Proof-of-Familiarity: A Privacy-Preserved Blockchain Scheme for Collaborative Medical Decision-Making
Abstract
:Featured Application
Abstract
1. Introduction
- Multi-dimensional personal data privacy policies imposed by individual institutes.
- Clinical data, medical decisions, and patient identities are being manipulated and distributed without proper acknowledgment and consent.
- Scalability and management difficulties during collaborative decision gathering and storing.
- Usage of centralized architecture with a single point of failure.
- Incompatibility with institutional and regional regulations in SDM-based medical treatment.
- Lack of association among health professionals.
1.1. The Contribution of the Paper
- This scheme provides a seamless sharing of decisions among the stakeholders.
- This scheme stores medical decisions and identities with an off-chain blockchain to increase confidentiality. Hence, the study fully complies with existing privacy regulations regarding PII.
- PoF, the first consensus algorithm so far, reflects the doctor’s skill, cured patient’s feedback, insurance company’s policy, and blockchain’s security concurrently in decision making.
1.2. Roadmap of the Paper
2. Literature Review
2.1. Blockchain
- Trusted transaction: Blockchain can digitally authenticate transaction regulations and nodes. Finally, the necessity of a trusted third party is useless. This largely reduces the settlement cost.
- Decentralized storage: Blockchain stores multiple copies of data in a physically parted location. Data integrity can be checked from all available nodes to remove a single point of failure.
- Traceability: Verification of corrupted information and nodes are possible by hash and timestamp validation. Data traceability also empowers the identification of the corrupted node. Eventually, this traceability and loyalty of blockchain encourages stakeholders for collaboration.
- Improved security: Double layer security (private-public key) checking and immutability of information with hash storing increases the security of blockchain over existing technologies.
- Header: Header stores information like version, threshold, timestamp, nonce, etc.
- Transaction counter: Transaction counter reflects the current block number.
- Transaction data: Use of this field varies on purpose (i.e., decision, rating, money, privacy rule etc.).
- Forking: Forking happens if a transaction faces concurrent and multiple correct paths. Three kinds of forking are hard fork, soft fork, and user-centric fork [41].
2.2. Collaborative Medical Decision-Making and Blockchain
Medical decision science is a field that encompasses several related pursuits. As a normative endeavor, it proposes standards for ideal decision making. As a descriptive endeavor, it seeks to explain how physicians and patients routinely make decisions, and has identified both barriers to, and facilitators of, effective decision making. As a prescriptive endeavor, it seeks to develop tools that can guide physicians, their patients, and health care policymakers to make good decisions in practice.[56]
3. Proposed Method
3.1. Architecture and Flow Chart of the Whole System
- Patient (P): Patient, P might be deprived and located in a distressed area without ample medical facilities. By this scheme, P achieves a decent treatment (medical decision) by collaborating with D, Ic, and Cp. P is equipped with a DBloc, an API, and a DBbc to manage identities and decisions.
- Doctor (D): Doctor, D collaborates with D, Ic, and Cp through PoF to help P with an expert decision. D has a DBloc, an API, and a DBbc to manage identities and decisions.
- Cured patient (Cp): Cured patient, Cp represents patients already treated with a similar disease. Cp collaborates with D, Ic, and Cp and helps P with the experience Cp gathered during diagnosis. A Cp also uses a DBloc, an API, and a DBbc to manage identities and decisions.
- Insurance company (Ic): Insurance company, Ic deals with health-related financial strategies of a P. Ic uses a DBbc, an API, and a DBloc to manage identities and decisions.
3.2. Proposed Proof of Familiarity (PoF) Consensus Algorithm
3.2.1. Functional Architecture Proof of Familiarity (PoF)
- The judgement of the doctor: While choosing a doctor’s decision, factors like job experience time (JET) and treatment success rate (TSR) are considered. IFI of a doctor (IFI_D) is calculated as IFI_D = {JET, TSR}.
- The perspective of the cured patient: Proposed system considers factors like treatment experience time (TET), current condition (CC), and experience of disease (ED) of cured patients. IFI of a cured patient (IFI_Cp) is calculated as: IFI_Cp = {TET, CC, ED}.
- Perception of insurance company: Financial policy is another significant aspect of collaborative medical decision-making. IFI of an insurance company (IFI_Ic) is calculated from settlement time (ST) and cover amount (CA). IFI_Ic is calculated as: IFI_Ic = {ST, CA}.
- Final collaborative medical decision: Finally, PoF calculates the final collaborative medical decision, Cd. Based on the IFI value (IFI_Ic, IFI_Cp, and IFI_D) of three entities, a winner is chosen from each of the entities (D, Ic, and Cp). After combining three winner’s decisions, Cd is decided for P.
3.2.2. Transactions in Proof of Familiarity (PoF)
3.2.3. Block Architecture
- Hash of last block: Hash of recently created block is stored by this field. This tracks originality of the data of this block. If modification happens to block 0, the header of block 1 will no longer point to the header of block 0. This corrupted block is disconnected from the rest of the block (blockchain).
- Timestamp: This field stores the approval time of the final collaborative medical decision, Cd.
- Flag 1: Patient’s NPII and clinical history are stored in ‘Flag 1′ field.
- Flag 2: Doctor’s NPII and decision history are stored in ‘Flag 2′ field.
- Flag 3: Insurance company’s NPII and policy history are stored in ‘Flag 3′ field.
- Flag 4: Cured patient’s NPII and clinical history are stored in ‘Flag 3′ field.
- PII Hash: Hash of the locally stored PII is stored in ‘hash’ field. This can cross check the originality of the information stored in local databases of P, D, Ic, and Cp.
- Decision: Accepted final collaborative medical decision, Cd are stored in ‘decision’ field.
- NPII: All other significant NPII (rules, conditions) is stored in the ‘NPII’ field of the block.
3.2.4. Proof of Familiarity (PoF) Algorithm
| Algorithm 1: Selection of final participating entities |
| Input: patients, P; cured patients, Cp; doctors, D; insurance companies, Ic; // all participating entities individual decision, Id; // decision of participating entities treatment experience time, TET; current condition, CC; experience of disease, ED // decision judging factors of cured patients job experience time, JET; treatment success rate, TSR; // decision judging factors of doctors settlement time, ST; cover amount, CA // decision judging factors of insurance companies blockchain database, DBbc; local database, DBloc // storing entities (local and blockchain database) Output: //individual familiarity index (IFI) of participating entities individual familiarity index of cured patient, IFI_Cp; Individual familiarity index of doctor, IFI_D; individual familiarity index of insurance company, IFI_Ic finally selected cured patient, Cp_FS; finally selected doctor, DFS; finally selected insurance company, Ic_FS individual familiarity index of finally selected cured patient, IFIFS_Cp; individual familiarity index of finally selected doctor, IFIFS_D; Individual familiarity index of finally selected insurance company, IFIFS_Ic individual decision of finally selected cured patient, Id_FS_Cp; individual decision of finally selected doctors, Id_FS_D; individual decision of finally selected insurance company, Id_FS_Ic Begin: verification of Cp, D, Ic from DBloc and DBbc // identity of participating entities are verified verification of JET, TSR, TET, CC, ED, ST, CA from DBloc and DBbc // decision judging factors are verified verification of Id of Cp, D, Ic from DBloc and DBbc // individual decisions are verified for each (Cp, D, Ic) IFI_Cp = Sum (TET, CC, ED) // individual familiarity index of cured patients FI_D = Sum (JET, TSR) // individual familiarity index of doctors IFI_Ic = Sum (ST, CA) // individual familiarity index of insurance companies end for each (Cp, D, Ic) Cp_Fs = Cp with max (IFI_Cp) // finally selected cured patient is chosen with maximum IFI DFS = D with max (IFI_D) // finally selected doctor is chosen with maximum IFI Ic_FS = Ic with max (IFI_Ic) // finally selected insurance company is chosen with maximum IFI end for each (Cp, D, Ic) Id_FS_Cp = Id with max (IFI_Cp) // individual decision of finally selected cured patient Id_FS_D = Id with max (IFI_D) // individual decision of finally selected doctor Id_FS_Ic = Id with max (IFI_Ic) // individual decision of finally selected insurance company end for each (Cp, D, Ic) IFIFS_Cp = Id with max (IFI_Cp) // IFI of finally selected cured patient IFIFS_D = Id with max (IFI_D) // IFI of finally selected doctor IFIFS_Ic = Id with max (IFI_Ic) // IFI of finally selected insurance company end End |
| Algorithm 2: Selecting and storing of final collaborative medical decision |
| Input: finally selected cured patient, Cp_FS; finally selected doctor, DFS; finally selected insurance company, Ic_FS individual familiarity index of finally selected cured patient, IFIFS_Cp; individual familiarity index of finally selected doctor, IFIFS_D; individual familiarity index of finally selected insurance company, IFIFS_Ic individual decision of finally selected cured patient, Id_FS_Cp; individual decision of finally selected doctors, Id_FS_D; individual decision of finally selected insurance company, Id_FS_Ic blockchain database, DBbc; local database, DBloc // storing entities (local and blockchain database) Output: final collaborative medical decision, Cd Begin: Cp_FS, DFS, Ic_FS broadcast Id_FS_Cp, Id_FS_D, Id_FS_Ic to Cp, D, Ic //decision broadcast for consensus Cd = combination of (Id_FS_Cp, Id_FS_D, Id_FS_Ic,) //aggregation of individual decision in medical decision Cd stores in DBbc //final collaborative medical decision is stored in blockchain Cp_FS; DFS; Ic_FS stores in DBloc //finally selected entities’ identities are stored in local database Hash of locally stored Cp_FS, DFS, Ic_FS from DBloc stores in DBbc // hash are stored in blockchain IFIFS_Cp, IFIFS_D, IFIFS_Ic stores in DBbc // IFI of finally selected participants are stored in blockchain JET, TSR, TET, CC, ED, ST, CA of Cp_SPE, DSPE, Ic_SPE is updated in DBbc and DBloc End |
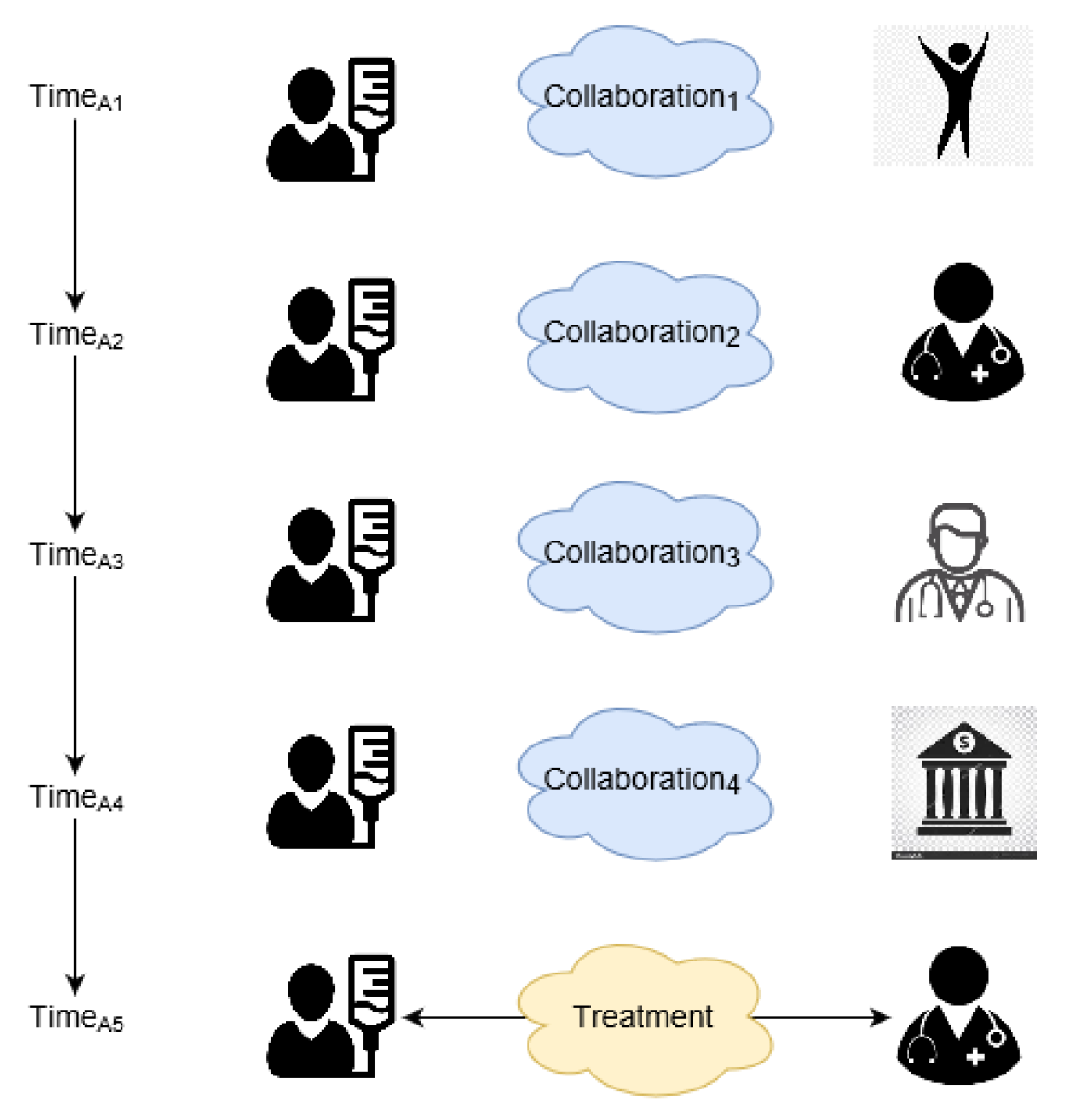
3.3. Running Example
- At time 0: Patient, P1 broadcasts desired medical problem to D1, D2, D3, Cp1, Cp2, Cp3, Ic1, Ic2 for collaborative medical decision gathering (Figure 8).
- At time 1: Participating entities (D1, D2, D3, Cp1, Cp2, Cp3, Ic1, Ic2) return individual decisions (judgment and policy) to PoF (Figure 9).
- At time 2: Based on IFI of D1, D2, D3, Cp1, Cp2, Cp3, Ic1, Ic2 (Table 4), PoF decides decision giving entities (D3, Ic1, Cp2) with maximum IFI of 0.83, 0.85, and 0.90, respectively. IFI is calculated from the considering factors mentioned in rightmost column of Table 4. The final decisions of D3, Ic1, Cp2 are sent again to D1, D2, D3, Cp1, Cp2, Cp3, Ic1, Ic2 for final consensus (Figure 10).
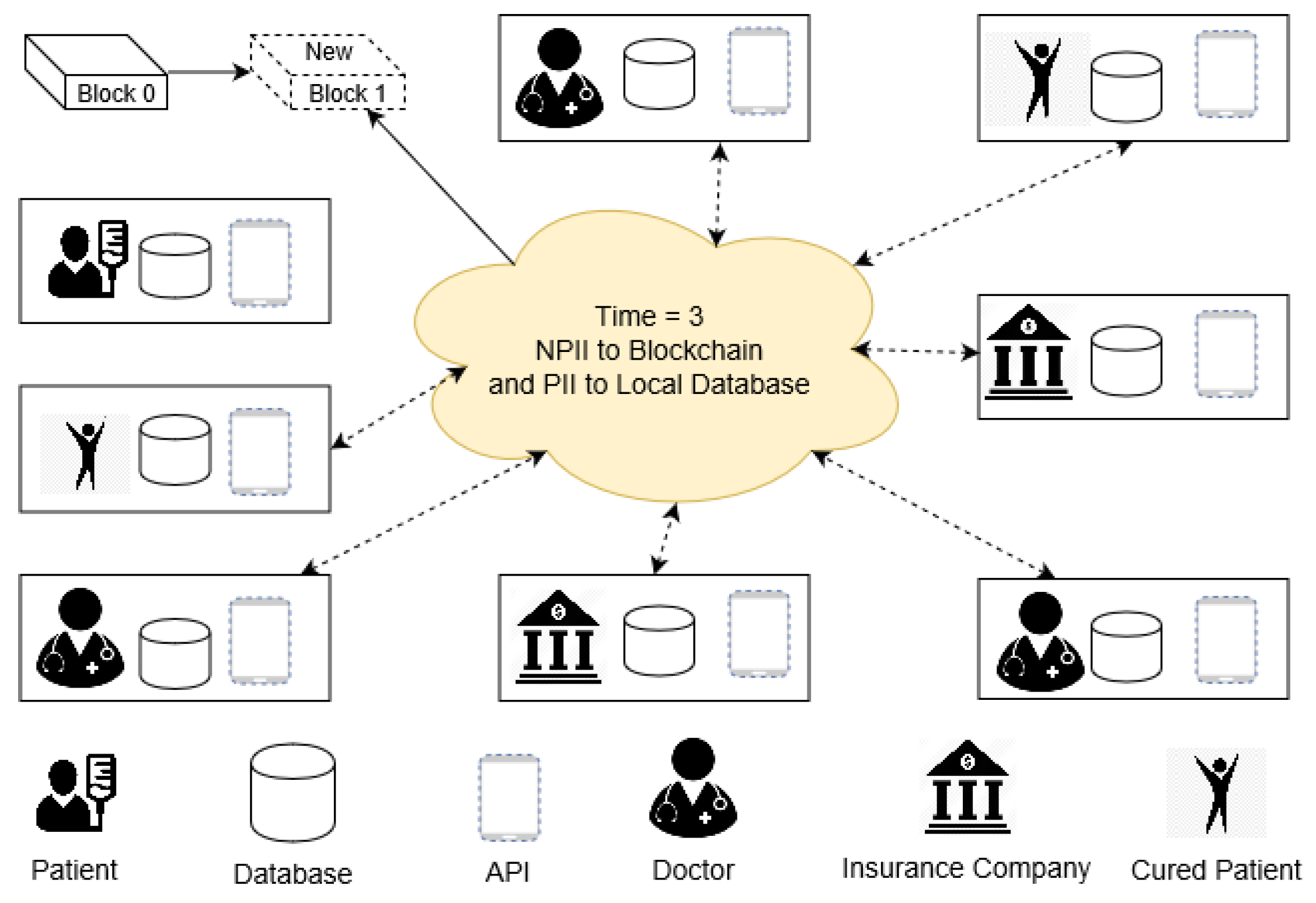
- At time 3: Sensitive personal information (PII & PPII) is stored in DBloc of D1, D2, D3, Cp1, Cp2, Cp3, Ic1, Ic2. Hash of the locally stored PII, PPII, and NPII are also stored as a new block (Figure 11).
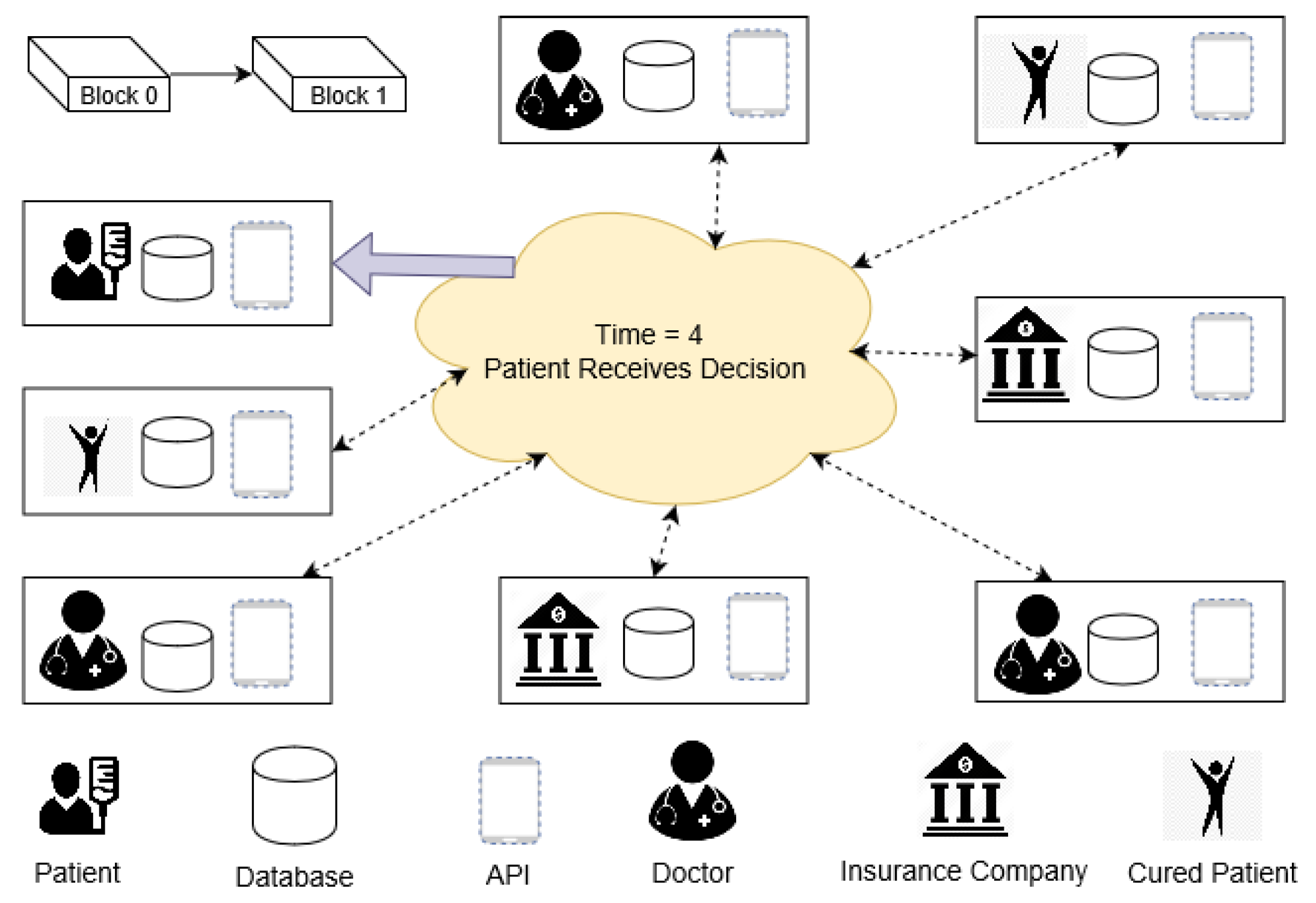
- At time 4: Final collaborative medical decision, Cd is created by aggregating decisions of D3, Ic1, Cp2 and back to P. Lastly, IFI of successful decision-makers are raised in DBloc and DBbc for future use (Figure 12). This rise of IFI is the only incentive in the proposed PoF scheme.
4. Implementation and Discussion
4.1. System Implementation
- Individual node writes data in local storage.
- Hash of the data and data size are published to the network.
- After agreement from the network (consensus), the hash of locally stored off-chain data and insensitive information are stored in blockchain as a new block without any associated costs.
- Addition of a new block finishes the blockchain transaction procedure.
- To ensure privacy blockchain’s activities are visible to chosen participants only.
- To enable mining to take place securely without proof of work and its associated costs.
- Facilitates privacy preservation and control over data with an easy to configure and deploy package by supporting both UNIX and Windows system.
- Provides a comprehensive JSON-RPC (Remote Procedure Call) application programming interface (API) for easy integration with the systems.
- The maximum block size is under the participant’s control, it solves block size monitoring issues.
- As this is a closed (consortium) system, it considers decision only from interested participants.
- In MultiChain 2.0, users are permitted to configure configuration parameters.
- This study uses a round robin scheduling scheme for PoF. P, D, Ic, and Cp must approve or deny a decision during their turn to generate a valid new block. For robustness of the system, mining diversity is set to 0.75 out of 1. For approving a new block, at least 75% of the total nodes or P, D, Ic, and Cp of a block must agree and respond. This mechanism saves the system from freezing up if any set of miners become inactive for a prolonged period (Figure 13).
4.2. Performance Analysis
4.2.1. No Single Point of Failure
4.2.2. Smaller Block Size
4.2.3. Comply with Privacy Policy
4.2.4. Security
4.2.5. Cost
4.2.6. Quality of Treatment
4.2.7. Time
4.2.8. Confidentiality and Privacy
- The attack on blockchain data (on-the-chain data): If a node (attacker) attempts to modify a block illicitly, the consensus from all legitimate nodes can demolish the attack. Similarly, decentralized architecture helps to retrieve lost information or corrupted information from leftover nodes. Block data can also cross check with locally stored hash information of similar data [45].
- The attack on local data store (off-the-chain data): If a node (attacker) attempts to modify locally stored information and successfully changes (corrupts) the local database information, the node will not be corrupted and unknown for long. During collaborative medical decision-making, hashes of every local databases and blockchain databases are cross-checked before a decision is finalized. While initiating the next collaboration, hashes of the corrupted node and the rest of the nodes will be mismatched. Because of this off-the-chain data storing architecture, hashes of local and blockchain databases can be checked.
4.2.9. Scalability
4.2.10. Throughput Performance
4.2.11. Comparison with a Few Other Consensus Algorithms
- Node management: In between the consortium and permissionless blockchain, consortium blockchain is more controlled by the peers and allows comparatively easy modification of block information. If blockchain nodes are limited, identities of blockchain nodes can also be anonymous. Therefore, the proposed method chooses the consortium system for efficient node management. However, PBFT [37] and Tendermint [40] assess identities of the available nodes during a consensus mechanism. Alternatively, most of the permissionless consensus (PoW [35], PoS [38], and Ripple [39]), nodes are able to join the network without any identity verification [82].
- Transmission rate: The proposed system experiences a higher transmission rate for three reasons. Firstly, this scheme is a consortium blockchain with a limited number of nodes, so consensus gathering needs reasonably less time. Secondly, the use of off-the-chain data storing architecture also reduces the overall block size. Finally, Multichain [79] allows for the configuration of block size and block time, so the overall throughput increases in the proposed scheme by many times. Alternatively, PoS encourages the owner of the coin to prolong the coin holding time [83], so it also experiences a slightly higher transmission time. Similarly, as PBFT needs several transactions among peers before approving a block, transaction time is also high like Ripple [84]. As PoW demands higher node performance, the overall bottleneck increases [82]. Similarly, Ripple needs to wait till 80% are in agreement, and it also needs a higher transaction time [82]. On the other hand, the proposed PoF based collaborative demands 75% agreement (which is also changeable).
- Energy consumption: In PoW, mining reward depends on the amount of work done, so the computer system of the miners consumes higher energy. Compared to PoW, PoS consensus gathering algorithm requires less energy but is still high [82]. Alternatively, the proposed system (PoF) consumes less energy, as no reward system is available on work.
- Scalability: As PoW and PoS have higher energy consumption rate and block size, they preserve a higher scalability issue. PoS improved scalability by achieving better latency with a smaller block size [84]. Alternatively, due to off-the-chain data storing facilities and lower block size, the proposed PoF based collaborative system is highly scalable [85]. PBFT, Ripple, and Tendermint also face lower scalability to the existing system for network bottleneck [85].
- Finality process: Unlike the PoW, PoS, Ripple, and Tendermint blockchain consensus algorithm, PoF follows an immediate or absolute finality process. That is, just after the agreement from decision giving entities a new block with the collaborative medical decision is created. Alternatively, most consensus algorithms (PoW, PoS, Ripple, and Tendermint) follow a probabilistic finality process that waits until a certain period before a block gets finalized [82]. However, real-world business also demands immediate finality, as no one wants to take the risk of losing assets during the waiting time [82,84].
- Adversary tolerated power: Adversary tolerated power states the amount of control an attacker must have to regulate a blockchain network. A node in PoW needs at least 25% computer power to manipulate or create a block. Similarly, an attacker needs to control over 51% (more than half) of the stakes to control over the blockchain [84]. In comparison to those, the proposed PoF restricts adversary tolerated power to 75%. That is, at least 75% of the participated entities must agree to take control of a chain [72].
4.3. Limitation and Future Work
4.3.1. Prioritization of Decision Giving Entities
4.3.2. Identical IFI of the Decision Giving Entities
4.3.3. The Inclusion of Critical Aspects of Medical Decision-Making
4.3.4. Real-Life System Implementation
4.3.5. Empirical Validation Comparison with Studies
5. Conclusions
- PoF based collaborative medical decision-making system provides middlemen with a less decentralized medical decision collaboration platform with no single point of failure.
- PoF based collaborative medical decision-making system uses modified blockchain architecture (off-the-chain) to secure clinical data privacy and security.
- PoF based collaborative medical decision-making system allows trusted participation of significant medical decision-giving entities to provide a better clinical decision.
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Christensen, C.; Larson, J.R., Jr. Collaborative medical decision making. Med. Decis. Mak. 1993, 13, 339–346. [Google Scholar] [CrossRef] [PubMed]
- Dowell, J.; Williams, B.; Snadden, D. Patient-Centered Prescribing: Seeking Concordance in Practice; CRC Press: Boca Raton, FL, USA, 2018; ISBN 1498793495. [Google Scholar]
- Making Health Care Decisions; Report; President’s Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research: Washington, DC, USA, 1982; volume 1, 57.
- Accenture. Available online: https://www.accenture.com/t20170411T012518__w__/us-en/_acnmedia/PDF-43/Accenture-Health-Are-You-One-Breach-Away-From-Losing-a-Healthcare-Consumer.pdf (accessed on 21 December 2018).
- Lord, N. Top 10 Biggest Healthcare Data Breaches. Available online: https://digitalguardian.com/blog/top-10-biggest-healthcare-data-breaches-all-time (accessed on 21 December 2018).
- Ahmed, M.; Ullah, A.S.S.M.B. Infrequent pattern mining in smart healthcare environment using data summarization. J. Supercomput. 2018, 74, 1–19. [Google Scholar] [CrossRef]
- Chaudhry, J.; Qidwai, U.; Miraz, M.H.; Ibrahim, A.; Valli, C. Data Security among ISO/IEEE 11073 Compliant Personal Healthcare Devices through Statistical Fingerprinting; Institute of Electrical and Electronics Engineers: Piscataway, NJ, USA, 2017. [Google Scholar]
- Jahan, S.; Chowdhury, M.; Islam, R.; Chaudhry, J. Securing Healthcare Data Using Biometric Authentication. In Proceedings of the Security and Privacy in Communication Networks: SecureComm 2017 International Workshops, ATCS and SePrIoT, Niagara Falls, ON, Canada, 22–25 October 2017; pp. 123–132. [Google Scholar]
- Saleem, K.; Tan, Z.; Buchanan, W. Security for cyber-physical systems in healthcare. In Health 4.0: How Virtualization and Big Data are Revolutionizing Healthcare; Springer: New York, NY, USA, 2017; pp. 233–251. [Google Scholar]
- Identity Theft Resource Center (ITRC). Available online: https://www.idtheftcenter.org/images/breach/2017Breaches/2017AnnualDataBreachYearEndReview.pdf (accessed on 21 November 2018).
- Ahmed, M.; Ullah, A.S.S.M.B. False Data Injection Attacks in Healthcare. In Proceedings of the Australasian Conference on Data Mining; Springer: Singapore, 2017; pp. 192–202. [Google Scholar]
- Snell, E. Healthcare data breach costs highest for 7 th straight year. Heal. IT Secur. 2017, 20. Available online: https//healthitsecurity. com/news/healthcare-data-breach-costshighest-for-7th-straight-year (accessed on 21 January 2019).
- Jensen, R.E.; Snyder, C.F.; Abernethy, A.P.; Basch, E.; Potosky, A.L.; Roberts, A.C.; Loeffler, D.R.; Reeve, B.B. Review of electronic patient-reported outcomes systems used in cancer clinical care. J. Oncol. Pract. 2013, 10, e215–e222. [Google Scholar] [CrossRef] [PubMed]
- Bardram, J.E.; Houben, S. Collaborative affordances of medical records. Comput. Support. Coop. Work 2018, 27, 1–36. [Google Scholar] [CrossRef]
- Park, E.S.; Cho, I.Y. Shared decision-making in the paediatric field: A literature review and concept analysis. Scand. J. Caring Sci. 2018, 32, 478–489. [Google Scholar] [CrossRef] [PubMed]
- Graffigna, G.; Barello, S. Patient engagement in healthcare: Pathways for effective medical decision making. Neuropsychol. Trends 2015, 17, 53–65. [Google Scholar]
- Thomas, P.A.; Kern, D.E.; Hughes, M.T.; Chen, B.Y. Curriculum Development for Medical Education: A Six-Step Approach; JHU Press: Baltimore, ML, USA, 2015; ISBN 1421418517. [Google Scholar]
- Makridakis, S.; Kirkham, R.; Wakefield, A.; Papadaki, M.; Kirkham, J.; Long, L. Forecasting, uncertainty and risk; perspectives on clinical decision-making in preventive and curative medicine. Int. J. Forecast. 2019, 35, 659–666. [Google Scholar] [CrossRef]
- Hesse, F.; Care, E.; Buder, J.; Sassenberg, K.; Griffin, P. A framework for teachable collaborative problem solving skills. In Assessment and Teaching of 21st Century Skills; Springer: New York, NY, USA, 2015; pp. 37–56. [Google Scholar]
- HIPAA (Office for Civil Rights). Available online: https://www.hipaajournal.com/healthcare-data-breach-statistics/ (accessed on 10 December 2018).
- Granja, C.; Janssen, W.; Johansen, M.A. Factors determining the success and failure of ehealth interventions: Systematic review of the literature. J. Med. Internet Res. 2018, 20, e10235. [Google Scholar] [CrossRef] [PubMed]
- Burke, W.; Oseni, T.; Jolfaei, A.; Gondal, I. Cybersecurity Indexes for eHealth. In Proceedings of the Australasian Computer Science Week Multiconference, Sydney, Australia, 29–31 January 2019; p. 17. [Google Scholar]
- Ahmed, M.; Ullah, A.S.S.M.B. Health Care Security Analytics. In Data Analytics; CRC Press: Boca Raton, FL, USA, 2018; pp. 427–440. [Google Scholar]
- Kayaalp, M. Patient Privacy in the Era of Big Data. Balkan Med. J. 2018, 35, 8–17. [Google Scholar] [CrossRef] [PubMed]
- Miraz, M.H.; Ali, M. Applications of Blockchain Technology beyond Cryptocurrency. arXiv, 2018; arXiv:1801.03528. [Google Scholar]
- Voss, W.G. European union data privacy law reform: General data protection regulation, privacy shield, and the right to delisting. Bus. Lawyer 2017, 72, 221–233. [Google Scholar]
- GDPR-EU. Available online: https://gdpr-info.eu/art-4-gdpr/ (accessed on 21 December 2018).
- Zhang, P.; White, J.; Schmidt, D.C.; Lenz, G.; Rosenbloom, S.T. Fhirchain: Applying blockchain to securely and scalably share clinical data. Comput. Struct. Biotechnol. J. 2018, 16, 267–278. [Google Scholar] [CrossRef] [PubMed]
- Zhang, P.; White, J.; Schmidt, D.C.; Lenz, G. Applying software patterns to address interoperability in blockchain-based healthcare apps. arXiv, 2017; arXiv:1706.03700. [Google Scholar]
- Chainforg Blockchain and GDPR. Available online: http://www.chainfrog.com/wp-content/uploads/2017/08/gdpr.pdf (accessed on 25 December 2018).
- Hibbard, J. Patient activation and health literacy: What’s the difference? How do each contribute to health outcomes. Stud Heal. Technol Inf. 2017, 240, 251–262. [Google Scholar]
- Blockchain: Technology Fundamentals of the Trust Machine. Available online: https://www.legalanalytics.law.cuhk.edu.hk/single-post/2017/12/23/Blockchain-Technology-Fundamentals-of-the-Trust-Machine (accessed on 15 May 2018).
- Kuo, T.-T.; Ohno-Machado, L. ModelChain: Decentralized Privacy-Preserving Healthcare Predictive Modeling Framework on Private Blockchain Networks. arXiv, 2018; arXiv:1802.01746. [Google Scholar]
- Ozercan, H.I.; Ileri, A.M.; Ayday, E.; Alkan, C. Realizing the potential of blockchain technologies in genomics. Genome Res. 2018, 28, 1255–1263. [Google Scholar] [CrossRef] [PubMed]
- Bitcoin: A Peer-to-Peer Electronic Cash System. Available online: https://bitcoin.org/en/bitcoin-paper (accessed on 15 June 2018).
- Chuen, D.L.E.E.K.; Deng, R.H. Handbook of Blockchain, Digital Finance, and Inclusion: Cryptocurrency, FinTech, InsurTech, Regulation, ChinaTech, Mobile Security, and Distributed Ledger; Academic Press: Cambridge, MA, USA, 2017; ISBN 0128123001. [Google Scholar]
- Castro, M.; Liskov, B. Practical Byzantine fault tolerance. OSDI 1999, 99, 173–186. [Google Scholar]
- Vasin, P. Blackcoin’s Proof-of-Stake Protocol v2. 2014. Available online: https//blackcoin.co/blackcoin-pos-protocolv2-whitepaper.pdf (accessed on 10 October 2018).
- Schwartz, D.; Youngs, N.; Britto, A. The Ripple protocol consensus algorithm. Ripple Labs Inc White Pap. 2014, 5, 1–8. [Google Scholar]
- Kwon, J. Tendermint: Consensus without Mining. 2014. Available online: https//tendermint.com/static/docs/tendermint.pdf (accessed on 10 December 2018).
- Castor, A. A (Short) Guide to Blockchain Consensus Protocols. 2017. Available online: http//www. coindesk.com/short-guide-blockchain-consensus-protocols (accessed on 10 December 2018).
- The Global Fintech Report. Available online: https://www.pwc.com/gx/en/industries/financial-services/assets/pwc-global-fintech-report-2017.pdf (accessed on 10 January 2019).
- Cocco, L.; Pinna, A.; Marchesi, M. Banking on blockchain: Costs savings thanks to the blockchain technology. Futur. Internet 2017, 9, 25. [Google Scholar] [CrossRef]
- Panarello, A.; Tapas, N.; Merlino, G.; Longo, F.; Puliafito, A. Blockchain and IoT integration: A systematic survey. Sensors 2018, 18, 2575. [Google Scholar] [CrossRef]
- Zyskind, G.; Nathan, O. Decentralizing privacy: Using blockchain to protect personal data. In Proceedings of the Security and Privacy Workshops (SPW), San Jose, CA, USA, 21–22 May 2015; pp. 180–184. [Google Scholar]
- Onik, M.M.H.; Miraz, M.H.; Kim, C.-S. A Recruitment and Human Resource Management Technique using Blockchain Technology for Industry 4.0. In Proceedings of the Smart Cities Symposium (SCS-2018), Manama, Bahrain, 22–23 April 2018; pp. 11–16. [Google Scholar]
- Nofer, M.; Gomber, P.; Hinz, O.; Schiereck, D. Blockchain. Bus. Inf. Syst. Eng. 2017, 59, 183–187. [Google Scholar] [CrossRef]
- Miraz, M.H.; Donald, D.C. Application of Blockchain in Booking and Registration Systems of Securities Exchanges. arXiv, 2018; arXiv:1806.09687. [Google Scholar]
- Al-Zaben, N.; Onik, M.M.H.; Yang, J.; Lee, N.-Y.; Kim, C.-S. General Data Protection Regulation Complied Blockchain Architecture for Personally Identifiable Information Management. In Proceedings of the International Conference on Computing, Electronics & Communications Engineering 2018 (iCCECE ’18), Southend, UK, 16–17 August 2018; pp. 72–88. [Google Scholar]
- Islam, A.; Kader, M.; Shin, S.Y. BSSSQS: A Blockchain Based Smart and Secured Scheme for Question Sharing in the Smart Education System. arXiv, 2018; arXiv:1812.03917. [Google Scholar]
- Swan, M. Blockchain: Blueprint for a New Economy; O’Reilly Media, Inc.: Sebastopol, CA, USA, 2015; ISBN 1491920475. [Google Scholar]
- Onik, M.M.H.; Ahmed, M. Blockchain in the Era of Industry 4.0. In Data Analytics; CRC Press: Boca Raton, FL, USA, 2018; pp. 259–298. [Google Scholar]
- Pinheiro, P.; Macedo, M.; Barbosa, R.; Santos, R.; Novais, P. Multi-agent Systems Approach to Industry 4.0: Enabling Collaboration Considering a Blockchain for Knowledge Representation. In Proceedings of the International Conference on Practical Applications of Agents and Multi-Agent Systems, Toledo, Spain, 20–22 June 2018; Springer: New York, NY, USA, 2018; pp. 149–160. [Google Scholar]
- Feng, L.; Zhang, H.; Chen, Y.; Lou, L. Scalable Dynamic Multi-Agent Practical Byzantine Fault-Tolerant Consensus in Permissioned Blockchain. Appl. Sci. 2018, 8, 1919. [Google Scholar] [CrossRef]
- Hölbl, M.; Kompara, M.; Kamišalić, A.; Nemec Zlatolas, L. A Systematic Review of the Use of Blockchain in Healthcare. Symmetry (Basel) 2018, 10, 470. [Google Scholar] [CrossRef]
- Schwartz, A.; Bergus, G. Medical Decision Making: A Physician’s Guide; Cambridge University Press: Cambridge, UK, 2008; ISBN 1107320062. [Google Scholar]
- Jayanti, A.; Neuvonen, M.; Wearden, A.; Morris, J.; Foden, P.; Brenchley, P.; Mitra, S. Healthcare decision-making in end stage renal disease-patient preferences and clinical correlates. BMC Nephrol. 2015, 16, 189. [Google Scholar] [CrossRef]
- Gatteschi, V.; Lamberti, F.; Demartini, C.; Pranteda, C.; Santamaría, V. Blockchain and Smart Contracts for Insurance: Is the Technology Mature Enough? Futur. Internet 2018, 10, 20. [Google Scholar] [CrossRef]
- Shae, Z.; Tsai, J.J.P. On the design of a blockchain platform for clinical trial and precision medicine. In Proceedings of the 2017 IEEE 37th International Conference on Distributed Computing Systems (ICDCS), Atlanta, GA, USA, 5–8 June 2017; pp. 1972–1980. [Google Scholar]
- Al Omar, A.; Bhuiyan, M.Z.A.; Basu, A.; Kiyomoto, S.; Rahman, M.S. Privacy-friendly platform for healthcare data in cloud based on blockchain environment. Future Gener. Comput. Syst. 2019, 95, 511–521. [Google Scholar] [CrossRef]
- Fan, K.; Wang, S.; Ren, Y.; Li, H.; Yang, Y. MedBlock: Efficient and Secure Medical Data Sharing Via Blockchain. J. Med. Syst. 2018, 42, 136. [Google Scholar] [CrossRef]
- Guo, R.; Shi, H.; Zhao, Q.; Zheng, D. Secure attribute-based signature scheme with multiple authorities for blockchain in electronic health records systems. IEEE Access 2018, 6, 11676–11686. [Google Scholar] [CrossRef]
- Lee, S.-J.; Cho, G.-Y.; Ikeno, F.; Lee, T.-R. BAQALC: Blockchain Applied Lossless Efficient Transmission of DNA Sequencing Data for Next Generation Medical Informatics. Appl. Sci. 2018, 8, 1471. [Google Scholar] [CrossRef]
- Azaria, A.; Ekblaw, A.; Vieira, T.; Lippman, A. Medrec: Using blockchain for medical data access and permission management. In Proceedings of the International Conference on Open and Big Data (OBD), Vienna, Austria, 22–24 August 2016; pp. 25–30. [Google Scholar]
- Dubovitskaya, A.; Xu, Z.; Ryu, S.; Schumacher, M.; Wang, F. Secure and trustable electronic medical records sharing using blockchain. In Proceedings of the AMIA Annual Symposium Proceedings; American Medical Informatics Association: Bethesda, MD, USA, 2017; Volume 2017, p. 650. [Google Scholar]
- Roehrs, A.; da Costa, C.A.; da Rosa Righi, R.; da Silva, V.F.; Goldim, J.R.; Schmidt, D.C. Analyzing the Performance of a Blockchain-based Personal Health Record Implementation. J. Biomed. Inform. 2019, 92, 103140. [Google Scholar] [CrossRef]
- Josh Youbase. Available online: https://www.youbase.io/ (accessed on 15 December 2018).
- Zheng, Z.; Xie, S.; Dai, H.-N.; Wang, H. Blockchain challenges and opportunities: A survey. Int. J. Web Grid Serv. 2018, 14, 252–275. [Google Scholar] [CrossRef]
- Chen, J.; Ma, X.; Du, M.; Wang, Z. A Blockchain Application for Medical Information Sharing. In Proceedings of the 2018 IEEE International Symposium on Innovation and Entrepreneurship (TEMS-ISIE), Beijing, China, 30 March–1 April 2018; pp. 1–7. [Google Scholar]
- Tseng, J.-H.; Liao, Y.-C.; Chong, B.; Liao, S. Governance on the Drug Supply Chain via Gcoin Blockchain. Int. J. Environ. Res. Public Health 2018, 15, 1055. [Google Scholar] [CrossRef] [PubMed]
- Greenspan, G. MultiChain Private Blockchain—White Paper. 2015. Available online: http//www. multichain.com/download/MultiChain-White-Paper.pdf (accessed on 10 May 2018).
- Greenspan, G. Off-Chain (Alpha 3) Multichain 2.0. Available online: https://www.multichain.com/blog/2018/06/scaling-blockchains-off-chain-data/ (accessed on 1 January 2019).
- Shrestha, A.K.; Vassileva, J. Blockchain-Based Research Data Sharing Framework for Incentivizing the Data Owners. In Proceedings of the International Conference on Blockchain; Springer: New York, NY, USA, 2018; pp. 259–266. [Google Scholar]
- Shrestha, A.K.; Vassileva, J. User-controlled privacy-preserving user profile data sharing based on blockchain. In Proceedings of the Future Technologies Conference (FTC), Vancouver, QC, Canada, 29–30 November 2017. [Google Scholar]
- Ramya, U.M.; Sindhuja, P.; Atsaya, R.A.; Dharani, B.B.; Golla, S.S.M.V. Reducing Forgery in Land Registry System Using Blockchain Technology. In Proceedings of the International Conference on Advanced Informatics for Computing Research; Springer: New York, NY, USA, 2018; pp. 725–734. [Google Scholar]
- Onik, M.M.H.; Al-Zaben, N.; Phan Hoo, H.; Kim, C.-S. MUXER—A New Equipment for Energy Saving in Ethernet. Technologies 2017, 5, 74. [Google Scholar] [CrossRef]
- Youssef, M.; Al Zahr, S.; Gagnaire, M. Translucent network design from a CapEx/OpEx perspective. Photonic Netw. Commun. 2011, 22, 85–97. [Google Scholar] [CrossRef]
- Maxwell, W.; Salmon, J. A guide to blockchain and data protection. Hogan Lovells, September 2017. [Google Scholar]
- About Throughput Performance—MultiChain Developer Q & A. Available online: https://www.multichain.com/qa/5556/about-throughput-performance (accessed on 14 March 2019).
- Inje University Haeundae Paik Hospital. Available online: http://haeundae.paik.ac.kr/eng/main/main.asp (accessed on 14 March 2019).
- Ashish Tool to Measure Blockchain Performance: Hyperledger Caliper. Available online: https://medium.com/coinmonks/tool-to-measure-blockchain-performance-hyperledger-caliper-f192adfba52 (accessed on 11 March 2019).
- Zheng, Z.; Xie, S.; Dai, H.; Chen, X.; Wang, H. An overview of blockchain technology: Architecture, consensus, and future trends. In Proceedings of the 2017 IEEE International Congress on Big Data (BigData Congress), Honolulu, HI, USA, 25–30 June 2017; pp. 557–564. [Google Scholar]
- Mingxiao, D.; Xiaofeng, M.; Zhe, Z.; Xiangwei, W.; Qijun, C. A review on consensus algorithm of blockchain. In Proceedings of the 2017 IEEE International Conference on Systems, Man, and Cybernetics (SMC), Banff, AB, Canada, 5–8 October 2017; pp. 2567–2572. [Google Scholar]
- Bach, L.M.; Mihaljevic, B.; Zagar, M. Comparative analysis of blockchain consensus algorithms. In Proceedings of the 2018 41st International Convention on Information and Communication Technology, Electronics and Microelectronics (MIPRO), Opatija, Croatia, 21–25 May 2018; pp. 1545–1550. [Google Scholar]
- Proof of Stake and Scalability—Pool Of Stake—Medium. Available online: https://medium.com/@poolofstake/proof-of-stake-and-scalability-2ecaa8fd5d7c (accessed on 10 March 2019).










| Entity | Provider | Healthcare Planer | Business Associate | Other | Total | |
|---|---|---|---|---|---|---|
| Year | ||||||
| 2009 | 14 | 1 | 3 | 0 | 18 | |
| 2010 | 134 | 21 | 44 | 0 | 199 | |
| 2011 | 137 | 20 | 42 | 1 | 200 | |
| 2012 | 155 | 22 | 36 | 4 | 217 | |
| 2013 | 199 | 18 | 56 | 5 | 278 | |
| 2014 | 202 | 71 | 41 | 0 | 314 | |
| 2015 | 196 | 62 | 11 | 0 | 269 | |
| 2016 | 257 | 51 | 19 | 0 | 237 | |
| 2017 | 288 | 52 | 19 | 0 | 259 | |
| Total | 1582 | 318 | 271 | 10 | 2181 | |
| Type | Public Blockchain | Private Blockchain | Consortium Blockchain | |
|---|---|---|---|---|
| Facts | ||||
| Definition | All participant can read, write, monitor, transact, download and start running a public node. | Instead of allowing anyone to control and participate in the verification, some specific number of nodes are selected. | Owner of the blockchain has the right to make rules and other terminologies. | |
| Cost | High | Medium | Low | |
| Security | High | Medium | Medium | |
| Privacy | Medium | High | High | |
| Transaction rate | Slower | Faster | Fastest | |
| Architecture | Decentralized | Partially decentralized | Partially decentralized or centralized | |
| Example | Bitcoin, Ethereum, Litcoin | R3, Corda, B3i | Monax, Multichain | |
| Use sector | Cryptocurrency | Government | Organization | |
| Schemes | Chen [69] | Fan [61] | Zhang [28] | Tseng [70] | Ryu [65] | Proof of Familiarity | |
|---|---|---|---|---|---|---|---|
| Features | |||||||
| Blockchain architecture | Public | Public | Public | Private | Public | Consortium | |
| Off-chain data | No | No | No | No | No | Yes | |
| Proposed new consensus | No | Yes | Yes | No | No | New | |
| Implementation cost | High | High | High | Medium | Low | Low | |
| Purpose of use | Data | Data | No | Drug supply | Data | Decision-making | |
| Entities | Individual Familiarity Index (IFI) | Considering Factors for Individual Familiarity Index (IFI) Calculation |
|---|---|---|
| doctor 1 (D1) | 0.25 | job experience time (0.10), treatment success rate (0.15) |
| doctor 2 (D2) | 0.50 | job experience time (0.30), treatment success rate (0.20) |
| doctor 3 (D3) | 0.85 | job experience time (0.35), treatment success rate (0.50) |
| cured patient 1 (Cp1) | 0.45 | treatment experience time (0.20), current condition (0.10), experience of disease (0.15) |
| cured patient 2 (Cp2) | 0.90 | treatment experience time (0.30), current condition (0.30), experience of disease (0.30) |
| cured patient 3 (Cp3) | 0.60 | treatment experience time (0.30), current condition (0.25), acquaintance with disease (0.05) |
| insurance company 1 (Ic1) | 0.85 | settlement time (0.60), cover amount (0.25) |
| insurance company 2 (Ic1) | 0.50 | settlement time (0.20), cover amount (0.30) |
| Algorithm | PoF (Proposed) | PoW [35] | PoS [38] | PBFT [37] | Ripple [39] | Tendermint [40] | |
|---|---|---|---|---|---|---|---|
| Fact | |||||||
| Node management | Permissioned | Open | Both | Permissioned | Open | Permissioned | |
| Transmission rate | Low | Low | Medium | High | High | Medium | |
| Energy consumption | Low | High | Medium | Low | Low | Low | |
| Scalability | High | Low | Low | Medium | Medium | Low | |
| Finality process | Immediate | Probabilistic | Probabilistic | Immediate | Probabilistic | Probabilistic | |
| Adversary tolerated Power | 0.75% diversity rate | < = 25% Computing Power | < 51% stake | < 33% Voting power | < 20% faulty nodes in UNL | < 33.3% Voting power | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, J.; Onik, M.M.H.; Lee, N.-Y.; Ahmed, M.; Kim, C.-S. Proof-of-Familiarity: A Privacy-Preserved Blockchain Scheme for Collaborative Medical Decision-Making. Appl. Sci. 2019, 9, 1370. https://doi.org/10.3390/app9071370
Yang J, Onik MMH, Lee N-Y, Ahmed M, Kim C-S. Proof-of-Familiarity: A Privacy-Preserved Blockchain Scheme for Collaborative Medical Decision-Making. Applied Sciences. 2019; 9(7):1370. https://doi.org/10.3390/app9071370
Chicago/Turabian StyleYang, Jinhong, Md Mehedi Hassan Onik, Nam-Yong Lee, Mohiuddin Ahmed, and Chul-Soo Kim. 2019. "Proof-of-Familiarity: A Privacy-Preserved Blockchain Scheme for Collaborative Medical Decision-Making" Applied Sciences 9, no. 7: 1370. https://doi.org/10.3390/app9071370
APA StyleYang, J., Onik, M. M. H., Lee, N.-Y., Ahmed, M., & Kim, C.-S. (2019). Proof-of-Familiarity: A Privacy-Preserved Blockchain Scheme for Collaborative Medical Decision-Making. Applied Sciences, 9(7), 1370. https://doi.org/10.3390/app9071370







