Abstract
Additive manufacturing has been widely used in various industries, including the healthcare sector. Over the last few decades, AM has been playing an important role in the medical field in different areas, including surgical planning, implants, and educational activities. For surgical applications, AM can help surgeons practice and plan an operation until they are confident with the process. This can help to reduce operational risk and time. In addition, it can help to demonstrate the problem to other colleagues. AM has also been used to produce 3D models to teach students and doctors about human anatomy. This paper aims to comprehensively review the diverse applications of additive manufacturing within the domains of surgical planning and medical education. By focusing on the multifaceted roles played by AM in these critical areas, a contribution to the growing body of knowledge that underscores the transformative potential of this technology in shaping the future of healthcare practices is sought to be made.
Keywords:
additive manufacturing; 3D printing; FDM; SLA; medical devices; healthcare; surgical planning 1. Introduction
Additive manufacturing (AM), also known as 3D printing, is an advancing technology that is revolutionizing the manufacturing sector and is progressively unveiling its potential within healthcare [1]. The process involves the creation of three-dimensional (3D) objects through successive material deposition in 2D layers. Originating in 1986 through the pioneering work of Charles Hull [2], 3D printers were initially embraced by the automobile and aerospace industries for prototyping purposes before mass production. Presently, the 3D-printing market, inclusive of both printers and services, constitutes an industry valued at around 18 billion dollars [3]. Apart from prototyping, 3D printing has diversified its applications to produce finalized items such as jewelry, heat exchangers, and medical implants. Its advantages over traditional manufacturing encompass the ability to fabricate objects with intricate internal structures, heightened versatility, customization, and reduced spatial demands.
More specifically, in the field of electronic equipment manufacturing, 3D printing has found its niche in the production of intricate components and circuitry. The ability to create complex shapes with precision has enabled faster prototyping and customization, reducing time to market for cutting-edge electronic devices. Recent reports from the literature such as the ones from Shi et.al. [4,5], indicate the use of 3D-printing applications in electromagnetic shielding. This flexibility has proven invaluable in the fast-paced world of consumer electronics, facilitating rapid design iterations and improvements. On the other hand, communication systems have also witnessed significant advancements through 3D printing. Antenna components, connectors, and other intricate parts can now be manufactured with greater precision at a reduced cost. The streamlined production process contributes to the development of more efficient and compact communication devices, fostering innovation in the telecommunications industry [6].
Aerospace represents another sector where 3D printing has left an indelible mark. The technology allows for the creation of lightweight and complex geometries, a crucial factor in designing components for aircraft and spacecraft. From turbine blades to structural components, 3D printing enhances the performance and fuel efficiency of aerospace systems while enabling a more sustainable approach to manufacturing [7].
When integrated with medical imaging, 3D printing can bring forth novel prospects in medical progress. Ongoing research in various medical domains actively explores clinical applications of this emerging technology. The capability to generate 3D models from patient data empowers physicians to craft bespoke prosthetics and implants, enhance visualization of intricate pathologies, and revolutionize medical training methodologies [8].
In recent decades, 3D printing has gained significant prominence, enabling the transformation of three-dimensional digital designs into tangible objects using 3D printers. Within the medical field, this technology finds applications in diverse areas such as orthopedics, spinal surgery, maxillofacial surgery, neurosurgery, and cardiac surgery [9]. Typically, doctors rely on 2D X-ray or computed tomography (CT) and magnetic resonance (MR) scans, requiring advanced visualization skills. While introducing renderings from various imaging techniques has enhanced the understanding of intricate pathologies, it lacks tactile feedback. Utilizing 3D printing, complex medical cases can be studied, surgical procedures practiced, and both students and patients can be effectively educated.
Moreover, certain surgical procedures are intricate, demanding precise guidance to prevent harm to vital body parts or ensure desirable aesthetic results. Achieving this guidance often involves significant exposure to ionizing radiation and can considerably extend the duration of surgeries [10]. Furthermore, anatomical irregularities may necessitate customized prosthetics for precise and effective repairs [10]. The imperative for enhanced visualization and superior surgical results has led to the development of 3D-printed anatomical models, personalized guides for patients, and prosthetics crafted through 3D printing. The expanding utilization of 3D printing in surgery has sparked interest in evaluating the current integration of this innovative technology.
This review provides a comprehensive exploration of the numerous advantages that 3D printing, or additive manufacturing (AM), brings to the medical field. The widespread use of AM in healthcare is highlighted while its pivotal role in surgical planning implants and medical education is emphasized. Notably, the article describes how AM enables surgeons to meticulously practice and plan surgeries, reducing operational risks and time. The technology’s capacity to produce detailed 3D models proves invaluable for teaching, enhancing the understanding of human anatomy among students and medical professionals. By thoroughly reviewing the diverse applications of AM in surgical planning and medical education, this article contributes valuable insights and practical guidance. This analysis underscores the transformative potential of 3D-printing technology in revolutionizing healthcare practices, offering new perspectives that are poised to shape the future of the medical field.
2. Workflow
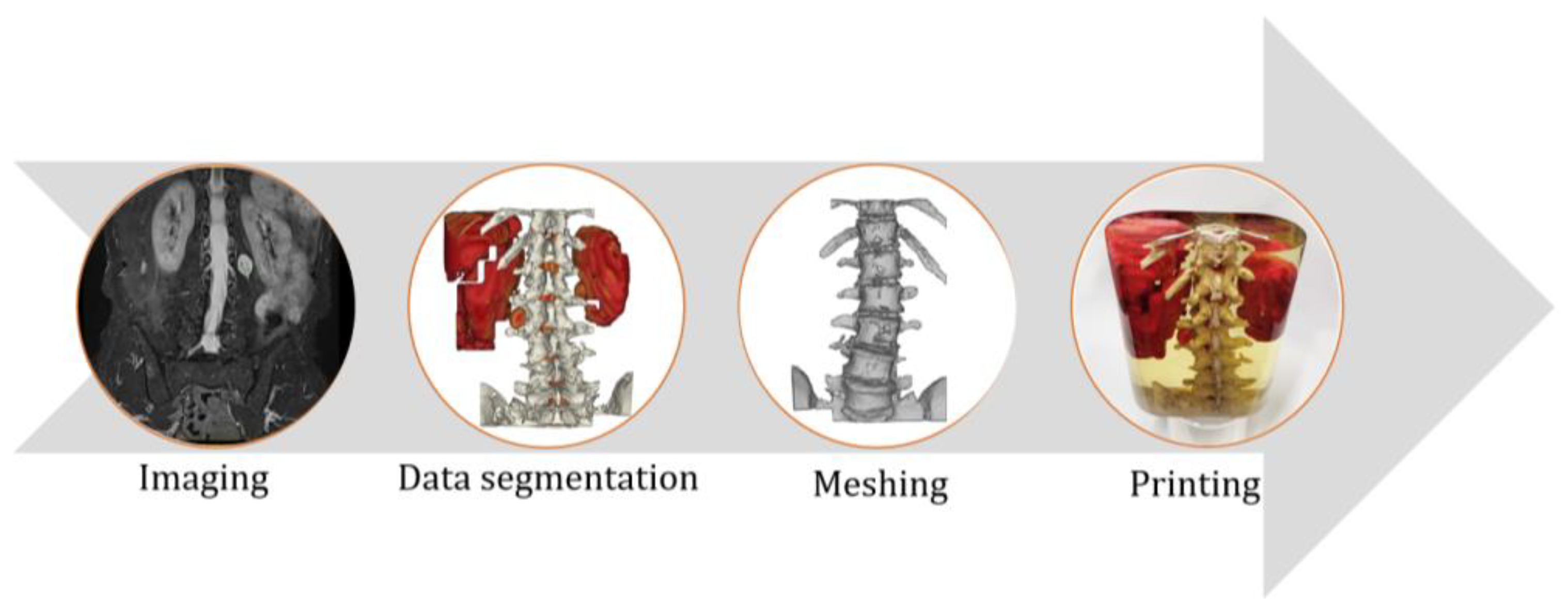
The overall workflow of generating a 3D model from imaging processes follows these stages (Figure 1):
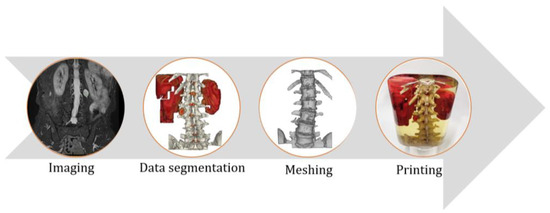
Figure 1.
A schematic of the workflow for a medical part.
- Medical imaging data acquisition
- Data processing and segmentation
- Meshing and conversion to 3D-printable file format,
- Printing the final part.
Each step is discussed in detail in the following section.
2.1. Imaging
In many hospitals, the pioneers in adopting 3D-printing technology are closely linked to medical imaging. Utilizable data from MRI, CT, and certain ultrasounds serve as a foundation for 3D printing [11]. However, not all scanning data is equal; low-resolution images can lead to disparities between the generated model and actual anatomy. Precision is crucial, as 3D models derived from scan data aid healthcare providers in comprehending a patient’s condition. Accurate data enhance the potential of 3D-printed models for personalized clinical education and patient-specific planning, significantly impacting healthcare [5].
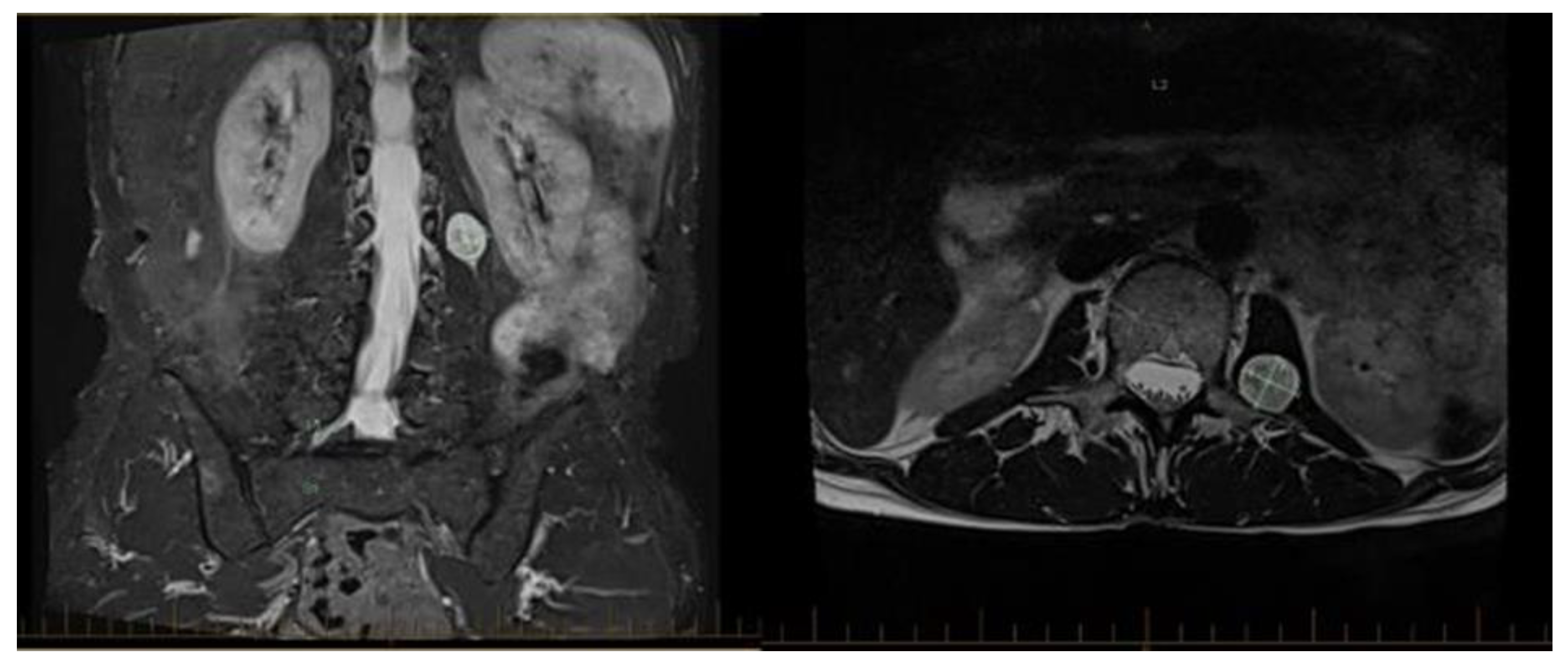
Radiologists, with their expertise in various imaging modalities, play a pivotal role in ensuring the highest-quality models are produced from the scans. Their skills are integral to the development and seamless integration of this transformative technology in medicine. These specialists need to ensure that the imaging is done with the specific intent of creating an accurate 3D model, with closely spaced scan slices. Figure 2 represents a single MRI image of a spine with a cancer tumor that has been detected next to it.
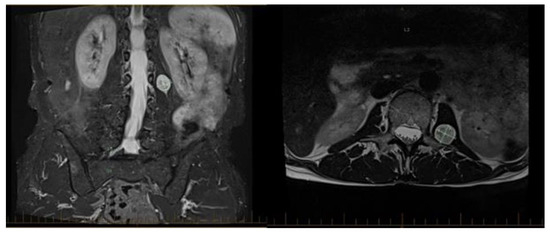
Figure 2.
An MRI image from a patient’s spine from different views to locate the cancer tumor.
An additional level of difficulty can be introduced when using scan data from multiple systems. In many cases, bone data, for example, are easier to obtain from CT scans, whereas soft-tissue data are easier to obtain from MRI scans. If both are needed, and if the scanning facility produces the scans on different machines, so with the patient in slightly different positions, data-fusion techniques need to be developed in order to fuse the two different data into a cohesive model.
2.2. Data Segmentation and Mesh Generation
Most medical imaging systems produce data as a series of 2D images, most commonly in DICOM file format. Special software is needed to transform this medical data into 3D files that are suitable for 3D-printing machines to construct the objects [11].
To convert medical-imaging data into 3D-printable data, there exist, today, numerous software options, ranging from open-source licensing, such as PostDICOM, Horos, RadiAnt, Navegatium, Pro Surgical 3D, MicroDicom, 3Dimviewer, Mango, Escape EMV, RTpotter, InVesalius, DICOM4QUI, and many more [https://www.postdicom.com/en/blog/top-25-free-dicom-viewers] (18 February 2024) to relatively expensive specialized medical CAD software such as Materials Mimics, 3-matic, 3D Slicer, Simpleware, Virtual Surgical Planning, D2P, and others, each offering unique features and applications [12].
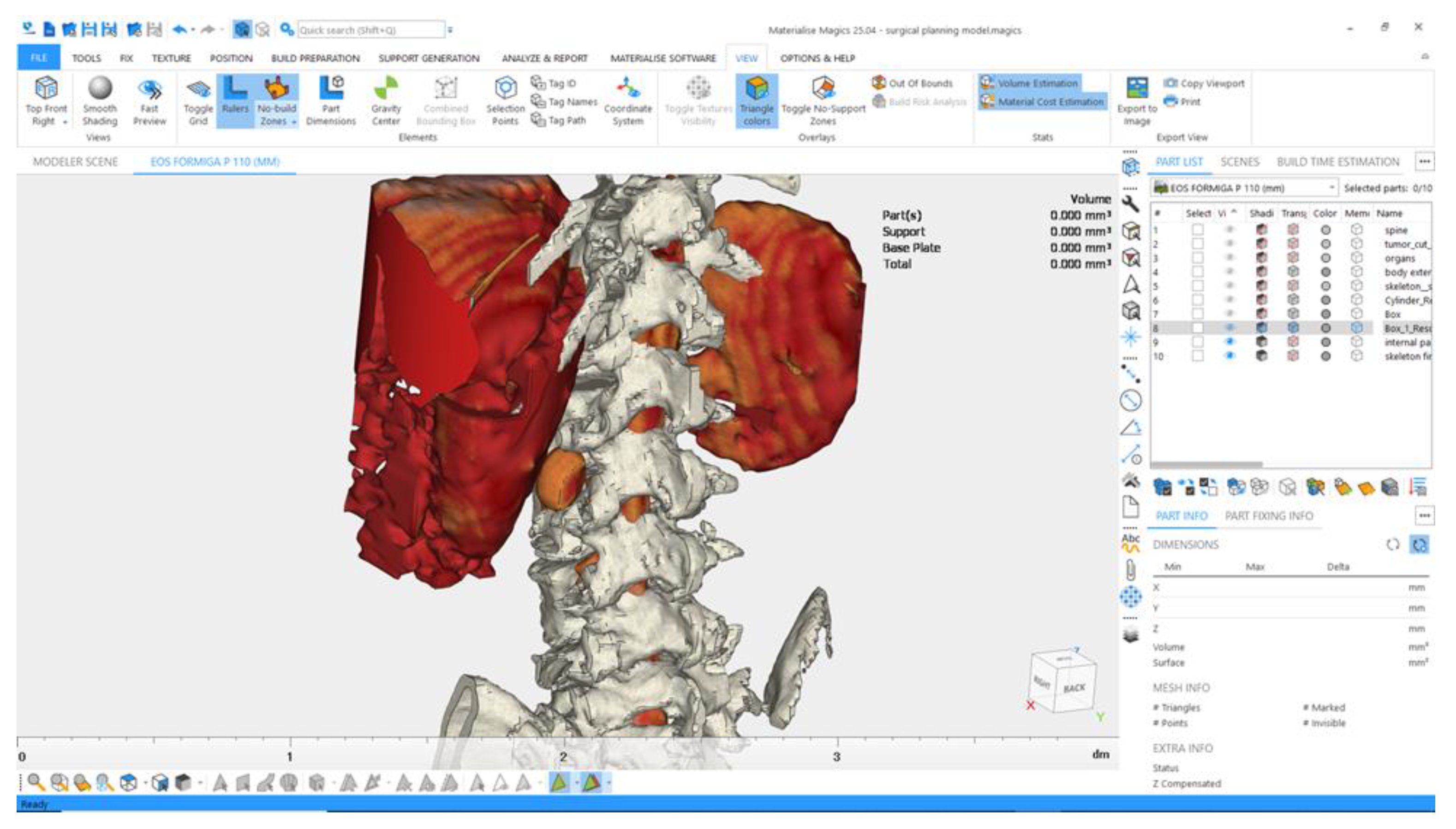
The overall workflow of converting DICOM files into 3D-printable files consists of, in a slice of the model, identifying the areas of interest such as bone and/or soft tissue by selecting different color ranges, or manually drawing around regions of interest, and then extrapolating the selected data through subsequent slices to create the 3D model. This can sometimes require manually selecting data in multiple regions of the model. Once the 3D model has been produced, it often requires digital post-processing to clean it up, smooth it or sharpen it, adjust colors and textures, etc. [12]. Figure 3 presents the final stage of preparation of a 3D model for printing in Magics.
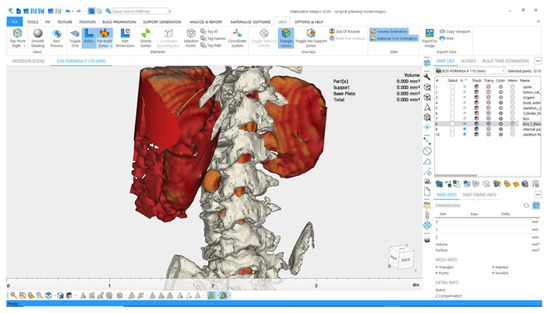
Figure 3.
A screenshot of the editing and mesh preparation step in Magics software (version 25.04).
2.3. 3D Printing and Post-Processing
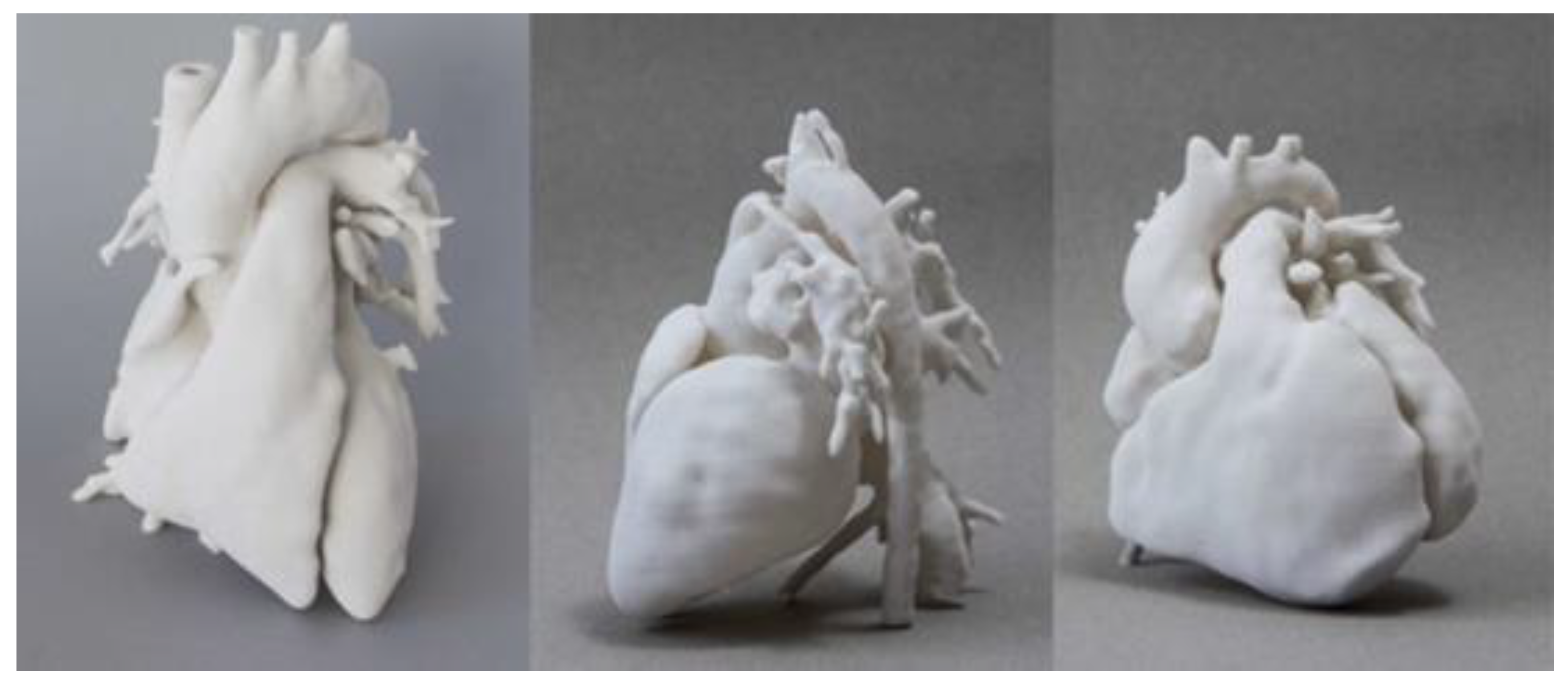
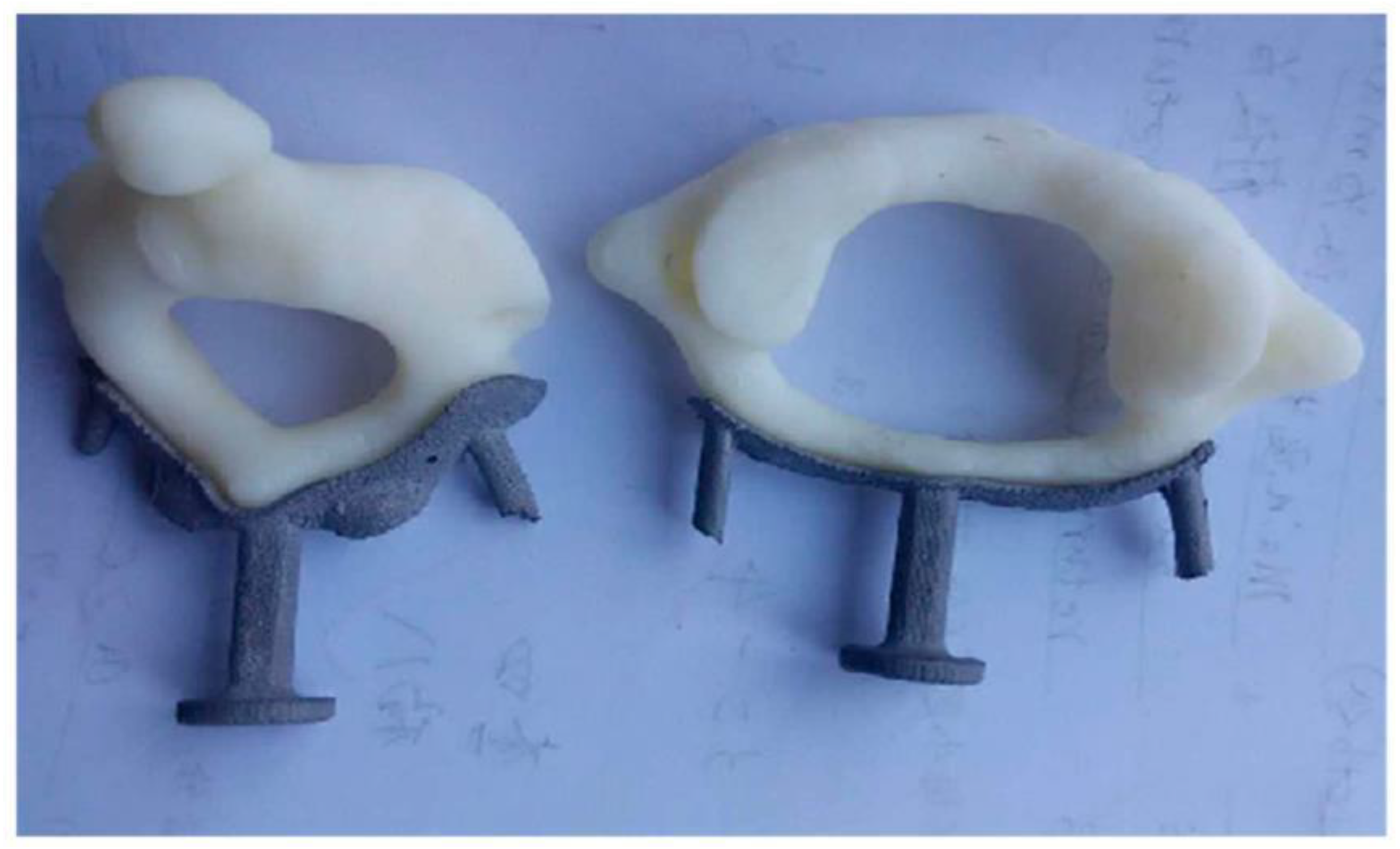
For 3D printing the models, different technologies can be used. For instance, vat photopolymerization (VPP), also known as Stereolithography (SLA), the pioneering 3D-printer technology for medical purposes, constructs 3D models by layering photoreactive resin material, subsequently solidified by ultraviolet light [10]. This method yields highly precise models but is confined to photopolymers, which can be costly. It also requires the use of sacrificial support material to support overhanging features, and this must be removed in a post-processing operation. Figure 4 depicts heart models manufactured via 3D-printing SLA method [13].
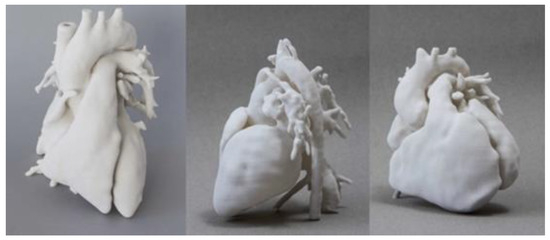
Figure 4.
Heart models manufactured via 3D-printing SLA method [13].
DIW, a type of extrusion-based 3D printing, involves the controlled deposition of materials in a layer-by-layer fashion. In the medical context, DIW 3D printing has shown promise in fabricating complex, patient-specific scaffolds for tissue engineering and regenerative medicine. The ability to precisely control the deposition of bioinks or other materials allows for the creation of intricate structures that mimic the natural environment of tissues. Additionally, DIW has been explored in the production of drug-delivery systems and custom implants tailored to individual patient needs [14].
Direct Ink Writing (DIW) 3D printing holds significant promise in the subsectors of surgical planning and education within the medical field. In the context of surgical planning, DIW technology allows for the fabrication of patient-specific models that replicate anatomical structures with high precision. Surgeons can use these 3D-printed models to enhance their preoperative planning, providing a tangible and accurate representation of the patient’s unique anatomy. This aids in better understanding complex cases, practicing procedures, and refining surgical approaches before entering the operating room. Additionally, DIW can be employed to create customized surgical guides and tools, improving intraoperative precision [15].
In the sector of medical education, DIW 3D printing contributes by producing detailed and realistic anatomical models for teaching purposes. These models serve as invaluable educational tools for students and practicing healthcare professionals, offering hands-on experiences that enhance their understanding of intricate anatomical structures. DIW facilitates the creation of complex anatomical features, allowing for a more comprehensive and realistic representation of human anatomy. This technology supports the development of educational resources, such as anatomical models and simulation tools, fostering a more immersive and effective learning environment for medical students and professionals alike. Thus, DIW 3D printing stands as a transformative technology with applications in surgical planning and education, ultimately improving patient outcomes and advancing medical training [16].
Powder bed fusion (PBF) employs a powder substrate fused by a powerful laser. Powder layers are successively applied and sintered into the desired 3D shape [14]. Unlike other 3D-printing techniques, PBF for polymers doesn’t necessitate support structures during printing, as objects are supported by the unfused powder in the bed. PBF technology is capable of producing metal, plastic, and ceramic items. However, its surface finish is often coarse, and can require post-processing. Figure 5 depicts a 3D-printed prosthetic socket and arm produced using PBF method.

Figure 5.
3D printed prosthetic socket and arm produced using PBF.
Material Extrusion (MEX) stands out as an economical 3D-printing method widely favored by consumers. These printers operate by heating a polymer filament in a printer head and depositing it at specified locations matching the model’s shape. The polymer solidifies as it cools, repeating this process layer by layer. Common materials include polylactic acid (PLA), acrylonitrile butadiene styrene (ABS), and other thermoplastics. However, the level of intricate detail achieved with MEX is usually lower than that of other techniques. Unlike PBF and inkjet methods, MEX-produced parts require additional support structures. Post printing, models often undergo surface smoothing and excess material removal through post-processing. The extent of post-processing depends on the printer type, quality, and materials used [16].
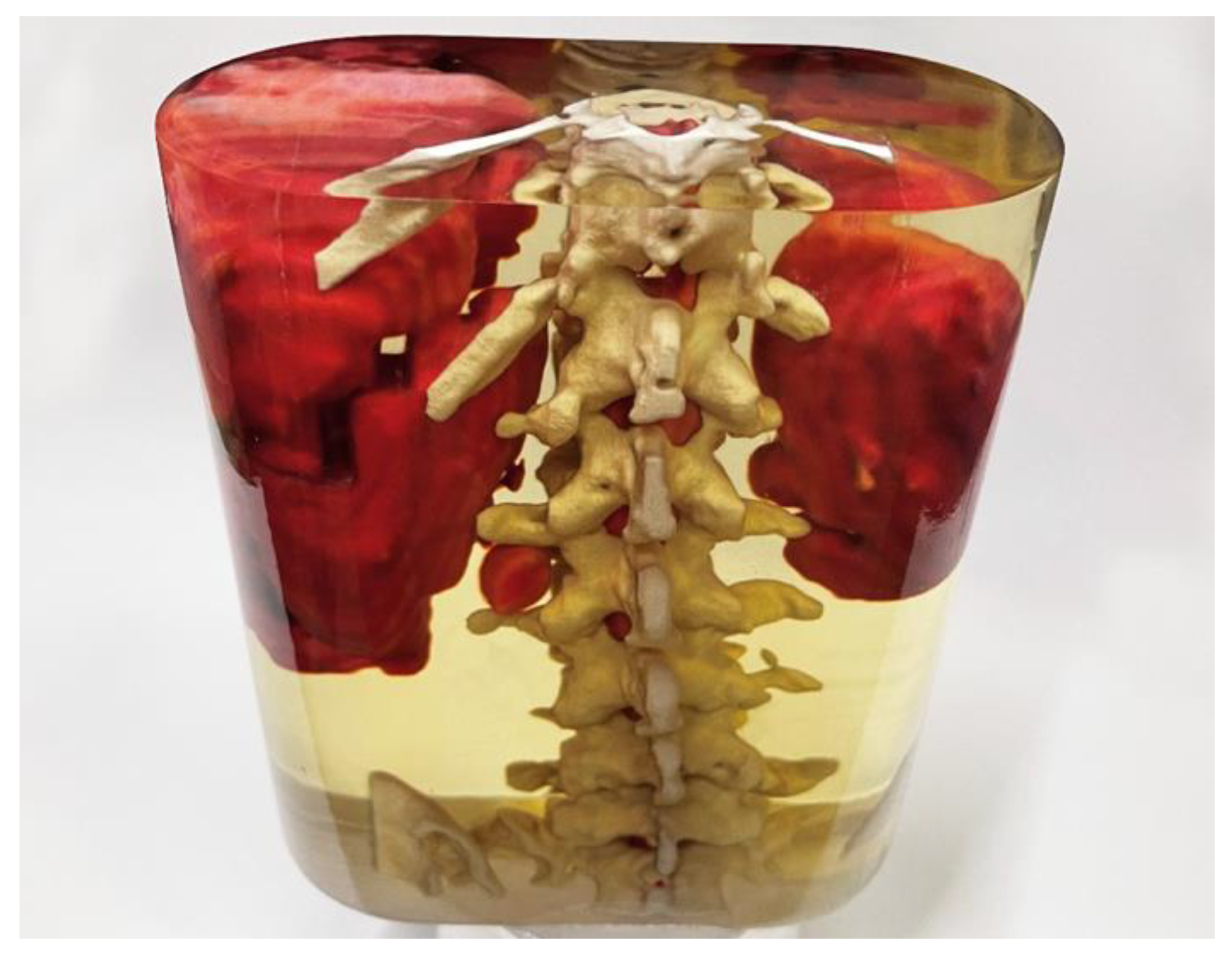
Material jetting (MJT) involves an inkjet print head forming small droplets from a liquid resin. This method uses a soluble support material that is relatively easy to dissolve or a waterjet blast-off. The biggest advantage of this technology is that it can print in multiple materials, including full-color and clear models or models with both soft and hard materials [15]. Figure 6 depicts such a case of a colored 3D-printed model of a tumor next to the spine printed with material jetting.

Figure 6.
A colored 3D-printed model of a tumor next to the spine printed with material jetting.
As this review looks into the diverse landscape of 3D-printing technologies in the medical field, it is imperative to explore potential future trends that could shape the trajectory of these innovations. In the sector of vat photopolymerization (VPP) and particularly Stereolithography (SLA), advancements in material science are anticipated, leading to the development of cost effective and versatile photopolymers. The ongoing research aims to overcome limitations related to material costs and post-processing steps, potentially expanding the range of applicable materials and minimizing the need for sacrificial support structures. Additionally, the integration of real-time imaging and diagnostic data into SLA processes may further enhance the precision and customization of 3D-printed medical models.
On the other hand, Direct Ink Writing (DIW) 3D printing is believed to be witnessing an evolution towards more sophisticated bioinks and materials suitable for intricate tissue-engineering applications. Predictions include the emergence of bioinks with enhanced biocompatibility and biomimicry, allowing for the fabrication of patient-specific scaffolds that closely mimic the natural tissue environment. As the understanding of regenerative medicine advances, DIW is likely to play a pivotal role in producing functional tissues and organs for transplantation, pushing the boundaries of personalized medicine.
Regarding Powder Bed Fusion (PBF, ongoing research seeks to refine the surface finish of printed objects, potentially reducing the need for extensive post-processing. Future trends may also involve the development of new materials for PBF, expanding its capabilities beyond metals, plastics, and ceramics. The medical field could witness increased adoption of PBF for the production of patient-specific implants with improved surface quality.
Also, Material Extrusion (MEX) is expected to undergo advancements in filament materials, potentially introducing new biocompatible polymers with improved structural properties. Future trends may focus on enhancing the precision and intricacy achievable with MEX, making it a more viable option for certain medical applications. Research efforts may also target the development of more efficient support structures, reducing post-processing requirements.
What is more, Material Jetting (MJT) is likely to witness increased integration of multi-material capabilities, enabling the creation of highly complex and customizable medical models. Future trends may involve the refinement of soluble support materials, streamlining post-processing steps and making MJT even more user-friendly. The expansion of color capabilities in 3D-printing models, as demonstrated in Figure 6, could become more widespread, enhancing the visual representation and educational value of printed medical models.
Thus, the future of 3D-printing technologies in the medical field looks promising. Advancements in materials, precision, and customization, along with a continuous focus on reducing post-processing steps, will contribute to the ongoing transformation of medical practices through innovative 3D-printing applications.
3. Educational Applications
3.1. Models of Human Organs
Medical professionals are in constant need of better tools that help them to save lives. 3D printing can be used to improve patient care, reduce costs, and increase the speed of every step in the medical value chain. Positive medical outcomes are usually decided by several factors: Well-briefed and prepared surgeons, efficient completion of the surgical procedure within the shortest possible timeframe, and an understanding of patient-specific risks to avoid complications during surgery.
All of these factors benefit greatly from using high-fidelity anatomical models made with 3D-printing technologies. As surgeons work in a real 3D world, it makes sense for them to analyze patient-specific 3D-printed models, particularly when complex pathologies are involved. This allows procedures to be refined during pre-surgery, meaning fewer complications, shorter procedures, and faster patient recovery times.
Anatomical models have found extensive applications in various surgical specialties, including maxillofacial surgery, cardiovascular surgery, vascular neurosurgery, dental surgery, general surgery, cranial/orbital surgery, orthopedics, and spinal surgery, as indicated by other studies [8,10,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45]. In maxillofacial surgery specifically, some studies [18] have highlighted the utility of anatomical models for implant shaping. Among these studies, some papers emphasized time reduction as a significant advantage. Furthermore, some studies confirmed that printed models offered accurate anatomical representations, leading to improved surgical outcomes, while some studies pointed out potential exposure to ionizing radiation and increased costs [18]. One study found the anatomical model to be an effective representation of the actual pathology without discussing associated costs, while another study acknowledged increased costs due to utilizing an anatomical model [19].
In our research, de-identified MRI data representing five common ventricular septal defect (VSD) subtypes (infundibular, membranous, inlet, muscular, and atrioventricular types) were retrieved from a radiology archive. Following the isolation of the heart in each image set, 3D volume rendering was applied to generate a digital heart model (Figure 7). After standard post-processing, synthetic models representing each VSD subtype were successfully produced.

Figure 7.
3D-printed heart model with VSDs.
These 3D heart models were used to develop a simulation-based educational curriculum focusing on the anatomy and clinical management of VSDs for pediatric residents. Furthermore, we successfully adapted the printing material to produce a heart model with a soft texture, facilitating the creation of surgical incisions and the placement of sutures within the models.
3.2. Human Body and Anatomy
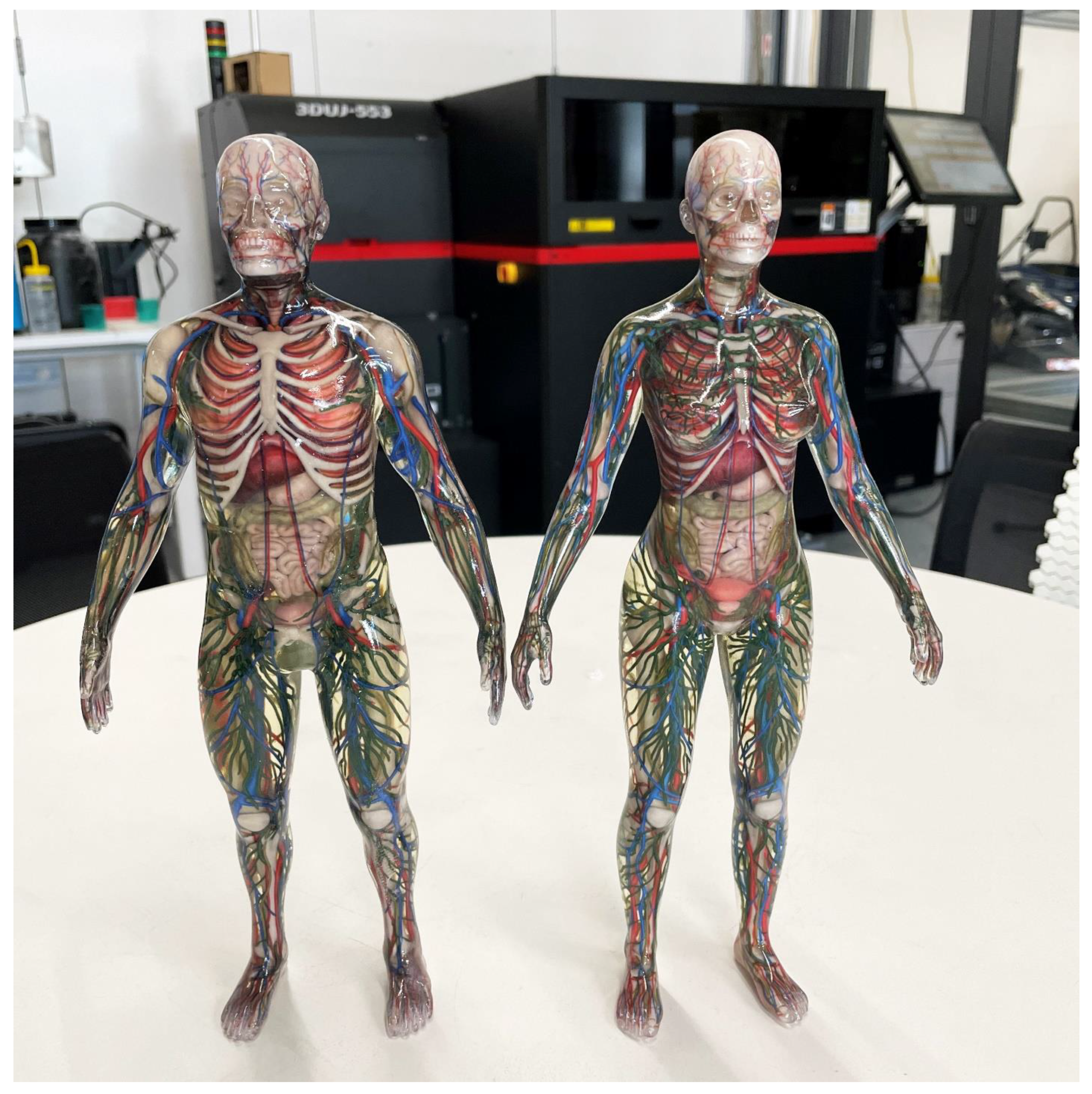
Another case of educational purposes regarding 3D printing can be with the printing of full-body anatomy models. In other cases, the anatomical model can be used to teach students and doctors about the anatomy. Figure 8 illustrates a 3D-printed full-body anatomy for the purpose of education.
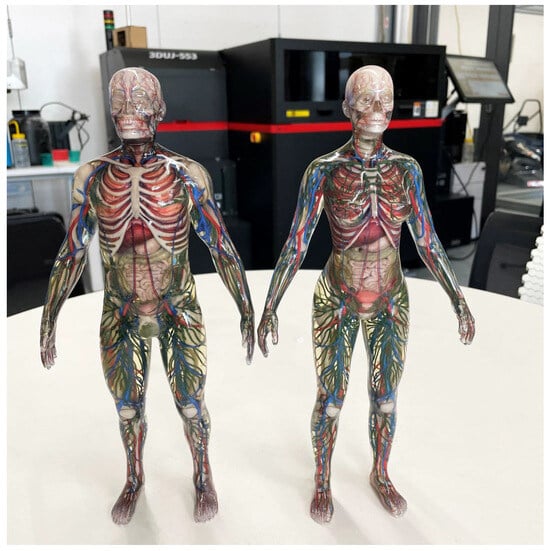
Figure 8.
A 3D-printed human body using inkjet printer for educational purposes.
The application and deeper understanding of full-color 3D printing, and how to apply it in ways that add true value, benefits all of engineering. But this example of using it to produce high-fidelity anatomical models can be of enormous benefit to the medical profession. It allows surgeons to use augmented 3D models to determine, and even practice performing, specific surgeries.
These 3D-printed models can display physical, spatial, and tactile information that computer models simply can’t provide. These can then also be used to help with the planning of patient-specific molds and surgical guides to allow for more accurate cuts, while implants can also be shaped to an exact replica of the anatomy prior to the surgical procedures. And these models can be used to aid more effective communication between the surgeon, their colleagues, and the patient.
3.3. Bone-Drilling Practice
As cadavers are becoming both expensive and harder to obtain, substitutes are needed to allow students to practice and learn the various skills they need. One such application is in bone-drilling practice, where nylon-printed bones, including their trabecular structures can be printed for medical students to practice honing their skills. This allows students easy access to an endless source of practice samples at relatively low costs.
The bone in Figure 9 is printed from a micro-CT scan of a real human bone and captures all the internal cavities and trabecular structures of the bone.

Figure 9.
Bone-drilling practice part made with powder bed fusion.
4. Applications of 3D Printing in the Medical Field
3D printing continues to find new and innovative applications in healthcare, transforming and enhancing lives in previously unimaginable ways. Its impact has been evident across a spectrum of medical disciplines, including but not limited to cardiothoracic surgery [46], cardiology [47], gastroenterology [48], neurosurgery [49], oral and maxillofacial surgery [14], ophthalmology [50], otolaryngology [51], orthopedic surgery [52], plastic surgery [53], podiatry [54], pulmonology [55], radiation oncology [56], transplant surgery [57], urology [58], and vascular surgery [59]. The diverse benefits of this technology have paved the way for various direct applications in the medical and clinical domain [60]:
- Utilized for personalized presurgical and treatment planning. Numerous studies have showcased the potential benefits of patient-specific presurgical planning [61,62,63,64,65,66]. Additionally, it allows the customization of prosthetics or surgical tools based on individual patient anatomy, enhancing the understanding of unique and complex anatomical structures in each case [64,65,66,67]. Moreover, 3D printing permits the accurate selection of prosthetic component sizes before implantation [68,69,70].
- Tailored surgical instruments and implants: This customization not only ensures precision but also reduces costs, attributed to the efficiency of additive-manufacturing techniques [71].
- Researching osteoporotic conditions enables a precise assessment of the patient’s bone condition, leading to informed decisions regarding surgical interventions [72].
- 3D printing facilitates the rapid prototyping of new design concepts or enhancements for existing medical devices, allowing for swift development and testing.
- 3D-printed patient-specific models have proven to enhance performance and accelerate learning, leading to improved knowledge, management, and confidence among trainees across various specialties [8,73]. The advantages of 3D printing in education include the reproducibility and safety of the 3D-printed models compared to cadaver dissection, the ability to model diverse physiological and pathological anatomy from extensive image datasets, and the potential to share 3D models among institutions, especially those with limited resources [74,75,76].
- Patient education is a crucial aspect of patient-centered care, and healthcare providers prioritize effective communication. Presenting imaging reports verbally or displaying CT and MRI scans to patients often falls short, as these 2D representations may not fully convey the complexities of 3D anatomy. In contrast, 3D printing offers a promising solution, enhancing doctor-patient communication by directly showcasing anatomical models [77,78].
- Enhancing Forensic Practices: Within legal proceedings, 3D models serve as invaluable tools to explain complex anatomical irregularities, bridging comprehension gaps that often arise with conventional cross-sectional imaging, especially for jury members [79].
- Bioprinting, an innovative application of 3D printing, facilitates the creation of implantable tissues. For instance, synthetic skin can be 3D printed and transplanted onto burn-injury patients, offering a groundbreaking solution for skin grafts [80]. Additionally, bioprinting finds utility in evaluating cosmetic, chemical, and pharmaceutical products through tissue testing [81].
- Personalized drug 3D printing involves layering powdered drugs to enhance their dissolution rate compared to conventional pills, ensuring faster absorption in the body [82]. This innovative approach not only accelerates drug delivery but also enables the customization of the required quantity according to individual patient needs, marking a significant advancement in pharmaceutical manufacturing [83]. We examine will further examine some case studies of these areas related to surgical planning in more detail below.
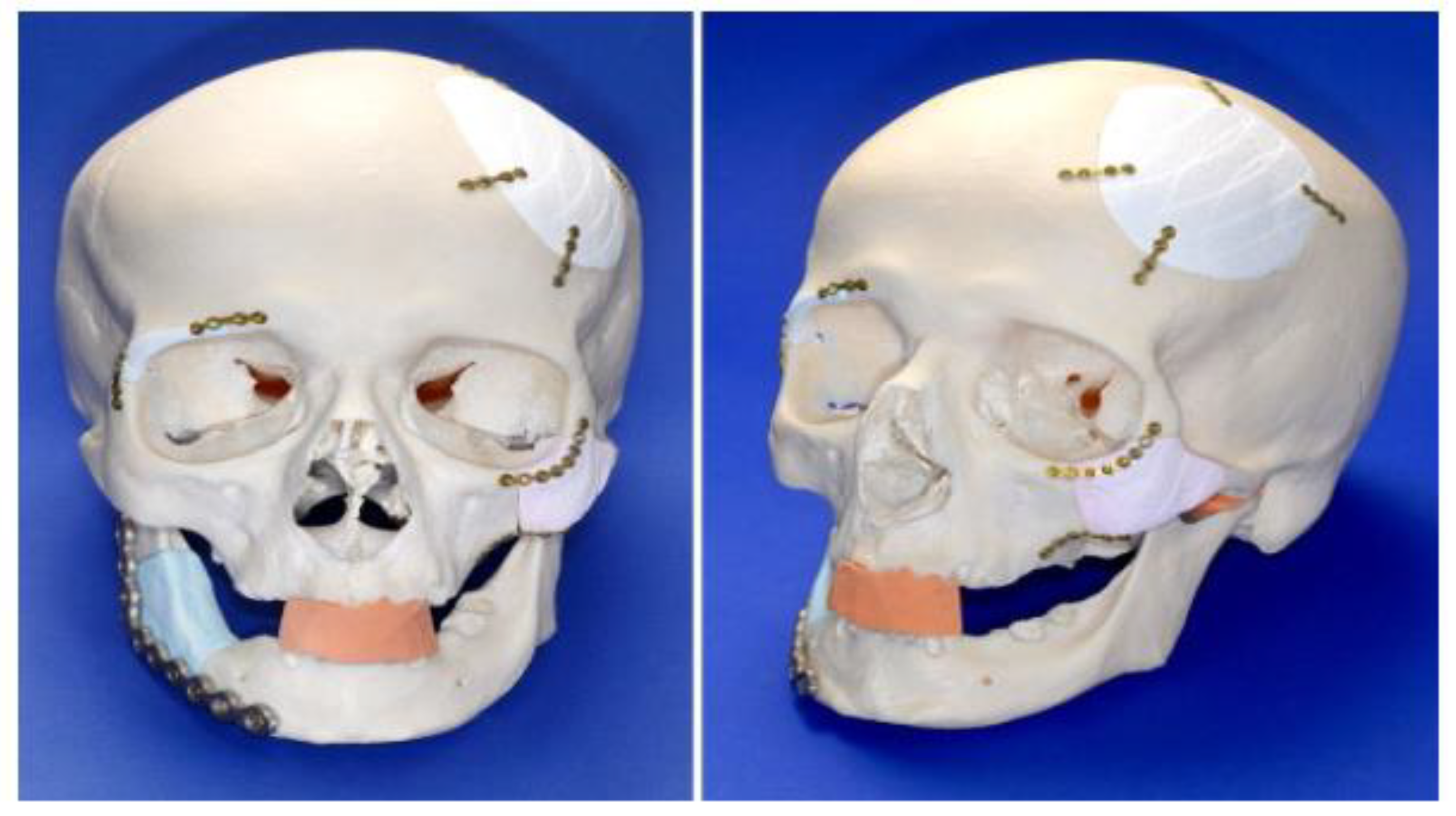
4.1. Surgical Practice and Implants
Anatomical models serve as molds for crafting prosthetics, exemplified in specific cranial and ear surgery cases. Additionally, personalized 3D-printed molds for prosthetics [84] have streamlined procedures like chin-augmentation surgery, reducing surgical duration and enhancing aesthetic outcomes due to precise profile matching. Additional research indicates that 3D-printing methods can directly produce final implants, notably prevalent in cranial surgery [85]. Custom cranial implants prove highly accurate, reducing operating-room time and correlating with improved clinical results across various studies.
Similarly, 3D-printed trays and fixation plates enhance medical outcomes and trim operation room time in maxillofacial surgery. A study [7] highlighted enhanced bone formation and angiogenesis with custom implants. Furthermore, complete dentures are also attainable through additive manufacturing, with results varying; some studies note slightly lower aesthetics for 3D-printed dentures, while others report aesthetics comparable to standard dentures, emphasizing the benefits of facial simulation before final prosthetic printing.
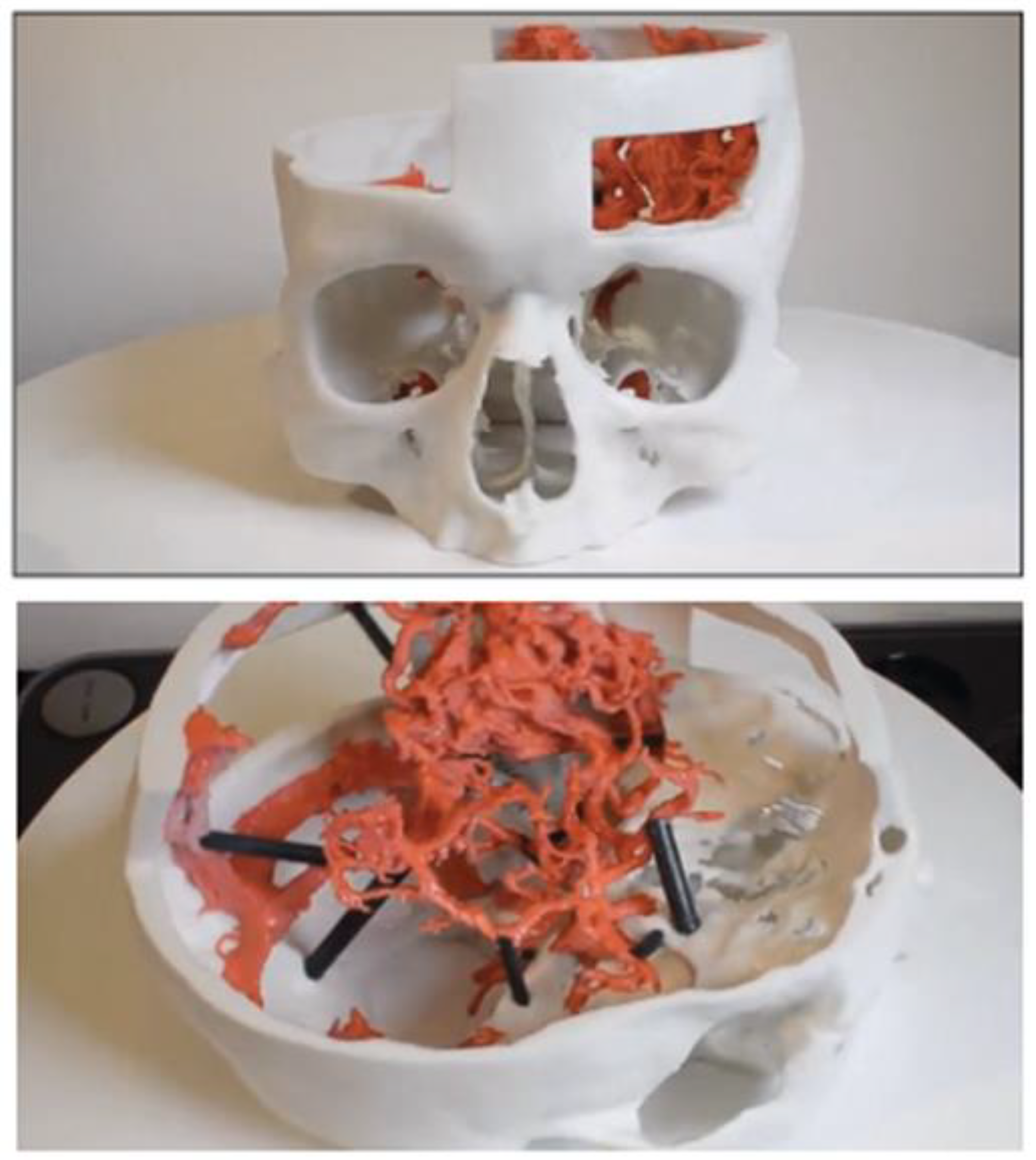
As a case study [86], a 43-year-old woman with a significant mandible defect initially underwent mandible reconstruction using an intraoperatively modeled reconstruction plate. However, this initial attempt failed due to asymmetrical mandibular contour, causing difficulties in jaw movement. The patient faced challenges in opening and closing her mouth, leading to saliva overflow, impaired oral food intake, and speech problems. To address these issues, a second surgical procedure was planned to involve a custom-designed implant. CT data were transferred to a CAD environment for implant design (Figure 10). Given the extent of the defect, reaching from the right condyle to the midline of the chin, a combination of mirror-imaging technique and another mandible was utilized as a template. The undamaged mandible was mirrored to the affected side, but due to the defect’s size exceeding the midline of the chin, additional scaling and templating from another mandible image was necessary to complete the implant contour design.
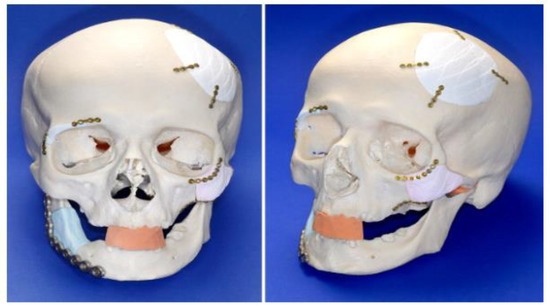
Figure 10.
Skull with 3D-printed embedded implants [86].
The designed implant was fabricated using stereolithography, creating an SLA model that served as a pattern for the titanium implant. The finalized implant was then forwarded to the maxillofacial department for the surgical procedure, as depicted in Figure 10.
4.2. Surgical Planning
Surgical procedures necessitate a deep understanding of human anatomy and the intricate relationships between various anatomical structures. Traditionally, this knowledge is imparted through the study of human cadavers in medical school’s preclinical studies and is further honed through practical experience during real surgeries [87]. Visualizations presented on 2D or 3D computer screens may not provide an intuitive grasp of complex anatomical intricacies [88,89] (see Figure 11). Moreover, the ability to practice both general surgical procedures and patient-specific techniques, especially in highly complex cases, enhances surgeons’ skills and outcomes [90].
Utilizing patient-specific scans to generate 3D models holds significant utility in various surgical and training contexts. Presently, PBF technologies for polymer and metal are considered the gold standard for surgical applications [91]. A study involving 158 students explored the pros and cons of 3D printing in surgery. Benefits highlighted encompass improved preoperative planning, model accuracy compared to the patient, and reduced surgery time [92]. Drawbacks include disparities between the 3D model and the patient’s physical condition, extended preoperative planning duration, and expenses related to printing machines and CAD software.
Across surgical specialties, 3D printing is revolutionizing the surgical process [93]. Surgeons employ 3D models to familiarize themselves with intricate structural abnormalities, enabling optimal surgical planning through rehearsal of complex procedures. This meticulous planning allows surgeons to anticipate and address potential issues in advance, potentially reducing surgery duration and errors. Despite the increased time invested in preoperative planning, it enhances surgeons’ skills and confidence before the actual procedure. In some instances, sterilized 3D models are brought into operating rooms to provide surgeons with enhanced visibility in challenging areas [92].
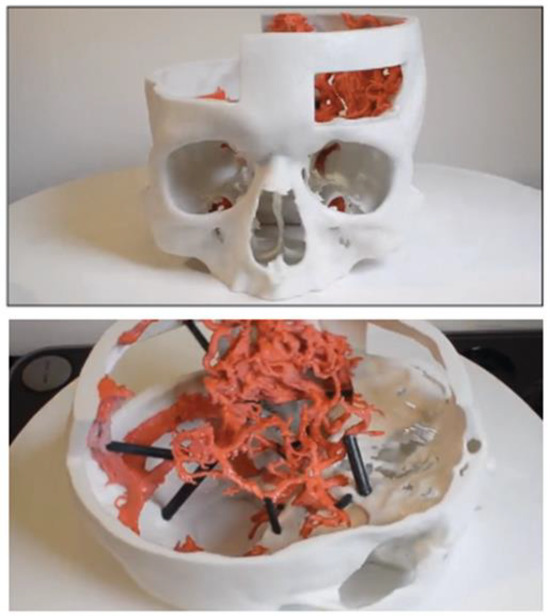
Figure 11.
Pre-surgical planning for neurosurgeons using a 3D-printed model [94].
Figure 11.
Pre-surgical planning for neurosurgeons using a 3D-printed model [94].
In interdisciplinary approaches, 3D-printed models facilitate shared understanding among medical teams, enabling patient absence during collaborative planning sessions. While the adoption of 3D printing in surgery is growing, the systematic review indicates limited efforts in in-house fabrication of customized implants or prostheses using 3D printing. This approach necessitates proficiency in CAD software, demanding additional skills, expertise, and time from the surgical team. Currently, radiological scans remain the most commonly used data for 3D-model printing.
Having a physical representation of a patient’s anatomy allows physicians to study and simulate surgeries more effectively compared to relying solely on 2D MRI or CT scans displayed on flat screens [95]. These models provide a tangible advantage over cadavers, which are often limited in availability and pose challenges in terms of cost [96]. Cadavers lack specific pathologies, offering more of an anatomy lesson than a realistic representation of a surgical case. Additionally, 3D models prove invaluable in studying complex spinal deformities. For training doctors in colonoscopies, high-quality 3D anatomical models, accurately representing specific pathologies, are essential, given the significance of colorectal cancer as the second leading cause of cancer-related deaths [73,96].
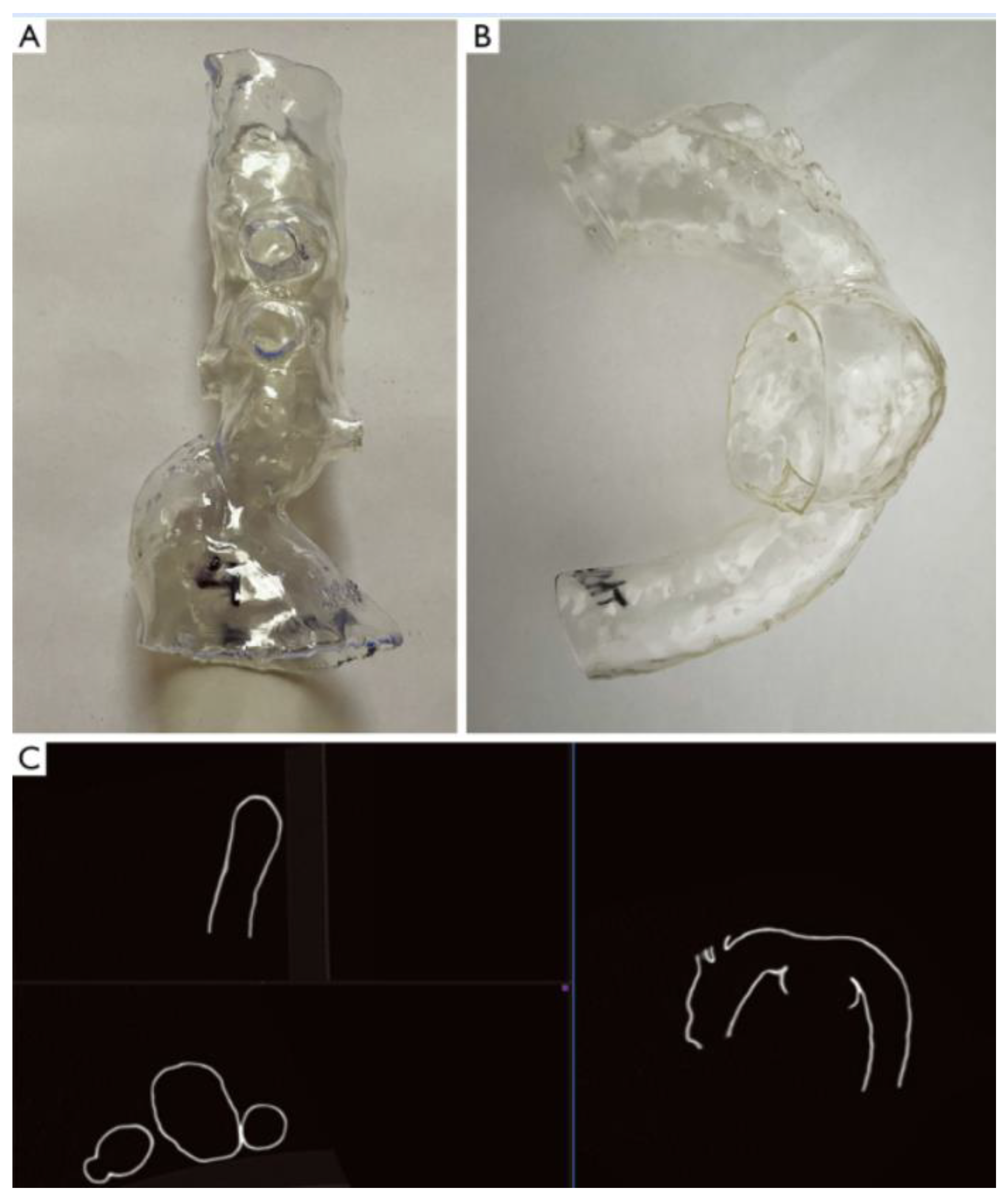
Neurosurgeons find 3D-printed neuroanatomical models particularly beneficial (Figure 12) [87,97,98], as they illuminate the complicated relationships among cranial nerves, vessels, cerebral structures, and skull architecture. These complexities are challenging to interpret using only 2D radiographic images, and even a small error in understanding this intricate anatomy could have severe consequences. Realistic 3D models depicting the relationship between a lesion and normal brain structures aid neurosurgeons in determining the safest surgical approach and allow for rehearsal of challenging cases.
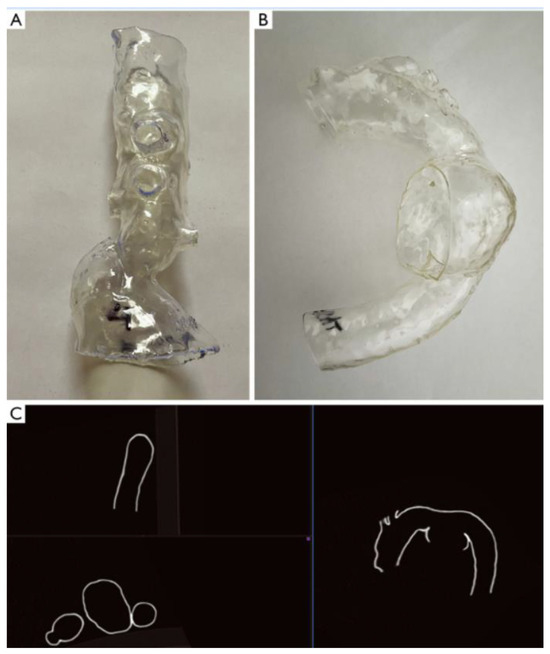
Figure 12.
Representative display of three-dimensionally printed aortic templates. A visceral template (A). An aortic arch template (B). Multiplanar reconstruction of CT-scanned aortic arch template (C) [87].
In another case study, 3D printing allowed surgeons to simulate procedures like endovascular stent implantation under conditions mimicking real tissues, eliminating any risk of patient complications [99,100,101,102].
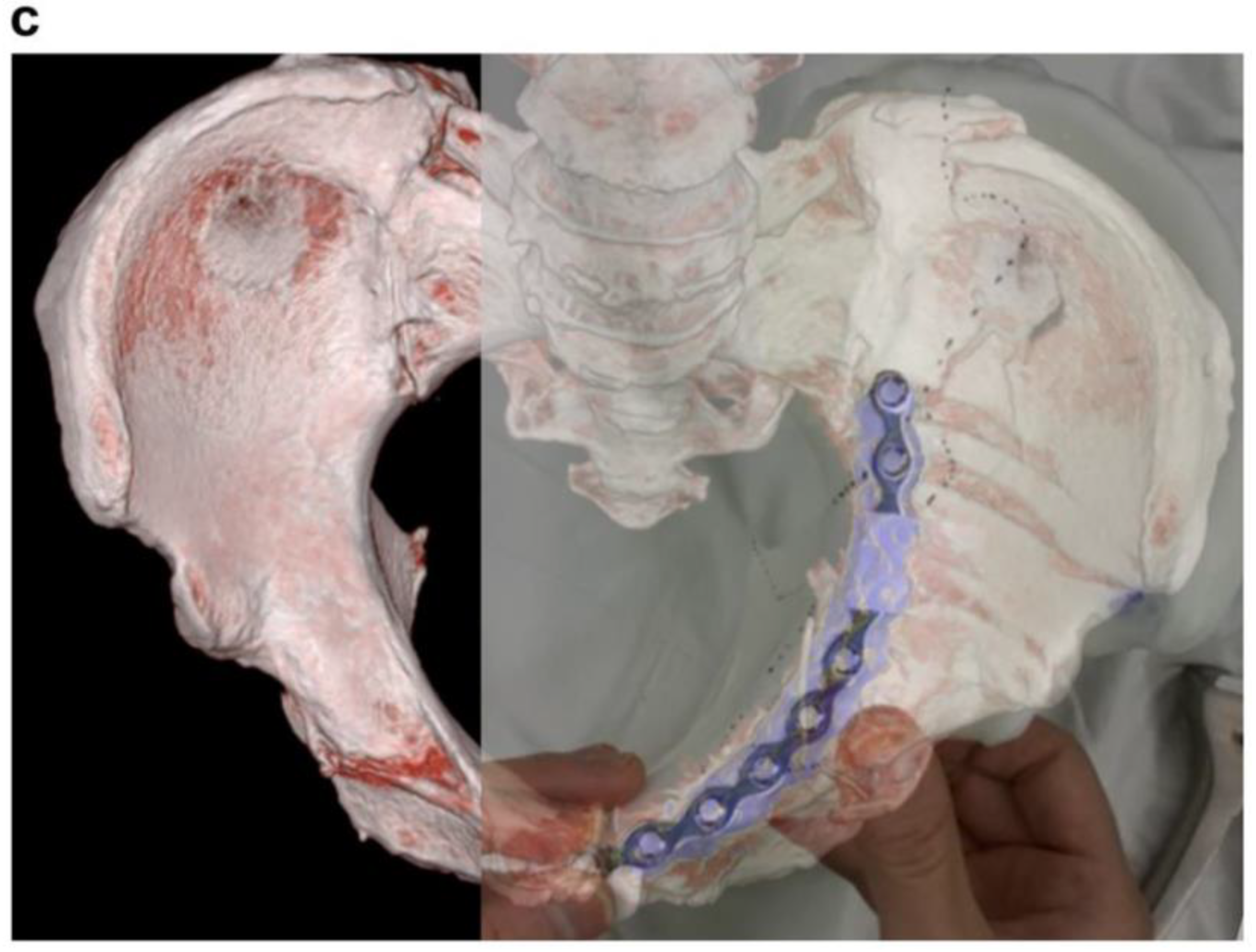
4.3. Surgical Plates and Pins
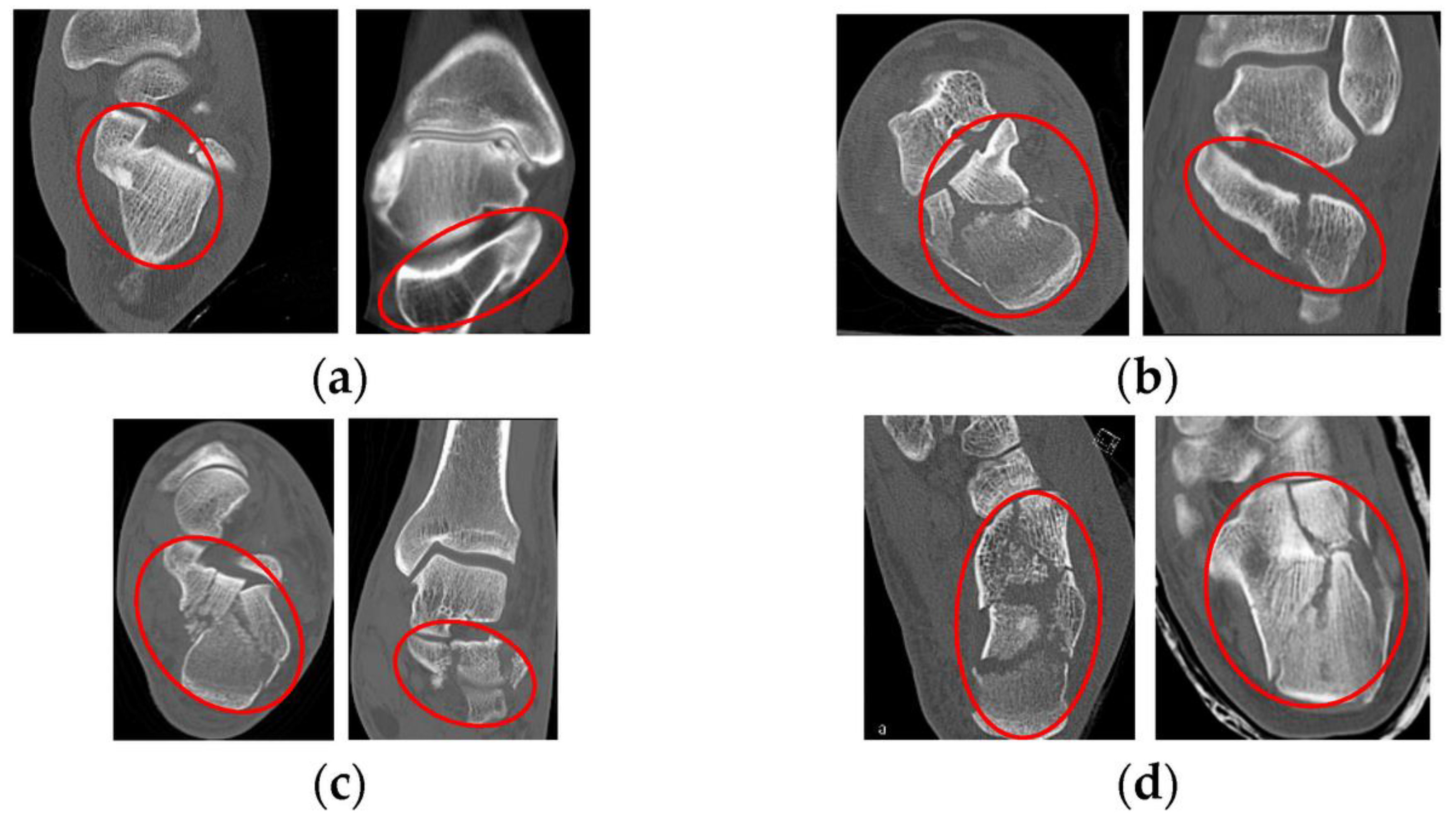
AM technology is also suitable for unilateral displaced intra-articular calcaneal fractures involving the posterior facet that require precise anatomic restoration. The contralateral unaffected calcaneus, devoid of any fractures, deformities, or surgical history, serves as a template for pre-shaping the plate before the surgery. It also acts as a guide for achieving anatomic reduction during the operation. It is important to note that Sanders type 4 calcaneal fractures may not be suitable for this minimally invasive approach. Additionally, fractures older than 3 weeks might pose challenges for reduction using this method [103]. Patients with a unilateral calcaneal fracture undergo a CT scan of both calcanei, with a slice thickness of 1 mm (see Figure 13).
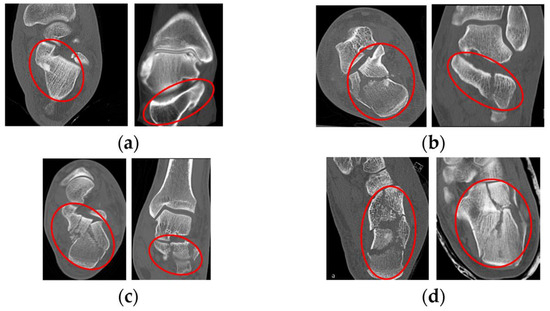
Figure 13.
The Sanders system of fracture classification on the calcaneus [1,2,49]: (a) Normal calcaneus in transverse and coronal images; (b) Type II; (c) Type III; and (d) Type IV [103].
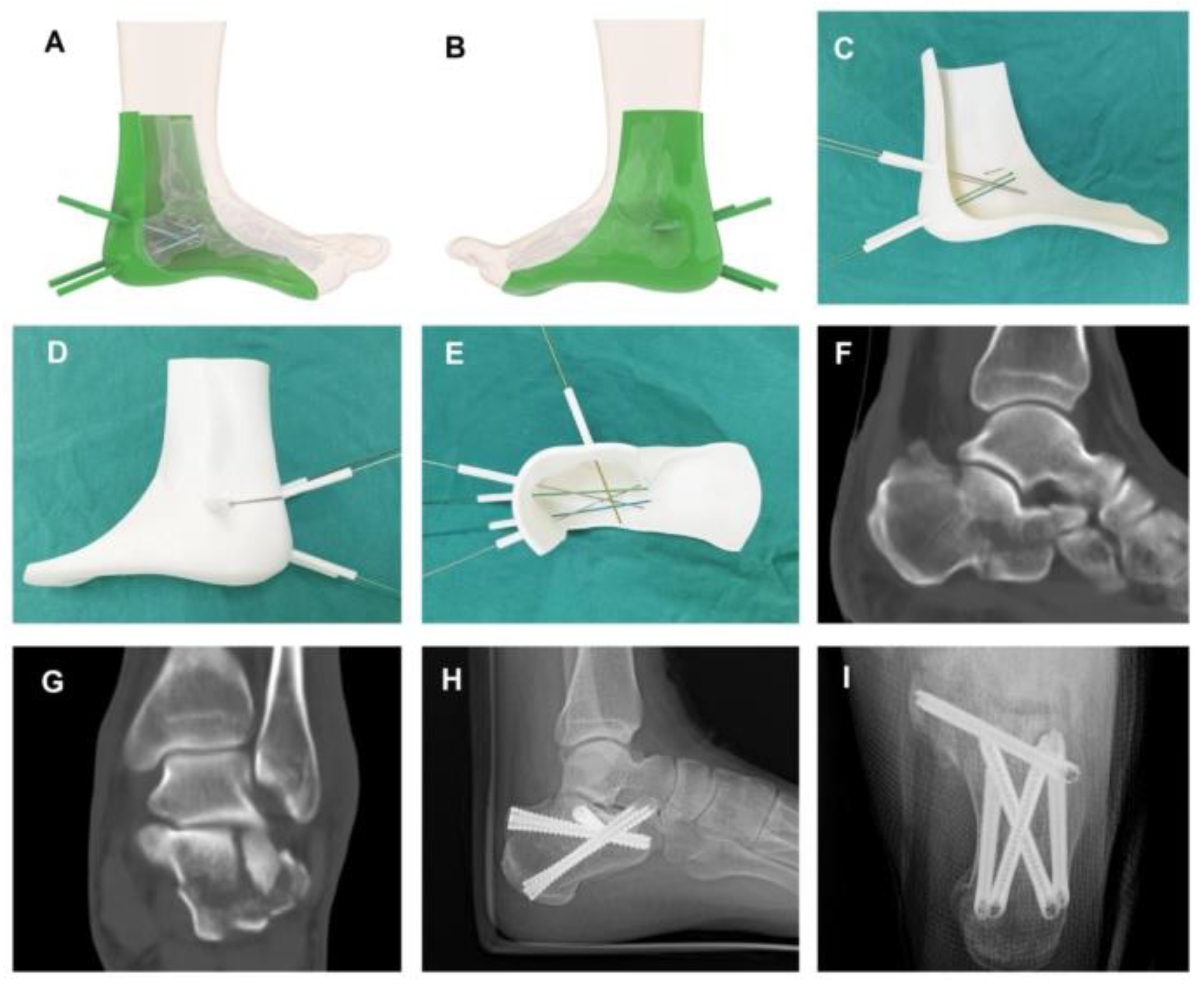
Utilizing the mirror-imaging technique, the normal side calcaneus is transformed into a model resembling the injured side’s calcaneus, likely similar to its pre-injury state (Figure 14). It takes approximately 3 h to print a 3D model using PBF polymer method.
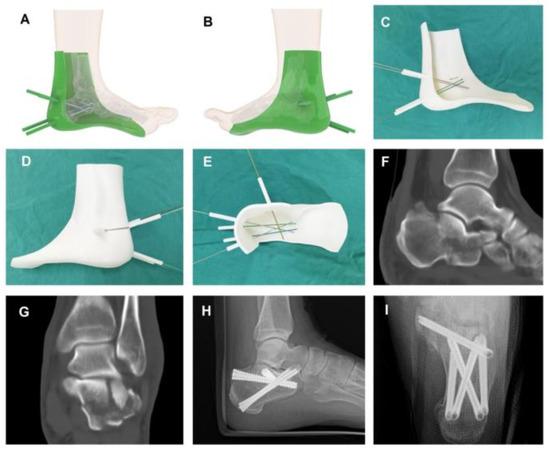
Figure 14.
The design, fabrication, and application of 3D-printed cast. (A,B) The reconstruction and design of 3D model based on CT data. (C–E) The 3D-printed cast with five cannulas for insertion of 1.5 mm K-wires. (F,G) CT images of a patient (male, 42 years of age) with displaced intra-articular calcaneal fracture, showing sustentaculum tali nondisplaced. (H,I) A fractured calcaneus treated with percutaneous reduction and 3D-printed cast assisted screw fixation [104].
The shape and size of the locking plate are chosen by attaching the plate to the real-size calcaneus model. Careful examination of plain radiographs and CT scans of the fractured calcaneus helps determine the correct position for the plate and which holes to use. For an AO Locking Calcaneal Plate, three proximal holes are cut—one each on the anterior, middle, and posterior portions—to allow the plate to smoothly advance through the small incision. The plate is bent to fit the model, securing the fracture fragments effectively (Figure 14).
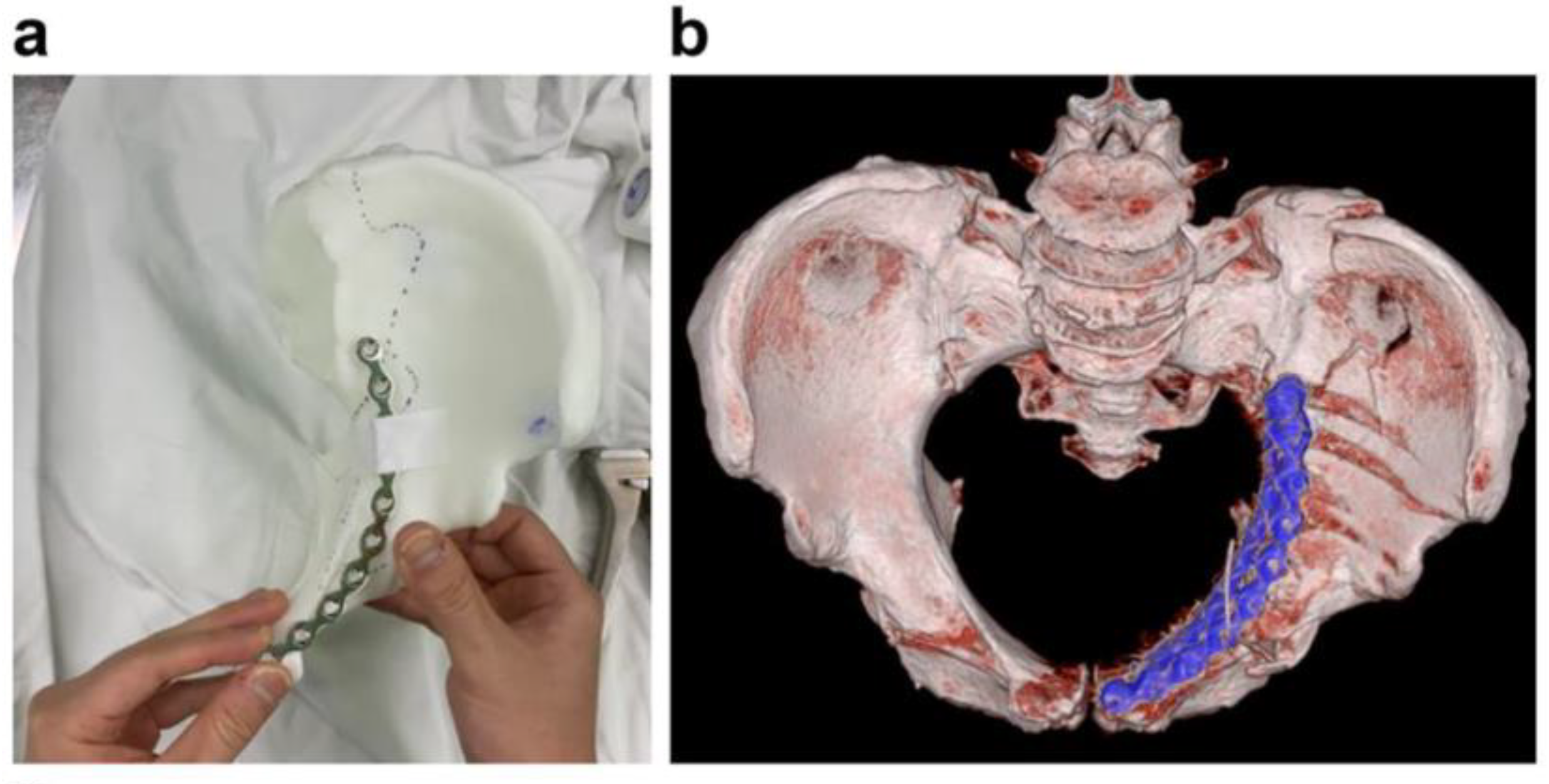
Fluoroscopic images are taken with the plate attached to the model to aid in deciding the plate’s proper position during its insertion through the incision (Figure 15-left). This can be done either before the operation or intraoperatively, just before inserting the plate through the incision. Both the pre-shaped locking plate and the 3D-printed model are sterilized before the surgery. The 3D-printed model serves as a reference for anatomical reduction of the fracture during the surgery.
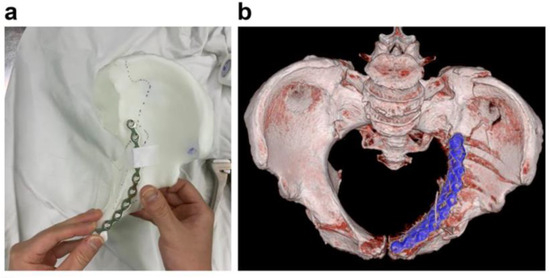
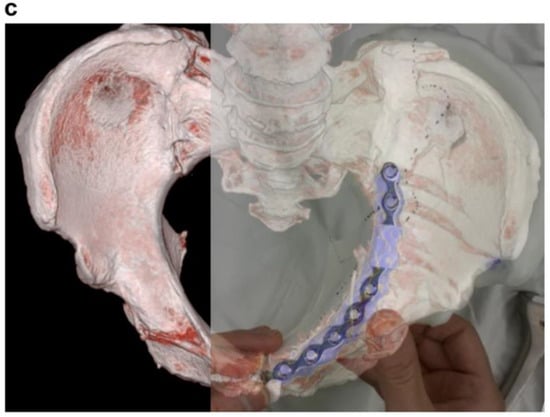
Figure 15.
Evaluation for anatomical mismatch of the pre-contoured plate. (a) Clinical photograph of the pre-contoured pelvic brim plate taped on the 3DP model. (b) Corresponding postoperative 3D-reconstructed view. (c) Superimposed photograph of (a,b) demonstrates no evidence of a mismatch [105].
During the procedure, the patient is positioned in the lateral decubitus position with a thigh tourniquet. Figure 15 shows such a procedure.
4.4. Drilling and Cutting Guides and Jigs
Another application of AM in medical field is using the 3D-printed guides for the drilling of bone. Thoracic pedicles, unlike those in the lumbar spine, have smaller diameters and show greater variability in size among individuals and between segments. Additionally, the thoracic spine is closely related to vital organs like the lungs, esophagus, aorta, and large blood vessels, making surgeries in this area delicate. Therefore, inserting thoracic pedicle screws demands extreme precision, as any deviation from the optimal position can lead to poor patient outcomes. Proper insertion within the pedicle, ensuring accurate positioning and orientation, is crucial before advancing to the vertebral body to guarantee safety and secure anchoring. Particularly, placing screws in the mid- and upper-thoracic region remains technically challenging [106,107]. Figure 16 illustrates the design of the navigational jig for the operation.
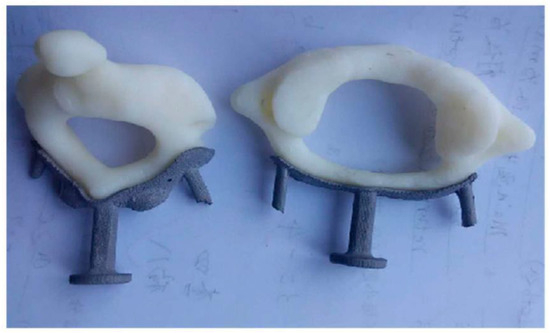
Figure 16.
Fitting of the metal template to the FDM-printed cervical vertebra model [108].
To enhance the precision and safety of thoracic pedicle screw placement, several techniques have been devised and tested in both cadaveric and clinical studies. In this case, the application of templates designed for cervical spine anatomy had not been assessed for the more complex thoracic spine. To address this gap, a straightforward, secure, and efficient method was developed to assist in the insertion of thoracic pedicle screws. This technique leveraged the concepts of reverse engineering and rapid prototyping. The experimental results show that the operational accuracy increases from 75% to 95% by using drilling jigs [108].
In another scenario, the use of a drilling jig is paramount to prevent potential damages. Drilling into the spine is inherently challenging, with significant risks of complications, including neurological and vascular issues due to improperly placed pedicle screws. Such misplacements could compromise the implants’ pull-out strength and escalate the risk of implant failure [109,110]. Therefore, ensuring accurate and safe screw placement within the pedicle is vital, especially in scoliosis surgery.
5. Discussion
The review presented herein underscores the transformative impact of AM in the fields of surgical planning and medical education within the healthcare sector. The widespread adoption of AM technologies has not only revolutionized the creation and customization of medical devices but has also significantly augmented the efficacy of clinical products [17,18,19]. The capacity of AM to facilitate intricate surgical planning and enhance educational practices is evident in its multifaceted applications.
One of the primary contributions of AM in healthcare is its pivotal role in surgical planning [20]. The ability of surgeons to practice and refine operative techniques using 3D-printed models contributes to a substantial reduction in operational risk and time [21,22]. The tangible and three-dimensional representation of anatomical structures allows surgeons to gain confidence in their procedures before entering the operating room [23]. Additionally, and the capacity to create patient-specific implants through AM ensures a higher degree of precision and compatibility, leading to improved surgical outcomes [24,25].
The educational arena has also witnessed a paradigm shift with the integration of AM [26,27,28]. The creation of detailed and accurate 3D models of human anatomy has become an invaluable tool for teaching both students and experienced medical professionals. AM facilitates a hands-on learning experience and enables a deeper understanding of complex anatomical structures [29]. These 3D models serve as effective visual aids, enhancing the comprehension of medical concepts and promoting better retention of knowledge among learners [30,31,32].
Despite the remarkable advancements, challenges persist in the field of AM in healthcare [33]. Issues such as insufficient mechanical properties in 3D printing, the imperative to scale up production for mass manufacturing, the development of intelligent printable biomaterials, and the intricate task of vascularization in 3D bioprinting pose ongoing hurdles [34,35,36,37,38]. Addressing these challenges will require innovative solutions and collaborative efforts between researchers and clinicians and industry stakeholders.
Looking ahead, it is evident that the healthcare sector is on the cusp of witnessing novel paradigms in AM technologies [39,40]. The continued exploration of specialized biomaterials, coupled with advancements in design adaptability and functional integration, is poised to redefine the landscape of clinical products [41,42]. Intelligent solutions to overcome current limitations will likely pave the way for a more widespread and impactful integration of AM in healthcare [43,44,45].
Finally, the transformative influence of AM in surgical planning and medical education is signaling a promising trajectory for the future of healthcare. As the field continues to evolve, addressing current challenges and embracing innovative solutions will be imperative for unlocking the full potential of AM technologies in enhancing patient care and medical education.
6. Conclusions
In conclusion, this comprehensive review illuminates the profound impact of additive manufacturing (AM) on the landscape of healthcare, portraying it as a cornerstone technology shaping the future of medical device production. The examination of AM technologies reveals a significant leap forward in the creation and customization of medical devices, amplifying their efficacy within clinical settings. The strategic integration of specialized biomaterials through AM emerges as a pivotal aspect, not only fostering superior functional integration but also affording an unprecedented degree of design adaptability. This adaptability, in turn, optimizes the development of clinical products, tailoring them to meet specific patient needs with precision. However, as the review depicts these advancements, it also sheds light on persistent challenges that demand innovative solutions. The limitations, posed by insufficient mechanical properties in 3D printing, the imperative need to scale up AM production for mass manufacturing, the ongoing quest for intelligent printable biomaterials, and the intricate task of vascularization in 3D bioprinting, form a complex tapestry of obstacles. It is in navigating these challenges that the true potential of AM in healthcare lies.
The analysis presented in this review serves not only as a comprehensive snapshot of the current state of AM technologies in healthcare but also as a roadmap for future trends in the sector. It underscores the critical importance of addressing these challenges head on, sparking innovation to overcome existing limitations. As the healthcare sector navigates these hurdles, this article foresees the emergence of novel paradigms in AM technologies, unlocking unprecedented possibilities for the future of healthcare manufacturing.
Author Contributions
Conceptualization, A.K., O.D., F.I.T.P., M.I. and T.G.; methodology, H.A.; software, H.A.; validation, A.K., O.D. and F.I.T.P.; formal analysis, H.A.; investigation, A.K., O.D., H.A., I.S.M. and L.M.U.; resources, A.K. and H.A.; writing—original draft preparation, H.A., S.C. and A.K.; writing—review and editing, A.K., O.D., F.I.T.P., M.I. and T.G.; visualization, A.K.; supervision, A.K., O.D., F.I.T.P., M.I. and T.G.; project administration, A.K. and O.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Berman, B. 3-D printing: The new industrial revolution. Bus. Horiz. 2012, 55, 155–162. [Google Scholar] [CrossRef]
- Hull, C.W. Apparatus for Production of Three-Dimensional Objects by Stereolithography. U.S. Patent Appl. Filed 638905, 8 August 1984. [Google Scholar]
- Wohlers, T.T.; Campbell, I.; Diegel, O.; Huff, R.; Kowen, J. Wohlers Report 2023: 3D Printing and Additive Manufacturing Global State of the Industry; Wohlers Associates: Fort Collins, CO, USA, 2023; ISBN 9781622049660. [Google Scholar]
- Shi, S.; Jiang, Y.; Ren, H.; Deng, S.; Sun, J.; Cheng, F.; Jing, J.; Chen, Y. 3D-Printed Carbon-Based Conformal Electromagnetic Interference Shielding Module for Integrated Electronics. Nanomicro Lett. 2024, 16, 85. [Google Scholar] [CrossRef]
- Jiang, Y.; Xu, Y.; Deng, S.; Ren, H.; Tao, X.; Liao, M.; Sun, J.; Shi, S. 3D Printing of Ultralight MWCNT@OCNF Porous Scaffolds for High-Efficiency Electromagnetic Interference Shielding. Carbohydr. Polym. 2023, 314, 120945. [Google Scholar] [CrossRef]
- Shi, S.; Zhou, D.; Jiang, Y.; Cheng, F.; Sun, J.; Guo, Q.; Luo, Y.; Chen, Y.; Liu, W. Lightweight Zn-Philic 3D-Cu Scaffold for Customizable Zinc Ion Batteries. Adv. Funct. Mater. 2024, 2312664. [Google Scholar] [CrossRef]
- Petrescu, R.V.V.; Petrescu, F.I.T. The Current Stage in Aerospace at the End of 2020. Indep. J. Manag. Prod. 2022, 13, 405–478. [Google Scholar] [CrossRef]
- Wurm, G.; Tomancok, B.; Pogady, P.; Holl, K.; Trenkler, J. Cerebrovascular stereolithographic biomodeling for aneurysm surgery. J. Neurosurg. 2004, 100, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Ghomi, E.R.; Khosravi, F.; Neisiany, R.E.; Singh, S.; Ramakrishna, S. Future of additive manufacturing in healthcare. Curr. Opin. Biomed. Eng. 2021, 17, 100255. [Google Scholar] [CrossRef]
- D’Urso, P.S.; Thompson, R.G.; Atkinson, R.; Weidmann, M.J.; Redmond, M.J.; I Hall, B.; Jeavons, S.J.; Benson, M.D.; Earwaker, W.S. Cerebrovascular biomodelling: A technical note. Surg. Neurol. 1999, 52, 490–500. [Google Scholar] [CrossRef]
- Reiss, S.; Thielmann, J.; Fischer, J.; Lottner, T.; Maier, A.; Westermann, D.; Mühlen, C.V.Z.; Heidt, T.; Bock, M. Combination of High Resolution MRI with 3D-Printed Needle Guides for Ex Vivo Myocardial Biopsies. Sci. Rep. 2024, 14, 606. [Google Scholar] [CrossRef]
- Seoane-Viaño, I.; Pérez-Ramos, T.; Liu, J.; Januskaite, P.; Guerra-Baamonde, E.; González-Ramírez, J.; Vázquez-Caruncho, M.; Basit, A.W.; Goyanes, A. Visualizing Disintegration of 3D Printed Tablets in Humans Using MRI and Comparison with in Vitro Data. J. Control. Release 2024, 365, 348–357. [Google Scholar] [CrossRef] [PubMed]
- File:Example-of-3D-Whole-Heart-Models-Manufactured-by-Means-of-3D-Printing-Showing-a-Normal-Heart-from-a-Healthy-Control-for.Jpg. Available online: https://commons.wikimedia.org/wiki/File:Example-of-3D-whole-heart-models-manufactured-by-means-of-3D-printing-showing-a-normal-heart-from-a-healthy-control-for.jpg (accessed on 4 March 2024).
- Valls-Esteve, A.; Tejo-Otero, A.; Lustig-Gainza, P.; Buj-Corral, I.; Fenollosa-Artés, F.; Rubio-Palau, J.; de la Torre, I.B.-M.; Munuera, J.; Fondevila, C.; Krauel, L. Patient-Specific 3D Printed Soft Models for Liver Surgical Planning and Hands-On Training. Gels 2023, 9, 339. [Google Scholar] [CrossRef]
- Krauel, L.; Valls-Esteve, A.; Tejo-Otero, A.; Fenollosa-Artés, F. 3D-Printing in Surgery: Beyond Bone Structures. A Review. Ann. 3D Print. Med. 2021, 4, 100039. [Google Scholar] [CrossRef]
- Kantaros, A.; Ganetsos, T. From Static to Dynamic: Smart Materials Pioneering Additive Manufacturing in Regenerative Medicine. Int. J. Mol. Sci. 2023, 24, 15748. [Google Scholar] [CrossRef]
- Petsiuk, A.; Lavu, B.; Dick, R.; Pearce, J.M. Waste Plastic Direct Extrusion Hangprinter. Inventions 2022, 7, 70. [Google Scholar] [CrossRef]
- Seoane-Viaño, I.; Otero-Espinar, F.J.; Goyanes, Á. 3D Printing of Pharmaceutical Products. In Additive Manufacturing; Elsevier: Amsterdam, The Netherlands, 2021; pp. 569–597. [Google Scholar]
- Boretti, A. A Perspective on 3D Printing in the Medical Field. Ann. 3D Print. Med. 2024, 13, 100138. [Google Scholar] [CrossRef]
- Betancourt, M.C.; Araújo, C.; Marín, S.; Buriticá, W. The Quantitative Impact of Using 3D Printed Anatomical Models for Surgical Planning Optimization: Literature Review. 3D Print. Addit. Manuf. 2023, 10, 1130–1139. [Google Scholar] [CrossRef]
- Langdon, C.; Hinojosa-Bernal, J.; Munuera, J.; Gomez-Chiari, M.; Haag, O.; Veneri, A.; Valldeperes, A.; Valls, A.; Adell, N.; Santamaria, V.; et al. 3D Printing as Surgical Planning and Training in Pediatric Endoscopic Skull Base Surgery—Systematic Review and Practical Example. Int. J. Pediatr. Otorhinolaryngol. 2023, 168, 111543. [Google Scholar] [CrossRef]
- Kantaros, A.; Ganetsos, T.; Piromalis, D. 3D and 4D Printing as Integrated Manufacturing Methods of Industry 4.0. Am. J. Eng. Appl. Sci. 2023, 16, 12–22. [Google Scholar] [CrossRef]
- Rath, S.N.; Sankar, S. 3D Printers for Surgical Practice. In 3D Printing in Medicine; Elsevier: Amsterdam, The Netherlands, 2023; pp. 127–147. ISBN 9780323898317. [Google Scholar]
- Kantaros, A.; Ganetsos, T. Integration of Cyber-Physical Systems, Digital Twins and 3D Printing in Advanced Manufacturing: A Synergistic Approach. Am. J. Eng. Appl. Sci. 2024, 17, 1–22. [Google Scholar] [CrossRef]
- Assink, N.; Oldhoff, M.G.E.; ten Duis, K.; Kraeima, J.; Doornberg, J.N.; Witjes, M.J.H.; de Vries, J.-P.P.M.; Meesters, A.M.L.; IJpma, F.F.A. Development of Patient-Specific Osteosynthesis Including 3D-Printed Drilling Guides for Medial Tibial Plateau Fracture Surgery. Eur. J. Trauma Emerg. Surg. 2023, 50, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Chytas, D.; Salmas, M.; Demesticha, T.; Troupis, T. Three-dimensional Printing in Anatomy Education: Is It Similarly Useful for Teaching of All Anatomical Regions and Structures? Anat. Sci. Educ. 2023, 16, 5–6. [Google Scholar] [CrossRef]
- Nguyen, P.; Stanislaus, I.; McGahon, C.; Pattabathula, K.; Bryant, S.; Pinto, N.; Jenkins, J.; Meinert, C. Quality Assurance in 3D-Printing: A Dimensional Accuracy Study of Patient-Specific 3D-Printed Vascular Anatomical Models. Front. Med. Technol. 2023, 5, 1097850. [Google Scholar] [CrossRef] [PubMed]
- Antreas, K.; Piromalis, D. Employing a Low-Cost Desktop 3D Printer: Challenges, and How to Overcome Them by Tuning Key Process Parameters. Int. J. Mech. Appl. 2021, 10, 11–19. [Google Scholar] [CrossRef]
- Antonowicz, A.; Wojtas, K.; Makowski, Ł.; Orciuch, W.; Kozłowski, M. Particle Image Velocimetry of 3D-Printed Anatomical Blood Vascular Models Affected by Atherosclerosis. Materials 2023, 16, 1055. [Google Scholar] [CrossRef]
- Ramirez, M.E.; Pena, I.R.; Castillo, R.E.B.; Sufianov, A.; Goncharov, E.; Sanchez, J.A.S.; Colome-Hidalgo, M.; Nurmukhametov, R.; Céspedes, J.R.C.; Montemurro, N. Development of a 3D Printed Brain Model with Vasculature for Neurosurgical Procedure Visualisation and Training. Biomedicines 2023, 11, 330. [Google Scholar] [CrossRef]
- Miao, H.; Ding, J.; Gong, X.; Zhao, J.; Li, H.; Xiong, K.; Zhou, X.; Liu, W.; Wu, F. Application of 3D-Printed Pulmonary Segment Specimens in Experimental Teaching of Sectional Anatomy. BMC Surg. 2023, 23, 109. [Google Scholar] [CrossRef]
- Moiduddin, K.; Mian, S.H.; Umer, U.; Alkhalefah, H.; Ahmed, F.; Hashmi, F.H. Design, Analysis, and 3D Printing of a Patient-Specific Polyetheretherketone Implant for the Reconstruction of Zygomatic Deformities. Polymers 2023, 15, 886. [Google Scholar] [CrossRef]
- Patel, P.; Dhal, K.; Gupta, R.; Tappa, K.; Rybicki, F.J.; Ravi, P. Medical 3D Printing Using Desktop Inverted Vat Photopolymerization: Background, Clinical Applications, and Challenges. Bioengineering 2023, 10, 782. [Google Scholar] [CrossRef]
- Kantaros, A.; Soulis, E.; Petrescu, F.I.T.; Ganetsos, T. Advanced Composite Materials Utilized in FDM/FFF 3D Printing Manufacturing Processes: The Case of Filled Filaments. Materials 2023, 16, 6210. [Google Scholar] [CrossRef] [PubMed]
- Kantaros, A.; Giannatsis, J.; Karalekas, D. A novel strategy for the incorporation of optical sensors in Fused Deposition Modeling parts. In Proceedings of the International Conference on Advanced Manufacturing Engineering and Technologies, Stockholm, Sweden, 27–30 October 2013; Universitets Service US AB, KTH Royal Institite of Technology: Stockholm, Sweden, 2013. ISBN 978-91-7501-893-5. Available online: https://www.researchgate.net/publication/269631461_A_novel_strategy_for_the_incorporation_of_optical_sensors_in_FDM_parts (accessed on 15 February 2023).
- Paxton, N.C.; Luposchainsky, S.; Reizabal, A.; Saiz, P.G.; Bade, S.; Woodruff, M.A.; Dalton, P.D. Manufacture of Biomimetic Auricular Surgical Implants Using 3D Printed High Density Polyethylene Microfibers. Adv. Mater. Technol. 2024, 9, 2301190. [Google Scholar] [CrossRef]
- Negrescu, A.-M.; Mocanu, A.-C.; Miculescu, F.; Mitran, V.; Constantinescu, A.-E.; Cimpean, A. In Vitro Studies on 3D-Printed PLA/HA/GNP Structures for Bone Tissue Regeneration. Biomimetics 2024, 9, 55. [Google Scholar] [CrossRef]
- Gabriel, E.; Olejnik, A.; Sztorch, B.; Frydrych, M.; Czerwińska, O.; Pietrzak, R.; Przekop, R.E. Application of L-FDM Technology to the Printing of Tablets That Release Active Substances—Preliminary Research. C 2024, 10, 23. [Google Scholar] [CrossRef]
- Kantaros, A.; Ganetsos, T.; Piromalis, D. 4D Printing: Technology Overview and Smart Materials Utilized. J. Mechatron. Robot. 2023, 7, 1–14. [Google Scholar] [CrossRef]
- Aversa, R.; Petrescu, F.I.T.; Petrescu, R.V.V.; Apicella, A. Biofidel FEA Modeling of Customized Hybrid Biological Hip Joint Prostheses, Part I: Biomechanical Behavior of Implanted Femur. Am. J. Biochem. Biotechnol. 2016, 12, 270–276. [Google Scholar] [CrossRef]
- Syed, J.; Dharrab, A.A.; Zafa, M.S.; Khand, E.; Aversa, R.; Petrescu, R.V.V.; Apicella, A.; Petrescu, F.I.T. Influence of Curing Light Type and Staining Medium on the Discoloring Stability of Dental Restorative Composite. Am. J. Biochem. Biotechnol. 2017, 13, 42–50. [Google Scholar] [CrossRef][Green Version]
- Lunguţ, E.F.; Matei, L.; Roşu, M.M.; Iliescu, M.; Radu, C. Biomechanical Hand Prosthesis Design. Machines 2023, 11, 964. [Google Scholar] [CrossRef]
- Lunguţ, E.F.; Radu Frenț, C.; Roşu, M.M.; Vlădăreanu, L.; Iliescu, M.; Matei, L. Rapid Prototyping Techniques for Innovative Hand Prosthesis. In Mechanisms and Machine Science; Springer Nature Switzerland: Cham, Switzerland, 2023; pp. 386–393. ISBN 9783031324451. [Google Scholar]
- Zhou, Y.; Riding, P.; Eccleston, K.; Tan, A.; Anton, E.; Platt, I.; Bateman, C.J.; Nelson, J.; Diegel, O. Additive Manufacturing of Human Torso Phantom for Microwave Imaging. In Proceedings of the 2022 IEEE Conference on Antenna Measurements and Applications (CAMA), Guangzhou, China, 14–17 December 2022; IEEE: Piscataway, NJ, USA, 2022; pp. 1–3. [Google Scholar]
- Sztorch, B.; Głowacka, J.; Romanczuk-Ruszuk, E.; Brząkalski, D.; Marciniec, B.; Przekop, R.E. High Flexural Modulus of PLA Composites for FDM 3D Printing Using Multifunctional Octaspherosilicates. Res. Sq. 2023. [Google Scholar] [CrossRef]
- Kurenov, S.N.; Ionita, C.; Sammons, D.; Demmy, T.L. Three-dimensional printing to facilitate anatomic study, device development, simulation, and planning in thoracic surgery. J. Thorac. Cardiovasc. Surg. 2015, 149, 973–979. [Google Scholar] [CrossRef] [PubMed]
- Vukicevic, M.; Mosadegh, B.; Min, J.K.; Little, S.H. Cardiac 3D printing and its future directions. JACC Cardiovasc. Imaging 2017, 10, 171–184. [Google Scholar] [CrossRef]
- Jeon, H.; Kang, K.; Park, S.A.; Kim, W.D.; Paik, S.S.; Lee, S.-H.; Jeong, J.; Choi, D. Generation of multilayered 3D structures of HepG2 cells using a bio-printing technique. Gut Liver 2017, 11, 121. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Yang, Y.; Yang, Z.; Ma, R.; Aimaijiang, M.; Xu, J.; Zhang, Y.; Zhou, Y. Four-Dimensional Printing and Shape Memory Materials in Bone Tissue Engineering. Int. J. Mol. Sci. 2023, 24, 814. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.; Zhang, X. 3D printing: Print the future of ophthalmology. Invest. Ophthalmol. Vis. Sci. 2014, 55, 5380–5381. [Google Scholar] [CrossRef] [PubMed]
- Crafts, T.D.; Ellsperman, S.E.; Wannemuehler, T.J.; Bellicchi, T.D.; Shipchandler, T.Z.; Mantravadi, A.V. Three-dimensional printing and its applications in otorhinolaryngology–head and neck surgery. Otolaryngol. Neck Surg. 2017, 156, 999–1010. [Google Scholar] [CrossRef] [PubMed]
- Auricchio, F.; Marconi, S. 3D printing: Clinical applications in orthopaedics and traumatology. EFORT Open Rev. 2016, 1, 121. [Google Scholar] [CrossRef] [PubMed]
- Chae, M.P.; Rozen, W.M.; McMenamin, P.G.; Findlay, M.W.; Spychal, R.T.; Hunter-Smith, D.J. Emerging applications of bedside 3D printing in plastic surgery. Front. Surg. 2015, 2, 25. [Google Scholar] [CrossRef] [PubMed]
- Williams, C.; James, A.; Chae, M.P.; Hunter-Smith, D.J. 3D printing in clinical podiatry: A pilot study and review. J. Foot Ankle Res. 2015, 8, 1. [Google Scholar] [CrossRef]
- Guibert, N.; Mhanna, L.; Didier, A.; Moreno, B.; Leyx, P.; Plat, G.; Mazieres, J.; Hermant, C. Integration of 3D printing and additive manufacturing in the interventional pulmonologist’s toolbox. Respir. Med. 2018, 134, 139–142. [Google Scholar] [CrossRef]
- Su, S.; Moran, K.; Robar, J.L. Design and production of 3D printed bolus for electron radiation therapy. J. Appl. Clin. Med. Phys. 2014, 15, 194–211. [Google Scholar] [CrossRef]
- Zein, N.N.; Hanouneh, I.A.; Bishop, P.D.; Samaan, M.; Eghtesad, B.; Quintini, C.; Miller, C.; Yerian, L.; Klatte, R. Three-dimensional print of a liver for preoperative planning in living donor liver transplantation. Liver Transplant. 2013, 19, 1304–1310. [Google Scholar] [CrossRef]
- Soliman, Y.; Feibus, A.H.; Baum, N. 3D printing and its urologic applications. Rev. Urol. 2015, 17, 20. [Google Scholar]
- Hangge, P.; Pershad, Y.; Witting, A.A.; Albadawi, H.; Oklu, R. Three-dimensional (3D) printing and its applications for aortic diseases. Cardiovasc. Diagn. Ther. 2018, 8 (Suppl. S1), S19. [Google Scholar] [CrossRef]
- Ballard, D.H.; Trace, A.P.; Ali, S.; Hodgdon, T.; Zygmont, M.E.; DeBenedectis, C.M.; Smith, S.E.; Richardson, M.L.; Patel, M.J.; Decker, S.J.; et al. Clinical applications of 3D printing: Primer for radiologists. Acad. Radiol. 2018, 25, 52–65. [Google Scholar] [CrossRef]
- Perica, E.; Sun, Z. Patient-specific three-dimensional printing for pre-surgical planning in hepatocellular carcinoma treatment. Quant. Imaging Med. Surg. 2017, 7, 668. [Google Scholar] [CrossRef]
- Wong, K.C. 3D-printed patient-specific applications in orthopedics. Orthop. Res. Rev. 2016, 8, 57–66. [Google Scholar] [CrossRef]
- Costello, J.P.; Olivieri, L.J.; Su, L.; Krieger, A.; Alfares, F.; Thabit, O.; Marshall, M.B.; Yoo, S.-J.; Kim, P.C.; Jonas, R.A.; et al. Incorporating three-dimensional printing into a simulation-based congenital heart disease and critical care training curriculum for resident physicians. Congenit. Heart Dis. 2015, 10, 185–190. [Google Scholar] [CrossRef]
- Frame, M.; Huntley, J.S. Rapid prototyping in orthopaedic surgery: A user’s guide. Sci. World J. 2012, 2012, 838575. [Google Scholar] [CrossRef] [PubMed]
- Mahaisavariya, B.; Sitthiseripratip, K.; Oris, P.; Tongdee, T. Rapid prototyping model for surgical planning of corrective osteotomy for cubitus varus: Report of two cases. Inj. Extra 2006, 37, 176–180. [Google Scholar] [CrossRef]
- Sheth, U.; Theodoropoulos, J.; Abouali, J. Use of 3-dimensional printing for preoperative planning in the treatment of recurrent anterior shoulder instability. Arthrosc. Tech. 2015, 4, e311–e316. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.-T.; Yang, X.-J.; Yan, B.; Zeng, T.-H.; Qiu, Y.-Y.; Chen, S.-J. Clinical application of three-dimensional printing in the personalized treatment of complex spinal disorders. Chin. J. Traumatol. 2016, 19, 31–34. [Google Scholar] [CrossRef] [PubMed]
- Hosny, A.; Dilley, J.D.; Kelil, T.; Mathur, M.; Dean, M.N.; Weaver, J.C.; Ripley, B. Pre-procedural fit-testing of TAVR valves using parametric modeling and 3D printing. J. Cardiovasc. Comput. Tomogr. 2019, 13, 21–30. [Google Scholar] [CrossRef]
- Vaishya, R.; Vijay, V.; Vaish, A.; Agarwal, A.K. Computed tomography based 3D printed patient specific blocks for total knee replacement. J. Clin. Orthop. Trauma 2018, 9, 254–259. [Google Scholar] [CrossRef]
- Chen, X.; Possel, J.K.; Wacongne, C.; Van Ham, A.F.; Klink, P.C.; Roelfsema, P.R. 3D printing and modelling of customized implants and surgical guides for non-human primates. J. Neurosci. Methods 2017, 286, 38–55. [Google Scholar] [CrossRef]
- De La Peña, A.; De La Peña-Brambila, J.; La Torre, J.P.-D.; Ochoa, M.; Gallardo, G.J. Low-cost customized cranioplasty using a 3D digital printing model: A case report. 3D Print. Med. 2018, 4, 4. [Google Scholar] [CrossRef]
- Dodziuk, H. Applications of 3D printing in healthcare. Kardiochirurgia I Torakochirurgia Pol. J. Thorac. Cardiovasc. Surg. 2016, 13, 283–293. [Google Scholar] [CrossRef]
- Khaled, S.A.; Burley, J.C.; Alexander, M.R.; Roberts, C.J. Desktop 3D printing of controlled release pharmaceutical bilayer tablets. Int. J. Pharm. 2014, 461, 105–111. [Google Scholar] [CrossRef]
- Walker, V. Implementing a 3D printing service in a biomedical library. J. Med. Libr. Assoc. JMLA 2017, 105, 55. [Google Scholar] [CrossRef] [PubMed]
- Lim, K.H.A.; Loo, Z.Y.; Goldie, S.J.; Adams, J.W.; McMenamin, P.G. Use of 3D printed models in medical education: A randomized control trial comparing 3D prints versus cadaveric materials for learning external cardiac anatomy. Anat. Sci. Educ. 2016, 9, 213–221. [Google Scholar] [CrossRef] [PubMed]
- Barbon, S.; Biccari, A.; Stocco, E.; Capovilla, G.; D’angelo, E.; Todesco, M.; Sandrin, D.; Bagno, A.; Romanato, F.; Macchi, V.; et al. Bio-Engineered Scaffolds Derived from Decellularized Human Esophagus for Functional Organ Reconstruction. Cells 2022, 11, 2945. [Google Scholar] [CrossRef] [PubMed]
- Andolfi, C.; Plana, A.; Kania, P.; Banerjee, P.P.; Small, S. Usefulness of three-dimensional modeling in surgical planning, resident training, and patient education. J. Laparoendosc. Adv. Surg. Tech. 2017, 27, 512–515. [Google Scholar] [CrossRef] [PubMed]
- Bernhard, J.-C.; Isotani, S.; Matsugasumi, T.; Duddalwar, V.; Hung, A.J.; Suer, E.; Baco, E.; Satkunasivam, R.; Djaladat, H.; Metcalfe, C.; et al. Personalized 3D printed model of kidney and tumor anatomy: A useful tool for patient education. World J. Urol. 2016, 34, 337–345. [Google Scholar] [CrossRef]
- Baier, W.; Warnett, J.M.; Payne, M.; Williams, M.A. Introducing 3D printed models as demonstrative evidence at criminal trials. J. Forensic Sci. 2018, 63, 1298–1302. [Google Scholar] [CrossRef]
- He, P.; Zhao, J.; Zhang, J.; Li, B.; Gou, Z.; Gou, M.; Li, X. Bioprinting of skin constructs for wound healing. Burn. Trauma 2018, 6, 5. [Google Scholar] [CrossRef] [PubMed]
- Zhou, G.; Jiang, H.; Yin, Z.; Liu, Y.; Zhang, Q.; Zhang, C.; Pan, B.; Zhou, J.; Zhou, X.; Sun, H.; et al. In vitro regeneration of patient-specific ear-shaped cartilage and its first clinical application for auricular reconstruction. EBioMedicine 2018, 28, 287–302. [Google Scholar] [CrossRef]
- Konta, A.A.; García-Piña, M.; Serrano, D.R. Personalised 3D printed medicines: Which techniques and polymers are more successful? Bioengineering 2017, 4, 79. [Google Scholar] [CrossRef]
- Kantaros, A.; Ganetsos, T.; Petrescu, F.I.T. Transforming Object Design and Creation: Biomaterials and Contemporary Manufacturing Leading the Way. Biomimetics 2024, 9, 48. [Google Scholar] [CrossRef]
- Munoz-Guijosa, J.M.; Martínez, R.Z.; Cendrero, A.M.; Lantada, A.D. Rapid Prototyping of Personalized Articular Orthoses by Lamination of Composite Fibers upon 3D-Printed Molds. Materials 2020, 13, 939. [Google Scholar] [CrossRef]
- Li, Z.; Lu, M.; Zhang, Y.; Wang, J.; Wang, Y.; Gong, T.; He, X.; Luo, Y.; Zhou, Y.; Min, L.; et al. Intercalary Prosthetic Reconstruction with Three-dimensional-printed Custom-made Porous Component for Defects of Long Bones with Short Residual Bone Segments after Tumor Resection. Orthop. Surg. 2024, 16, 374–382. [Google Scholar] [CrossRef]
- Meyer-Szary, J.; Luis, M.S.; Mikulski, S.; Patel, A.; Schulz, F.; Tretiakow, D.; Fercho, J.; Jaguszewska, K.; Frankiewicz, M.; Pawłowska, E.; et al. The Role of 3D Printing in Planning Complex Medical Procedures and Training of Medical Professionals—Cross-Sectional Multispecialty Review. Int. J. Environ. Res. Public Health 2022, 19, 3331. [Google Scholar] [CrossRef] [PubMed]
- Rynio, P.; Wojtuń, M.; Wójcik, Ł.; Kawa, M.; Falkowski, A.; Gutowski, P.; Kazimierczak, A. The Accuracy and Reliability of 3D Printed Aortic Templates: A Comprehensive Three-Dimensional Analysis. Quant. Imaging Med. Surg. 2022, 12, 1385–1396. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.S.; Hansgen, A.R.; Wink, O.; Quaife, R.A.; Carroll, J.D. Rapid prototyping: A new tool in understanding and treating structural heart disease. Circulation 2008, 117, 2388–2394. [Google Scholar] [CrossRef]
- Suzuki, M.; Ogawa, Y.; Kawano, A.; Hagiwara, A.; Yamaguchi, H.; Ono, H. Rapid prototyping of temporal bone for surgical training and medical education. Acta Otolaryngol. 2004, 124, 400–402. [Google Scholar] [CrossRef]
- Knox, K.; Kerber, C.W.; Singel, S.A.; Bailey, M.J.; Imbesi, S.G. Rapid prototyping to create vascular replicas from CT scan data: Making tools to teach, rehearse, and choose treatment strategies. Catheter. Cardiovasc. Interv. 2005, 65, 47–53. [Google Scholar] [CrossRef]
- Malik, H.H.; Darwood, A.R.; Shaunak, S.; Kulatilake, P.; El-Hilly, A.A.; Mulki, O.; Baskaradas, A. Three-dimensional printing in surgery: A review of current surgical applications. J. Surg. Res. 2015, 199, 512–522. [Google Scholar] [CrossRef]
- Martelli, N.; Serrano, C.; van den Brink, H.; Pineau, J.; Prognon, P.; Borget, I.; El Batti, S. Advantages and disadvantages of 3-dimensional printing in surgery: A systematic review. Surgery 2016, 159, 1485–1500. [Google Scholar] [CrossRef]
- Hughes, B.; Wilson, G. 3D/additive printing manufacturing: A brief history and purchasing guide. Technol. Eng. Teach. 2015, 75, 18. [Google Scholar]
- Kantaros, A. Bio-Inspired Materials: Exhibited Characteristics and Integration Degree in Bio-Printing Operations. Am. J. Eng. Appl. Sci. 2022, 15, 255–263. [Google Scholar] [CrossRef]
- Liu, K.; Fang, K.; Chen, W.; Zhang, C.; Sun, L.; Zhu, J. Hydroxyethyl methyl cellulose controls the diffusion behavior of pico-liter scale ink droplets on silk to improve inkjet printing performance. Int. J. Biol. Macromol. 2023, 224, 1252–1265. [Google Scholar] [CrossRef] [PubMed]
- Banks, J. Adding value in additive manufacturing: Researchers in the United Kingdom and Europe look to 3D printing for customization. IEEE Pulse 2013, 4, 22–26. [Google Scholar] [CrossRef] [PubMed]
- Klein, G.T.; Lu, Y.; Wang, M.Y. 3D printing and neurosurgery--ready for prime time? World Neurosurg. 2013, 80, 233–235. [Google Scholar] [CrossRef] [PubMed]
- Singare, S.; Dichen, L.; Bingheng, L.; Zhenyu, G.; Yaxiong, L. Customized design and manufacturing of chin implant based on rapid prototyping. Rapid Prototyp. J. 2005, 11, 113–118. [Google Scholar] [CrossRef]
- Kalejs, M.; von Segesser, L.K. Rapid prototyping of compliant human aortic roots for assessment of valved stents. Interact. Cardiovasc. Thorac. Surg. 2009, 8, 182–186. [Google Scholar] [CrossRef] [PubMed]
- Bruyere, F.; Leroux, C.; Brunereau, L.; Lermusiaux, P. Rapid prototyping model for percutaneous nephrolithotomy training. J. Endourol. 2008, 22, 91–96. [Google Scholar] [CrossRef] [PubMed]
- Sulaiman, A.; Boussel, L.; Taconnet, F.; Serfaty, J.M.; Alsaid, H.; Attia, C.; Huet, L.; Douek, P. In vitro non-rigid life-size model of aortic arch aneurysm for endovascular prosthesis assessment. Eur. J. Cardio-Thorac. Surg. 2008, 33, 53–57. [Google Scholar] [CrossRef] [PubMed]
- Armillotta, A.; Bonhoeffer, P.; Dubini, G.; Ferragina, S.; Migliavacca, F.; Sala, G.; Schievano, S. Use of rapid prototyping models in the planning of percutaneous pulmonary valved stent implantation. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2007, 221, 407–416. [Google Scholar] [CrossRef] [PubMed]
- Rahmaniar, W.; Wang, W.-J. Real-Time Automated Segmentation and Classification of Calcaneal Fractures in CT Images. Appl. Sci. 2019, 9, 3011. [Google Scholar] [CrossRef]
- Song, Q.; Li, T.; Xia, H.; Li, Y.; Feng, C.; Lin, Y.; Wang, H.; Hu, J.; Jiang, Q. Three-Dimensional Printed Cast Assisted Screw Fixation of Calcaneal Fractures: A Prospective Study. BMC Musculoskelet. Disord. 2023, 24, 802. [Google Scholar] [CrossRef]
- Sakong, S.-Y.; Cho, J.-W.; Kim, B.-S.; Park, S.-J.; Lim, E.-J.; Oh, J.-K. The Clinical Efficacy of Contouring Periarticular Plates on a 3D Printed Bone Model. J. Pers. Med. 2023, 13, 1145. [Google Scholar] [CrossRef]
- Panjabi, M.M.; O’holleran, J.D.; Crisco, J.J.; Kothe, R. Complexity of the thoracic spine pedicle anatomy. Eur. Spine J. 1997, 6, 19–24. [Google Scholar] [CrossRef]
- Vaccaro, A.R.; Rizzolo, S.J.; Balderston, R.A.; Allardyce, T.J.; Garfin, S.R.; Dolinskas, C.; An, H.S. Placement of pedicle screws in the thoracic spine. Part II: An anatomical and radiographic assessment. JBJS 1995, 77, 1200–1206. [Google Scholar] [CrossRef]
- Wang, D.; Wang, Y.; Wang, J.; Song, C.; Yang, Y.; Zhang, Z.; Lin, H.; Zhen, Y.; Liao, S. Design and Fabrication of a Precision Template for Spine Surgery Using Selective Laser Melting (SLM). Materials 2016, 9, 608. [Google Scholar] [CrossRef] [PubMed]
- Lu, S.; Zhang, Y.Z.; Wang, Z.; Shi, J.H.; Chen, Y.B.; Xu, X.M.; Xu, Y.Q. Accuracy and efficacy of thoracic pedicle screws in scoliosis with patient-specific drill template. Med. Biol. Eng. Comput. 2012, 50, 751–758. [Google Scholar] [CrossRef] [PubMed]
- Lu, S.; Xu, Y.Q.; Chen, G.P.; Zhang, Y.Z.; Lu, D.; Chen, Y.B.; Shi, J.H.; Xu, X.M. Efficacy and accuracy of a novel rapid prototyping drill template for cervical pedicle screw placement. Comput. Aided Surg. 2011, 16, 240–248. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).