Abstract
Ginger in its many forms, from juices of the fresh rhizome, to ginger powder and ginger essential oil, is growing in popularity for claimed universal health benefits. Nevertheless, and contrarily to the common notion of the public, ginger is not devoid of side effects, especially interactions with other drugs, and many of the claimed benefits remain to be substantiated. This work presents a comprehensive revision of the current state of the art on ginger pharmacokinetics and bioavailability, interaction with active pharmaceutical ingredients, raising awareness of the risks of uncontrolled ginger consumption. A second section of the work described the verified actions of various extracts of ginger, or of their main active ingredients, gingerols, based mainly on data obtained from controlled clinical trials. Finally, the last section is devoted to innovative technological solutions to improve the bioavailability of gingerols and ginger extracts that are expected to ultimately lead to the development of more consumer-compliant products.
1. Introduction
1.1. Ginger in History and in the Present Day
Ginger is long known to man. Its history dates back over 5000 years when the Indians and ancient Chinese cultivated it as a tonic root for all ailments. The plant, of scientific name Zingiber officinale, is originally from southern parts of ancient China and from there it spread to India, Maluku Islands (so-called Spice Islands), the rest of Asia and West Africa. Ginger first appeared in Europe in the 1st century, from Roman trade with India. It was extensively used by the Romans, falling out of use during the middle ages [1]. Ginger has been used, since old times, in a variety of traditional medicines, including Chinese, Ayurvedic (from India) and Unani (Perso-Arabic) [2]. In the ayurvedic tradition, ginger is considered a universal medicine, but it is used with stronger incidence in the treatment of nausea and indigestion [3].
In the present day, ginger is used both in food and as a herbal medicine. The World Health organisation (WHO) monograph on ginger compiles the results on anti-emetic, cholagogic and anti-inflammatory properties available in a variety of sources, including the pharmacopeias of Japan, China, Thailand, UK, Europe and Africa [4]. In food, ginger is most commonly used as a spice. The rhizomes are dried and ground to a powder that has flowery-spicy taste and aroma. Both ginger spice and ginger essential oil are recognised as food additives by the US Food and Drug Administration (FDA) and they have been granted the GRAS status (“Generally Recognised as Safe”) [5]. Other ginger-derived food products include ginger pickles, ginger preserves, ginger beer and juices made from fresh ginger. Candied ginger is eaten per se or incorporated into chocolates and confectionery. Various extracts are added to yogurt and other dairy products. The use of ginger as a dietary supplement and functional food is a growing trend. Ginger is one of top-selling herbs in the market, estimated to have an annual sales growth of 6.5% and to reach a value 4.18 billion UD dollars by 2022. The consumers’ market is predicted to expand even faster, at an estimated rate of 7.5% every year until 2022 [6].
1.2. Ginger Chemistry
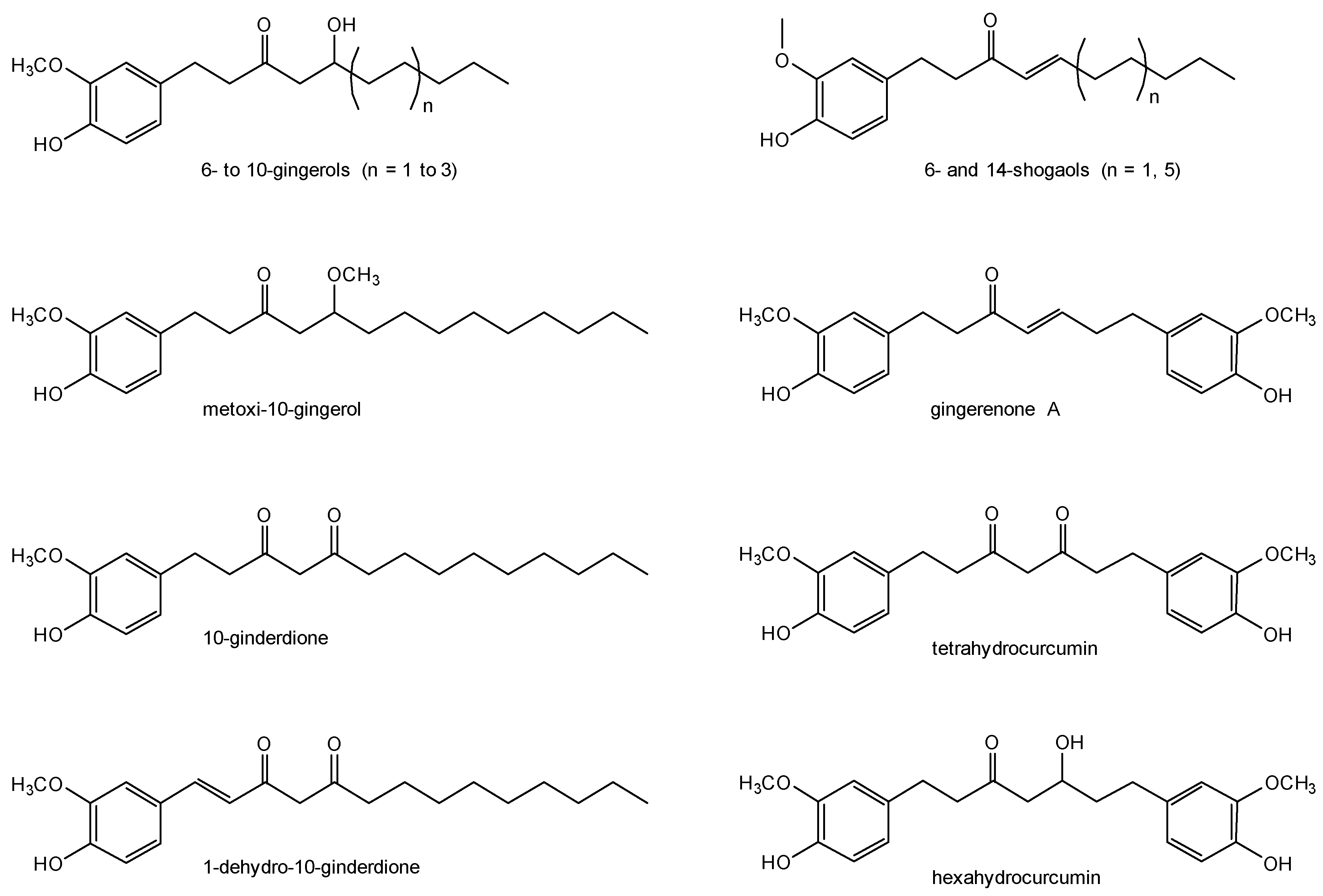
Ginger contains starch as the most abundant ingredient, making 40–60% (m/m) of the dry rhizome. The contents in protein, lipids and fiber vary according to the cultivars and the different maturity stages: the percentage of the crude protein is 6.2–19.8%, lipids 5.7–14.5% and crude fibers 1.1–7.0%. The active components are obtained by extraction. This process can be done using organic solvents that, once dried, afford the oleoresin in yields of 4–7.5% (m/m), or by steam distillation that affords obtain ginger oil [7]. The extracts contain a large variety of compounds, of which at least 115 have already been identified and that include gingerols, shogaols, β-carotene, capsaicin, caffeic acid, curcuminoids and salicylate [8]. Gingerols are the most abundant active components in fresh ginger, whereas in dry ginger the shogaols are more abundant; this happens because the heat associated with drying degrades gingerols into shogaols [9]. The family of gingerols is quite extensive, with up to 31 identified in fresh ginger so far [10]. Besides 4-, 6-, 8-, and 10-gingerols, as well as 6- and 14-shogaols, a number of other bioactive components are known, mainly for their anti-inflammatory activity; these include methoxy-10-gingerol, 10-gingerdione, 1-dehydro-10-gingerdione, hexahydrocurcumin, tetrahydrocurcumin, and gingerenone A (Figure 1) [11,12].
Figure 1.
Structural representation of the most relevant bioactive compounds occurring in ginger.
6-gingerol, with the IUPAC name (S)-5-hydroxy-1-(4-hydroxy-3-methoxyphenyl)-3-decanone, is the main pungent and bioactive component of ginger. 6-gingerol is soluble in ethanol, benzene, ether, chloroform, methanol (1 mg/mL), and DMSO and insoluble in water. The log P of 6-gingerol is predicted to lie between 2.48 and 3.62, and it has been provisionally categorised as a BCS class I compound, that is, a compound with low solubility and low permeability (BCS stands for Biopharmaceutical Classification System) [13]. Extraction of 6-gingerol is usually carried out by chromatographic purification of extracts obtained by maceration of fresh ginger with different solvents like methanol [14], hexane [15] or acetone. The yields of these processes are, however, very low, lying between 0.1 and 0.6%. Furthermore, the use of organic solvents makes the product inadequate for food applications. Attempts to obtain gingerol with supercritical CO2 [16,17] and subcritical water [18] are reported, but these methods afford, rather than pure 6-gingerol, a mixture of 6, 8- and 10-gingerols, as well as 6-shogaol. Pure 6-gingerol can be obtained by total synthesis, involving more than ten steps and various precursors [19].
2. Pharmacology of Ginger
2.1. Pharmacokinetics from Oral Intake
The amount of ginger active components that reach the bloodstream following oral intake is relatively low due to losses during gastroenteric absorption. Furthermore, gingerols, like most orally administered apolar phenolic compounds, undergo glucuronide and sulfate conjugation that takes place primarily in the intestinal mucosa and secondarily in the liver and other tissues [20]. This way, plasma components of ginger are typically found in the conjugated forms rather than the free ones. This was demonstrated by a study on mice treated with 250 mg/kg of ginger extract. The study monitored the main active components of ginger in the free form, revealing very low seric levels [21]. Also remarkable are the different absorption kinetics observed for each one of the components. The 6-gingerol plasma peak was observed at roughly two hours of administration (but with a large error, 27.18 ± 38.43 μg/L), while 10-gingerol peaked at 30 min (55.95 ± 31.61 μg/L) and 8-gingerol was practically undetected; 6-shogaol peaked at 10 min with only 4.04 ± 5.37 μg/L.
Pharmacokinetics of ginger in humans was investigated using an escalation study with 27 healthy subjects. A single oral dose of ginger extracts was administered, with concentrations standardised to 5% of total gingerols and ranging from 100 mg to 2.0 g. The subjects were monitored for 6-, 8-, 10-gingerols and 6-shogaol [22]. The compounds were rapidly absorbed, with a tmax of 55 to 65.6 min (range: 45–120 min) and elimination half-lives (t1/2β) of 75 to 120 min at the highest dose, 2.0 g. No free 6-, 8-, 10-gingerols or 6-shogaol were observed in the plasma, in agreement with the studies performed with mice. Instead, their circulating metabolites were detected, mostly glucuronides and/or sulphates (Table 1).

Table 1.
Pharmacokinetic parameters for the main active components of ginger.
It should be noted that only 6-gingerol conjugates were detectable in subjects taking doses below 1.0 g, and for this reason, the low doses are not listed in the Table 1. The AUC values for the doses of 250 and 500 mg of ginger presented low values, of 2.8 and 5.3 μg·min·mL−1 respectively. For the two lowest doses of ginger tested, 100 and 250 mg, the Cmax of 6-gingerol conjugates had values of 0.3 and 0.4 μg/mL, respectively. Ginger was well tolerated in all subjects.
Ginger metabolism and excretion is still not fully determined. Studies using 6-gingerol as a model show that this molecule is extensively metabolised in the liver by enzymes of the uridine diphosphate glucuronosyltransferase family to form glucuronide conjugates [20,23]. Roughly, half of the administered 6-gingerol is excreted through the bile as a glucuronide, with only 2–3% appearing in the urine in the free form [20]. Other metabolites, formed by hepatic oxidation and eliminated in the urine, include 9-hydroxy-6-gingerol, vanillic acid, ferulic acid, (S)-(+)-4-hydroxy-6-oxo-8-(4-hydroxy-3-methoxyphenyl)octanoic acid, and 4-(4-hydroxy-3-methoxyphenyl)butanoic acid.
2.2. Safety and Interactions
Ginger is a very safe herbal medicine, able to be used even in pregnancy [24,25]. Nevertheless, it is not completely free from side effects (see Section 2.2.1) and it also displays a long list of interactions with other compounds, from pharmaceutical active ingredients (APIs) to vitamins and nutrients. In these interactions, ginger acts mostly as a bioenhancer, that is, an agent that enhances the bioavailability of other substances, as detailed in Section 2.2.2. This effect may be associated with the presence of piperine-like compounds in ginger [26]. Piperine, the pungent compound in black pepper, is a well-known bioenhancer. However, ginger interactions with APIs are not fully predictable and reduction of bioavailability is also reported, as described in Section 2.2.3.
2.2.1. Adverse Effects
Ginger consumption rarely induces side effects. Gastrointestinal complications are reported in a clinical trial with patients taking 2 g of ginger powder per day, but the incidence is in similar numbers in the test group and the placebo group [27].
Anticoagulant activity with platelet inactivation may occur with very high doses of ginger. Aggregation of platelets was reduced by roughly one third in patients with a previous history of myocardial infarction taking a daily dose of 10 g ginger powder [28]. There is no action on platelet aggregation at daily doses of 4 g or less [28,29,30].
2.2.2. Bioavailability Enhancement with Ginger
The most comprehensive list of bioenhancing interactions of ginger with other compounds is available in a patent [31]. Ginger aqueous and methanolic extracts are claimed to increase the bioavailability of various APIs by up to 1.5 folds, as listed in Table 2.

Table 2.
Maximal enhancement of the bioavailability of APIs, vitamins and amino acids claimed to occur when ginger extracts are taken concomitantly [31].
A bioenhancing effect is also reported for ginger oleoresin. When given to mice at a dose of 30 mg/kg of body weight, ginger oleoresin enhanced the bioavailaibility of the antiviral drug atazanvir and accelerated its absorption [32].
2.2.3. Ginger May Lower Bioavailability of Some Substances
The interaction of ginger with the immunosuppressant drug cyclosporine was studied in mice under different conditions of administration, leading to distinct results. The administration of ginger juice (5 mL/kg), both at the same time and two hours before oral administration of cyclosporine led to reduction in the bioavailability of this API, with reductions of 63% and 40% in the respective AUC [33]. Note that these results are in contrast with the claims in the patent of Qazi et al. [31], in which 30–35 mg/kg ginger extract in co-administration with cyclosporine is said to afford a bioavailability increase of 116% (measurements done in plasma over 24 h).
The variability of the reported results allows postulating that high doses of ginger are required for it to feature an enhancing action on the absorption of APIs. In turn, an antagonistic action with other substances may occur when ginger is taken concomitantly in low doses, such as those arising from juices and infusions.
2.3. Biological Activity
Ginger is indicated in Ayurvedic, Chinese and Unani traditional medicines for a large variety of pathologies and ailments, often being considered a panacea or universal medicine. Most of this knowledge is, however, empirical, and only in the latest decades has clinical trial-based evidence been gathered on the activities of ginger. This section presents a selection of the most relevant results coming from clinical trials.
2.3.1. Anti-Inflammatory and Analgesic Activities
The anti-inflammatory activity of ginger was demonstrated in a clinical trial monitoring pro-inflammatory enzymes such as cyclo-oxygenase (COX) and lipo-oxygenases (LOX-5, LOX-12 and LOX-15). Following the daily intake of 2 g of ginger powder for 28 days, the lower activity of these enzymes was confirmed by reductions in the levels of the pro-inflammatory substances they produce, particularly eicosanoids and prostaglandin E2 (PGE2) [27].
In clinical terms, the effect of ginger is more of a long-term one than an immediate one (as observed with non-steroid anti-inflammatory APIs). A clinical study measured the effect of ginger reduction of pain, swelling and mobility on 24 healthy male volunteers subject to eccentric muscle exercise to generate acute inflammation and muscle pain. 24 h and 48 h after the strong exercise, volunteers were given 2 g of ginger or a placebo. The pain and swelling, measured 45 min after the intake, were similar in the ginger group and the placebo group; interestingly, the same measurements were repeated 24 h after ginger ingestion and improvements were observed. This study suggests ginger may attenuate the day-to-day progression of muscle inflammation and the associated pain [34]. Another study compared the effect of 2 g of either raw or heat-treated ginger on two groups of volunteers (34 and 40 men, respectively) and again reduction of pain was observed three days after the exercise, with values of 25% for the raw ginger group and 23% for the heat-treated ginger group [35]. As mentioned in Section 1.2., gingerols are sensitive to heat, and thus the lower activity observed in this study for the second group is due to the lower content in gingerols. This study confirms that, in humans, gingerols are involved in the anti-inflammatory and analgesic actions. For pure 6-gingerol, both activities are already demonstrated in mice models [36].
Clinical trials investigating osteoarthritis (OA) pain management also show incoherent results for ginger, which may be associated with the different composition of the tested formulations. A trial employing an unknown composition of ginger hydroxymethoxyphenols at a daily dose of 170 mg for three weeks showed no improvement in motion-derived joint pain (test group with n = 56) [37]. In turn, another study with 40 patients taking, over a month, a daily dose of 30 mg of ginger extract (by cold ethanol percolation, 30 mg of extract corresponding to 1 g of dry ginger powder) showed a significant reduction (>50%) in the pain associated with motion of the affected joints [38]. Another study with a larger number of patients (n = 103) taking capsules with whole ginger powder at daily doses of 0.25 g for six weeks also showed reduction of knee pain (average of c.a. 30%), which was more significant in patients having OA for less than three years [39].
The use of ginger as an anti-inflammatory and analgesic agent in migraine was reported in 1990, in a single-patient case study. The patient consumed 1.5 to 2 g of powdered ginger per day (doses of 500 mg at four-hour intervals) and reported the abortion of migraine 30 min after the first dose of 500 mg [40]. The anti-neuroinflammatory activity of ginger was confirmed by in vitro studies on microglia cells [41] and it is associated mainly with the component 10-gingerol, rather than 6-gingerol [42].
2.3.2. Anti-Emetic Activity
The anti-emetic activity of ginger is best documented in cases of pregnancy, with various clinical trials showing its practical utility [43]. In eleven out of the twelve trials conducted, ginger powder, at a daily dose ≥1 g, was able to reduce or eliminate hyperemesis gravidarium [44] and the episodes of nausea vomiting associated with pregnancy [45,46,47,48,49,50,51,52,53,54].
The use of ginger as an antiemetic is also reported for motion and post-operative sickness cases, but studies are somewhat scarcer. Regarding motion sickness, the most relevant trial was conducted on a group of 80 navy cadets, with 40 taking 1 g of ginger powder in a single dose and the other 40 taking placebo. The cadets were monitored for 4 h following ingestion. The ginger-treated group had no emesis and exhibited a strong reduction of symptoms, such as cold sweating and vertigo, in comparison with the placebo group; note that in the placebo group there were also a few incidences of vomiting [55,56]. Ginger’s motion-sickness preventive action in individuals with extreme or very high susceptibility to this condition was demonstrated by two studies which resorted to motion-induced sickness, that is, the volunteers were placed in tilted rotating chairs [57,58]. In one of these, 12 young volunteers were given 1.9 g of ginger powder, while another 12 received dimenhydrinate (an anti-histamine and CNS depressant that blocks vertigo impulses). Results show ginger is superior to dimenhydrate in preventing the gastrointestinal symptoms of motion sickness [57]. The second study followed double-blind, randomised, placebo-controlled protocols to compare the action of two doses of ginger. 1 g of ginger powder was shown to be as effective as 2 g of ginger powder in reducing motion-induced nausea, with both doses being significantly more effective than the placebo [58]. A third trial, sponsored by NASA, tested the effects of ginger on healthy volunteers, that is, people not particularly prone to motion sickness. A dose of 1 g of ginger powder was compared with 0.6 g of scopolamine (an anti-emetic API) and the effectiveness was measured by the ability of the volunteers to tilt their head (without utter discomfort) while they were spinning on the rotating chair. The results of the group taking ginger (n = 8) were poor, volunteers performing very close to the placebo group; moreover, the ginger group scored much worse than that of scopolamine (also with n = 8) [59]. Nevertheless, this form of measuring the resilience to sickness may not be the most clinically relevant.
In post-operative sickness, 1 g of ginger (taken before the operation) was demonstrated by two case studies to reduce the incidence and severity of nausea to roughly half of that observed in the placebo group [60,61]. Ginger may also be useful in combination therapy with conventional antiemetic drugs to prevent acute nausea resulting from chemotherapeutic drugs, as demonstrated by a large scale (n = 576) double-blind study [62]. Also noteworthy is a single-blind, randomised, controlled, cross-over study, conducted in two oncology clinics on 60 women taking chemotherapeutic drugs for breast cancer and treated with ginger oil, inhaled continuously from an aromatherapy necklace. The results of this study showed that patients, after the fifth day of treatment with ginger oil, had higher gastrointestinal comfort and were thus able to ingest food in amounts that were closer to their daily energetic requirements than those of the placebo group (note: these were wearing a necklace with matching odour but no ginger oil) [63].
2.3.3. Ginger in Dysmenorrhea
Dysmenorrhea is a perimenstrual female dysfunction characterised by low abdominal or pelvic pain and often accompanied by back pain and nausea. As described in the previous subsections, ginger combines analgesic and anti-emetic activities, thus being very suited for the management of this condition. The beneficial action of ginger in dysmenorrhea is demonstrated by six clinical trials [64] that evidence its overall effectiveness, at different doses, in significantly reducing pain when compared with a placebo. In one of these trials, the tested daily dose was quite low—150 mg per day of ginger powder, taken for five consecutive days—and still there was a reduction of both severity and duration of pain in the test group (n = 59) [65]. Another two trials reported that 1 g of ginger powder (taken along the day in four doses of 250 mg) reduced the severity of pain as effectively as NSAIDs, namely mefenamic acid (3–4 × 250 mg per day) [66,67] and ibuprofen (4 × 400 mg per day) [67]. Finally, another trial reports a wide set of benefits from the intake of 2g of ginger per day, which include relief of cramping, colicky pain in lower abdomen, nausea, and even diarrhoea [68].
2.3.4. Anti-Diabetes Activity
The benefits of ginger intake in the management of type-2 diabetes seem to be progressive, that is, better results are achieved when ginger is taken daily over a prolonged period of time. A two-month length clinical trial in a group of 32 patients taking 2 g of ginger powder daily showed reduction of the insulin resistance index (HOMA model) but not of the fasting plasma glucose (FPG) levels [69]. Another trial on 35 patients taking 1.6 g ginger daily for three months showed that ginger did reduce FPG levels besides increasing the sensitivity to insulin [70,71]. Also noteworthy is that this activity appears to be dose-dependent: two trials studying the effect of a ginger daily dose of 3 g, show faster onsets of hypoglycaemic activity, starting from one month in one study [72] or two months in the other [73]. The intake of two grams of ginger daily also helps reduce chronic inflammation associated with diabetes by lowering the levels of C-reactive protein [70,74] (but note that this does not occur with only 1 g daily [75]).
In dialysis patients, the hypoglycemic effect of ginger is even more noteworthy, being observed at lower doses and shorter times of supplementation. A trial on patients subjected to peritoneal dialysis taking 1 g ginger powder for 10 weeks showed a reduction in FPG of roughly 20% in the ginger group (n = 18), a value significantly different from that of the placebo group (also with n = 18) [75].
2.3.5. Cancer Preventive Activity
A small clinical trial using only 9 participants in the test group investigated the ability of ginger powder, at a daily dose of 2 g for 28 days, to prevent the development of colon cancer. All the participants had increased risk for this kind of cancer, previously determined by their medical background, and the action of ginger was measured by making a post-treatment sigmoidoscopy with collection of intestinal tissue for immunohistochemical studies. The colon crypts, tube-like formations that line the colon and produce mucus, were measured to determine their content in cancer and apoptosis biomarkers. Results showed that the treatment with ginger restored the levels of these biomarkers back to ‘normality’, that is to values typical of healthy individuals [76].
The cancer preventive action of ginger also seems to be associated with reduction of inflammation, which is commonly linked with cancer. In a trial with 10 participants having increased risk for colon cancer, the intake of 2 g of ginger powder daily for 28 days reduced significantly the expression of the pro-inflammatory enzyme COX-1 in the intestinal wall (biopsy extraction) in comparison with the placebo group (n = 11) [77]. Also noteworthy is the fact that the same dose was studied, in parallel, on healthy volunteers (that is, with no risk for colon cancer) and ginger did not reduce their levels of COX-1 [77].
2.3.6. Equivocal Activities
To fully comply with its traditional reputation of panacea, ginger should be able to provide cure against practically all ailments. Nevertheless, it lies far from it and a few studies are already demonstrating the equivocal activities on conditions such as IBS, fatty liver and obesity.
A pilot study on irritable bowel syndrome (IBS) patients who were randomly consuming placebo or ginger powder at daily doses of 1 g or 2 g for 28 days, the ginger groups (n = 15) did not show better effects than the placebo one [78].
Similarly, in non-alcoholic fatty liver disease (NAFLD), no significant reduction of liver fibrosis, the main pathophysiologic alteration of the disease, was observed between the ginger group and the placebo group (both with n = 22); patients in the test group were taking 2 g of ginger powder per day for 3 months [79].
Ginger also failed to demonstrate any slimming or appetite reduction action. A daily dose of 2 g of ginger powder for three months caused no changes in body mass, body fat and total energy and macronutrients intake in a group of 40 women in regard to the control (40 women taking placebo) [80,81].
3. Encapsulation of Ginger
3.1. Dispersion and Micronisation
Encapsulation of ginger essential oil or ginger oleoresin by forming a dispersion into a polymer or other carrier agent, with subsequent drying and micronisation (commonly in one step, by spray-drying), is a common solution for the protection of the active ingredients against volatilisation or against degradation by heat and light. In addition, liquid and semi-solid extracts are turned into powdered solids which are easier to store and handle.
In the case of ginger essential oil, encapsulation can be achieved with various agents including inulin, whey protein (WP) [82] and a WP/maltodextrin blend [83]. For ginger oleoresin, various methods and dispersing agents are described by Janayudin et al. [84], including chitosan and blends of maltodextrin with caseinate or arabic gum. Chitosan [85] and chitosan-alginate mixtures [86] can also be used to form microcapsules with the oleoresin of red ginger, a subspecies of ginger containing higher amounts of 10-gingerol, 6-gingerdiol and its acetylated derivatives [87].
3.2. Liposomal Ginger
Some liposomal ginger products are available on the market, namely a combination of ginger, curcumin and docosahexaenoic acid (an omega-3 fatty acid) named ‘Micelle Liposomal Curcumin Gold’ [88] and another comprising turmeric, lemon and ginger, called ‘Synchro Gold Lemon Ginger’ [89]. Inclusion of a lipophilic drug into liposomes aims usually at increasing its bioavailability, which, in the case of the two marketed herbal supplements, would refer to oral absorption, given that these are to be taken by this route. Nevertheless, to the best of our knowledge, the effect of liposomes on the oral bioavailability of the active components from ginger remains yet to be demonstrated by any in vivo studies or clinical trials.
Available research into the benefits of liposomes for ginger biotechnological applications includes the evaluation of stability and dermal bioavailability. Inclusion of ginger extract into nanoliposomes was shown to help preserve its antioxidant properties [90] and its skin permeability, measured on an in vitro goat skin model [91].
4. Novel Drug Delivery Technologies Based on Ginger
4.1. Ginger-Derived Nanoparticles (GDPs)
Fresh ginger juice can be used to afford, by a controlled methodology [92,93,94], ginger-derived nanoparticles (GDPs) that are suitable for loading and carrying APIs or other compounds. GDPs from ginger contain lipids, mainly phosphatidic acids (41.9% of total lipids), digalactosyldiacylglycerol (27.4%) and monogalactosyldiacylglycerol (18.9%) [95], as well as a fair amount of RNA [94]. GDPs have, thus, an intrinsic immunomodulatory activity, inducing production of the cytokines IL-6 and IL-10 when incubated with macrophages. Furthermore, they are not destroyed in the stomach [94], and they are able to enter liver cells (hepatocytes) in mice [96], where they demonstrated a protective effect against alcohol-induced liver damage.
The high biocompatibility of GDPs and their ability to easily fuse with biological membranes owing to the high content in phosphatidic acids makes them excellent candidates for innovative biological therapies. Chronic diseases associated with genetic dysfunction, such as ulcerative colitis, can be treated by gene therapy or by knocking out a target gene using small interfering RNAs (siRNAs). SiRNAs are small double-strand sequences able to knock down specific genes, in this case CD98. GDPs loaded with siRNA-CD98 were tested both in vitro and in vitro as an innovative therapy for ulcerative colitis. In vitro studies on the RAW 264.7 and colon-26 cell lines show successful transfection, with distribution of the GDPs throughout the cells and inhibition of the expression of CD98 gene by roughly 20% in colon-26 cells and 50% in RAW cells. The GDPs have also good distribution in vivo, with studies on mice demonstrating that they have a preferential action (CD98 knock-out) on the ileum and the colon [95].
4.2. Ginger-Derived Nano-Vectors (GDNVs)
GDPs can be transformed into other kinds of carriers by extracting the lipids they contain and leaving the RNA behind. The extracted lipids form, by sonication, nano-sized vesicles that received the acronym of GDNVs. These new carriers are taken up by intestinal cells, as demonstrated in vitro on the Colon-26 and HT-29 human colon adenocarcinoma cell lines, and biocompatible as demonstrated by the lack of toxicity in vivo on mice. Furthermore, they act effectively as carriers for oral administration of the antitumoral drug doxorubicin and this therapy successfully inhibited tumor growth in a Colon-26 xenograft tumor mouse model [97].
5. Closing Remarks
Ginger is currently a very popular spice, transcending its original countries of use into the western societies, where the fusion of flavours and gastronomic influences is a growing trend. Ginger is also common in juice blends, infusions and even yogurt, bringing pungent, fresh and flowery notes to their aroma and flavour. While these foods are certain to please the eclectic consumer, they have no medicinal value, since the amount of ginger is practically neglectable. Ginger-based functional foods are, alas, a mere consumer’s hype.
As a medicinal herb, powdered ginger rhizome is available from a large variety of suppliers, in capsules containing approximately 500 mg of powder. The recommended daily doses vary between one and three capsules, which translate into doses of 500 to 1500 mg. According to the clinical studies revised in the present paper, these doses are useful in the prevention of motion sickness, which can be achieved with a single dose of 1 g, and also suitable for alleviation of dysmenorrhea-associated pain, with improvements starting after four days of treatment. However, it must be recalled that, in order for ginger to produce any of the multiple other benefits herein described, higher doses (2 or 3 g) are required.
Words of caution on the use of ginger as a medicinal herb are also in order, with particular highlight to its interference with other APIs, observed in mice. Ginger-API interactions are thus also presumed to occur in humans, although it remains to be ascertained as to which extent and at which doses. Also relevant is the fact that for the majority of ginger’s prescribed effects, a prolonged time of treatment is required, and this increases the risk of interactions whenever the patient needs to take other APIs during such time. Given that the ginger-API interactions occur mainly on the intestines, a proper encapsulation of ginger extracts should be able to prevent such interactions making it safer and improving its bioavailability. This area of application still requires further investigation, namely to quantify the increase in bioavailability and to verify whether interactions can indeed be prevented. With the growing interest of western societies in ginger as a natural medicine, in the next decades we can expect research to grow to deepen our knowledge on this herb and to find a plethora of novel, safer applications.
Funding
LAQV/REQUIMTE (project PEst C-QUI/UI0062/2019) is funded by Fundação para a Ciência e a Tecnologia (FCT, Portugal), the European Union, QREN, and European Fund for Regional Development (FEDER), through the programme COMPETE.
Acknowledgments
Thanks are due to Fundação para a Ciência e a Tecnologia (FCT, Portugal), European Union, QREN, European Fund for Regional Development (FEDER), through the programme COMPETE, for general funding (project PEst C-QUI/UI0062/2019).
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| API | Active Pharmaceutical Ingredient |
| GDP | Ginger-Derived nanoParticles |
| GDNV | Ginger-Derived Nano Vectors |
| HOMA | Homeostasis Model Assessment |
| IBS | Irritable Bowel Syndrome |
| IL | InterLeukin |
| NAFLD | Non-Alcoholic Fatty Liver Disease |
| NASA | National Aeronautics and Space Agency |
| NSAID | Non-Steroid Anti-Inflammatory Drug |
| RNA | RiboNucleic Acid |
| WP | Whey Protein |
References
- Bode, A.M.; Dong, Z. The Amazing and Mighty Ginger. In Herbal Medicine: Biomolecular and Clinical Aspects, 2nd ed.; Benzie, I.F.F., Wachtel-Galor, S., Eds.; CRC Press/Taylor & Francis: Boca Raton, FL, USA, 2011. [Google Scholar]
- Ali, B.H.; Blunden, G.; Tanira, M.O.; Nemmar, A. Some physico-chemical, pharmacological and toxicological properties of ginger (Zingerber officinale)—A review. Food Chem. Toxicol. 2008, 46, 409–410. [Google Scholar] [CrossRef]
- Tapsell, L.C.; Hemphill, I.; Cobiac, L.; Patch, C.S.; Sullivan, D.R.; Fenech, M.; Roodenrys, S.; Keogh, J.B.; Clifton, P.M.; Williams, P.G.; et al. Health benefits of herbs and spices: The past, the present, the future. Med. J. Aust. 2006, 185, S4–S24. [Google Scholar]
- WHO. WHO Monographs on Selected Medicinal Plants—Volume 1. WHO Essential Medicines and Health Products Information Portal; WHO: Geneva, Switzerland, 2018. [Google Scholar]
- US Food and Drug Administration. CFR—Code of Federal Regulations, Title 21—Food and Drugs, Chapter I—Food and Drug Administation, Subchapter B—Food for Human Consumption (continued), Part 182—Substances Generally Recognized as Safe, Subpart A—General Provisions: Sec. 182.20. Available online: https://www.ecfr.gov/cgi-bin/text-idx?SID=dfc2dae5c6f384d423719ba6d29c7c1b&mc=true&node=se21.3.182_120&rgn=div8 (accessed on 28 January 2019).
- Transparency Market Research. Ginger Market (Form—Fresh, Dried, Pickled, Preserved, Crystallized, and Powdered; Distribution Channel—Modern Grocery Retail, Traditional Grocery Retail, and Non-Grocery Retail; Application—Culinary, Soups and Sauces, Snacks & Convenience Food, Bakery Products, Alcoholic Beverages, Non-Alcoholic Beverages, and Chocolate and Confectionery)—Global Industry Analysis, Size, Share, Growth, Trends and Forecast 2017—2022. Available online: https://www.transparencymarketresearch.com/ginger-market.html (accessed on 28 January 2019).
- Pratap, S.R.; Gangadharappa, H.V.; Mruthunjaya, K. Ginger: A Potential Neutraceutical, An Updated Review. Int. J. Pharmacogn. Phytochem. Res. 2017, 9, 1227–1238. [Google Scholar] [CrossRef]
- Schulick, P. Ginger: Common Spice and Wonder Drug, 3rd ed.; Hohm Press: Prescott, AZ, USA, 2012. [Google Scholar]
- Jolad, S.D.; Lantz, R.C.; Chen, G.J.; Bates, R.B.; Timmermann, B.N. Commercially processed dry ginger (Zingiber officinale): Composition and effects on LPS-stimulated PGE2 production. Phytochemistry 2005, 66, 1614–1635. [Google Scholar] [CrossRef] [PubMed]
- Jiang, H.; Solyom, A.M.; Timmermann, B.N.; Gang, D.R. Characterization of gingerol-related compounds in ginger rhizome (Zingiber officinale Rosc.) by high-performance liquid chromatography/electrospray ionization mass spectrometry. Rapid Commun. Mass Spectrom. 2005, 19, 2957–2964. [Google Scholar] [CrossRef] [PubMed]
- Kiuchi, F.; Shibuya, M.; Sankawa, U. Inhibitors of Prostaglandin Biosynthesis from Ginger. Chem. Pharm. Bull. 1982, 30, 754–757. [Google Scholar] [CrossRef]
- Koh, E.M.; Kim, H.J.; Kim, S.; Choi, W.H.; Choi, Y.H.; Ryu, S.Y.; Kim, Y.S.; Koh, W.S.; Park, S.Y. Modulation of macrophage functions by compounds isolated from Zingiber officinale. Planta Med. 2009, 75, 148–151. [Google Scholar] [CrossRef] [PubMed]
- Waldmann, S.; Almukainzi, M.; Bou-Chacra, N.A.; Amidon, G.L.; Lee, B.-J.; Feng, J.; Kanfer, I.; Zuo, J.Z.; Wei, H.; Bolger, M.B.; et al. Provisional Biopharmaceutical Classification of Some Common Herbs Used in Western Medicine. Mol. Pharm. 2012, 9, 815–822. [Google Scholar] [CrossRef]
- Johji, Y.; Michihiko, M.; Rong, H.Q.; Hisashi, M.; Hajime, F. The Anti-Ulcer Effect in Rats of Ginger Constituents. J. Ethnopharmacol. 1988, 23, 299–304. [Google Scholar] [CrossRef]
- Priyarani, M.; Padmakumari, K.P.; Sankariyutty, B.; Lijocherian, O.; Nisha, V.M.; Raghu, K.G. Inhibitory potential of ginger extracts against enzymes linked to type 2 diabetes, inflammation and induced oxidative stress. Int. J. Food Sci. Nutr. 2011, 62, 106–110. [Google Scholar] [CrossRef] [PubMed]
- Yonei, Y.; Ohinata, H.; Yoshida, R.; Shimizu, Y.; Yokoyama, C. Extraction of Ginger Flavor with Liquid or Supercritical Carbon Dioxide. J. Supercrit. Fluids 1995, 8, 156–161. [Google Scholar] [CrossRef]
- Salea, R.; Veriansyah, B.; Tjandrawinata, R.R. Optimization and Scale-up Process for Supercritical Fluids Extraction of Ginger Oil from Zingiber Officinale Var. Amarum. J. Supercrit. Fluids 2016, 120, 285–294. [Google Scholar] [CrossRef]
- Švarc-Gajić, J.; Cvetanović, A.; Segura-Carretero, A.; Linares, I.B.; Mašković, P. Characterisation of Ginger Extracts Obtained by Subcritical Water. J. Supercrit. Fluids 2016, 123, 92–100. [Google Scholar] [CrossRef]
- Solladié, G.; Ziani-Chérif, C. Total Synthesis of Natural Gingerols, the Three Active Principles of Ginger. J. Org. Chem. 1993, 58, 2181–2185. [Google Scholar] [CrossRef]
- Nakazawa, T.; Ohsawa, K. Metabolism of [6]-gingerol in rats. Life Sci. 2002, 70, 2165–2175. [Google Scholar] [CrossRef]
- Mukkavilli, R.; Yang, C.; Tanwar, R.S.; Ghareeb, A.; Luthra, L.; Aneja, R. Absorption, Metabolic Stability, and Pharmacokinetics of Ginger Phytochemicals. Molecules 2017, 22, 553. [Google Scholar] [CrossRef]
- Zick, S.M.; Djuric, Z.; Ruffin, M.T.; Litzinger, A.J.; Normolle, D.P.; Alrawi, S.; Feng, M.R.; Brenner, D.E. Pharmacokinetics of 6-gingerol, 8-gingerol, 10-gingerol, and 6-shogaol and conjugate metabolites in healthy human subjects. Cancer Epidemiol. Biomark. Prev. 2008, 17, 1930–1936. [Google Scholar] [CrossRef]
- Hoehle, S.I.; Pfeiffer, E.; Metzler, M. Glucuronidation of curcuminoids by human microsomal and recombinant UDP-glucuronosyltransferases. Mol. Nutr. Food Res. 2007, 51, 932–938. [Google Scholar] [CrossRef]
- Portnoi, G.; Chng, L.-A.; Karimi-Tabesh, L.; Koren, G.; Tan, M.P.; Einarson, A. Prospective comparative study of the safety and effectiveness of ginger for the treatment of nausea and vomiting in pregnancy. Am. J. Obstet. Gynecol. 2003, 189, 1374–1377. [Google Scholar] [CrossRef]
- Heitmann, K.; Nordeng, H.; Holst, L. Safety of ginger use in pregnancy: Results from a large population-based cohort study. Eur. J. Clin. Pharmacol. 2013, 69, 269–277. [Google Scholar] [CrossRef]
- Govindarajan, V.S. Ginger-chemistry, technology, and quality evaluation: Part 2. Crit. Rev. Food Sci. Nutr. 1982, 17, 189–258. [Google Scholar] [CrossRef]
- Zick, S.M.; Turgeon, D.K.; Vareed, S.K.; Ruffin, M.T.; Litzinger, A.J.; Wright, B.D.; Alrawi, S.; Normolle, D.P.; Djuric, Z.; Brenner, D.E. Phase II study of the effects of ginger root extract on eicosanoids in colon mucosa in people at normal risk for colorectal cancer. Cancer Prev. Res. 2011, 4, 1929–1937. [Google Scholar] [CrossRef]
- Bordia, A.; Verma, S.K.; Srivastava, K.C. Effect of ginger (Zingiber officinale Rosc.) and fenugreek (Trigonella foenumgraecum L.) on blood lipids, blood sugar and platelet aggregation in patients with coronary artery disease. Prostaglandins Leukot. Essent. Fatty Acids 1997, 56, 379–384. [Google Scholar] [CrossRef]
- Jiang, X.; Williams, K.M.; Liauw, W.S.; Ammit, A.J.; Roufogalis, B.D.; Duke, C.C.; Day, R.O.; McLachlan, A.J. Effect of ginkgo and ginger on the pharmacokinetics and pharmacodynamics of warfarin in healthy subjects. Br. J. Clin. Pharmacol. 2005, 59, 425–432. [Google Scholar] [CrossRef] [PubMed]
- Marx, W.; McKavanagh, D.; McCarthy, A.L.; Bird, R.; Ried, K.; Chan, A.; Isenring, L. The Effect of Ginger (Zingiber officinale) on Platelet Aggregation: A Systematic Literature Review. PLoS ONE 2015, 10, e0141119. [Google Scholar]
- Qazi, G.N.; Tikoo, L.C.; Gupta, A.K.; Ganjoo, K.S.; Gupta, D.K.; Jaggi, B.S.; Singh, R.P.; Singh, G.; Chandan, K.B.; Suri, K.A.; et al. Bioavailability Enhancing Activity of Zingiber Officinale Linn and Its Extracts/Fractions Thereof. Patent WO2003049753A1, 19 June 2003. [Google Scholar]
- Prakash, S.; Kherde, P.; Rangari, V. Bioenhancement effect of piperine and ginger oleo resin on the bioavailability of atazanvir. Int. J. Pharm. Pharm. Sci. 2015, 7, 241–245. [Google Scholar]
- Chiang, H.-M.; Chao, P.-D.L.; Hsiu, S.-L.; Wen, K.-C.; Tsai, S.-Y.; Hou, Y.-C. Ginger Significantly Decreased the Oral Bioavailability of Cyclosporine in Rats. Am. J. Chinese Med. 2006, 34, 845–855. [Google Scholar] [CrossRef]
- Black, C.D.; O’Connor, P.J. Acute effects of dietary ginger on muscle pain induced by eccentric exercise. Phytother. Res. 2010, 24, 1620–1626. [Google Scholar] [CrossRef]
- Black, C.D.; Herring, M.P.; Hurley, D.J.; O’Connor, P.J. Ginger (Zingiber officinale) reduces muscle pain caused by eccentric exercise. J. Pain. 2010, 11, 894–903. [Google Scholar] [CrossRef]
- Young, H.-Y.; Luo, Y.-L.; Cheng, H.-Y.; Hsieh, W.-C.; Liao, J.-C.; Peng, W.-H. Analgesic and Anti-Inflammatory Activities of [6]-Gingerol. J. Ethnopharmacol. 2005, 96, 207–210. [Google Scholar] [CrossRef]
- Bliddal, H.; Rosetzsky, A.; Schlichting, P.; Weidner, M.S.; Andersen, L.A.; Ibfelt, H.-H.; Christensen, K.; Jensen, O.N.; Barslev, J. A randomized, placebo-controlled, cross-over study of ginger extracts and Ibuprofen in osteoarthritis. Osteoarth. Cartil. 2000, 8, 9–12. [Google Scholar] [CrossRef]
- Haghighi, M.; Khalvat, A.; Toliat, T.; Jallaei, S. Comparing the effects of ginger (Zingiber officinale) extract and ibuprofen on patients with ostheoarthritis. Arch. Iran. Med. 2005, 8, 267–271. [Google Scholar]
- Zakeri, Z.; Izadi, S.; Bari, Z.; Soltani, F.; Narouie, B.; Ghasemi-rad, M. Evaluating the effects of ginger extract on knee pain, stiffness and difficulty in patients with knee osteoarthritis. J. Med. Plant Res. 2011, 5, 3375–3379. [Google Scholar]
- Mustafa, T.; Srivastava, K.C. Ginger (Zingiber Officinale) in Migraine Headache. J. Ethnopharmacol. 1990, 29, 267–273. [Google Scholar] [CrossRef]
- Jung, H.W.; Yoon, C.-H.; Park, K.M.; Han, H.S.; Park, Y.-K. Hexane fraction of Zingiberis Rhizoma Crudus extract inhibits the production of nitric oxide and proinflammatory cytokines in LPS-stimulated BV2 microglial cells via the NF-kappaB pathway. Food Chem. Toxicol. 2009, 47, 1190–1197. [Google Scholar] [CrossRef] [PubMed]
- Ho, S.-C.; Chang, K.-S.; Lin, C.-C. Anti-neuroinflammatory capacity of fresh Ginger is attributed mainly to 10-Gingerol. Food Chem. 2013, 141, 3183–3191. [Google Scholar] [CrossRef] [PubMed]
- Viljoen, E.; Visser, J.; Musekiwa, A. A systematic review and meta-analysis of the effect and safety of ginger in the treatment of pregnancy-associated nausea and vomiting. Nutr. J. 2014, 13, 20. [Google Scholar] [CrossRef]
- Fischer-Rasmussen, W.; Kjaer, S.K.; Dahl, C.; Asping, U. Ginger treatment of hyperemesis gravidarum. Eur. J. Obstet. Gynecol. Reprod. Biol. 1991, 38, 19–24. [Google Scholar] [CrossRef]
- Basirat, Z.; Moghadamnia, A.A.; Kashifard, M.; Sarifi-Razavi, A. The effect of ginger biscuit on nausea and vomiting in early pregnancy. Acta Med. Iran. 2009, 4, 51–56. [Google Scholar]
- Chittumma, P.; Kaewkiattikun, K.; Wiriyasiriwach, B. Comparison of the effectiveness of ginger and vitamin B6 for treatment of nausea and vomiting in early pregnancy: A randomized double-blind controlled trial. J. Med. Assoc. Thai 2007, 90, 15–20. [Google Scholar] [PubMed]
- Ensiyeh, J.; Sakineh, M.A. Comparing ginger and vitamin B6 for the treatment of nausea and vomiting in pregnancy: A randomised controlled trial. Midwifery 2005, 25, 649–653. [Google Scholar] [CrossRef]
- Keating, A.; Chez, R.A. Ginger syrup as an antiemetic in early pregnancy. Altern. Ther. Health Med. 2002, 8, 89–91. [Google Scholar]
- Mohammadbeigi, R.; Shahgeibi, S.; Soufizadeh, N.; Rezaiie, M.; Farhadifar, F. Comparing the effects of ginger and metoclopramide on the treatment of Pregnancy nausea. Pak. J. Biol. Sci. 2011, 14, 817–820. [Google Scholar] [PubMed]
- Ozgoli, G.; Goli, M.; Simbar, M. Effects of ginger capsules on pregnancy, nausea, and vomiting. J. Altern. Complement. Med. 2009, 15, 243–246. [Google Scholar] [CrossRef] [PubMed]
- Pongrojpaw, D.; Somprasit, C.; Chanthasenanont, M.D. A randomized comparison of ginger and dimenhydrinate in the treatment of nausea and vomiting in pregnancy. J. Med. Assoc. Thai 2007, 90, 1703–1709. [Google Scholar]
- Smith, C.; Crowther, C.; Willson, K.; Hotham, N.; McMillian, V. A randomized controlled trial of ginger to treat nausea and vomiting in pregnancy. Obstet. Gynecol. 2004, 103, 639–645. [Google Scholar] [CrossRef]
- Sripramote, M.; Lekhyananda, N. A randomized comparison of ginger and vitamin B6 in the treatment of nausea and vomiting of pregnancy. J. Med. Assoc. Thai 2003, 86, 846–853. [Google Scholar]
- Vutyavanich, T.; Kraisarin, T.; Ruangsri, R. Ginger for nausea and vomiting in pregnancy: Randomized, double-masked, placebo-controlled trial. Obstet. Gynecol. 2001, 97, 577–582. [Google Scholar] [CrossRef]
- Grøntved, A.; Hentzer, E. Vertigo-reducing effect of ginger root. A controlled clinical study. J. Otorhinolaryngol. Relat. Spec. 1986, 48, 282–286. [Google Scholar] [CrossRef]
- Grøntved, A.; Brask, T.; Kambskard, J.; Hentzer, E. Ginger root against seasickness: A controlled trial on the open sea. Acta otoralyngol. 1988, 105, 45–49. [Google Scholar] [CrossRef]
- Mowrey, D.B.; Clayson, D.E. Motion sickness, ginger, and psychophysics. Lancet 1982, 319, 655–657. [Google Scholar] [CrossRef]
- Lien, H.-C.; Sun, W.M.; Chen, Y.-H.; Kim, H.; Hasler, W.; Owyang, C. Effects of ginger on motion sickness and gastric slowwave dysrhythmias induced by circular vection. Am. J. Physiol. Gastrointest. Liver Physiol. 2003, 284, G481–G489. [Google Scholar] [CrossRef]
- Stewart, J.J.; Wood, M.J.; Wood, C.D.; Mims, M.E. Effects of ginger on motion sickness susceptibility and gastric function. Pharmacology 1991, 42, 111–120. [Google Scholar] [CrossRef]
- Bone, M.E.; Wilkinson, D.J.; Young, J.R.; McNeil, J.; Charlton, S. Ginger root—A new aniemetic: The effect of ginger root on postoperative nausea and vomiting after gynaecological surgery. Anesthesia 1990, 45, 669–671. [Google Scholar] [CrossRef]
- Phillips, S.; Ruggier, R.; Hutchinson, S.E. Zingiber officinale (ginger)—An antiemetic for day case surgery. Anaesthesia 1993, 48, 715–717. [Google Scholar] [CrossRef]
- Ryan, J.L.; Heckler, C.E.; Roscoe, J.A.; Dakhil, S.R.; Kirshner, J.; Flynn, P.J.; Hickok, J.T.; Morrow, G.R. Ginger (Zingiber officinale) reduces acute chemotherapy-induced nausea: A URCC CCOP study of 576 patients. Support Care Can. 2012, 20, 1479–1489. [Google Scholar] [CrossRef]
- Lua, P.L.; Salihah, N.; Mazlan, N. Effects of Inhaled Ginger Aromatherapy on Chemotherapy-Induced Nausea and Vomiting and Health-Related Quality of Life in Women with Breast Cancer. Complement. Med. 2015, 23, 396–404. [Google Scholar] [CrossRef]
- Chen, C.H.; Barrett, B.; Kwekkeboom, K.L. Efficacy of Oral Ginger (Zingiber officinale) for Dysmenorrhea: A Systematic Review and Meta-Analysis. Evid. Based Compl. Altern. Med. 2006, 2006, 6295737. [Google Scholar] [CrossRef]
- Rahnama, P.; Montazeri, A.; Huseini, H.F.; Kianbakht, S.; Naseri, M. Effect of Zingiber officinale R. Rhizomes (ginger) on pain relief in primary dysmenorrhea: A placebo randomized trial. BMC Complement. Altern. Med. 2012, 12, 92. [Google Scholar] [CrossRef]
- Shirvani, M.A.; Motahari-Tabari, N.; Alipour, A. The effect of mefenamic acid and ginger on pain relief in primary dysmenorrhea: A randomized clinical trial. Arch. Gynecol. Obstet. 2015, 291, 1277–1281. [Google Scholar] [CrossRef]
- Ozgoli, G.; Goli, M.; Moattar, F. Comparison of effects of ginger, mefenamic acid, and ibuprofen on pain in women with primary dysmenorrhea. J. Altern. Complement. Med. 2009, 15, 129–132. [Google Scholar] [CrossRef]
- Halder, A. Effect of progressivemuscle relaxation versus intake of ginger powder on dysmenorrhoea amongst the nursing students in Pune. Nurs. J. India 2012, 103, 152–156. [Google Scholar]
- Mahluji, S.; Ostadrahimi, A.; Mobasseri, M.; Attari, V.E.; Payahoo, L. Anti-inflammatory effects of Zingiber officinale in type 2 diabetic patients. Adv. Pharm. Bull. 2013, 3, 273. [Google Scholar]
- Arablou, T.; Aryaeian, N.; Valizadeh, M.; Sharifi, F.; Hosseini, A.F.; Djalali, M. The effect of Ginger consumption on some cardiovascular risk factors in patients with type 2 diabetes mellitus. Razi J. Med. Sci. 2014, 21, 1–12. [Google Scholar]
- Arablou, T.; Aryaeian, N.; Valizadeh, M.; Sharifi, F.; Hosseini, A.F.; Djalali, M. The effect of Ginger consumption on glycemic status, lipid profile and some inflammatory markers in patients with type 2 diabetes mellitus. Int. J. Food Sci. Nutr. 2014, 65, 515–520. [Google Scholar] [CrossRef]
- Andallu, B.; Radhika, B.; Suryakantham, V. Effect of Aswagandha, Ginger and Mulberry on Hyperglycemia and Hyperlipidemia. Plant Foods Hum. Nutr. 2004, 58, 1–7. [Google Scholar] [CrossRef]
- Mozaffari-Khosravi, H.; Talaei, B.; Jalali, B.A.; Najarzadeh, A.; Mozayan, M.R. The effect of ginger powder supplementation on insulin resistance and glycemic indices in patients with type 2 diabetes: A randomized, double-blind, placebo-controlled trial. Complement. Ther. Med. 2014, 22, 9–16. [Google Scholar] [CrossRef]
- Atashak, S.; Piri, M.; Jafari, A.; Azarbayjani, M.A. Effects of 10 week resistance training and ginger consumption on C-reactive protein and some cardiovascular risk factors in obese men. Iranian Soc. Physiol. Pharmacol. 2010, 14, 318–328. [Google Scholar]
- Imani, H.; Tabibi, H.; Najafi, I.; Atabak, S.; Hedayati, M.; Rahmani, L. Effects of ginger on serum glucose, advanced glycation end products, and inflammation in peritoneal dialysis patients. Nutrition 2015, 31, 703–707. [Google Scholar] [CrossRef]
- Citronberg, J.; Bostick, R.; Ahearn, T.; Turgeon, D.K.; Ruffin, M.T.; Djuric, Z.; Sen, A.; Brenner, D.E.; Zick, S.M. Effects of Ginger Supplementation on Cell Cycle Biomarkers in the Normal-Appearing Colonic Mucosa: Results from a Pilot, Randomized, Controlled Trial. Cancer Prev. Res. 2013, 6, 271–281. [Google Scholar] [CrossRef]
- Jiang, Y.; Turgeon, D.K.; Wright, B.D.; Sidahmed, E.; Ruffin, M.T.; Brenner, D.E.; Sen, A.; Zick, S.M. Effect of ginger root on cyclooxygenase-1 and 15-hydroxyprostaglandin dehydrogenase expression in colonic mucosa of humans at normal and increased risk for colorectal cancer. Eur. J. Cancer Prev. 2013, 22, 455–460. [Google Scholar] [CrossRef]
- Van Tilburg, M.A.; Palsson, O.S.; Ringel, Y.; Whitehead, W.E. Is ginger effective for the treatment of irritable bowel syndrome? A double blind randomized controlled pilot trial. Complement. Therap. Med. 2014, 22, 17–20. [Google Scholar] [CrossRef]
- Rahimlou, M.; Yari, Z.; Hekmatdoost, A.; Alavian, S.M.; Keshavarz, S.A. Ginger supplementation in nonalcoholic fatty liver disease: A randomized, double-blind, placebo-controlled pilot study. Hepatitis Mon. 2016, 16, e34897. [Google Scholar] [CrossRef]
- Ebrahimzadeh Attari, V.; Asghari Jafarabadi, M.; Zemestani, M.; Ostadrahimi, A. Effect of Zingiber officinale supplementation on obesity management with respect to the uncoupling protein 1-3826A>G and β3-adrenergic receptor Trp64Arg polymorphism. Phytother. Res. 2015, 29, 1032–1039. [Google Scholar] [CrossRef]
- Ebrahimzadeh Attari, V.; Ostadrahimi, A.; Asghari Jafarabadi, M.; Mehralizadeh, S.; Mahluji, S. Changes of serum adipocytokines and bodyweight following Zingiber officinale supplementation in obese women: A RCT. Eur. J. Nutr. 2016, 55, 2129–2136. [Google Scholar] [CrossRef]
- Fernandes, R.V.B.; Botrel, D.A.; Silva, E.K.; Pereira, C.G.; do Carmo, E.L.; Dessimoni, A.L.A.; Borges, S.V. Microencapsulated ginger oil properties: Influence of operating parameters. Drying Technol. 2017, 35, 1098–1107. [Google Scholar] [CrossRef]
- Toure, A.; Xiaoming, Z.; Jia, C.-S.; Zhijian, D. Microencapsulation and Oxidative Stability of Ginger Essential Oil in Maltodextrin/Whey Protein Isolate (MD/WPI). Int. J. Dairy Sci. 2007, 2, 387–392. [Google Scholar]
- Jayanudin; Rochmadi; Fahrurrozi, M.; Wirawan, S.K. Microencapsulation Technology of Ginger Oleoresin with Chitosan as Wall Material: A review. J. Appl. Pharm. Sci. 2016, 12, 209–223. [Google Scholar] [CrossRef]
- Jayanudin; Rochmadi. Encapsulation of red ginger oleoresin (Zingiber officinale var rubrum) with chitosan as wall material. Int. J. Pharm. Pharm. Sci. 2017, 9, 29–34. [Google Scholar]
- Jayanudin; Rochmadi; Wiratni; Yulvianti, M.; Barleany, D.R.; Ernayati, W. Encapsulation Red Ginger Oleoresin (Zingiber officinale var. Rubrum) with Chitosan-alginate as Wall Material Using Spray Drying. Res. J. Appl. Sci. Eng. Technol. 2015, 10, 1370–1378. [Google Scholar] [CrossRef]
- Tanaka, K.; Arita, M.; Sakurai, H.; Ono, N.; Tezuka, Y. Analysis of Chemical Properties of Edible and Medicinal Ginger by Metabolomics Approach. BioMed Res. Int. 2015, 2015, 671058. [Google Scholar] [CrossRef]
- Purathrive. Could Ginger Be Used Medicinally? purathrive.com, 2019. Available online: https://purathrive.com/could-ginger-be-used-medicinally (accessed on 12 March 2019).
- Synchro. Gold (Lemon ginger). besynchro.com, 2019. Available online: https://besynchro.com/collections/shop/products/synchro-gold-lemon-ginger (accessed on 12 March 2019).
- Ganji, S.; Sayyed-Alangi, S.Z. Encapsulation of ginger ethanolic extract in nanoliposome and evaluation of its antioxidant activity on sunflower oil. Chem. Pap. 2017, 71, 1781–1789. [Google Scholar] [CrossRef]
- Baskar, V.; Selvakumar, K.; Madhan, R.; Srinivasan, G.; Muralidharan, M. Study on improving bioavailability ratio of anti-inflammatory compound from ginger through nano transdermal delivery. Asian J. Pharm. Clin. Res. 2012, 5, 241–246. [Google Scholar]
- Ju, S.; Mu, J.; Dokland, T.; Zhuang, X.; Wang, Q.; Jiang, H.; Xiang, X.; Deng, Z.B.; Wang, B.; Zhang, L.; et al. Grape exosomelike nanoparticles induce intestinal stem cells and protect mice from dss-induced colitis. Mol. Ther. 2013, 21, 1345–1357. [Google Scholar] [CrossRef]
- Wang, B.; Zhuang, X.; Deng, Z.B.; Jiang, H.; Mu, J.; Wang, Q.; Xiang, X.; Guo, H.; Zhang, L.; Dryden, G.; et al. Targeted drug delivery to intestinal macrophages by bioactive nanovesicles released from grapefruit. Mol. Ther. 2014, 22, 522–534. [Google Scholar] [CrossRef]
- Mu, J.; Zhuang, X.; Wang, Q.; Jiang, H.; Deng, Z.B.; Wang, B.; Zhang, L.; Kakar, S.; Jun, Y.; Miller, D.; et al. Interspecies communication between plant and mouse gut host cells through edible plant derived exosome-like nanoparticles. Mol. Nutr. Food Res. 2014, 58, 1561–1573. [Google Scholar] [CrossRef]
- Zhang, M.; Wang, X.; Han, M.K.; Collins, J.F.; Merlin, D. Oral administration of ginger-derived nanolipids loaded with siRNA as a novel approach for efficient siRNA drug delivery to treat ulcerative colitis. Nanomedicine 2017, 12, 1927–1943. [Google Scholar] [CrossRef]
- Zhuang, X.; Deng, Z.B.; Mu, J.; Zhang, L.; Yan, J.; Miller, D.; Feng, W.; McClain, C.J.; Zhang, H.G. Ginger-derived nanoparticles protect against alcohol-induced liver damage. J. Extracell. Vesicles 2015, 4, 28713. [Google Scholar] [CrossRef]
- Zhang, M.; Xiao, B.; Wang, H.; Han, M.K.; Zhang, Z.; Viennois, E.; Xu, C.; Merlin, D. Edible Ginger-derived Nano-lipids Loaded with Doxorubicin as a Novel Drug-delivery Approach for Colon Cancer Therapy. Mol. Ther. 2016, 24, 1783–1796. [Google Scholar] [CrossRef]
© 2019 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).