Abstract
Neuroscience and biological evidence emphasizes the profound influence of natural light on human health, offering benefits such as reducing fatigue, heightened alertness in healthcare providers, and improving patient outcomes. The objective of this review is to identify scientific studies and research to evaluate and report evidence of indoor lighting conditions’ influence on health outcomes, which can be used to develop lighting designs that align circadian rhythms in healthcare settings. A comprehensive search was conducted to identify rigorous empirical studies focused on the link between interior lighting conditions with health outcomes in the healthcare environment. For a comprehensive review of the existing literature, a four-phased methodology was employed including literature search, screening, and selection. Literature appraisals were conducted to determine the relevance and quality of evidence for each study identified. In addition, using a thematic analysis, patterns were identified, analyzed, and interpreted within the literature review. Accordingly, the results were organized into two main groups interventional human subjects and simulation-based studies. Despite evidence that natural light influences human health and happiness, a synthesis of reviewed studies suggests that the evidence for the benefits of artificial lighting in healthcare settings is less conclusive, with potential factors including variations in lighting design, inconsistent implementation of lighting interventions, and differing sample populations across studies. We conclude with an executive summary suggesting that future research should use standardized metrics and methods to focus on bridging the gap between theoretical understanding and practical application in lighting design for healthcare environments. Collaboration among architects, designers, lighting experts, and healthcare professionals can address these factors contributing to building a stronger evidence-based design for the benefits of artificial lighting in healthcare settings.
1. Introduction
Light plays a vital role in human life, extending beyond its significance for basic vision. Light profoundly influences various aspects of our lives, including our overall well-being, mood, creativity, and cognitive abilities [1,2]. In addition, researchers are increasingly interested in understanding how light affects human health, particularly its effect on the circadian system [1].
All life evolved under 24 h solar days with dark nights (<0.3 lux) and bright days (>10,000 lux). During the course of the evolution of life, these solar days were internalized in virtually all species of plants and animals [3]. The internal 24 h cycles are approximate, and these so-called circadian rhythms are driven by self-sustaining circadian clocks that require exposure to relatively bright light at daytime to synchronize (entrain) internal rhythms to the external environment [2,4]. Nevertheless, modern interior environments tend to be significantly dimmer at daytime and brighter at nighttime compared to the natural environment in which our ancestors evolved [5]. The recognition of the discrepancy between the optimal functioning of our circadian rhythms and its impact on our health and well-being is growing [5,6,7]. As a result, there is a growing understanding of the need to address this issue. The goal of this review is to highlight lighting design opportunities that can be used to enhance circadian hygiene within healthcare settings. Table 1 is the graphical process of this review paper.

Table 1.
Graphical process of this paper.
There has been a significant amount of research published exploring how lighting designs may impact circadian health in recent years. Lighting design interventions and indoor circadian hygiene have rarely been reviewed and discussed to identify and collect evidence about their association. Understanding the health effects of lighting conditions in healthcare settings is crucial, as lighting plays a pivotal role in creating environments that not only support patient healing but also enhance staff performance, improve safety, and contribute to overall well-being. This comprehensive review considers the physiological, psychological, and practical aspects of healthcare facility design and operation. Furthermore, the research identifies and addresses issues and shortages related to implementing lighting designs and interventions to support health and well-being within healthcare facilities. By doing so, this study aims to contribute insights that can inform future developments in lighting systems tailored to the unique needs of healthcare environments.
This review aims to identify interventions in lighting conditions and the potential effects on health outcomes in healthcare settings. Lighting intervention is a broad concept in this study, including using dynamic, blue-depleted, and bio-adaptive lighting systems, as well as other lighting interventions intended to influence health. This literature review will address the following questions: (1) What can previous studies and research tell us about the effects of interior lighting conditions in healthcare environments? (2) Would improving lighting conditions increase the safety and health of healthcare workers and patients? (3) Is there scientifically conceivable evidence that interior lighting conditions improve clinical outcomes and staff health status? (4) What insights can be gained regarding effective methodologies for assessing the effects of interior lighting conditions on health outcomes and staff well-being in healthcare settings?
2. Background
2.1. Circadian Clocks and Rhythms
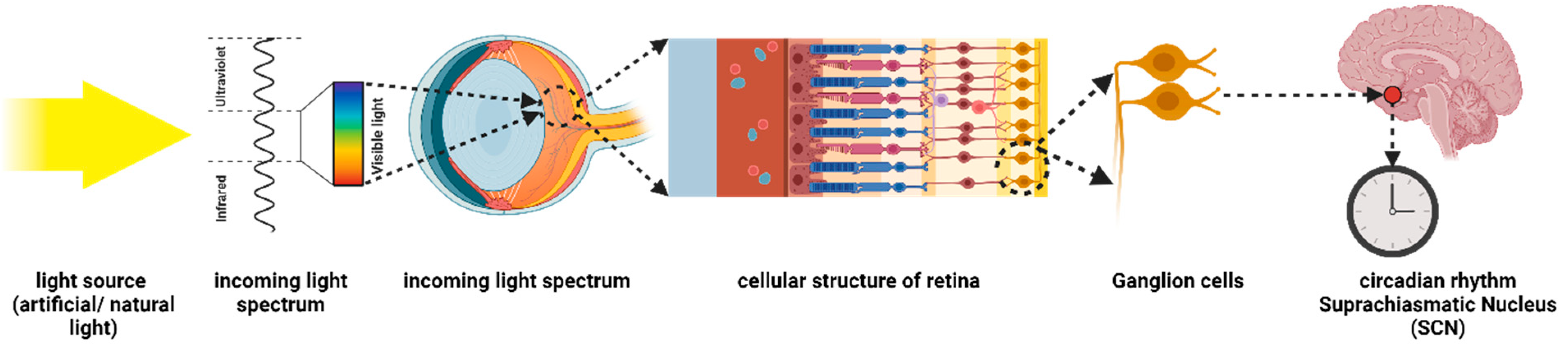
A circadian cycle is a series of processes occurring approximately every 24 h, which is derived from the Latin words “circa” and “diem” meaning about and day, respectively [2]. The circadian system is regulated by a central biological clock in the hypothalamic suprachiasmatic nucleus (SCN). Different physiological and behavioral processes are coordinated through it on a 24 h basis cycle [2,8]. Environmental cues, primarily light, stimulate the circadian clock. It is through the intrinsically photosensitive retinal ganglion cells (ipRGCs) located in the eye that light information is transmitted to the central clock in the SCN. These cells contribute specifically to the regulation of the circadian system as well as non-image-forming functions [9,10]. ipRGCs regulate circadian rhythms by releasing the photopigment called melanopsin [11,12]. Their photoreceptors are specifically sensitive to short-wavelength (blue) light, which makes them distinct from rods and cones that mediate visual perception [12,13]. ipRGCs are essential for synchronizing the circadian rhythm to the external cycles of day and night, which is vital for maintaining a healthy sleep–wake patterns and circadian balance [9,12,13] (Figure 1).
Figure 1.
Schematic diagram of the retina photoreceptors: the retina at the back of the eye with a variety of cells, including ipRGCs (intrinsically photosensitive retinal ganglion cells), adapted from [14,15].
The widespread use of artificial lighting over the past century has introduced a new phenomenon, known as artificial light at night (ALAN), to human beings, which was absent throughout our evolutionary history [1,8]. During the early 20th century, when artificial electric lighting became widespread, the natural balance between light and darkness rapidly deteriorated. The transition from incandescent lighting to fluorescent lighting marked a significant milestone, offering improved efficiency and longer-lasting illumination compared to traditional options [16,17]. Subsequently, the development of LED lighting further revolutionized the industry by providing even greater energy efficiency, durability, and design flexibility. These lighting innovations have empowered architects and designers to explore new frontiers in shaping and enhancing architectural spaces, opening up a realm of possibilities for creative and dynamic lighting designs. The advancements in lighting technology have not only improved energy efficiency but have also contributed to the aesthetic and functional aspects of architectural environments [18,19]. However, these modern lighting advances have led to an increased uncoupling of internal circadian rhythms from the external environment driven mainly by ALAN exposure. Indeed, a significant majority (>80%) of humans no longer have the opportunity to experience naturally dark nights due to the constant presence of ALAN [20]. This disruption of the light–dark cycle has profound implications for our biological rhythms and represents a significant departure from the natural light environment under which humans have evolved for millennia [20]. The loss of dark nights is expected to increase further in the coming years. Globally, exposure to ALAN is expanding at a rate of approximately 2% annually, driven by factors such as global population growth, urbanization, and industrialization [21].
2.2. Circadian Hygiene in Healthcare Settings
Disruption of natural light–dark cycles can lead to various physiological and behavioral changes, including sleep disturbances, fatigue, mood alterations, and impaired cognitive function [22]. The prevalence of ALAN has also influenced human lifestyle patterns, particularly with the rise of industrialization [8]. This has led to the increased necessity of night shift work in occupations such as firefighting and healthcare, where round-the-clock operations are required. These changes in work schedules further contribute to the disruption of the circadian rhythm [7,22].
Night shift healthcare workers play a critical role in healthcare settings by providing continuous care, responding to emergencies, monitoring patients, assisting with procedures, and ensuring patient comfort and well-being throughout the night [23]. It is essential to implement measures that support the physical and mental health of these night shift staff [24]. However, designing lighting systems in healthcare spaces can be challenging due to the diverse chronobiological requirements of different individuals [25,26]. Healthcare facilities encompass various functional areas, including patient rooms and nurse stations. Patients require dark and quiet nighttime environments to facilitate healing, whereas night shift staff require well-lit spaces to optimize their circadian synchronization with their inverted sleep/wake cycles [22,24]. Balancing these contrasting institutional lighting needs is crucial for creating a suitable environment that promotes both patient recovery and staff well-being.
Among the wide range of lighting strategies and designs, circadian lighting is designed to positively affect human circadian system by sending appropriately timed signals to the central clock in the brain [27,28,29]. In healthcare settings, the design of circadian lighting aims to synchronize the lighting environment with the natural circadian rhythm. This approach is intended to enhance patient outcomes and staff performance by maximizing the therapeutic and restorative properties of healthcare spaces [25,28]. Specifically, a healthy lighting design for nurses during night shifts considers their need for alertness and cognitive functioning, while also creating a restful environment during breaks [24,26]. Nurse-centered lighting design can be a beneficial approach in creating a healthy environment specifically tailored to the needs of night shift nurses [11,23]. Following this approach, it is highly recommended for night shift nurses to be exposed to bright, blue-enriched light during their working hours [30]. The designer tries to provide lighting that mimics daylight with a higher color temperature (around 4000–6500 Kelvin) [30]. Additionally, the use of gradual transition lighting, starting with bright, blue-enriched light at the beginning of the shift and gradually transitioning to warmer and dimmer light towards the end of the shift, is another important consideration that can be implemented [24,26,30]. The gradual change in lighting can effectively signal to the body that the work shift, and thus the circadian “day”, is coming to a close, facilitating the winding down process and preparation for sleep after work [26,30]. Simultaneously, a patient-centered lighting design can be implemented to fulfill the chronobiological needs of patients [31]. According to this approach, dimmed lighting with lower intensity and warmer color temperatures (approximately 2700–3000 Kelvin) during nighttime hours is utilized to establish a soothing, tranquil, and sleep-promoting environment for hospitalized patients [25,32]. In order to quantify the non-visual effects of light on circadian health, different metrics have also been recommended and are often used in studies. Table 2 summarizes these metrics and related information.

Table 2.
An overview on lighting metrics.
3. Methods
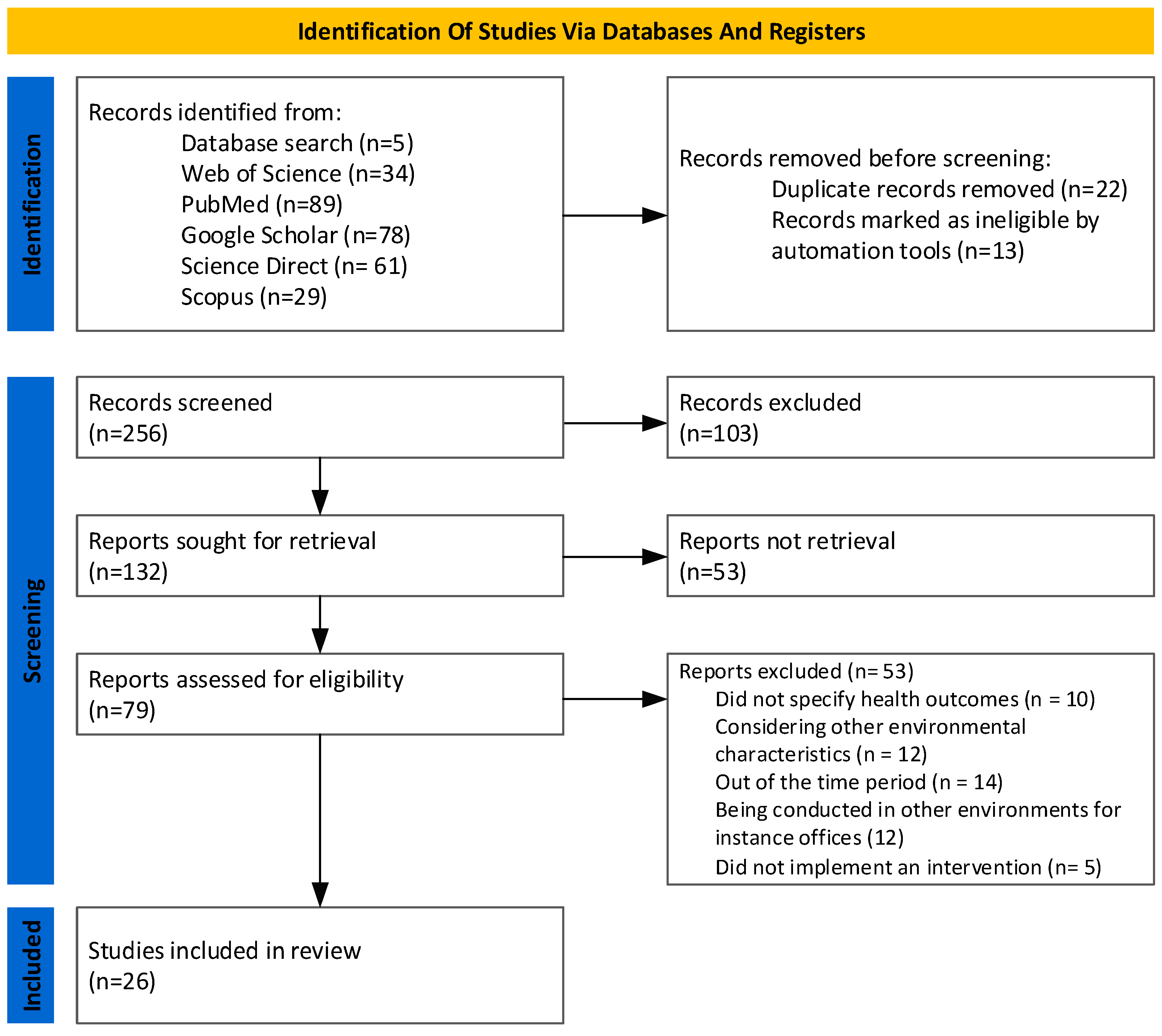
Based on studies that examine the effects of indoor lighting conditions on health outcomes in healthcare environments, this review paper discusses the findings. In the present study, a systematic literature review method was employed to ensure clarity of communication, validity of selection of studies, and presentation of conclusions based on the retrieved information [49]. The PRISMA guidelines were followed to provide validity in the selection of papers [50] (Figure 2).
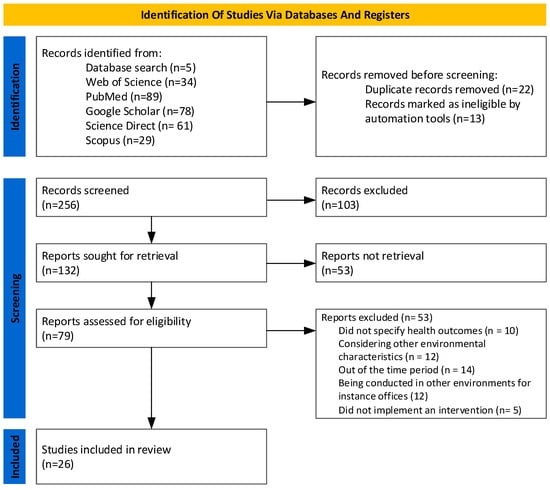
Figure 2.
PRISMA 2020 flow diagram: the screening process of studies reviewed by the authors.
3.1. Information Sources and Study Selection
A literature search was conducted using five online scientific databases (PubMed, ScienceDirect, Scopus, Google Scholar, and Web of Science). Among the databases searched, PubMed and Scopus covered human-related research, and ScienceDirect and Web of Science covered technical and health-related publications. Keywords were searched using “AND” to search two or more concepts of interest and “OR” between each category (Boolean operators), allowing for the filtering out of unrelated candidates while providing more relevant and accurate results. A hand search of references of articles identified in the primary search and a review of their reference lists led to the discovery of additional articles. There are a number of keywords that were used in this study: circadian lighting design, non-image-forming effects of (day)light, non-visual effects of (day)light, circadian lighting, circadian rhythm, healthcare lighting, health outcomes, patient satisfaction, and staff performance.
3.2. Eligibility Criteria
This review included only studies conducted in healthcare environments. English was the language of publication for all articles in the qualitative synthesis. The years of consideration were 2002–2023, and 2002 was chosen as a cutoff point since it was the year when ipRGC functionality was discovered [51]. Being out of time period, considering other environmental characteristics, or not specifying health outcomes led to 53 articles being excluded from the list of 79 eligible articles.
3.3. Screening
An illustration of the screening process can be found in Figure 2. Search terms related to lighting and health were filtered using the filter TKA (Title–Keywords–Abstract) so that articles with different topics were excluded.
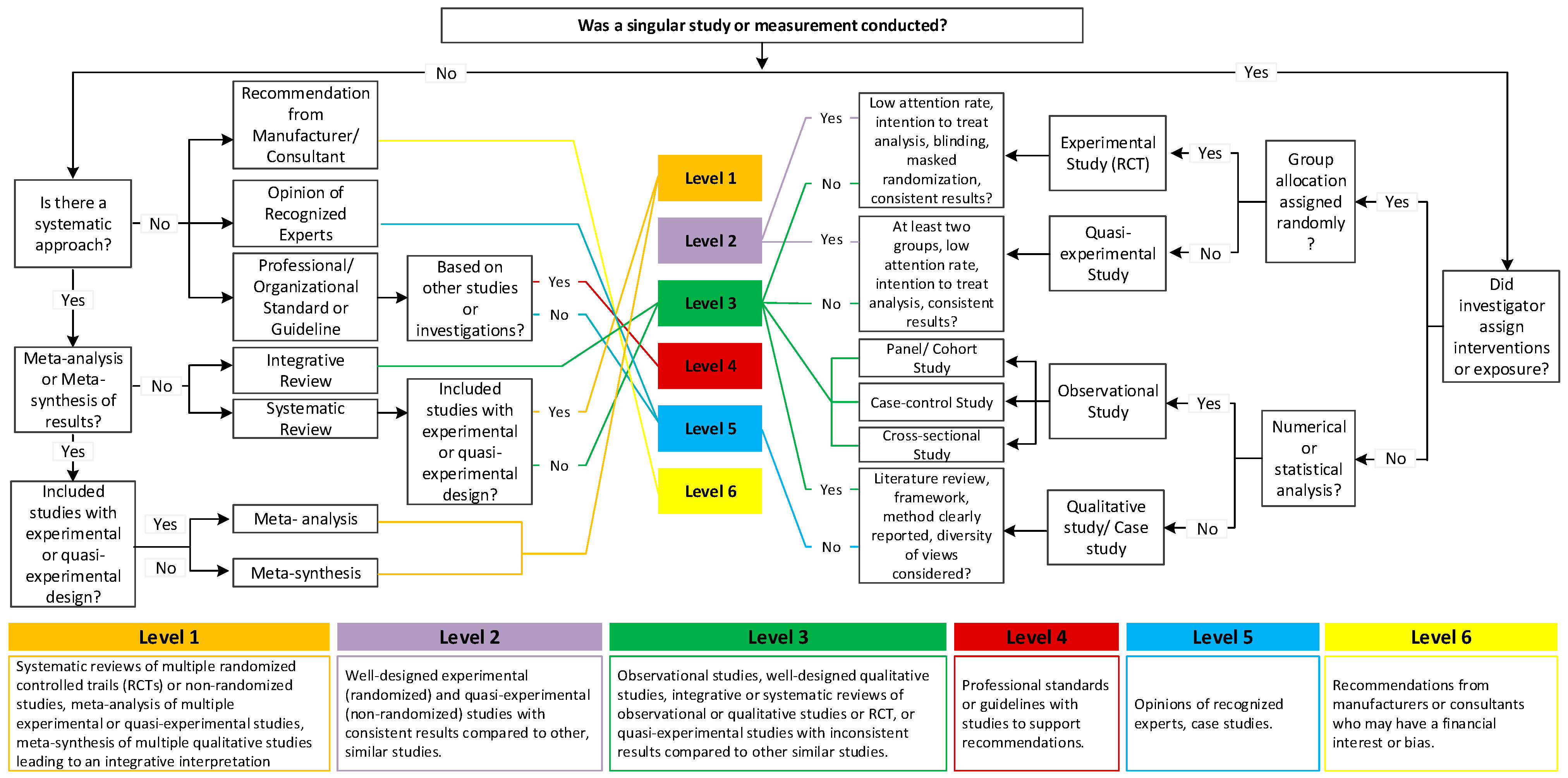
3.4. Appraisal of Healthcare Design and Research Studies Based on Levels of Evidence
With more evidence emerging about how the built environment impacts patients and staff in healthcare environments, creating an individual ranking system for evidence based on its effectiveness and appropriateness is essential. Based on a broad consensus among experts and stakeholders in the field, Figure 3 presents a hierarchical rating scale that can be used for healthcare design. This appraisal is not intended to provide healthcare leaders and designers with a tool for assessing the validity, credibility, or reliability of statements about how specific design features influence outcomes, but rather to provide a tool for evaluating the credibility, reliability, and validity of this study and its findings [52,53,54].
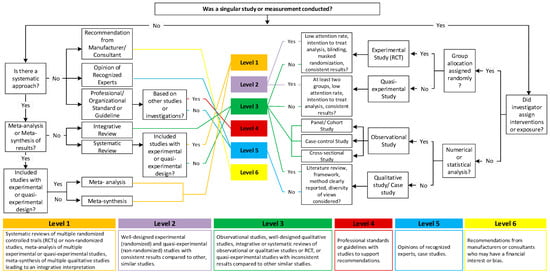
Figure 3.
Research appraisal flowchart (level of evidence) following Stichler’s (2010) framework; adapted from [52,53,54].
4. Results
There were 26 studies identified in this review.
4.1. Study Methodological Characteristics
Interventions and Human Participant Studies
Of these 26 studies, 21 were mixed methods of human interventional studies. They integrated quantitative evaluation approaches including experimental studies [25,26,32,55,56,57] and a quasi-experimental study [57] with qualitative research methods including observational methods [6,26,27,32,57,58,59,60,61,62,63,64,65,66] and case studies [23,58,62,64,65] to evaluate the effectiveness, efficacy, or other results from an intervention. Table 3 provides a summary.

Table 3.
Summary of studies with the interventions and human participant studies.
This paper included and reviewed 21 papers exploring lighting-related occupational health outcomes. Their results can be categorized into five groups including sleep-related, mood and psychological, patient-related, nurse-related, and environmental and psychosocial. These groupings are not mutually exclusive, and some health outcomes may overlap across different categories. Presented here are the results and conclusions from all articles that have been included. The remaining tables depict the investigated health outcome measures. Some publications examined more than one health benefit associated with lighting conditions within healthcare environments.
4.2. Sleep-Related Health Outcomes
Ten of the reviewed articles specifically investigated sleep-related health outcomes, focusing on sleep quality, sleep–wake patterns, and duration (refer to Table 4).
Natural light cycles promote alertness and wakefulness by synchronizing individuals’ circadian rhythms to the daily environment [2,32,67]. On the other hand, as a result of artificial light exposure at night (ALAN), circadian rhythms can be disrupted, which can affect sleep quality and make it more difficult to fall asleep [32,60]. However, the results across studies have not consistently supported this viewpoint regarding ALAN. In one study conducted in institutionalized elderly patients with dementia, activity and sleep were investigated using a wrist activity monitor (Actillume) [32]. Each patient received one of four treatments at random: evening bright light (2500 lux from 17:30 to 19:30), morning bright light (500 lux from 9:30 to 11:30), evening dim red light (red light less than 50 lux between 17:30 and 19:30), or daytime sleep restriction (DSR). Interestingly, the effect of increasing light exposure in the mornings or evenings on sleep or alertness during the day was inconclusive [32]. In another study of a younger population of hospitalized inpatients, sleep–wake activity patterns were also assessed using wrist actigraphs/light meters. There were chronic light exposure levels that did not adequately synchronize circadian rhythms with a mean daytime light intensity of 104.80 lux. This low light level caused sleep disturbances as well as circadian disruptions [60]. In medical inpatients, there was no synchronization of light exposure with sleep–wake patterns, suggesting a need for further investigation of how manipulating light exposure can be beneficial [60]. In one study, simulated natural lighting systems were used in intensive care units (ICUs) as part of an intervention research project to support patients’ circadian rhythms compared with traditional lighting systems [56]. Although interviews with patients who had experienced sleep disorders revealed their satisfaction with the dynamic lighting environment, this study only used self-reported subjective measures from the patients and did not provide clear objective evidence that the light intervention influenced factors such as circadian rhythm maintenance and subsequent recovery [56]. In a similar study, dynamic lighting interventions were evaluated on sleep outcomes in inpatients. By providing low nocturnal light exposure, and 2 h of bright light (1750 lux) during the day, the lighting system with a dynamic 24 h light/dark cycle can improve inpatient sleep compared to traditional lighting systems [25]. However, additional clinical research is needed to identify the effective lighting design and strategy to improve health outcomes and status in healthcare settings [25]. Conversely, no significant improvement was reported in sleep quality, mood, or well-being among psychiatric inpatients in response to a dynamic circadian lighting system [55]. The lack of reported effects on circadian interventions in institutionalized patients [32,55] is not unexpected, as psychiatric disorders themselves may cause circadian disruption regardless of lighting conditions [68]. Taken together, the dynamic lighting approach for non-psychiatric inpatients shows therapeutic promise [25,56,60]. According to a study results between a blue-light-depleted lighting system and a blue-light-emitting lighting system showed improved nocturnal melatonin levels and rhythmicity, as well as improved sleep measures [6].

Table 4.
Thematic analysis of reviewed papers: sleep-related health outcomes.
Table 4.
Thematic analysis of reviewed papers: sleep-related health outcomes.
| Category | Ref. | Setting | Participants | Study Design | Intervention | Mediating Factor | Level |
|---|---|---|---|---|---|---|---|
| Sleep Quality | [32] | Nursing home | Nursing home residents (58 women, 19 men) | Randomized controlled trial | Evening bright light, morning bright light, daytime sleep restriction, evening dim red light | Lighting intensity, timing | 2 |
| [56] | Intensive care units | Patients (n = 19) | Descriptive correlational studies | Cycled lighting environment | Lighting intensity, timing, wavelength | 3a | |
| [25] | Patients’ room | Cardiology ward patients (n = 196) | Controlled clinical trial | Dynamic lighting system | Lighting intensity | 3a | |
| [55] | Patients’ room | Psychiatric patients (n = 54) | Randomized controlled trial | Adjustable lighting | Lighting intensity, CCT, wavelength | 2 | |
| [6] | Patients’ room | Healthy people (n = 12) | Randomized controlled trial | Dynamic lighting system | Blue-depleted light | 2 | |
| [66] | Patients’ room | Psychiatric patients | Randomized controlled trial | Dynamic lighting system | Blue-depleted light | 2 | |
| Sleep- wake Patterns | [64] | Patients’ room | Dementia patients (n = 13) | Pilot study, observations | Biodynamic lighting system | Lighting intensity, CCT | 3a |
| [60] | Patients’ room | Medical inpatients (women = 23; men = 17) | Correlational study or non-experimental study | Dynamic lighting system | Lighting intensity | 2 | |
| Duration | [64] | Patients’ room | Dementia patients (n = 13) | Pilot study, observations | Biodynamic lighting system | Lighting intensity, CCT | 3a |
4.3. Mood and Psychological Outcomes
Of the twenty-one studies identified by our search strategy, four investigated the relationship between indoor lighting conditions and mood-related factors. These studies utilized four different assessments to evaluate mood and psychological outcomes (see Table 5).
Current evidence suggests that lighting conditions can have significant effects on mood and psychological outcomes, and the use of appropriate lighting levels, color temperatures, and lighting strategies may contribute to improved mood, enhanced cognitive performance, and increased well-being [4,23,25,55,60]. This assumption was addressed in one study that investigated the effects of rechargeable, blue-depleted, and proximity-sensing lighting systems on health outcomes in a hospital setting. As a result of comparing the three lighting systems with overhead lights at night, it was determined which one provided wireless task lighting more effectively and could minimize disruption to patients overnight. In hospital settings rich in blue-wavelength emission, typical hospital lighting might disrupt the circadian rhythms of patients at night. In an intervention, healthcare providers avoided overhead patient room lighting and used physiologically neutral lighting instead. Among 33 nurses surveyed, high satisfaction scores were obtained, and the lighting pods were perceived as providing adequate lighting for overnight care. Additionally, the lighting intervention led to a median improvement in hospital anxiety and depression scale scores for patients [23]. It is worth noting that while many studies have suggested positive effects of lighting conditions on mood and psychological outcomes, there is also some conflicting evidence. One study used the Profile of Mood States BriefTM form to assess daily mood of medical inpatients. Even though higher light exposure was associated with lower fatigue and reduced total mood disturbance, particularly in pain-stricken patients, the authors stressed that further research is required to determine how light exposure affects mood and psychological outcomes of medical inpatients [60]. Compared to standard lighting conditions (fixed intensity fluorescent), dynamic lighting intervention in a hospital setting did not affect subjective mood (hospital anxiety and depression scale survey) for inpatients. In common with the previously mentioned studies, the authors emphasized the critical necessity for additional clinical research to find solid evidence of artificial lighting design on mood- and psychological-related health outcomes, aiming to establish the best lighting strategies for promoting them in healthcare settings [25]. Similarly for psychiatric inpatients, there were no effects on measures of depression and well-being when implementing a circadian lighting system (dynamic) as an intervention compared to standard lighting conditions (fixed intensity fluorescent) [55].

Table 5.
Thematic analysis of reviewed papers: mood and psychological health outcomes.
Table 5.
Thematic analysis of reviewed papers: mood and psychological health outcomes.
| Category | Ref. | Setting | Participants | Study Design | Intervention | Mediating Factor | Level |
|---|---|---|---|---|---|---|---|
| Mood Status | [60] | Patients’ room | Medical inpatients (women = 23, men = 17) | Correlational study or non-experimental study | Dynamic lighting system | Light intensity | 2 |
| [25] | Patients’ room | Cardiology ward patients (n = 196) | Controlled clinical trial | Dynamic lighting system | Lighting intensity | 3 | |
| Fatigue Status | [64] | Patients’ room | Dementia patients (n = 13) | Pilot study, observations | Biodynamic lighting system | Lighting intensity, CCT | 3 |
| Anxiety | [25] | Patients’ room | Cardiology ward patients (n = 196) | Controlled clinical trial | Dynamic lighting system | Lighting intensity | 3 |
| [23] | Intermediate acuity unit | Nurses (n = 33), patients (n = 21) | Non-randomized, controlled interventional trial | Blue-depleted lighting at night | Lighting spectrum, intensity | 2 | |
| Depression | [25] | Patients’ room | Cardiology ward patients (n = 196) | Controlled clinical trial | Dynamic lighting system | Lighting intensity | 3 |
| [23] | Intermediate acuity unit | Nurses (n = 33), patients (n = 21) | Non-randomized, controlled interventional trial | Blue-depleted lighting at night | Lighting spectrum, intensity | 2 | |
| [55] | Patients’ room | Psychiatric patients (n = 74) | Randomized controlled groups | Adjustable lighting | Lighting spectrum | 2 |
4.4. Patient-Related Health Outcomes
Among the twenty-one articles meeting our inclusion criteria, seven specifically investigated the effect of indoor lighting conditions on patient-related health outcomes. Together, these studies measured six different parameters to assess the effects of lighting conditions on patient well-being (see Table 6). Among the parameters of alertness, pain, and psychotropic medications, analyses of the data in these studies did not support the hypothesis that dynamic circadian lighting systems improve these measures [32,58,60]. Despite two studies investigating the effect of dynamic lighting interventions on delirium development in ICUs and CCUs, both reports found no association between lighting and delirium [27,61]. While it has been recognized that a proper exposure to natural light and properly timed artificial light can improve sleep quality and regulate circadian rhythms, which may help patients recover more quickly, researchers did not find that dynamic lighting systems shortened hospital stays for patients in the CCU [27,58,66].
Two of the studies explored the relationship between lighting conditions and physical activity of patients. In common with many of the measures discussed above, the direct impact of lighting on physical activity has not been extensively studied, yet there is some evidence suggesting that it can indirectly influence patient movement and engagement. These dynamic systems have shown potential in enhancing sleep quality, mood, and overall well-being among patients, without negatively affecting any other outcomes. When patients experience improved sleep and mood, it is possible that they may feel more energized and motivated to participate in physical activity. This assumption, however, is not fully supported by current clinical evidence [27,63]; thus, it is clear that more focused clinical studies in larger cohorts must be conducted to thoroughly explore this potential intervention.

Table 6.
Thematic analysis of reviewed papers: patient-related health outcomes.
Table 6.
Thematic analysis of reviewed papers: patient-related health outcomes.
| Category | Ref. | Setting | Participants | Study Design | Intervention | Mediating Factor | Level |
|---|---|---|---|---|---|---|---|
| Physical Activity | [27] | CCU | Patients (n = 748) | Retrospective cohort study | Dynamic lighting system | CCT | 3 |
| Length of Hospitalization | [26] | Nurse station | Patients (n = 1073) | Field survey | Blue-enriched lighting system | CCT | 3 |
| [27] | CCU | Patient (n = 748) | Retrospective cohort study | Dynamic lighting system | CCT | 2 | |
| [58] | Patient’s room | Depressed patients (n = 30) | Pilot study, observations | Dynamic lighting system | CCT, light intensity | 3 | |
| Delirium | [27] | CCU | Patient (n = 748) | Retrospective cohort study | Dynamic lighting system | CCT | 3 |
| Psychotropic Medication | [32] | Nursing home | Nursing home residents (58 women, 19 men) | Randomized controlled trial | Dynamic lighting system | Light intensity, timing | 2 |
| [61] | Intensive care unit | Patients (n = 183) | Retrospective cohort study | Dynamic lighting system | CCT | 2 | |
| [58] | Patient’s room | Depressed patients (n = 30) | Pilot study, observations | Dynamic lighting system | CCT, light intensity | 2 | |
| Alertness | [32] | Nursing home | Nursing home residents (58 women, 19 men) | Randomized controlled trial | Dynamic lighting system | Light intensity, timing | 2 |
| Pain | [60] | Patients’ room | Medical inpa-tients (women = 23; men = 17) | Correlational study or non-experimental study | Dynamic lighting system | Light intensity | 2 |
4.5. Nurse-Related Health Outcomes
In addition to patient outcomes, the effects of dynamic circadian lighting design on healthcare staff performance, retention, and well-being are also critically relevant. Several studies investigated the perceptions and satisfaction of nurses and staff members (Table 7), specifically concerning the physical environment and lighting conditions in the institutional setting.
It has been suggested that errors caused by fatigue during patient care have significant negative impacts on the healthcare system [69]. Previous research has reported that blue-enriched light can enhance alertness and attention [70]. In one study, however, interventional blue-enriched lighting had little effect on reducing medical error rates in an adult ICU within a university hospital [6].
Nurses’ perception of the healthcare environment has a direct impact on their work experience and patient care as well as the well-being of the staff. Dynamic lighting systems implemented in healthcare settings have the potential to influence how nurses perceive their environment, which in turn can impact their job satisfaction, performance, and overall experience [23,65]. Nurses in medical–surgical hospital units have found that standard lighting at decentralized stations and at bedsides were the least favorable for job performance, and that more control over that would improve satisfaction [24]. Another study found that institutional care staff considered a dynamic circadian lighting system more satisfactory and more suitable for work compared to the existing lighting system [28]. Although some of these studies should be replicated due to their small sample sizes, taken together, these studies indeed suggest that implementation of dynamic lighting can improve healthcare worker job satisfaction, in turn potentially leading to improved patient care and well-being for both the patients and staff.

Table 7.
Thematic analysis of reviewed papers: nurse-related health outcomes.
Table 7.
Thematic analysis of reviewed papers: nurse-related health outcomes.
| Category | Ref. | Setting | Participants | Study Design | Intervention | Mediating Factor | Level |
|---|---|---|---|---|---|---|---|
| Medical Errors | [6] | Hospital | Nonpatient (n = 12) | Retrospective cohort study | Dynamic lighting system | Blue-depleted light | 2 |
| Environmental Perception | [62] | Nurse home | Patients (n = 1073) | Case study, observation | Dynamic lighting system | Controlling strategy (intelligent, personalized) | 3 |
| [28] | Nursing home | Staff members (n = 42) | Observation | Tunable lighting systems | CCT, controlling strategy | 2 | |
| Satisfaction | [23] | Intermediate acuity unit | Nurses (n = 33), patients (n= 21) | Non-randomized, controlled interventional trial | Blue-depleted lighting at night | Lighting spectrum, intensity | 2 |
| [65] | Pharmacy | Employee (n = 8) | Case study, observation | Dynamic lighting system | Lighting intensity, CCT | 3 | |
| [28] | Nursing home | Staff members (n = 42) | Observation | Tunable lighting systems | CCT, controlling strategy | 2 |
4.6. Environmental and Psychosocial Outcomes
Physical environment and psychosocial variables are examined in this section to understand how they influence health outcomes (see Table 8). Environmental experience encompasses how individuals perceive the overall physical setting and how it impacts their well-being, and user preference also needs to be taken into account to acknowledge the subjective nature of individuals’ preferences in healthcare environments. Understanding user preferences for environmental lighting can provide insights into environmental lighting control to optimize patient-centered care. By considering these factors, healthcare environments can be designed and customized to enhance patient experiences and contribute to positive health outcomes [28,32,56,65,71]. However, more assessments of the effects of healthcare lighting conditions on patient outcomes are needed because the majority of these studies (Table 7) have very small sample sizes and thus need to be interpreted with caution.

Table 8.
Thematic analysis of reviewed papers: environmental and psychosocial health outcomes.
5. Simulation-Based Studies
This section provides an overview of simulation-based methods in lighting design studies, summarizing key results and methodologies employed. The focus is on the use of simulation tools to assess lighting conditions in healthcare environments (Table 9). Many of these simulations were based on default parameters regarding surface spectral properties. The parameters included visible transmission through windows and reflectance through walls, ceilings, and floors. In the simulation-based research, different software packages were used, and two main approaches were identified: retrospective evaluation, which measures light received at a sensor point to assess effectiveness, and prospective evaluation, which predicts future lighting conditions. Retrospective evaluation is more straightforward because it measures light based on how the human eye responds to light and introduces the concept of “circadian efficacy” to assess light quality. This approach is also based on the measuring spectral distribution of light received at a sensor point. However, prospective evaluation is more challenging since few simulation tools can accurately predict how light affects our body’s circadian rhythms [72,73]. In order to fill this gap, a methodology that incorporates existing technology with novel calculations was proposed. In this method, light sources with known spectra were used to calculate their circadian effectiveness. Despite challenges in obtaining spectral information for specific lamps used over their lifespan, the paper relied on standard CIE illuminants and specific lamp spectra from Philips Lighting. To determine the circadian weighting, the radiometric spectra were analyzed for their short-wavelength content. Applying this method to a range of illumination sources resulted in a chart that can be used in a temporally neutral application to assess the circadian potential of a light source [72,73].
Using a patient-centered approach, researchers estimated whether lighting conditions would be sufficient for circadian entrainment [73]. In one study, circadian stimulus (CS) was calculated at the eye level of a patient, and CS autonomy was calculated. It was calculated by counting days in which CS was greater than 0.35 for at least one hour in the morning, which was hypothesized to be sufficient to entrain circadian rhythms. Using Daysim, dynamic daylighting was calculated and melanopic lux values were converted. Data from this study were used to analyze non-visual effects in healthcare settings throughout the year [74]. In the latest study, visual and non-visual lighting performance in nursing homes was simulated using a methodological framework. ALFA (Adaptive Lighting for Alertness) is an innovative software tool that measures the adequacy of lighting strategies for providing residents with adequate luminous conditions and circadian stimulation to occupants. Testing of proposed improvement strategies demonstrated that robust methodologies and tools can be used to comprehensively address visual comfort, task performance, and circadian well-being in healthcare settings [75]. The reviewed papers mainly considered architectural elements such as window orientation, window-to-wall ratio (WWR), shading devices, and locations to estimate lighting performance. Visual and non-visual simulations were used to compute levels of comfort and non-visual stimulation experienced by vulnerable populations in healthcare environments. Only two papers focused primarily on non-visual performance, proposing strategies to enhance current conditions. These studies utilized 3D modeling and exported their models to ALFA, considering various parameters such as location, timing, materials, grid-based analysis, and orientations to address both visual and non-visual requirements [75,76].

Table 9.
Thematic analysis of reviewed papers: simulation-based studies.
Table 9.
Thematic analysis of reviewed papers: simulation-based studies.
| Ref. | Research Setting | Evaluation Metrics | Studies Parameters | Software | Architectural Elements |
|---|---|---|---|---|---|
| [72] | Virtual patient room | Circadian stimulus | Lighting intensity, timing, spectrum | Statistical analysis, DAYSIM, field measurements | Window orientation, WWR, glazing material, shading device |
| [73] | Virtual patient room | Circadian stimulus | Lighting intensity | Statistical analysis, Radiance, field measurements | WWR, glazing materials, latitude |
| [75] | Nursing home | Circadian stimulus, Photopic Lux, EML, CS, plane Lux, M/P | Lighting intensity, timing, spectrum | ALFA | Location, timing, sky condition, materials, luminaires, furniture position |
| [74] | Patient room | EML, photopic lux | Lighting intensity, timing | Statistical analysis, Honeybee, Rhino, field measurements | Materials, orientation, WWR |
| [76] | Patient room | Melanopic EDI, melanopic DER, climate-based metrics | Lighting intensity, timing | ALFA | WWR, orientation, location, sky conditions, materials |
6. Discussion
We undertook a comprehensive review of 21 peer-reviewed publications spanning from 2002 to July 2023, exploring lighting designs that facilitate proper circadian alignment in healthcare environments and their associated health outcomes. The synthesis of these studies suggests that although natural light is integral for establishing a healthy indoor environment, practical limitations related to architectural factors like building forms, orientations, and regional climate hinder the provision of sufficient natural light. Consequently, artificial lighting approaches emerge as a complementary strategy to ensure adequate indoor lighting that meets well-being thresholds for health care facilities. Indeed, evidence-based indoor lighting recommendations for healthy individuals have been recently proposed [77]. Rigorous modeling and clinical studies testing these suggested parameters in an institutional environment will be necessary to provide converging evidence on the appropriate lighting approaches for patients and institutional staff to optimize recovery and well-being.
As part of ANSI/IES RP-29-20, a new guideline for healthcare design, recommendations are provided for optimal lighting in hospitals and health care facilities. These guidelines emphasize the diverse lighting requirements of patients, medical professionals, and family members, and they need to be embraced and implemented. Taking into account factors such as color tunable lighting systems and lighting systems that promote good circadian health to improve mood, comfort, sleep, and physical recovery, new standards in medical and healthcare lighting focus on human-centered lighting to improve patient, staff, and visitor experiences [78]. Moreover, these guidelines can serve as a basis for a few design recommendations. In a daytime setting, for instance, an EDI of approximately 250 lux is aimed for during the day. In order to do this, we can increase the availability and accessibility of natural daylight, adjust the spectral content of electrical lighting to increase the amount of melanopic daylight efficacy ratio (DER), enhance surface reflectance and furnishings, and minimize glare to increase the amount of vertical illumination. DER, color rendition index, and energy efficiency should all be taken into account when designing healthcare lighting. The goal in evenings and nights is to enhance visual guidance while minimizing disruption to sleep and circadian rhythms. Sleep environments should be kept below 10 lux, with blackout blinds and orientation lighting as necessary. Melanopic EDI targets can be achieved with warm white LEDs with DERs below 0.35. It is possible to use task lighting to support activities while maintaining melanopic EDI below 10 lux [77].
Our systematic review revealed diverse study samples that ranged from those with disrupted circadian rhythms, mood disorders in ICUs and CCUs, individuals with dementia or cognitive impairments, elderly residents in nursing homes, and nurses working in healthcare settings. There are, however, limitations associated with small sample sizes. Considering the small number of participants, the results may not be generalizable. It is therefore recommended to interpret the results of studies with limited sample sizes with caution and to be aware of the potential biases that could result. The studies identified in this systematic review provided initial and potentially valuable insights into the effects of lighting conditions on patient-related health outcomes. However, further research should be conducted with larger samples to confirm and extend their conclusions. The approaches of the reviewed papers to the lighting designs in healthcare settings can be broadly categorized into two groups: simulation-based and human case interventions. Considering the limited number of simulation-based studies in healthcare environments, it is challenging to identify the most effective tools. The human intervention studies further delineate into five distinct dimensions—sleep-related, mood and psychological, patient-related, nurse-related, and environmental and psychosocial health outcomes. An important aspect of evaluating these results is recognizing the importance of critically reviewing all evidence to determine if it is effective in answering key research questions: lighting design influences health outcomes in healthcare settings, whether the results are appropriate for the study design and sample, and how easily recommendations can be implemented in a wide variety of environments, populations, and circumstances.
Whereas an abundance of neuroscience and biological evidence underscores the profound impact of natural light on human health and well-being, encompassing benefits such as fatigue mediation, improved alertness in health providers, and positive environmental experiences for patients and their families, the reviewed papers present a mixed outlook on the benefits of artificial lighting in terms of health outcomes. Although some advocate for the potential benefits of adjustable lighting mimicking natural light, others report conflicting or inconclusive results. In order to understand how artificial lighting designs affect the occupants of healthcare facilities, more rigorously controlled interventions and comprehensive experiments within controlled institutional environments are necessary. It will offer the chance to consider the multifaceted influences of various parameters on circadian health. Despite significant technological advancements in the electric lighting market, bench scientific studies, and the daylighting and building automation sectors, a noteworthy observation from the reviewed papers is the continued independence of these sectors. This lack of integration hinders the realization of healthier environments for patients and night-shift medical staff. Integrating these sectors, however, offers a dual advantage: it enhances user-centered lighting, particularly for patients and nurses, contributing significantly to improved health outcomes. Additionally, this integration provides an opportunity for a thorough post-occupancy evaluation (POE) that incorporates both technical environmental assessment (TEA) and observer-based environmental assessment (OBEA) simultaneously. TEA involves objective measurements and technical assessments, encompassing metrics like illuminance levels, color temperature, and spectral distribution to provide quantitative data on the physical aspects of lighting. In contrast, OBEA relies on subjective assessments from healthcare staff or patients, capturing perceptions, preferences, and qualitative feedback. Combining these assessments facilitates the generation of holistic design recommendations that address both technical and human dimensions of lighting in healthcare facilities. Furthermore, the inclusion of field measurements alongside simulation results enhances the credibility and applicability of the results, strengthening the evidence base for recommendations on lighting design in healthcare settings. To bridge the gap between simulation results and real-world applications, future research should prioritize longitudinal studies conducted in actual healthcare settings. Additionally, these studies must assess the effectiveness of institutional lighting interventions over time in both patients and healthcare staff, considering the dynamic and diverse nature of healthcare environments also necessitates a thorough examination of how staffing patterns such as rotating shifts and interdepartmental exchanges may influence the effectiveness of biodynamic lighting. Moreover, a broader exploration of healthcare settings beyond virtual patient rooms is essential to ensure the generalizability of results to common areas, surgical suites, emergency rooms, and other critical spaces. Future studies should move beyond reliance on default spectral properties for surfaces and strive for more accurate spectral representations to enhance the reliability of simulation results. A notable gap highlighted in the text is the relative neglect of lighting considerations for night shift workers, particularly those stationed in nursing areas. While the focus on patient rooms is pivotal, achieving a comprehensive understanding of the lighting needs of healthcare professionals working during nighttime hours is equally crucial. Future studies should address this imbalance, fostering a holistic approach to healthcare lighting. Another crucial aspect to consider is the potential influence of confounding variables which may distort the results of a study. Among these variables is the impact of medications and drugs administered to patients, including the widespread use of melatonin supplements among hospitalized individuals. Although this review primarily focuses on the impact of lighting systems on health outcomes, with melatonin suppression index (MSI) serving as a tool to gauge the effects of ALAN on circadian rhythmicity in patients, it would be beneficial to incorporate the use of melatonin into future studies for a more comprehensive understanding.
Ultimately, these studies demonstrate that chronobiological principles can be applied to building and hospital design, and provide a theoretical basis for future studies. Evidence-based design benefits both clinical and nonclinical populations.
7. Conclusions and Future Directions
We have highlighted the current evidence on the importance of lighting design in healthcare environments for promoting proper circadian alignment and its associated health outcomes, providing insights into the diverse health benefits that may be achieved through biologically appropriate lighting designs and conditions in healthcare settings. In total, twenty-six sources assessed lighting conditions and systems in healthcare environments from a circadian health perspective. Among them, twenty-one papers focused on the interventional human subject studies. The body of neuroscientific and biological evidence indicates that exposure to natural light cycles has positive health and well-being benefits for human, including reduced fatigue, increased alertness in healthcare providers, and positive patient and family experiences. However, the reviewed papers provide mixed views on the health benefits of ALAN exposure in institutional environments; the lack of consistent results likely reflects the paucity of research in this emerging area. Despite some arguing for the benefits of adjustable lighting systems with the aim of mimicking natural light, other studies have reported conflicting or inconclusive results. Five papers were simulation-based and conducted across various latitudes, appropriate window design and ratio, interior spatial properties to ensure that the indoor lighting conditions are healthy for patients and staffs. Qualitatively, the positive outcomes of some studies suggest that pursuing institutional natural and artificial lighting designs is a beneficial approach; however, the low number of studies prevents a quantitative assessment of the current evidence in the field. Thus, there remains much to be explored regarding the efficacy of artificial lighting designs in healthcare facilities, necessitating more rigorous control interventions and more comprehensive experiments within well-controlled environments, and replication of these studies considering the multifaceted influence of various parameters on circadian health. Further research in this field is required to establish conclusive evidence. In addition, implementing circadian-aligned lighting designs in healthcare environments requires collaborative efforts among architects, lighting designers, healthcare professionals, and researchers. Artificial lighting systems, including spectrally tailored lighting and personalized bio-adaptive lighting, can supplement daylight and modulate light intensity and spectrum according to circadian needs; robust full spectrum lighting during the day and minimal (sub-individual melatonin suppression level) ALAN exposure. The integration of lighting control technologies, such as dynamic adjustment of light levels and color temperature based on natural light availability and time of day, is essential for achieving circadian alignment. These technologies, combined with occupancy and daylight sensors, can optimize energy efficiency while maintaining proper sleep–wake cycles. Along with additional lighting simulations and additional studies with the consistence use of standardized lighting metrics for evaluating and optimizing lighting designs in healthcare settings, designers will be able to make informed decisions about lighting design, ensuring that buildings offer healthy, comfortable, and visually appealing environments that promote well-being, productivity, and energy efficiency.
8. Executive Summary
The burgeoning field of evaluating architectural lighting on health issues is dynamic. Despite a lack of consensus at present, several trends and emerging methodologies could be observed in the systematic review. Metrics, tools, and methodologies for evaluating the effects of architectural changes on health issues continue to evolve, with a growing emphasis on multidisciplinary approaches and comprehensive assessments. Open questions persist regarding the long-term effects of architectural changes, optimal study designs, and the integration of patient-reported outcomes. Addressing dissimilar results among similar studies remains a challenge, highlighting the need for standardized methodologies and rigorous study designs. Whereas counting the number of papers on a specific topic can indicate research interest, it may not always reflect the quality or significance of findings. Moreover, regarding the diverse populations studied, aggregating results requires careful consideration of potential confounding factors and heterogeneity across populations. Meta-analyses and systematic reviews can offer valuable insights but must account for contextual differences and individual variations.
In summary, future research should focus on bridging the gap between theoretical understanding and practical application in lighting design for healthcare environments. By addressing the limitations identified in our systematic review, embracing collaborative, interdisciplinary approaches, and standardizing lighting measurements, we can advance our understanding of the role of lighting in promoting circadian health and well-being in healthcare settings, and ultimately enhance the quality of care provided to patients and fostering supportive environments for healthcare providers.
Author Contributions
Conceptualization: S.N.H., J.C.W., I.S., R.J.N. and N.K.; Methodology: S.N.H. and J.C.W.; Writing—Original Draft Preparation: S.N.H., I.S. and J.C.W.; Writing—Review and Editing: J.C.W., R.J.N., N.K. and S.N.H.; Visualization: S.N.H. and I.S.; Supervision: R.J.N.; Funding Acquisition: R.J.N. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by the National Institutes of Health grants R21AT011238 and R21CA276027 to RJN and Alzheimer’s Association grant 23AARG-1028933 to JCW. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the Alzheimer’s Association.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Fonken, L.K.; Nelson, R.J. The Effects of Light at Night on Circadian Clocks and Metabolism. Endocr. Rev. 2014, 35, 648–670. [Google Scholar] [CrossRef]
- Bedrosian, T.A.; Fonken, L.K.; Nelson, R.J. Endocrine Effects of Circadian Disruption. Annu. Rev. Physiol. 2016, 78, 109–131. [Google Scholar] [CrossRef]
- Kyba, C.C.M.; Mohar, A.; Posch, T. How Bright Is Moonlight? Astron. Geophys. 2017, 58, 1.31–1.32. [Google Scholar] [CrossRef]
- Kuijsters, A.; Redi, J.; de Ruyter, B.; Heynderickx, I. Lighting to Make You Feel Better: Improving the Mood of Elderly People with Affective Ambiences. PLoS ONE 2015, 10, e0132732. [Google Scholar] [CrossRef]
- Weil, Z.M.; Fonken, L.K.; Walker, W.H.; Bumgarner, J.R.; Liu, J.A.; Melendez-Fernandez, O.H.; Zhang, N.; DeVries, A.C.; Nelson, R.J. Dim Light at Night Exacerbates Stroke Outcome. Eur. J. Neurosci. 2020, 52, 4139–4146. [Google Scholar] [CrossRef]
- Vethe, D.; Scott, J.; Engstrøm, M.; Salvesen, Ø.; Sand, T.; Olsen, A.; Morken, G.; Heglum, H.S.; Kjørstad, K.; Faaland, P.M.; et al. The Evening Light Environment in Hospitals Can Be Designed to Produce Less Disruptive Effects on the Circadian System and Improve Sleep. Sleep 2021, 44, zsaa194. [Google Scholar] [CrossRef]
- Figueiro, M.G.; Sahin, L.; Wood, B.; Plitnick, B. Light at Night and Measures of Alertness and Performance. Biol. Res. Nurs. 2016, 18, 90–100. [Google Scholar] [CrossRef]
- Navara, K.J.; Nelson, R.J. The Dark Side of Light at Night: Physiological, Epidemiological, and Ecological Consequences. J. Pineal Res. 2007, 43, 215–224. [Google Scholar] [CrossRef]
- Hattar, S.; Liao, H.W.; Takao, M.; Berson, D.M.; Yau, K.W. Melanopsin-Containing Retinal Ganglion Cells: Architecture, Projections, and Intrinsic Photosensitivity. Science 2002, 295, 1065–1070. [Google Scholar] [CrossRef]
- Nelson, R.J.; Bumgarner, J.R.; Liu, J.A.; Love, J.A.; Meléndez-Fernández, O.H.; Becker-Krail, D.D.; Walker, W.H.; Walton, J.C.; DeVries, A.C.; Prendergast, B.J. Time of Day as a Critical Variable in Biology. BMC Biol. 2022, 20, 142. [Google Scholar] [CrossRef]
- Houser, K.W.; Esposito, T. Human-Centric Lighting: Foundational Considerations and a Five-Step Design Process. Front. Neurol. 2021, 12, 630553. [Google Scholar] [CrossRef]
- Vetter, C.; Pattison, P.M.; Houser, K.; Herf, M.; Phillips, A.J.K.; Wright, K.P.; Skene, D.J.; Brainard, G.C.; Boivin, D.B.; Glickman, G. A Review of Human Physiological Responses to Light: Implications for the Development of Integrative Lighting Solutions. LEUKOS 2022, 18, 387–414. [Google Scholar] [CrossRef]
- Rea, M.S.; Nagare, R.; Figueiro, M.G. Modeling Circadian Phototransduction: Retinal Neurophysiology and Neuroanatomy. Front. Neurosci. 2021, 14, 615305. [Google Scholar] [CrossRef]
- Saey, T.H. Seeing the Light: Transforming Nerve Cells into Photoreceptors to Restore Vision. Sci. News 2015, 187, 22–26. [Google Scholar] [CrossRef]
- SOLEMMA. Adaptive Lighting for Alertness A New Circadian Lighting Design Software. Available online: www.solemma.com/alfa (accessed on 26 March 2024).
- Chellappa, S.L.; Steiner, R.; Blattner, P.; Oelhafen, P.; Götz, T.; Cajochen, C. Non-Visual Effects of Light on Melatonin, Alertness and Cognitive Performance: Can Blue-Enriched Light Keep Us Alert? PLoS ONE 2011, 6, e16429. [Google Scholar] [CrossRef]
- Moore-Ede, M.; Heitmann, A.; Guttkuhn, R. Circadian Potency Spectrum with Extended Exposure to Polychromatic White LED Light under Workplace Conditions. J. Biol. Rhythm. 2020, 35, 405–415. [Google Scholar] [CrossRef]
- Wang, R.; Yang, B.; Yao, Y.; Bloom, M.S.; Feng, Z.; Yuan, Y.; Zhang, J.; Liu, P.; Wu, W.; Lu, Y.; et al. Residential Greenness, Air Pollution and Psychological Well-Being among Urban Residents in Guangzhou, China. Sci. Total Environ. 2020, 711, 134843. [Google Scholar] [CrossRef]
- Zolfaghari, Z.; R.Jones, J. Study of the Effect of Light Emitting Diode (LED) on the Optimum Window-to-Wall Ratio and Whole-Building Energy Consumption in Open Offices. Ph.D. Dissertation, Virginia Polytechnic Institute and State University, Blacksburg, Virginia, 2022. [Google Scholar] [CrossRef]
- Falchi, F.; Cinzano, P.; Duriscoe, D.; Kyba, C.C.M.; Elvidge, C.D.; Baugh, K.; Portnov, B.A.; Rybnikova, N.A.; Furgoni, R. The New World Atlas of Artificial Night Sky Brightness. Sci. Adv. 2016, 2, e1600377. [Google Scholar] [CrossRef] [PubMed]
- Kyba, C.C.M.; Kuester, T.; Sánchez de Miguel, A.; Baugh, K.; Jechow, A.; Hölker, F.; Bennie, J.; Elvidge, C.D.; Gaston, K.J.; Guanter, L. Artificially Lit Surface of Earth at Night Increasing in Radiance and Extent. Sci. Adv. 2017, 3, e1701528. [Google Scholar] [CrossRef] [PubMed]
- Hansen, J. Night Shift Work and Risk of Breast Cancer. Curr. Environ. Health Rep. 2017, 4, 325–339. [Google Scholar] [CrossRef]
- Albala, L.; Bober, T.; Hale, G.; Warfield, B.; Collins, M.L.; Merritt, Z.; Steimetz, E.; Nadler, S.; Lev, Y.; Hanifin, J. Effect on Nurse and Patient Experience: Overnight Use of Blue-Depleted Illumination. BMJ Open Qual. 2019, 8, e000692. [Google Scholar] [CrossRef] [PubMed]
- Hadi, K.; DuBose, J.R.; Ryherd, E. Lighting and Nurses at Medical–Surgical Units. HERD: Health Environ. Res. Des. J. 2016, 9, 17–30. [Google Scholar] [CrossRef] [PubMed]
- Giménez, M.C.; Geerdinck, L.M.; Versteylen, M.; Leffers, P.; Meekes, G.J.B.M.; Herremans, H.; de Ruyter, B.; Bikker, J.W.; Kuijpers, P.M.J.C.; Schlangen, L.J.M. Patient Room Lighting Influences on Sleep, Appraisal and Mood in Hospitalized People. J. Sleep Res. 2017, 26, 236–246. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Broman, A.T.; Priest, G.; Landrigan, C.P.; Rahman, S.A.; Lockley, S.W. The Effect of Blue-Enriched Lighting on Medical Error Rate in a University Hospital ICU. Jt. Comm. J. Qual. Patient Saf. 2021, 47, 165–175. [Google Scholar] [CrossRef]
- Pustjens, T.; Schoutens, A.M.; Janssen, L.; Heesen, W.F. Effect of Dynamic Light at the Coronary Care Unit on the Length of Hospital Stay and Development of Delirium: A Retrospective Cohort Study. J. Geriatr. Cardiol. 2018, 15, 567–573. [Google Scholar] [PubMed]
- Schledermann, K.M.; Hansen, T.S.; Bjørner, T. Perceived Visual Comfort and Usefulness of a Circadian Lighting System Implemented at a Nursing Home. Multimed. Tools Appl. 2023, 82, 5253–5269. [Google Scholar] [CrossRef]
- Amirazar, A.; Azarbayjani, M.; Im, O.-K.; Zarrabi, H.; Ashrafi, R.; Cox, R.; Johnson, A. Assessing the Circadian Potential of an Office Building in the Southeastern US. In Proceedings of the 2018 Symposium on Simulation for Architecture and Urban Design—SimAUD, Delft, The Netherlands, 4–7 June 2018. [Google Scholar]
- Griepentrog, J.E.; Labiner, H.E.; Gunn, S.R.; Rosengart, M.R. Bright Environmental Light Improves the Sleepiness of Nightshift ICU Nurses. Crit. Care 2018, 22, 295. [Google Scholar] [CrossRef] [PubMed]
- Lledó, R. Human Centric Lighting, a New Reality in Healthcare Environments; Springer International Publishing: Berlin/Heidelberg, Germany, 2019; pp. 23–26. [Google Scholar] [CrossRef]
- Ancoli-Israel, S.; Martin, J.L.; Kripke, D.F.; Marler, M.; Klauber, M.R. Effect of Light Treatment on Sleep and Circadian Rhythms in Demented Nursing Home Patients. J. Am. Geriatr. Soc. 2002, 50, 282–289. [Google Scholar] [CrossRef]
- Lowry, G. A Comparison of Metrics Proposed for Circadian Lighting and the Criterion Adopted in the WELL Building Standard; CIBSE Technical Symposium: London, UK, 2018; Volume 10. [Google Scholar]
- Aubé, M.; Roby, J.; Kocifaj, M. Evaluating Potential Spectral Impacts of Various Artificial Lights on Melatonin Suppression, Photosynthesis, and Star Visibility. PLoS ONE 2013, 8, e67798. [Google Scholar] [CrossRef] [PubMed]
- Sano, I.; Tanito, M.; Okuno, T.; Ishiba, Y.; Ohira, A. Estimation of the Melatonin Suppression Index through Clear and Yellow-Tinted Intraocular Lenses. Jpn. J. Ophthalmol. 2014, 58, 320–326. [Google Scholar] [CrossRef]
- Truong, W.; Zandi, B.; Trinh, V.Q.; Khanh, T.Q. Circadian Metric—Computation of Circadian Stimulus Using Illuminance, Correlated Colour Temperature and Colour Rendering Index. Build. Environ. 2020, 184, 107146. [Google Scholar] [CrossRef]
- Rea, M.S.; Nagare, R.; Figueiro, M.G. Corrigendum: Modeling Circadian Phototransduction: Quantitative Predictions of Psychophysical Data (Front. Neurosci., (2021), 15, (615322), 10.3389/Fnins.2021.615322). Front. Neurosci. 2022, 16, 849800. [Google Scholar] [CrossRef]
- Erdem, T.; Demir, H.V. Color-Enrichment Semiconductor Nanocrystals for Biorhythm-Friendly Backlighting. Z. Fur Phys. Chem. 2018, 232, 1457–1468. [Google Scholar] [CrossRef]
- Lucas, R.J.; Peirson, S.N.; Berson, D.M.; Brown, T.M.; Cooper, H.M.; Czeisler, C.A.; Figueiro, M.G.; Gamlin, P.D.; Lockley, S.W.; O’Hagan, J.B.; et al. Measuring and Using Light in the Melanopsin Age. Trends Neurosci. 2014, 37, 1–9. [Google Scholar] [CrossRef]
- Brown, T.M. Melanopic Illuminance Defines the Magnitude of Human Circadian Light Responses under a Wide Range of Conditions. J. Pineal Res. 2020, 69, e12655. [Google Scholar] [CrossRef]
- Shin, J.; Meridew, C.; Athey, A.; Killgore, W.; Gehrels, J.A. Basic and Translational Sleep Science. Sleep 2019, 41, A74. [Google Scholar]
- Oh, J.H.; Yang, S.J.; Do, Y.R. Healthy, Natural, Efficient and Tunable Lighting: Four-Package White LEDs for Optimizing the Circadian Effect, Color Quality and Vision Performance. Light Sci. Appl. 2014, 3, e141. [Google Scholar] [CrossRef]
- Esposito, T.; Houser, K. Correlated Color Temperature Is Not a Suitable Proxy for the Biological Potency of Light. Sci. Rep. 2022, 12, 20223. [Google Scholar] [CrossRef]
- Moore-ede, M.; Heitmann, A. Circadian Potency Spectrum in Light-Adapted Humans. J. Cell Sci. Ther. 2022, 13, 1–6. [Google Scholar] [CrossRef]
- Liu, T. Lighting Evaluation and Design for the Stockholm Metro System Based on Current Models for Non- Visual Responses Lighting Evaluation and Design for the Stockholm Metro System. Master’s Thesis, KTH Royal Institute Of Technology School Of Architecture and the Built Environment, Stockholm, Sweden, 2020. Available online: http://kth.divaportal.org/smash/get/diva2:1463572/FULLTEXT01.pdf (accessed on 26 March 2024).
- Kolberg, E.; Pallesen, S.; Hjetland, G.J.; Nordhus, I.H.; Thun, E.; Flo-Groeneboom, E. Insufficient Melanopic Equivalent Daylight Illuminance in Nursing Home Dementia Units across Seasons and Gaze Directions. Light. Res. Technol. 2022, 54, 163–177. [Google Scholar] [CrossRef]
- Acosta, I.; Campano, M.Á.; Leslie, R.; Radetsky, L. Daylighting Design for Healthy Environments: Analysis of Educational Spaces for Optimal Circadian Stimulus. Sol. Energy 2019, 193, 584–596. [Google Scholar] [CrossRef]
- Reinhart, C.F.; Mardaljevic, J.; Rogers, Z. Dynamic Daylight Performance Metrics for Sustainable Building Design. LEUKOS 2006, 3, 7–31. [Google Scholar] [CrossRef]
- Booth, A.; Papaioannou, D.; Sutton, A. Systematic Approaches to the Literature. Syst. Approaches A Succesful Lit. Rev. 2012. ISBN-13: 978-0857021359. [Google Scholar]
- Pagé, G.; Lavoie, K. Entre Soutien et Contrôle: La Parole Des Actrices et Des Acteurs Sociaux Sur Les Pratiques d’accompagnement Des Familles En Situation de Vulnérabilité. Serv. Soc. 2021, 67, 1. [Google Scholar] [CrossRef]
- van Duijnhoven, J.; Aarts, M.P.J.; Aries, M.B.C.; Rosemann, A.L.P.; Kort, H.S.M. Systematic Review on the Interaction between Office Light Conditions and Occupational Health: Elucidating Gaps and Methodological Issues. Indoor Built Environ. 2019, 28, 152–174. [Google Scholar] [CrossRef]
- Jiang, S. Positive Distractions and Play in the Public Spaces of Pediatric Healthcare Environments: A Literature Review. HERD Health Environ. Res. Des. J. 2020, 13, 171–197. [Google Scholar] [CrossRef] [PubMed]
- Stichler, J.F. Weighing the Evidence. HERD Health Environ. Res. Des. J. 2010, 3, 3–7. [Google Scholar] [CrossRef] [PubMed]
- Marquardt, G.; Motzek, T. How to Rate the Quality of a Research Paper: Introducing a Helpful Algorithm for Architects and Designers. HERD Health Environ. Res. Des. J. 2013, 6, 119–127. [Google Scholar] [CrossRef]
- Okkels, N.; Jensen, L.G.; Skovshoved, L.C.; Arendt, R.; Blicher, A.B.; Vieta, E.; Straszek, S. Lighting as an Aid for Recovery in Hospitalized Psychiatric Patients: A Randomized Controlled Effectiveness Trial. Nord. J. Psychiatry 2020, 74, 105–114. [Google Scholar] [CrossRef]
- Engwall, M.; Fridh, I.; Johansson, L.; Bergbom, I.; Lindahl, B. Lighting, Sleep and Circadian Rhythm: An Intervention Study in the Intensive Care Unit. Intensive Crit. Care Nurs. 2015, 31, 325–335. [Google Scholar] [CrossRef]
- Gleason, J.D.; Oishi, M.; Simkulet, M.; Tuzikas, A.; Brown, L.K.; Brueck, S.R.J.; Karlicek, R.F. A Novel Smart Lighting Clinical Testbed. In Proceedings of the 2017 39th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Jeju Island, Republic of Korea, 11–15 July 2017; IEEE: Piscataway, NJ, USA, 2017; pp. 4317–4320. [Google Scholar] [CrossRef]
- Canazei, M.; Weninger, J.; Pohl, W.; Marksteiner, J.; Weiss, E.M. Effects of Dynamic Bedroom Lighting on Measures of Sleep and Circadian Rest-Activity Rhythm in Inpatients with Major Depressive Disorder. Sci. Rep. 2022, 12, 6137. [Google Scholar] [CrossRef] [PubMed]
- Soltic, S.; Chalmers, A. Optimization of LED Lighting for Clinical Settings. J. Healthc. Eng. 2019, 2019, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Bernhofer, E.I.; Higgins, P.A.; Daly, B.J.; Burant, C.J.; Hornick, T.R. Hospital Lighting and Its Association with Sleep, Mood and Pain in Medical Inpatients. J. Adv. Nurs. 2014, 70, 1164–1173. [Google Scholar] [CrossRef] [PubMed]
- Estrup, S.; Kjer, C.K.W.; Poulsen, L.M.; Gøgenur, I.; Mathiesen, O. Delirium and Effect of Circadian Light in the Intensive Care Unit: A Retrospective Cohort Study. Acta Anaesthesiol. Scand. 2018, 62, 367–375. [Google Scholar] [CrossRef] [PubMed]
- Flyvholm, A.; Sen, S.; Xylakis, E.; Nielsen, L.; Triantafyllidis, G.; Andresen, L.; Pedersen, M.M. A Personalised and Adaptive Intelligent System to Adjust Circadian Lighting for Elderly Housing. In Proceedings of the 15th International Symposium on Ambient Intelligence and Embedded Systems, Heraklion, Greece, 21–23 September 2016. [Google Scholar]
- Pohl, W.; Canazei, M.; Neier, L.M.; Tanzer, K.; Weninger, J. Health Effects of Biodynamic Ligting in Clinics. In Proceedings of the LUX EUROPA, European Lighting Conference, Ljubljana, Slovenia, 18–20 September 2017. [Google Scholar]
- van Lieshout-van Dal, E.; Snaphaan, L.; Bongers, I. Biodynamic Lighting Effects on the Sleep Pattern of People with Dementia. Build. Environ. 2019, 150, 245–253. [Google Scholar] [CrossRef]
- McCunn, L.J.; Wright, J. Hospital Employees’ Perceptions of Circadian Lighting: A Pharmacy Department Case Study. J. Facil. Manag. 2019, 17, 422–437. [Google Scholar] [CrossRef]
- Scott, J.; Langsrud, K.; Goulding, I.R.; Kallestad, H. Let There Be Blue-Depleted Light: In-Patient Dark Therapy, Circadian Rhythms and Length of Stay. BJPsych Adv. 2021, 27, 73–84. [Google Scholar] [CrossRef]
- Rea, M.S.; Figueiro, M.G.; Bierman, A.; Bullough, J.D. Circadian Light. J. Circadian Rhythm. 2010, 8, 2. [Google Scholar] [CrossRef]
- Wilkerson, A.; Safranek, S.; Irvin, L.; Tredinnick, L. Lighting System Control Data to Improve Design and Operation: Tunable Lighting System Data from NICU Patient Rooms. LEUKOS 2023, 19, 94–109. [Google Scholar] [CrossRef]
- Grissinger, M. An Exhausted Workforce Increases the Risk of Errors. P T A Peer-Rev. J. Formul. Manag. 2009, 34, 120–123. [Google Scholar]
- Studer, P.; Brucker, J.M.; Haag, C.; Van Doren, J.; Moll, G.H.; Heinrich, H.; Kratz, O. Effects of Blue- and Red-Enriched Light on Attention and Sleep in Typically Developing Adolescents. Physiol. Behav. 2019, 199, 11–19. [Google Scholar] [CrossRef]
- Graves, E.; Davis, R.G.; DuBose, J.; Campiglia, G.C.; Wilkerson, A.; Zimring, C. Lighting the Patient Room of the Future: Evaluating Different Lighting Conditions for Performing Typical Nursing Tasks. HERD Health Environ. Res. Des. J. 2021, 14, 234–253. [Google Scholar] [CrossRef] [PubMed]
- Pechacek, C.S.; Andersen, M.; Lockley, S.W. Preliminary Method for Prospective Analysis of the Circadian Efficacy of (Day)Light with Applications to Healthcare Architecture. LEUKOS—J. Illum. Eng. Soc. N. Am. 2008, 5, 1–26. [Google Scholar] [CrossRef]
- Acosta, I.; Leslie, R.; Figueiro, M. Analysis of Circadian Stimulus Allowed by Daylighting in Hospital Rooms. Light. Res. Technol. 2017, 49, 49–61. [Google Scholar] [CrossRef]
- Song, H.; Jiang, W.; Cui, P. A Study on Nonvisual Effects of Natural Light Environment in a Maternity Ward of a Hospital in Cold Area. BioMed Res. Int. 2022, 2022, 8608892. [Google Scholar] [CrossRef]
- Carmon, D.; Altomonte, S. Lighting for Circadian Well-Being: A Simulation-Based Workflow for the Visual and Non-Visual Lighting Design of a Nursing Home. In Proceedings of the 17th IBPSA Conference, Bruges, Belgium, 1–3 September 2021. [Google Scholar]
- Englezou, M.; Michael, A. Evaluation of Visual and Non-Visual Effects of Daylighting in Healthcare Patient Rooms Using Climate-Based Daylight Metrics and Melanopic Metrics. E3S Web Conf. 2022, 362, 01003. [Google Scholar] [CrossRef]
- Brown, T.M.; Brainard, G.C.; Cajochen, C.; Czeisler, C.A.; Hanifin, J.P.; Lockley, S.W.; Lucas, R.J.; Münch, M.; O’Hagan, J.B.; Peirson, S.N.; et al. Recommendations for Daytime, Evening, and Nighttime Indoor Light Exposure to Best Support Physiology, Sleep, and Wakefulness in Healthy Adults. PLoS Biol. 2022, 20, e3001571. [Google Scholar] [CrossRef]
- Illuminating Engineering Society. ANSI/IES RP-29-22, Recommended Practice: Lighting Hospital and Healthcare Facilities; IES: New York, NY, USA, 2022. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).