Research on the Network Structure Characteristics of Doctors and the Influencing Mechanism on Recommendation Rates in Online Health Communities: A Multi-Dimensional Perspective Based on the “Good Doctor Online” Platform
Abstract
1. Introduction
- What are the differences in the network’s structural characteristics across different disease types of physicians? How do these differences reflect the functional division of labor and organizational logic within medical specialties?
- What heterogeneous structural characteristics do physician groups of different professional titles (chief physicians/resident physicians) demonstrate within medical collaboration networks? What influences do these structural differences exert on medical service quality transmission?
- What are the key factors that influence physician recommendation rates in online health communities? Specifically, how does post-consultation evaluation function as a core element of social trust negotiation within recommendation mechanisms?
- How do network structural characteristics in digital medical ecosystems influence physician recommendation rates through social trust negotiation processes? What implications does this operational mechanism hold for platform management?
2. Related Studies
2.1. Definition and Classification of OHC
2.2. Quality Evaluation of OHC Information Services
2.3. Application of Social Network Analysis (SNA) in Online Health Communities
2.4. Influencing Factors of OHC Information Services
3. Research Design
3.1. Data Sources
3.2. Research Methods
3.2.1. Network Analysis
3.2.2. Influencing Factors Investigation
4. Results
4.1. Social Network Analysis
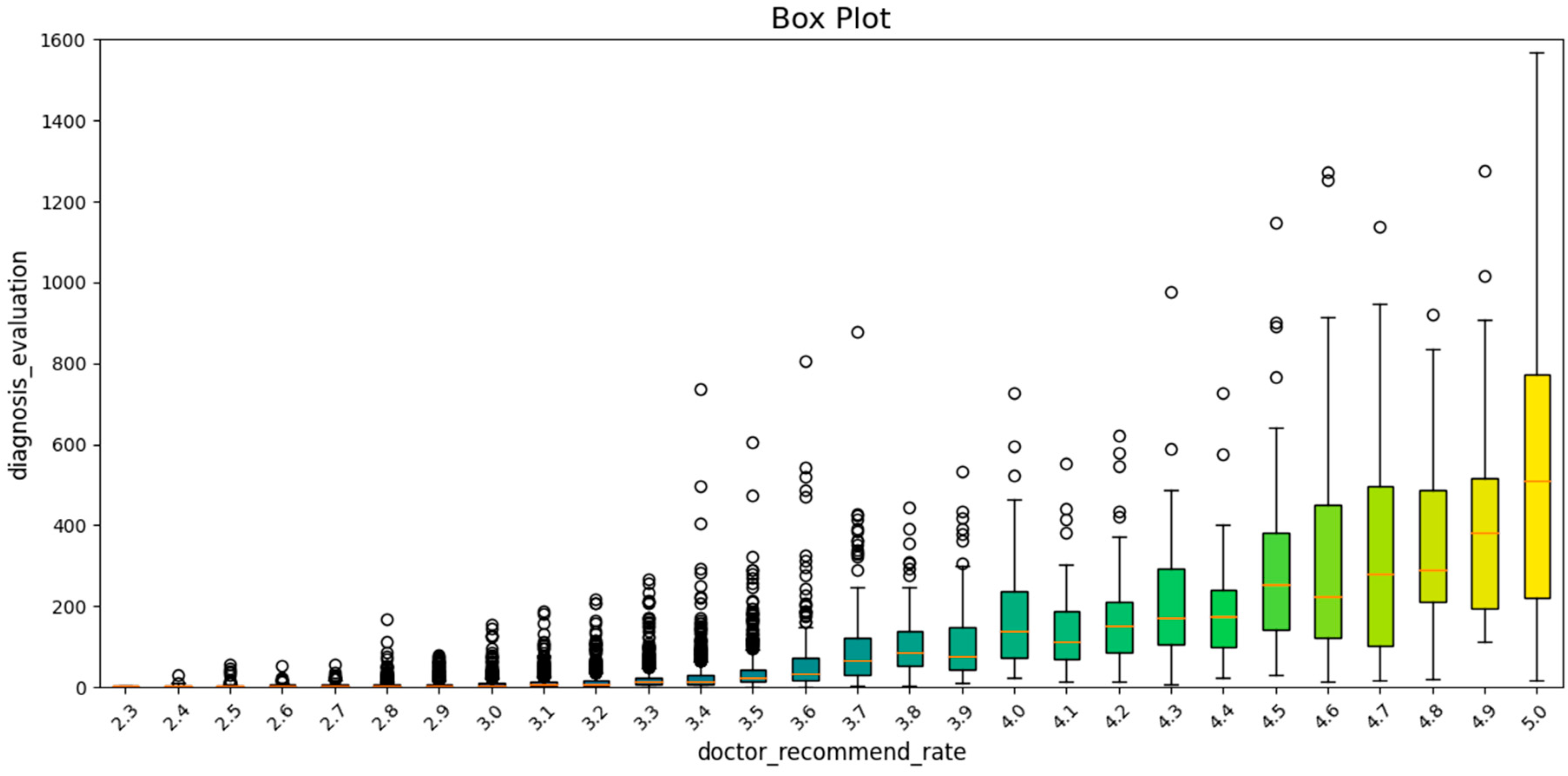
4.2. Exploration of Recommendation Rate Influencing Factors
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yang, X.; Li, J.; Wang, H. Study on the Knowledge Adoption Behavior of Chronic Disease Users in Online Health Communities. J. Inf. Syst. 2020, 2, 67–76. [Google Scholar]
- Zhai, Y.; Zhang, X.; Wang, F. User Participation Behavior in Online Health Communities: A Case Study of ‘Baidu Quit Smoking Bar’. Libr. Inf. Work 2017, 61, 75–82. [Google Scholar] [CrossRef]
- Chomutare, T.; Årsand, E.; Hartvigsen, G. Characterizing Development Patterns of Health-Care Social Networks. Netw. Model. Anal. Health Inform. Bioinform. 2013, 2, 147–157. [Google Scholar] [CrossRef][Green Version]
- Stewart, S.A.; Abidi, S.S.R. Applying Social Network Analysis to Understand the Knowledge Sharing Behaviour of Practitioners in a Clinical Online Discussion Forum. J. Med. Internet Res. 2012, 14, e170. [Google Scholar] [CrossRef]
- Ni, Z.; Wang, C.; Si, X. Analysis of the Differences between Knowledge Sharing and Fake Information Dissemination in Online Health Communities from the Perspective of Social Networks. Inf. Theory Pract. 2023, 46, 67–75. [Google Scholar] [CrossRef]
- Fineschi, D.; Acciai, S.; Napolitani, M.; Scarafuggi, G.; Messina, G.; Guarducci, G.; Nante, N. Game of Mirrors: Health Profiles in Patient and Physician Perceptions. Int. J. Environ. Res. Public Health 2022, 19, 1201. [Google Scholar] [CrossRef]
- Johnston, A.C.; Worrell, J.L.; Di Gangi, P.M.; Wasko, M. Online Health Communities: An Assessment of the Influence of Participation on Patient Empowerment Outcomes. Inf. Technol. People 2013, 26, 213–235. [Google Scholar] [CrossRef]
- Okour, M.N.S.D. The Role of Social Support and Patient Empowerment Through Online Health Communities in Enhancing Patient-Physician Relationship. Int. J. Prof. Bus. Rev. 2023, 8, e03809. [Google Scholar] [CrossRef]
- Zhang, B.; Zheng, Y.R.; Cui, H.L.; Shan, S.Y. Research on information organization optimization of online health websites in China. Libr. Sci. Res. 2022, 12, 32+25–101. [Google Scholar]
- Imlawi, J. Health Website Success: User Engagement in Health-Related Websites. Int. J. Interact. Mob. Technol. 2017, 11, 49–64. [Google Scholar] [CrossRef]
- Wang, R.Y.; Strong, D.M. Beyond Accuracy: What Data Quality Means to Data Consumers. J. Manag. Inf. Syst. 2020, 37, 45–67. [Google Scholar] [CrossRef]
- Jiang, Z.; Li, Q.; Xing, S.; Hu, M. Construction and Empirical Study of Information Service Quality Evaluation Index System for Online Health Communities. Intell. Explor. 2020, 4, 78–85. [Google Scholar]
- Sun, Y.; Zhang, Y.; Gwizdka, J.; Trace, C.B. Consumer evaluation of the quality of online health information: Systematic literature review of relevant criteria and indicators. J. Med. Internet Res. 2019, 21, e12522. [Google Scholar] [CrossRef]
- Xu, Z.; Shang, S. Research on User Experience Evaluation of Online Health Communities Based on Fuzzy Hierarchical Analysis. Int. J. Med. Inform. 2021, 42, 24–31. [Google Scholar]
- Boyer, C.; Gaudinat, A.; Baujard, V.; Geissbühler, A. Health on the Net Foundation: Assessing the quality of health web pages all over the world. Stud. Health Technol. Inform. 2007, 129 Pt 2, 1017–1021. [Google Scholar]
- Venkatasubramanian, M. Applications of Qualitative Content Analysis: Evaluating the Reliability and Quality of Health Information Websites. Qual. Res. Rep. Commun. 2021, 22, 89–96. [Google Scholar] [CrossRef]
- Sun, W.; Luo, A.; Bian, Z.; Zhao, B.; Liu, P.; Wang, K.; Liu, Y.; Xie, W.; Wang, F. Assessing the quality of online health information about breast cancer from Chinese language websites: Quality assessment survey. JMIR Cancer 2021, 7, e25783. [Google Scholar] [CrossRef]
- Zhang, Y.; Kim, Y. Consumers’ Evaluation of Web-Based Health Information Quality: Meta-analysis. J. Med. Internet Res. 2022, 24, e36463. [Google Scholar] [CrossRef]
- Xu, R.; Zhang, Q. Understanding Online Health Groups for Depression: Social Network and Linguistic Perspectives. J. Med. Internet Res. 2016, 18, e63. [Google Scholar] [CrossRef]
- Lu, Y.; Luo, S.; Liu, X. Development of Social Support Networks by Patients with Depression Through Online Health Communities: Social Network Analysis. JMIR Med. Inform. 2021, 9, e24618. [Google Scholar] [CrossRef]
- Curran, J.; Abidi, S.S.R. Evaluation of a Discussion Forum for Knowledge Sharing Among Emergency Practitioners: A Social Network Approach. Stud. Health Technol. Inform. 2006, 124, 941–946. [Google Scholar] [PubMed]
- Chuang, K.Y.; Yang, C.C. How Do e-Patients Connect Online? A Study of Social Support Roles in Health Social Networking. In Proceedings of the 6th International Conference: Social Computing, Behavioral-Cultural Modeling and Prediction, Washington, DC, USA, 2–5 April 2013; pp. 193–200. [Google Scholar] [CrossRef]
- Zhang, M.; Yang, C.C. The Differences of User Behavior Between Forum and Facebook for Smoking Cessation Intervention. Proc. Am. Soc. Inf. Sci. Technol. 2012, 49, 1–4. [Google Scholar] [CrossRef]
- Durant, K.T.; McCray, A.T.; Safran, C. Social Network Analysis of an Online Melanoma Discussion Group. Summit Transl. Bioinform. 2010, 2010, 6–10. [Google Scholar] [PubMed]
- Dias, A.; Chomutare, T.; Botsis, T. Exploring the Community Structure of a Diabetes Forum. Stud. Health Technol. Inform. 2012, 180, 833–837. [Google Scholar]
- Gong, L.; Guo, Y.; Kong, Y.; Hu, D. A study on the influencing factors of continuous use intention of online health community users based on integrated model. J. Med. Inform. 2022, 43, 23–29. [Google Scholar]
- Topaloglu, H.; Gumussoy, C.A.; Bayraktaroglu, A.E.; Calisir, F. The relative importance of usability and functionality factors for e-health web sites. Hum. Factors Ergon. Manuf. Serv. Ind. 2013, 23, 336–345. [Google Scholar] [CrossRef]
- Calvano, J.D.; Fundingsland, E.L., Jr.; Lai, D.; Silacci, S.; Raja, A.S.; He, S. Applying website rankings to digital health centers in the United States to assess public engagement: Website usability study. JMIR Hum. Factors 2021, 8, e20721. [Google Scholar] [CrossRef]
- Shim, M.; Jo, H.S. What Quality Factors Matter in Enhancing the Perceived Benefits of Online Health Information Sites? Application of the Updated DeLone and McLean Information Systems Success Model. Int. J. Med. Inform. 2020, 137, 104093. [Google Scholar] [CrossRef]
- Maloney-Krichmar, D.; Preece, J. A Multilevel Analysis of Sociability, Usability, and Community Dynamics in an Online Health Community. ACM Trans. Comput.-Hum. Interact. 2005, 12, 201–232. [Google Scholar] [CrossRef]
- Hong, T. Contributing Factors to the Use of Health-Related Websites. J. Health Commun. 2006, 11, 149–165. [Google Scholar] [CrossRef]
- Czaja, S.J.; Sharit, J.; Lee, C.C.; Nair, S.N.; Hernández, M.A.; Arana, N.; Fu, S.H. Factors influencing use of an e-health website in a community sample of older adults. J. Am. Med. Inform. Assoc. 2013, 20, 277–284. [Google Scholar] [CrossRef] [PubMed]
- Freeman, L. The Development of Social Network Analysis: A Study in the Sociology of Science; Empirical Press: New York, NY, USA, 2004; Volume 1, pp. 159–167. [Google Scholar]
- Python Software Foundation. Available online: https://www.python.org/ (accessed on 3 April 2025).
- Gephi Consortium. Available online: https://gephi.org/ (accessed on 3 April 2025).
- IBM. Available online: https://www.ibm.com/spss (accessed on 3 April 2025).
- Zhu, M.; Wang, L. The Role of Key Opinion Leaders in Knowledge Diffusion within Healthcare Networks. Health Serv. Res. 2020, 55, 13210. [Google Scholar]
- Lee, H.; Chen, T. Social Network Analysis of Junior Physicians’ Resource Acquisition. Soc. Sci. Med. 2020, 262, 113345. [Google Scholar] [CrossRef]
- Abbasi-Moghaddam, M.A.; Zarei, E.; Bagherzadeh, R.; Dargahi, H.; Farrokhi, P. Evaluation of Service Quality from Patients’ Viewpoint. BMC Health Serv. Res. 2019, 19, 170. [Google Scholar] [CrossRef]
- Chen, X.; Wang, H.; Li, X. Doctor Recommendation Under Probabilistic Linguistic Environment Considering Patient’s Risk Preference. Ann. Oper. Res. 2024, 341, 555–581. [Google Scholar] [CrossRef]
- Gruzd, A.; Haythornthwaite, C. Enabling Community Through Social Media. J. Med. Internet Res. 2013, 15, e248. [Google Scholar] [CrossRef]

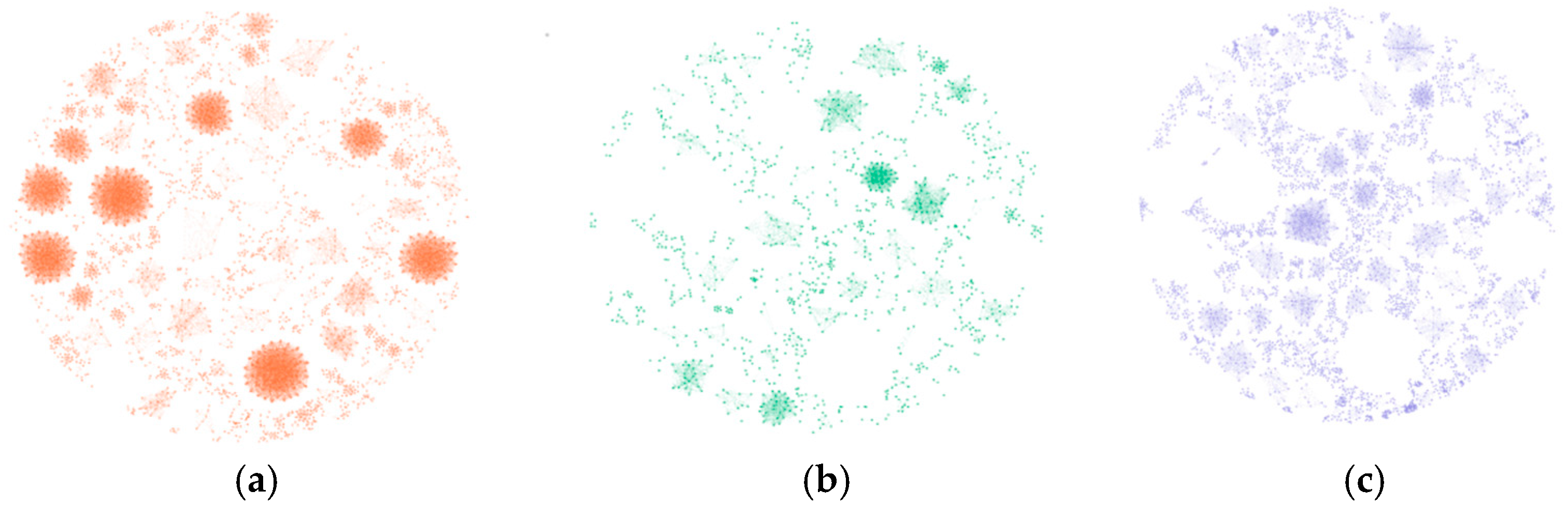


| Network Indicators | Depression | Leukemia | Diabetes |
|---|---|---|---|
| Average Degree | 17.378 | 7.929 | 7.234 |
| Graph Density | 0.007 | 0.007 | 0.002 |
| Connected Components | 720 | 371 | 1240 |
| Modularity | 0.94 | 0.936 | 0.982 |
| Network Indicators | Chief Doctor | Deputy Chief Doctor | Attending Doctor | Resident Doctor |
|---|---|---|---|---|
| Average Degree | 9.353 | 6.647 | 3.444 | 0.804 |
| Graph Density | 0.003 | 0.003 | 0.002 | 0.003 |
| Connected Components | 961 | 946 | 682 | 209 |
| Modularity | 0.982 | 0.98 | 0.971 | 0.942 |
| Doctor Recommendation Rate | Doctor Online Work Quantity | Personal Webpage Visits | Article Count | Total Post-Consultation Patient Count | Post-Consultation Evaluation | Thank-You Letter Count | Gratitude Gift Count | |
|---|---|---|---|---|---|---|---|---|
| Doctor Recommendation Rate | 1 | 0.459 | 0.369 | 0.122 | 0.526 | 0.602 | 0.554 | 0.42 |
| Doctor Online Work Quantity | 0.459 | 1 | 0.263 | 0.274 | 0.717 | 0.743 | 0.706 | 0.724 |
| Personal Webpage Visits | 0.369 | 0.263 | 1 | 0.151 | 0.273 | 0.278 | 0.259 | 0.176 |
| Article Count | 0.122 | 0.274 | 0.151 | 1 | 0.163 | 0.148 | 0.137 | 0.148 |
| Total Post-Consultation Patient Count | 0.562 | 0.717 | 0.273 | 0.163 | 1 | 0.807 | 0.743 | 0.696 |
| Post-Consultation Evaluation | 0.602 | 0.743 | 0.278 | 0.148 | 0.807 | 1 | 0.981 | 0.787 |
| Thank-You Letter Count | 0.554 | 0.706 | 0.259 | 0.137 | 0.743 | 0.981 | 1 | 0.755 |
| Gratitude Gift Count | 0.420 | 0.724 | 0.176 | 0.148 | 0.696 | 0.787 | 0.755 | 1 |
| Standard Error | |
|---|---|
| Doctor Recommendation Rate | 0.4424 |
| Doctor Online Work Quantity | 1924.798 |
| Personal Webpage Visits | 232.508 |
| Article Count | 84.311 |
| Total Post-Consultation Patient Count | 741.467 |
| Post-Consultation Evaluation | 115.195 |
| Thank-You Letter Count | 52.065 |
| Gratitude Gift Count | 169.859 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, H.; Wang, C.; Qi, H. Research on the Network Structure Characteristics of Doctors and the Influencing Mechanism on Recommendation Rates in Online Health Communities: A Multi-Dimensional Perspective Based on the “Good Doctor Online” Platform. Appl. Sci. 2025, 15, 4583. https://doi.org/10.3390/app15084583
Wang H, Wang C, Qi H. Research on the Network Structure Characteristics of Doctors and the Influencing Mechanism on Recommendation Rates in Online Health Communities: A Multi-Dimensional Perspective Based on the “Good Doctor Online” Platform. Applied Sciences. 2025; 15(8):4583. https://doi.org/10.3390/app15084583
Chicago/Turabian StyleWang, Hao, Chen Wang, and Huiying Qi. 2025. "Research on the Network Structure Characteristics of Doctors and the Influencing Mechanism on Recommendation Rates in Online Health Communities: A Multi-Dimensional Perspective Based on the “Good Doctor Online” Platform" Applied Sciences 15, no. 8: 4583. https://doi.org/10.3390/app15084583
APA StyleWang, H., Wang, C., & Qi, H. (2025). Research on the Network Structure Characteristics of Doctors and the Influencing Mechanism on Recommendation Rates in Online Health Communities: A Multi-Dimensional Perspective Based on the “Good Doctor Online” Platform. Applied Sciences, 15(8), 4583. https://doi.org/10.3390/app15084583







