Abstract
Postural abnormalities in the sagittal plane are common in Parkinson’s disease (PD) and increase the risk of falls. Previous studies have reported short-term benefit of corrective corsets in PD patients assessed by clinical and instrumental methods, while long-term effects on sagittal posture in upright standing and during walking remain unexplored. Fifteen PD patients with postural abnormalities on the sagittal plane, evaluated via the NeuroPostureApp, and ten healthy subjects matched for age and BMI were assessed by 3D motion analysis in upright posture. Then, the PD patients were evaluated with and without the K1 Posture Keeper during standing and walking at baseline (T0) and after three months of use (T1). The results showed an anteriorization of the head–cervical region with respect to the trunk and a whole-body misalignment in PD patients compared to healthy controls. The use of the K1 Posture Keeper induced a back shift of the nasion with a better alignment of the head with respect to the trunk, pelvis, and feet in upright standing and during walking, underlining an improvement in the sagittal alignment of the entire body in PD. These findings showed the therapeutical role of K1 Posture Keeper on sagittal posture in static and dynamic conditions, potentially due to proprioceptive reorganization.
1. Introduction
Parkinson’s disease (PD) is the second most common neurodegenerative disease, due to a progressive degeneration of the nigrostriatal dopaminergic pathway with loss of substantia nigra pars compacta (SNpc) neurons and depletion of dopamine [1].
PD causes several motor impairments such as slow movements, rigidity, reduced mobility, disturbances of balance, impaired gait, recurrent falls, and postural abnormalities [1,2,3,4].
Posture is the position of the human-body segments in space, physiologically placed within normal ranges in upright standing [5] and during walking [6]. The central nervous system (CNS) regulates postural stability via processing the peripheral sensory afferents (visual, stomatognathic, vestibular, and somatosensory) and modulating neuromuscular adaptations of the myofascial chains [7] with biomechanical strategies against gravity [7,8,9], trying to ensure balance in the most unstable postural conditions [10].
Axial postural abnormalities are not uncommon in PD [4,11,12], and are defined as involuntary, reversible postures including bending of the trunk on the frontal and sagittal plane as well as anterior bending of the neck [13]. The pathophysiology of these conditions is still largely obscure [14]; however a recent Task Force Consensus by the International Movement Disorder Society clarified nosology and cut-off values to classify the six main axial postural abnormalities in PD [13]. On the sagittal plane, the term “camptocormia” was defined as an anterior trunk bending >45° (with thoracic fulcrum) or >30° (with lumbar fulcrum), whereas the term “Anterior trunk flexion” was proposed with the thoracic (≥25° to ≤45°) or lumbar fulcrum (>15° to ≤30°). With regards to the neck bending, “antecollis” was used to define an anterior neck bending of >45°, whereas “anterior neck flexion” was used for alterations of > 35° to ≤45. Finally, on the frontal plane, the term “Pisa syndrome” was used to define a lateral bending of the trunk >10°, whereas “lateral trunk flexion” was chosen for angles of ≥ 5° to ≤10 [13].
Among axial postural abnormalities, camptocormia is present in over 10% of the general PD population and over 50% of PD patients presenting with at least one postural abnormality [11]. Moreover, postural alterations are linked to motor impairment and loss of functional independence [15] as well as increased risk of fall [4]. Trunk postural abnormalities on the sagittal plane can be classified as higher or lower on the basis of whether the fulcrum is located at the thoracic (C7 to T12-L1) or lumbar level (L1-Sacrum, hip flexion), respectively [4,16,17]. According to several previous studies [4,16,17,18,19,20], one of the main hallmarks of these alterations is the reversibility, namely the occurrence during standing and walking with the dramatic reduction in supine position or when leaning against a wall [13]. When the postural abnormality did not resolve during the supine position of the patient or when he is leaning against a wall, it could be considered non-reversable structured postural deformity.
From a clinical point of view, the abnormalities can be classified as non-structural or structural [21]. The term “structural” indicates the presence of morphological abnormalities within the bones and soft tissues (fascia, muscles, ligaments, tendons). In addition, structural misalignments reveal a more severe clinical problem because they are less flexible and less prone to correction compared to the non-structural disorders. One of various tests used as a clinical measure to screen structural thoracic hyper-kyphosis, with moderate diagnostic properties, is occiput to wall distance (OWD), revealing the presence of a structured hyper-kyphosis when the OWD ≥ 6.5 cm (cut-off point) [22].
Management of axial postural abnormalities in PD generally failed to show consistent, long-lasting improvements [14]. Considering the reversibility of these conditions, their management could be highly relevant to improving gait and balance. Indeed, a number of previous studies in the body of evidence have focused on the improvement in these parameters by targeting camptocormia and anterior trunk flexion in static conditions with several pharmacological and nonpharmacological interventions [18,23,24,25,26,27,28]. These included dopaminergic therapy [18], lidocaine injections [23], deep brain stimulation (DBS) [18,24,25], physical therapy [26,27,28]. Corsets and orthoses are commonly cited among the management strategies for postural abnormalities of PD, but only a few studies, with limited sample sizes and heterogeneous measurements, investigated the impact of orthoses with inconsistent results [27,29,30,31,32].
Posture can be quantitatively evaluated by different instrumental methods. To facilitate clinical application and standardize the calculation of posture degrees, the MDS Task Force Consensus recommended photograph analysis using the NeuroPostureApp, a freeware software-based measurement tool or wall goniometers [13]. Moreover, the recommendation of how to calculate the sagittal angles was provided for higher and lower postural abnormalities [12,33]. Besides photographic analysis, other instrumental evaluations of posture are available. In particular, baropodometry allows the quantification of any postural elements, such as postural stability [9], feet morphology, and symmetry in load distribution [34]. Furthermore, X-rays and 3D stereophotogrammetry are the gold standards for the evaluation of sagittal parameters and whole-body posture in static conditions [5] and for kinematic parameters of the entire body during walking in both the healthy and neurological population [6,35]. Several studies quantitatively evaluated the postural instability of PD patients using baropodometry [29,36] or force plates [37,38] in static and dynamic conditions and other ones have used X-rays and/or 3D optoelectronic system for evaluation of sagittal posture during standing [39,40]. Other studies have investigated the typical kinematic patterns in subjects with PD [19,20,41,42,43,44] via 3D motion analysis. This evidence underlined the fundamental role of quantitative posture and gait evaluation to aid in diagnosis and to encourage symptom monitoring, therapy management, rehabilitation, and fall risk assessment and prevention in PD patients [42].
Regarding the use of instrumental evaluation to assess treatment efficacy, a previous study assessed the standing posture and balance of PD patients with DBS and postural abnormalities on the sagittal plane after lidocaine injection in combination with physical therapy [23]. Another study examined the effect of a back active correction keeper on balance parameters in a small sample of people with PD showing an improvement in static and dynamic balance parameters [29]. Finally, one study investigated the effect of a spinal kypho-orthosis on gait and trunk flexion reporting a short-term effect for gait performance, particularly during turning and erect posture [32].
Nevertheless, to the best of our knowledge, no study instrumentally assessed whole-body sagittal alignment in both static and dynamic conditions before and after the treatment with a spinal orthosis in PD patients with postural abnormalities on the sagittal plane as defined by the recent MDS Task Force Consensus.
Therefore, the aims of the present study are the following: I) to evaluate the sagittal misalignment of PD patients in upright standing and during walking using 3D motion analysis with a specific whole-body marker set (DB-Total protocol); II) to assess the short- and long-term effects of the K1 Posture Keeper shirt on sagittal posture during static and dynamic conditions.
2. Materials and Methods
2.1. Population
A cross-sectional observational study was accomplished, recruiting 15 patients with PD showing postural abnormalities on the sagittal plane [anterior trunk flexion thoracic fulcrum (C7-T12 vertebrae) or camptocormia] according to the MDS Task Force Consensus [12,13] in the 2nd Division of Neurology at the University of Campania “Luigi Vanvitelli”, and 10 healthy individuals without postural alterations and matched for age and BMI as healthy control group.
The present study was conducted in accordance with the Declaration of Helsinki; ethical approval was obtained from the ethical committee of the University of Campania “Luigi Vanvitelli”, and all participants of the study signed a written informed consent. The following inclusion criteria were used for the recruitment of PD patients: age range 18–90 years; BMI < 26 Kg/m2; (Hoehn and Yahr) < 3; presence of sagittal misalignments according to the MDS Task Force Consensus [13]; OWD ≤ 6.5 cm [22]. Exclusion criteria were the presence of structured hyper-kyphosis; presence of spinal deformities that require the use of fixed correction devices; subjects who had previously made use of the K1 Posture Keeper system; subjects with cognitive problems that do not allow them to understand the correct use of the orthosis and the instructions given for execution of the test. For the clinical evaluation, the following rating scales were used: Hoehn and Yahr scale, Movement Disorder Society Unified Parkinson’s Disease Rating Scale (MDS-UPDRS), and the OWD test.
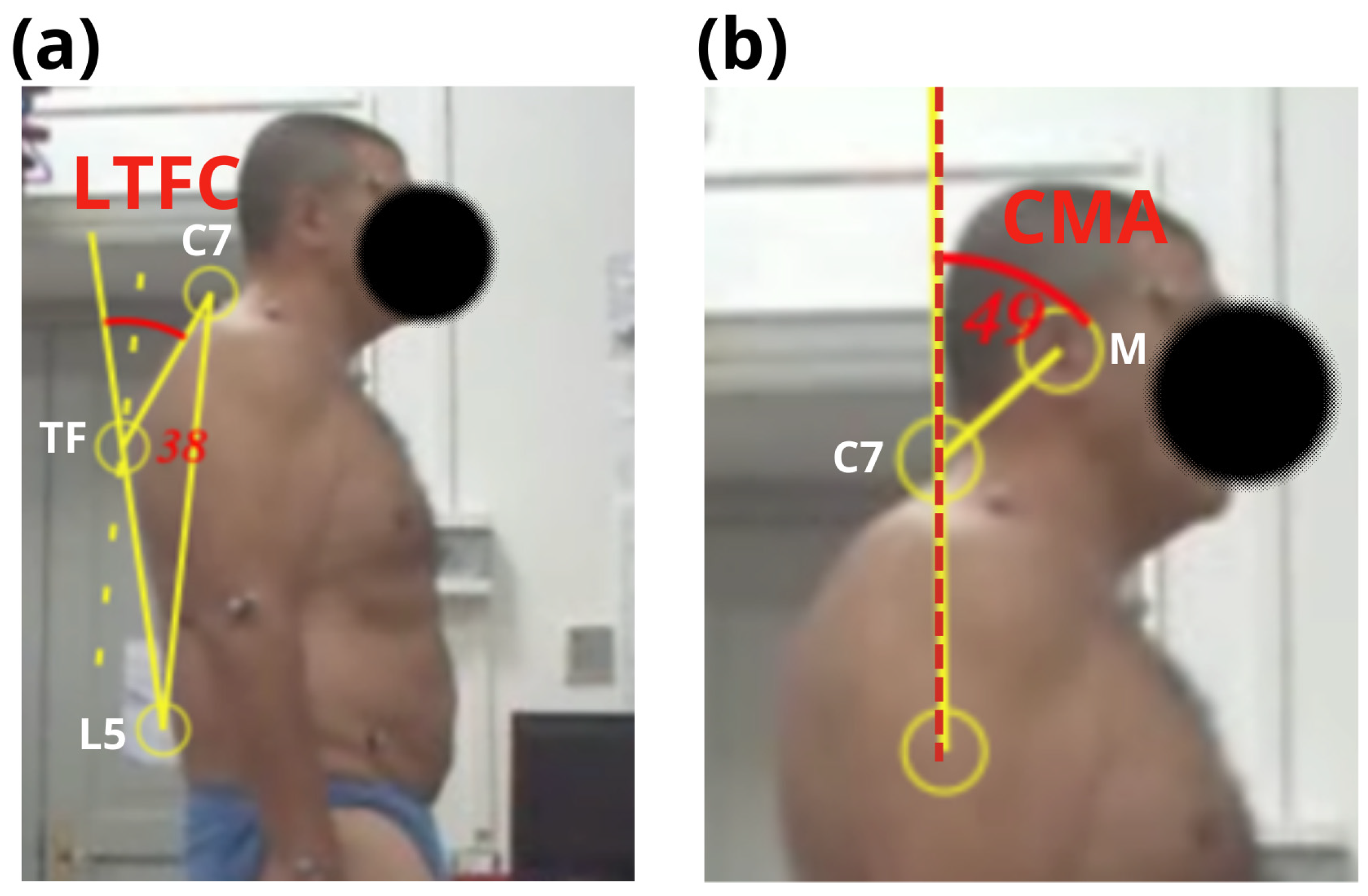
During the recruitment phase, each PD patient in treatment at the structure was evaluated by an expert neurologist: firstly, for each subject a recommended photograph analysis was implemented using the NeuroPostureApp [13] in order to measure the following sagittal angles: L5-thoracic fulcrum-C7 (LTFC) and C7-auditory meatus–vertical axis (CMA) angles for thoracic and cervical regions [12], respectively (Figure 1). The cut-off values for these angles were considered in accordance with the MDS Task Force Consensus [13] to identify the type of sagittal postural alteration of PD patients. Then, patients considered eligible (with postural abnormalities on sagittal plane) were asked to lean against the wall and the OWD was measured to identify reversable postural abnormality in order to exclude the subjects with the presence of structured thoracic hyper-kyphosis in accordance with [18].
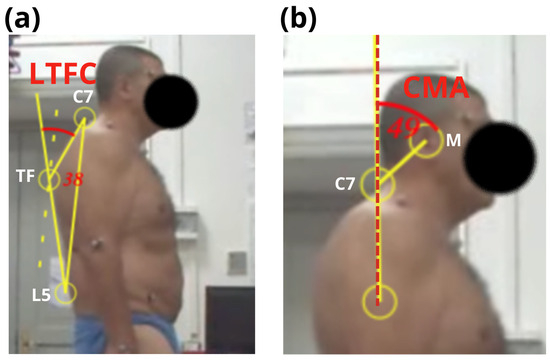
Figure 1.
Graphical representation of L5-thoracic fulcrum-C7 (a) and C7-auditory meatus–vertical axis (b) angles via NeuroPostureApp in a PD patient, as previously defined in [12]. The LTFC and CMA angles and the dashed vertical axis are marked in red. Figure notes: thoracic fulcrum (TF); cervical (C); lumbar (L); auditory meatus (M); L5-thoracic fulcrum-C7 (LTFC); C7-auditory meatus–vertical axis (CMA).
2.2. Instrumental Methods
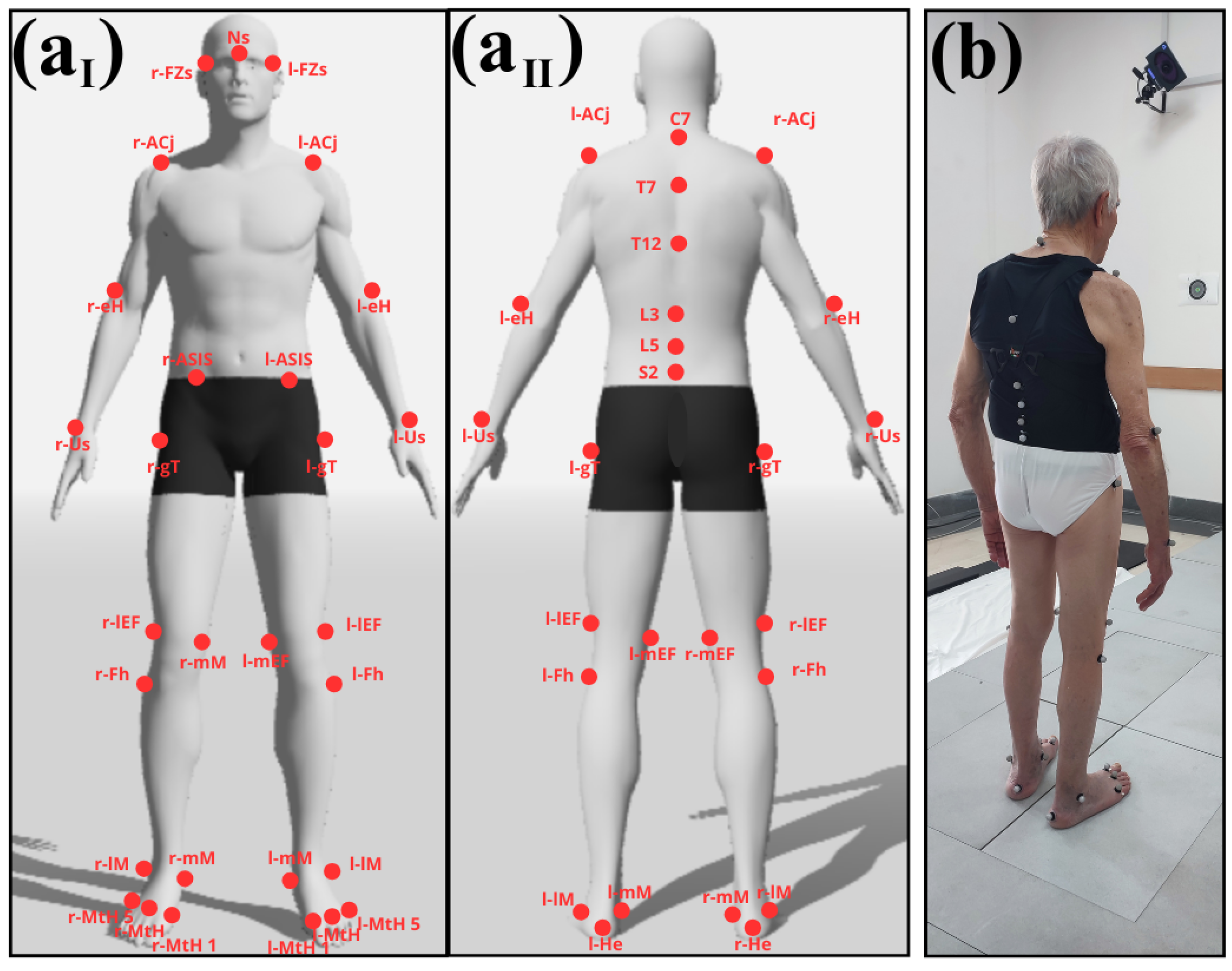
Each subject underwent 3D-stereophotogrammetric examination, performed by an optoelectronic system composed of eight Smart-D cameras (BTS Bioengineering, Milano, Italy) set at a frequency of 100 Hz and two force platforms (BTS Bioengineering, Milano, Italy) using DB-Total marker set [5], including 37 reflective markers placed on the following body landmarks: nasion (Ns), frontozygomatic suture (FZs), spinous processes of C7-T7-T12-L3-L5-S2, acromioclavicular joint (ACj), epicondylus humeri (eH), ulnar styloid (Us), anterior superior iliac spine (ASIS), greater trochanter (gT), medial (mEF) and lateral (lEF) epicondylus femoris, fibular head (Fh), medial (mM) and lateral (lM) malleoli, I–III and V metatarsal heads (MtHs), and heel (He) bilaterally (as represented in Figure 2).
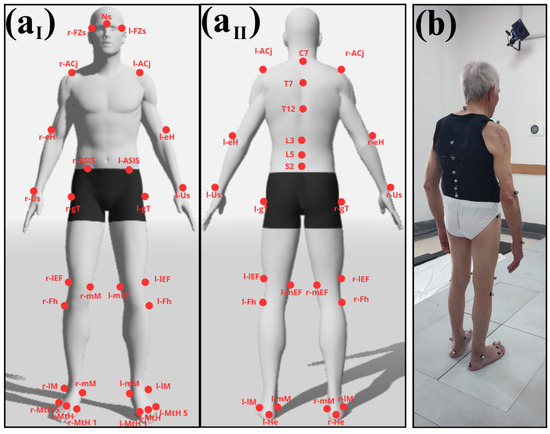
Figure 2.
(a) DB-total marker set on frontal plane anterior (aI) and posterior (aII) prospective. (b) PD patient wearing K1 Posture Keeper. Figure notes: cervical (C), thoracic (T), lumbar (L), sacrum (S), nasion (Ns), frontozygomatic suture (FZs), acromioclavicular joint (ACj), epicondylus humeri (eH), ulnar styloid (Us), anterior superior iliac spine (ASIS), greater trochanter (gT), medial (mEF) and lateral (lEF) epicondylus femoris, fibular head (Fh), medial (mM) and lateral (lM) malleoli, metatarsal heads (MtHs), and heel (He).
2.3. Orthosis
K1 Posture Keeper (e-Keep; Dual Sanitaly, Turin, Italy) is a commercial shirt (Figure 2b) developed for the correction and stabilization of the trunk in painful postural syndrome, curved back or juvenile kyphosis, and scapulo-thoracic non-neurological dyskinesia as reported by [29]. K1 Posture Keeper is wearable as a jersey, less invasive, and better tolerated by the patient with respect to a rigid corset. The size of the K1 Posture Keeper has been previously identified, according to information about the patient’s circumference of the thorax and the waist, detected by an expert operator during the recruitment.
2.4. Procedure and Data Collection
All recruited PD patients underwent 3D motion analysis at Functional Anatomy Laboratory of University of Campania “Luigi Vanvitelli” following a two-part procedure: the first part at T0, before the prolonged treatment with K1 Posture Keeper shirt, and the second at T1, after three months with the orthosis. Each part was further divided into two sessions: in the first, the patients were assessed without the K1 shirt, while in the second one, they were wearing the orthosis.
Therefore, the entire procedure consisted of four conditions: T0 without K1, T0 with K1, T1 without K1, and T1 with K1. The healthy group was acquired only at T0 without the orthosis. Each measure was collected in a static condition, with subjects in upright standing position, and a dynamic one, walking barefoot on a 6 m walkway at a self-selected normal-pace speed. Walking trial was performed three times consecutively. Healthy group was acquired only during upright standing, collecting all parameters only in static condition.
For each subject, the following preparation steps were applied before the acquisition:
In the first session, an expert operator (physiatrist, expert in functional anatomy and 3D motion analysis) identified body landmarks, where the reflective markers were placed according to the DB-Total marker set protocol (Figure 2).
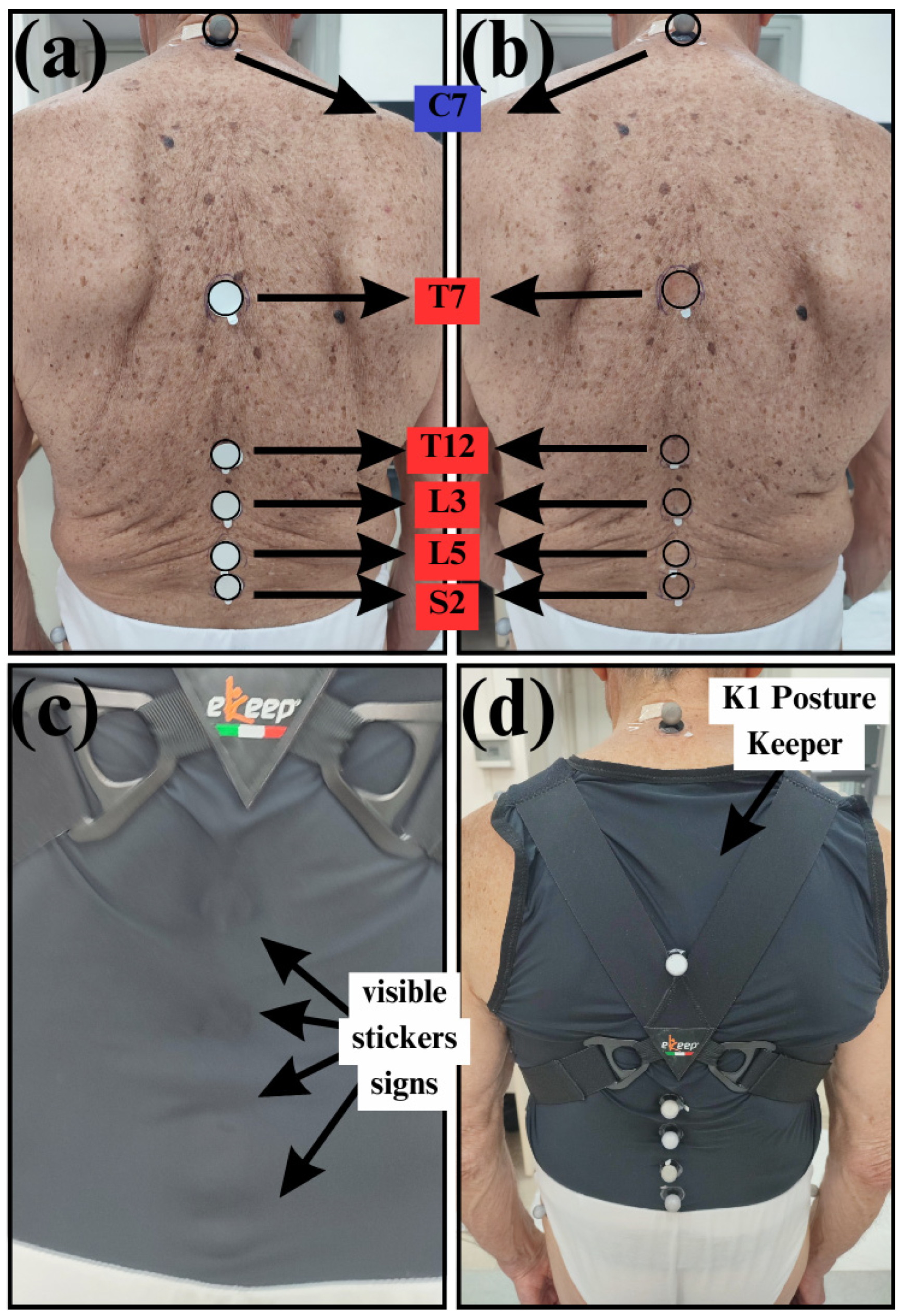
In the second session, the same operator circled the T7, T12, L3, L5, and S2 markers using a dermographic pen and removed them. Subsequently, he placed circular double-sided stickers inside the body landmarks (Figure 3a) and then, the cover of the stickers was removed (Figure 3b). Afterwards, the patient was instructed on how to wear the orthosis and the operator ensured that the shirt adhered to the patient’s back, making the sticker signs visible (Figure 3c). Finally, the reflective markers were placed on the orthosis at the body landmarks, identified thanks to visible sticker signs (Figure 3d).
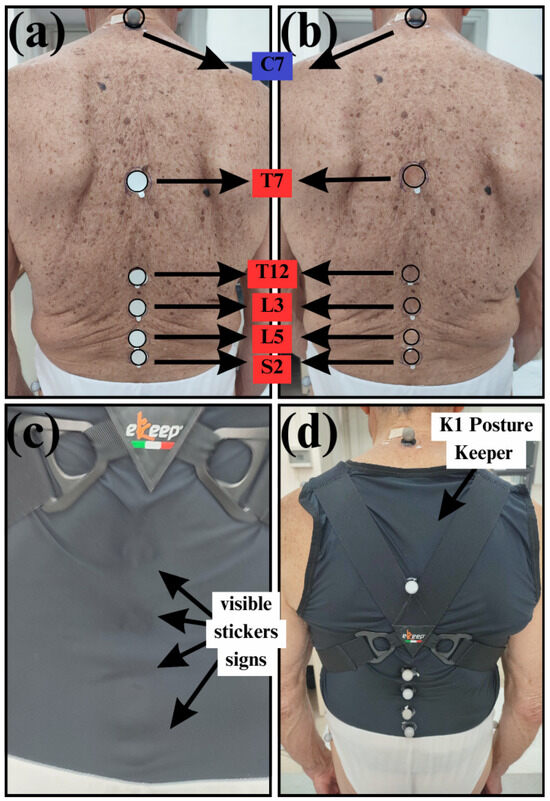
Figure 3.
Procedure for marker placement during evaluation session with orthosis: (a) circular double-sided stickers placed at the body landmarks (T7, T12, L3, L5 and S2) previously marked; (b) removing of the sticker cover; (c) patient wearing the orthosis, making sticker signs visible; (d) reflective markers placed on the orthosis at the body landmarks, identified thanks to visible sticker signs. Figure notes: C: cervical; T: thoracic; L: lumbar; S: sacrum. Markers highlighted in red are those placed on the orthosis.
At the end of the study, the Quebec User Evaluation of Satisfaction with Assistive Technology (QUEST) questionnaire [45] was administrated to the PD group to assess the benefit perceived in wearing the orthosis and their satisfaction (values range from 1 to 5).
The following eleven whole-body parameters defined in previous studies [5,6] were calculated on the sagittal plane by BTS Smart Clinic Software (1.10): sagittal vertical axes (SVAs), C7-nasion (CNA), cervical tilt (CT), dorsal (DA), lumbar (LA), trunk tilt (TT), heel-S2-nasion (HSN), heel-S2-C7 (HSC), heel-S2-T7 (HST), heel-S2, S2-C7 (SCA), and S2-T7 (STA) angles. Moreover, the occiput point was obtained with a specific algorithm implemented by BTS software in order to calculate two other sagittal angles in PD and healthy groups, heel-S2-occiput (HSO) and S2-C7-occiput angles (SCO). All parameters were exported from BTS software and imported into MATLAB (https://www.mathworks.com/products/matlab.html, accessed on 15 February 2025) for further processing. Mean values and standard deviations (SDs) across all subjects were calculated for static parameters of both healthy and PD groups. Kinematic curves of whole-body parameters for PD group were processed with a custom script in MATLAB obtaining the following additional values: excursion range and average, previously defined in [6]. In addition, the other nine kinematic parameters were computed, referring to gait variable scores (GVSs) for the lower limbs’ range of movement: pelvic tilt, rotation and obliquity, hip flexion–extension, adduction–abduction and rotation, knee flexion–extension, ankle dorsiflexion, and foot progression. Eventually, the Gait Profile Score (GPS) was obtained by the sum of the root mean square (RMS) of differences between a patient’s data and a reference value relating to a population of healthy individuals. Higher GVS and GPS scores indicated larger deviations from a physiological gait according to [46].
2.5. Statistical Analysis
The Shapiro–Wilk and Mauchly tests were used to assess the assumptions of normality and sphericity, respectively, for all the variables of interest; if the latter assumption was not satisfied, the Greenhouse–Geisser correction was applied.
Significant differences (level of significance α = 0.05) for all static parameters of upright standing posture were tested between healthy and PD groups only for the first condition (T0 without K1) via T-Test for independent samples or Wilcoxon Mann–Whitney test, according to the type of data distribution (parametric or non-parametric, respectively).
Successively, significant differences (level of significance α = 0.05) for all static and kinematic parameters were tested in PD group for multiple comparisons across four conditions (T0 without K1, T0 with K1, T1 without K1, and T1 with K1) via parametric repeated measure–ANOVA or non-parametric repeated measure–ANOVA (Friedman test). Moreover, when a significant difference was found (p-value < 0.05), post hoc tests with Tukey correction were executed to explore specific effect of each comparison (T0 without K1 vs. T0 without K1, T0 without K1 vs. T1 without K1, T0 without K1 vs. T1 with K1, T0 with K1 vs. T1 without K1, T0 with K1 vs. T1 with K1, T1 without K1 vs. T1 with K1). Statistical analysis on collected data was performed by Jamovi (Version 2.3.18).
3. Results
3.1. Baseline Features
The demographic and clinical data of 15 PD patients and the healthy control group are presented in Table 1. The prevalence of anterior trunk flexion with thoracic fulcrum was 60% (mean LTFC angle ± SD: 41° ± 3.6°), whereas the prevalence of camptocormia with thoracic fulcrum was 40% (mean LTFC angle ± SD: 49.5° ± 2.1°). Regarding the cervical postural abnormalities on the sagittal plane, Table 1 shows that antecollis was observed in 80% of participants (mean C7–auditory meatus–vertical axis (CMA) angle ± SD: 53.8° ± 3.8°) and normal neck posture in 20% (mean CMA angle ± SD: 33° ± 1.1°). No participant showed an anterior neck flexion (Table 1).

Table 1.
Demographic and clinical variables of the enrolled population. All numerical parametric and non-parametric data were reported as mean ± SD or median (Q1–Q3), respectively; categorical variables are reported as absolute (N) and relative (%) frequencies.
3.2. Inter-Group (Healthy vs. PD Groups) Postural Differences in Upright Standing
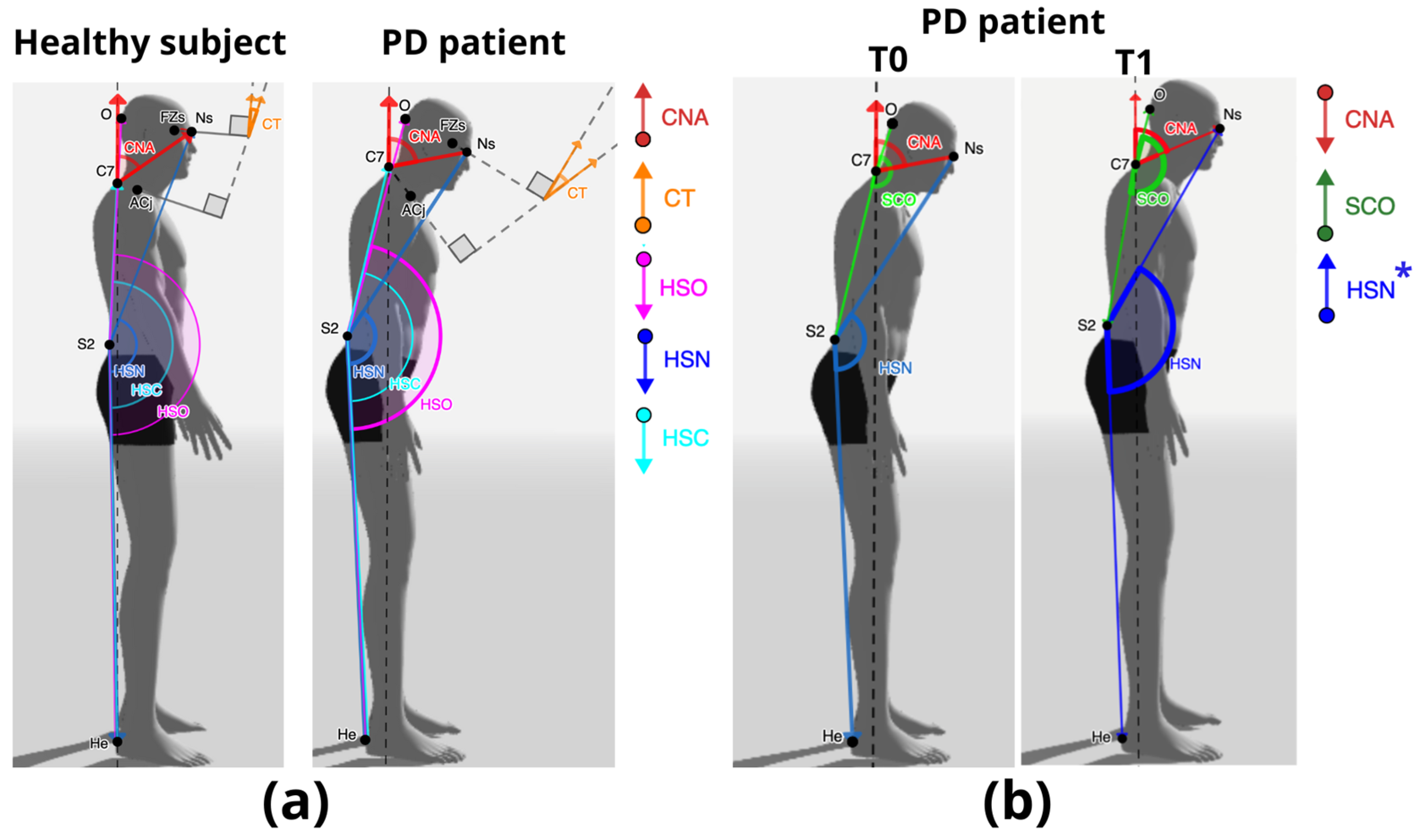
The comparison between the PD and healthy groups showed a significant decrease in the PD group for the following sagittal parameters in upright posture: HSO (t = 2.46; p = 0.024), HSN (t = 3.29; p = 0.004), and HSC (U = 23.0; p = 0.045) (Figure 4a, Table 2). Instead, a significant increase was found for CNA (t = −4.20; p ≤ 0.001) and for CT (t= −2.46 p= 0.025) in the PD group compared to the healthy one (Figure 4a, Table 2).
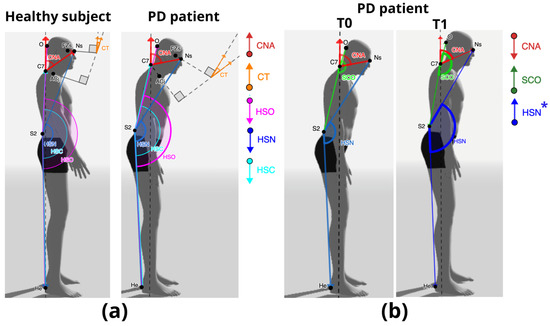
Figure 4.
Graphical representation of sagittal whole-body parameters resulted in significant differences in various comparisons: (a) healthy versus PD group in upright standing; (b) PD group without K1 versus with K1 during upright standing and walking at T0 and T1 (* the asterisk indicates a significant difference only during walking). T0 (before treatment), T1 (after treatment with K1 Posture Keeper). Figure Notes: the black dashed line indicates the vertical axis; the grey dashed lines represent head and thoracic planes with their corresponding perpendicular lines. The down and up arrows indicate a significant decrease and increase in parameters, respectively. Nasion (Ns), occiput (O), cervical (C), frontozygomatic suture (FZs), acromioclavicular joint (ACj), sacrum (S), heel (He); C7-nasion (CNA), cervical tilt (CT), S2-C7-occiput (SCO), heel-sacrum-occiput (HSO), heel-sacrum-nasion (HSN), and heel-sacrum-C7 (HSC) angles.

Table 2.
Comparison of sagittal parameters assessed in upright posture between healthy and PD groups via parametric t-test for independent samples or non-parametric Wilcoxon Mann–Whitney test (level of significance α = 0.05).
3.3. Intragroup (PD Patients) Postural Differences in Upright Standing Before and After Treatment with K1 Posture Keeper
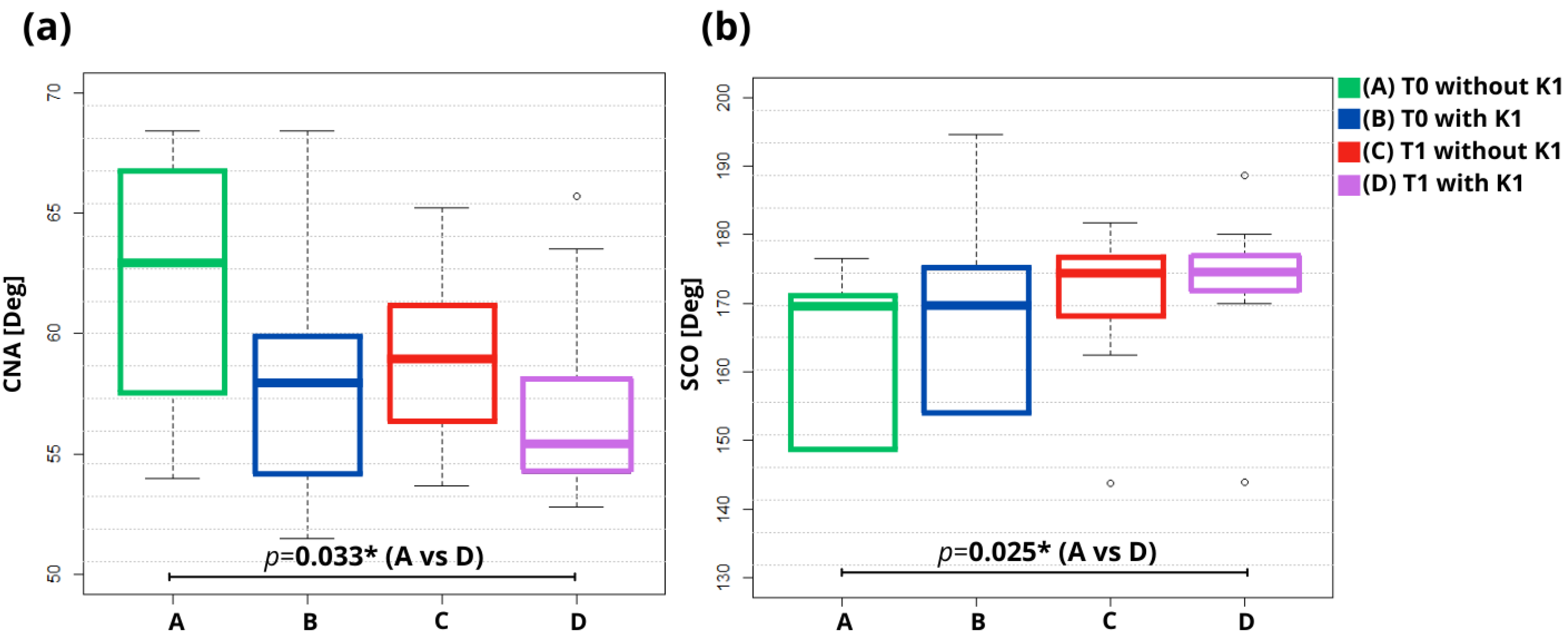
The multiple comparison across four conditions [T0 without (A) and with (B) orthosis and T1 without (C) and with (D) orthosis] in upright standing showed for the PD group a significant effect of the K1 Posture Keeper orthosis on the following sagittal parameters in upright posture: CNA (F = 4.57; p = 0.011) and SCO (χ2 = 5.96; p = 0.049). In particular, a significant decrease in CNA (p = 0.033) and increase in SCO (p = 0.045) angles was found in T1 with K1 compared to T0 without K1 (Table 3, Figure 4b and Figure 5).

Table 3.
Multiple comparisons of sagittal parameters assessed in upright posture across four conditions (T0 without K1, T0 with K1, T1 without K1 and T1 with K1) via parametric repeated measure–ANOVA or non-parametric repeated measure–ANOVA (Friedman test). Results of post hoc tests with Tukey correction for each comparison (level of significance α = 0.05).
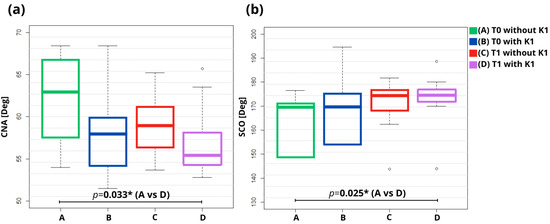
Figure 5.
Boxplot of significant differences (p-value ≤ 0.05) for static parameters in multiple comparisons implemented via repeated measures-ANOVA. Figure Notes: Significant differences are highlighted in bold (“*” p < 0.05). T0 without K1 (A); T0 with K1 (B); T1 without K1 (C); T1 with K1 (D); (a) C7-nasion (CNA) and (b) S2-C7-occiput (SCO) angles; degree (Deg).
3.4. Intragroup (PD Patients) Kinematic Differences During Walking Before and After Treatment with K1 Posture Keeper
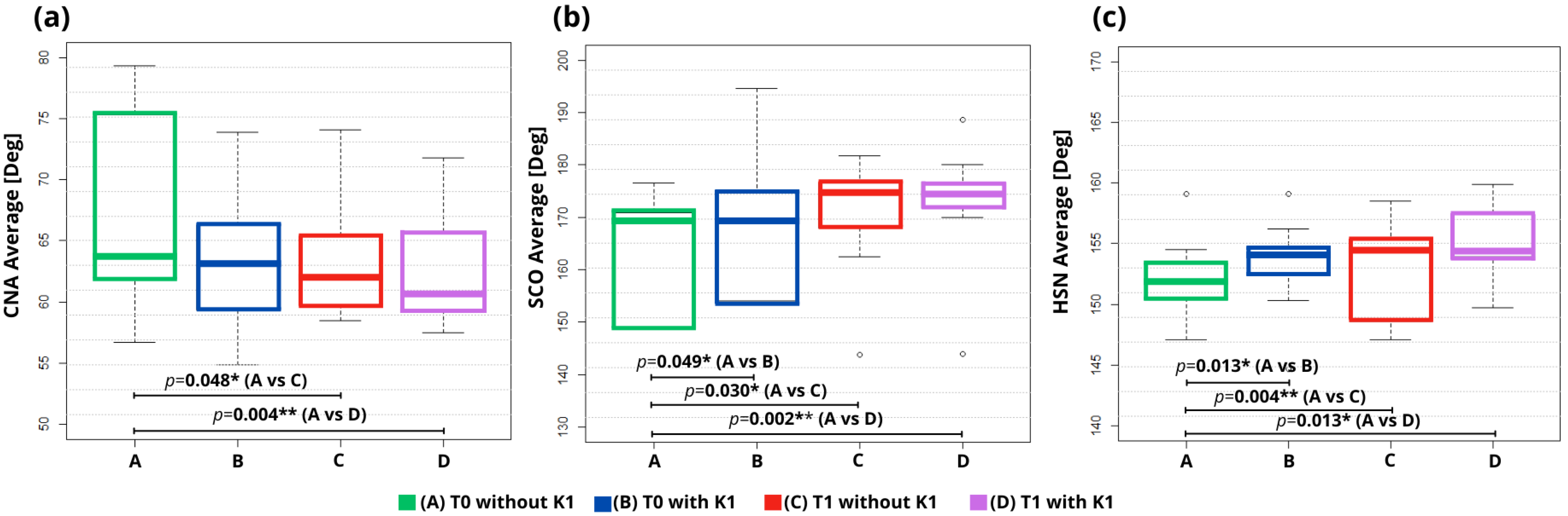
The multiple comparison across four conditions during walking showed a significant effect of K1 Posture Keeper on the following sagittal kinematic parameters of PD patients: CNA (χ2 = 8.83; p = 0.04 for average and χ2 = 12.8; p = 0.005 for range), DA (χ2 = 9.56; p = 0.023 for range), STA (χ2 = 8.93; p = 0.030 for range), SCO (χ2 = 9.0; p = 0.029 for average) and HSN (χ2 = 9.38; p = 0.025 for average).
In particular, the results of the post-hoc tests corrected for multiple comparisons with the Tukey method (Table 4 and Figure 4b) showed a significant decrease in CNA average in both T1 without (p = 0.048) and with K1 (p = 0.004) conditions compared to T0 without K1 one (Figure 6a); a significant increase in SCO average in T0 with K1 (p = 0.049) and in T1 without (p = 0.030) and with K1 (p = 0.002) conditions compared to T0 without K1 (Figure 6b), and of HSN average in T0 with K1 (p = 0.013) and T1 without (p = 0.004) and with K1 (p = 0.013) compared to T0 without K1 (Figure 6c).

Table 4.
Multiple comparisons for additional values (Average and Excursion Range) of sagittal parameters assessed during walking across four conditions (T0 without K1, T0 with K1, T1 without K1, and T1 with K1) via parametric repeated measure–ANOVA or non-parametric repeated measure–ANOVA (Friedman test). Results of post hoc tests with Tukey correction for each comparison (level of significance α = 0.05).
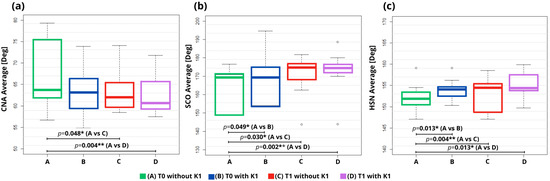
Figure 6.
Boxplot of significant differences (p-value ≤ 0.05) for average of kinematic parameters in multiple comparisons implemented via repeated measures–ANOVA. Figure Notes: Significant differences are highlighted in bold (“*” p < 0.05, “**” p < 0.01). T0 without K1 (A); T0 with K1 (B); T1 without K1 (C); T1 with K1 (D); (a) C7-nasion (CNA), (b) S2-C7-occiput (SCO) and (c) heel-sacrum-nasion (HSN) angles; degree (Deg).
Moreover, as far as the excursion range is concerned, statistical analysis (Table 4) underlined a significant decrease in CNA range in T1 without K1 condition compared to T0 without (p = 0.002) and with K1 (p = 0.001), and in T1 with K1 compared to T0 without K1 (p = 0.008) and with K1 (p = 0.006); DA range in T1 without K1 compared to T0 without (p = 0.037) and with K1 (p = 0.030), and in T1 with K1 compared to T0 without K1 (p = 0.011) and with K1 (p = 0.009). The only significant increase was found for STA range in T1 with K1 compared to T0 without K1 (p = 0.002).
No significant difference was found for all GVS of various joints and GPS in multiple comparisons across four conditions.
3.5. The QUEST Questionnaire
The results of the Quebec User Evaluation of Satisfaction with Assistive Technology (QUEST) questionnaire provided insights into various dimensions of PD patient satisfaction. The mean scores of each category are reported in Table 5.

Table 5.
Mean value of QUEST questionnaire scores (range from 1 to 5 points) across participants.
4. Discussion
The present study aimed to quantitatively assess postural abnormalities on the sagittal plane in Parkinson’s disease patients by 3D motion analysis using an accurate whole-body marker set (DB-Total protocol); moreover, the impact of the treatment with the K1 Posture Keeper shirt on the sagittal posture during upright standing and walking was investigated.
As reported in previous studies [44,47], marked anteflexion of the thoracolumbar spine on the sagittal plane causes the forward shift of the center of pressure. This could limit the ability of the individual to respond to balance perturbations and could lead to reduced postural stability and increased risk of falls and back pain [4,15]. Indeed, sagittal postural alterations, encompassing anterior trunk flexion, camptocormia, and antecollis, have been identified as disabling conditions in PD [15]. However, given the reversibility of PD-associated postural abnormalities, the use of adjustable orthoses might allow the straightening of the trunk, improving the whole-body sagittal alignment with positive effects on postural stability in both static and dynamic conditions in PD patients with anteflexion of the thoracolumbar spine and/or anterior bending of the neck. To the best of our knowledge, this is the first study to quantitively evaluate by 3D motion analysis the effect of treatment with a corrective corset (K1 Posture Keeper) in both static and dynamic conditions in PD patients with sagittal misalignment according to the MDS Task Force Consensus [13].
Demographic data are presented in Table 1, showing a prevalence of male subjects (69,2%) in the PD population and underlining a slightly larger prevalence of anterior trunk flexion with thoracic fulcrum (60%) associated to a larger prevalence of antecollis (80%) that occurred in the upright standing position. Moreover, 40% of the PD patients presented camptocormia with thoracic fulcrum. These findings, revealed by clinical examination executed via NeuroPostureApp, showed postural abnormalities with anterior sagittal bending at head-cervical region and an anterior trunk flexion at thoracic level.
The comparison of 3D-motion analysis parameters between the healthy and PD populations during upright standing (Table 2) showed a significant increase in the C7-nasion-angle (CNA) and a significant decrease in the S2-C7-occiput (SCO) angles in PD patients, confirming the abnormal anterior position of the head with respect to the trunk and, in particular, of the nasion with respect to C7 and of the occiput with respect to C7 and sacrum. Moreover, the significant increase in cervical tilt (CT) angle revealed a flexion of the head with respect to the trunk in PD patients (Table 2; Figure 4a). In addition, the significant decrease found for the heel-S2-occiput (HSO), heel-S2-nasion (HSN), and heel-S2-C7 (HSC) anterior whole-body angles underlined the significant anterior position, respectively, of the occiput, nasion and C7 with respect to the sacrum and to the heel (Table 2; Figure 4a). These findings regarding the sagittal alignment of the whole body confirmed the anteriorization of the head-cervical region with respect to the sacral region and to the feet in PD patients compared to healthy controls (Figure 4a), whereas only a trend of increased trunk tilt and decreased dorsal angle were found. Therefore, in this sample of patients, the abnormality of the cervical–head region is more relevant with respect to trunk one (hyper-kyphosis or trunk tilt).
As far as the PD group was concerned, significant short- and long-term improvements were observed after wearing the K1 Posture Keeper. This effect was quantified through whole-body assessment of the sagittal posture during standing and walking via 3D motion analysis. Indeed, in upright standing, the results showed a significant increase in SCO angle in the measure acquired at T1 when wearing the orthosis with respect to baseline condition (T0 without wearing K1) (Table 3; Figure 4b and Figure 5b). In particular, this improvement was observed for the head–cervical region with a significant decrease in CNA in T1 with the K1 condition with respect to T0 without K1 (Table 3 and Figure 5a), underlining a decrease in antecollis in upright standing (Figure 4b). These results showed that wearing the K1 Posture Keeper could lead to long-term sagittal improvements during upright posture in PD population, inducing a posteriorization of the cervical–head region compared with the T0 condition, with a trend of normalization of the occiput and nasion values with respect to the C7 and sacrum ones, as represented in Figure 4b.
Furthermore, the evaluation of whole-body posture during walking confirmed the therapeutic role of the K1 Posture Keeper in PD patients. In fact, the results reported in Table 4 showed a significant increase in SCO average in all conditions with respect to T0 without K1, and a significant decrease in CNA average in T1 with and without K1 compared to T0 without K1 (Figure 6a,b), suggesting a reduction in the antecollis during walking. Moreover, a significant increase in HSN average in T0 with K1 and in T1 without K1 compared to T0 without K1 (Table 4 and Figure 6c) confirmed the back shift of the nasion with a better alignment of the head with respect to the trunk, pelvis, and feet, underlining an improvement in the sagittal alignment of the entire body in PD patients during walking (Figure 4b).
Additionally, a significant decrease in the excursion range values of CNA and DA found in T1 compared to T0 (Table 4) could suggest a greater postural stability of PD patients during walking due to a reduction in oscillations on the sagittal plane thanks to the long-term effect of the K1 Posture Keeper.
These results are in line with a previous work by Morone [29], reporting an improvement in static and dynamic balance while wearing a posture shirt, also suggesting a possible therapeutic role in reducing the risk of falls
Other previous evidence includes that from Jo and colleagues, reporting an improvement in the forward bend posture and gait parameters while wearing a spinal kypho-orthosis [32]. Mukai et al. also reported an improvement in neck flexion in people with PD using a neck corset combined with lidocaine injection [30]. However, no previous studies have reported the long-term effect of orthoses on postural alterations in PD. We could speculate that a reorganization of the proprioceptive/sensory system following the wearing of the corset could be at the basis of our findings. Indeed, altered proprioception is described in people with PD, particularly with axial abnormalities [48]. It was proposed that proprioceptive dysregulation could contribute to camptocormia development. According to this hypothesis, proprioceptive information is sent to supraspinal areas, where inappropriate feed forward information is sent back to spinal interneuron circuits for adjusting the tone of axial muscles resulting in unbalanced muscle loading that might cause rigidity and, eventually, camptocormia [49]. Moreover, PD patients with postural alterations have been showed to have altered subjective vertical position [50,51]. Indeed, corrective orthoses could help rebalance the proprioceptive input and improve the vertical perception, thus ameliorating the postural alteration.
Finally, regarding the subjective perception of participants using the K1 Posture Keeper, the QUEST questionnaire highlighted positive feedback about the usability, durability, and comfort of the corset (Table 5), only reporting a mild discomfort in the hot days of the summer season. All PD patients perceived a benefit in wearing the orthosis on postural stability and upper back pain during daily activities. In conclusion, the daily use of the K1 Posture Keeper in PD patients with cervical and thoracic abnormalities can improve the sagittal misalignment of the whole body, reducing the upper back pain and the risk of falls.
Limitations and Future Perspectives
The present study suffers from some limitations. First, the lack of a PD control group and the small sample size limit the generalizability of the present study’s results. Second, a specific corrective orthosis was used in this study; therefore, our results could not directly extend to other corrective corsets. Moreover, only people with postural abnormalities on the sagittal plane were enrolled; therefore, the evidence in the present study could not be generalized to other axial postural abnormalities on the other planes, such as Pisa syndrome. Additionally, patients were assessed only in a supervised laboratory-based setting. Future studies with a larger sample size, including patients with axial abnormalities beyond the sagittal plane, implementing other corrective corsets, and assessing posture parameters in free-living, unsupervised conditions could help overcome these limitations and further expand the findings of this study. Finally, future longitudinal studies are warranted to investigate whether the observed improvements in gait and balance parameters in order to reduce risk of falls and to obtain an improvement in functional mobility and independence, as well as to assess the long-term (beyond three months) effects and further postural changes over time.
5. Conclusions
This study highlighted the whole-body misalignment on the sagittal plane in PD patients with thoracic and cervical abnormalities, showing a significant anterior shift in the head–neck region with respect to the pelvic one and to the feet support surface, with only a slight increase in trunk tilt and dorsal kyphosis. Moreover, the results of the present study demonstrated the therapeutic role of the K1 Posture Keeper shirt in improving sagittal posture in upright standing and sagittal kinematic parameters during walking. This could be due to proprioceptive reorganization following the corset use. These findings could be relevant to improve the management of postural abnormalities in neurological and rehabilitative setting through a practical and low-cost approach with an acceptable profile of invasiveness and comfort by patients with Parkinson’s Disease.
Author Contributions
Conceptualization, P.D.B.; data curation, A.F., C.I.D.G., G.M. and N.S.; formal analysis, P.D.B., A.F., C.I.D.G. and E.B.; investigation, P.D.B., A.F., C.I.D.G., G.M. and N.S.; methodology, P.D.B., A.F. and C.I.D.G.; project administration, P.D.B. and M.A.B.M.; supervision, P.D.B. and M.A.B.M.; writing—original draft, P.D.B., A.F. and C.I.D.G.; writing—review and editing, P.D.B., A.F., C.I.D.G., E.B., G.M., N.S. and M.A.B.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted according to the guidelines of the Declaration of Helsinki and approved by the local Ethics Committee.
Informed Consent Statement
Informed consent was obtained from all subjects involved in this study.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Acknowledgments
The authors extend their thanks to Dual Sanitaly S.P.A. for providing the K1 Posture Keeper shirts to patients free of charge.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Poewe, W.; Seppi, K.; Tanner, C.M.; Halliday, G.M.; Brundin, P.; Volkmann, J.; Schrag, A.-E.; Lang, A.E. Parkinson Disease. Nat. Rev. Dis. Primer 2017, 3, 17013. [Google Scholar] [CrossRef] [PubMed]
- Viseux, F.J.F.; Delval, A.; Defebvre, L.; Simoneau, M. Postural Instability in Parkinson’s Disease: Review and Bottom-up Rehabilitative Approaches. Neurophysiol. Clin. 2020, 50, 479–487. [Google Scholar] [CrossRef] [PubMed]
- Mirelman, A.; Bonato, P.; Camicioli, R.; Ellis, T.D.; Giladi, N.; Hamilton, J.L.; Hass, C.J.; Hausdorff, J.M.; Pelosin, E.; Almeida, Q.J. Gait Impairments in Parkinson’s Disease. Lancet Neurol. 2019, 18, 697–708. [Google Scholar] [CrossRef]
- Doherty, K.M.; Van De Warrenburg, B.P.; Peralta, M.C.; Silveira-Moriyama, L.; Azulay, J.-P.; Gershanik, O.S.; Bloem, B.R. Postural Deformities in Parkinson’s Disease. Lancet Neurol. 2011, 10, 538–549. [Google Scholar] [CrossRef] [PubMed]
- De Blasiis, P.; Fullin, A.; Sansone, M.; Del Viscovo, L.; Napolitano, F.; Terracciano, C.; Lus, G.; Melone, M.A.B.; Sampaolo, S. Quantitative Evaluation of Upright Posture by X-Ray and 3D Stereophotogrammetry with a New Marker Set Protocol in Late Onset Pompe Disease. J. Neuromuscul. Dis. 2021, 8, 979–988. [Google Scholar] [CrossRef]
- De Blasiis, P.; Fullin, A.; Sansone, M.; Perna, A.; Caravelli, S.; Mosca, M.; De Luca, A.; Lucariello, A. Kinematic Evaluation of the Sagittal Posture during Walking in Healthy Subjects by 3D Motion Analysis Using DB-Total Protocol. J. Funct. Morphol. Kinesiol. 2022, 7, 57. [Google Scholar] [CrossRef]
- De Blasiis, P.; Fullin, A.; De Girolamo, C.I.; Amata, O.; Caravaggi, P.; Caravelli, S.; Mosca, M.; Lucariello, A. Posture and Vision: How Different Distances of Viewing Target Affect Postural Stability and Plantar Pressure Parameters in Healthy Population. Heliyon 2024, 10, e39257. [Google Scholar] [CrossRef] [PubMed]
- De Blasiis, P.; Caravaggi, P.; Fullin, A.; Leardini, A.; Lucariello, A.; Perna, A.; Guerra, G.; De Luca, A. Postural Stability and Plantar Pressure Parameters in Healthy Subjects: Variability, Correlation Analysis and Differences under Open and Closed Eye Conditions. Front. Bioeng. Biotechnol. 2023, 11, 1198120. [Google Scholar] [CrossRef] [PubMed]
- Fullin, A.; Caravaggi, P.; Picerno, P.; Mosca, M.; Caravelli, S.; De Luca, A.; Lucariello, A.; De Blasiis, P. Variability of Postural Stability and Plantar Pressure Parameters in Healthy Subjects Evaluated by a Novel Pressure Plate. Int. J. Environ. Res. Public. Health 2022, 19, 2913. [Google Scholar] [CrossRef] [PubMed]
- Moffa, S.; Perna, A.; Candela, G.; Cattolico, A.; Sellitto, C.; De Blasiis, P.; Guerra, G.; Tafuri, D.; Lucariello, A. Effects of Hoverboard on Balance in Young Soccer Athletes. J. Funct. Morphol. Kinesiol. 2020, 5, 60. [Google Scholar] [CrossRef] [PubMed]
- Tinazzi, M.; Gandolfi, M.; Ceravolo, R.; Capecci, M.; Andrenelli, E.; Ceravolo, M.G.; Bonanni, L.; Onofrj, M.; Vitale, M.; Catalan, M.; et al. Postural Abnormalities in Parkinson’s Disease: An Epidemiological and Clinical Multicenter Study. Mov. Disord. Clin. Pract. 2019, 6, 576–585. [Google Scholar] [CrossRef]
- Margraf, N.G.; Wolke, R.; Granert, O.; Berardelli, A.; Bloem, B.R.; Djaldetti, R.; Espay, A.J.; Fasano, A.; Furusawa, Y.; Giladi, N.; et al. Consensus for the Measurement of the Camptocormia Angle in the Standing Patient. Park. Relat. Disord. 2018, 52, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Tinazzi, M.; Geroin, C.; Bhidayasiri, R.; Bloem, B.R.; Capato, T.; Djaldetti, R.; Doherty, K.; Fasano, A.; Tibar, H.; Lopiano, L.; et al. Task Force Consensus on Nosology and Cut-Off Values for Axial Postural Abnormalities in Parkinsonism. Mov. Disord. Clin. Pract. 2022, 9, 594–603. [Google Scholar] [CrossRef]
- Geroin, C.; Artusi, C.A.; Nonnekes, J.; Aquino, C.; Garg, D.; Dale, M.L.; Schlosser, D.; Lai, Y.; Al-Wardat, M.; Salari, M.; et al. Axial Postural Abnormalities in Parkinsonism: Gaps in Predictors, Pathophysiology, and Management. Mov. Disord. 2023, 38, 732–739. [Google Scholar] [CrossRef] [PubMed]
- Geroin, C.; Artusi, C.A.; Gandolfi, M.; Zanolin, E.; Ceravolo, R.; Capecci, M.; Andrenelli, E.; Ceravolo, M.G.; Bonanni, L.; Onofrj, M.; et al. Does the Degree of Trunk Bending Predict Patient Disability, Motor Impairment, Falls, and Back Pain in Parkinson’s Disease? Front. Neurol. 2020, 11, 207. [Google Scholar] [CrossRef] [PubMed]
- Fasano, A.; Geroin, C.; Berardelli, A.; Bloem, B.R.; Espay, A.J.; Hallett, M.; Lang, A.E.; Tinazzi, M. Diagnostic Criteria for Camptocormia in Parkinson’s Disease: A Consensus-Based Proposal. Park. Relat. Disord. 2018, 53, 53–57. [Google Scholar] [CrossRef] [PubMed]
- Magrinelli, F.; Geroin, C.; Squintani, G.; Gandolfi, M.; Rizzo, G.; Barillari, M.; Vattemi, G.; Morgante, F.; Tinazzi, M. Upper Camptocormia in Parkinson’s Disease: Neurophysiological and Imaging Findings of Both Central and Peripheral Pathophysiological Mechanisms. Park. Relat. Disord. 2020, 71, 28–34. [Google Scholar] [CrossRef] [PubMed]
- Ali, F.; Matsumoto, J.Y.; Hassan, A. Camptocormia: Etiology, Diagnosis, and Treatment Response. Neurol. Clin. Pract. 2018, 8, 240–248. [Google Scholar] [CrossRef] [PubMed]
- Soares, C.; Vilas-Boas, M.D.C.; Lopes, E.M.; Choupina, H.; Soares-dos-Reis, R.; Fitas, D.; Cunha, J.P.S.; Monteiro, P.; Linhares, P.; Rosas, M.J. Automated and Objective Measures of Gait Dynamics in Camptocormia Parkinson’s Disease Subthalamic Deep Brain Stimulation. Clin. Neurol. Neurosurg. 2019, 186, 105537. [Google Scholar] [CrossRef] [PubMed]
- Tramonti, C.; Di Martino, S.; Unti, E.; Frosini, D.; Bonuccelli, U.; Rossi, B.; Ceravolo, R.; Chisari, C. Gait Dynamics in Pisa Syndrome and Camptocormia: The Role of Stride Length and Hip Kinematics. Gait Posture 2017, 57, 130–135. [Google Scholar] [CrossRef] [PubMed]
- Czaprowski, D.; Stoliński, Ł.; Tyrakowski, M.; Kozinoga, M.; Kotwicki, T. Non-Structural Misalignments of Body Posture in the Sagittal Plane. Scoliosis Spinal Disord. 2018, 13, 6. [Google Scholar] [CrossRef]
- Wiyanad, A.; Chokphukiao, P.; Suwannarat, P.; Thaweewannakij, T.; Wattanapan, P.; Gaogasigam, C.; Amatachaya, P.; Amatachaya, S. Is the Occiput-Wall Distance Valid and Reliable to Determine the Presence of Thoracic Hyperkyphosis? Musculoskelet. Sci. Pract. 2018, 38, 63–68. [Google Scholar] [CrossRef]
- Sakai, T.; Nagai, S.; Takao, K.; Tsuchiyama, H.; Ikeda, K. Effect of Intramuscular Lidocaine Injection with Physical Therapy on Camptocormia in Patients with Parkinson’s Disease Who Had Previously Had Deep Brain Stimulation. J. Phys. Ther. Sci. 2023, 35, 66–69. [Google Scholar] [CrossRef]
- Chieng, L.O.; Madhavan, K.; Wang, M.Y. Deep Brain Stimulation as a Treatment for Parkinson’s Disease Related Camptocormia. J. Clin. Neurosci. 2015, 22, 1555–1561. [Google Scholar] [CrossRef]
- Micheli, F.; Cersósimo, M.G.; Piedimonte, F. Camptocormia in a Patient with Parkinson Disease: Beneficial Effects of Pallidal Deep Brain Stimulation: Case Report. J. Neurosurg. 2005, 103, 1081–1083. [Google Scholar] [CrossRef] [PubMed]
- Gandolfi, M.; Tinazzi, M.; Magrinelli, F.; Busselli, G.; Dimitrova, E.; Polo, N.; Manganotti, P.; Fasano, A.; Smania, N.; Geroin, C. Four-Week Trunk-Specific Exercise Program Decreases Forward Trunk Flexion in Parkinson’s Disease: A Single-Blinded, Randomized Controlled Trial. Park. Relat. Disord. 2019, 64, 268–274. [Google Scholar] [CrossRef]
- de Sèze, M.-P.; Creuzé, A.; de Sèze, M.; Mazaux, J.-M. An Orthosis and Physiotherapy Programme for Camptocormia: A Prospective Case Study. J. Rehabil. Med. 2008, 40, 761–765. [Google Scholar] [CrossRef]
- Lee, K.H.; Kim, J.M.; Kim, H.S. Back Extensor Strengthening Exercise and Backpack Wearing Treatment for Camptocormia in Parkinson’s Disease: A Retrospective Pilot Study. Ann. Rehabil. Med. 2017, 41, 677–685. [Google Scholar] [CrossRef] [PubMed]
- Morone, G.; Iosa, M.; Cocchi, I.; Paolucci, T.; Arengi, A.; Bini, F.; Marinozzi, F.; Ciancarelli, I.; Paolucci, S.; De Angelis, D. Effects of a Posture Shirt with Back Active Correction Keeper on Static and Dynamic Balance in Parkinson’s Disease. J. Bodyw. Mov. Ther. 2021, 28, 138–143. [Google Scholar] [CrossRef]
- Mukai, Y.; Furusawa, Y.; Morimoto, Y.; Hama, Y.; Kawazoe, T.; Saitoh, Y.; Sakamoto, T.; Takahashi, Y.; Murata, M. Lidocaine Injections and Neck Corset Wearing Improve Dropped Head Syndrome in Parkinson’s Disease and Related Disorders. Clin. Park. Relat. Disord. 2019, 1, 82–85. [Google Scholar] [CrossRef] [PubMed]
- Ye, B.K.; Kim, H.-S.; Kim, Y.W. Correction of Camptocormia Using a Cruciform Anterior Spinal Hyperextension Brace and Back Extensor Strengthening Exercise in a Patient With Parkinson Disease. Ann. Rehabil. Med. 2015, 39, 128. [Google Scholar] [CrossRef]
- Jo, G.; Park, J.; Yoon, J.-Y.; Kim, H.; Kim, S.C.; Park, S.-H. Effect of Spinal Kypho-Orthosis to Gait and Forward Flexion in Parkinson Disease. J. Phys. Ther. Sci. 2018, 30, 988–992. [Google Scholar] [CrossRef]
- Tinazzi, M.; Gandolfi, M.; Artusi, C.A.; Lanzafame, R.; Zanolin, E.; Ceravolo, R.; Capecci, M.; Andrenelli, E.; Ceravolo, M.G.; Bonanni, L.; et al. Validity of the Wall Goniometer as a Screening Tool to Detect Postural Abnormalities in Parkinson’s Disease. Park. Relat. Disord. 2019, 69, 159–165. [Google Scholar] [CrossRef]
- DE Blasiis, P.; Fullin, A.; Caravaggi, P.; Lus, G.; Melone, M.A.; Sampaolo, S.; DE Luca, A.; Lucariello, A. Long-Term Effects of Asymmetrical Posture in Boxing Assessed by Baropodometry. J. Sports Med. Phys. Fit. 2022, 62, 350–355. [Google Scholar] [CrossRef]
- De Blasiis, P.; Fullin, A.; Mazzoli, D.; Bruno, G.; Napolitano, F.; De Luca, A.; Melone, M.A.B.; Sampaolo, S. Sagittal Kinematics and Imbalance of the Spine and Whole Body during Walking in Late-Onset Pompe Disease. J. Neurophysiol. 2023, 130, 353–363. [Google Scholar] [CrossRef]
- Paolucci, T.; Iosa, M.; Morone, G.; Fratte, M.D.; Paolucci, S.; Saraceni, V.M.; Villani, C. Romberg Ratio Coefficient in Quiet Stance and Postural Control in Parkinson’s Disease. Neurol. Sci. 2018, 39, 1355–1360. [Google Scholar] [CrossRef]
- Nardone, A.; Schieppati, M. Balance in Parkinson’s Disease under Static and Dynamic Conditions. Mov. Disord. 2006, 21, 1515–1520. [Google Scholar] [CrossRef]
- St George, R.J.; Gurfinkel, V.S.; Kraakevik, J.; Nutt, J.G.; Horak, F.B. Case Studies in Neuroscience: A Dissociation of Balance and Posture Demonstrated by Camptocormia. J. Neurophysiol. 2018, 119, 33–38. [Google Scholar] [CrossRef]
- Arii, Y.; Sawada, Y.; Kawamura, K.; Miyake, S.; Taichi, Y.; Izumi, Y.; Kuroda, Y.; Inui, T.; Kaji, R.; Mitsui, T. Immediate Effect of Spinal Magnetic Stimulation on Camptocormia in Parkinson’s Disease. J. Neurol. Neurosurg. Psychiatry 2014, 85, 1221–1226. [Google Scholar] [CrossRef]
- de Sèze, M.P.; Guillaud, E.; Slugacz, L.; Cazalets, J.R. An Examination of Camptocormia Assessment by Dynamic Quantification of Sagittal Posture. J. Rehabil. Med. 2015, 47, 72–79. [Google Scholar] [CrossRef]
- Costa, T.M.; Simieli, L.; Bersotti, F.M.; Mochizuki, L.; Barbieri, F.A.; Coelho, D.B. Gait and Posture Are Correlated Domains in Parkinson’s Disease. Neurosci. Lett. 2022, 775, 136537. [Google Scholar] [CrossRef]
- Di Biase, L.; Di Santo, A.; Caminiti, M.L.; De Liso, A.; Shah, S.A.; Ricci, L.; Di Lazzaro, V. Gait Analysis in Parkinson’s Disease: An Overview of the Most Accurate Markers for Diagnosis and Symptoms Monitoring. Sensors 2020, 20, 3529. [Google Scholar] [CrossRef]
- Panero, E.; Dimanico, U.; Artusi, C.A.; Gastaldi, L. Standardized Biomechanical Investigation of Posture and Gait in Pisa Syndrome Disease. Symmetry 2021, 13, 2237. [Google Scholar] [CrossRef]
- Yao, M.; Zhou, L.; Tan, Y.; Jiang, H.; Chen, Z.; Zhu, L.; Luo, N.; Wu, Q.; Kang, W.; Liu, J. Gait Characteristics and Brain Activity in Parkinson’s Disease with Concomitant Postural Abnormalities. Aging Dis. 2020, 11, 791. [Google Scholar] [CrossRef]
- Demers, L.; Weiss-Lambrou, R.; Ska, B. The Quebec User Evaluation of Satisfaction with Assistive Technology (QUEST 20): An Overview of Recent Progress. Technol. Disabil. 2002, 14, 101–105. [Google Scholar] [CrossRef]
- De Blasiis, P.; Siani, M.F.; Fullin, A.; Sansone, M.; Melone, M.A.B.; Sampaolo, S.; Signoriello, E.; Lus, G. Short and Long Term Effects of Nabiximols on Balance and Walking Assessed by 3D-Gait Analysis in People with Multiple Sclerosis and Spasticity. Mult. Scler. Relat. Disord. 2021, 51, 102805. [Google Scholar] [CrossRef]
- Bartolić, A.; Pirtošek, Z.; Rozman, J.; Ribarič, S. Postural Stability of Parkinson’s Disease Patients Is Improved by Decreasing Rigidity. Eur. J. Neurol. 2005, 12, 156–159. [Google Scholar] [CrossRef]
- Schulz-Schaeffer, W.J. Camptocormia in Parkinson’s Disease: A Muscle Disease Due to Dysregulated Proprioceptive Polysynaptic Reflex Arch. Front. Aging Neurosci. 2016, 8, 128. [Google Scholar] [CrossRef]
- Srivanitchapoom, P.; Hallett, M. Camptocormia in Parkinson’s Disease: Definition, Epidemiology, Pathogenesis and Treatment Modalities. J. Neurol. Neurosurg. Psychiatry 2016, 87, 75–85. [Google Scholar] [CrossRef]
- Mikami, K.; Shiraishi, M.; Kamo, T. Subjective Vertical Position Allows Prediction of Postural Deterioration in Patients with Parkinson’s Disease. Park. Dis. 2019, 2019, 1875435. [Google Scholar] [CrossRef]
- Shiraishi, M.; Mikami, K.; Kamo, H.; Okuma, Y.; Tsunemi, T.; Fujimoto, K.; Kamo, T.; Yokota, Y.; Nogawa, S.; Osada, T.; et al. The Effect of Subjective Postural Vertical on Forward Flexed Posture in Parkinson’s Disease. Park. Relat. Disord. 2024, 129, 107102. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).