Innovations and Technological Advances in Healthcare Remote Monitoring Systems for the Elderly and Vulnerable People: A Scoping Review
Abstract
:1. Introduction
- Limited access to healthcare services, often requiring frequent in-person visits for medical evaluations;
- Reliance on manual vital sign monitoring devices, which can be difficult to use without assistance;
- Challenges in adopting wearable health technologies, due to technological barriers, limited digital literacy, and the absence of user-friendly devices tailored to their needs.
2. Materials and Methods
2.1. Identifying the Research Question
- What are the recent advances in developed and integrated technologies that focus on elderly and vulnerable people’s health, and what are the current methods in physiological signal analysis?
2.2. Identifying Relevant Studies
- For older adults: “aging population” OR “old people” OR “elderly population” OR “senior” OR “old population” OR “geriatric”.
- For health systems monitoring: “remote monitoring systems” OR “telemetry” OR “e-health” OR “telehealth” OR “healthcare”.
- For wearable devices: “smart bands” OR “smartwatches” OR “wearable sensors” OR “wearable devices” OR “wristbands”.
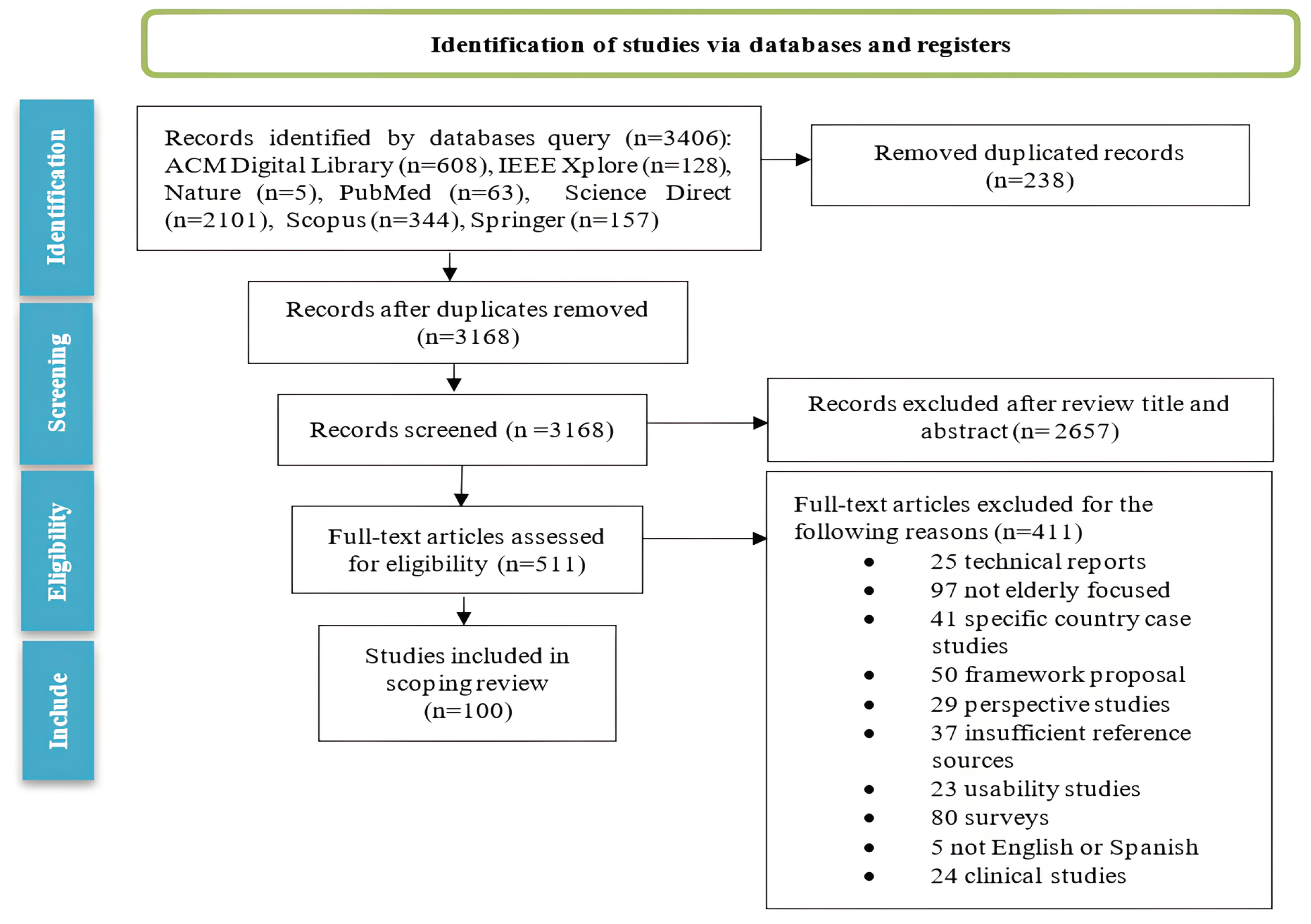
2.3. Study Selection
- Publication Type: Journal papers or conference proceedings must be indexed in databases recognized for their scientific rigor.
- Topic Relevance: They must monitor vital signs, fall detection, and emergency alerts.
- Technological Scope: They should encompass a range of topics, including physiological signal analysis, artificial intelligence techniques, intelligent computing algorithms, the Internet of Things (IoT), communication technologies, information processing, storage and deployment techniques, expert knowledge-based systems, embedded systems, sensors, telehealth, and e-health.
- Integration Level: They should cover work ranging from physiological signal analysis to integrated home systems featuring a network of intelligent sensors.
- Publication Type: Technical reports, clinical studies, survey articles, framework proposals, usability studies, qualitative studies, studies that do not focus on the elderly, case studies specific to particular countries, and publications unavailable in English or Spanish.
2.4. Charting the Data
2.5. Collating, Summarizing, and Reporting the Results
3. Results and Discussion
3.1. What Are the Recent Advances in Developed and Integrated Technologies Focused on Elderly and Vulnerable People’s Health?
3.1.1. Intelligent Homes
3.1.2. Wearable Devices
3.1.3. Web-Based and Mobile Applications for Healthcare Monitoring
3.1.4. Integrated Healthcare Systems
3.1.5. Discussion of Key Studies Regarding the Research Question
3.2. What Are the Current Physiological Signal Analysis Methods?
Discussion of Key Studies in This Subsection
3.3. Key Considerations
3.4. Limitations
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| No. | Ref. | Country, Year | Technology Used | Physiological Signals Sensed | Type of Device | Key Findings |
|---|---|---|---|---|---|---|
| 1. | [34] | Qatar, 2020 | Multicore processors, compressive sensing theory | ECG | Wearable medical sensors | Optimizing power consumption of wearable medical sensors and practical applications in remote health monitoring systems. |
| 2. | [100] | Italy, 2020 | Service-oriented architecture, Bluetooth | Various physiological signals | Bluetooth medical devices | Facilitates exchange and utilization of services, information, and documents in home care, cloud-based infrastructure, and web portals. |
| 3. | [28] | Italy, 2020 | IoT, wearable sensors | Heart rate, blood pressure, temperature | Wearable devices | IoT-based health monitoring systems offer continuous and real-time health data for elderly care. |
| 4. | [111] | China, 2020 | Cloud computing, wearable sensors | Heart rate, blood pressure, temperature | Wearable devices | Cloud-based health monitoring systems for elderly care using wearable technology provide scalable and efficient health monitoring solutions. |
| 5. | [77] | India, 2020 | IoT, wearable sensors | Heart rate, blood pressure, temperature | Wearable devices | IoT-enabled wearable health monitoring systems enhance elderly care through real-time data. |
| 6. | [96] | Portugal, 2020 | IoT, wearable sensors | Heart rate, blood pressure, temperature | Wearable devices | IoT-based wearable health monitoring systems enhance elderly care through real-time data collection and analysis. |
| 7. | [65] | Malaysia, 2020 | Wearable sensors, IoT, cloud computing | Heart rate, blood pressure, temperature | Wearable devices | Cloud-based health monitoring systems offer scalable solutions for elderly care using wearable technology. |
| 8. | [83] | China, 2020 | Wearable sensors, cloud computing | Heart rate, blood pressure, temperature | Wearable devices | Cloud-based systems for health monitoring offer scalable and efficient solutions for elderly care. |
| 9. | [46] | India, 2020 | IoT, wearable sensors, cloud computing | Heart rate, blood pressure, temperature | Wearable devices | Cloud-based health monitoring systems for elderly care offer scalable and efficient solutions. |
| 10. | [95] | USA, 2020 | Wearable sensors, IoT, cloud computing | Heart rate, blood pressure, temperature | Wearable devices | Cloud-based health monitoring systems offer scalable solutions for elderly care using wearable technology. |
| 11. | [54] | China, 2020 | Wearable sensors, IoT | Heart rate, blood pressure, temperature | Wearable devices | Wearable technology and IoT provide continuous and real-time health data for elderly care. |
| 12. | [47] | Portugal, 2020 | Wearable sensors, IoT | Heart rate, blood pressure, temperature | Wearable devices | Advancements in wearable technology and IoT improve elderly health monitoring. |
| 13. | [90] | Iran, 2020 | IoT, wearable sensors | Heart rate, blood pressure, temperature | Wearable devices | IoT-enabled wearable health monitoring systems enhance elderly care through real-time data. |
| 14. | [103] | Canada, 2021 | CNN, phase-based video motion processing algorithm | Heart rate, breathing rate | Android application | Higher accuracy and efficiency in estimating HR and BR compared to traditional methods, practical applications in healthcare, and disease prevention for elderly individuals. |
| 15. | [102] | Indonesia, 2021 | Signal conditioning circuit, ATMega328P microcontroller, Android application | Heart rate | Heart rate monitoring device, Android application | Efficiently monitors and retrieves patient data, providing a customizable alert mechanism through the mobile application. |
| 16. | [58] | USA, 2021 | IoT, Wearable sensors | Heart rate, blood pressure, temperature | Wearable devices | IoT-based health monitoring systems enhance elderly care through real-time data collection and analysis. |
| 17. | [29] | China, 2021 | IoT, cloud computing, wearable sensors | Heart rate, blood pressure, temperature | Wearable devices | Integrating IoT and cloud computing enhances the efficiency and accessibility of health monitoring systems. |
| 18. | [27] | France, 2021 | IoT, cloud computing, wearable sensors | Heart rate, blood pressure, temperature | Wearable devices | Wearable devices and cloud computing significantly improve healthcare monitoring and patient management. |
| 19. | [114] | China, 2021 | Wearable sensors, IoT | Heart rate, blood pressure, temperature | Wearable devices | Current technologies in wearable health monitoring systems offer improved care for elderly individuals. |
| 20. | [104] | Romania, 2021 | Google Fit application, wearable sensors | Various physiological signals | Mobile application, web dashboard | Enhances communication, continuous patient health monitoring, real-time analysis, and alerts for detected anomalies. |
| 21. | [105] | Italy, 2021 | e-health, cloud-based platform | Various physiological signals | Vital sign sensors, gateway (tablet), panic button | Enables remote management of cerebrovascular risk factors, is highly compliant with measurement tasks, and improves health outcomes for TIA/stroke patients. |
| 22. | [106] | Spain, 2021 | Sensors, cloud server, mobile application | Heart issues, falls, temperature changes | Smart garment | Provides real-time monitoring and alerts and ensures user-friendliness and effectiveness in remote monitoring of elderly individuals. |
| 23. | [37] | India, 2021 | MyRIO 1900, IoT sensors, web publishing tool | Heart rate, body temperature, blood pressure, oxygen level, breathing rate | Wearable sensors, web-based application | Cost-effective health condition diagnosis, remote access for monitoring, and live video feeds of patients. |
| 24. | [43] | China, 2021 | Cloud computing, wearable sensors | Heart rate, blood pressure, temperature | Wearable devices | Cloud-based health monitoring systems for elderly care using wearable technology provide scalable and efficient health monitoring solutions. |
| 25. | [50] | Romania, 2021 | Cloud computing, wearable sensors, IoT | Heart rate, blood pressure, temperature | Wearable devices | Cloud-based health monitoring systems for elderly care offer scalable and efficient wearable technology solutions. |
| 26. | [30] | Turkey, 2021 | IoT, wearable sensors, cloud computing | Heart rate, blood pressure, temperature | Wearable devices | Cloud computing integration in wearable health monitoring systems enhances data accessibility and efficiency. |
| 27. | [70] | Egypt, 2021 | IoT, wearable sensors | Heart rate, blood pressure, temperature | Wearable devices | IoT-enabled wearable health monitoring systems enhance elderly care through real-time data. |
| 28. | [36] | India, 2021 | IoT, sensors, AI technology | Temperature, heart rate, ECG, blood pressure, SPO2 | Sensors, microcontroller, mobile application | Allows continuous monitoring of hospital and home patients and provides healthcare professionals with real-time data access. |
| 29. | [31] | USA, 2022 | IoT, wearable sensors | Heart rate, blood pressure, temperature | Wearable devices | IoT and wearable technology provide effective health monitoring solutions for elderly care. |
| 30. | [61] | Thailand, 2022 | Cloud computing, wearable sensors | Heart rate, blood pressure, temperature | Wearable devices | Cloud-based systems offer scalable and efficient health monitoring solutions for elderly care. |
| 31. | [123] | China, 2022 | IoT, wearable sensors | Heart rate, blood pressure, temperature | Wearable devices | IoT-based health monitoring systems offer continuous and real-time health data for elderly care. |
| 32. | [44] | Romania, 2022 | Cloud computing, wearable sensors | Heart rate, blood pressure, temperature | Wearable devices | Cloud-based systems offer scalable and efficient health monitoring solutions for elderly care. |
| 33. | [101] | Italy, 2022 | Bluetooth, Android app, MariaDB | Blood pressure, heart rate | Wearable devices | Enhances healthcare delivery, cost-efficiency, and patient monitoring by leveraging remote monitoring and real-time data access. |
| 34. | [62] | Brazil, 2022 | Internet of Things, Firebase platform | Heart rate, blood oxygenation, temperature | Wearable glove | Offers real-time data monitoring and presents a cost-effective alternative to commercial devices. |
| 35. | [35] | Malaysia, 2022 | MAX30102, GPS, NodeMCU, Blynk application | Heart rate, oxygen saturation | Wearable prototype | Provides real-time monitoring, patient location information, and a user-friendly mobile application. |
| 36. | [109] | Italy, 2022 | Wearable sensors, IoT | Heart rate, blood pressure, temperature | Wearable devices | Advancements in wearable technology and IoT integration improve health monitoring for elderly individuals. |
| 37. | [89] | Poland, 2022 | IoT, wearable sensors | Heart rate, blood pressure, oxygen saturation | Wearable devices, mobile applications | IoT-based healthcare systems offer real-time monitoring and improved patient outcomes. |
| 38. | [38] | China, 2022 | IoT, wearable sensors | Heart rate, blood pressure, temperature | Wearable devices | IoT-based health monitoring systems improve elderly care through real-time data collection and analysis. |
| 39. | [40] | Germany, 2022 | Wearable sensors, IoT | Heart rate, blood pressure, temperature | Wearable devices | Wearable technology and IoT for health monitoring elderly individuals offer effective health monitoring solutions. |
| 40. | [74] | India, 2022 | IoT, wearable sensors | Heart rate, blood pressure, temperature | Wearable devices | Prototype for geriatric health monitoring using an IoT cloud platform for data transmission. |
| 41. | [119] | Taiwan, 2022 | IoT, wearable sensors | Heart rate, blood pressure, temperature | Wearable devices | IoT-based health monitoring systems offer continuous and real-time health data for elderly care. |
| 42. | [87] | China, 2022 | Wearable sensors, IoT | Heart rate, blood pressure, temperature | Wearable devices | Wearable technology and IoT offer effective health monitoring solutions for elderly care. |
| 43. | [60] | Malaysia, 2022 | Wearable sensors, IoT | Heart rate, blood pressure, temperature | Wearable devices | Wearable technology and IoT for health monitoring elderly individuals offer effective health monitoring solutions. |
| 44. | [86] | Ukraine, 2022 | Cloud computing, wearable sensors | Heart rate, blood pressure, temperature | Wearable devices | Cloud-based systems offer scalable and efficient health monitoring solutions for elderly care. |
| 45. | [45] | Saudi Arabia, 2022 | IoT, wearable sensors | Heart rate, blood pressure, temperature | Wearable devices | Wearable health monitoring systems for elderly individuals provide comprehensive and real-time health data. |
| 46. | [69] | Portugal, 2022 | Wearable sensors, IoT, cloud computing | Heart rate, blood pressure, temperature | Wearable devices | Cloud-based health monitoring systems for elderly care using wearable technology provide scalable and efficient solutions. |
| 47. | [78] | Saudi Arabia, 2022 | Wearable sensors, IoT | Heart rate, blood pressure, temperature | Wearable devices | Wearable health monitoring systems provide comprehensive health data for elderly care. |
| 48. | [99] | Slovakia, 2022 | IoT, wearable sensors | Heart rate, blood pressure, temperature | Wearable devices | IoT-enabled health monitoring systems for elderly individuals enhance real-time data collection and care. |
| 49. | [73] | India, 2022 | IoT, wearable sensors | Heart rate, blood pressure, temperature | Wearable devices | Wearable health monitoring systems for elderly individuals provide comprehensive and real-time health data. |
| 50. | [112] | India, 2022 | IoT, wearable sensors, cloud computing | Heart rate, blood pressure, respiration rate | Wearable belt-based sensor | The system integrates various biomedical sensors and offers timely alerts to healthcare providers. |
| 51. | [48] | United Kingdom, 2022 | Wearable sensors, IoT, AI | Heart rate, blood pressure, temperature | Wearable devices | AI and IoT integration in wearable health monitoring systems enhances elderly care. |
| 52. | [94] | India, 2022 | Wearable sensors, IoT | Heart rate, blood pressure, temperature | Evaluation on wearable devices | An in-depth evaluation of the performance of machine learning algorithms in system-on-chips embedded in a wearable healthcare monitoring device. |
| 53. | [32] | China, 2023 | Wearable sensors, cloud computing | Heart rate, blood pressure, temperature | Wearable devices | Cloud-based systems for health monitoring offer scalable and efficient solutions for elderly care. |
| 54. | [51] | Mexico, 2023 | Wearable sensors, IoT | Heart rate, blood pressure, temperature | Wearable devices | Wearable health monitoring systems provide continuous and real-time health data for elderly care. |
| 55. | [97] | USA, 2023 | Wearable sensors, IoT, cloud computing | Heart rate, blood pressure, temperature | Wearable devices | Cloud-based health monitoring systems for elderly care using wearable technology provide scalable and efficient solutions. |
| 56. | [72] | Saudi Arabia, 2023 | IoT, wearable sensors, cloud computing | Heart rate, blood pressure, temperature | Wearable devices | Cloud computing integration in wearable health monitoring systems enhances data accessibility and efficiency. |
| 57. | [25] | India, 2023 | Cloud computing, wearable sensors | Heart rate, blood pressure, temperature | Wearable devices | Cloud-based systems provide scalable and efficient health monitoring solutions for elderly care. |
| 58. | [107] | Taiwan, 2023 | IoT devices, smart necklace, mobile application | Various physiological signals | Wearable devices, mobile application | Provides real-time positioning and environmental monitoring and enhances caregiver monitoring capabilities. |
| 59. | [93] | Japan, 2023 | Blockchain, Wear OS, Bluetooth | Various physiological signals | Wearable devices | Confirmed effectiveness in the pilot test; further validation is needed. |
| 60. | [110] | Thailand, 2023 | IoT, MAX30102, LM35, NodeMCU ESP32 DevKit, myHealth application | Pulse, oxygen saturation, temperature | Wearable device, mobile application | Monitors vital health parameters and provides accurate measurements and valuable functionalities. |
| 61. | [26] | Philippines, 2023 | Various technologies | Various physiological signals | Wearable devices | Provides real-time health monitoring and improves elderly care. |
| 62. | [63] | Honduras, 2023 | Smart home technology, IoT, AI | Heart rate, movement, fall detection | Home-based sensors, wearable devices | Smart home systems provide efficient and real-time health monitoring, enhancing elderly care. |
| 63. | [76] | India, 2023 | Cloud computing, wearable sensors | Heart rate, blood pressure, temperature | Wearable devices | Cloud-based health monitoring systems for elderly care using wearable technology provide scalable and efficient health monitoring solutions. |
| 64. | [117] | China, 2023 | Wearable sensors, IoT | Heart rate, blood pressure, temperature | Wearable devices | Technological advancements in wearables and IoT enhance elderly health monitoring. |
| 65. | [121] | India, 2023 | Wearable sensors, IoT | Heart rate, blood pressure, temperature | Wearable devices | Wearable health monitoring systems provide comprehensive health data for elderly care. |
| 66. | [39] | China, 2023 | IoT, wearable sensors | Heart rate, blood pressure, temperature | Wearable devices | IoT-enabled wearable health monitoring systems enhance elderly care through real-time data. |
| 67. | [92] | Brazil, 2023 | Wearable sensors, IoT | Heart rate, blood pressure, temperature | Wearable devices | Developed a prototype system for healthcare monitoring that uses wearable devices to collect physiological data from patients. |
| 68. | [64] | Iraq, 2023 | IoT, wearable sensors | Heart rate, blood pressure, temperature | Wearable devices | IoT-based health monitoring systems offer continuous and real-time health data for elderly care. |
| 69. | [81] | China, 2023 | Wearable sensors, IoT | Heart rate, blood pressure, temperature | Wearable devices | Wearable health monitoring systems provide continuous and real-time health data for elderly care. |
| 70. | [118] | China, 2023 | IoT, wearable sensors | Heart rate, blood pressure, temperature | Sensor and wearable device | Evaluation of a frequency-tracking algorithm for vital sign monitoring using radar data. |
| 71. | [52] | India, 2023 | Wearable sensors, IoT | Heart rate, blood pressure, temperature | Wearable devices | Wearable technology and IoT offer effective health monitoring solutions for elderly care. |
| 72. | [66] | Croatia, 2023 | Wearable sensors, IoT | Heart rate, blood pressure, temperature | Wearable devices | Examines the potential of IoT technology and wearable devices and introduces a conceptual framework for the use of wearable devices as health monitoring observers. |
| 73. | [49] | Brazil, 2023 | Wearable sensors, IoT | Heart rate, blood pressure, temperature | Wearable devices | Introduces the VitalSense model, a multi-tier remote health monitoring system for elderly care in smart cities. |
| 74. | [82] | India 2023 | Wearable sensors, IoT | Heart rate, blood pressure, temperature | Wearable devices | IoT-enabled health monitoring systems for elderly individuals provide real-time data and enhance care. |
| 75. | [56] | Ecuador, 2023 | Wearable sensors, IoT | Heart rate, blood pressure, temperature | Wearable devices | Wearable technology and IoT provide continuous and real-time health data for elderly care. |
| 76. | [71] | Kuwait, 2023 | IoT, wearable sensors, cloud computing | Heart rate, blood pressure, temperature | Wearable devices | Cloud computing integration in wearable health monitoring systems enhances data accessibility and efficiency. |
| 77. | [55] | Kazakhstan, 2023 | Wearable sensors, IoT, AI | Heart rate, blood pressure, temperature | Wearable devices | AI and IoT integration in wearable health monitoring systems enhances elderly care. |
| 78. | [115] | India, 2023 | IoT, wearable sensors | Heart rate, blood pressure, temperature | Wearable devices | IoT-based wearable health monitoring systems for elderly care provide real-time data and enhance elderly care. |
| 79. | [116] | China, 2023 | Wearable sensors, IoT | Heart rate, blood pressure, temperature | Wearable devices | Wearable health monitoring systems provide comprehensive health data for elderly care. |
| 80. | [59] | Philippines, 2023 | IoT, wearable sensors | Heart rate, blood pressure, temperature | Wearable devices | IoT-based wearable health monitoring systems enhance elderly care through real-time data collection and analysis. |
| 81. | [120] | United Kingdom, 2023 | Wearable sensors, IoT | Heart rate, blood pressure, temperature | Wearable devices | Wearable technology and IoT for health monitoring in elderly individuals offer effective solutions. |
| 82. | [124] | China, 2023 | Wearable sensors, IoT | Heart rate, blood pressure, temperature | Wearable devices | The system improves the activity recognition efficiency and stability in real time by using multi-sensor wearables and a two-channel neural network. |
| 83. | [75] | Iraq, 2023 | IoT, wearable sensors | Heart rate, blood pressure, temperature | Wearable devices | Wearable health monitoring systems provide comprehensive health data for elderly care. |
| 84. | [68] | Iraq, 2023 | Wearable sensors, IoT | Heart rate, blood pressure, temperature | Wearable devices | IoT-enabled health monitoring systems for elderly individuals provide real-time data and enhance care. |
| 85. | [42] | Norway, 2023 | Wearable sensors, IoT | Heart rate, blood pressure, temperature | Wearable devices | Wearable health monitoring systems provide continuous and real-time health data for elderly care. |
| 86. | [91] | China, 2023 | IoT, Wearable sensors | Heart rate, blood pressure, temperature | Wearable devices | Development of an IoT-based health monitoring system for elderly care through real-time data collection and analysis. |
| 87. | [41] | China, 2024 | IoT, wearable sensors | Heart rate, blood pressure, temperature | Wearable devices | A fully comprehensive and unobtrusive in-home health monitoring system tailored to elderly individuals living alone. |
| 88. | [33] | India, 2024 | Wearable sensors, IoT | Heart rate, blood pressure, temperature | Wearable devices | Wearable health monitoring systems provide continuous and real-time health data for elderly care. |
| 89. | [53] | China, 2024 | Wearable sensors, IoT | Heart rate, blood pressure, temperature | Wearable devices | IoT-enabled health monitoring systems for elderly individuals provide real-time data and enhance care. |
| 90. | [67] | China, 2024 | Wearable sensors, IoT | Heart rate, blood pressure, temperature | Wearable devices | Advancements in wearable technology and IoT improve elderly health monitoring. |
| 91. | [79] | India, 2024 | Wearable sensors, cloud computing | Heart rate, blood pressure, temperature | Wearable devices | Cloud-based systems for health monitoring offer scalable and efficient solutions for elderly care. |
| 92. | [98] | Spain, 2024 | Wearable sensors, IoT | Heart rate, blood pressure, temperature | Wearable devices | A semi-automatic mobile health system to analyze the relationship between preclinical chronic pain in elderly individuals and various physiological and stress indicators. |
| 93. | [85] | Canada, 2024 | Wearable sensors, IoT | Heart rate, blood pressure, temperature | Wearable devices | Wearable technology and IoT offer effective health monitoring solutions for elderly care. |
| 94. | [122] | Italy, 2024 | Wearable sensors, IoT | Heart rate, blood pressure, temperature | Wearable devices | Wearable health monitoring systems provide comprehensive health data for elderly care. |
| 95. | [88] | China, 2024 | Wearable sensor | Breath rate, heart rate | Wearable sensor | An innovative ionic conductive wearable material designed for real-time posture assessment and injury prevention in elderly individuals. |
| 96. | [8] | China, 2024 | Sensing technology and intelligent algorithms | Heart rate monitoring, sleep monitoring, oxygen monitoring | Wearable smart bracelet | An intelligent bracelet designed under humanized design principles, with advanced sensing technology and user-friendly features. |
| 97. | [108] | USA, 2024 | Smartphone camera, machine learning | Blood pressure | Mobile and web application | Face videos captured by a webcam or smartphone camera can help to detect hypertension-related complications early. |
| 98. | [57] | Bangladesh, 2024 | ESP32 module, GSM module, mobile application | Heart rate, oxygen saturation, temperature | Medicine reminder unit, mobile application | Improves medication adherence and patient safety through timely reminders and health monitoring features. |
| 99. | [84] | China 2024 | IoT, wearable sensors, cloud computing | Heart rate, blood pressure, temperature | Wearable devices | Cloud computing integration in wearable health monitoring systems enhances data accessibility and efficiency. |
| 100. | [113] | Mexico, 2024 | Bluetooth, IMUs | Biomechanical signals | Sensors on the body | A computer model for gait assessment in Parkinson’s disease through advanced signal processing for biomechanical indicators to enhance treatment personalization. |
References
- World Health Organization. World Report on Ageing and Health. 2015. Available online: https://iris.who.int/bitstream/handle/10665/186463/9789240694811_eng.pdf?sequence=1 (accessed on 18 February 2025).
- Dugarova, E.; Kalapurakal, R.; Conceição, P.; Horvath, B.; Lane, R.; Schmid, K.; Rafeh, A.; Ainbinder, L.; Herrmann, M.; Staab, S.; et al. United Nations Development Programme. Ageing Older Persons and the 2030 Agenda for Sustainable Development. 2017. Available online: https://www.un.org/development/desa/dspd/wp-content/uploads/sites/22/2017/08/Ageing-Older-Persons-and-2030-Agenda_Issues-Brief-low-resolution-.pdf (accessed on 18 February 2025).
- World Health Organization. Ageing and Health. 2024. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 18 February 2025).
- United Nations, Department of Economic and Social Affairs. World Social Report: Leaving No One Behind in an Ageing World; United Nations Publication: New York, NY, USA, 2023; Available online: https://desapublications.un.org/publications/worldsocial-report-2023-leaving-no-one-behind-ageing-world (accessed on 18 February 2025).
- Guzmán-Olea, E.; Agis-Juárez, R.A.; Bermúdez-Morales, V.H.; Torres-Poveda, K.; Madrid-Marina, V.; López-Romero, D.; Maya-Pérez, E. Estado de salud y valoración gerontológica en adultos mayores mexicanos ante la pandemia por COVID-19. Gac. Medica Mex. 2020, 156, 412–417. [Google Scholar] [CrossRef]
- Wróbel-Lachowska, M.; Dominiak, J.; Woźniak, M.P.; Bartłomiejczyk, N.; Diethei, D.; Wysokińska, A.; Niess, J.; Grudzień, K.; Woźniak, P.W.; Romanowski, A. ‘That’s when I put it on’: Stakeholder perspectives in large-scale remote health monitoring for older adults. Pers. Ubiquitous Comput. 2023, 27, 2193–2210. [Google Scholar] [CrossRef]
- Statista Research Department. Number of Users of Smartwatches Worldwide from 2020 to 2029. Available online: https://www.statista.com/forecasts/1314339/worldwide-users-of-smartwatches (accessed on 28 February 2025).
- Zhu, L.; Gao, Y. Design of Health Monitoring for Elderly Wearable Smart Bracelets Based on Humanized Concept. Adv. Comput. Signals Syst. 2024, 8, 1–9. [Google Scholar] [CrossRef]
- Smith, A.A.; Li, R.; Tse, Z.T.H. Reshaping healthcare with wearable biosensors. Sci. Rep. 2023, 13, 4998. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Moreno, F.M.; Bermudez-Edo, M.; Pérez-Mármol, J.M.; Garrido, J.L.; Rodríguez-Fórtiz, M.J. Systematic design of health monitoring systems centered on older adults and ADLs. BMC Med. Inform. Decis. Mak. 2023, 23, 300. [Google Scholar] [CrossRef]
- Saleh, S.; Saeidi, T.; Timmons, N.; Razzaz, F. A comprehensive review of recent methods for compactness and performance enhancement in 5G and 6G wearable antennas. Alex. Eng. J. 2024, 95, 132–163. [Google Scholar] [CrossRef]
- INEGI. Comunicado de Prensa Núm. 568/22 30 de Septiembre de 2022 Página 1/6 Estadísticas a Propósito del día Internacional de las Personas Adultas Mayores • Según la Encuesta Nacional de Ocupación y Empleo Nueva Edición ENOE. 2022. Available online: https://www.inegi.org.mx/contenidos/saladeprensa/aproposito/2022/EAP_ADULMAY2022.pdf (accessed on 30 November 2023).
- PROGRAMA Institucional del Instituto Nacional de las Personas Adultas. 2021. Available online: https://www.dof.gob.mx/nota_detalle_popup.php?codigo=5616097#:~:text=Para (accessed on 20 November 2023).
- Gallegos-Carrillo, K.; Honorato-Cabañas, Y.; Macías, N.; García-Peña, C.; Flores, Y.N.; Salmerón, J. Preventive health services and physical activity improve health-related quality of life in Mexican older adults. Salud Publica Mex. 2019, 61, 106–115. [Google Scholar] [CrossRef]
- Aakesh, U.; Rajasekaran, Y.; Sudhakar, T. Review on Healthcare Monitoring and Tracking Wristband for Elderly People using ESP-32. In Proceedings of the 2023 5th International Conference on Smart Systems and Inventive Technology (ICSSIT), Tirunelveli, India, 23–25 January 2023; pp. 523–529. [Google Scholar]
- Mohan, D.; Al-Hamid, D.Z.; Chong, P.H.J.; Sudheera, K.L.K.; Gutierrez, J.; Chan, H.C.; Li, H. Artificial Intelligence and IoT in Elderly Fall Prevention: A Review. IEEE Sens. J. 2024, 24, 4181–4198. [Google Scholar] [CrossRef]
- Fasoli, A.; Beretta, G.; Pravettoni, G.; Sanchini, V. Mapping emerging technologies in aged care: Results from an in-depth online research. BMC Health Serv. Res. 2023, 23, 528. [Google Scholar] [CrossRef]
- Masoumian Hosseini, M.; Masoumian Hosseini, S.T.; Qayumi, K.; Hosseinzadeh, S.; Sajadi Tabar, S.S. Smartwatches in healthcare medicine: Assistance and monitoring; a scoping review. BMC Med. Inform. Decis. Mak. 2023, 23, 248. [Google Scholar] [CrossRef]
- Wüller, H.; Behrens, J.; Garthaus, M.; Marquard, S.; Remmers, H. A scoping review of augmented reality in nursing. BMC Nurs. 2019, 18, 19. [Google Scholar] [CrossRef] [PubMed]
- Kazanskiy, N.L.; Khonina, S.N.; Butt, M.A. A review on flexible wearables-Recent developments in non-invasive continuous health monitoring. Sens. Actuators Phys. 2024, 366, 114993. [Google Scholar] [CrossRef]
- Ma, B.; Yang, J.; Wong, F.K.Y.; Wong, A.K.C.; Ma, T.; Meng, J.; Zhao, Y.; Wang, Y.; Lu, Q. Artificial intelligence in elderly healthcare: A scoping review. Ageing Res. Rev. 2023, 83, 101808. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. Theory Pract. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Levac, D.; Colquhoun, H.; O’brien, K.K. Scoping studies: Advancing the methodology. Implement. Sci. 2010, 5, 69. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Das, S.; Adhikary, A.; Laghari, A.A.; Mitra, S. Eldo-care: EEG with Kinect sensor based telehealthcare for the disabled and the elderly. Neurosci. Inform. 2023, 3, 100130. [Google Scholar] [CrossRef]
- Mendoza, M.B.; McAndrew, B.N.; Zari, B.B.; Bhie, D.S.J.; Joseph, T.D.K. VitalWatch: Empowering Health with Web-based Vital Sign Monitoring and Alert System using NI MyRIO. In Proceedings of the ICSIMA 2023—9th IEEE International Conference on Smart Instrumentation, Measurement and Applications, Kuala Lumpur, Malaysia, 17–18 October 2023; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2023; pp. 139–143. [Google Scholar] [CrossRef]
- Abbas, M.; Somme, D.; Jeannès, R.L.B. D-SORM: A digital solution for remote monitoring based on the attitude of wearable devices. Comput. Methods Programs Biomed. 2021, 208, 106247. [Google Scholar] [CrossRef] [PubMed]
- Rienzo, M.D.; Rizzo, G.; Işilay, Z.M.; Lombardi, P. Seismote: A multi-sensor wireless platform for cardiovascular monitoring in laboratory, daily life, and telemedicine. Sensors 2020, 20, 680. [Google Scholar] [CrossRef]
- Han, P.; Li, L.; Zhang, H.; Guan, L.; Marques, C.; Savović, S.; Ortega, B.; Min, R.; Li, X. Low-cost plastic optical fiber sensor embedded in mattress for sleep performance monitoring. Opt. Fiber Technol. 2021, 64, 102541. [Google Scholar] [CrossRef]
- Hanifi, K.; Karsligil, M.E. Elderly Fall Detection with Vital Signs Monitoring Using CW Doppler Radar. IEEE Sens. J. 2021, 21, 16969–16978. [Google Scholar] [CrossRef]
- Hu, Y.; Zhang, F.; Wu, C.; Wang, B.; Liu, K.J. DeFall: Environment-Independent Passive Fall Detection Using WiFi. IEEE Internet Things J. 2022, 9, 8515–8530. [Google Scholar] [CrossRef]
- Zhang, W.; Zhang, H.; Wu, M.; Jin, G.; Zhong, L.; Wang, Z. An AIOT-based Health Monitoring System Integrating Contact and Non-contact Detections. In Proceedings of the 2023 IEEE 6th International Conference on Electronics and Communication Engineering, ICECE 2023, Xi’an, China, 15–17 December 2023; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2023; pp. 224–228. [Google Scholar] [CrossRef]
- Maity, S.; Maji, S.; Sil, S.; Roy, A.; Sarkar, S.; Dhabal, S.; Venkateswaran, P. Homecare Robotic Systems: Wearable Remote Sensing with Interactive AI Features. In Proceedings of the APSCON 2024–2024 IEEE Applied Sensing Conference, Goa, India, 22–24 January 2024; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2024. [Google Scholar] [CrossRef]
- Djelouat, H.; Disi, M.A.; Boukhenoufa, I.; Amira, A.; Bensaali, F.; Kotronis, C.; Politi, E.; Nikolaidou, M.; Dimitrakopoulos, G. Real-time ECG monitoring using compressive sensing on a heterogeneous multicore edge-device. Microprocess. Microsyst. 2020, 72, 102839. [Google Scholar] [CrossRef]
- Hasman, N.A.; Maharum, S.M.M.; Ahmad, I.; Mansor, Z. Prototype Development of an IoT Health Monitoring Device for Elderly Patient. In Proceedings of the 8th IEEE International Conference on Smart Instrumentation, Measurement and Applications, ICSIMA 2022, Melaka, Malaysia, 26–28 September 2022; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2022; pp. 350–354. [Google Scholar] [CrossRef]
- Sangeethalakshmi, K.; Preethi, U.; Pavithra, S. Patient health monitoring system using IoT. Mater. Today Proc. 2023, 80, 2228–2231. [Google Scholar] [CrossRef]
- Swain, K.; Cherukuri, M.; Mishra, S.K.; Appasani, B.; Patnaik, S.; Bizon, N. Li-care: A labview and iot based ehealth monitoring system. Electronics 2021, 10, 3137. [Google Scholar] [CrossRef]
- Zhang, B.; Zhu, L.; Pei, Z.; Zhai, Q.; Zhu, J.; Zhong, X.; Yi, J.; Liu, T. A Framework for Remote Interaction and Management of Home Care Elderly Adults. IEEE Sens. J. 2022, 22, 11034–11044. [Google Scholar] [CrossRef]
- Guo, P.; Li, Q.; Zhu, Y.; Hejiaojiao, H.; Yang, J.; Zhang, C.; Gao, J.; Wang, X. A Household Multimodal Physiological Signals Monitoring System. In Proceedings of the ITNEC 2023—IEEE 6th Information Technology, Networking, Electronic and Automation Control Conference, Chongqing, China, 24–26 February 2023; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2023; pp. 1715–1718. [Google Scholar] [CrossRef]
- Friedrich, P.; Gaiduk, M.; Alarcón, Á.S.; Scherz, D.; Madrid, N.M.; Seepold, R.; Gaßner, M.; Fuchs, D. Assistive health systems for home-dwelling elderly: Connecting training and monitoring technologies to a data integration platform. Procedia Comput. Sci. 2022, 207, 3002–3011. [Google Scholar] [CrossRef]
- Huang, Z.; Li, J.; He, Z. Full-coverage unobtrusive health monitoring of elders at homes. Internet Things 2024, 26, 101182. [Google Scholar] [CrossRef]
- Djenouri, Y.; Belbachir, A.N.; Cano, A.; Belhadi, A. Spatio-temporal visual learning for home-based monitoring. Inf. Fusion 2024, 101, 101984. [Google Scholar] [CrossRef]
- Zhang, S.; Liu, X.; Liu, Y.; Ding, B.; Guo, S.; Wang, J. Accurate Respiration Monitoring for Mobile Users with Commercial RFID Devices. IEEE J. Sel. Areas Commun. 2021, 39, 513–525. [Google Scholar] [CrossRef]
- Alexandrescu, A.; Botezatu, N.; Lupu, R. Monitoring and processing of physiological and domotics parameters in an Internet of Things (IoT) assistive living environment. In Proceedings of the 2022 26th International Conference on System Theory, Control and Computing, ICSTCC 2022—Proceedings, Sinaia, Romania, 19–21 October 2022; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2022; pp. 362–367. [Google Scholar] [CrossRef]
- Thaljaoui, A.; El, S.; Zeadally, S.; Alourani, A. Remote monitoring system using Light Fidelity and InfraRed. Comput. Electr. Eng. 2022, 101, 108073. [Google Scholar] [CrossRef]
- Srinivasan, A.; Natarajan, N.; Karunakaran, R.V.; Elangovan, R.; Shankar, A.; Sabharish, P.M.; Sreeja, B.S.; Radha, S. Elder Care System using IoT and Machine Learning in AWS Cloud. In Proceedings of the HONET 2020—IEEE 17th International Conference on Smart Communities: Improving Quality of Life Using ICT, IoT and AI, Charlotte, NC, USA, 14–16 December 2020; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2020; pp. 92–98. [Google Scholar] [CrossRef]
- Lousado, J.P.; Antunes, S. e-Health Monitoring System for Senior Citizens based on LoRa Technology. In Proceedings of the 2020 5th International Conference on Smart and Sustainable Technologies (SpliTech), Split, Croatia, 23–26 September 2020. [Google Scholar]
- Wu, J.; Dahnoun, N. A health monitoring system with posture estimation and heart rate detection based on millimeter-wave radar. Microprocess. Microsyst. 2022, 94, 104670. [Google Scholar] [CrossRef]
- Rodrigues, V.F.; da Rosa Righi, R.; da Costa, C.A.; Zeiser, F.A.; Eskofier, B.; Maier, A.; Kim, D. Digital health in smart cities: Rethinking the remote health monitoring architecture on combining edge, fog, and cloud. Health Technol. 2023, 13, 449–472. [Google Scholar] [CrossRef]
- Paraschiv, E.A.; Tudora, E.; Tirziu, E.; Alexandru, A. IoT Cloud Computing-based Remote Healthcare Monitoring System for an Elderly-Centered Care. In Proceedings of the 2021 9th E-Health and Bioengineering Conference, EHB, Iasi, Romania, 18–19 November 2021; pp. 19–22. [Google Scholar] [CrossRef]
- Del-Valle-Soto, C.; Briseño, R.A.; Valdivia, L.J.; Velázquez, R.; Nolazco-Flores, J.A. Non-Invasive Monitoring of Vital Signs for the Elderly Using Low-Cost Wireless Sensor Networks: Exploring the Impact on Sleep and Home Security. Future Internet 2023, 15, 287. [Google Scholar] [CrossRef]
- Tewari, R.C.; Sharma, S.; Routray, A.; Maiti, J. Effective fall detection and post-fall breath rate tracking using a low-cost CW Doppler radar sensor. Comput. Biol. Med. 2023, 164, 107315. [Google Scholar] [CrossRef]
- Li, Q.; Liu, J.; Gravina, R.; Zang, W.; Li, Y.; Fortino, G. A UWB-Radar-Based Adaptive Method for In-Home Monitoring of Elderly. IEEE Internet Things J. 2024, 11, 6241–6252. [Google Scholar] [CrossRef]
- Zhang, G. A wearable device for health management detection of multiple physiological parameters based on ZigBee wireless networks. Meas. J. Int. Meas. Confed. 2020, 165, 108168. [Google Scholar] [CrossRef]
- Yazici, A.; Zhumabekova, D.; Nurakhmetova, A.; Yergaliyev, Z.; Yatbaz, H.Y.; Makisheva, Z.; Lewis, M.; Ever, E. A smart e-health framework for monitoring the health of the elderly and disabled. Internet Things 2023, 24, 100971. [Google Scholar] [CrossRef]
- Guamán-Egas, J.; Castro-Martin, A.P. Fall Detection with Artificial Intelligence and IoT Health Monitoring System. In Proceedings of the ECTM 2023–2023 IEEE 7th Ecuador Technical Chapters Meeting, Ambato, Ecuador, 10–13 October 2023; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2023. [Google Scholar] [CrossRef]
- Paul, L.C.; Ahmed, S.S.; Rani, T.; Haque, M.A.; Roy, T.K.; Hossain, M.N.; Hossain, M.A. A smart medicine reminder kit with mobile phone calls and some health monitoring features for senior citizens. Heliyon 2024, 10, e26308. [Google Scholar] [CrossRef] [PubMed]
- Valero, M.; Clemente, J.; Li, F.; Song, W.Z. Health and sleep nursing assistant for real-time, contactless, and non-invasive monitoring. Pervasive Mob. Comput. 2021, 75, 101422. [Google Scholar] [CrossRef]
- Yang, L. Data monitoring for a physical health system of elderly people using smart sensing technology. Wirel. Netw. 2023, 29, 3665–3678. [Google Scholar] [CrossRef]
- Ismail, S. Personalised Geriatric Health Monitoring: The Need for Process Mining Approach. In Proceedings of the IVIT 2022–Proceedings of 1st International Visualization, Informatics and Technology Conference, Kuala Lumpur, Malaysia, 1–2 November 2022; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2022; pp. 143–147. [Google Scholar] [CrossRef]
- Samartkit, P.; Pullteap, S.; Bernal, O. A non-invasive heart rate and blood pressure monitoring system using piezoelectric and photoplethysmographic sensors. Meas. J. Int. Meas. Confed. 2022, 196, 111211. [Google Scholar] [CrossRef]
- Matsuo, A.K.; Guterres, B.A.; Colares, N.D.; Pessoa, O.N.; Santos, A.E.; Luiz, D.F.; Carvalho, C.B.; Junior, S.S. A Low-cost IoT Mobile System for Monitoring Vital Signs of Elderly People. In Proceedings of the 2022 Symposium on Internet of Things, SIoT 2022, São Paulo, Brazil, 24–28 October 2022; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2022. [Google Scholar] [CrossRef]
- Ulloa, A.I.S.; Ramos, L.G.G.; Espinoza, M.J.M.; Lagos, F.D.L.C.; Cruz, K.F.M. loT Based Prototype for Monitoring the Elderly. In Proceedings of the 2023 IEEE 41st Central America and Panama Convention, CONCAPAN XLI 2023, Tegucigalpa, Honduras, 8–10 November 2023; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2023. [Google Scholar] [CrossRef]
- Zearah, S.A.; Abed, A.M.; Hussian, A.; Ettyem, S.A.; Hussam, R.; Matti, I. Internet of Things and wearable device-basedtracking of an elderly person’s physical activity. In Proceedings of the 1st International Conference on Emerging Research in Computational Science, ICERCS 2023—Proceedings, Coimbatore, India, 7–9 December 2023; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2023. [Google Scholar] [CrossRef]
- Yew, H.T.; Ng, M.F.; Ping, S.Z.; Chung, S.K.; Chekima, A.; Dargham, J.A. IoT Based Real-Time Remote Patient Monitoring System. In Proceedings of the 2020 16th IEEE International Colloquium on Signal Processing & Its Applications (CSPA), Langkawi, Malaysia, 28–29 February 2020; pp. 176–179. [Google Scholar]
- Zovko, K.; Šerić, L.; Perković, T.; Belani, H.; Šolić, P. IoT and health monitoring wearable devices as enabling technologies for sustainable enhancement of life quality in smart environments. J. Clean. Prod. 2023, 413, 137506. [Google Scholar] [CrossRef]
- Yurong, N. Research on the remote monitoring system for falls in the elderly based on the internet of things and six axis acceleration sensors. Meas. Sens. 2024, 32, 101085. [Google Scholar] [CrossRef]
- Dujaili, M.J.A.; Dhaam, H.Z.; Mezeel, M.T. An intelligent fall detection algorithm for elderly monitoring in the internet of things platform. Multimed. Tools Appl. 2024, 83, 5683–5695. [Google Scholar] [CrossRef]
- Famá, F.; Faria, J.N.; Portugal, D. An IoT-based interoperable architecture for wireless biomonitoring of patients with sensor patches. Internet Things 2022, 19, 100547. [Google Scholar] [CrossRef]
- Zouka, H.A.E.; Hosni, M.M. Secure IoT communications for smart healthcare monitoring system. Internet Things 2021, 13, 100036. [Google Scholar] [CrossRef]
- Aldousari, A.; Alotaibi, M.; Khajah, F.; Jaafar, A.; Alshebli, M.; Kanj, H. A Wearable IOT- based Healthcare Monitoring System for Elderly People. In Proceedings of the BioSMART 2023—Proceedings: 5th International Conference on Bio-Engineering for Smart Technologies, Paris, France, 7–9 June 2023; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2023. [Google Scholar] [CrossRef]
- Alshammari, H.H. The internet of things healthcare monitoring system based on MQTT protocol. Alex. Eng. J. 2023, 69, 275–287. [Google Scholar] [CrossRef]
- Rajesh, T.; Babu, T.; Nair, R.R.; Nivedha, S. Secure remote health monitoring system and assessment using IoT. In Proceedings of the 2022 International Conference on Artificial Intelligence and Data Engineering (AIDE), Karkala, India, 22–23 December 2022; pp. 295–300. [Google Scholar]
- Lakshmi, P.P.; Nair, H.; Pravin, N.; Sreedher, A. Smart Health Monitoring System for the Elderly. In Proceedings of the 2nd IEEE International Conference on Advanced Technologies in Intelligent Control, Environment, Computing and Communication Engineering, ICATIECE 2022, Bangalore, India, 16–17 December 2022; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2022. [Google Scholar] [CrossRef]
- Farej, Z.K.; Al-hayaly, H.Y. Accuracy Evaluation of Healthcare Monitoring System Based on ESP32 Microcontroller with IoT. In Proceedings of the 2023 International Conference on Engineering, Science and Advanced Technology (ICESAT), Mosul, Iraq, 21–22 June 2023; pp. 90–94. [Google Scholar]
- Ahila, A.; Dahan, F.; Alroobaea, R.; Alghamdi, W.Y.; Mohammed, M.K.; Hajjej, F.; mohammed alsekait, D.; Raahemifar, K. A smart IoMT based architecture for E-healthcare patient monitoring system using artificial intelligence algorithms. Front. Physiol. 2023, 14, 1125952. [Google Scholar] [CrossRef]
- Rathy, G.A.; Sivasankar, P.; Fadhil, T.Z. An efficient IoT based biomedical health monitoring and diagnosing system using myRIO. Telkomnika Telecommun. Comput. Electron. Control 2020, 18, 3050–3057. [Google Scholar] [CrossRef]
- Kamruzzaman, M.M.; Alanazi, S.; Alruwaili, M.; Alrashdi, I.; Alhwaiti, Y.; Alshammari, N. Fuzzy-assisted machine learning framework for the fog-computing system in remote healthcare monitoring. Meas. J. Int. Meas. Confed. 2022, 195, 111085. [Google Scholar] [CrossRef]
- Ediga, P.; Gullapelly, P.; Edukulla, T.; Nunna, K.; Al-Farouni, M.; V, R.; Singh, N.; Kumar, A. Promoting sustainable living: IoT-integrated smart homes for elderly people. E3S Web Conf. 2024, 507, 01033. [Google Scholar] [CrossRef]
- Vijender, V.E.B.; Solanki, K.; Kumar, R.; Atiqur, M.; Ahad, R. Intelligent Systems Reference Library 165 A Handbook of Internet of Things in Biomedical and Cyber Physical System; Springer: Berlin/Heidelberg, Germany, 2020. [Google Scholar]
- Yi, X.; Yan, Z.; Zhou, X.; Liu, Y.; Huang, F.; Liu, Z. Design of Intelligent Wearable Devices for the Elderly Based on ARM. In Proceedings of the Proceedings–2023 3rd Asia-Pacific Conference on Communications Technology and Computer Science, ACCTCS 2023, Shenyang, China, 25–27 February 2023; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2023; pp. 263–266. [Google Scholar] [CrossRef]
- Aakesh, U.; Rajasekaran, Y.; Janney, J.B. Wristband for Elderly Individuals: Esp-32 and Arduino Nano Enabled Solution for Health Monitoring and Tracking. In Proceedings of the 2023 IEEE Asia-Pacific Conference on Geoscience, Electronics and Remote Sensing Technology: Global Challenges in Geoscience, Electronics, and Remote Sensing: Future Directions in City, Land, and Ocean Sustainable Development, AGERS 2023, Surabaya, Indonesia, 19–20 December 2023; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2023; pp. 26–33. [Google Scholar] [CrossRef]
- Hu, J.; Wang, J.; Xie, H. Wearable bracelets with variable sampling frequency for measuring multiple physiological parameter of human. Comput. Commun. 2020, 161, 257–265. [Google Scholar] [CrossRef]
- Liao, Y.; Tian, S.; Li, Y.; Li, L.; Chen, X.; Chen, J.; Yang, F.; Gao, M. Ambient nano RF-Energy driven self-powered wearable multimodal real-time health monitoring. Nano Energy 2024, 128, 109915. [Google Scholar] [CrossRef]
- Tanbeer, S.K.; Sykes, E.R. MiVitals–Mixed Reality Interface for Vitals Monitoring: A HoloLens based prototype for healthcare practices. Comput. Struct. Biotechnol. J. 2024, 24, 160–175. [Google Scholar] [CrossRef]
- Semenov, A.; Semenova, O.; Meulesteen, S.; Koval, K.; Datsiuk, D.; Fomenko, H.; Ageyev, D. Cellular IoT Personal Health and Safety Monitoring. In Proceedings of the 2022 IEEE 9th International Conference on Problems of Infocommunications Science and Technology, PIC S and T 2022—Proceedings, Kharkiv, Ukraine, 10–12 October 2022; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2022; pp. 433–438. [Google Scholar] [CrossRef]
- Du, L.; Guo, B.; Dong, Y.; Kong, D.; Zhao, J.; Liu, X.; Liu, J. A wearable omnidirectional inertial switch of security detection for the elderly. Microsyst. Technol. 2022, 28, 2011–2021. [Google Scholar] [CrossRef]
- Zhang, Y.A.; Wang, C.Y.; Wang, X.X.; Yin, M.; Wang, K.; Zhou, D.W.; Zheng, H.L.; Yu, S.S.; Li, S.; Chen, K.Z.; et al. Mechanical robust, adhesive, self-healable and biodegradable protein-based electronic skin sensors for smart elderly care. Chem. Eng. J. 2024, 482, 148785. [Google Scholar] [CrossRef]
- Nowosielski, L.; Dudziński, B.; Ślubowska, A.M. “Smart clothing” wearable for vital signs monitoring. Prz. Elektrotechniczny 2022, 98, 62–66. [Google Scholar] [CrossRef]
- Hosseinzadeh, M.; Koohpayehzadeh, J.; Ghafour, M.Y.; Ahmed, A.M.; Asghari, P.; Souri, A.; Pourasghari, H.; Rezapour, A. An elderly health monitoring system based on biological and behavioral indicators in internet of things. J. Ambient. Intell. Humaniz. Comput. 2023, 14, 5085–5095. [Google Scholar] [CrossRef]
- Qin, W.F.; Xue, Y.; Peng, H.; Li, G.; Chen, W.; Zhao, X.; Pang, J.; Zhou, B. Wearable real-time multi-health parameter monitoring system. Int. J. Cloth. Sci. Technol. 2024, 36, 17–33. [Google Scholar] [CrossRef]
- da Rosa Fröhlich, W.; Rigo, S.J.; Bez, M.R. ATHENA I—An architecture for near real-time physiological signal monitoring and pattern detection. Future Gener. Comput. Syst. 2023, 150, 395–411. [Google Scholar] [CrossRef]
- Nakamura, K.; Yamazaki, K.; Arano, Y.; Yamazaki, A.; Koga, H.; Ohta, N.; Mitsuhashi, T.; Obinata, H.; Ohyama, Y. Pilot test of the mutual assistance system using a wearable device for the elderly in WEB3.0 technology. In Proceedings of the Proceedings—2023 14th IIAI International Congress on Advanced Applied Informatics, IIAI-AAI 2023, Koriyama, Japan, 8–13 July 2023; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2023; pp. 705–708. [Google Scholar] [CrossRef]
- Nandi, P.; Anupama, K.R.; Bajaj, A.; Shukla, S.; Musale, T.; Kachadiya, S. Performance evaluation of Machine Learning algorithms on System on Chips in Wearables for Healthcare Monitoring. Procedia Comput. Sci. 2022, 218, 2755–2766. [Google Scholar] [CrossRef]
- Hahnen, C.; Freeman, C.G.; Haldar, N.; Hamati, J.N.; Bard, D.M.; Murali, V.; Merli, G.J.; Joseph, J.I.; Helmond, N.V. Accuracy of vital signs measurements by a smartwatch and a portable health device: Validation study. JMIR mHealth uHealth 2020, 8, e16811. [Google Scholar] [CrossRef]
- Correia, B.; Dias, N.; Costa, P.; Pêgo, J.M. Validation of a wireless bluetooth photoplethysmography sensor used on the earlobe for monitoring heart rate variability features during a stress-inducing mental task in healthy individuals. Sensors 2020, 20, 3905. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Y.; Spies, C.; Magin, J.; Bhosai, S.J.; Snyder, L.; Dunn, J. Investigating the accuracy of blood oxygen saturation measurements in common consumer smartwatches. PLoS Digit. Health 2023, 2, e0000296. [Google Scholar] [CrossRef]
- Gungormus, D.B.; Garcia-Moreno, F.M.; Bermudez-Edo, M.; Sánchez-Bermejo, L.; Garrido, J.L.; Rodríguez-Fórtiz, M.J.; Pérez-Mármol, J.M. A semi-automatic mHealth system using wearable devices for identifying pain-related parameters in elderly individuals. Int. J. Med. Inform. 2024, 184, 105371. [Google Scholar] [CrossRef]
- Přibil, J.; Přibilová, A.; Frollo, I. Comparison of Three Prototypes of PPG Sensors for Continual Real-Time Measurement in Weak Magnetic Field. Sensors 2022, 22, 3769. [Google Scholar] [CrossRef]
- MacIs, S.; Loi, D.; Ulgheri, A.; Pani, D.; Solinas, G.; Manna, S.L.; Cestone, V.; Guerri, D.; Raffo, L. Design and Usability Assessment of a Multi-Device SOA-Based Telecare Framework for the Elderly. IEEE J. Biomed. Health Inform. 2020, 24, 268–279. [Google Scholar] [CrossRef]
- Palma, L.D.; Attivissimo, F.; Nisio, A.D.; Lanzolla, A.M.L.; Ragolia, M.A.; Spadavecchia, M. Development of a web-based system for interfacing a portable Bluetooth vital sign monitor. In Proceedings of the 2022 IEEE International Symposium on Medical Measurements and Applications, MeMeA 2022—Conference Proceedings, Messina, Italy, 22–24 June 2022; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2022. [Google Scholar] [CrossRef]
- Fajrin, H.R.; Adi, B.S.; Purwoko, H.; Sari, I.P. Telemedicine-equipped android interface-based heart rate monitoring. Indones. J. Electr. Eng. Comput. Sci. 2021, 21, 1332–1340. [Google Scholar] [CrossRef]
- Wang, H.; Zhou, Y.; Saddik, A.E. VitaSi: A real-time contactless vital signs estimation system. Comput. Electr. Eng. 2021, 95, 107392. [Google Scholar] [CrossRef]
- Gîstescu, A.E.; Proca, T.; Milut, C.M.; Iftene, A. MedPlus—A cross-platform application that allows remote patient monitoring. Procedia Comput. Sci. 2021, 192, 3751–3760. [Google Scholar] [CrossRef]
- Ajčević, M.; Furlanis, G.; Naccarato, M.; Caruso, P.; Polverino, P.; Marsich, A.; Accardo, A.; Manganotti, P. e-Health solution for home patient telemonitoring in early post-acute TIA/Minor stroke during COVID-19 pandemic. Int. J. Med. Inform. 2021, 152, 104442. [Google Scholar] [CrossRef]
- Luna-Perejón, F.; Muñoz-Saavedra, L.; Castellano-Domínguez, J.M.; Domínguez-Morales, M. IoT garment for remote elderly care network. Biomed. Signal Process. Control 2021, 69, 102848. [Google Scholar] [CrossRef]
- Liang, Y.S.; Tseng, Y.T.; Lin, H.Y. Design and Development of a User-Centric Wearable Device Application for Elderly Care. In Proceedings of the Proceedings of the 2023 IEEE 6th International Conference on Knowledge Innovation and Invention, ICKII 2023, Sapporo, Japan, 11–13 August 2023; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2023; pp. 29–32. [Google Scholar] [CrossRef]
- Alam, K.S.; Mamun, S.M.; Rabbani, M.; Sridevi, P.; Ahamed, S.I. UbiHeart: A novel approach for non-invasive blood pressure monitoring through real-time facial video. Smart Health 2024, 32, 100473. [Google Scholar] [CrossRef]
- Ciocca, G.; Napoletano, P.; Romanato, M.; Schettini, R. A health telemonitoring platform based on data integration from different sources. In Proceedings of the IEEE International Conference on Consumer Electronics—Berlin, ICCE-Berlin, Berlin, Germany, 2–6 September 2022; Volume 2022. [Google Scholar] [CrossRef]
- Sinchai, A.; Thippakdee, C.; Theeranukul, C.; Sri-Utaiwong, C.; Phasujit, T.; Malithong, P. A real-time web-based application of healthcare monitoring and notification system using IoT technology. In Proceedings of the ACM International Conference Proceeding Series, Tokyo Japan, 22–24 September 2023; Association for Computing Machinery: New York, NY, USA, 2023; Volume 9, pp. 104–112. [Google Scholar] [CrossRef]
- Ding, S.; Wang, X. Medical remote monitoring of multiple physiological parameters based on wireless embedded internet. IEEE Access 2020, 8, 78279–78292. [Google Scholar] [CrossRef]
- Nimi, W.S.; Jose, P.S.H.; Jegan, R.; El-Shahat, A. A Reliable and Smart E-Healthcare System for Monitoring Intravenous Fluid Level, Pulse, and Respiration Rate. Int. J. Reliab. Qual. E-Healthc. 2022, 11, 19. [Google Scholar] [CrossRef]
- Sánchez-Fernández, L.P.; Sánchez-Pérez, L.A.; Martínez-Hernández, J.M. Computer model for gait assessments in Parkinson’s patients using a fuzzy inference model and inertial sensors. Artif. Intell. Med. 2025, 160, 103059. [Google Scholar] [CrossRef]
- Ren, W.; Qi, F.; Foroughian, F.; Kvelashvili, T.; Liu, Q.; Kilic, O.; Long, T.; Fathy, A.E. Vital sign detection in any orientation using a distributed radar network via modified independent component analysis. IEEE Trans. Microw. Theory Tech. 2021, 69, 4774–4790. [Google Scholar] [CrossRef]
- Rosaline, R.A.A.; Ponnuviji, N.P.; Subbu, S.L.; Manisha, G. Enhancing lifestyle and health monitoring of elderly populations using CSA-TkELM classifier. Knowl.-Based Syst. 2023, 276, 110758. [Google Scholar] [CrossRef]
- Yang, L.; Yu, Y.; Hou, W.; Wu, X.; Chen, L. An Automatic Remote Health Risk Assessment system based on LSTM for elderly. In Proceedings of the Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society, EMBS, Sydney, Australia, 24–27 July 2023; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2023. [Google Scholar] [CrossRef]
- Wang, Y.; An, X.; Xu, W. Intelligent medical IoT health monitoring system based on VR and wearable devices. J. Intell. Syst. 2023, 32, 20220291. [Google Scholar] [CrossRef]
- Cao, L.; Wei, R.; Zhao, Z.; Wang, D.; Fu, C. A Novel Frequency-Tracking Algorithm for Noncontact Vital Sign Monitoring. IEEE Sens. J. 2023, 23, 23044–23057. [Google Scholar] [CrossRef]
- Lin, B.S.; Yu, T.; Peng, C.W.; Lin, C.H.; Hsu, H.K.; Lee, I.J.; Zhang, Z. Fall Detection System with Artificial Intelligence-Based Edge Computing. IEEE Access 2022, 10, 4328–4339. [Google Scholar] [CrossRef]
- Khan, S.; Alzaabi, A.; Ratnarajah, T.; Arslan, T. Novel statistical time series data augmentation and machine learning based classification of unobtrusive respiration data for respiration Digital Twin model. Comput. Biol. Med. 2024, 168, 107825. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharyya, T.; Ghosal, P. A Fall Detection System using Hybrid Inertial and Physiological Signal Classifiers for Dynamic Environments. In Proceedings of the Proceedings—2023 IEEE International Symposium on Smart Electronic Systems, iSES 2023, Ahmedabad, India, 18–20 December 2023; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2023; pp. 51–56. [Google Scholar] [CrossRef]
- Caroppo, A.; Manni, A.; Rescio, G.; Siciliano, P.; Leone, A. Vital signs estimation in elderly using camera-based photoplethysmography. Multimed. Tools Appl. 2024, 83, 65363–65386. [Google Scholar] [CrossRef]
- Wu, S.; Ou, J.; Shu, L.; Hu, G.; Song, Z.; Xu, X.; Chen, Z. MhNet: Multi-scale spatio-temporal hierarchical network for real-time wearable fall risk assessment of the elderly. Comput. Biol. Med. 2022, 144, 105355. [Google Scholar] [CrossRef]
- Ren, Y.; Zhu, D.; Tong, K.; Xv, L.; Wang, Z.; Kang, L.; Chai, J. PDC–HAR: Human activity recognition via multi-sensor wearable networks using two-channel convolutional neural networks. Pervasive Mob. Comput. 2024, 97, 101868. [Google Scholar] [CrossRef]
| Database | Science Direct | Springer Link | IEEE Xplore | ACM Digital Library | Scopus | Google Scholar | PubMed |
|---|---|---|---|---|---|---|---|
| Papers | 39 | 6 | 38 | 1 | 14 | 1 | 1 |
| English | 39 | 6 | 38 | 1 | 14 | 1 | 1 |
| Total 100 |
| Research Domain | Technology and Sensors Used | Applications | Novelty | References |
|---|---|---|---|---|
| Smart home health systems | IoT, ESP8266, ESP32, ATMega microcontrollers, sensors for vital signs | Smart home health monitoring, activity recognition | Integration of IoT into home health systems, AI for activity detection, low-cost solutions | [34,35,36,37,41,42] |
| Home care and elderly assistants | IoT, AI, cameras, sensors (heart rate, SPO2, body temperature), Raspberry Pi Pico, wearable sensors, LiFi, radar, RFID | Patient health monitoring, fall detection, action classification, smart mattress for sleep monitoring, real-time movement monitoring | Non-intrusive, comprehensive health monitoring, low-cost smart mattress for heart rate and respiration, AI integration for fall detection | [29,33,38,39,40,43,44,52,53,75] |
| IoT health monitoring systems | Wearable sensors (ECG, respiration, pulse wave, bioimpedance), ZigBee, millimeter-wave radar, cloud computing, AI | Remote health monitoring, fall detection, vital sign tracking, geriatric health monitoring | Integration of IoT, AI, and cloud computing for real-time health monitoring | [62,64,65,66,67,68,69,79] |
| Remote monitoring and smart medicine | Wearable devices, AI, IoT, mobile apps, sensors (heart rate, BP, ECG), deep learning, ThingSpeak platform, cloud computing | Medication adherence, real-time health monitoring, chronic condition management, fall detection, smart reminders | Integration of medication reminders with health monitoring, real-time patient status monitoring, AI, and cloud integration | [57,58,59,71,72,73,76,78] |
| Study Focus | Technology and Sensors Used | Applications | Novelty | References |
|---|---|---|---|---|
| Designed wristbands | Custom-designed wristbands, ARM-based devices, wearable smart bracelets | Health monitoring for elderly individuals, emergency alerts, physiological parameter measurement | Focused on data collection and presentation without analysis, humanized design, integration of multiple physiological parameters | [8,63,81,82,83] |
| Design of wearables | Multimodal sensors, LTE-connected wearables, smart gloves, accelerometers, omnidirectional inertial switch, ionic conductive material | Real-time health monitoring, fall detection, personal safety, posture assessment | Integration of multiple vital sign sensors and novel materials (i-gluten) for sustainability and enhanced sensing | [62,84,85,86,87,88] |
| Clothing | Smart textiles, biomedical sensors, body area network (BAN), biosensors | Physiological signal collection, environmental protection, health monitoring | Integration of sensors into esthetic and functional garments, ThingSpeak server connectivity, elastic biosensors for accurate measurements | [71,89,90,91] |
| Commercial smartwatches | BITalino, TicWatchPro, Polar H10, James One, BodiMetrics, Everlast TR10, Empatica E4 | Vital sign monitoring, stress level tracking, remote healthcare monitoring | Infrastructure for real-time health tracking, Web3-based monitoring, comparison of consumer smartwatches, PPG sensor evaluation in weak magnetic fields | [40,42,49,92,93,94,95,96,97,98,99] |
| Platform Type | Technology Used | Primary Use Cases | Innovative Features | References |
|---|---|---|---|---|
| Mobile Apps | Android-based systems, Bluetooth, wearable technology, facial video processing | Assists elderly, continuous vital sign monitoring, TIA/stroke telemonitoring, medication reminders | Accuracy in monitoring, real-time tracking, integration with wearable devices, SMS alerts | [57,100,101,102,103,104,105,106,107,108] |
| Web Apps | Web dashboards, server applications, Web3 technology, CSS/HTML, MQTT messaging | Health data aggregation, remote monitoring, patient–healthcare provider communication | Real-time alerts, seamless integration of data sources, cost-effectiveness, sustainability in healthcare | [89,93,101,104,109,110] |
| Category | Technologies and Sensors Used | Applications | References |
|---|---|---|---|
| Intelligent homes, Section 3.1.1 | Microcontrollers (ESP8266, ESP32, ATMega), IoT sensors, AI, LiFi, RFID, millimeter-wave radar, UWB radar, wearable sensors, cloud computing, MQTT, smart cameras | Home care monitoring, patient management, fall detection, health tracking, e-health monitoring, IoT-based monitoring, remote sensing, assistive health systems | [29,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61] |
| Wearable devices, Section 3.1.2 | Smart clothing, wristbands, smartwatches, IoT sensors, ECG, PPG, LTE, inertial sensors, AI, i-gluten conductive material, body area network (BAN) | Health tracking, elderly monitoring, fall detection, emergency alerts, fitness tracking | [8,40,42,49,62,63,71,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99] |
| Web-based and mobile applications, Section 3.1.3 | Android apps, web platforms, Bluetooth, MQTT, AI, facial recognition, cloud-based dashboards, telemedicine | Remote health tracking, medication reminders, telemonitoring, real-time alerts, doctor–patient communication | [57,89,93,100,101,102,103,104,105,106,107,108,109,110] |
| Integrated healthcare systems, Section 3.1.4 | ARM-embedded platforms, AI, IoMT, fuzzy inference systems, BLE, IMUs, cloud computing, holographic visualization | Multi-parameter monitoring, real-time health alerts, gait assessment, telemedicine | [85,111,112,113] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
González-Baldovinos, D.L.; Sánchez-Fernández, L.P.; Cano-Rosas, J.L.; López-Chau, A.; Guevara-López, P. Innovations and Technological Advances in Healthcare Remote Monitoring Systems for the Elderly and Vulnerable People: A Scoping Review. Appl. Sci. 2025, 15, 3200. https://doi.org/10.3390/app15063200
González-Baldovinos DL, Sánchez-Fernández LP, Cano-Rosas JL, López-Chau A, Guevara-López P. Innovations and Technological Advances in Healthcare Remote Monitoring Systems for the Elderly and Vulnerable People: A Scoping Review. Applied Sciences. 2025; 15(6):3200. https://doi.org/10.3390/app15063200
Chicago/Turabian StyleGonzález-Baldovinos, Diana Lizet, Luis Pastor Sánchez-Fernández, Jose Luis Cano-Rosas, Asdrúbal López-Chau, and Pedro Guevara-López. 2025. "Innovations and Technological Advances in Healthcare Remote Monitoring Systems for the Elderly and Vulnerable People: A Scoping Review" Applied Sciences 15, no. 6: 3200. https://doi.org/10.3390/app15063200
APA StyleGonzález-Baldovinos, D. L., Sánchez-Fernández, L. P., Cano-Rosas, J. L., López-Chau, A., & Guevara-López, P. (2025). Innovations and Technological Advances in Healthcare Remote Monitoring Systems for the Elderly and Vulnerable People: A Scoping Review. Applied Sciences, 15(6), 3200. https://doi.org/10.3390/app15063200








