Abstract
Type 1 Diabetes Mellitus (DM1) is a metabolic disease that is characterized by chronic hyperglycemia due to a lack of pancreatic insulin production. This forces patients to perform several blood glucose measurements per day—by means of capillary glucometers—in order to infer a trend and try to predict future values. In this way, a decision about the insulin dosage that has to be exogenously injected to maintain glycemia within the desirable levels is made. Unfortunately, this method usually suffers from relatively high imprecision. However, recent advances in information and communication technologies (ICT), along with novel biosensors that could provide a real-time comprehensive condition of the patient, offer a new perspective in DM1 management. In this sense, new disruptive technologies like Big Data, the Internet of Things (IoT), and Cloud Computing, as well as Machine Learning (ML) can play an important role in managing DM1. In this work, firstly, an analysis of previously published ICT-based methods for the management of diabetes continuous monitoring is carried out. In this way, an assessment of the possible lack of such proposals is presented, along with the challenges to be overcome in forthcoming smart DM1 management systems. Finally, an overview of a holistic ICT-based platform for DM1 management that try to solve the limitations of previous works, while at the same time, taking advantage of the abovementioned disruptive technologies is hereby proposed.
1. Introduction
Type 1 Diabetes Mellitus (DM1) is a disease characterized by high blood sugar levels that result from the body’s inability to produce and/or use insulin. In a healthy human, glucose homeostasis represents a closed-loop system that is able to regulate the blood glucose levels. The pancreas presents β cells that are sensitive to high glucose levels and produce insulin, a strong hormone that is able to reduce hyperglycemia.
This regulation is not possible in DM1, since it is an auto-immune disease in which the body destroys the insulin-producing cells in the pancreas. In this sense, DM1 is the more chronic form of diabetes. Patients with DM1 do not produce any insulin and must exogenously inject this hormone—or wear an insulin pump—in order to reduce their glucose levels. Moreover, patients affected by diabetes need to check their glucose level several times per day (through capillary glucometers), so that, based on these data, as well as other factors, like meals, exercise, and many others, they can decide when to inject insulin and how much is required to avoid hyperglycemia. Insulin can be delivered either by multiple daily injections or by continuous infusion, using a pump, which permeates under the skin.
In this context, new technological possibilities offer a new horizon in diabetes management. Although the first steps towards an artificial pancreas (AP) were undertaken 50 years ago [1], when the concept of a computer-supported system emulating the behavior of a pancreas by using a control algorithm was introduced, promising that technological advances achieved in recent years are supposed to bring a revolution in this field. Nowadays, an AP (which has not been completely achieved yet) is presumed to be composed of a Continuous Glucose-Monitoring (CGM) device aimed at checking the patient’s glucose levels in real time (a feature that is already available) and injecting (a feature that is not yet commercially available) insulin (and glucagon, if applicable) into his or her body, along with a control system based on a closed loop, which must decide the amount of hormone (insulin or glucagon) to be injected [2,3].
2017 was a particularly significant year regarding the AP [4]. Clinical trials were performed and their results were published, showing a good performance under real and demanding situations. Even a commercial hybrid closed-loop system is commercially available at present, Medtronic MiniMed 670G, which automatically adjusts basal insulin every five minutes based on CGM readings and is able to stop insulin up to 30 min before reaching a preset low limit. It also automatically restarts insulin when patient’s levels recover [5]. Nowadays, in this field, a total of 18 different closed-loop AP systems were identified as being in clinical phase development [6].
On the other hand, beyond the AP and CGM devices, others in the field of biometrics make it possible to maintain 24-h monitoring of the patient, thus recording important information about his or her health that could be interesting and properly used in a DM1 management context. Variables, like temperature, exercise, heart rate, and perspiration, among others, can be monitored continuously. However, the inclusion of new monitored features simultaneously generates a large amount of information and creates a new problem: the need to handle it in an appropriate information and communication technologies (ICT) framework that is designed to collect and gather data, process it, and obtain useful knowledge. In this sense, well-known improvements in computer science are able to tackle these challenges, and, at this point, technologies like smartphones and ideas, like the Internet of Things (IoT), Big Data, and Cloud Computing arise, which are powerful options for dealing with a huge quantity of information. In this sense, recent developments have introduced both the idea of a Body Area Network (BAN)—along with some other sensors—to gather relevant information and the use of platforms to display data and ease the diabetes management [7]. This way, the most relevant approaches in this field have been properly summarized by Lanzola et al. [8]. Nonetheless, although they are really valuable contributions, the consideration of some ICT possibilities that are available at present (such as smartbands, smartwatches and so on), is not taken into account, and going further, a comprehensive focusing of all the previous contributions, thus leading to a lack of features regarding a complete platform for DM1 management. Furthermore, some recent approaches to model and predict blood glucose concentration, as well as insulin boluses (with decision support), which have been recently and successfully developed [9,10,11,12] could be considered and included into a more holistic perspective.
Therefore, for the stated purpose, there is a need for a platform that provides a framework in which the mentioned possibilities in diabetes management are properly exploited to the highest level, allowing for a complete, comprehensive, and holistic management, developed in real time. Therefore, in this work, an analysis of existing ICT-based methods for the management of diseases which need continuous monitoring (with an emphasis on DM1) is carried out. Then, an evaluation of the possible lack of such proposals is presented, along with the challenges that should be overcome in forthcoming smart DM1 management systems. Finally, a new ICT-based platform for DM1 management, which takes advantage of recent computer science technologies is proposed.
2. ICT-Based Approaches for the Management of Diseases Which Need Permanent Monitoring (With an Emphasis on DM1)
2.1. Telemedicine
In the scientific literature, some approaches that ease the management of some illnesses by taking advantage of the possibilities of ICT can be found, especially those that need permanent monitoring, as is the case in DM1.
A body area network (BAN) is a wireless network of wearable computing devices that are widely used in remote monitoring in telemedicine. A BAN represents all of the applications and communications on, in and near the body, so it is a necessary approach to be taken into account in telemedicine. One of the most attractive applications to use BANs is the monitoring of physiological signals from patients in the medical environment. On the other hand, a wireless body-area network (WBAN) is a special purpose wireless-sensor network that incorporates different networks and wireless devices to enable remote monitoring for various environments. The idea of a BAN is introduced in [13], focusing on epilepsy sufferers. Via a 24-h monitoring method, the system aims to notify the person of the possibility of an epileptic attack. In this way, such paper could suggest, in a DM1 context, the need to predict glucose evolution and alert not only the patient but also health professionals via the Internet or mobile phone in case of emergency. However, this proposal could be completed with a proper information-exchange platform, as also occurs in [14].
When using a BAN, we need a device that is able to play the role of a Body Gateway and a Network Hub. This device is easily identified with a smartphone. The possibilities of this device in diabetes management have already been pointed out initially in [15]. In this work, some data on food and insulin—along with location and activity—are registered in the phone so that glucose patterns can be identified and advice about insulin doses can be offered by the smartphone. However, nowadays, technology makes it easy to wear more precise biometric sensors to successfully connect all of them and to obtain a good comprehension. However, a smartphone can help not only being a simple gateway but also it can further be considered a tool to manage information. A review of how new applications designed for smartphones can help in diabetes management is presented in [16]. In this work, we can see that so far, applications are limited and focus on some specific part of the management (tracking physical activity, glycemia control, etc.), but there is no complete perspective of the problem.
On the other hand, currently, it is not possible to think about an approach to an artificial pancreas without considering a CGM device. This mechanism has led to a revolution in diabetes care [17], since it can provide the magnitude, tendency, frequency, and duration of the fluctuations of the glucose levels in diabetic patients. When compared with conventional glucose monitoring (fingerstick, capillary blood glucose monitoring), which can provide between three and ten measures of glucose per day, CGM can deliver up to one measure per minute (1440 data per day). Therefore, this is a sample frequency which is sufficient to be the input of a control system, although Kovatchev et al. [18] indicate that CGM still bears some limitations, such as transient loss of sensitivity and random noise. The novelties in this area are continuously arising. In 2014 the release of the flash glucose monitoring system Freestyle Libre, Abbott Laboratories, involved somehow a revolution due to its accuracy and affordability [19]. The possibilities of these devices, with regard to connectivity, are still growing.
Regarding the problem of the management of information, a promising work related to diabetes management is reported in [20], where a healthcare platform for type 2 diabetes is presented, also using smartphones. In this proposal, different information is collected, such as physical activity, heart rate, or amount of food. It is able to show activity goals, activity states, and dietary records. Nonetheless, the proposed system uses uncomfortable sensors, and some important features are not measured, like glycemia. Furthermore, it is not able to deal with risky situations. In fact, in diabetes management, this is an important issue, mainly due to the risk that is involved in a hypoglycemia. In [21], an alarm-based mobile diabetes management system (ADMAN) is proposed. By using remote monitoring, it is aimed at improving diabetes control in elderly patients. Although it includes an emergency system, most of the features are not monitored and there is no prediction of future glycemia levels. Other good examples on data management using smartphones are iBGSTAR®, manufactured by Sanofi (Paris, France), in combination with the Diabetes Manager app, also from Sanofi, or the G5 Mobile CGM System by Dexcom Inc. (San Diego, CA, USA).
The IoT is proposed as a good environment for diabetes management in [22]. Smartphones are proposed for remote collection and monitoring of data, with feedback for the patient and medical caregivers. Although such work is a complete proposal, some of the features are not monitored, and, what is more, CGM is not included. In another vein, the proposed model tries to modify, through advice, the patient’s insulin dosage, but it should be noted that, without 24-h monitoring, this could not be carried out 100% successfully.
Advancements in cloud computing are proposed in [23] for diabetes control. In this case, the cloud provides an easy way to exchange information, but unfortunately full monitoring and management of emergency situations is missing.
On the other hand, it should be mentioned another approach, called COMMODITY12 [7], which is presented as a personal-health system to assist diabetic patients. This proposition consists of wearable and portable devices that acquire vital body signs, which are interpreted by algorithms based on expert knowledge. Active feedback goes directly to the patient or health professionals. Although it is an interesting proposal that includes physical activity and heart rate, it could be completed with other features from biosensors. Expert knowledge is used to interpret data, but the potential of other machine learning methods may be bigger; for instance, they may be able to predict glycemia or to make autonomous decisions. These tasks are not expected in this system, not even to avoid hypoglycemia. Lastly, the lack of inclusion of CGM in the monitoring, which should be an essential part, is an omission that needs to be rectified. A similar weakness can be found in [24]. Although the development of a BAN is complete, including others features that are usually non-considered (like body temperature, for example) and there is an online display to offer information, there should be a generation of knowledge.
Finally, it is necessary to deal with the acceptance level of telemedicine. A continuous monitoring, recording personal data, and a complete characterization of the patient could be considered as an interference in private life. This could lead to an attitude of rejection from the user. These issues are compiled in [25]. In this work, it is explained that variables, like age, gender, and previous experiences with telemedicine can modulate its level of acceptance.
So, after this review, we can conclude that, in order to develop a complete DM1 management system, it is necessary for a BAN to collect data, which should include glycemia and insulin, but also other kind of relevant features, like heart rate, physical activity, or slept hours. Moreover, a smartphone is a cornerstone to play the role of a Body Gateway, and also could provide enhanced information thanks to some software applications. Finally, IoT and Cloud Computing will allow for remote management, and the entire system must provide auto-adjustment, decision support, and advice to the patient, when considering machine learning algorithms or deep learning procedures.
As previously mentioned, a complete review of these systems has been presented recently in [8], offering an interesting overview of the current scenario and the previous attempts. Nonetheless, a complete approach for diabetes management that includes a complete characterization of the patient’s state as well as knowledge discovery—in an ICT environment—is missed.
2.2. Methods of Connection
Taking advantage of new continuous biometric sensors will create a technological structure in the patient that will generate a huge amount of data. Initially, it has to be ensured that the systems have enough compatibility between clinical devices, platform management, and computerized records in medical institutions in order to promote the sharing of data. This interoperability includes biosensors, which have to be ready to send collected data in an understandable way. In this sense, an accepted criterion is Health Level 7 (HL7) [26], which is the most important standard for the transfer of clinical and administrative data between software applications used by various healthcare providers. It defines a method of moving clinical data between independent medical applications in near real time.
Initially, some approaches like Mobile Access to Health Information (MAHI) [27] introduced interaction between diabetic patients and medical staff through a phone connected by Bluetooth to a glucometer. Unfortunately, asynchronous communications meant that it was impossible to generate advice and warnings in real time.
Managing data is a distinctive issue in Wireless Sensor Networks, where the main feature is the mobility of the source of the information [28]. Low-power body area networks can be a solution, because of their low power consumption and their mobility features. Today, these wireless communications can be hosted on smartphones, namely Bluetooth Low Energy (BLE), as well as Near Field Communication (NFC) or WiFi. An example can be health monitoring of patients in their bedrooms [29].
As described above, several types of new sensors have burst onto the technological landscape, and this means there is a broad range of different communications requirements in the IoT environment. Therefore, the chosen method of transmitting data must allow for high continuous data transmission, low consumption, high payload size, and sufficient bandwidth. To achieve this, some approaches have been followed previously. The problem of energy saving in a heath monitoring system with smartphones is studied in [30]. Taking advantage of Zigbee and Bluetooth communications, low wastage of energy is achieved. However, such work is not focused on any disease in particular, and the study of forecasted situations is omitted. ZigBee and Bluetooth have been implemented successfully in low-power wireless body area networks with discrete sensors, such as blood pressure monitors and weighing scales [31]. Others with greater complexity like pulse oximeters or electrocardiograms have been simplified by reducing the sample frequency [32]. Recently, NFC has been proven as a proper choice to monitor glycemia in the successful device Abbot Freestyle Libre, a flash blood glucose monitoring system with a popularity constantly raising in the past two years [19].
To provide inter-operability between devices, Continua Alliance (C.A.) has defined proper communications protocols, like the Bluetooth Health Device Profile (HDP), which ensures a reliable and secure way to transmit information. This ecosystem uses IEEE 1073 standards to define their protocols and create compatibility [33]. Although these standards have also been described by C.A. for ZigBee, some medical sensors are not still developed, such as electrocardiograms (ECG), due to their complexity. Notwithstanding, important researches have successfully taken place by using a 6LoWPAN approach [34] as well as NFC [35]. In any case, these three methods (Bluetooth, ZigBee, NFC) provide a convenient IoT environment, which will be described later.
2.3. Communications Environment
In order to connect the IoT devices to the cloud for the processing of data, it is essential to provide a communications infrastructure with channels for transmitting a large amount of data. In this way, nowadays, the connection possibilities have been expanded and it is possible to find a wide range of ways to transmit information. Providing devices with a Wi-Fi transmitter can open new perspectives that will allow an increase in connectivity between medical equipment. However, out of the range of a Wi-Fi net, which can be available in a patient’s home or, for instance, in a hospital environment, it will be necessary to rely on a smartphone 4G connection to launch data to the cloud. In any case, it is possible to provide self and independent connections to every device through its own SIM cards.
The communication between the devices can also be based on Bluetooth, which, in the form of BLE, is a promising way to gather information. This is the communication technology proposed in the architecture presented in this paper. BLE has been designed taking into account the requirements of the IoT, allowing for the transmission of data without the need to establish a connection, so that the pairing and transfer are faster (3 ms). Therefore, in a discrete transmission, sensors can sleep and wake up periodically to transmit, which involves a saving of energy. BLE is able to develop several functions, from the gathering of data to remote management.
Other types of connections are also interesting alternatives. ZigBee is an IEEE 802.15.4—based specification for a suite of high-level communication protocols that are used to create personal area networks with small, low-power digital radios, such as for home automation, medical device data collection, and other low-power low-bandwidth needs that are designed for small-scale projects that need wireless connection. It is intended to be simpler and less expensive than other wireless personal area networks (WPANs), and it is able to connect more than 65,000 nodes with a lower energy consumption because the nodes can go sleep when they are not in use. However, in our case, that number of nodes is not necessary and the sensors cannot be deactivated because monitoring is carried out 24 h per day.
On the other hand, NFC is a set of communication protocols that enable two electronic devices to establish communication by bringing them close to each other. By now, this technology is in use in the Abbott Freestyle Libre CGM device. Another possibility can come from ANT+, which is a wireless technology that encourages interoperability and open access to data between different manufacturers of smartphones, diagnostics, power meters, heart rate monitors, remote control systems, and so on.
In view of the above, it can be noticed that different problems regarding the interconnection between all of the devices involved in a smart diabetes monitoring system could arise due to a lack of communication compatibility. Such fact has been properly analyzed in [14]. Furthermore, it should be noted that the proprietary software/protocols and the companies policies could also represent some barriers in the creation of an integrated system In this sense, it is fare to mention the efforts of the Nightscout Project [36], an open source, “do-it-yourself” project that allows for real time access to a CGM data via personal website, smartwatch viewers, or apps and widgets available for smartphones. It was developed by parents of children with DM1 and has continued being developed, maintained, and supported by volunteers.
3. Challenges to be Overcome in an ICT—Based Diabetes Management System
After a complete review of the scientific literature, it is possible to identify some characteristics to be improved in order to draft a holistic solution for management of DM1 by means of ICT technologies.
Firstly, the potential of CGM as a masterpiece in diabetes control and management is still unfolding. Unfortunately, this device has not been developed enough until recent years. Even today, the CGM devices that are available on the market present some problems, such as lack of accuracy, decalibration, and sometimes a short usable period. Moreover, complaints are frequently made about the lag time between the data provided by the CGM and the real glucose level in the bloodstream of the patient. This is due to the fact that the CGM is not measuring directly from the blood; the value that the CGM device offers is an estimate based on the interstitial fluid glucose that exists under the skin, whose magnitude is delayed by some minutes with respect to the actual value that are present in the bloodstream. This fact can be perceived as a disadvantage. However, recent research has found that this lag time is not more than 5–10 min [37]. Moreover, mathematical methods can suitably compensate for the lack of accuracy due to this delay. In fact, some of the tests deployed by Basu [38] confirm a delay of just six minutes. Luckily, novel technologies in this area make more reliable, affordable, and user-friendly devices possible. This will necessarily lead to an increasing number of studies that include CGM in innovative diabetes management analysis.
In another vein, it is remarkable that previous works suffer from the absence of global monitoring of the patient. Moreover, apart from the obvious features that have an impact on diabetes control (glycemia itself, insulin, meals), studies have proven that other variables can influence glycemia trends significantly. For example, physical activity is widely assumed to be an influencing variable [39], and its monitoring is starting to be essential in diabetes management, usually being recorded with accelerometers. Heart-rate is also an emerging feature that is beginning to be considered as a required variable for a realistic diabetes management system. However, the potential of this component is often undervalued and is usually related only to hypoglycemia [40]. Other variables, such as exhaled breath [41] or polarimetry to monitor changes in the aqueous humor of the eye [42], have been studied, but such research is only at an early stage. On the other hand, other variables whose consideration makes intuitive sense are studied, at most, in a controlled environment under laboratory conditions of temperature, perspiration, and so on, and in isolation. Others, like the influence of schedule or weekday, are well-known [43], but have not been studied in the context discussed in this work. Therefore, to the best of the authors’ knowledge, there is not a global study in which all of them are monitored at the same time.
In addition, the way in which these features are treated lacks an expanded vision. Some variables, like insulin, could be treated in different ways, for instance, from an “on board” perspective, both basal insulin and remaining fast-insulin, which can act with low (but noticeable) intensity for several hours, are taken into account. Although this concept has been introduced for insulin, it could be extended similarly to other features. This possibility has not been studied yet.
Going further, it has not been possible for the authors of this paper to find a work that compares and ranks the importance of all of the features that have an impact on diabetes control and offers a definitive set of variables that are to be taken into account.
The potential of new improvements in ICT has still not been exploited to its full extent. To begin with, a uniform way to deal with information is needed, and in this sense, approaches like the mentioned HL7 have established a path to follow. In any case, the diversity of communication channels, including WiFi, ZigBee, 6LowPAN, and BLE, offers several options that need to be studied and specified.
Smartphones, at this moment, present a level of adaptability that is difficult to reach for any other device, due to their versatility, growing power, connectivity, and mobility options. They allow for us to make the software responsible for modeling the dynamics of the system, performing glucose prediction, optimizing the solution and controlling the process, and also managing information between CGM devices and an insulin pump, thanks to the possibilities of their connectivity [44]. Other features are also interesting, like forward emergency calls in case of risk to the patient providing the location, via GPS [45], or actualize its software when required. However, there are some doubts about the approval of smartphones as medical devices (class III, high risk). The controller application installed in the phone has to be reliable enough, avoiding opposition with other applications running in the device. Other circumstances, such as an eventual discharge of battery or a loss of connectivity, must be prevented. These pros and cons are properly discussed in [46].
Groundbreaking advances in electronics have introduced miniaturization and more powerful innovations in biometrics, the field in which measurable biological characteristics are studied. Nowadays, it is possible to measure certain variables, most of them vital signs, in a continuous mode, such as heart rate, exercise, and others. All of these measurements take part in the complex blood glucose balance and must be taken into account. Some years ago, it was difficult to obtain a compilation of data for a full day, but nowadays, different devices like smartbands, smartwatches, and other fitness and medical wearables make this objective easy, offering a lot of useful information [47]. These disruptive innovations have potential in the field of healthcare and have been studied recently. Nonetheless, restrictions due to size, battery length, and the fact that these devices are sometimes conceived for other use than that by healthcare professionals casts some doubts about their accuracy [48]. In such work, their usefulness in DM1 management is one of the ideas, which is discussed.
Modeling techniques based on artificial intelligence methods open the possibility of predicting glycaemia and thus anticipating actuation and trying to follow the different steps of the so-called Kowalski path [49], which describes the stages that are to be followed in order to obtain an artificial pancreas. Unfortunately, such methods have not been studied under the preceding considerations. In this sense, the fields of work that have been opened are immense and promising. Implementing a predictive model in order to forecast the evolution of the patient is something highly desirable. It could anticipate risky situations or even provide a decision support. Unluckily, the development and validation of models using Machine Learning techniques requires the collection of clinical data, which should be preferably carried out at different centers to ensure that the models are well-calibrated to different populations of patients. Going further, the model needs to be auto-adaptable to changes in the health and routine of the patient, avoiding wrong predictions, and, consequently, undesirable situations. Anyway, an initial stage of development of an ICT-based platform would help in the data collection and the testing stage, even allowing a test environment where patients would be under observation, minimizing the risks.
Finally, after reviewing the existing telemedicine platforms proposals, a scheme able to deal with novel ICT advances, while at the same time, exploiting all of their possibilities is lacking. For instance, some of the existing platforms connect patients and medical staff, but do not offer an optimized solution, do not take into account a suboptimal features set, or do not consider the ability to manage emergency situations.
It is time to aim for a complete management system and, with the aim of synthesizing the previous considerations; it is possible to summarize the above in terms of the following challenges:
- Full sensor integration. Technological advances have introduced new sensors, some of them specifically designed for diabetes care and others conceived for health information generally. These devices use different means of transmitting information. Therefore, it is necessary to create a platform that is able to deal with all of them successfully.
- Novel ways to deal with information, generating new variables. The need to include the “on board” concept in other features has been studied. Moreover, it is necessary to generate, in a consistent way, a definitive features set that differentiates the importance and relevance of the different variables.
- Pattern identification/prediction of glycemia. Being able to identify patterns enables us to make predictions. In this sense, glycemia prediction is the most interesting ability that is mentioned in this work. A reliable forecast allows for the anticipation of risky situations, such as hypoglycemia or maintained hyperglycemia. In this sense, the application of Machine Learning techniques is continually growing. Artificial Neural Networks offer an adaptive and flexible way to predict glycemia or give some advice about the insulin dosage [12].
- Optimized solutions. With the previous step solved, it is possible to offer a suggestion about insulin dosage or health tips. Global diabetes management will advise about insulin injections (with the proper dosage), which will always require the user’s approval, thus avoiding the misfortune of wrong decisions. Going further, the platform needs to be able to identify suboptimal situations, for instance, a sedentary lifestyle or lack of rest. Using a cloud computing resource, the complexity of the computerized models and the optimization process can be overcome without limitations.
- Management of a big amount of data. CGM usually provides data with a periodicity that ranges from 1 to 5 min. Other sensors previously mentioned, for instance, a heart-rate monitor, should also capture data in the range of minutes. This leads to the generation of a huge amount of data that have been compiled at short intervals. Thus, it is a good decision to introduce Big Data analysis [50,51]. This is a concept that applies to data sets that are so large or complex that traditional data-processing applications become useless. Some challenges in this field include analysis, capture, search, sharing, storage, transfer, visualization, querying, updating, and information privacy. The term “Big Data” often refers simply to the use of predictive analytics or certain other advanced methods in order to extract value from the data. It is easy to find examples of the use of this resource in health care to add useful knowledge to the obtained data [52].
- Emergency control. Under certain circumstances, the diabetes platform needs to take control of the situation. The main dangerous situation is strong hypoglycemia, which can lead to a loss of consciousness, or, in extreme cases, death. To mitigate the consequences of hypoglycemia, it is necessary, firstly, to stop the infusion pump in the case of a diabetic person using the device, for example, and secondly, to warn emergency services and medical staff about the status of the patient. Moreover, the systems will provide a historical record of the last hours, including insulin dosages, meals, and physical activity.
- Easy inter-connection between patients, caregivers, and medical workers. In a world that is characterized by information flows, it is mandatory to address valuable knowledge in many directions, contacting all of the subjects involved in the diabetes management.
Multiple access points have to be available to check data and processes and to change settings, which can be done not only via the patient’s smartphone, but also remotely via the Internet or another smartphone (which could be useful for monitoring children or aged/impaired patients).
- User-oriented environment. In a health care context, the focus must always be on the user. A proper interface, from a cross-platform perspective, is essential to enable patients to take advantage of this work’s concept. Furthermore, a friendly way to provide information is necessary when considering a population sector with special requirements, such as people with disabilities, the elderly, or children. Customizable options will result in a good user experience.
- Privacy, security, integrity. These usual concepts in ICT frameworks are also critical in the proposal of this work, and in fact, personal data are being processed. Therefore, control mechanisms need to be provided in order to assure a proper management of such sensitive information [53].
Once more, it is necessary to remark that, although some previous proposals offer some of these points, to the best of the authors’ knowledge, there is not one that is complete with all of them.
4. Towards a Complete Solution by Means of an ICT Structure
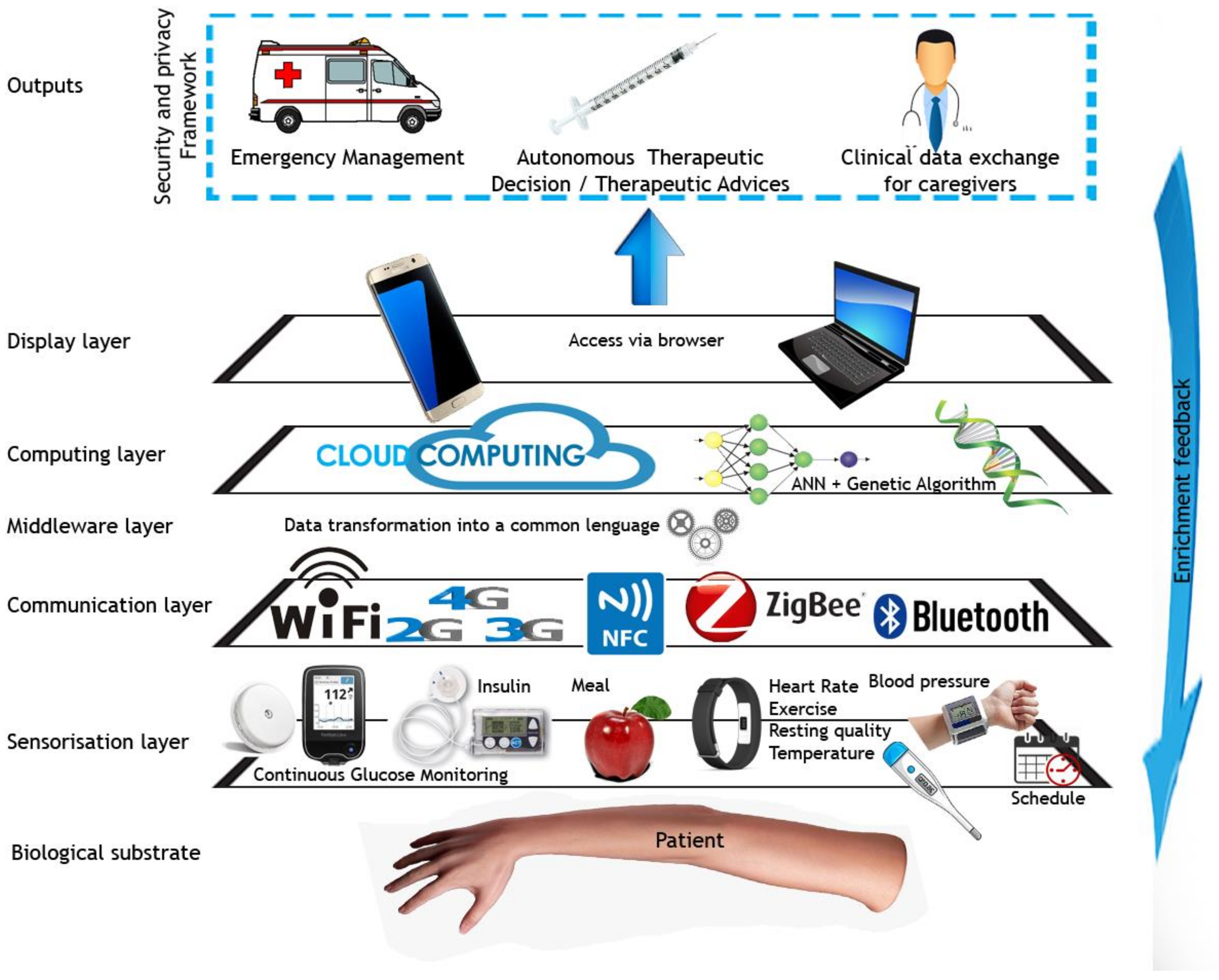
In this section, the structure of an IoT platform that is aimed at managing diabetes, modeled in layers where different technological issues are arranged, is presented as a summary of the present work. This structure can also be found in several areas, such as energy savings in buildings or smart services in cities [54], but has not been employed in a diabetes management system up to now. Therefore, as shown in Figure 1, the configuration of an integral diabetes management platform should be built as follows:
Figure 1.
Proposed layered structure for an artificial pancreas.
- Biological substrate. This is the layer where the patient is located. His or her physical changes, reflected in skin, blood, movement, and so on, will be disaggregated as variables to be measured. This layer is where the inception of the data occurs, where it is generated, and, finally, where the system’s outputs will actuate (via therapeutic decisions).
- Sensorization layer. Input data are acquired from a plethora of sensors, all of them connected to an IoT framework. Sensors can be configured and controlled remotely through the Internet, enabling a variety of monitoring applications and creating a technological structure.
- Communication layer. This tier allows for data permeation until the next stage. All of the sensors must support several communication channels in order to connect easily. Avoiding direct input/output (I/O) through regular wiring, Wi-Fi, 4G, ZigBee (or 6LowPAN), and Bluetooth connections need to be available to support direct access to sensors, mainly via another smart device (smartphone, tablet) used as a gateway, following an IoT approach. All of the elements are connected to each other by using a little Local Area Network (LAN), and, likewise, to a smartphone (or the cloud).
- Middleware layer. Given the heterogeneity of data sources and the necessity of a seamless integration of devices and networks covered by the sensors and communication layer of our architecture, a middleware mediator is needed to deal with this task. Therefore, the transformation of the collected data from the different data sources into a common language representation is performed in the middleware layer. As mentioned before, HL7 is a proper candidate to deal with this task.
The ontology implemented to represent the knowledge of the bloodstream glucose level clearly follows a user-centric approach, which takes into account all of the information characterizing the situations, the devices and their status, and the patient himself of herself.
- Computing and management layer. In this layer, data collected are handled in order to carry out a data analysis, obtain a glucose prediction, and chose an optimal therapeutic solution. Here, is where a data-processing center and modeling core are placed. Pervasive computing has to be done on two levels: one local, in the smartphone, and another in the cloud. In this way, it is possible to avoid the risk of lack of connection to the Internet or battery failure. Data harvested are sent, via LAN, to a smartphone, or maybe, in some circumstances (e.g., the absence of a smartphone), directly from the sensors to the cloud, if it is provided. Therefore, ubiquitous computing allows for a powerful and safe way to address the problem.
- Display layer (interface). Access to the system will be via browser. Thus, the parameters can be adjusted either by a smartphone or by a computer, local, or external, which is close to the patient or remote for healthcare staff. Data collected are also accessible, as well as statistics and the general status of the glycemia control system. It should be noted that the previous layer must have reached a blood glucose (BG) prediction and an optimized solution of insulin input, and this can be shown to the user either for information only or to await confirmation or variation.
- Outputs. With the goal of integral management, the platform, thanks to all of the data collected and available resources, needs to be ready to cover the following exposed requirements.
And as a result, it is possible to obtain:
- Concerning therapeutic decisions: As a consequence of data processing, artificial intelligence modeling, and optimization processes, the platform has to be ready to offer a BG prediction as continuous information for the patient or remote caregivers in order to forecast an undesirable situation, adopt autonomous therapeutic decisions in a safe way in order to avoid hyperglycemia or to maintain euglycemia (normal levels of glycemia) in well-known situations, and give therapeutic advice, that is, create valuable knowledge offering guidelines that could be helpful to both the patient and the clinical staff.
- Emergency management: A comprehensive management system must be ready to deal with a risky situation. For instance, when hypoglycemia occurs, insulin delivery should be stopped and the patient’s awareness should be checked, for example, by asking him or her and awaiting a reaction. In case of loss of consciousness, making an automatic call to the emergency services with a description of the situation and a GPS location would be an expected behavior of the platform.
- Clinical data exchange for caregivers: Health-care researchers can benefit from an easy and real-time exchange of data that have been previously filtered and processed, and the platform should then be ready to incorporate professionals’ feedback. This remote data exchange will also enable parents (in the case of diabetic children) and elderly people’s caregivers to control from afar and also to use automatic notifications in the case of abnormal situations.
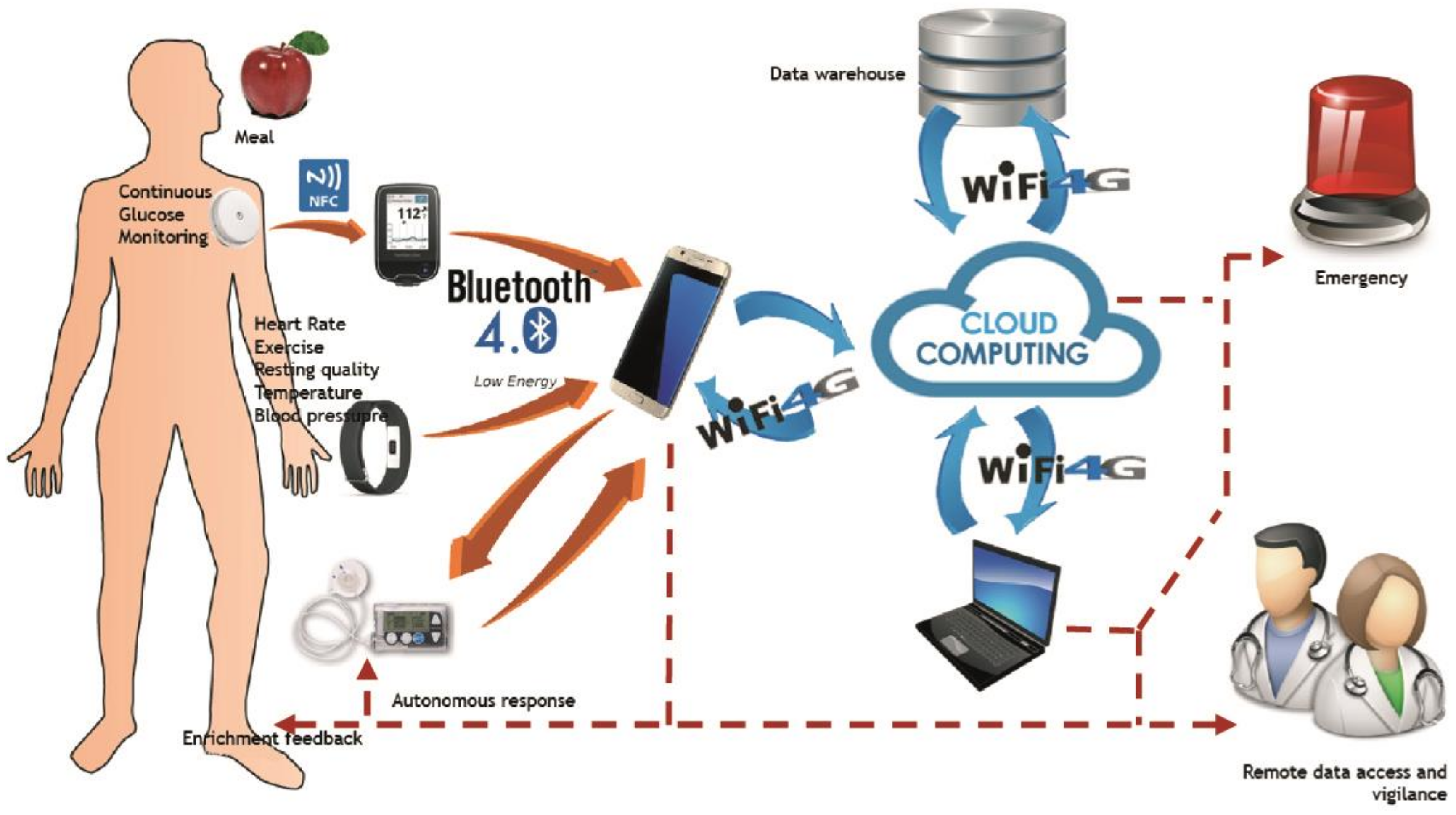
This structure needs to be networked properly. In this sense, as can be seen in Figure 2, the system architecture would be composed of a local gateway (smartphone) that is connected to the Internet via 4G or through a domestic WiFi. The smartphone will be exclusive for each patient. It is on the Internet that it is possible to place the data warehouse and a processing center, as well as the modeling core. Moreover, by using the Internet, the management of the system via a Web browser will be possible.
Figure 2.
Diagram of the flows of data.
The smartphone is responsible for collecting data from the sensors. It also has to be reliable to establish and manage connections with devices that are attached to the patient. By using several methods of communication (BLE is a good candidate, but 6LoWPAN, NFC, and so on can also be used), the exchange of data becomes possible so that a plethora of biometric meters can be interlinked.
BLE has been developed to have a very low consumption of energy, even lower than 6LoWPAN. This is possible due to a simplified protocol that facilitates the scanning and a required standby time before the transmission of data, thanks to the reduction from 16 channels to only 3 for advertising [55]. In addition, connection is faster and takes place automatically when scanning, so connection and transmission are available in the mentioned 3 ms. The BLE peak current is under 17.5 mA, so coin cell batteries are adequate as a power supply, which is a very important feature in the interest of miniaturization.
Sensors which lie on a patient’s skin could connect by using Bluetooth, NFC, or other means of communication.
5. Conclusions
Our world is, in a very remarkable way, changing continuously thanks to technological advances. All of these improvements have become revolutionary in a lot of areas, making life easier in many ways. In the struggle to obtain a full, complete, and definitive way to control diabetes, some boosts have been obtained thanks to the development of new devices like CGM devices or insulin pumps.
Notwithstanding, science has continued its advance and new systems can be found now. This work has reviewed diabetes management architectures using modern perspectives in the area of ICT, innovating throughout novel electronics and communications.
Some ICT platforms have been checked, showing the absence and incompleteness of existing works. In this sense, IoT and Big Data analysis have been explained in this context, showing that these approaches are the best candidates to improve diabetes management, that is, the best solution to deal with such a large amount of data, and, going further, Cloud Computing plays a promising role. On the other hand, pervasive computing will allow for the manipulation and calculation as well as helping in medical decisions. In this sense, an ICT-based platform for DM1 management that takes advantage of the abovementioned disruptive technologies has been proposed.
Moreover, in order to gather information, BLE has been shown to be the best solution, but other possibilities have also been pointed out, such as WiFi, 4G, ZigBee, and others, which have been introduced as ways to link information.
To conclude, we have been shown that it is necessary to face new challenges that come from today’s technological reality. With this perspective, it is possible to sketch new platforms whose schemas have been proposed, offering some guidelines that should be followed.
Acknowledgments
This work has been sponsored by the Spanish Ministry of Economy and Competitiveness through the PERSEIDES (ref. TIN2017-86885-R) and CHIST-ERA (ref. PCIN-2016-010) projects.
Author Contributions
Ignacio Rodríguez-Rodríguez and José-Víctor Rodríguez drafted the manuscript and designed the figures, Miguel Ángel Zamora-Izquierdo were involved in planning and supervised the work.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Albisser, A.M.; Leibel, B.S.; Ewart, T.G.; Davidovac, Z.; Botz, C.K.; Zingg, W. An artificial endocrine pancreas. Diabetes 1974, 23, 389–396. [Google Scholar] [CrossRef] [PubMed]
- Peyser, T.; Dassau, E.; Breton, M.; Skyler, J.S. The artificial pancreas: Current status and future prospects in the management of diabetes. Ann. N. Y. Acad. Sci. 2014, 1311, 102–123. [Google Scholar] [CrossRef] [PubMed]
- Cobelli, C.; Renard, E.; Kovatchev, B. Artificial pancreas: Past, present, future. Diabetes 2011, 60, 2672–2682. [Google Scholar] [CrossRef] [PubMed]
- Kovatchev, B. The artificial pancreas in 2017: The year of transition from research to clinical practice. Nat. Rev. Endocrinol. 2018, 14, 74–76. [Google Scholar] [CrossRef] [PubMed]
- Bergenstal, R.M.; Garg, S.; Weinzimer, S.A.; Buckingham, B.A.; Bode, B.W.; Tamborlane, W.V.; Kaufman, F.R. Safety of a hybrid closed-loop insulin delivery system in patients with type 1 diabetes. JAMA 2016, 316, 1407–1408. [Google Scholar] [CrossRef] [PubMed]
- Trevitt, S.; Simpson, S.; Wood, A. Artificial pancreas device systems for the closed-loop control of type 1 diabetes: What systems are in development? J. Diabetes Sci. Technol. 2016, 10, 714–723. [Google Scholar] [CrossRef] [PubMed]
- Kafalı, Ö.; Bromuri, S.; Sindlar, M.; van der Weide, T.; Aguilar Pelaez, E.; Schaechtle, U.; Alves, B.; Zufferey, D.; Rodriguez-Villegas, E.; Schumacher, M.; et al. COMMODITY12: A smart e-health environment for diabetes management. J. Ambient Intell. Smart Environ. 2013, 5, 479–502. [Google Scholar]
- Lanzola, G.; Losiouk, E.; Del Favero, S.; Facchinetti, A.; Galderisi, A.; Quaglini, S.; Magni, L.; Cobelli, C. Remote blood glucose monitoring in mHealth scenarios: A review. Sensors 2016, 16, 1983. [Google Scholar] [CrossRef] [PubMed]
- Juhl, R.; Møller, J.K.; Jørgensen, J.B.; Madsen, H. Modeling and Prediction Using Stochastic Differential Equations. In Prediction Methods for Blood Glucose Concentration; Springer International Publishing: New York, NY, USA, 2016; pp. 183–209. [Google Scholar]
- Palumbo, P.; Pepe, P.; Panunzi, S.; De Gaetano, A. Recent Results on Glucose–Insulin Predictions by Means of a State Observer for Time Delay Systems. In Prediction Methods for Blood Glucose Concentration; Springer International Publishing: New York, NY, USA, 2016; pp. 227–241. [Google Scholar]
- Kirchsteiger, H.; Efendic, H.; Reiterer, F.; del Re, L. Alternative Frameworks for Personalized Insulin–Glucose Models. In Prediction Methods for Blood Glucose Concentration; Springer International Publishing: New York, NY, USA, 2016; pp. 1–29. [Google Scholar]
- Cappon, G.; Vettoretti, M.; Facchinetti, A.; Sparacino, G. A Neural Network Based Approach to Personalize Insulin Bolus Calculation Using Continuous Glucose Monitoring. J. Diabetes Sci. Technol. 2018, 12, 265–272. [Google Scholar] [CrossRef] [PubMed]
- Broens, T.; Van Halteren, A.; Van Sinderen, M.; Wac, K. Towards an application framework for context-aware m-health applications. Int. J. Internet Protoc. Technol. 2007, 2, 109–116. [Google Scholar] [CrossRef]
- Yuce, M.R. Implementation of wireless body area networks for healthcare systems. Sens. Actuators A Phys. 2010, 162, 116–129. [Google Scholar] [CrossRef]
- Preuveneers, D.; Berbers, Y. Mobile phones assisting with health self-care: A diabetes case study. In Proceedings of the 10th International Conference on Human Computer Interaction with Mobile Devices and Services, Amsterdam, The Netherlands, 2–5 September 2008; ACM: New York, NY, USA, 2008; pp. 177–186. [Google Scholar]
- Sieverdes, J.C.; Treiber, F.; Jenkins, C.; Hermayer, K. Improving diabetes management with mobile health technology. Am. J. Med. Sci. 2013, 345, 289–295. [Google Scholar] [CrossRef] [PubMed]
- Cappon, G.; Acciaroli, G.; Vettoretti, M.; Facchinetti, A.; Sparacino, G. Wearable Continuous Glucose Monitoring Sensors: A Revolution in Diabetes Treatment. Electronics 2017, 6, 65. [Google Scholar] [CrossRef]
- Kovatchev, B.P.; Renard, E.; Cobelli, C.; Zisser, H.C.; Keith-Hynes, P.; Anderson, S.M.; Brown, S.A.; Chernavvsky, D.R.; Breton, M.D.; Farret, A.; et al. Feasibility of outpatient fully integrated closed-loop control first studies of wearable artificial pancreas. Diabetes Care 2013, 36, 1851–1858. [Google Scholar] [CrossRef] [PubMed]
- Leelarathna, L.; Wilmot, G. Flash forward: A review of flash glucose monitoring. Diabet. Med. 2018, 35, 472–482. [Google Scholar] [CrossRef] [PubMed]
- Nachman, L.; Baxi, A.; Bhattacharya, S.; Darera, V.; Deshpande, P.; Kodalapura, N.; Mageshkumar, V.; Rath, S.; Shahabdeen, J.; Acharya, R. Jog falls: A pervasive healthcare platform for diabetes management. In Proceedings of the International Conference on Pervasive Computing, Newcastle, UK, 18–22 June 2010; pp. 94–111. [Google Scholar]
- Al Kukhun, D.; Soukkarieh, B.; Sèdes, F. ADMAN: An alarm-based mobile diabetes management system for mobile geriatric teams. In Proceedings of the East European Conference on Advances in Databases and Information Systems, Poitiers, France, 8–11 September 2015; Springer: Cham, Switzerland, 2015; pp. 527–535. [Google Scholar]
- Al-Taee, M.A.; Al-Nuaimy, W.; Al-Ataby, A.; Muhsin, Z.J.; Abood, S.N. Mobile health platform for diabetes management based on the Internet-of-Things. In Proceedings of the 2015 IEEE Jordan Conference on Applied Electrical Engineering and Computing Technologies (AEECT), The Dead Sea, Jordan, 3–5 November 2015; pp. 1–5. [Google Scholar]
- Hsu, W.C.; Lau, K.H.K.; Huang, R.; Ghiloni, S.; Le, H.; Gilroy, S.; Abrahamson, M.; Moore, J. Utilization of a cloud-based diabetes management program for insulin initiation and titration enables collaborative decision making between healthcare providers and patients. Diabetes Technol. Ther. 2016, 18, 59–67. [Google Scholar] [CrossRef] [PubMed]
- Vivekanandan, S.; Devanand, M. Remote monitoring for diabetes disorder: Pilot study using InDiaTel prototype. Eur. Res. Telemed/La Rech. Eur. Téléméd. 2015, 4, 63–69. [Google Scholar] [CrossRef]
- Rho, M.J.; Kim, H.S.; Chung, K.; Choi, I.Y. Factors influencing the acceptance of telemedicine for diabetes management. Clust. Comput. 2015, 18, 321–331. [Google Scholar] [CrossRef]
- Dolin, R.H.; Alschuler, L.; Boyer, S.; Beebe, C.; Behlen, F.M.; Biron, P.V.; Shabo, A. HL7 clinical document architecture, release 2. J. Am. Med. Inform. Assoc. 2006, 13, 30–39. [Google Scholar] [CrossRef] [PubMed]
- Mamykina, L.; Mynatt, E.D.; Kaufman, D.R. Investigating health management practices of individuals with diabetes. In Proceedings of the SIGCHI Conference on Human Factors in Computing Systems, Montreal, QC, Canada, 22–27 April 2006; pp. 927–936. [Google Scholar]
- Lim, H.B.; Teo, Y.M.; Mukherjee, P.; Lam, V.T.; Wong, W.F.; See, S. Sensor grid: Integration of wireless sensor networks and the grid. In Proceedings of the IEEE Conference on Local Computer Networks 30th Anniversary (LCN’05), Sydney, Australia, 15–17 November 2005; pp. 91–99. [Google Scholar]
- Choi, J.M.; Choi, B.H.; Seo, J.W.; Sohn, R.H.; Ryu, M.S.; Yi, W.; Park, K.S. A system for ubiquitous health monitoring in the bedroom via a Bluetooth network and wireless LAN. In Proceedings of the 26th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, IEMBS’04, San Francisco, CA, USA, 1–5 September 2004; Volume 2, pp. 3362–3365. [Google Scholar]
- Talpur, M.S.H.; Bhuiyan, M.Z.A.; Wang, G. Energy-efficient healthcare monitoring with smartphones and IoT technologies. Int. J. High Perform. Comput. Netw. 2015, 8, 186–194. [Google Scholar] [CrossRef]
- Omre, A.H.; Keeping, S. Bluetooth low energy: Wireless connectivity for medical monitoring. J. Diabetes Sci. Technol. 2010, 4, 457–463. [Google Scholar] [CrossRef] [PubMed]
- Jara, A.J.; Fernández, D.; López, P.; Zamora, M.A.; Ubeda, B.; Skarmeta, A.G. Evaluation of Bluetooth low energy capabilities for continuous data transmission from a wearable electrocardiogram. In Proceedings of the 2012 Sixth International Conference on Innovative Mobile and Internet Services in Ubiquitous Computing (IMIS), Palermo, Italy, 4–6 July 2012; pp. 912–917. [Google Scholar]
- Carroll, R.; Cnossen, R.; Schnell, M.; Simons, D. Continua: An interoperable personal healthcare ecosystem. IEEE Pervasive Comput. 2007, 6, 90–94. [Google Scholar] [CrossRef]
- Jara, A.J.; Zamora-Izquierdo, M.A.; Skarmeta, A.F. Interconnection framework for mHealth and remote monitoring based on the Internet of Things. IEEE J. Sel. Areas Commun. 2013, 31, 47–65. [Google Scholar] [CrossRef]
- Jara, A.J.; Lopez, P.; Fernandez, D.; Zamora, M.A.; Ubeda, B.; Skarmeta, A.F. Communication protocol for enabling continuous monitoring of elderly people through near field communications. Interact. Comput. 2013. [Google Scholar] [CrossRef]
- The Nightscout Project. Available online: http://www.nightscout.info (accessed on 17 February 2018).
- Wientjes, K.J.; Schoonen, A.J. Determination of time delay between blood and interstitial adipose tissue glucose concentration change by microdialysis in healthy volunteers. Int. J. Artif. Organs 2001, 24, 884–889. [Google Scholar] [CrossRef] [PubMed]
- Basu, A.; Dube, S.; Veettil, S.; Slama, M.; Kudva, Y.C.; Peyser, T.; Basu, R. Time lag of glucose from intravascular to interstitial compartment in type 1 diabetes. J. Diabetes Sci. Technol. 2015, 9, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Borghouts, L.B.; Keizer, H.A. Exercise and insulin sensitivity: A review. Int. J. Sports Med. 2000, 21, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Alexakis, C.; Nyongesa, H.O.; Saatchi, R.; Harris, N.D.; Davies, C.; Emery, C.; Ireland, R.H.; Heller, S.R. Feature extraction and classification of electrocardiogram (ECG) signals related to hypoglycaemia. In Proceedings of the Computers in Cardiology, Thessaloniki Chalkidiki, Greece, 21–24 September 2003; pp. 537–540. [Google Scholar]
- Minh, T.D.; Oliver, S.R.; Ngo, J.; Flores, R.; Midyett, J.; Meinardi, S.; Carlson, M.K.; Rowland, F.S.; Blake, D.R.; Galassetti, P.R. Noninvasive measurement of plasma glucose from exhaled breath in healthy and type 1 diabetic subjects. Am. J. Physiol. Endocrinol. Metab. 2011, 300, E1166–E1175. [Google Scholar] [CrossRef] [PubMed]
- Baba, J.S.; Cameron, B.D.; Theru, S.; Cote, G.L. Effect of temperature, pH, and corneal birefringence on polarimetric glucose monitoring in the eye. J. Biomed. Opt. 2002, 7, 321–328. [Google Scholar] [CrossRef] [PubMed]
- Drouin, P. Blood glucose control on Sunday in IDDM patients: Intensified conventional insulin therapy versus continuous subcutaneous insulin infusion. Diabetes Res. Clin. Pract. 1998, 3, 175–180. [Google Scholar]
- Place, J.; Robert, A.; Brahim, N.B.; Keith-Hynes, P.; Farret, A.; Pelletier, M.J.; Buckingham, B.; Breton, M.; Kovatchev, B.; Renard, E. DiAs web monitoring: A real-time remote monitoring system designed for artificial pancreas outpatient trials. J. Diabetes Sci. Technol. 2013, 7, 1427–1435. [Google Scholar] [CrossRef] [PubMed]
- Dassau, E.; Jovanovic, L.; Doyle, F.J.; Zisser, H.C. Enhanced 911/global position system wizard: A telemedicine application for the prevention of severe hypoglycemia—Monitor, alert, and locate. J. Diabetes Sci. Technol. 2009, 3, 1501–1506. [Google Scholar] [CrossRef] [PubMed]
- Rigla, M. Smart telemedicine support for continuous glucose monitoring: The embryo of a future global agent for diabetes care. J. Diabetes Sci. Technol. 2011, 5, 63–67. [Google Scholar] [CrossRef] [PubMed]
- Ding, S.; Schumacher, M. Sensor monitoring of physical activity to improve glucose management in diabetic patients: A review. Sensors 2016, 16, 589. [Google Scholar] [CrossRef] [PubMed]
- Case, M.A.; Burwick, H.A.; Volpp, K.G.; Patel, M.S. Accuracy of smartphone applications and wearable devices for tracking physical activity data. JAMA 2015, 313, 625–626. [Google Scholar] [CrossRef] [PubMed]
- Kowalski, A.J. Can we really close the loop and how soon? Accelerating the availability of an artificial pancreas: A roadmap to better diabetes outcomes. Diabetes Technol. Ther. 2009, 11, S113–S119. [Google Scholar] [CrossRef] [PubMed]
- Assunção, M.D.; Calheiros, R.N.; Bianchi, S.; Netto, M.A.; Buyya, R. Big Data computing and clouds: Trends and future directions. J. Parallel Distributed Comput. 2015, 79, 3–15. [Google Scholar] [CrossRef]
- Hashem, I.A.T.; Yaqoob, I.; Anuar, N.B.; Mokhtar, S.; Gani, A.; Khan, S.U. The rise of “big data” on cloud computing: Review and open research issues. Inf. Syst. 2015, 47, 98–115. [Google Scholar] [CrossRef]
- Marr, B. How Big Data Is Changing Healthcare; Forbes/Tech: Jersey City, NJ, USA, 2015. [Google Scholar]
- Vayena, E.; Dzenowagis, J.; Brownstein, J.S.; Sheikh, A. Policy implications of big data in the health sector. Bull. World Health Organ. 2018, 96, 66–68. [Google Scholar] [CrossRef] [PubMed]
- Moreno-Cano, M.V.; Zamora-Izquierdo, M.A.; Skarmeta, A.F. An IoT Based Framework for User Centric Smart Building Services. Int. J. Web Grid Serv. 2015, 11, 78–101. [Google Scholar] [CrossRef]
- Campo, C.; Mendoza, F.A.; Sánchez, D.D.; García-Rubio, C.; López, A.M. Secure Service Discovery based on Trust Management for ad-hoc Networks. J. UCS 2006, 12, 340–356. [Google Scholar]
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).