421–429. [Google Scholar] [CrossRef]
- Park, S. Tools for assessing fall risk in the elderly: A systematic review and meta-analysis. Aging Clin. Exp. Res. 2018, 30, 1–16. [Google Scholar] [CrossRef]
- Tinetti, M.; Williams, T.; Mayewski, R. Fall risk index for elderly patients based on number of chronic disabilities. Am. J. Med. 1986, 80, 429–434. [Google Scholar] [CrossRef]
- Berg, K. Balance and its measure in the elderly: A review. Physiother. Can. 1989, 41, 240–246. [Google Scholar] [CrossRef]
- Whitney, S.; Hudak, M.; Marchetti, G. The dynamic gait index relates to self-reported fall history in individuals with vestibular dysfunction. J. Vestib. Res. 2000, 10, 99–105. [Google Scholar] [CrossRef]
- Horak, F.B. Postural orientation and equilibrium: What do we need to know about neural control of balance to prevent falls? Age Ageing 2006, 35 (Suppl. S2), ii7–ii11. [Google Scholar] [CrossRef] [PubMed]
- Bet, P.; Castro, P.; Ponti, M. Fall detection and fall risk assessment in older person using wearable sensors: A systematic review. Int. J. Med. Inform. 2019, 130, 103946. [Google Scholar]
- Wang, K.; Delbaere, K.; Brodie, M.; Lovell, N.; Kark, L.; Lord, S.; Redmond, S. Differences between gait on stairs and flat surfaces in relation to fall risk and future falls. IEEE J. Biomed. Health Inform. 2017, 21, 1479–1486. [Google Scholar] [CrossRef]
- Najafi, B.; Aminian, K.; Loew, F.; Blanc, Y.; Robert, P. Measurement of stand-sit and sit-stand transitions using a miniature gyroscope and its application in fall risk evaluation in the elderly. IEEE Trans. Biomed. Eng. 2002, 49, 843–851. [Google Scholar] [CrossRef] [PubMed]
- Di Rosa, M.; Hausdorff, J.; Stara, V.; Rossi, L.; Glynn, L.; Casey, M.; Burkard, S.; Cherubini, A. Concurrent validation of an index to estimate fall risk in community dwelling seniors through a wireless sensor insole system: A pilot study. Gait Posture 2017, 55, 6–11. [Google Scholar] [CrossRef]
- Nait Aicha, A.; Englebienne, G.; Van Schooten, K.; Pijnappels, M.; Kröse, B. Deep learning to predict falls in older adults based on daily-life trunk accelerometry. Sensors 2018, 18, 1654. [Google Scholar] [CrossRef] [PubMed]
- Drover, D.; Howcroft, J.; Kofman, J.; Lemaire, E. Faller classification in older adults using wearable sensors based on turn and straight-walking accelerometer-based features. Sensors 2017, 17, 1321. [Google Scholar] [CrossRef]
- Hua, A.; Quicksall, Z.; Di, C.; Motl, R.; LaCroix, A.; Schatz, B.; Buchner, D. Accelerometer-based predictive models of fall risk in older women: A pilot study. NPJ Digit. Med. 2018, 1, 1–8. [Google Scholar]
- Sun, R.; Sosnoff, J. Novel sensing technology in fall risk assessment in older adults: A systematic review. BMC Geriatr. 2018, 18, 1–10. [Google Scholar]
- Howcroft, J.; Kofman, J.; Lemaire, E. Prospective fall-risk prediction models for older adults based on wearable sensors. IEEE Trans. Neural Syst. Rehabil. Eng. 2017, 25, 1812–1820. [Google Scholar] [CrossRef]
- Greene, B.; McGrath, D.; Walsh, L.; Doheny, E.; McKeown, D.; Garattini, C.; Cunningham, C.; Crosby, L.; Caulfield, B.; Kenny, R. Quantitative falls risk estimation through multi-sensor assessment of standing balance. Physiol. Meas. 2012, 33, 2049. [Google Scholar] [CrossRef] [PubMed]
- Senden, R.; Savelberg, H.; Grimm, B.; Heyligers, I.; Meijer, K. Accelerometry-based gait analysis, an additional objective approach to screen subjects at risk for falling. Gait Posture 2012, 36, 296–300. [Google Scholar] [CrossRef] [PubMed]
- Doi, T.; Hirata, S.; Ono, R.; Tsutsumimoto, K.; Misu, S.; Ando, H. The harmonic ratio of trunk acceleration predicts falling among older people: Results of a 1-year prospective study. J. Neuroeng. Rehabil. 2013, 10, 7. [Google Scholar] [CrossRef]
- Farshchiansadegh, A.; Others Engineering in Medicine and Biology Society (EMBC). A body machine interface based on inertial sensors. In Proceedings of the 2014 36th Annual International Conference of the IEEE, Chicago, IL, USA, 26–30 August 2014. [Google Scholar]
- Kargar, B.; Mollahosseini, A.; Struemph, T.; Pace, W.; Nielsen, R.; Mahoor, M. Automatic measurement of physical mobility in get-up-and-go test using kinect sensor. In Proceedings of the 2014 36th Annual International Conference of The IEEE Engineering In Medicine And Biology Society, Chicago, IL, USA, 26–30 August 2014; pp. 3492–3495. [Google Scholar]
- Yamada, M.; Aoyama, T.; Nakamura, M.; Tanaka, B.; Nagai, K.; Tatematsu, N.; Uemura, K.; Nakamura, T.; Tsuboyama, T.; Ichihashi, N. The reliability and preliminary validity of game-based fall risk assessment in community-dwelling older adults. Geriatr. Nurs. 2011, 32, 188–194. [Google Scholar] [CrossRef] [PubMed]
- Kwok, B.; Clark, R.; Pua, Y. Novel use of the Wii Balance Board to prospectively predict falls in community-dwelling older adults. Clin. Biomech. 2015, 30, 481–484. [Google Scholar] [CrossRef]
- Nishiguchi, S.; Yamada, M.; Uemura, K.; Matsumura, T.; Takahashi, M.; Moriguchi, T.; Aoyama, T. A novel infrared laser device that measures multilateral parameters of stepping performance for assessment of all risk in elderly individuals. Aging Clin. Exp. Res. 2013, 25, 311–316. [Google Scholar] [CrossRef]
- Poggio, T.; Girosi, F. Networks for approximation and learning. Proc. IEEE 1990, 78, 1481–1497. [Google Scholar] [CrossRef]
- Cortes, C.; Vapnik, V. Support-vector networks. Mach. Learn. 1995, 20, 273–297. [Google Scholar] [CrossRef]
- Makino, K.; Lee, S.; Bae, S.; Chiba, I.; Harada, K.; Katayama, O.; Tomida, K.; Morikawa, M.; Shimada, H. Simplified Decision-Tree Algorithm to Predict Falls for Community-Dwelling Older Adults. J. Clin. Med. 2021, 10, 5184. [Google Scholar] [CrossRef]
- Chen, M.; Wang, H.; Yu, L.; Yeung, E.H.K.; Luo, J.; Tsui, K.-L.; Zhao, Y. A Systematic Review of Wearable Sensor-Based Technologies for Fall Risk Assessment in Older Adults. Sensors 2022, 22, 6752. [Google Scholar] [CrossRef]
- Shany, T.; Redmond, S.J.; Narayanan, M.R.; Lovell, N.H. Toward the development of a falls risk prediction system using wearable sensors: A systematic review. J. Biomed. Health Inform. 2015, 19, 1216–1227. [Google Scholar]
- Islam, M.M.; Tayan, O.; Islam, M.R.; Islam, M.S.; Nooruddin, S.; Kabir, M.N.; Islam, M.R. Deep Learning-Based Systems Developed for Fall Detection: A Review. IEEE Access 2020, 8, 166117–166137. [Google Scholar] [CrossRef]
- Hannink, J.; Kautz, T.; Pasluosta, C.F.; Gaßner, H.; Klucken, J.; Eskofier, B.M. Sensor-based gait parameter extraction with deep convolutional neural networks. IEEE J. Biomed. Health Inform. 2017, 21, 85–93. [Google Scholar] [CrossRef]
- Savadkoohi, M.; Oladunni, T.; Thompson, L.A. Deep Neural Networks for Human’s Fall-risk Prediction using Force-Plate Time Series Signal. Expert Syst. Appl. 2021, 182, 115220. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Pan, X. Deep Learning for Inertial Positioning: A Survey. IEEE Trans. Intell. Transp. Syst. 2023, 25, 10506–10523. [Google Scholar] [CrossRef]
- Li, Y.; Wang, L. Human Activity Recognition Based on Residual Network and BiLSTM. Sensors 2022, 22, 635. [Google Scholar] [CrossRef]
- Zhao, Y.; Yang, R.; Chevalier, G.; Xu, X.; Zhang, Z. Deep Residual Bidir-LSTM for Human Activity Recognition Using Wearable Sensors. Math. Probl. Eng. 2018, 2018, 7316954. [Google Scholar] [CrossRef]
- Lee, P.; Chen, T.-B.; Wang, C.-Y.; Hsu, S.-Y.; Liu, C.-H. Detection of Postural Control in Young and Elderly Adults Using Deep and Machine Learning Methods with Joint–Node Plots. Sensors 2021, 21, 3212. [Google Scholar] [CrossRef]
- Meyer, B.M.; Tulipani, L.J.; Gurchiek, R.D.; Allen, D.A.; Adamowicz, L.; Larie, D.; Solomon, A.J.; Cheney, N.; McGinnis, R.S. Wearables and Deep Learning Classify Fall Risk From Gait in Multiple Sclerosis. IEEE Trans. Inf. Technol. Biomed. 2021, 25, 1824–1831. [Google Scholar] [CrossRef]
- Tunca, C.; Salur, G.; Ersoy, C. Deep Learning for Fall Risk Assessment with Inertial Sensors: Utilizing Domain Knowledge in Spatio-Temporal Gait Parameters. IEEE J. Biomed. Health Inform. 2020, 24, 1994–2005. [Google Scholar] [CrossRef]
- Kiprijanovska, I.; Dimitrova, G.; Kiprovski, T. Predictive models for time-series forecasting: Case study for production planning. In Proceedings of the 2020 43rd International Convention on Information, Communication and Electronic Technology (MIPRO), Opatija, Croatia, 28 September–2 October 2020; pp. 1098–1103. [Google Scholar] [CrossRef]
- Yıldız, A. Towards Environment-Aware Fall Risk Assessment: Classifying Walking Surface Conditions Using IMU-Based Gait Data and Deep Learning. Brain Sci. 2023, 13, 1428. [Google Scholar] [CrossRef] [PubMed]
- Cubuk, E.D.; Zoph, B.; Shlens, J.; Le, Q.V. AutoAugment: Learning Augmentation Policies from Data. In Proceedings of the IEEE/CVF Conference on Computer Vision and Pattern Recognition (CVPR), Long Beach, CA, USA, 15–20 June 2019. [Google Scholar]
- Wen, Q.; Sun, L.; Yang, F.; Song, X.; Gao, J.; Wang, X.; Xu, H. Time Series Data Augmentation for Deep Learning: A Survey. arXiv 2020, arXiv:2002.12478. [Google Scholar]
- Casolaro, A.; Capone, V.; Iannuzzo, G.; Camastra, F. Deep Learning for Time Series Forecasting: Advances and Open Problems. Information 2023, 14, 598. [Google Scholar] [CrossRef]
- Chandrasekaran, V.; Goeckner, D.; Wang, J.; Mayeux, R. Inertial Sensors for Smartphones: Capabilities and Accuracy. Sensors 2020, 20, 1650. [Google Scholar] [CrossRef]
- Oshin, S.; Wixted, J.; Burchell, B.; Hale, J.; Vaughan, N. Accuracy of Accelerometer and Gyroscope in Smartphones: Evaluation and Sensor Fusion. J. Mob. Technol. Med. 2014, 3, 28–34. [Google Scholar] [CrossRef]
- Del Rosario, M.B.; Redmond, S.J.; Lovell, N.H. Tracking the evolution of smartphone sensing for monitoring human movement. Sensors 2015, 15, 18901–18933. [Google Scholar] [CrossRef]
- Caruso, M.; Mariani, B. Smartphone-based accelerometers for gait analysis: A validation study with older adults. Gait Posture 2020, 81, 127–133. [Google Scholar] [CrossRef]
- Horak, F.B.; Wrisley, D.M.; Frank, J. The Balance Evaluation Systems Test (BESTest) to differentiate balance deficits. Phys. Ther. 2009, 89, 484–498. [Google Scholar]
- Ullah, A.; Ahmad, J.; Muhammad, K.; Sajjad, M.; Baik, S.W. Action recognition in video sequences using deep bi-directional LSTM with CNN features. IEEE Access 2017, 6, 1155–1166. [Google Scholar] [CrossRef]
- Muhammad, K.; Hussain, T.; Tanveer, M.; Sannino, G.; de Albuquerque, V.H.C. Cost-effective video summarization using deep CNN with hierarchical weighted fusion for IoT surveillance networks. IEEE Internet Things J. 2020, 7, 4455–4463. [Google Scholar] [CrossRef]
- Sun, W.; Qin, N.; Huang, D.; Liu, Z.; Ni, S. QN-S3VM method for evaluation of liver functional reserve. In 2020 Chinese Automation Congress (CAC); IEEE: Shanghai, China, 2020; pp. 5629–5634. [Google Scholar]
- DataCamp. Cross-Entropy Loss Function in Machine Learning: Enhancing Model Accuracy. 2023. Available online: https://www.datacamp.com (accessed on 15 September 2023).
- Analytics Vidhya. Binary Cross Entropy/Log Loss for Binary Classification. Analytics Vidhya. 2024. Available online: https://www.analyticsvidhya.com (accessed on 15 September 2023).
- Brownlee, J. How to Stop Training Deep Neural Networks at the Right Time Using Early Stopping. Machine Learning Mastery, 2019. Available online: https://machinelearningmastery.com/early-stopping-to-avoid-overtraining-neural-network-models/ (accessed on 15 September 2023).
- Cerqueira, V.; Torgo, L.; Mozetic, I. Evaluating time series forecasting models: An empirical study on performance estimation methods. Mach. Learn. 2020, 109, 1997–2028. [Google Scholar] [CrossRef]
- Baldi, P.; Brunak, S.; Chauvin, Y.; Andersen, C.A.; Nielsen, H. Assessing the accuracy of prediction algorithms for classification: An overview. Bioinformatics 2000, 16, 412–424. [Google Scholar] [CrossRef] [PubMed]
- Sokolova, M.; Lapalme, G. A systematic analysis of performance measures for classification tasks. Inf. Process. Manag. 2009, 45, 427–437. [Google Scholar] [CrossRef]
- Powers, D.M. Evaluation: From precision, recall and F-measure to ROC, informedness, markedness and correlation. J. Mach. Learn. Technol. 2011, 2, 37–63. [Google Scholar]
- Sasaki, Y. The Truth of the F-Measure; University of Manchester: Manchester, UK, 2007; Volume 1, pp. 1–5. [Google Scholar]
- Brodersen, K.H.; Ong, C.S.; Stephan, K.E.; Buhmann, J.M. The balanced accuracy and its posterior distribution. In Proceedings of the 2010 20th International Conference on Pattern Recognition, Istanbul, Turkey, 23–26 August 2010; pp. 3121–3124. [Google Scholar]
- Benavoli, A.; Corani, G.; Mangili, F. Time-series cross-validation. J. Mach. Learn. Res. 2017, 18, 1–35. [Google Scholar]
- Michie, D.; Spiegelhalter, D.J.; Taylor, C.C. Machine Learning, Neural and Statistical Classification; Ellis Horwood: Hertfordshire, UK, 1994. [Google Scholar]
- Chakraborty, P.R.; Sorwar, G. A Machine Learning Approach to Identify Fall Risk for Older Adults. Smart Health 2022, 26, 100303. [Google Scholar] [CrossRef]

| Age (Years) | Body Mass (kg) | Height (cm) | ||||
|---|---|---|---|---|---|---|
| Non Fallers | Fallers | Non Fallers | Fallers | Non Fallers | Fallers | |
| Mean | ||||||
| Std. Deviation | ||||||
| Task | Accuracy | Precision | Recall | F1-Score | Specificity | Balanced Accuracy |
|---|---|---|---|---|---|---|
| Sitting to standing | 0.6503 | 0.6009 | 0.9610 | 0.7496 | 0.2672 | 0.6317 |
| Stand on tiptoe | 0.7548 | 1.0000 | 0.5290 | 0.6893 | 1.0000 | 0.7630 |
| Left single leg support | 0.7491 | 0.9880 | 0.6812 | 0.8066 | 0.9744 | 0.8278 |
| Right single leg support | 0.7333 | 0.8024 | 0.6931 | 0.7438 | 0.7841 | 0.7386 |
| Correction with a step forward | 0.8102 | 0.8079 | 0.8117 | 0.8340 | 0.8077 | 0.8097 |
| Correction with a step back | 0.8362 | 0.9655 | 0.8248 | 0.8917 | 0.9371 | 0.8828 |
| Correction with a left lateral step | 0.7229 | 0.8361 | 0.7795 | 0.8068 | 0.5597 | 0.6696 |
| Correction with a right lateral step | 0.7243 | 0.8640 | 0.7275 | 0.7902 | 0.7166 | 0.7220 |
| Standing, eyes open, firm surface | 0.7635 | 0.7335 | 1.0000 | 0.8463 | 0.3220 | 0.6610 |
| Standing, eyes open, foam surface | 0.7958 | 0.7248 | 0.9948 | 0.8386 | 0.5648 | 0.7816 |
| Bent over, eyes closed | 0.7727 | 0.9986 | 0.6207 | 0.7656 | 0.9987 | 0.8097 |
| Gait speed change | 0.8330 | 0.9413 | 0.8059 | 0.8683 | 0.8916 | 0.8487 |
| Walk with horizontal head turns | 0.7231 | 0.8163 | 0.7538 | 0.7838 | 0.6621 | 0.7079 |
| Walking with a pivot turn | 0.8713 | 0.9038 | 0.8493 | 0.8757 | 0.8966 | 0.8729 |
| Walking over obstacles | 0.8943 | 0.8728 | 0.9922 | 0.9287 | 0.6725 | 0.8324 |
| Timed Up and Go (TUG) test | 0.7841 | 0.7135 | 0.9670 | 0.8211 | 0.5918 | 0.7794 |
| Dual task over 3 m | 0.6744 | 0.7417 | 0.7963 | 0.7680 | 0.4190 | 0.6077 |
| All combined | 0.8855 | 0.9014 | 0.8793 | 0.8902 | 0.8924 | 0.8859 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Robles Cruz, D.; Puebla Quiñones, S.; Lira Belmar, A.; Quintana Figueroa, D.; Reyes Hidalgo, M.; Taramasco Toro, C. Fall Risk Classification Using Trunk Movement Patterns from Inertial Measurement Units and Mini-BESTest in Community-Dwelling Older Adults: A Deep Learning Approach. Appl. Sci. 2024, 14, 9170. https://doi.org/10.3390/app14209170
Robles Cruz D, Puebla Quiñones S, Lira Belmar A, Quintana Figueroa D, Reyes Hidalgo M, Taramasco Toro C. Fall Risk Classification Using Trunk Movement Patterns from Inertial Measurement Units and Mini-BESTest in Community-Dwelling Older Adults: A Deep Learning Approach. Applied Sciences. 2024; 14(20):9170. https://doi.org/10.3390/app14209170
Chicago/Turabian StyleRobles Cruz, Diego, Sebastián Puebla Quiñones, Andrea Lira Belmar, Denisse Quintana Figueroa, María Reyes Hidalgo, and Carla Taramasco Toro. 2024. "Fall Risk Classification Using Trunk Movement Patterns from Inertial Measurement Units and Mini-BESTest in Community-Dwelling Older Adults: A Deep Learning Approach" Applied Sciences 14, no. 20: 9170. https://doi.org/10.3390/app14209170







