Differential Relapse of Proximal and Distal Segments after Mandibular Setback Surgery
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
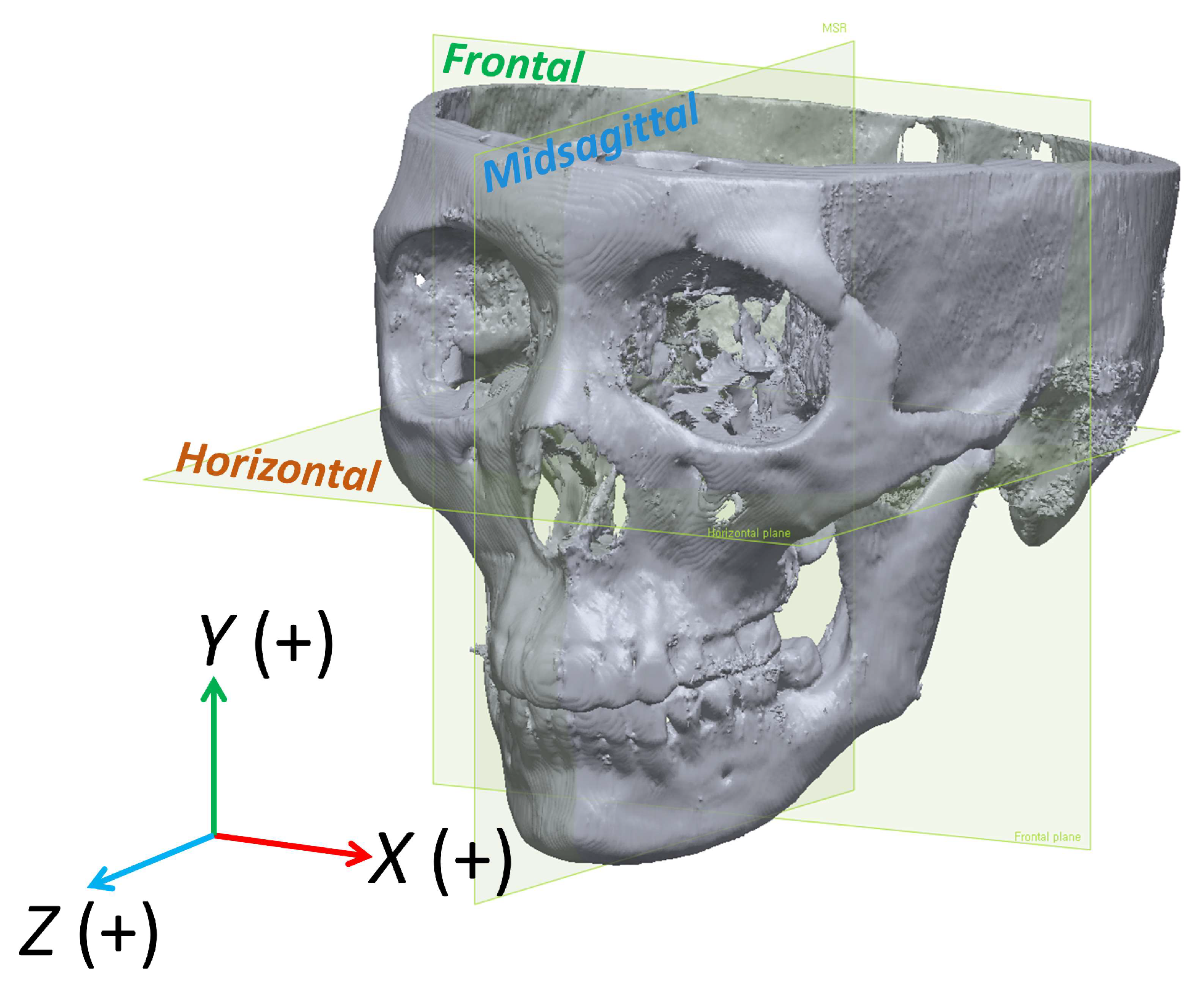
2.2. Data Acquisition and Generation of 3D Skull Model
2.3. Measurements of Variables
2.3.1. Landmarks and Measurement of Changes to Mandible
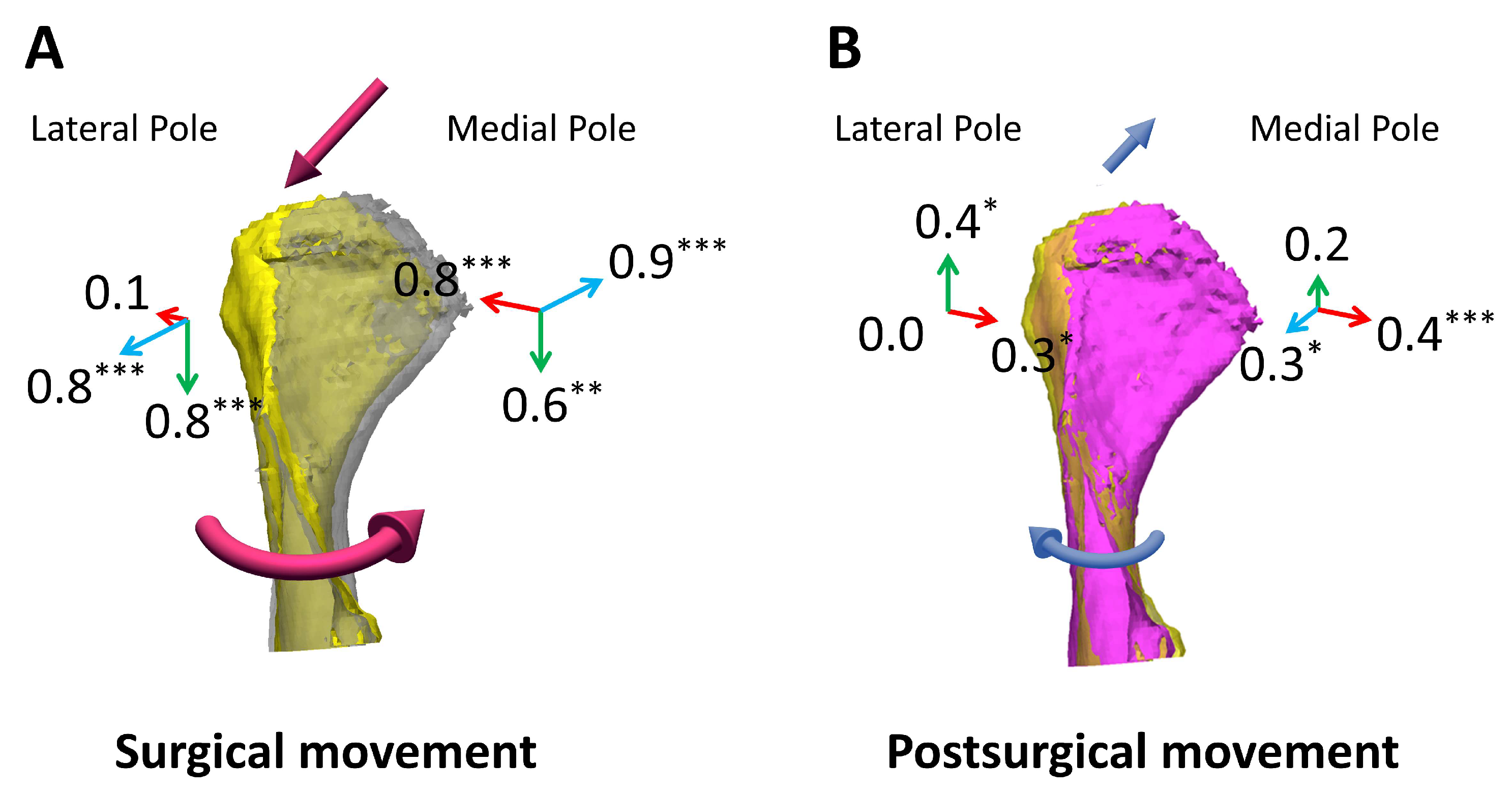
2.3.2. Measurement of Condylar Displacement
2.3.3. Measurement of the Center of Rotation of the Proximal and Distal Segments
2.4. Validation of Variable Measurement
2.5. Statistical Analysis
3. Results
3.1. Condylar Displacement
3.2. Relapse of Proximal and Distal Segments and Their Center of Rotation
3.3. Associations between VBS Development and Center of Rotation
3.4. Associations between VBS Development and Postsurgical Changes
3.5. Comparison of Postsurgical Changes between Single-Jaw and Double-Jaw Surgeries
4. Discussion
5. Conclusions
- The mandibular condyles rotated medially with lateral and downward movement during mandibular setback surgery. They gradually recovered during postsurgical orthodontic treatment but never fully returned to the pretreatment position.
- During the postoperative healing period, the mesial and distal fragments of the mandible each have different centers of rotation (CRot) and move differently.
- Increased VBS during surgery was correlated with greater relapse of the mandibular setback and a corresponding posterosuperior shift of the CRot of the distal segment.
- Two regression equations were formulated to predict the coordinates of the CRot of the distal segment for the postsurgical relapse. These can be used to simulate relapse during the surgery simulation, although they need external validation.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kim, J.-W.; Lee, N.-K.; Yun, P.-Y.; Moon, S.-W.; Kim, Y.-K. Postsurgical Stability After Mandibular Setback Surgery with Minimal Orthodontic Preparation Following Upper Premolar Extraction. J. Oral Maxillofac. Surg. 2013, 71, 1968.e1–1968.e11. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.-S.; Lee, S.-C.; Kyung, H.-M.; Park, H.-S.; Kwon, T.-G. Stability of Mandibular Setback Surgery with and Without Presurgical Orthodontics. J. Oral Maxillofac. Surg. 2014, 72, 779–787. [Google Scholar] [CrossRef] [PubMed]
- Ko, E.W.-C.; Hsu, S.S.-P.; Hsieh, H.-Y.; Wang, Y.-C.; Huang, C.S.; Chen, Y.R. Comparison of Progressive Cephalometric Changes and Postsurgical Stability of Skeletal Class III Correction with and without Presurgical Orthodontic Treatment. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2011, 69, 1469–1477. [Google Scholar] [CrossRef] [PubMed]
- Al-Delayme, R.M.A.; Alsagban, A.A.R.; Ahmed, F.T.; Farag, A.; Al-Allaq, T.; Virdee, P.; Alnajjar, Z.; Alsamaraie, S.A.I.; Elnashef, S.; Arab, L.; et al. The Direction of Double-Jaw Surgery Relapse for Correction of Skeletal Class III Deformity: Bilateral Sagittal Split Versus Intraoral Vertical Ramus Setback Osteotomies. J. Maxillofac. Oral Surg. 2019, 18, 280–287. [Google Scholar] [CrossRef] [PubMed]
- Lee, N.-K.; Kim, Y.-K.; Yun, P.-Y.; Kim, J.-W. Evaluation of Post-Surgical Relapse after Mandibular Setback Surgery with Minimal Orthodontic Preparation. J. Cranio-Maxillofac. Surg. Off. Publ. Eur. Assoc. Cranio-Maxillofac. Surg. 2013, 41, 47–51. [Google Scholar] [CrossRef]
- Park, H.-M.; Yang, I.-H.; Choi, J.-Y.; Lee, J.-H.; Kim, M.-J.; Baek, S.-H. Postsurgical Relapse in Class III Patients Treated with Two-Jaw Surgery: Conventional Three-Stage Method Versus Surgery-First Approach. J. Craniofac. Surg. 2015, 26, 2357–2363. [Google Scholar] [CrossRef]
- Proffit, W.R.; Phillips, C.; Turvey, T.A. Stability After Mandibular Setback: Mandible-Only Versus 2-Jaw Surgery. J. Oral Maxillofac. Surg. 2012, 70, e408–e414. [Google Scholar] [CrossRef]
- Cho, H.J. Long-Term Stability of Surgical Mandibular Setback. Angle Orthod. 2007, 77, 851–856. [Google Scholar] [CrossRef]
- Proffit, W.R.; Turvey, T.A.; Phillips, C. The Hierarchy of Stability and Predictability in Orthognathic Surgery with Rigid Fixation: An Update and Extension. Head Face Med. 2007, 3, 21. [Google Scholar] [CrossRef]
- Komori, E.; Aigase, K.; Sugisaki, M.; Tanabe, H. Cause of Early Skeletal Relapse after Mandibular Setback. Am. J. Orthod. Dentofac. Orthop. 1989, 95, 29–36. [Google Scholar] [CrossRef]
- Chou, J.I.-C.; Fong, H.-J.; Kuang, S.-H.; Gi, L.-Y.; Hwang, F.-Y.; Lai, Y.-C.; Chang, R.C.-S.; Kao, S.-Y. A Retrospective Analysis of the Stability and Relapse of Soft and Hard Tissue Change after Bilateral Sagittal Split Osteotomy for Mandibular Setback of 64 Taiwanese Patients. J. Oral Maxillofac. Surg. 2005, 63, 355–361. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.-H.; Lee, J.-H.; Cho, J.-Y.; Lee, J.-H.; Kim, K.-W. Skeletal Stability After Simultaneous Mandibular Angle Resection and Sagittal Split Ramus Osteotomy for Correction of Mandible Prognathism. J. Oral Maxillofac. Surg. 2007, 65, 192–197. [Google Scholar] [CrossRef]
- Paeng, J.-Y.; Hong, J.; Kim, C.-S.; Kim, M.-J. Comparative Study of Skeletal Stability between Bicortical Resorbable and Titanium Screw Fixation after Sagittal Split Ramus Osteotomy for Mandibular Prognathism. J. Cranio-Maxillofac. Surg. Off. Publ. Eur. Assoc. Cranio-Maxillofac. Surg. 2012, 40, 660–664. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.J.; Hwang, S.J. Change in Condylar Position in Posterior Bending Osteotomy Minimizing Condylar Torque in BSSRO for Facial Asymmetry. J. Cranio-Maxillofac. Surg. 2014, 42, 325–332. [Google Scholar] [CrossRef] [PubMed]
- Costa, F.; Robiony, M.; Toro, C.; Sembronio, S.; Polini, F.; Politi, M. Condylar Positioning Devices for Orthognathic Surgery: A Literature Review. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2008, 106, 179–190. [Google Scholar] [CrossRef]
- Wolford, L.M.; Reiche-Fischel, O.; Mehra, P. Changes in Temporomandibular Joint Dysfunction after Orthognathic Surgery. J. Oral Maxillofac. Surg. 2003, 61, 655–660. [Google Scholar] [CrossRef] [PubMed]
- Batbold, M.; Lim, S.-H.; Jeong, S.-R.; Oh, J.-S.; Kim, S.-J.; Kim, Y.-J.; Cho, J.-H.; Kang, K.-H.; Kim, M.; Hong, M.; et al. Vertical Bony Step between Proximal and Distal Segments after Mandibular Setback Is Related with Relapse: A Cone-Beam Computed Tomographic Study. Am. J. Orthod. Dentofac. Orthop. 2022, 161, e524–e533. [Google Scholar] [CrossRef]
- Yang, H.J.; Hwang, S.J. Contributing Factors to Intraoperative Clockwise Rotation of the Proximal Segment as a Relapse Factor after Mandibular Setback with Sagittal Split Ramus Osteotomy. J. Cranio-Maxillofac. Surg. 2014, 42, e57–e63. [Google Scholar] [CrossRef]
- Kim, H.-M.; Lim, S.-H.; Oh, J.-S.; Jeong, S.-R.; Kang, S.-G. Orthodontic Treatment with Isolated Mandibular Setback Surgery: Use of 3D Surgical Simulation including Postsurgical Relapse of Mandibular Setback. Clin. J. Korean Assoc. Orthod. 2022, 12, 36–52. [Google Scholar] [CrossRef]
- Olbrisch, C.; Santander, P.; Moser, N.; Klenke, D.; Meyer-Marcotty, P.; Quast, A. Three-Dimensional Mandibular Characteristics in Skeletal Malocclusion: A Cross-Sectional Study. J. Orofac. Orthop. Fortschritte Kieferorthopadie Organ Off. J. Dtsch. Ges. Kieferorthopadie 2024, 85, 134–145. [Google Scholar] [CrossRef]
- You, K.H.; Lee, K.J.; Lee, S.H.; Baik, H.S. Three-Dimensional Computed Tomography Analysis of Mandibular Morphology in Patients with Facial Asymmetry and Mandibular Prognathism. Am. J. Orthod. Dentofac. Orthop. Off. Publ. Am. Assoc. Orthod. Its Const. Soc. Am. Board Orthod. 2010, 138, 540.e1–e8; discussion 540–541. [Google Scholar] [CrossRef] [PubMed]
- Ehardt, L.; Ruellas, A.; Edwards, S.; Benavides, E.; Ames, M.; Cevidanes, L. Long-Term Stability and Condylar Remodeling after Mandibular Advancement: A 5-Year Follow-Up. Am. J. Orthod. Dentofac. Orthop. Off. Publ. Am. Assoc. Orthod. Its Const. Soc. Am. Board Orthod. 2021, 159, 613–626. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.; Park, J.U. Three-Dimensional Evaluation of Positional Change of the Condyle after Mandibular Setback by Means of Bilateral Sagittal Split Ramus Osteotomy. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2002, 94, 305–309. [Google Scholar] [CrossRef] [PubMed]
- Hwang, H.-S.; Jiang, T.; Sun, L.; Lee, K.-M.; Oh, M.-H.; Biao, Y.; Oh, H.-K.; Bechtold, T.E. Condylar Head Remodeling Compensating for Condylar Head Displacement by Orthognathic Surgery. J. Cranio-Maxillofac. Surg. 2019, 47, 406–413. [Google Scholar] [CrossRef]
- Küçükçakır, O.; Ersan, N.; Arslan, Y.Z.; Cansız, E. Evaluation of Mandibular Condyle Position in Class III Patients after Bimaxillary Orthognathic Surgery: A Cone-Beam Computed Tomography Study. Korean J. Orthod. 2024, 54, 247–256. [Google Scholar] [CrossRef]
- Choi, B.-J.; Kim, B.-S.; Lim, J.-M.; Jung, J.; Lee, J.-W.; Ohe, J.-Y. Positional Change in Mandibular Condyle in Facial Asymmetric Patients after Orthognathic Surgery: Cone-Beam Computed Tomography Study. Maxillofac. Plast. Reconstr. Surg. 2018, 40, 13. [Google Scholar] [CrossRef]
- Shujaat, S.; Shaheen, E.; Politis, C.; Jacobs, R. Three-Dimensional Evaluation of Distal and Proximal Segment Skeletal Relapse Following Isolated Mandibular Advancement Surgery in 100 Consecutive Patients: A One-Year Follow-up Study. Int. J. Oral Maxillofac. Surg. 2022, 51, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Rizk, M.Z.; Torgersbråten, N.; Mohammed, H.; Franzen, T.J.; Vandevska-Radunovic, V. Stability of Single-Jaw vs Two-Jaw Surgery Following the Correction of Skeletal Class III Malocclusion: A Systematic Review and Meta-Analysis. Orthod. Craniofac. Res. 2021, 24, 314–327. [Google Scholar] [CrossRef]
- Fujioka, M.; Fujii, T.; Hirano, A. Comparative Study of Mandibular Stability after Sagittal Split Osteotomies: Biocortical versus Monocortical Osteosynthesis. Cleft Palate-Craniofacial J. Off. Publ. Am. Cleft Palate-Craniofacial Assoc. 2000, 37, 551–555. [Google Scholar] [CrossRef]
- Ellis, E.; Esmail, N. Malocclusions Resulting from Loss of Fixation after Sagittal Split Ramus Osteotomies. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2009, 67, 2528–2533. [Google Scholar] [CrossRef]




| Variables | Description |
|---|---|
| Reference planes | |
| Frankfort horizontal (FH) plane | Constructed by orbitale on the right side and porion on both sides. |
| Horizontal plane | Constructed by medial pole of right condyle and parallel to FH plane. |
| Frontal plane | Constructed by porion on both sides and perpendicular to horizontal plane. |
| Midsagittal plane | Constructed by nasion, basion, and ANS, and perpendicular to horizontal and frontal plane. |
| Landmarks and measurements | |
| Menton (Me) | The most inferior midpoint on the symphysis. |
| Me-Y | Measured the vertical change in menton along the y-axis. |
| Pogonion (Pog) | The most anterior midpoint on the symphysis. |
| Pog-Z | Measured the anteroposterior change in pogonion along the z-axis. |
| Vertical bony step (VBS) | The vertical distance between the proximal segment and distal segment along a line between the first and second molars and 95° to the molar occlusal plane which is constructed by the mesiobuccal cusp tip of the mandibular first molar and the distobuccal cusp tip of the mandibular second molar. |
| Center of rotation (CRot) | A specific point or axis around which the jaw or certain bony segments are rotating during surgical or orthodontic procedures. |
| Variables | T1–T0 | T2–T1 |
|---|---|---|
| Proximal segment (PS) | ||
| PS rotation (°) | 0.3 | 0.4 |
| Distal segment (DS) | ||
| DS rotation (°) | 0.5 | |
| VBS (mm) | 0.2 | 0.3 |
| Pog-Z (mm) | 0.2 | 0.1 |
| Me-Y (mm) | 0.1 | 0.1 |
| Movement Direction | Surgical Change | p Value | Postsurgical Change | p Value | Total Change | p Value | |
|---|---|---|---|---|---|---|---|
| T1–T0 | T2–T1 | T2–T0 | |||||
| Medial pole | Mediolateral (X) 1 | −0.8 ± 0.9 | <0.001 * | +0.4 ± 0.6 | 0.001 * | −0.4 ± 0.9 | 0.027 * |
| Superoinferior (Y) 2 | −0.5 ± 0.8 | 0.003 *,† | +0.2 ± 0.9 | 0.279 | −0.3 ± 1.0 | 0.067 | |
| Anterorposterior (Z) 3 | −0.9 ± 0.7 | <0.001 * | +0.3 ± 0.8 | 0.041 * | −0.6 ± 0.8 | <0.001 * | |
| Lateral pole | Mediolateral (X) 1 | −0.1 ± 0.7 | 0.582 | +0.3 ± 0.6 | 0.028 * | +0.2 ± 0.7 | 0.175 |
| Superoinferior (Y) 2 | −0.8 ± 0.6 | <0.001 * | +0.4 ± 0.8 | 0.013 * | −0.4 ± 0.7 | 0.004 * | |
| Anterorposterior (Z) 3 | +0.8 ± 0.9 | <0.001 * | −0.0 ± 1.1 | 0.941 | +0.8 ± 1.1 | <0.001 *,† |
| Variables | T1–T0 | p Value | T2–T1 | p Value | |
|---|---|---|---|---|---|
| Proximal Segment (PS) | PS rotation (°) | 2.1 ± 2.9 | <0.001 * | −2.4 ± 2.1 | <0.001 *,† |
| Distal Segment (DS) | DS rotation (°) | −2.0 ± 2.3 | <0.001 * | ||
| VBS (mm) | −6.2 ± 2.9 | <0.001 * | 4.4 ± 1.8 | <0.001 * | |
| Pog-Z (mm) | 13.6 ± 5.3 | <0.001 * | 4.0 ± 1.9 | <0.001 * | |
| Me-Y (mm) | −0.8 ± 1.9 | 0.015 *,† | 2.3 ± 1.2 | <0.001 * | |
| VBS (T1–T0) | ||
|---|---|---|
| Variables (T2–T1) | r (ρ) | p Value |
| Proximal segment | ||
| PS rotation (°) | 0.024 | 0.897 † |
| Distal segment | ||
| DS rotation (°) | 0.243 | 0.181 |
| Crot-Y | −0.465 | 0.010 * |
| Crot-Z | 0.433 | 0.017 * |
| Pog-Z (mm) | −0.623 | 0.000 * |
| Me-Y (mm) | −0.389 | 0.034 * |
| Type of Surgery | |||||
|---|---|---|---|---|---|
| 1-Jaw Surgery | 2-Jaw Surgery | ||||
| Variables (T2–T1) | Mean | SD | Mean | SD | p Value |
| PS rotation (°) | −2.59 | 1.84 | −2.31 | 2.52 | 0.731 |
| DS rotation (°) | −2.15 | 2.10 | −1.92 | 2.61 | 0.792 |
| Pog-Z (mm) | 4.23 | 1.56 | 3.69 | 2.20 | 0.445 |
| Me-Y (mm) | 2.31 | 0.78 | 2.20 | 1.52 | 0.799 |
| VBS (mm) | 4.41 | 1.54 | 4.31 | 2.19 | 0.886 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, J.-D.; Lim, S.-H.; Park, J.H. Differential Relapse of Proximal and Distal Segments after Mandibular Setback Surgery. Appl. Sci. 2024, 14, 9299. https://doi.org/10.3390/app14209299
Kim J-D, Lim S-H, Park JH. Differential Relapse of Proximal and Distal Segments after Mandibular Setback Surgery. Applied Sciences. 2024; 14(20):9299. https://doi.org/10.3390/app14209299
Chicago/Turabian StyleKim, Jin-Deok, Sung-Hoon Lim, and Jae Hyun Park. 2024. "Differential Relapse of Proximal and Distal Segments after Mandibular Setback Surgery" Applied Sciences 14, no. 20: 9299. https://doi.org/10.3390/app14209299
APA StyleKim, J.-D., Lim, S.-H., & Park, J. H. (2024). Differential Relapse of Proximal and Distal Segments after Mandibular Setback Surgery. Applied Sciences, 14(20), 9299. https://doi.org/10.3390/app14209299






