Fracture Resistance of CAD/CAM Onlays Versus Direct Composite Repairs for Ceramic Crown Chipping
Abstract
Featured Application
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample Preparation
2.2. Sample Size Calculation
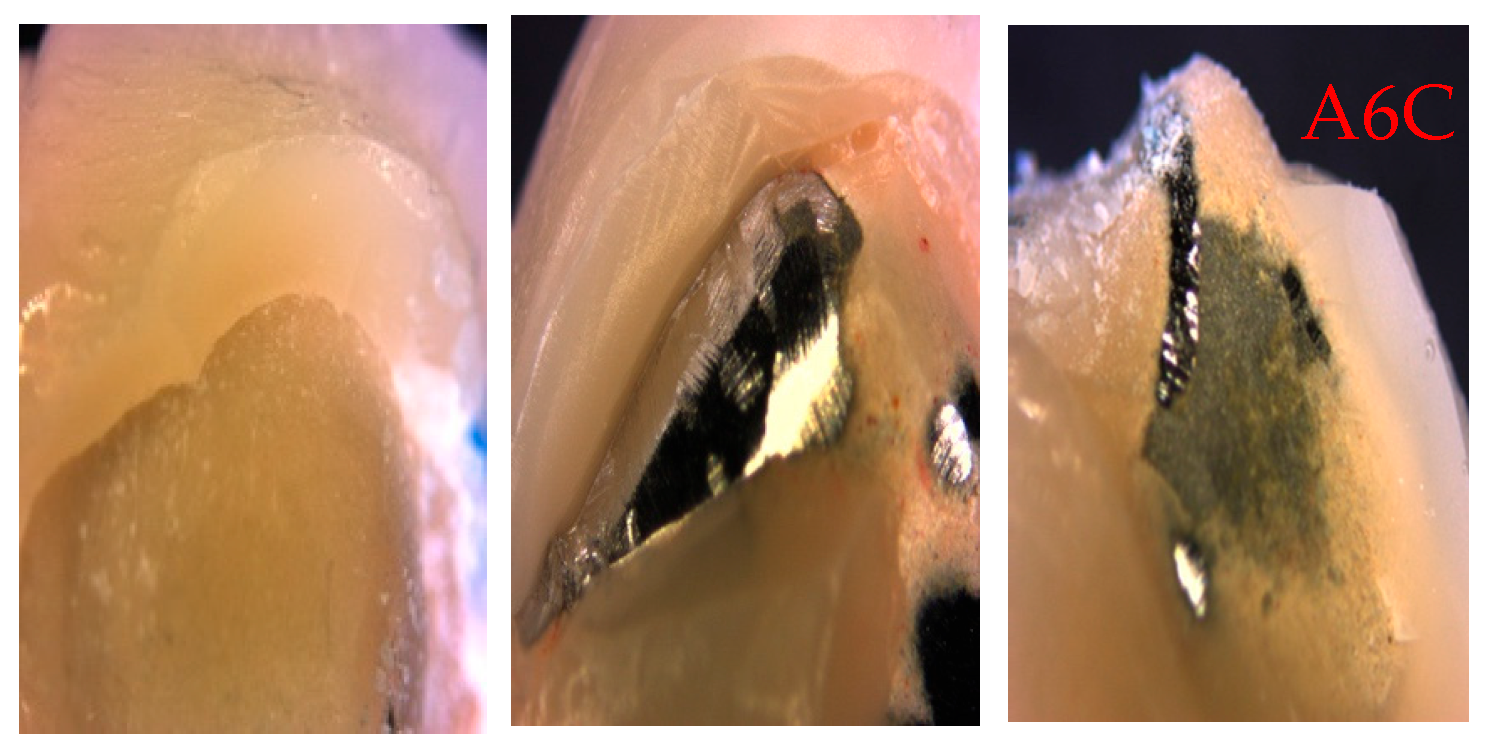
2.3. Crown Repair Process
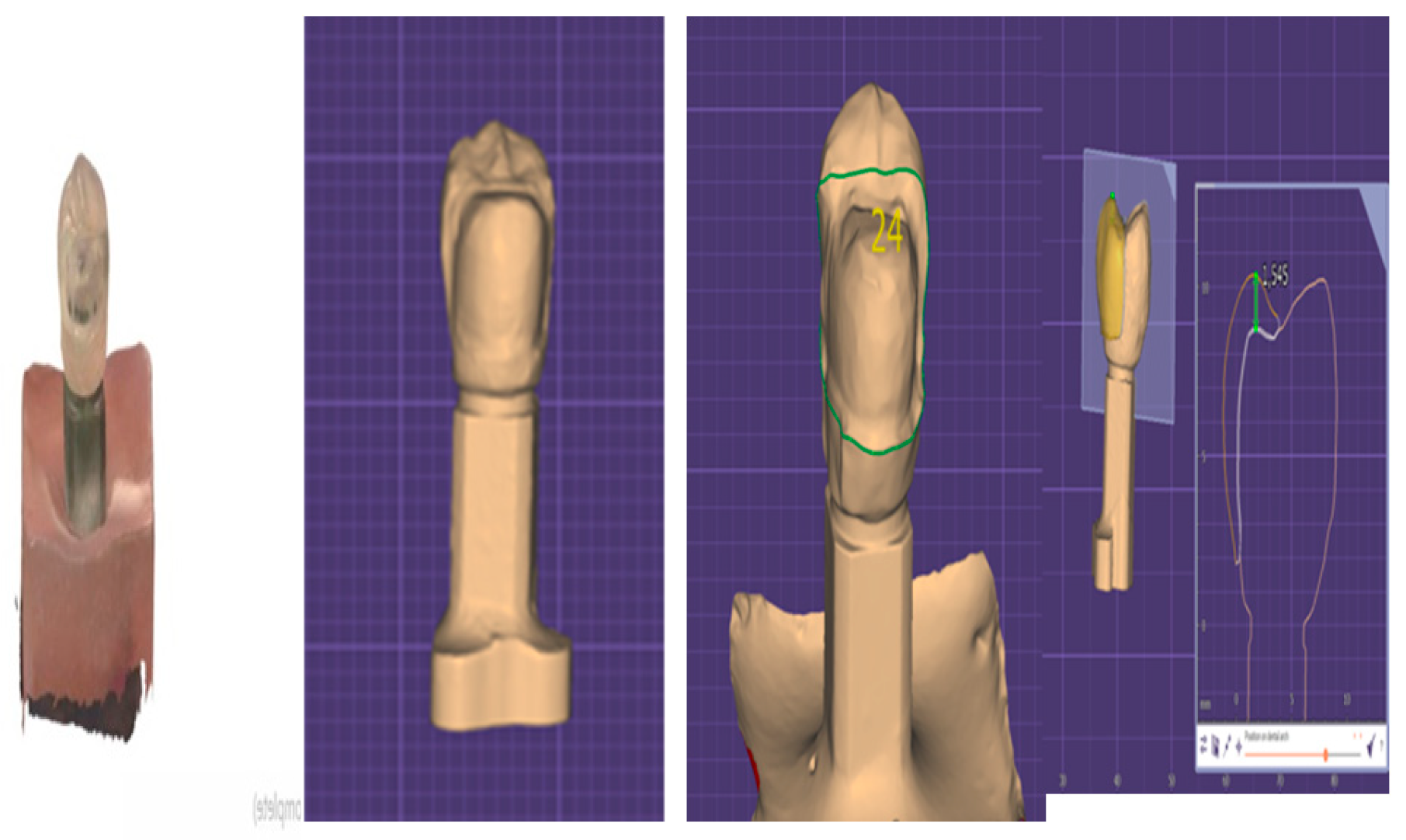
2.4. Restoration Fabrication
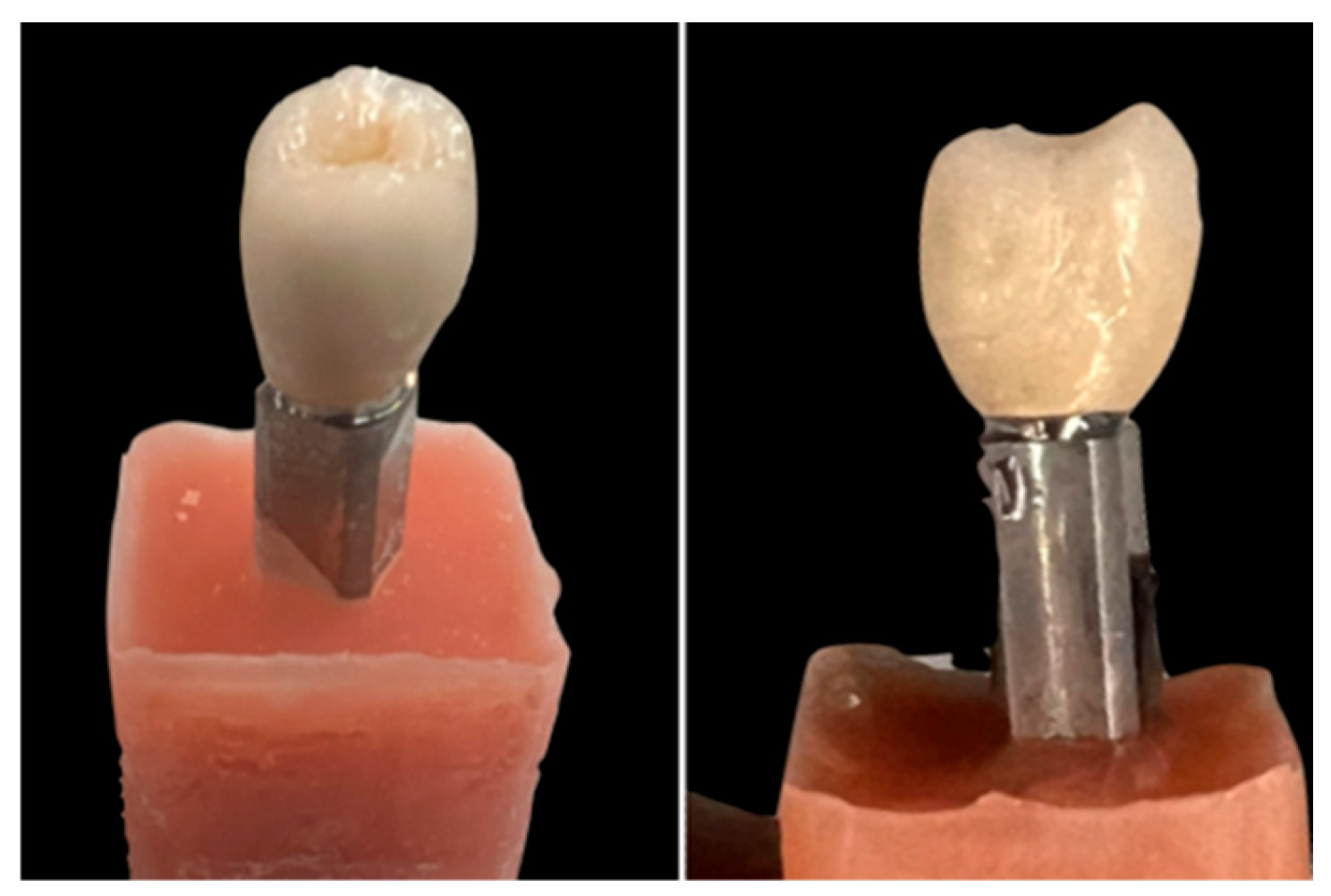
2.5. Cementation Process
2.6. Fracture Resistance Testing
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviation
| CAD/CAM | computer-aided design and computer-aided manufacturing |
References
- Aziz, A.; El-Mowafy, O. Six-year clinical performance of lithium disilicate glass-ceramic CAD-CAM versus metal-ceramic crowns. J. Adv. Prosthodont. 2023, 15, 44–54. [Google Scholar] [CrossRef] [PubMed]
- Ille, C.E.; Jivanescu, A.; Pop, D.; Stoica, E.T.; Flueras, R.; Talpos-Niculescu, I.C.; Cosoroaba, R.M.; Popovici, R.A.; Olariu, I. Exploring the Properties and Indications of Chairside CAD/CAM Materials in Restorative Dentistry. J. Funct. Biomater. 2025, 16, 46. [Google Scholar] [CrossRef] [PubMed]
- Rexhepi, I.; Santilli, M.; D’Addazio, G.; Tafuri, G.; Manciocchi, E.; Caputi, S.; Sinjari, B. Clinical Applications and Mechanical Properties of CAD-CAM Materials in Restorative and Prosthetic Dentistry: A Systematic Review. J. Funct. Biomater. 2023, 14, 431. [Google Scholar] [CrossRef]
- Guth, J.F.; Erdelt, K.; Keul, C.; Burian, G.; Schweiger, J.; Edelhoff, D. In vivo wear of CAD-CAM composite versus lithium disilicate full coverage first-molar restorations: A pilot study over 2 years. Clin. Oral Investig. 2020, 24, 4301–4311. [Google Scholar] [CrossRef]
- Suganna, M.; Kausher, H.; Tarek Ahmed, S.; Sultan Alharbi, H.; Faraj Alsubaie, B.; Ds, A.; Haleem, S.; Meer Rownaq Ali, A.B. Contemporary Evidence of CAD-CAM in Dentistry: A Systematic Review. Cureus 2022, 14, e31687. [Google Scholar] [CrossRef]
- Gracis, S.; Thompson, V.P.; Ferencz, J.L.; Silva, N.R.; Bonfante, E.A. A new classification system for all-ceramic and ceramic-like restorative materials. Int. J. Prosthodont. 2015, 28, 227–235. [Google Scholar] [CrossRef]
- Sulaiman, T.A.; Suliman, A.A.; Abdulmajeed, A.A.; Zhang, Y. Zirconia restoration types, properties, tooth preparation design, and bonding. A narrative review. J. Esthet. Restor. Dent. 2024, 36, 78–84. [Google Scholar] [CrossRef]
- Yeslam, H.E.; Freifrau von Maltzahn, N.; Nassar, H.M. Revolutionizing CAD/CAM-based restorative dental processes and materials with artificial intelligence: A concise narrative review. PeerJ 2024, 12, e17793. [Google Scholar] [CrossRef]
- Albergardi, A.B.S.; Limirio, J.; Gomes, J.M.L.; Pesqueira, A.A.; Pellizzer, E.P. Effect of surface treatments on the bond strength of resin-repaired resin matrix CAD-CAM ceramic: A scoping review. J. Dent. 2025, 154, 105594. [Google Scholar] [CrossRef]
- Emam, M.; Eldimeery, A.; Salah, T. Fracture Resistance of Custom Lithium Disilicate Implant Restorations with Two Fabrication Techniques and Two Designs. Int. J. Oral Maxillofac. Implants 2022, 37, 677–684. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Son, K.; Lee, K.B. Marginal and Internal Fit of Ceramic Restorations Fabricated Using Digital Scanning and Conventional Impressions: A Clinical Study. J. Clin. Med. 2020, 9, 4035. [Google Scholar] [CrossRef]
- Alghazzawi, T.F. Advancements in CAD/CAM technology: Options for practical implementation. J. Prosthodont. Res. 2016, 60, 72–84. [Google Scholar] [CrossRef]
- Belli, R.; Wendler, M.; Zorzin, J.I.; Lohbauer, U. Practical and theoretical considerations on the fracture toughness testing of dental restorative materials. Dent. Mater. 2018, 34, 97–119. [Google Scholar] [CrossRef]
- Sulaiman, T.A. Materials in digital dentistry—A review. J. Esthet. Restor. Dent. 2020, 32, 171–181. [Google Scholar] [CrossRef]
- Abu Alhuda, S.; Arossi, G.A.; Anagnostopoulos-King, F.; Alkhubaizi, Q.; Mokeem, L.S.; Melo, M.A.S.d. Current Evidence and Advances in CAD-CAM Resin Composite Blocks for Chairside Dental Restorations: Where Are We Now? A Scoping Review. Appl. Sci. 2024, 14, 10423. [Google Scholar] [CrossRef]
- Cui, X.; Wang, F.; Tang, K.; Dai, S.; Duan, L.; Niu, L.; Vyas, Y.; Tay, F.; Chen, J.; Zhang, X. A narrative review of the factors that affect the mechanical properties of polymer-infiltrated ceramics used for dental restorations. J. Dent. 2025, 157, 105732. [Google Scholar] [CrossRef]
- Lupu, I.C.; Tatarciuc, M.S.; Vitalariu, A.M.; Bobu, L.; Diaconu, D.A.; Vasluianu, R.I.; Stamatin, O.; Cretu, C.I.; Dima, A.M. Bonding Strategies for Zirconia Fixed Restorations: A Scoping Review of Surface Treatments, Cementation Protocols, and Long-Term Durability. Biomimetics 2025, 10, 632. [Google Scholar] [CrossRef] [PubMed]
- Moreschi, L.; De Carli, J.P.; Fuhr, M.C.S.; Dos Santos, R.B.; da Silva, P.R.P.; Corazza, P.H. Evaluation of compressive and adhesive strengths of a hybrid ceramic and 5Y-PSZ zirconia cemented with three different materials. Eur. J. Oral Sci. 2025, 133, e70017. [Google Scholar] [CrossRef] [PubMed]
- Szawioła-Kirejczyk, M.; Chmura, K.; Gronkiewicz, K.; Gala, A.; Loster, J.E.; Ryniewicz, W. Adhesive Cementation of Zirconia Based Ceramics-Surface Modification Methods Literature Review. Coatings 2022, 12, 1067. [Google Scholar] [CrossRef]
- Alsaeed, A.Y. Bonding CAD/CAM materials with current adhesive systems: An overview. Saudi Dent. J. 2022, 34, 259–269. [Google Scholar] [CrossRef]
- Cuzic, C.; Rominu, M.; Pricop, A.; Urechescu, H.; Pricop, M.O.; Rotar, R.; Cuzic, O.S.; Sinescu, C.; Jivanescu, A. Clinician’s Guide to Material Selection for All-Ceramics in Modern Digital Dentistry. Materials 2025, 18, 2235. [Google Scholar] [CrossRef]
- Nogueira, I.O.; Oliveira, P.F.G.; Magno, M.B.; Ferreira, D.; Maia, L.C.; Rabello, T.B. Does the application of an adhesive layer improve the bond strength of etched and silanized glass-ceramics to resin-based materials? A systematic review and meta-analysis. J. Prosthet. Dent. 2021, 125, 56–64. [Google Scholar] [CrossRef] [PubMed]
- Alenezi, A.; Alsweed, M.; Alsidrani, S.; Chrcanovic, B.R. Long-Term Survival and Complication Rates of Porcelain Laminate Veneers in Clinical Studies: A Systematic Review. J. Clin. Med. 2021, 10, 1074. [Google Scholar] [CrossRef] [PubMed]
- Sailer, I.; Strasding, M.; Valente, N.A.; Zwahlen, M.; Liu, S.; Pjetursson, B.E. A systematic review of the survival and complication rates of zirconia-ceramic and metal-ceramic multiple-unit fixed dental prostheses. Clin. Oral Implants Res. 2018, 29 (Suppl. 16), 184–198. [Google Scholar] [CrossRef]
- Harouny, R.; Hardan, L.; Harouny, E.; Kassis, C.; Bourgi, R.; Lukomska-Szymanska, M.; Kharouf, N.; Ball, V.; Khairallah, C. Adhesion of Resin to Lithium Disilicate with Different Surface Treatments before and after Salivary Contamination-An In-Vitro Study. Bioengineering 2022, 9, 286. [Google Scholar] [CrossRef]
- Blatz, M.B.; Alvarez, M.; Sawyer, K.; Brindis, M. How to Bond Zirconia: The APC Concept. Compend. Contin. Educ. Dent. 2016, 37, 611–617; quiz 618. [Google Scholar]
- Beji Vijayakumar, J.; Varadan, P.; Balaji, L.; Rajan, M.; Kalaiselvam, R.; Saeralaathan, S.; Ganesh, A. Fracture resistance of resin based and lithium disilicate endocrowns. Which is better?—A systematic review of in-vitro studies. Biomater. Investig. Dent. 2021, 8, 104–111. [Google Scholar] [CrossRef]
- Kavut, I.; Kulunk, S. Evaluation of the core thickness and resin cement on the fracture strength of zirconia-based multilayer computer-aided design/computer-aided manufacturing ceramic crowns. J. Int. Dent. Med. 2019, 7, 16. [Google Scholar] [CrossRef]
- Malpartida-Carrillo, V.; Tinedo-Lopez, P.L.; Ortiz-Culca, F.; Guerrero, M.E.; Amaya-Pajares, S.P.; Ozcan, M. Fracture Resistance of Cement-retained, Screw-retained, and Combined Cement- and Screw-retained Metal-ceramic Implant-supported Molar Restorations. J. Contemp. Dent. Pract. 2020, 21, 868–873. [Google Scholar]
- Sailer, I.; Makarov, N.A.; Thoma, D.S.; Zwahlen, M.; Pjetursson, B.E. All-ceramic or metal-ceramic tooth-supported fixed dental prostheses (FDPs)? A systematic review of the survival and complication rates. Part I: Single crowns (SCs). Dent. Mater. 2015, 31, 603–623. [Google Scholar] [CrossRef]
- Teichmann, M.; Gockler, F.; Weber, V.; Yildirim, M.; Wolfart, S.; Edelhoff, D. Ten-year survival and complication rates of lithium-disilicate (Empress 2) tooth-supported crowns, implant-supported crowns, and fixed dental prostheses. J. Dent. 2017, 56, 65–77. [Google Scholar] [CrossRef]
- Ashour, A.M.; El-Kateb, M.M.; Azer, A.S. The effect of two preparation designs on the fracture resistance and marginal adaptation of two types of ceramic crowns using CAD/CAM technology (In vitro study). BMC Oral Health 2024, 24, 1065. [Google Scholar] [CrossRef]
- Hofsteenge, J.W.; Carvalho, M.A.; Botenga, E.L.F.; Cune, M.S.; Ozcan, M.; Magne, P.; Gresnigt, M.M.M. Effect of preparation design on fracture strength of compromised molars restored with direct composite resin restorations: An in vitro and finite element analysis study. J. Prosthet. Dent. 2024, 131, 1150–1158. [Google Scholar] [CrossRef] [PubMed]
- Refaie, A.; Bourauel, C.; Fouda, A.M.; Keilig, L.; Singer, L. The effect of cyclic loading on the fracture resistance of 3D-printed and CAD/CAM milled zirconia crowns-an in vitro study. Clin. Oral Investig. 2023, 27, 6125–6133. [Google Scholar] [CrossRef] [PubMed]
- Gungor, M.B.; Nemli, S.K.; Bal, B.T.; Tamam, E.; Yilmaz, H.; Aydin, C. Fracture resistance of monolithic and veneered all-ceramic four-unit posterior fixed dental prostheses after artificial aging. J. Oral Sci. 2019, 61, 246–254. [Google Scholar] [CrossRef] [PubMed]
- Channarong, W.; Lohawiboonkij, N.; Jaleyasuthumkul, P.; Ketpan, K.; Duangrattanaprathip, N.; Wayakanon, K. Fracture resistance of bonded ceramic overlay restorations prepared in various designs. Sci. Rep. 2022, 12, 16599. [Google Scholar] [CrossRef]
- Oyar, P.; Durkan, R. Effect of cavity design on the fracture resistance of zirconia onlay ceramics. Niger. J. Clin. Pract. 2018, 21, 687–691. [Google Scholar] [CrossRef]
- Alassar, R.M.; Samy, A.M.; Abdel-Rahman, F.M. Effect of cavity design and material type on fracture resistance and failure pattern of molars restored by computer-aided design/computer-aided manufacturing inlays/onlays. Dent. Res. J. 2021, 18, 14. [Google Scholar] [CrossRef]
- Jurado, C.A.; Mekled, S.; Abuhammoud, S.; Azpiazu-Flores, F.X.; Vegh, D.; Wang, T.; Morton, D. Fracture resistance of partial and complete coverage veneers and ceramic crowns for maxillary central incisors. J. Prosthet. Dent. 2024, 132, 420.e1–420.e6. [Google Scholar] [CrossRef]

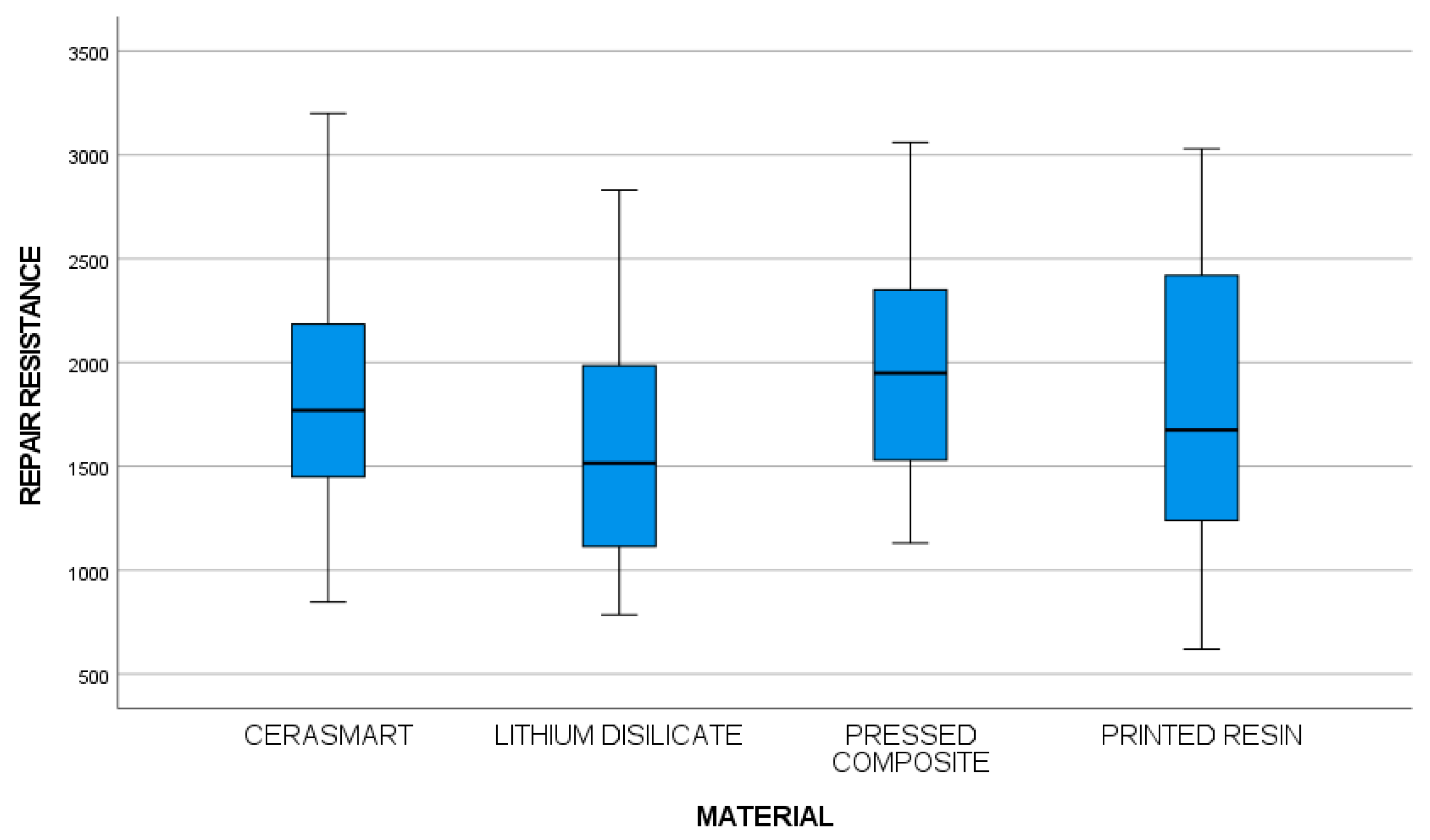
| Sample | Average | Median | Standard Deviation | Minimum | Maximum | Range | Standardized Kurtosis | Standardized Skew | |
|---|---|---|---|---|---|---|---|---|---|
| GROUP A: Original metal ceramic crowns (initial crowns) | 100 | 2969.88 | 3033.50 | 742.91 | 1363 | 4153 | 2790 | −0.62 | −0.37 |
| GROUP B: Repair hybrid milled (Cerasmart) onlay crowns | 20 | 1901.35 | 1770.00 | 668.54 | 847.0 | 3200.0 | 2353.0 | −0.24 | 0.75 |
| GROUP C: Repair disilicate ceramic onlay crowns | 20 | 1578.8 | 1444.5 | 5,185,978 | 785 | 2831 | 2046.0 | 0.45 | 0.23 |
| GROUP D: Repair pressed resin onlay crowns | 20 | 1997 | 1875 | 5,665,231 | 1130 | 3060 | 1930 | 0.74 | 0.21 |
| GROUP E: Repair printed resin onlay crowns | 20 | 1826.8 | 1480 | 761,221 | 620 | 3030 | 2410 | 0.87 | 0.16 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodeja-Vazquez, M.; Figueras-Álvarez, O.; Aschkar-Carretero, A.; Corominas-Delgado, C.; Costa-Palau, S.; Cabratosa-Termes, J.; Real-Voltas, F. Fracture Resistance of CAD/CAM Onlays Versus Direct Composite Repairs for Ceramic Crown Chipping. Appl. Sci. 2025, 15, 10706. https://doi.org/10.3390/app151910706
Rodeja-Vazquez M, Figueras-Álvarez O, Aschkar-Carretero A, Corominas-Delgado C, Costa-Palau S, Cabratosa-Termes J, Real-Voltas F. Fracture Resistance of CAD/CAM Onlays Versus Direct Composite Repairs for Ceramic Crown Chipping. Applied Sciences. 2025; 15(19):10706. https://doi.org/10.3390/app151910706
Chicago/Turabian StyleRodeja-Vazquez, Mariona, Oscar Figueras-Álvarez, Alma Aschkar-Carretero, Cristina Corominas-Delgado, Santiago Costa-Palau, Josep Cabratosa-Termes, and Francisco Real-Voltas. 2025. "Fracture Resistance of CAD/CAM Onlays Versus Direct Composite Repairs for Ceramic Crown Chipping" Applied Sciences 15, no. 19: 10706. https://doi.org/10.3390/app151910706
APA StyleRodeja-Vazquez, M., Figueras-Álvarez, O., Aschkar-Carretero, A., Corominas-Delgado, C., Costa-Palau, S., Cabratosa-Termes, J., & Real-Voltas, F. (2025). Fracture Resistance of CAD/CAM Onlays Versus Direct Composite Repairs for Ceramic Crown Chipping. Applied Sciences, 15(19), 10706. https://doi.org/10.3390/app151910706






