The Functional Resonance Analysis Method (FRAM) Application in the Healthcare Sector: Lessons Learned from Two Case Studies on Medical Device Management
Abstract
Featured Application
Abstract
1. Introduction
2. Materials and Methods
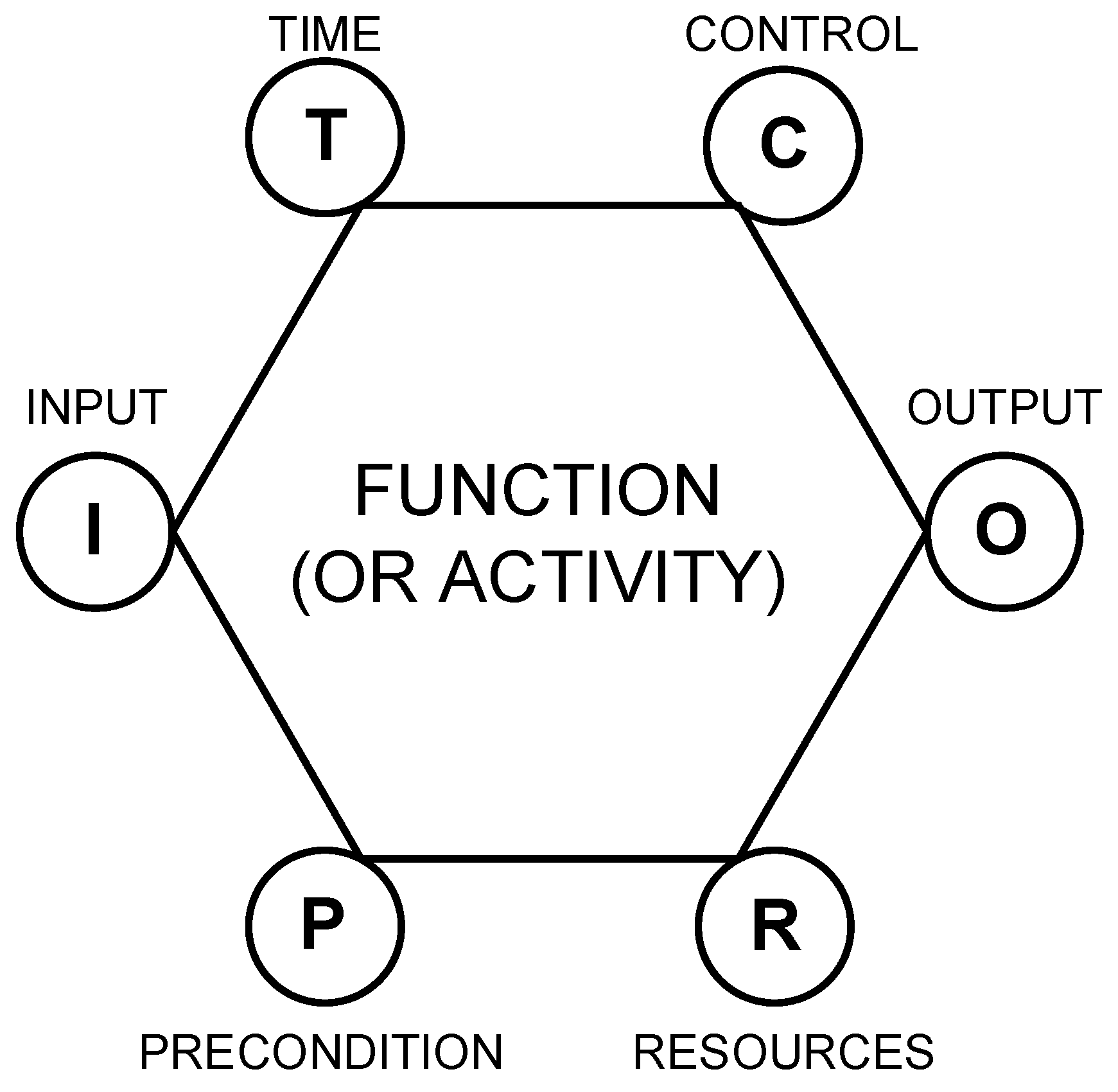
2.1. Functional Resonance Analysis Method (FRAM) Main Features
2.2. Study Features
3. Case Study 1
3.1. Case Study Context and Goal of the Analysis
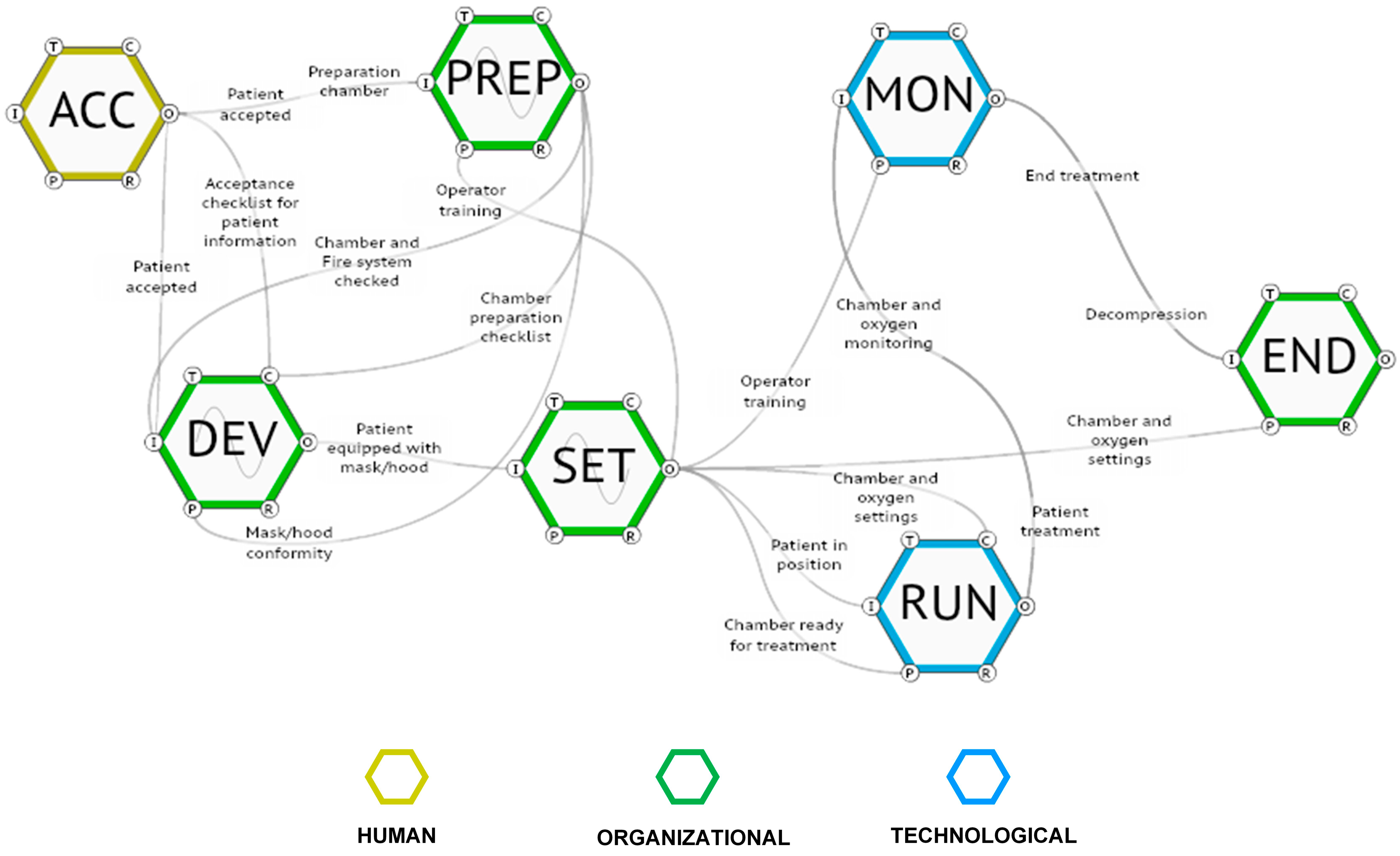
3.2. Identification and Definition of the Functions
- ACC. Patient acceptance: the function that activates the entire process is related to the patient’s suitability for the oxygen therapy treatment. Hospital staff has to verify the patient’s anamnesis and the request for the treatment issued by a specialist. In this phase, the patient should be informed about the risks related to the treatment, the prohibition of introducing flammable objects into the room, etc. The output of this organizational function is represented by the patient’s suitability for the oxygen treatment.
- PREP. Chamber preparation: the hospital staff has to check the correct functioning of the HBOT room, including its safety systems, such as the fire extinguishing devices, as well as the masks/hoods to be used by the patients during the treatment. At the same time, the intervention threshold of the oxygen analyzer has to be set.
- DEV. Provide devices: the hospital staff provides patients with a hood or a mask depending on the type of therapy and verifies they are worn correctly.
- SET. Chamber closing and oxygen settings: once patients are equipped with the mask/hood and are in the correct position inside the chamber, the door is closed, and the HBOT room is set for the treatment.
- RUN. Running treatment: the treatment is performed.
- MON. Monitoring: during the treatment, the hospital staff has to monitor the correct functioning of the system and the proper percentage of oxygen administered. This control is carried out both outside the HBOT room through a control panel and inside the room (usually by a nurse who assists patients).
- END. End treatment: when the treatment time is completed, the staff starts the decompression phase that is concluded with the opening of the chamber door.
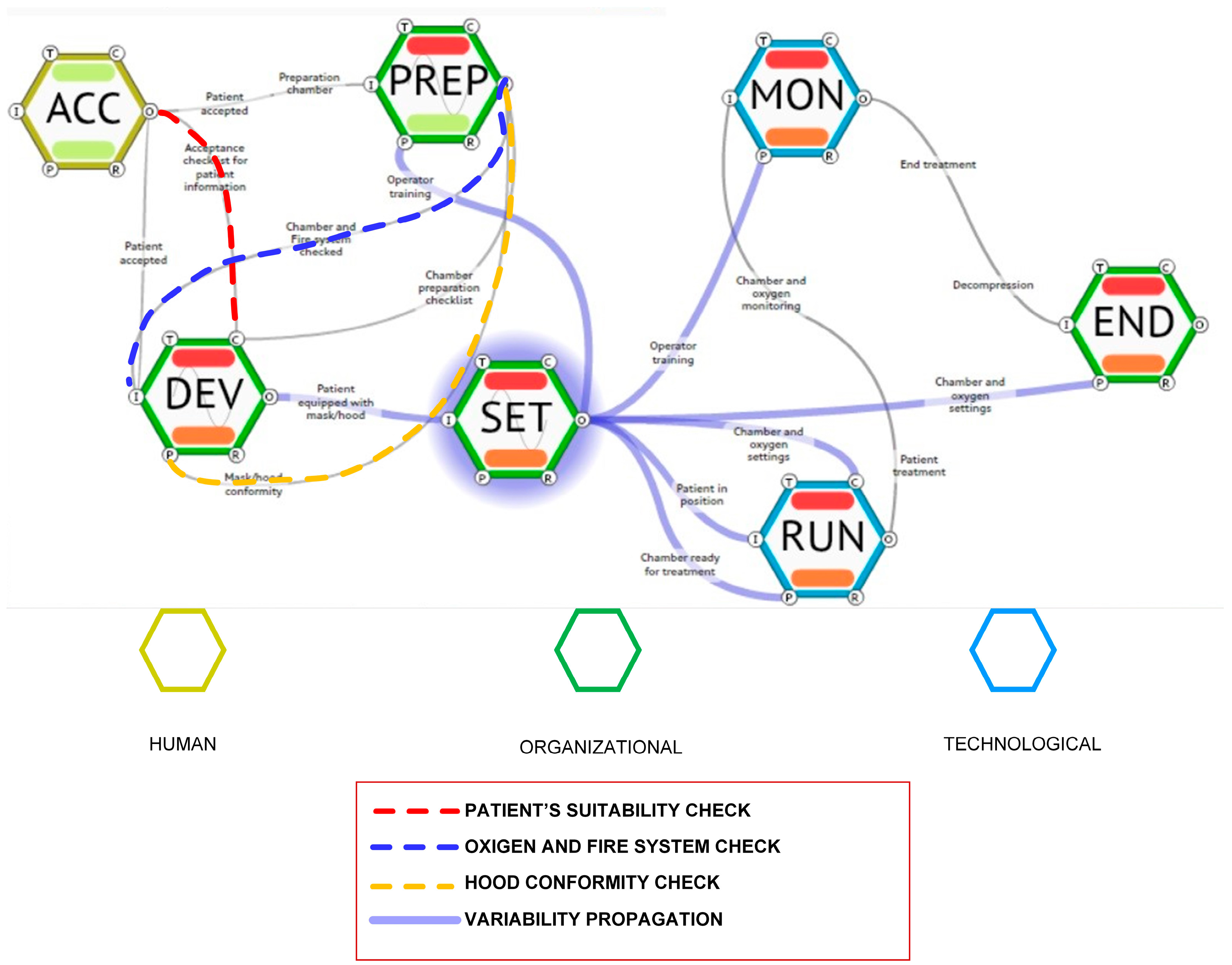
3.3. Definition of the Variability
3.4. Variability Aggregation
- The inaccurate acceptance of the patients, which as a result allowed one of them to bring a gas hand warmer inside the chamber (Function ACC).
- The inaccurate chamber preparation, when the hospital staff missed the fire extinguishing system check (Function PREP).
- The lack of conformity of hoods: tampering with the hoods by the hospital staff caused an increase in the percentage of oxygen in the chamber, and the wrong setting of the oxygen analyzer did not allow the alarm system to detect the too-high percentage of oxygen (Function DEV).
3.5. Results
4. Case Study 2
4.1. Case Study Context and Goal of the Analysis
- Projectile effect: Magnetic fields can attract objects toward the magnet, posing dangers to both patients and operators. The static magnetic field is conventionally categorized into two zones: Zone 1 (close to the magnet’s center) and Zone 2 (surrounding the magnet with decreasing magnetic intensity). Ferromagnetic objects in the former area are subject to torsion, and if the object is inside the patient’s body, it can potentially cause tissue damage. In the latter, ferromagnetic objects are also subject to a translational force, leading to the “projectile effect,” where these objects can be rapidly drawn into the magnet, potentially leading to injury or damaging the magnet. Several accidents are reported, which have involved the presence in the room of oxygen and helium cylinders, cleaning trolleys, metal chairs, scissors, etc. [68].
- Twisting: this effect is due to the deflection or torsion of magnetic objects, such as vascular clips and cochlear implants, that can lead to incorrect implant functioning or cause damage to patients.
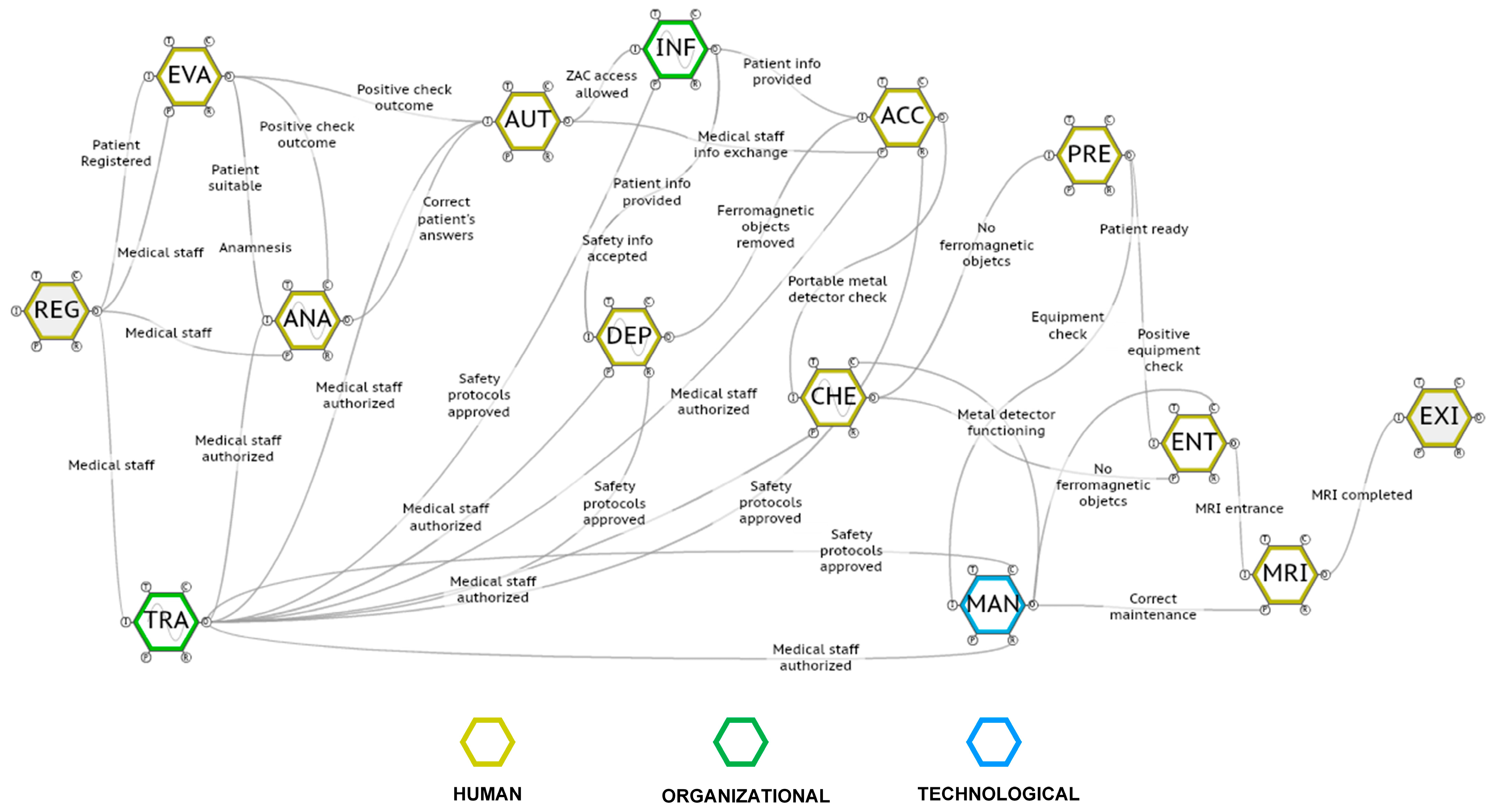
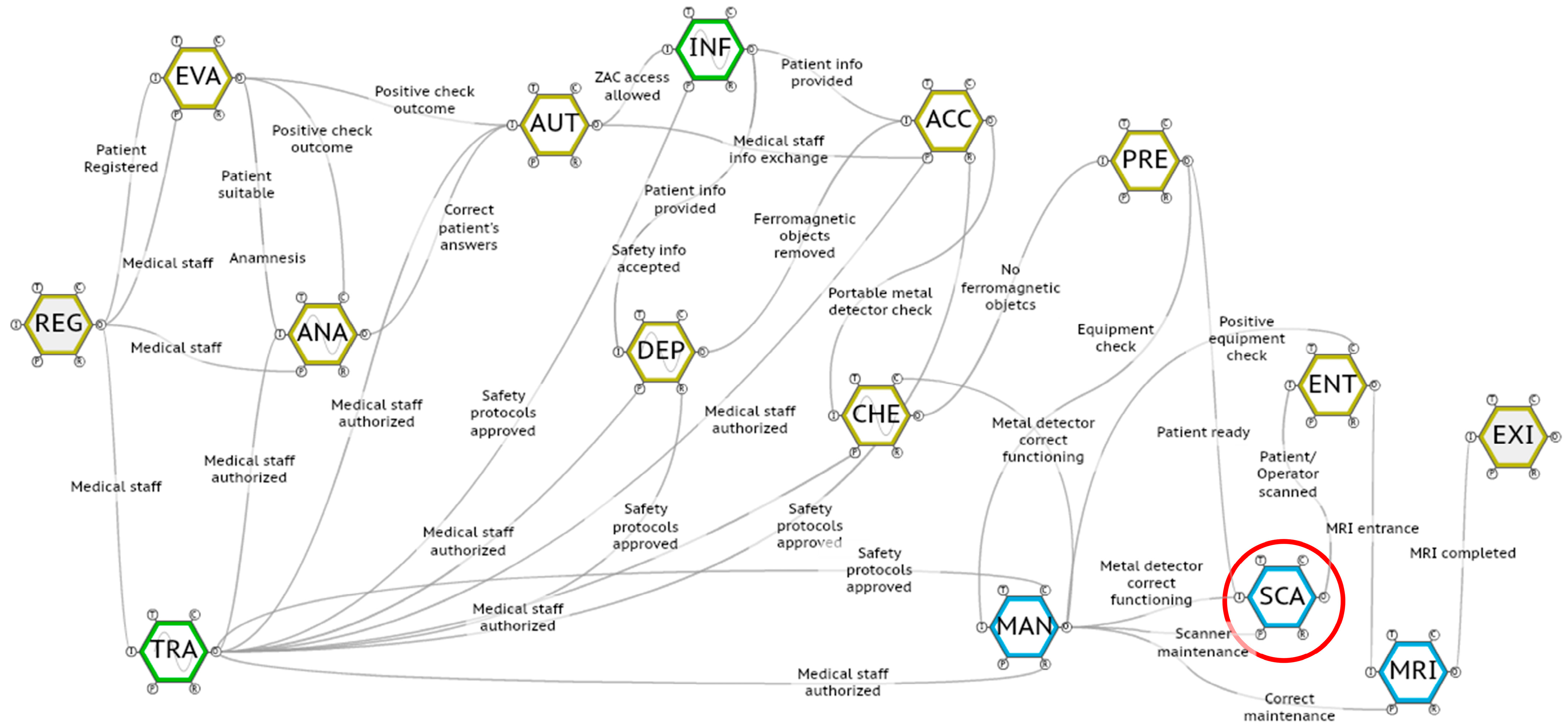
4.2. Identification and Definition of the Functions
- REG. To register the patient for an MRI examination (this activity is carried out outside the MRI room).
- EVA. To evaluate the MRI examination request issued by the medical staff: in more detail, the MRI staff, after having assessed the appropriateness of the diagnostic investigation, must identify any contraindications to carrying out the examination (e.g., the presence of ferromagnetic prostheses, implantable medical devices, etc.). In this phase, it is essential to make an initial distinction between patients who are able to provide adequate information for the safe execution of the MRI examination or not.
- ANA. To perform the patient anamnesis: in order to identify any contraindications to carrying out the diagnostic test or to the entry of occasional workers into the MRI room, the interested parties must be subjected to an anamnesis by filling in an anamnestic questionnaire. If the information provided by the patient/caregiver is not considered sufficient, or if a patient is unconscious, the MRI staff may request further investigations (e.g., X-rays to verify the presence of ferromagnetic objects inside the patient’s body or specialist visits in the case of the presence of medical devices such as pacemakers).
- AUT. To issue the authorization for performing an MRI examination: once all necessary information is gathered and evaluated, MRI staff releases the authorization to carry out the MRI examination.
- INF. To provide information for entry to the MRI room: both patients and workers who are allowed access to the Controlled Access Zone (ZAC) are provided with specific information concerning the MRI-related risks and safety procedures.
- DEP. To deposit all ferromagnetic objects: before entering the ZAC, both patients and workers are asked to leave all hazardous objects out of the ZAC.
- ACC. To access the ZAC: once the permission to enter the ZAC is given, both patients and workers are authorized to enter the ZAC.
- CHE. To perform the metal detector check: in the ZAC, both patients and workers are scanned with a portable metal detector to verify that there are no ferromagnetic objects.
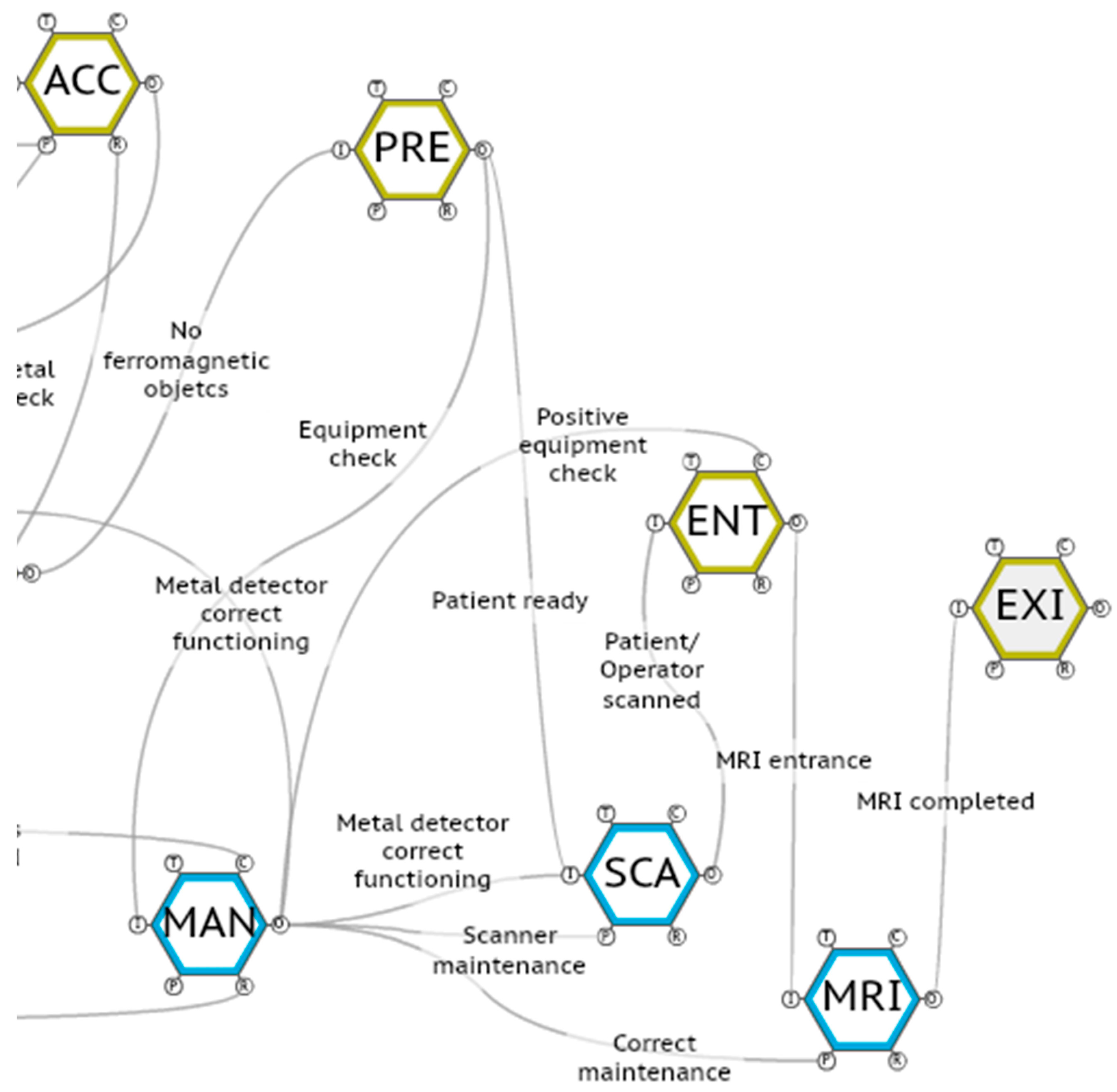
- PRE. To prepare the patient for the examination: the patient is prepared to undergo the MRI examination (e.g., the contrast liquid is administered).
- ENT. To enter the MRI room.
- MRI. To perform the MRI examination.
- EXI. To exit the MRI room.
- 13.
- TRA. To train authorized healthcare personnel.
- 14.
- MAN. To verify the correct maintenance of the MRI device.
4.3. Definition of the Variability and Aggregation
- Untrained/unauthorized hospital personnel enter the MRI room for different tasks, such as picking documents and avoiding the metal detector check;
- When an emergency occurs, the patient is rapidly brought to the MRI room without passing the previous check phases.
4.4. Identification of Possible Solutions
4.5. Results
- REG. To register the patient for an MRI examination;
- EVA. To evaluate the MRI examination request issued by the medical staff.
- ANA. To perform the patient anamnesis.
- AUT. To issue the authorization for performing an MRI examination;
- INF. To provide information for entry to the MRI room;
- DEP. To deposit all ferromagnetic objects;
- ACC. To access the ZAC;
- CHE. To perform the metal detector check;
- PRE. To prepare the patient for the examination
- SCA. To pass the ferromagnetic scan before entering the MRI room;
- ENT. To enter the MRI room;
- MRI. To perform the MRI examination;
- EXI. To exit the MRI room;
- TRA. To train authorized healthcare personnel;
- MAN. To verify the correct maintenance of the MRI device.
5. Discussion
5.1. Research Implications
5.2. Research Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Plsek, E.P.; Greenhalgh, T. Complexity science: The challenge of complexity in health care. BMJ 2001, 323, 625–628. [Google Scholar] [CrossRef]
- Sujan, M.; Lounsbury, O.; Pickup, L.; Kaya, G.K.; Earl, L.; McCulloch, P. What kinds of insights do Safety-I and Safety-II approaches provide? A critical reflection on the use of SHERPA and FRAM in healthcare. Saf. Sci. 2024, 173, 106450. [Google Scholar] [CrossRef]
- Weaver, S.; Stewart, K.; Kay, L. Systems-Based investigation of patient safety incidents. Future Healthc. J. 2021, 8, e593–e597. [Google Scholar] [CrossRef]
- McNab, D.; McKay, J.; Shorrock, S.; Luty, S.; Bowie, P. Development and application of ‘systems thinking’ principles for quality improvement. BMJ Open Qual. 2020, 9, e000714. [Google Scholar] [CrossRef]
- Sezdi, M. Medical Technology Management and Patient Safety. In A Roadmap of Biomedical Engineers and Milestones; Kara, S., Ed.; InTech: Rijeka, Croatia, 2012; pp. 183–208. [Google Scholar]
- Mitchell, R.J.; Williamson, A.; Molesworth, B. Use of a human factors classification framework to identify causal factors for medication and medical device-related adverse clinical incidents. Saf. Sci. 2015, 79, 163–174. [Google Scholar] [CrossRef]
- Li, J.; Mao, Y.; Zhang, J. Maintenance and quality control of medical equipment based on information fusion technology. Comput. Intell. Neurosci. 2022, 1, 9333328. [Google Scholar] [CrossRef]
- European Union, Regulation (EU) 2017/745 of the European Parliament and of the Council of 5 April 2017 on Medical Devices, Amending Directive 2001/83/EC, Regulation (EC) No 178/2002 and Regulation (EC) No 1223/2009 and Repealing Council Directives 90/385/EEC and 93/42/EEC. Available online: https://eur-lex.europa.eu/legal-content/EN/TXT/HTML/?uri=CELEX:32017R0745 (accessed on 26 June 2024).
- Khider, M.O.; Hamza, A.O. Medical equipment maintenance management system: Review and analysis. J. Clin. Eng. 2022, 47, 151–159. [Google Scholar] [CrossRef]
- Ellis, A.L.; Churruca, K.; Clay-Williams, R.; Pomare, C.; Austin, E.; Long, J.C.; Grødahl, A.; Braithwaite, J. Patterns of resilience: A scoping review and bibliometric analysis of resilient health care. Saf. Sci. 2019, 118, 241–257. [Google Scholar] [CrossRef]
- McNab, D.; Bowie, P.; Morrison, J.; Ross, A. Understanding patient safety performance and educational needs using the ‘Safety-II’ approach for complex systems. Educ. Prim. Care 2016, 27, 443–450. [Google Scholar] [CrossRef]
- Agostini, L.; Onofrio, R.; Piccolo, C.; Stefanini, A. A Management Perspective on Resilience in Healthcare: A Framework and Avenues for Future Research. BMC Health Serv. Res. 2023, 23, 774. [Google Scholar] [CrossRef]
- Verhagen, M.J.; de Vos, M.S.; Sujan, M.; Hamming, J.F. The problem with making Safety-II work in healthcare. BMJ Qual. Saf. 2022, 31, 402–408. [Google Scholar] [CrossRef]
- Smith, A.F.; Plunkett, E. People, systems and safety: Resilience and excellence in healthcare practice. Anaesthesia 2019, 74, 508–517. [Google Scholar] [CrossRef]
- Barros-Martins, J.; Carim, G.; Saurin, T.A.; Costella, M.F. Integrating Safety-I and Safety-II: Learning from failure and success in construction sites. Saf. Sci. 2022, 148, 105672. [Google Scholar] [CrossRef]
- Raben, D.C.; Bogh, S.B.; Viskum, B.; Mikkelsen, K.L.; Hollnagel, E. Proposing Leading Indicators for Blood Sampling: Application of a Method Based on the Principles of Resilient Healthcare. Cogn. Technol. Work. 2017, 19, 809–817. [Google Scholar] [CrossRef]
- Wears, R.L.; Hollnagel, E.; Braithwaite, J. Resilient Health Care, Volume 2: The Resilience of Everyday Clinical Work; Ashgate Publishing, Ltd.: Hampshire, UK, 2015. [Google Scholar]
- Saurin, T.A.; Rosso, C.B.; Da Costa, D.G.; Pasin, S.S. Where process improvement meets resilience: A study of the preparation and administration of drugs in a surgical inpatient unit. In Delivering Resilient Health Care; Hollnagel, E., Braithwaite, J., Wears, R., Eds.; Routledge: London, UK, 2019; pp. 174–185. [Google Scholar] [CrossRef]
- Costella, M.F.; Abreu Saurin, T.; Buarque de Macedo Guimarães, L. A method for assessing health and safety management systems from the resilience engineering perspective. Saf. Sci. 2009, 47, 1056–1067. [Google Scholar] [CrossRef]
- Machen, S. Thematic reviews of patient safety incidents as a tool for systems thinking: A quality improvement report. BMJ Open Qual. 2023, 12, e002020. [Google Scholar] [CrossRef]
- Lombardi, M.; Fargnoli, M.; Parise, G. Risk Profiling from the European Statistics on Accidents at Work (ESAW) Accidents′ Databases: A Case Study in Construction Sites. Int. J. Environ. Res. Public Health 2019, 16, 4748. [Google Scholar] [CrossRef]
- Nakhal Akel, A.J.; Di Gravio, G.; Fedele, L.; Patriarca, R. Learning from Incidents in Socio-Technical Systems: A Systems-Theoretic Analysis in the Railway Sector. Infrastructures 2022, 7, 90. [Google Scholar] [CrossRef]
- Amoore, J.N. A structured approach for investigating the causes of medical device adverse events. J. Med. Eng. 2014, 2014, 314138. [Google Scholar] [CrossRef]
- Nakhal Akel, A.J.; Patriarca, R.; Tronci, M.; Agnello, P.; Ansaldi, S.M.; Ledda, A. A STAMP model for safety analysis in industrial plants. Chem. Eng. Trans. 2022, 91, 403–408. [Google Scholar] [CrossRef]
- McNab, D.; Freestone, J.; Black, C.; Carson-Stevens, A.; Bowie, P. Participatory Design of an Improvement Intervention for the Primary Care Management of Possible Sepsis Using the Functional Resonance Analysis Method. BMC Med. 2018, 16, 174. [Google Scholar] [CrossRef]
- Arcuri, R.; Bulhões, B.; Jatobá, A.; Bellas, H.C.; Koster, I.; d’Avila, A.L.; Vidal, M.C.R.; Burns, C.M.; de Carvalho, P.V.R. Gatekeeper family doctors operating a decentralized referral prioritization system: Uncovering improvements in system resilience through a grounded-based approach. Saf. Sci. 2020, 121, 177–190. [Google Scholar] [CrossRef]
- Hollnagel, E. Looking for patterns in everyday clinical work. In Resilient Health Care, Volume 2: The Resilience of Everyday Clinical Work; Wears, R.L., Hollnagel, E., Braithwaite, J., Eds.; CRC Press: London, UK, 2015; pp. 145–161. [Google Scholar] [CrossRef]
- Hollnagel, E. FRAM: The Functional Resonance Analysis Method: Modelling Complex Socio-Technical Systems; CRC Press: London, UK, 2012. [Google Scholar]
- Fargnoli, M.; Murgianu, L. A Resilience Engineering Approach for the Risk Assessment of IT Services. Appl. Sci. 2023, 13, 11132. [Google Scholar] [CrossRef]
- Delikhoon, M.; Zarei, E.; Banda, O.V.; Faridan, M.; Habibi, E. Systems Thinking Accident Analysis Models: A Systematic Review for Sustainable Safety Management. Sustainability 2022, 14, 5869. [Google Scholar] [CrossRef]
- Patriarca, R.; Di Gravio, G.; Woltjer, R.; Costantino, F.; Praetorius, G.; Ferreira, P.; Hollnagel, E. Framing the FRAM: A literature review on the functional resonance analysis method. Saf. Sci. 2020, 129, 104827. [Google Scholar] [CrossRef]
- Salehi, V.; Veitch, B.; Smith, D. Modeling complex socio-technical systems using the FRAM: A literature review. Hum. Factors Ergon. Manuf. Serv. Ind. 2021, 31, 118–142. [Google Scholar] [CrossRef]
- Buikstra, E.; Strivens, E.; Clay-Williams, R. Understanding variability in discharge planning processes for the older person. Saf. Sci. 2020, 121, 137–146. [Google Scholar] [CrossRef]
- Damen, N.L.; de Vos, M.S.; Moesker, M.J.; Braithwaite, J.; de Lind van Wijngaarden, R.A.F.; Kaplan, J.; Hamming, J.F.; Clay-Williams, R. Preoperative anticoagulation management in everyday clinical practice: An International comparative analysis of work-as-done using the functional resonance analysis method. J. Patient Saf. 2018, 17, 157–165. [Google Scholar] [CrossRef]
- Hogerwaard, M.; Stolk, M.; Dijk, L.V.; Faasse, M.; Kalden, N.; Hoeks, S.E.; Bal, R.; Horst, M.T. Implementation of Barcode Medication Administration (BMCA) Technology on Infusion Pumps in the Operating Rooms. BMJ Open Qual. 2023, 12, e002023. [Google Scholar] [CrossRef]
- van Stralen, S.A.; van Eikenhorst, L.; Vonk, A.S.; Schutijser, B.C.; Wagner, C. Evaluating deviations and considerations in daily practice when double-checking high-risk medication administration: A qualitative study using the FRAM. Heliyon 2024, 10, e25637. [Google Scholar] [CrossRef]
- Hedqvist, A.T.; Praetorius, G.; Ekstedt, M.; Lindberg, C. Entangled in complexity: An ethnographic study of organizational adaptability and safe care transitions for patients with complex care needs. J. Adv. Nurs. 2024, 1–18. [Google Scholar] [CrossRef]
- Ransolin, N.; Wachs, P.; Bueno, W.P. A functional perspective for Intensive Care Unit modelling. Production 2023, 33, e20220081. [Google Scholar] [CrossRef]
- Gustafson, O.; Vollam, S.; Morgan, L.; Watkinson, P. A human factors analysis of missed mobilisation after discharge from intensive care: A competition for care? Physiotherapy 2021, 113, 131–137. [Google Scholar] [CrossRef]
- Oduyale, M.S.; Patel, N.; Borthwick, M.; Claus, S. Coadministration of multiple intravenous medicines: Intensive care nurses’ views and perspectives. Nurs. Crit. Care 2020, 25, 156–164. [Google Scholar] [CrossRef]
- Raben, D.C.; Viskum, B.; Mikkelsen, K.L.; Hounsgaard, J.; Bogh, S.B.; Hollnagel, E. Application of a non-linear model to understand healthcare processes: Using the functional resonance analysis method on a case study of the early detection of sepsis. Reliab. Eng. Syst. Saf. 2018, 177, 1–11. [Google Scholar] [CrossRef]
- Meeuwis, C.J.; Steinmetz, V.; Hamming, J.F.; Dekker, S.W.A. A FRAM Requirements Analysis for Safety Differently Investigations. Saf. Sci. 2020, 125, 104653. [Google Scholar] [CrossRef]
- Damoiseaux-Volman, B.A.; Medlock, S.; van der Eijk, M.D.; Romijn, J.A.; Abu-Hanna, A.; van der Velde, N. Falls and delirium in older inpatients: Work-as-imagined, work-as-done and preferences for clinical decision support systems. Saf. Sci. 2021, 142, 105355. [Google Scholar] [CrossRef]
- Pickup, L.; Atkinson, S.; Hollnagel, E.; Bowie, P.; Gray, S.; Rawlinson, S.; Forrester, K. Blood Sampling-Two Sides to the Story. Appl. Ergon. 2017, 59, 234–242. [Google Scholar] [CrossRef]
- Goldman, J.; Rafie, K.; Thomas, T.; Chartan, C.; Marshall, P.; Fontenot, T.; Williams, E. Use of functional resonance analysis (FRAM) as a non-biased incident analysis method in a PICU. Crit. Care Med. 2015, 43, 330. [Google Scholar] [CrossRef]
- Alm, H.; Woltjer, R. Patient Safety Investigation through the Lens of FRAM. In Human Factors: A System View of Human, Technology and Organization; Shaker Publishing: Maastricht, The Netherlands, 2010; pp. 153–165. [Google Scholar]
- Salihoglu, E.; Beşikçi, E.B. The use of Functional Resonance Analysis Method (FRAM) in a maritime accident: A case study of Prestige. Ocean Eng. 2020, 219, 108223. [Google Scholar] [CrossRef]
- Adriaensen, A.; Patriarca, R.; Smoker, A.; Bergstrom, J. A socio-technical analysis of functional properties in a joint cognitive system: A case study in an aircraft cockpit. Ergonomics 2019, 62, 1598–1616. [Google Scholar] [CrossRef]
- Adhita, I.; Furusho, M. Ship-to-Ship collision analyses based on functional resonance analysis method. J. ETA Marit. Sci. 2021, 9, 102–109. [Google Scholar] [CrossRef]
- De Carvalho, P.V.R. The use of Functional Resonance Analysis Method (FRAM) in a mid-air collision to understand some characteristics of the air traffic management system resilience. Reliab. Eng. Sys. Saf. 2011, 96, 1482–1498. [Google Scholar] [CrossRef]
- França, J.E.M.; Vaz, M.I.; Coutinho, B.R.; Pina, L. Analyzing organizational gaps in process accidents with FRAM: The case of the Imperial Sugar refinery explosion (2008). Process Saf. Prog. 2023, 42, S87–S96. [Google Scholar] [CrossRef]
- França, J.E.; Hollnagel, E.; dos Santos, I.J.L.; Haddad, A.N. Analysing human factors and non-technical skills in offshore drilling operations using FRAM (functional resonance analysis method). Cogn. Technol. Work 2021, 23, 553–566. [Google Scholar] [CrossRef]
- Samaras, E.A.; Samaras, G.M. Confronting systemic challenges in interoperable medical device safety, security & usability. J. Biomed. Inform. 2016, 63, 226–234. [Google Scholar] [CrossRef]
- The Irish Times, 10 Patients and Nurse Die Within Seconds in Hospital Fire. Available online: https://www.irishtimes.com/news/10-patients-and-nurse-die-within-seconds-in-hospital-fire-1.121775 (accessed on 26 June 2024).
- Van Dijk, L.M.; Meulman, M.D.; Van Eikenhorst, L.; Merten, H.; Schutijser, B.C.F.M.; Wagner, C. Can using the functional resonance analysis method, as an intervention, improve patient safety in hospitals?: A stepped wedge design protocol. BMC Health Serv. Res. 2021, 21, 1228. [Google Scholar] [CrossRef]
- Alvim, H.; Diogo, M.T.; Leão, R.P.; Camacho, O.; Baptista, J.; Nobrega, J. Fire drills in Hyperbaric Medicine. In Proceedings of the 9th International Conference on Occupational Risk Prevention, Santiago de Chile, Chile, 9–11 November 2021; Universitat Politècnica de Catalunya: Santiago de Chile, Chile, 2011. [Google Scholar]
- Hollnagel, E.; Goteman, Ö. The Functional Resonance Accident Model; University of Linköping SE-58183: Linköping, Sweden, 2004. [Google Scholar]
- Simini, B. Milan Fire fuels concerns over hyperbaric oxygen facilities. Lancet 1997, 350, 1375. [Google Scholar] [CrossRef]
- Kot, J.; Desola, J.; Lind, F.; Mueller, P.; Jansen, E.; Burman, F. A European code of good practice for hyperbaric oxygen therapy—Review 2022. Diving Hyperb. Med. 2023, 53 (Suppl. 4), 1–17. [Google Scholar] [CrossRef]
- Sheffield, P.; Desautels, D.A. Hyperbaric and hypobaric chamber fires: A 73-year analysis. Undersea Hyperb. Med. 1997, 24, 153–164. [Google Scholar]
- Kot, J.; Houman, R.; Gough-Allen, R. Safety in Hyperbaric Medicine. In Handbook on Hyperbaric Medicine; Mathieu, D., Ed.; Springer: Dordrecht, The Netherlands, 2006; pp. 691–711. [Google Scholar] [CrossRef]
- Jain, K.K. Hyperbaric Chambers: Equipment, Technique, and Safety. In Textbook of Hyperbaric Medicine, 6th ed.; Springer: Cham, Switzerland, 2017; pp. 61–78. [Google Scholar] [CrossRef]
- Mortensen, C. Hyperbaric oxygen therapy. Curr. Anaesth. Crit. Care 2008, 19, 333–337. [Google Scholar] [CrossRef]
- Mathieu, D.; Ratzenhofer-Komenda, B.; Kot, J. Hyperbaric oxygen therapy for intensive care patients: Position statement by the European Committee for Hyperbaric Medicine. Diving Hyperb. Med. 2015, 45, 42–46. [Google Scholar]
- Rees Hill, FRAM Model Visualiser (FMV). Available online: https://functionalresonance.com/the%20fram%20model%20visualiser/ (accessed on 29 June 2024).
- Carr, M.W.; Grey, M.L. Magnetic Resonance Imaging: Overview, risks, and safety measures. Am. J. Nurs. 2002, 102, 26–33. [Google Scholar] [CrossRef]
- Stecco, A.; Saponaro, A.; Carriero, A. Patient safety issues in magnetic resonance imaging: State of the art. La Radiol. Medica 2007, 112, 491–508. [Google Scholar] [CrossRef]
- Mansouri, M.; Aran, S.; Harvey, H.B.; Shaqdan, K.W.; Abujudeh, H.H. Rates of safety incident reporting in MRI in a large academic medical center. J. Magn. Reson. Imaging 2016, 43, 998–1007. [Google Scholar] [CrossRef]
- Sammet, S. Magnetic resonance safety. Abdom. Radiol. 2016, 41, 444–451. [Google Scholar] [CrossRef]
- Hartwig, V.; Virgili, G.; Mattei, F.; Biagini, C.; Romeo, S.; Zeni, O.; Scarfì, M.R.; Massa, R.; Campanella, F.; Landini, L.; et al. Occupational exposure to electromagnetic fields in magnetic resonance environment: An update on regulation, exposure assessment techniques, health risk evaluation, and surveillance. Med. Biol. Eng. Comput. 2022, 60, 297–320. [Google Scholar] [CrossRef]
- Hoy, K.M.; Fallon, E.; Kelly, M. Paediatric Homecare Risk Management: An Application of Functional Resonance Analysis Method (FRAM). Safety 2023, 9, 52. [Google Scholar] [CrossRef]
- Grant, E.; Salmon, P.M.; Stevens, N.J.; Goode, N.; Read, G.J. Back to the future: What do accident causation models tell us about accident prediction? Saf. Sci. 2018, 104, 99–109. [Google Scholar] [CrossRef]
- Nakhal Akel, A.J.; Patriarca, R.; De Carlo, F.; Leoni, L. A System-Theoretic Fuzzy Analysis (STheFA) for systemic safety assessment. Process Saf. Environ. Prot. 2023, 177, 1181–1196. [Google Scholar] [CrossRef]
- Bueno, W.P.; Wachs, P.; Saurin, T.A.; Ransolin, N.; Souza Kuchenbecker, R. Making resilience explicit in FRAM: Shedding light on desired outcomes. Hum. Factors Ergon. Manuf. Serv. Ind. 2021, 31, 579–597. [Google Scholar] [CrossRef]
- CEN, EN 16081:2011+A1:2013. Hyperbaric Chambers—Specific Requirements for Fire Extinguishing Systems—Performance, Installation and Testing. Available online: https://standards.cencenelec.eu/dyn/www/f?p=CEN:110:0::::FSP_PROJECT,FSP_ORG_ID:40720,622704&cs=10C7DD7C4BE3D92A3428A86F5260BDDF6 (accessed on 26 June 2024).
- CEN, EN 14931:2006. Pressure Vessels for Human Occupancy (PVHO)—Multi-Place Pressure Chamber Systems for Hyperbaric Therapy—Performance, Safety Requirements and Testing. Available online: https://standards.cencenelec.eu/dyn/www/f?p=205:110:0::::FSP_PROJECT:20999&cs=173518D05560B6CC40B44D00505852F82 (accessed on 26 June 2024).
- Meulman, M.D.; Merten, H.; van Munster, B.; Wagner, C. Comparing Guidelines to Daily Practice When Screening Older Patients for the Risk of Functional Decline in Hospitals: Outcomes of a Functional Resonance Analysis Method (FRAM) Study. J. Patient Saf. 2023, 20, 461–473. [Google Scholar] [CrossRef]
- Werle, N.B.; Saurin, T.A.; Soliman, M. Collaborative Use of Slack Resource as a Support to Resilience: Study of a Maternity Ward; Working Across Boundaries: Resilient Health Care; Braithwaite, J., Hollnagel, E., Hunte, G., Eds.; CRC Press: Boca Raton, FL, USA, 2019; Volume 5, pp. 137–153. [Google Scholar] [CrossRef]
- Guo, Y.; Hu, S.; Jin, Y.; Xi, Y.; Li, W. A Hybrid Probabilistic Risk Analytical Approach to Ship Pilotage Risk Resonance with FRAM. J. Mar. Sci. Eng. 2023, 11, 1705. [Google Scholar] [CrossRef]
- O’Hara, J.K.; Baxter, R.; Hardicre, N. ‘Handing over to the patient’: A FRAM analysis of transitional care combining multiple stakeholder perspectives. Appl. Ergon. 2020, 85, 103060. [Google Scholar] [CrossRef]
- Falegnami, A.; Costantino, F.; Di Gravio, G.; Patriarca, R. Unveil key functions in socio-technical systems: Mapping FRAM into a multilayer network. Cogn. Technol. Work 2020, 22, 877–899. [Google Scholar] [CrossRef]
- Jiang, Z.; Zhao, T.; Wang, S.; Ren, F. A Novel Risk Assessment and Analysis Method for Correlation in a Complex System Based on Multi-Dimensional Theory. Appl. Sci. 2020, 10, 3007. [Google Scholar] [CrossRef]
- Ouyang, W.; Gan, X.; Wu, Y.; Qu, K.; Wang, J. Human Factors Analysis of the Improved FRAM Method for Take-Off Quality Lateral Shift. Appl. Sci. 2023, 13, 5216. [Google Scholar] [CrossRef]
- Hulme, A.; Stanton, N.A.; Walker, G.H.; Waterson, P.; Salmon, P.M. What do applications of systems thinking accident analysis methods tell us about accident causation? A systematic review of applications between 1990 and 2018. Saf. Sci. 2019, 117, 164–183. [Google Scholar] [CrossRef]
- Patriarca, R.; Del Pinto, G.; Di Gravio, G.; Costantino, F. FRAM for Systemic Accident Analysis: A Matrix Representation of Functional Resonance. Int. J. Reliab. Qual. Saf. Eng. 2018, 25, 1850001. [Google Scholar] [CrossRef]
- Patriarca, R.; Di Gravio, G.; Costantino, F. A Monte Carlo evolution of the Functional Resonance Analysis Method (FRAM) to assess performance variability in complex systems. Saf. Sci. 2017, 91, 49–60. [Google Scholar] [CrossRef]
- Kaya, G.K.; Ozturk, F.; Sariguzel, E.E. System-based risk analysis in a tram operating system: Integrating Monte Carlo simulation with the functional resonance analysis method. Reliab. Eng. Syst. Saf. 2021, 215, 107835. [Google Scholar] [CrossRef]
- Fu, S.; Yu, Y.; Chen, J.; Han, B.; Wu, Z. Towards a probabilistic approach for risk analysis of nuclear-powered icebreakers using FMEA and FRAM. Ocean Eng. 2022, 260, 112041. [Google Scholar] [CrossRef]
- Slim, H.; Nadeau, S. A Mixed Rough Sets/Fuzzy Logic Approach for Modelling Systemic Performance Variability with FRAM. Sustainability 2020, 12, 1918. [Google Scholar] [CrossRef]
- Saurin, T.A.; Werle, N.J.B. A framework for the analysis of slack in socio-technical systems. Reliab. Eng. Syst. Saf. 2017, 167, 439–451. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fargnoli, M.; Murgianu, L.; Tronci, M. The Functional Resonance Analysis Method (FRAM) Application in the Healthcare Sector: Lessons Learned from Two Case Studies on Medical Device Management. Appl. Sci. 2024, 14, 9495. https://doi.org/10.3390/app14209495
Fargnoli M, Murgianu L, Tronci M. The Functional Resonance Analysis Method (FRAM) Application in the Healthcare Sector: Lessons Learned from Two Case Studies on Medical Device Management. Applied Sciences. 2024; 14(20):9495. https://doi.org/10.3390/app14209495
Chicago/Turabian StyleFargnoli, Mario, Luca Murgianu, and Massimo Tronci. 2024. "The Functional Resonance Analysis Method (FRAM) Application in the Healthcare Sector: Lessons Learned from Two Case Studies on Medical Device Management" Applied Sciences 14, no. 20: 9495. https://doi.org/10.3390/app14209495
APA StyleFargnoli, M., Murgianu, L., & Tronci, M. (2024). The Functional Resonance Analysis Method (FRAM) Application in the Healthcare Sector: Lessons Learned from Two Case Studies on Medical Device Management. Applied Sciences, 14(20), 9495. https://doi.org/10.3390/app14209495







