Associations of Balance, Strength, and Gait Speed with Cognitive Function in Older Individuals over 60 Years: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
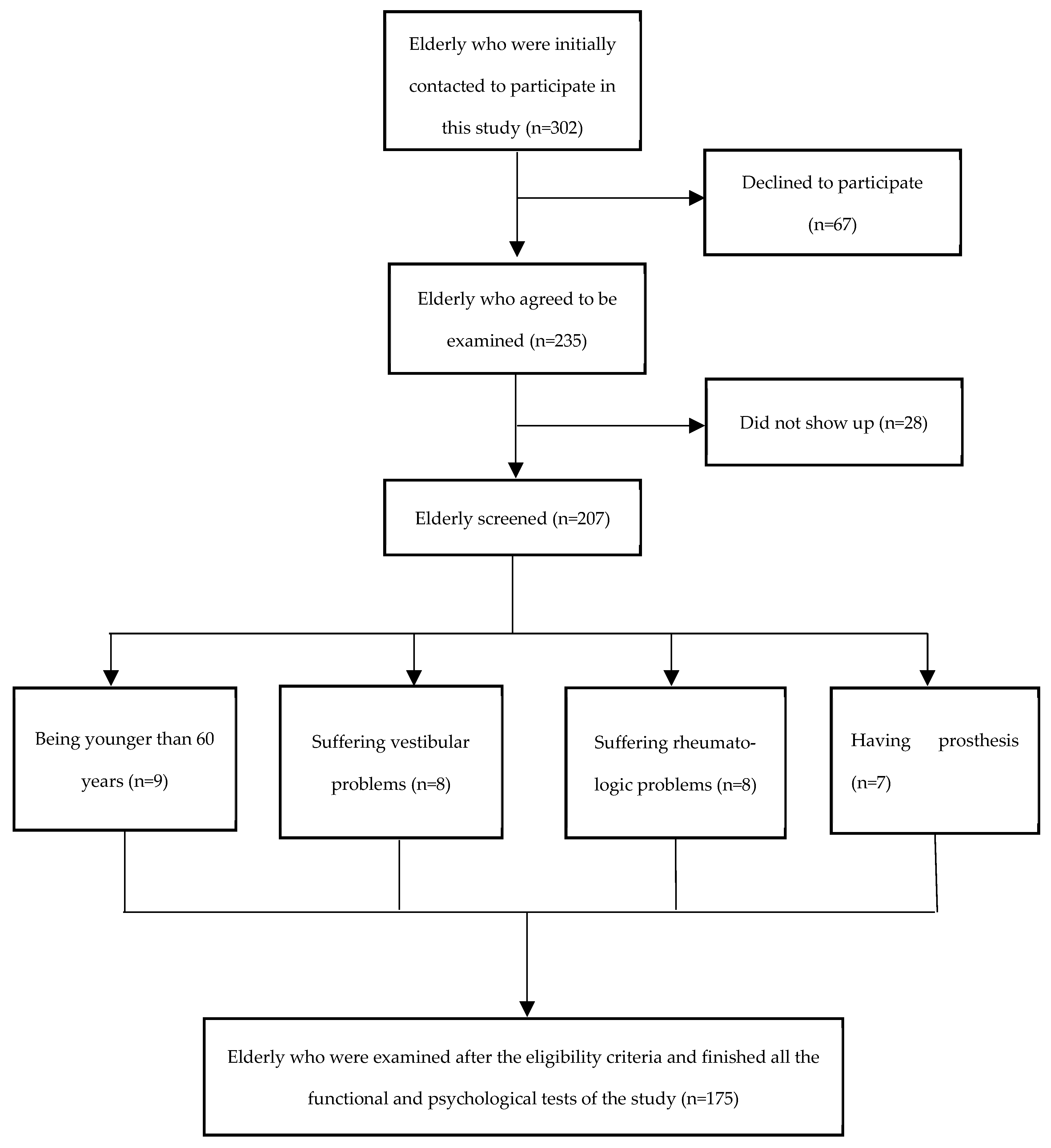
2.1. Participants
2.2. Sociodemographic and Anthropometric Information
2.3. Fall Risk Outcomes
2.3.1. Balance Confidence
2.3.2. Gait Speed
2.3.3. Handgrip Strength
2.3.4. Dynamic Balance
2.4. Cognitive Function Outcomes
2.4.1. Global Cognitive Function and Screener for Mild Cognitive Impairment
2.4.2. Verbal Fluency
2.4.3. Language
2.5. Statistical Analysis
3. Results
4. Discussion
4.1. Dynamic balance
4.2. Gait Speed
4.3. Handgrip Strength
4.4. Balance Confidence
4.5. Covariates
4.6. Limitations and Strengths
4.7. Implications and Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Fact Sheets: Falls. Available online: https://www.who.int/news-room/fact-sheets/detail/falls (accessed on 28 August 2023).
- Racey, M.; Markle-Reid, M.; Fitzpatrick-Lewis, D.; Ali, M.U.; Gagne, H.; Hunter, S.; Ploeg, J.; Sztramko, R.; Harrison, L.; Lewis, R.; et al. Fall Prevention in Community-Dwelling Adults with Mild to Moderate Cognitive Impairment: A Systematic Review and Meta-Analysis. BMC Geriatr. 2021, 21, 689. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Ageing & Life Course Unit. In WHO Global Report on Falls Prevention in Older Age; World Health Organization: Paris, France, 2007. [Google Scholar]
- Enderlin, C.; Rooker, J.; Ball, S.; Hippensteel, D.; Alderman, J.; Fisher, S.J.; McLeskey, N.; Jordan, K. Summary of Factors Contributing to Falls in Older Adults and Nursing Implications. Geriatr. Nurs. 2015, 36, 397–406. [Google Scholar] [CrossRef]
- Cadore, E.L.; Rodríguez-Mañas, L.; Sinclair, A.; Izquierdo, M. Effects of Different Exercise Interventions on Risk of Falls, Gait Ability, and Balance in Physically Frail Older Adults: A Systematic Review. Rejuvenation Res. 2013, 16, 105–114. [Google Scholar] [CrossRef] [PubMed]
- Pirker, W.; Katzenschlager, R. Gait Disorders in Adults and the Elderly: A Clinical Guide. Wien. Klin. Wochenschr. 2017, 129, 81–95. [Google Scholar] [CrossRef]
- Zhai, M.; Huang, Y.; Zhou, S.; Jin, Y.; Feng, J.; Pei, C.; Wen, L.; Wen’s, L. Effects of Age-Related Changes in Trunk and Lower Limb Range of Motion on Gait. BMC Musculoskelet. Disord. 2023, 24, 234. [Google Scholar] [CrossRef]
- Kyrdalen, I.L.; Thingstad, P.; Sandvik, L.; Ormstad, H. Associations between Gait Speed and Well-Known Fall Risk Factors among Community-Dwelling Older Adults. Physiother. Res. Int. 2019, 24, e1743. [Google Scholar] [CrossRef]
- Štefan, L.; Kasović, M.; Zvonar, M. Gait Speed as a Screening Tool for Foot Pain and the Risk of Falls in Community-Dwelling Older Women: A Cross-Sectional Study. Clin. Interv. Aging 2020, 15, 1569–1574. [Google Scholar] [CrossRef]
- Cuevas-Trisan, R. Balance Problems and Fall Risks in the Elderly. Clin. Geriatr. Med. 2019, 35, 173–183. [Google Scholar] [CrossRef]
- Viswanathan, A.; Sudarsky, L. Balance and Gait Problems in the Elderly. Handb. Clin. Neurol. 2012, 103, 623–634. [Google Scholar]
- Szlejf, C.; Suemoto, C.K.; Lotufo, P.A.; Benseñor, I.M. Association of Sarcopenia With Performance on Multiple Cognitive Domains: Results From the ELSA-Brasil Study. J. Gerontol. A Biol. Sci. Med. Sci. 2019, 74, 1805–1811. [Google Scholar] [CrossRef]
- Taani, M.H.; Siglinsky, E.; Kovach, C.R.; Buehring, B. Psychosocial Factors Associated With Reduced Muscle Mass, Strength, and Function in Residential Care Apartment Complex Residents. Res. Gerontol. Nurs. 2018, 11, 238–248. [Google Scholar] [CrossRef] [PubMed]
- Bohannon, R.W. Grip Strength: An Indispensable Biomarker For Older Adults. Clin. Interv. Aging 2019, 14, 1681–1691. [Google Scholar] [CrossRef] [PubMed]
- Chantanachai, T.; Sturnieks, D.L.; Lord, S.R.; Payne, N.; Webster, L.; Taylor, M.E. Risk Factors for Falls in Older People with Cognitive Impairment Living in the Community: Systematic Review and Meta-Analysis. Ageing Res. Rev. 2021, 71, 101452. [Google Scholar] [CrossRef] [PubMed]
- Montilla-Ibáñez, A.; Martínez-Amat, A.; Lomas-Vega, R.; Cruz-Díaz, D.; la Torre-Cruz, M.J.D.; Casuso-Pérez, R.; Hita-Contreras, F. The Activities-Specific Balance Confidence Scale: Reliability and Validity in Spanish Patients with Vestibular Disorders. Disabil. Rehabil. 2017, 39, 697–703. [Google Scholar] [CrossRef]
- Gómez Montes, J.F.; Curcio, C.L.; Alvarado, B.; Zunzunegui, M.V.; Guralnik, J. Validity and Reliability of the Short Physical Performance Battery (SPPB): A Pilot Study on Mobility in the Colombian Andes. Colomb. Med. 2013, 44, 165–171. [Google Scholar] [CrossRef]
- Ruiz-Ruiz, J.; Mesa, J.L.M.; Gutiérrez, A.; Castillo, M.J. Hand Size Influences Optimal Grip Span in Women but Not in Men. J. Hand Surg. Am. 2002, 27, 897–901. [Google Scholar] [CrossRef]
- Dodds, R.M.; Syddall, H.E.; Cooper, R.; Benzeval, M.; Deary, I.J.; Dennison, E.M.; Der, G.; Gale, C.R.; Inskip, H.M.; Jagger, C.; et al. Grip Strength across the Life Course: Normative Data from Twelve British Studies. PLoS ONE 2014, 9, e113637. [Google Scholar] [CrossRef]
- Bohannon, R.W. Test-Retest Reliability of Measurements of Hand-Grip Strength Obtained by Dynamometry from Older Adults: A Systematic Review of Research in the PubMed Database. J. Frailty Aging 2017, 6, 83–87. [Google Scholar] [CrossRef]
- Podsiadlo, D.; Richardson, S. The Timed “Up & Go”: A Test of Basic Functional Mobility for Frail Elderly Persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar] [CrossRef]
- Shumway-Cook, A.; Brauer, S.; Woollacott, M. Predicting the Probability for Falls in Community-Dwelling Older Adults Using the Timed up and Go Test. Phys. Ther. 2000, 80, 896–903. [Google Scholar] [CrossRef] [PubMed]
- Johansen, K.L.; Stistrup, R.D.; Schjøtt, C.S.; Madsen, J.; Vinther, A. Absolute and Relative Reliability of the Timed ‘Up & Go’ Test and ‘30second Chair-Stand’ Test in Hospitalised Patients with Stroke. PLoS ONE 2016, 11, e0165663. [Google Scholar] [CrossRef]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. ‘Mini-Mental State’. A Practical Method for Grading the Cognitive State of Patients for the Clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Jia, X.; Wang, Z.; Huang, F.; Su, C.; Du, W.; Jiang, H.; Wang, H.; Wang, J.; Wang, F.; Su, W.; et al. A Comparison of the Mini-Mental State Examination (MMSE) with the Montreal Cognitive Assessment (MoCA) for Mild Cognitive Impairment Screening in Chinese Middle-Aged and Older Population: A Cross-Sectional Study. BMC Psychiatry 2021, 21, 485. [Google Scholar] [CrossRef] [PubMed]
- Santos-Eggimann, B.; Ballan, K.; Fustinoni, S.; Büla, C. Measuring Slowness in Old Age: Times to Perform Moberg Picking-Up and Walking Speed Tests. J. Am. Med. Dir. Assoc. 2020, 21, 1729–1734.e2. [Google Scholar] [CrossRef] [PubMed]
- Lezak, M.D.; Howieson, D.; Loring, D.; Hannay, H.; Fischer, J. Neuropsychological Assessment; Oxford University Press: New York, NY, USA, 2004. [Google Scholar]
- Strauss, E.; Sherman, E.M.S.; Spreen, O. A Compendium of Neuropsychological Tests: Administration, Norms and Commentary; Oxford University Press: New York, NY, USA, 2006. [Google Scholar]
- Williams, B.W.; Mack, W.; Henderson, V.W. Boston Naming Test in Alzheimer’s Disease. Neuropsychologia 1989, 27, 1073–1079. [Google Scholar] [CrossRef]
- Greene, B.R.; Kenny, R.A. Assessment of Cognitive Decline through Quantitative Analysis of the Timed up and Go Test. IEEE Trans. Biomed. Eng. 2012, 59, 988–995. [Google Scholar] [CrossRef] [PubMed]
- Katsumata, Y.; Todoriki, H.; Yasura, S.; Dodge, H.H. Timed up and Go Test Predicts Cognitive Decline in Healthy Adults Aged 80 and Older in Okinawa: Keys to Optimal Cognitive Aging (KOCOA) Project. J. Am. Geriatr. Soc. 2011, 59, 2188–2189. [Google Scholar] [CrossRef] [PubMed]
- Kose, Y.; Ikenaga, M.; Yamada, Y.; Morimura, K.; Takeda, N.; Ouma, S.; Tsuboi, Y.; Yamada, T.; Kimura, M.; Kiyonaga, A.; et al. Timed Up and Go Test, Atrophy of Medial Temporal Areas and Cognitive Functions in Community-Dwelling Older Adults with Normal Cognition and Mild Cognitive Impairment. Exp. Gerontol. 2016, 85, 81–87. [Google Scholar] [CrossRef]
- Van Patten, R.; Lee, E.E.; Graham, S.A.; Depp, C.A.; Kim, H.C.; Jeste, D.V.; Twamley, E.W. The Utility of the Timed Up-and-Go Test in Predicting Cognitive Performance: A Cross-Sectional Study of Independent Living Adults in a Retirement Community. J. Appl. Gerontol. 2020, 39, 1163–1168. [Google Scholar] [CrossRef]
- Ng, T.K.S.; Han, M.F.Y.; Loh, P.Y.; Kua, E.H.; Yu, J.; Best, J.R.; Mahendran, R. Differential Associations between Simple Physical Performance Tests with Global and Specific Cognitive Functions in Cognitively Normal and Mild Cognitive Impairment: A Cross-Sectional Cohort Study of Asian Community-Dwelling Older Adults. BMC Geriatr. 2022, 22, 798. [Google Scholar] [CrossRef]
- Donoghue, O.A.; Horgan, N.F.; Savva, G.M.; Cronin, H.; O’Regan, C.; Kenny, R.A. Association between Timed Up-and-Go and Memory, Executive Function, and Processing Speed. J. Am. Geriatr. Soc. 2012, 60, 1681–1686. [Google Scholar] [CrossRef]
- Mumic de Melo, L.; Hotta Ansai, J.; Giusti Rossi, P.; Carvalho Vale, F.A.; Cristhine de Medeiros Takahashi, A.; Pires de Andrade, L. Performance of an Adapted Version of the Timed Up-and-Go Test in People with Cognitive Impairments. J. Mot. Behav. 2019, 51, 647–654. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.L.; Chen, T.F.; Tseng, W.Y. White Matter Pathways Underlying Chinese Semantic and Phonological Fluency in Mild Cognitive Impairment. Neuropsychologia 2020, 149, 107671. [Google Scholar] [CrossRef] [PubMed]
- Valkanova, V.; Esser, P.; Demnitz, N.; Sexton, C.E.; Zsoldos, E.; Mahmood, A.; Griffanti, L.; Kivimäki, M.; Singh-Manoux, A.; Dawes, H.; et al. Association between Gait and Cognition in an Elderly Population Based Sample. Gait Posture 2018, 65, 240–245. [Google Scholar] [CrossRef] [PubMed]
- Amboni, M.; Barone, P.; Hausdorff, J.M. Cognitive Contributions to Gait and Falls: Evidence and Implications. Mov. Disord. 2013, 28, 1520–1533. [Google Scholar] [CrossRef] [PubMed]
- Chou, M.Y.; Nishita, Y.; Nakagawa, T.; Tange, C.; Tomida, M.; Shimokata, H.; Otsuka, R.; Chen, L.K.; Arai, H. Role of Gait Speed and Grip Strength in Predicting 10-Year Cognitive Decline among Community-Dwelling Older People. BMC Geriatr. 2019, 19, 186. [Google Scholar] [CrossRef]
- Collyer, T.A.; Murray, A.M.; Woods, R.L.; Storey, E.; Chong, T.T.J.; Ryan, J.; Orchard, S.G.; Brodtmann, A.; Srikanth, V.K.; Shah, R.C.; et al. Association of Dual Decline in Cognition and Gait Speed With Risk of Dementia in Older Adults. JAMA Netw. Open 2022, 5, e2214647. [Google Scholar] [CrossRef]
- Falck, R.S.; Wilcox, S.; Best, J.R.; Chandler, J.L.; Liu-Ambrose, T. The Association Between Physical Performance and Executive Function in a Sample of Rural Older Adults from South Carolina, USA. Exp. Aging Res. 2017, 43, 192–205. [Google Scholar] [CrossRef]
- Huang, X.; Alcantara, L.S.; Tan, C.S.; Ng, Y.L.; Van Dam, R.M.; Hilal, S. Handgrip Strength and Cognitive Performance in a Multiethnic Cohort in Singapore. J. Alzheimer’s Dis. 2022, 90, 1547–1555. [Google Scholar] [CrossRef]
- Luo, J.; Su, L.; Ndeke, J.M.; Wang, F.; Hendryx, M. Gait Speed, Handgrip Strength, and Cognitive Impairment among Older Women—A Multistate Analysis. Exp. Gerontol. 2022, 169, 111947. [Google Scholar] [CrossRef]
- Jin, Y.L.; Xu, L.; Jiang, C.Q.; Zhang, W.S.; Pan, J.; Zhu, F.; Zhu, T.; Thomas, G.N.; Lam, T.H. Association of Hand Grip Strength with Mild Cognitive Impairment in Middle-Aged and Older People in Guangzhou Biobank Cohort Study. Int. J. Environ. Res. Public Health 2022, 19, 6464. [Google Scholar] [CrossRef] [PubMed]
- Veronese, N.; Stubbs, B.; Trevisan, C.; Bolzetta, F.; De Rui, M.; Solmi, M.; Sartori, L.; Musacchio, E.; Zambon, S.; Perissinotto, E.; et al. What Physical Performance Measures Predict Incident Cognitive Decline among Intact Older Adults? A 4.4year Follow up Study. Exp. Gerontol. 2016, 81, 110–118. [Google Scholar] [CrossRef] [PubMed]
- Atkinson, H.H.; Rapp, S.R.; Williamson, J.D.; Lovato, J.; Absher, J.R.; Gass, M.; Henderson, V.W.; Johnson, K.C.; Kostis, J.B.; Sink, K.M.; et al. The Relationship Between Cognitive Function and Physical Performance in Older Women: Results From the Women’s Health Initiative Memory Study. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2010, 65A, 300. [Google Scholar] [CrossRef] [PubMed]
- Prokopidis, K.; Giannos, P.; Ispoglou, T.; Kirk, B.; Witard, O.C.; Dionyssiotis, Y.; Scott, D.; Macpherson, H.; Duque, G.; Isanejad, M. Handgrip Strength Is Associated with Learning and Verbal Fluency in Older Men without Dementia: Insights from the NHANES. GeroScience 2023, 45, 1049–1058. [Google Scholar] [CrossRef] [PubMed]
- Chen, P.H.; Yang, Y.Y.; Liao, Y.Y.; Cheng, S.J.; Wang, P.N.; Cheng, F.Y. Factors Associated with Fear of Falling in Individuals with Different Types of Mild Cognitive Impairment. Brain Sci. 2022, 12, 990. [Google Scholar] [CrossRef]
- Tiernan, C.; Schwarz, D.J.; Goldberg, A. Associations of Usual and Fast Gait Speed with Physical Performance and Balance Confidence in Community-Dwelling Older Adults: Implications for Assessment. J. Geriatr. Phys. Ther. 2023. [Google Scholar] [CrossRef]
- Qin, H.Y.; Zhao, X.D.; Zhu, B.G.; Hu, C.P. Demographic Factors and Cognitive Function Assessments Associated with Mild Cognitive Impairment Progression for the Elderly. BioMed Res. Int. 2020, 2020, 3054373. [Google Scholar] [CrossRef]
| Characteristics | Total (n = 175) | Men (n = 38) | Women (n = 137) | ||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||
| Age (years) | 66.64 | 5.58 | 64.98 | 4.84 | 67.11 | 5.70 | |
| BMI (kg/m2) | 29.80 | 4.78 | 30.14 | 3.93 | 29.71 | 5.01 | |
| N | Percentage | N | Percentage | N | Percentage | ||
| Occupational status | Retired | 150 | 85.71 | 26 | 69.42 | 124 | 94.51 |
| Working | 6 | 3.42 | 4 | 10.52 | 2 | 1.46 | |
| Unemployed | 19 | 10.87 | 8 | 10.06 | 11 | 4.03 | |
| Marital Status | Single | 5 | 2.85 | 4 | 10.52 | 1 | 0.73 |
| Married/ cohabiting | 121 | 69.14 | 7 | 18.42 | 114 | 83.21 | |
| Separated/divorced/widowed | 49 | 28.01 | 27 | 71.06 | 22 | 16.06 | |
| Educational level | No formal education | 60 | 34.28 | 12 | 31.58 | 48 | 35.03 |
| Primary education | 81 | 46.28 | 17 | 44.75 | 64 | 46.71 | |
| Secondary education | 24 | 17.51 | 6 | 15.78 | 18 | 13.13 | |
| University | 10 | 5.71 | 3 | 7.89 | 7 | 5.13 | |
| Mean | SD | Mean | SD | Mean | SD | ||
| MMSE (score) | 25.93 | 3.01 | 26.47 | 2.44 | 25.78 | 3.15 | |
| Phonologic fluency (w) | 32.07 | 12.69 | 37.05 | 12.19 | 30.70 | 12.51 | |
| Semantic fluency (w) | 31.75 | 10.25 | 34.79 | 13.65 | 30.90 | 8.98 | |
| Language (score) | 10.45 | 2.86 | 11.79 | 2.50 | 10.08 | 2.85 | |
| TUG (s) | 7.09 | 1.53 | 6.77 | 1.47 | 7.17 | 1.55 | |
| Handgrip strength (kg) | 25.59 | 8.12 | 37.77 | 7.28 | 22.21 | 4.14 | |
| ABC (score) | 76.27 | 21.61 | 83.77 | 17.45 | 74.20 | 22.25 | |
| Gait speed (s) | 2.283 | 0.50 | 2.09 | 0.46 | 2.33 | 0.51 | |
| MMSE | Phonologic Fluency | Semantic Fluency | Language | ||
|---|---|---|---|---|---|
| TUG | −0.236 ** | −0.122 | −0.303 ** | −0.219 ** | |
| Handgrip strength | 0.140 | 0.201 ** | 0.190 * | 0.264 ** | |
| ABC | 0.135 | 0.161 * | 0.277 ** | 0.205 ** | |
| Gait speed | −0.150 * | −0.139 | −0.352 ** | −0.297 ** | |
| Age (years) | −0.149 * | -0.144 | −0.385 ** | −0.353 ** | |
| Sex | −0.095 | −0.207 ** | −0.157 * | −0.246 ** | |
| Educational level | 0.330 ** | 0.509 ** | 0.318 ** | 0.542 ** | |
| BMI (kg/m2) | −0.068 | 0.046 | −0.110 | −0.066 | |
| Variable | B | β | t | 95% CI | p-Value | ||
|---|---|---|---|---|---|---|---|
| MMSE | TUG | −0.538 | −0.275 | −2.254 | −1.09 | −0.67 | 0.025 |
| Educational level | 1.268 | 0.319 | 3.838 | 0.616 | 1.920 | <0.001 | |
| Phonologic fluency | Educational level | 7.360 | 0.041 | 5.965 | 4.921 | 9.797 | <0.001 |
| Age | −0.554 | −0.244 | −3.551 | −0.862 | −0.246 | <0.001 | |
| Semantic fluency | Educational level | 3.678 | 0.273 | 3.364 | 1.520 | 5.873 | 0.001 |
| Gait speed | −4.931 | −0.241 | −1.970 | −9.873 | 0.011 | 0.049 | |
| TUG | −1.378 | −0.207 | −2.572 | −2.437 | −0.320 | 0.011 | |
| ABC | 0.077 | 0.163 | 2.045 | 0.003 | 0.152 | 0.042 | |
| Language | Educational level | 1.796 | 0.476 | 6.613 | 1.260 | 0.233 | <0.001 |
| Gait speed | −1.654 | −0.290 | −2.661 | −2.882 | −0.427 | 0.009 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jiménez-García, J.D.; Ortega-Gómez, S.; Martínez-Amat, A.; Álvarez-Salvago, F. Associations of Balance, Strength, and Gait Speed with Cognitive Function in Older Individuals over 60 Years: A Cross-Sectional Study. Appl. Sci. 2024, 14, 1500. https://doi.org/10.3390/app14041500
Jiménez-García JD, Ortega-Gómez S, Martínez-Amat A, Álvarez-Salvago F. Associations of Balance, Strength, and Gait Speed with Cognitive Function in Older Individuals over 60 Years: A Cross-Sectional Study. Applied Sciences. 2024; 14(4):1500. https://doi.org/10.3390/app14041500
Chicago/Turabian StyleJiménez-García, José Daniel, Sonia Ortega-Gómez, Antonio Martínez-Amat, and Francisco Álvarez-Salvago. 2024. "Associations of Balance, Strength, and Gait Speed with Cognitive Function in Older Individuals over 60 Years: A Cross-Sectional Study" Applied Sciences 14, no. 4: 1500. https://doi.org/10.3390/app14041500
APA StyleJiménez-García, J. D., Ortega-Gómez, S., Martínez-Amat, A., & Álvarez-Salvago, F. (2024). Associations of Balance, Strength, and Gait Speed with Cognitive Function in Older Individuals over 60 Years: A Cross-Sectional Study. Applied Sciences, 14(4), 1500. https://doi.org/10.3390/app14041500










