Abstract
The validity and reliability of the Lower Extremity Motor Coordination Test (LEMOCOT) were assessed in patients with multiple sclerosis (MS). The study involved 60 participants diagnosed with MS (mean age: 48.13 years, range: 24–80 years). Intra-rater reliability was assessed within-day (n = 12), and inter-rater reliability was assessed within-day (n = 45) and between-days (n = 22). For known-groups validity, test scores were compared between participants of different sexes; for convergent validity, test scores were correlated with age, the Five-Repetition Sit-to-Stand test (FSTS), the Berg Balance Scale (BBS), the Lower Extremity Functional Scale (LEFS), and the Expanded Disability Status Scale (EDSS). To test the discriminant validity, the LEMOCOT test scores were correlated with the Mini-Mental State Evaluation (MMSE) and compared according to social history (living alone or not). The LEMOCOT test was tested under three different conditions and found to be very reliable (intraclass correlation coefficient, ICC2,1 > 0.94) with an acceptable error level (standard error of the measurement, SEM, between 1.39 and 3.47 targets and 95% minimum detectable change; MDC95%, between 3.84 and 9.58 targets). Convergent validity was verified, as the LEMOCOT registered very strong correlations with the FSTS test (r = −0.851) and the BBS scale (r = 0.815), a strong correlation with the LEFS scale (r = 0.78), a moderate correlation with the EDSS scale (r = −0.634), all highly significant (p < 0.001), and a weak correlation with age (r = −0.332, p < 0.01). Discriminant validity was also confirmed, as the LEMOCOT demonstrated a weak correlation with the MMSE scale (r = 0.365, p = 0.017) and no differences relative to living environment or sex. The LEMOCOT demonstrated excellent reliability and validity for patients with MS.
1. Introduction
Multiple Sclerosis (MS) is defined as a chronic, autoimmune, inflammatory disease of the central nervous system (CNS) [1]. There is degeneration and inflammation of the white and gray matter of the CNS, resulting in a disturbance in the cognitive and motor levels of the patients [2]. It occurs with greater frequency in the age group of 20–50 years, with twice the probability of occurrence of the disease in the female sex [1,3,4,5]. Severe fatigue, muscle weakness, spasticity, paresthesias, motor dysfunctions, communication disorders, balance disorders, and reduced motor coordination in the lower limbs (LLs), resulting in gait disturbance and falls as a consequence, are some of the clinical characteristics of the disease [6,7,8,9].
In this population group, the strength is reduced in the LLs compared to healthy individuals, which makes the deficit even more pronounced when the muscle contractions are performed at a higher speed [10,11]. During walking, it is necessary to have correct motor coordination of the body parts, as well as precise positioning of the foot during the support phase, and to be able to respond to internal and external stimuli, resulting in detailed positioning of the foot during walking and thus ensuring safe movement and avoiding falls [12]. Therefore, the existence of an appropriate evaluation of the coordination of the movement of the LLs with valid and reliable tools is a very important factor for the rehabilitation of patients with neurological gait disorders [13,14,15].
One of the tests to evaluate motor coordination is the Lower Extremity Motor Coordination Test (LEMOCOT) [12,13,14,16]. The LEMOCOT has been used and is a reliable and valid test for the motor coordination of LL in patients with stroke [14,16] and Autosomal Recessive Spastic Charlevoix–Saguenay (ARSACS) [17]. It is also one of the best prognostic indicators of social participation after stroke rehabilitation, with a program of intensive functional intervention lasting 6 months, or for any changes in the coordination of movements during the patient’s stay in an intensive care unit [14,18]. Furthermore, it is used for the assessment of rehabilitation in elderly people with LL impairment, as well as after surgery to assess the speed of recovery [19]. The LEMOCOT has been used as a clinical tool to evaluate the motor coordination of LLs in patients with MS [14,15,16]. It assesses the ability of individuals to perform controlled, precise, rapid, and repetitive movements, taking into account the speed as well as the quality of the movement. The LEMOCOT evaluates and quantifies the quality of movement.
The objective of this study was to test the validity and reliability of the LEMOCOT in patients with MS as an initial evaluation of its measurement properties.
2. Materials and Methods
2.1. Participants
Sixty adults (31 men and 29 women), aged 24–80 years (mean age: 48.13 years (SD: 10.7)), consented to participate in the study. Participants were diagnosed with MS in the early and middle stages of the disease and were selected based on convenience and purposeful sampling. Subjects had a mean weight of 76.43 kg (range: 49–110 kg, SD: 12.29), a mean height of 171.88 cm (range: 150–190 cm, SD: 9.711), and an Expanded Disability Status Scale (EDSS) mean of 2.34 (score range: 1–5, SD: 1.36). EDSS classifies patients into mild disability (EDSS 0–3.5), moderate disability (EDSS 4.0–5.5), and severe disability (EDSS 6.0–6.5) [9,20]. Participants had MS duration mean: 12.55 years (SD: 9.58) (1–33 years).
2.2. Ethics
The research took place in the outpatient clinic of the Neurological Clinic of the Athens Naval Hospital in the period 07/2022-04/2023. Prior approval was granted by the Scientific Council of the Athens Naval Hospital (Prot. No.: 3797/15.04.2022) and the Ethics Committee of the University of West Attica (No. Prot.: 67991/21.07.2022), according to the Declaration of Helsinki principles. All patients were informed about the methods and purpose of the study, followed by a written invitation and detailed information through an information leaflet. Those who agreed to participate completed the relevant consent form. Each patient was assigned a code to maintain confidentiality and anonymity.
2.3. Study Design
The test-retest reliability within the same day (intra- and inter-rater) and between days (inter-rater), as well as the construct validity (known groups, convergent, divergent) of the LEMOCOT, were systematically examined.
2.4. Procedures
Patients performed the LEMOCOT [17], as well as 5 other valid and reliable instruments, on the same day in the outpatient neurology clinic. Specifically, the Five-Repetition Sit-to-Stand test (FSTS) [21] was performed after the LEMOCOT. The patients then filled in the following scales with clarifications provided by either of the examiners administering the scales at the time: (a) the Berg Balance Scale (BBS) [22,23] and (b) the Lower Extremity Functional Scale (LEFS) [24]; (c) the Mini-Mental State Evaluation (MMSE) was completed only for patients as deemed necessary by the principal investigator (D.Z.) and their attending physician (M.M.) (n = 42), with the rest of participants given the score corresponding to healthy individuals (n = 18). The order of performing the tests and completing the scales was always the same [25]. Finally, the results of the Expanded Disability Status Scale (EDSS) evaluation were recorded from the patient’s history. This history was taken by their treating neurologist and the principal investigator. In addition, information regarding the participant’s living environment (living alone or not) was collected.
Reliability measurements were conducted by a physiotherapist (D.Z.—examiner 1) and a physical medicine and rehabilitation doctor (M.M.—examiner 2), in a randomized order for participants that were assessed by both examiners. Of the 60 participants, 45 were assessed by both examiners on the same day, with a 30-min time interval (within-day inter-rater reliability). Additionally, 12 participants were assessed twice on the same day with a 30-min time interval by the same examiner (within-day intra-rater reliability). Finally, reliability was examined in 22 patients by both examiners with a 4-week time interval between measurements (between-days inter-rater reliability). The initial aim was to re-assess all participants, which was not procedurally feasible for the clinic routine, so those who were re-examined in the outpatient clinic within the measurement period were re-evaluated on a second day. The LEMOCOT test was performed first with the dominant and then with the non-dominant LL. In order to minimize fatigue, the test was carried out in the morning to early afternoon, usually 9.00 am–1.30 pm.
To perform the LEMOCOT test, 2 targets—one central and one more distant—were placed 30 cm apart, attached to a thin piece of rigid foam on the floor (50 × 55 × 0.8 cm). The 2 targets had a red color and a diameter of 6 cm (Figure 1) [16,17].
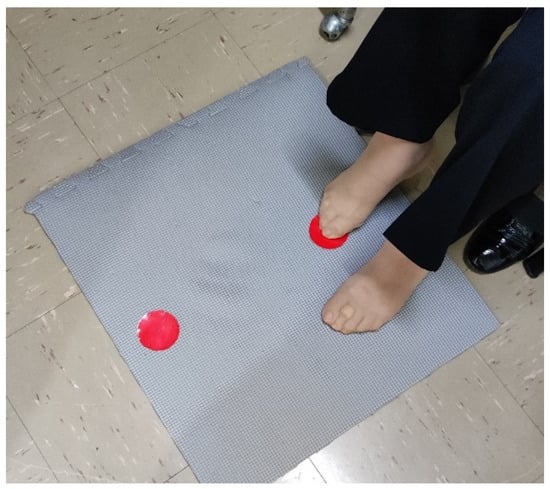
Figure 1.
Setup for conducting the LEMOCOT.
Participants were placed in a comfortable sitting position on a chair, without shoes. Their knees were bent at about 90°, the soles of their feet were in contact with the floor, and the heel of the LL under examination was initially placed on the proximal target. This position was varied according to the person’s height so that there was the same distance for each participant at 30 cm [14,15,16,17,25]. In order to start the test, the patient’s big toe was placed on the central target. Then, they had to alternately touch with the tip of their big toe the central and the farthest targets for 20 s.
The instruction was to move their foot as quickly as possible and touch the targets with the greatest possible accuracy. The number of targets sequentially touched in 20 secs was recorded [12,16,25]. Participants were instructed not to decrease the level of accuracy or movement quality to increase speed [14,15,16,25]. If the big toe did not touch the target, the target was not recorded. The initial toe placement on the proximal target was not counted [16,25]. A test trial was performed with the dominant LL for 5–10 s, and then the test was performed with the dominant LL for 20 s, and then with the non-dominant LL for another 20 s [14,16,17,25].
2.5. Statistical Analysis
All continuous variables were analyzed for normality of distribution with the Kolmogorov–Smirnov (KS) test. The descriptive statistics of participants and their scores on the scales used are reported in Table 1. Between-side (dominant vs non-dominant) comparisons were also performed (related samples t-tests).

Table 1.
Descriptive statistics of the first measurement taken for all scales used (n = 60).
The test-retest reliability was calculated using the two-way mixed effects absolute agreement single rater Intraclass Correlation Coefficient (ICC 2,1) [26], the standard error of the measurement (SEM), and the minimum detectable change (MDC95%) [27]. ICCs less than 0.5 were considered poor, 0.5–0.75 moderate, 0.75–0.90 good, and greater than 0.90 excellent [26]. The SEM and MDC95% are indicators of the error level inherent within the measurement, with the SEM denoting the amount of variability inherent in repeated measurements, and the MDC representing the smallest amount of change that can be detected between two time periods that is not due to measurement error [27].
For known-groups validity, test scores were compared between men and women, with independent samples t-tests; for convergent validity, test scores were correlated with age, the FSTS, the BBS, the LEFS, and the EDSS. Pearson’s correlation values were considered very weak if below 0.20, weak if 0.20–0.39, moderate if 0.40–0.59, strong if 0.60–0.79, and very strong if above 0.80 [28,29]. To test the discriminant validity, LEMOCOT test scores were correlated with the MMSE and compared according to the social history (living alone or not) [29]. An a priori sample size estimation was conducted to limit the possibility of incurring a type I error; therefore, for the eight hypotheses relating to the validity of the LEMOCOT (6 correlations and 2 between-group differences in interest), the adjusted a-level would be α = 0.005/8 = 0.00625. This means that to achieve 80% power with a fair correlation of r = 0.44, the required sample size would be n = 60 participants. An online program for computing power and sample size for correlational designs (https://sample-size.net/correlation-sample-size/ (accessed on 1 June 2023)) [30] was utilized.
All statistical analyses and processing were conducted with the IBM SPSS Statistics, v. 28.0 program. The significance level was set at α = 0.05.
3. Results
The scores of all variables were normally distributed (KS test, p > 0.05), apart from the EDSS scores (KS test, p < 0.001); therefore, patient scores on all scales used are analytically presented as mean (SD) values, as well as minimum and maximum scores, and for EDSS, as median (interquartile range) scores as well (Table 1).
For the study population, no significant differences were identified for the LEMOCOT between dominant and non-dominant sides (related samples t-test, p > 0.05).
3.1. Reliability Assessment
3.1.1. Intra-Rater Reliability
Intra-rater reliability was checked by the same examiner, recording the performance of the LEMOCOT in 12 people with MS, with the results presented in detail in Table 2A. Excellent intra-rater reliability was found with ICC2,1 (95% CI) = 0.96–0.97 (0.85–0.99), with acceptable error level SEM: 3.01–3.13 targets, and MDC95%: 8.32–9.58 targets.

Table 2.
LEMOCOT test (A) intra-rater within-day reliability (n = 12), (B) inter-rater within-day reliability (n = 45), and (C) inter-rater between-days reliability (n = 22) of patients with mild to moderate MS.
3.1.2. Inter-Rater Reliability
To check inter-rater reliability, the results of measurements by two examiners with the LEMOCOT test from 45 patients on the same day (Table 2B), and from 22 patients on different days (Table 2C), were analyzed. Excellent intra-rater reliability was found under both conditions, with ICC (95% CI) = 0.94–0.99 (0.89–0.99), acceptable error level SEM: 1.39–3.20 targets, and MDC: 3.84–8.84 targets.
3.2. Validity Examination
To test the convergent and discriminant validity of the LEMOCOT, the results of the LEMOCOT were correlated with performance scores of the FSTS test and the BBS, LEFS, EDSS, and MMSE scales from all participants (n = 60) with MS, as well as their age and sex.
3.2.1. Known Groups Validity Examination
No significant differences in the LEMOCOT scores could be detected between male (mean [SD]: 25.24 [15.75]) and female (mean [SD]: 23.05 [10.81]) participants (mean difference: 2.19, t = 0.631, p = 0.53).
3.2.2. Convergent Validity Examination
Correlations between the LEMOCOT scores and the FSTS test, the EDSS, the BBS, the LEFS scales, and the participants’ age were performed to test for convergent validity of the LEMOCOT scores, with the LEMOCOT registering:
- very strong negative correlation with the FSTS test (r = −0.851, p < 0.001),
- strong negative correlation with the EDSS scale (r = −0.634, p < 0.001),
- very strong positive correlation with the BBS scale (r = 0.815, p < 0.001),
- strong positive correlation with the LEFS scale (r = 0.780, p < 0.001),
- weak negative correlation with participant’s age (r = −0.332, p < 0.01),
Therefore, the LEMOCOT’s convergent validity could be verified, as it strongly correlated to the FSTS test, the BBS, and the LEFS scales as well; it moderately correlated to the EDSS scale and demonstrated a fair correlation to the age of the participants.
3.2.3. Discriminant Validity Examination
To test the discriminant validity, the LEMOCOT scores were correlated with the MMSE scale, with their correlation found to be weak (r = 0.365, p = 0.017). Additionally, no significant differences in patient LEMOCOT scores were detected relative to their living environment (living alone or not).
4. Discussion
The LEMOCOT was thoroughly examined for reliability and validity in patients with MS. The test proved easy to administer, with participants able to understand how to appropriately perform the test with minimal instruction provided. No other special training or standardization was required between examiners prior to the test administration. Although blinding of the examiners could not be performed, the examiners themselves agreed not to influence participants at all during the test performance, omitting any verbal or other encouragement during the 20 s the LEMOCOT lasted. All instruction on correct test performance was provided beforehand and was standardized between examiners, as presented in Section 2.
For the sample of patients tested, the results showed no differences between the dominant and non-dominant LLs in people with early- and middle-stage MS; therefore, no asymmetries in the coordination of the LL movements in the present study could be identified. One might speculate that such coordination symmetry between the lower limbs might be related to force symmetry. However, in other studies such as the study by Farrell et al. (2021) [9], participating subjects with MS showed strength asymmetries in both upper limbs (ULs) and LLs, but that particular study included participants with MS that had progressed to a severe stage with equally severe impairments. Muscle weakness is considered one of the first symptoms of MS and indicates strength asymmetries in most muscle groups resulting in fatigue and gait disturbances in these individuals [9,11].
In our study, it was also observed that for test-retest reliability, the mean of the targets in the second measurement (both on the same and a different day) was slightly higher. A previous study examining test-retest reliability [16] reported a similar pattern of results in individuals with motor coordination problems, mostly patients with stroke. Desrosiers et al. (2005) [16] attributed this performance enhancement to the patient’s familiarity with the test at the second measurement. Since there was no intervention program between test-retest measurements, most likely the performance enhancement noted could also have been due to patient familiarization or temperature variation, as not all patients were re-measured at exactly the same time of day, depending on their appointment times, and fatigue relating to high temperatures may have affected measurements.
However, the intra- and inter-rater reliability was found to be excellent for both LLs, with ICC values ranging between 0.94 and 0.99, comparatively higher than another previous reliability study conducted in patients with stroke [16]. The SEM for test-retest measurements taken on either the same day by the same or different examiners or on different days by two different examiners was between 1.5 and 3.5 targets, representing the amount of variability due to measurement error upon repeated measurements. Similar SEM values (1.55–3.87 targets) were reported in a previous study of the LEMOCOT’s reliability in patients with stroke [16]. The MDC values denoting the amount of true change in a variable were 5.9–8.3 targets for the dominant LL and 4.22–9.58 targets for the non-dominant LL, depending on the type of reliability measured, indicating a true change occurring if 9–10 more targets were registered during the conduct of the LEMOCOT. Therefore, our study demonstrated adequate inter- and intra-rater reliability of this test in a Greek population of people with MS, satisfactory for further use in clinical practice.
To test for convergent validity, the LEMOCOT scores’ association with the FSTS test, BBS, EDSS, LEFS scales, and age were examined. The strongest negative correlation of the LEMOCOT test was found to be with the FSTS test. According to [21], the FSTS test is characterized as a time trial because patients must complete five repetitions of alternate sitting-to-standing as quickly as possible. It is an expected finding since, in the FSTS test, the time should be reduced, while in the LEMOCOT test, the targets should be increased to demonstrate increased motor coordination. Also, a very strong positive correlation was found with the BBS scale, which assesses functional balance and requires good coordination of the LLs, such as transfers from one chair to another, turning 360°, or placing the feet in succession on steps or stools [17,31].
The LEMOCOT test demonstrated a weak negative correlation with participants’ age, and the result was statistically significant. In the study by Lessard et al. (2017), for ARSACS sufferers, a negative association also emerged [17]. The MO of the LEMOCOT test measurements is moderately negatively correlated with the EDSS scale, meaning that the higher the score on the EDSS scale, the lower the coordination. Given that MS is a progressive disease, it is expected that the coordination of the movements in the LLs is burdened [17].
To test known-groups validity, differences in the LEMOCOT scores between participants of the different sexes were conducted; however, no significant differences were noted (p > 0.1). The results are similar to the study by Lessard et al. (2017), which reported how both sexes with ARSACS may show the same degree of reduction in coordination so that their difference will not be noticeable [17]. Therefore, the test scores seem to be not affected by sex for the tested sample of participants with MS. To assess the discriminant validity, a correlation of the LEMOCOT test with the MMSE cognitive test was carried out, with a weak correlation noted.
To test the discriminant validity, the LEMOCOT test was weakly correlated with the MMSE scale (r = 0.365). This trend for correlation raises issues of investigating the association of any cognitive or concentration deficits with the performance of different stages of MS on the test. The MO of the LEMOCOT test was correlated with the MMSE scale and their correlation was found to be weakly positive (r = 0.365, p = 0.017). Most likely, people with cognitive disorders do not score lower on the LEMOCOT test than people without cognitive disorders. Therefore, since cognitive impairment did not strongly affect LEMOCOT performance, it can be used in MS patients who present with mild to moderate cognitive impairment. Also, the study by [16] showed no trend of association in individuals with stroke. This is due to the fact that the participants had to understand the instructions they were going to follow, so they had little or no cognitive deficits.
4.1. Limitations
Our initial objective was to additionally correlate the LEMOCOT with both the 2-Minute Walk Test (2MWT) and the Timed Up and Go Test (TUG), which are reliable and valid tools for MS [32,33], but this was not possible due to lack of space in the outpatient clinic where all the other tests were administered. Furthermore, not all patients were evaluated a second time, as they did not attend the outpatient clinic again during the period that the study was in progress. Also, due to fatigue, some patients refused to participate or to be re-evaluated for a second time. The use of convenience sampling in this study, although justified due to time constraints, might have potentially resulted in selection bias, thereby influencing the generalizability of our results. Also, due to time constraints, longitudinal validity was not examined in our study. Finally, as there is no gold standard test to assess lower limb coordination, external criterion validity could not be examined.
4.2. Suggestions for Future Research
A future study to test inter-rater reliability on a larger sample of participants with MS may be necessary. Additionally, it is recommended to verify the current measurements in a larger sample, including patients with MS from various parts of Greece or other countries, so that the sample is not limited only to the prefecture of Attica and specifically to one hospital in Athens. Screening tools such as the LEMOCOT can be instrumental in designing rehabilitation programs that target LL movement coordination, resulting in improvement in patient quality of life, such as avoiding falls and improving walking ability under different conditions of speed or increased complexity, due to environmental influences in vulnerable populations such as people with MS.
5. Conclusions
The LEMOCOT, as a tool to assess LL coordination in patients with MS, demonstrated good known-groups, convergent, and discriminant validity, and very high intra- and inter-rater reliability, with measurement on the same and different days. Motor coordination tests in the LL, such as the LEMOCOT and the FSTS, showed a negative strong correlation. The LEMOCOT is proposed for further use in patients with MS.
Author Contributions
Conceptualization, V.S. and D.Z.; methodology, V.S., D.Z., T.K.D. and M.M.; validation, V.S., D.Z., T.K.D. and M.M.; formal analysis, G.A.K., D.Z., A.C. and V.S.; investigation, T.K.D., M.M., G.A.K., D.Z., A.C. and V.S.; resources, T.K.D., M.M., D.Z., A.C. and V.S.; data curation, G.A.K., D.Z., A.C. and V.S.; writing—original draft preparation, G.A.K., D.Z., A.C. and V.S.; writing—review and editing, G.A.K., D.Z., A.C. and V.S.; visualization, G.A.K., D.Z., A.C. and V.S.; supervision, V.S.; project administration, G.A.K., D.Z., M.M., A.C. and V.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Scientific Council of the Athens Naval Hospital (protocol code: 3797, date of approval: 15 April 2022) and the Ethics Committee of the University of West Attica, Athens, Greece (protocol code: 67991, date of approval: 21 July 2022).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patients to publish this paper.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors on request.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Castillo-Buenoa, I.; Ramos-Campob, D.J.; Rubio-Arias, J.A. Effects of full-body vibratory training in patients with multiple sclerosis: A systematic review. Neurología 2018, 33, 534–548. [Google Scholar]
- Ghahfarrokhi, M.M.; Banitalebi, E.; Faramarzi, M.; Motl, R. Feasibility and efficacy of home-based neurofunctional exercise vs. resistance exercise programs for ambulatory disability of multiple sclerosis patients with cognitive impairment. Mult. Scler. Relat. Disord. 2022, 58, 103400. [Google Scholar] [CrossRef]
- Kessler, M.; Martin, S. Physiotherapy Interventions in Patients with Neurological Diseases, 2nd ed.; Constantaras Medical Publications: Athens, Greece, 2015; pp. 547–549. [Google Scholar]
- Walton, C.; King, R.; Rechtman, L.; Kaye, W.; Leray, E.; Marrie, R.A.; Robertson, N.; La Rocca, N.; Uitdehaag, B.; van der Mei, I.; et al. Rising prevalence of multiple sclerosis worldwide: Insights from the Atlas of MS. Mult. Scler. J. 2020, 26, 1816–1821. [Google Scholar] [CrossRef]
- El-Wahsh, S.; Balandin, S.; Bogaardt, H.; Kumfor, F.; Ballard, K.J. Managing communication changes in persons with multiple sclerosis: Findings from qualitative focus groups. Int. J. Lang. Commun. Disord. 2022, 57, 680–694. [Google Scholar] [CrossRef]
- Doskas, T.; Vavougios, G.; Karampetsou, P.; Kormas, C.; Synadinakis, E.; Stavrogianni, K.; Sionidou, P.; Serdari, A.; Vorvolakos, T.; Iliopoulos, I.; et al. Neurocognitive impairment and social cognition in multiple sclerosis. Int. J. Neurosci. 2022, 132, 1229–1244. [Google Scholar] [CrossRef] [PubMed]
- Braley, T.J.; Chervin, R.D. Fatigue in multiple sclerosis: Mechanisms, evaluation, and treatment. Sleep 2010, 33, 1061–1079. [Google Scholar] [CrossRef] [PubMed]
- Abasıyanik, Z.; Kahraman, T. Effect of dual-task training on cognitive functions in persons with multiple sclerosis: A systematic review and meta-analysis. Mult. Scler. Relat. Disord. 2022, 62, 103801. [Google Scholar] [CrossRef]
- Farrell, J.W., III; Motl, R.W.; Learmonth, Y.C.; Pilutti, L.A. Persons with Multiple Sclerosis Exhibit Strength Asymmetries in both Upper and Lower Extremities. Physiotherapy 2021, 111, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Sieljacks, P.S.; Soberg, C.A.; Michelsen, A.S.; Dalgas, U.; Hvid, L.G. Lower extremity muscle strength across the adult lifespan in multiple sclerosis: Implications for walking and stair climbing capacity. Exp. Gerontol. 2020, 139, 111025. [Google Scholar] [CrossRef] [PubMed]
- Stagsted, R.A.; Ramari, C.; Skjerbaek, A.G.; Thrue, C.; Dalgas, U.; Hvid, L.G. Lower extremity muscle power—A critical determinant of physical function in aging and multiple sclerosis. Exp. Gerontol. 2021, 150, 111347. [Google Scholar] [CrossRef] [PubMed]
- Handelzalts, S.; Koren, Y.; Goldhamer, N.; Yeshurun Tayer, A.; Parmet, Y.; Shmuelof, L.; Bar Haim, S. Insights into motor performance deficits after stroke: An automated and refined analysis of the lower-extremity motor coordination test (LEMOCOT). J. Neuroeng. Rehabil. 2021, 18, 155. [Google Scholar] [CrossRef]
- Pinheiro, M.B.; Parreiras de Menezes, K.K.; Teixeira-Salmela, L.F. Review of the psychometric properties of lower limb motor coordination tests. Fisioter. Mov. 2014, 27, 541–553. [Google Scholar] [CrossRef][Green Version]
- Pinheiro, M.B.; Scianni, A.A.; Ada, L.; Faria, C.D.; Teixeira-Salmela, L.F. Reference Values and Psychometric Properties of the Lower Extremity Motor Coordination Test. Arch. Phys. Med. Rehabil. 2014, 95, 1490–1497. [Google Scholar] [CrossRef] [PubMed]
- Parreiras de Menezes, K.K.; Scianni, A.A.; Faria-Fortini, I.; Avelino, P.R.; Faria, C.; Teixeira-Salmela, L. Measurement properties of the lower extremity motor coordination test in individuals with stroke. J. Rehabil. Med. 2015, 47, 502–507. [Google Scholar] [CrossRef] [PubMed]
- Desrosiers, J.; Rochette, A.; Corriveau, H. Validation of a New Lower-Extremity Motor Coordination Test. Arch. Phys. Med. Rehabil. 2005, 86, 993–998. [Google Scholar] [CrossRef] [PubMed]
- Lessard, I.; Lavoie, C.; Côté, I.; Mathieu, J.; Brais, B.; Gagnon, C. Validity and reliability of the LEMOCOT in the adult ARSACS population: A measure of lower limb coordination. J. Neurol. Sci. 2017, 377, 193–196. [Google Scholar] [CrossRef] [PubMed]
- Desrosiers, J.; Malouin, F.; Richards, C.; Bourbonnais, D.; Rochette, A.; Bravo, G. Comparison of changes in upper and lower extremity impairments and disabilities after stroke. Int. J. Rehabil. Res. 2003, 26, 109–116. [Google Scholar] [PubMed]
- Antosiak-Cyrak, K.; Wiczyński, G.; Podciechowska, K.; Rostkowska, E. Reliability of a New Lower-Extremity Motor Coordination Test. Pol. J. Sport Tour. 2015, 22, 219–223. [Google Scholar] [CrossRef][Green Version]
- Kurtzke, J.F. Rating neurologic impairment in multiple sclerosis: An expanded disability status scale (EDSS). Neurology 1983, 33, 1444–1452. [Google Scholar] [CrossRef] [PubMed]
- Møller, A.B.; Bibby, B.M.; Skjerbæk, A.G.; Jensen, E.; Sørensen, H.; Stenager, E.; Dalgas, U. Validity and variability of the 5-repetition sit-to-stand test in patients with multiple sclerosis. Disabil. Rehabil. 2012, 34, 2251–2258. [Google Scholar] [CrossRef] [PubMed]
- Lampropoulou, S.; Gizeli, A.; Kalivioti, C.; Billis, E.; Gedikoglou, I.; Nowicky, A. Cross Cultural Adaptation of Berg Balance Scale in Greek for Various Balance Impairments. J. Phys. Med. Rehabil. Disabil. 2016, 2, 11. [Google Scholar]
- Ross, E.; Purtill, E.; Uszynski, M.; Hayes, S.; Casey, B.; Browne, C.; Coote, S. Cohort Study Comparing the Berg Balance Scale and the Mini-BESTest in People Who Have Multiple Sclerosis and Are Ambulatory. Phys. Ther. 2016, 96, 1448–1455. [Google Scholar] [CrossRef]
- Stasi, S.; Papathanasiou, G.; Korres, N.; Marinakis, G.; Chronopoulos, E.; Baltopoulos, P.I.; Papaioannou, N.A. Validation of the Lower Extremity Functional Scale in community-dwelling elderly people (LEFS-Greek); determination of functional status cut-off points using TUG test. Eur. Geriatr. Med. 2013, 4, 237–241. [Google Scholar] [CrossRef]
- Yıldırım, Y.; Kara, Β.; Erbayraktar, S.; Sayhan, S. Assessment of Lower Extremity Motor Coordination in operated patients. J. Musculoskelet. Res. 2008, 11, 107–115. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef]
- Weir, J.P. Quantifying test-retest reliability using the intraclass correlation coefficient and the SEM. J. Strength Cond. Res. 2005, 19, 231–240. [Google Scholar] [PubMed]
- Portney, L.G.; Watkins, M.P. Foundations of Clinical Research: Applications to Practice, 3rd International ed.; Pearson Education Ltd.: Harlow, UK, 2014. [Google Scholar]
- Evans, J.D. Straightforward Statistics for the Behavioral Sciences; Brooks/Cole Publishing: Pacific Grove, CA, USA, 1996. [Google Scholar]
- Hulley, S.B.; Cummings, S.R.; Browner, W.S.; Grady, D.G.; Newman, T.B. Designing Clinical Research: An Epidemiologic Approach, 4th ed.; Wolters Kluwer/Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2013; p. 79. [Google Scholar]
- Carr, J.; Shepherd, R. Neurological Rehabilitation: Optimizing Motor Performance, 2nd ed.; Churchill Livingstone: Edinburgh, UK, 2010. [Google Scholar]
- Sebastião, E.; Sandroff, B.M.; Learmonth, Y.C.; Motl, R.W. Validity of the Timed Up and Go Test as a Measure of Functional Mobility in Persons With Multiple Sclerosis. Arch. Phys. Med. Rehabil. 2016, 97, 1072–1077. [Google Scholar] [CrossRef] [PubMed]
- Scalzitti, D.A.; Harwood, K.J.; Maring, J.R.; Leach, S.J.; Ruckert, E.A.; Costello, E. Validation of the 2-Minute Walk Test with the 6-Minute Walk Test and Other Functional Measures in Persons with Multiple Sclerosis. Int. J. MS Care 2018, 20, 158–163. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).

