Systematic Review of Level 1 and Level 2 Screening Tools for Autism Spectrum Disorders in Toddlers
Abstract
:1. Introduction
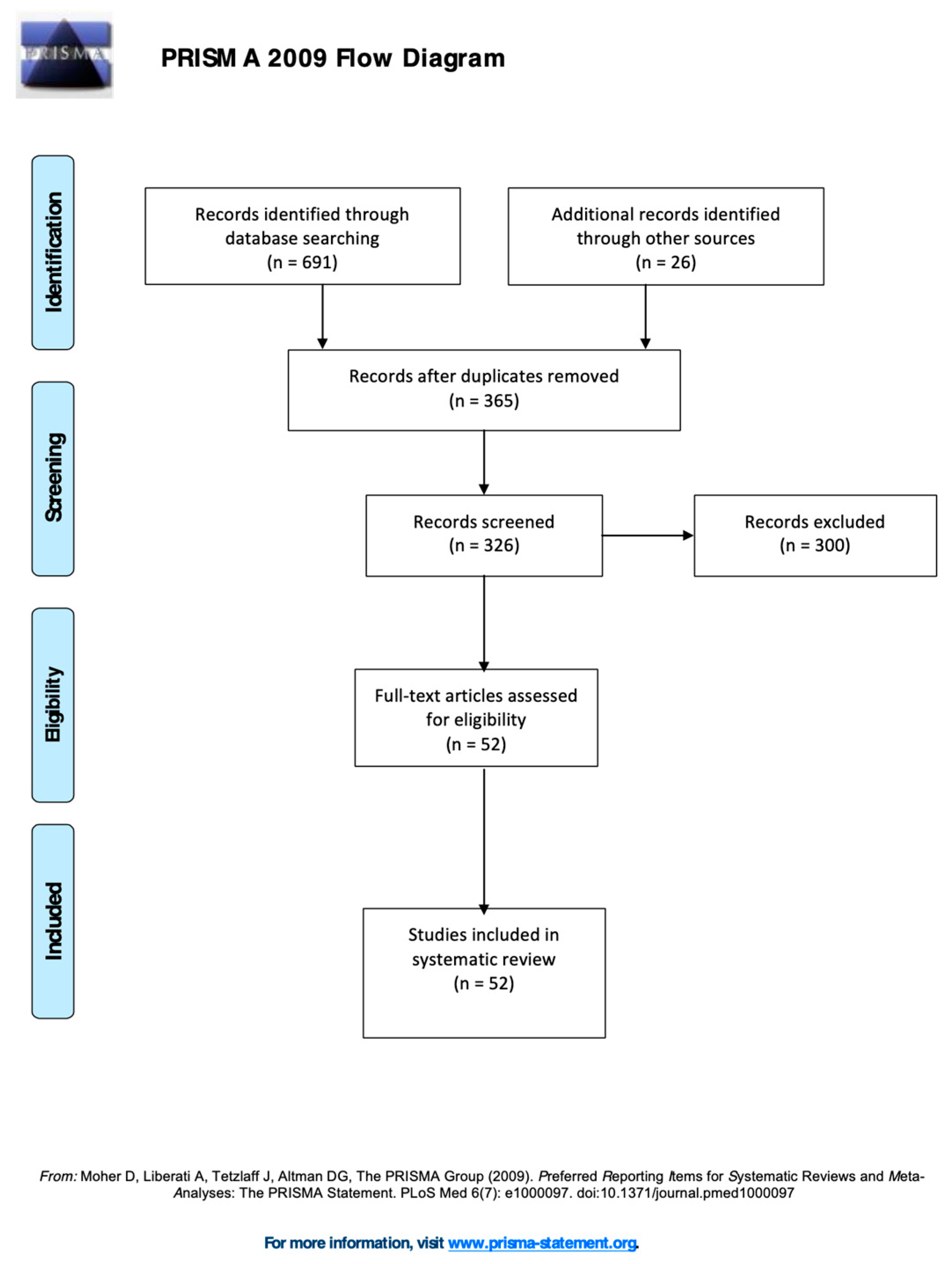
2. Materials and Methods
3. Results
3.1. Overview of the Studies and Measures
3.2. Overview of the Studies and Measures
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5), 5th ed.; American Psychiatric Press: Washington, DC, USA, 2013. [Google Scholar]
- Christensen, D.L.; Maenner, M.J.; Bilder, D.; Constantino, J.N.; Daniels, J.; Durkin, M.S.; Fitzgerald, R.T.; Kurzius-Spencer, M.; Pettygrove, S.D.; Robinson, C.; et al. Prevalence and Characteristics of Autism Spectrum Disorder Among Children Aged 4 Years—Early Autism and Developmental Disabilities Monitoring Network, Seven Sites, United States, 2010, 2012, and 2014. MMWR Surveill. Summ. 2019, 68, 1–19. [Google Scholar]
- Christensen, D.L.; Braun, K.V.N.; Baio, J.; Bilder, D.; Charles, J.; Constantino, J.N.; Daniels, J.; Durkin, M.S.; Fitzgerald, R.T.; Kurzius-Spencer, M.; et al. Prevalence and characteristics of autism spectrum disorder among children aged 8 years—Autism and developmental disabilities monitoring network, 11 sites, United States, 2012. MMWR Surveill. Summ. 2018, 65, 1. [Google Scholar]
- Filipek, P.A.; Accardo, P.J.; Ashwal, S.; Baranek, G.T.; Cook, E.H.; Dawson, G.; Gordon, J.S.; Gravel, C.P.; Johnson, R.J.; Kallen, S.E.; et al. Practice parameter: Screening and diagnosis of autism: Report of the Quality Standards Subcommittee of the American Academy of Neurology and the Child Neurology Society. Neurology 2000, 55, 468–479. [Google Scholar] [PubMed]
- Marchetti, A.; Castelli, I.; Cavalli, G.; Di Terlizzi, E.; Lecciso, F.; Lucchini, B.; Massaro, D.; Petrocchi, S.; Valle, A. Theory of Mind in typical and atypical developmental settings: Some considerations from a contextual perspective. In Reflective Thinking in Educational Settings: A Cultural Frame Work; Antonietti, A., Confalonieri, E., Eds.; Cambridge University Press: Cambridge, UK, 2014; pp. 102–136. [Google Scholar]
- Falkmer, T.; Anderson, K.; Falkmer, M.; Horlin, C. Diagnostic procedures in autism spectrum disorders: A systematic literature review. Eur. Child Adolesc. Psychiatry 2013, 22, 329–340. [Google Scholar] [PubMed]
- Volkmar, F.; Siegel, M.; Woodbury-Smith, M.; King, B.; McCracken, J.; State, M. Practice parameter for the assessment and treatment of children and adolescents with autism spectrum disorder. J. Am. Acad. Child Adolesc. Psychiatry 2014, 53, 237–257. [Google Scholar] [PubMed] [Green Version]
- Lord, C.; Rutter, M.; Le Couteur, A. Autism Diagnostic Interview-Revised: A revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. JADD 1994, 24, 659–685. [Google Scholar]
- Lord, C.; Luyster, R.J.; Gotham, K.; Guthrie, W. Autistic Diagnosis Observation Scale 2 Manual; Hogrefe: Florence, Italy, 2013. [Google Scholar]
- Dawson, G.; Rogers, S.; Munson, J.; Smith, M.; Winter, J.; Greenson, J.; Donaldson, A.; Varley, J. Randomized, controlled trial of an intervention for toddlers with autism: The Early Start Denver Model. Pediatrics 2010, 125, e17–e23. [Google Scholar] [CrossRef] [Green Version]
- Perry, A.; Cummings, A.; Geier, J.D.; Freeman, N.L.; Hughes, S.; LaRose, L.; Managhan, T.; Reitzel, J.A.; Williams, J. Effectiveness of intensive behavioral intervention in a large, community-based program. Res. Autism Spectr. Disord. 2008, 2, 621–642. [Google Scholar] [CrossRef]
- Sallows, G.O.; Graupner, T.D. Intensive behavioral treatment for children with autism: Four-year outcome and predictors. Am. J. Ment. Retard. 2005, 110, 417–438. [Google Scholar] [CrossRef]
- Leo, M.; Carcagnì, P.; Del Coco, M.; Spagnolo, P.; Mazzeo, P.L.; Celeste, G.; Distante, C.; Lecciso, F.; Levante, A.; Rosato, A.C.; et al. Towards the Automatic Assessment of Abilities to produce Facial Expressions: The case study of children with ASD. In Proceedings of the 20th Italian National Conference on Photonic Technologies, Lecce, Italy, 23–25 May 2018; p. 4. [Google Scholar]
- Leo, M.; Carcagnì, P.; Distante, C.; Spagnolo, P.; Mazzeo, P.L.; Rosato, A.C.; Petrocchi, S.; Pellegrino, C.; Levante, A.; De Lumè, F.; et al. Computational Assessment of Facial Expression Production in ASD Children. Sensors 2018, 18, 3993. [Google Scholar] [CrossRef] [Green Version]
- Leo, M.; Carcagnì, P.; Distante, C.; Mazzeo, P.L.; Spagnolo, P.; Levante, A.; Petrocchi, S.; Lecciso, F. Computational Analysis of Deep Visual Data for Quantifying Facial Expression Production. Appl. Sci. 2019, 9, 4542. [Google Scholar]
- Daniels, A.M.; Mandell, D.S. Explaining differences in age at autism spectrum disorder diagnostic: A critical review. Autism 2014, 18, 583–597. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Anderson, D.K.; Liang, J.W.; Lord, C. Predicting young adult outcome among more and less cognitively able individuals with autism spectrum disorders. J. Child Psychol. Psychiatry 2014, 55, 485–494. [Google Scholar] [CrossRef]
- Lecciso, F.; Petrocchi, S.; Savazzi, F.; Marchetti, A.; Nobile, M.; Molteni, M. The association between maternal resolution of the diagnosis of autism, maternal mental representations of the relationship with the child, and children’s attachment. Lifesp. Disabil. 2013, 16, 21–38. [Google Scholar]
- Robins, D.L.; Dumont-Mathieu, T.M. Early screening for autism spectrum disorders: Update on the modified checklist for autism in toddlers and other measures. J. Dev. Behav. Pediatrics 2006, 27, S111–S119. [Google Scholar] [CrossRef] [Green Version]
- Lauritsen, M.B.; Pedersen, C.B.; Mortensen, P.B. Effects of familial risk factors and place of birth on the risk of autism: A nationwide register-based study. J. Child Psychol. Psychiatry 2005, 46, 963–971. [Google Scholar] [PubMed]
- Daniels, A.M.; Halladay, A.K.; Shih, A.; Elder, L.M.; Dawson, G. Approaches to enhancing the early detection of autism spectrum disorders: A systematic review of the literature. J. Am. Acad. Child Adolesc. Psychiatry 2014, 53, 141–152. [Google Scholar] [CrossRef]
- García-Primo, P.; Hellendoorn, A.; Charman, T.; Roeyers, H.; Dereu, M.; Roge, B.; Baduel, S.; Muratori, F.; Narzisi, A.; Van Daalen, E.; et al. Screening for autism spectrum disorders: State of the art in Europe. Eur. Child Adolesc. Psychiatry 2014, 23, 1005–1021. [Google Scholar] [CrossRef]
- McPheeters, M.L.; Weitlauf, A.S.; Vehorn, A.; Taylor, C.; Sathe, N.A.; Krishnaswami, S.; Fonnesbeck, C.; Warren, Z.E. Screening for Autism Spectrum Disorder in Young Children: A Systematic Evidence Review for the U.S. Preventive Services Task Force; Evidence Synthesis No. 129; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2016.
- Sappok, T.; Heinrich, M.; Underwood, L. Screening tools for autism spectrum disorders. Adv. Autism 2015, 1, 12–29. [Google Scholar] [CrossRef]
- Zwaigenbaum, L.; Bauman, M.L.; Fein, D.; Pierce, K.; Buie, T.; Davis, P.A.; Newschaffer, C.; Robins, D.L.; Wetherby, A.; Choueiri, R.; et al. Early screening of autism spectrum disorder: Recommendations for practice and research. Pediatrics 2015, 136, S41–S59. [Google Scholar] [CrossRef] [Green Version]
- Marlow, M.; Servili, C.; Tomlinson, M. A review of screening tools for the identification of autism spectrum disorders and developmental delay in infants and young children: Recommendations for use in low-and middle-income countries. Autism Res. 2019, 12, 176–199. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-García, A.B.; Galindo-Villardón, P.; Nieto-Librero, A.B.; Martín-Rodero, H.; Robins, D.L. Toddler Screening for Autism Spectrum Disorder: A Meta-Analysis of Diagnostic Accuracy. JADD 2019, 49, 1837–1852. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thabtah, F.; Peebles, D. Early Autism Screening: A Comprehensive Review. Int. J. Environ. Res. Public Health 2019, 16, 3502. [Google Scholar] [CrossRef] [Green Version]
- Mokkink, L.B.; Terwee, C.B.; Patrick, D.L.; Alonso, J.; Stratford, P.W.; Knol, D.L.; Bouter, L.M.; De Vet, H.C. The COSMIN checklist for assessing the methodological quality of studies on measurement properties of health status measurement instruments: An international Delphi study. Qual. Life Res. 2010, 19, 539–549. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mokkink, L.B.; Terwee, C.B.; Patrick, D.L.; Alonso, J.; Stratford, P.W.; Knol, D.L.; Bouter, L.M.; de Vet, H.C. The COSMIN study reached international consensus on taxonomy, terminology, and definitions of measurement properties for health-related patient-reported outcomes. J. Clin. Epidem. 2010, 63, 737–745. [Google Scholar] [CrossRef] [Green Version]
- Terwee, C.B.; Mokkink, L.B.; Knol, D.L.; Ostelo, R.W.; Bouter, L.M.; de Vet, H.C. Rating the methodological quality in systematic reviews of studies on measurement properties: A scoring system for the COSMIN checklist. Qual. Life Res. 2012, 21, 651–657. [Google Scholar] [CrossRef] [Green Version]
- Levante, A.; Petrocchi, S.; Lecciso, F. Systematic review protocol of measures for the early detection of risk of Autism Spectrum Disorder risk in toddlers. Lifesp. Dis. 2019, 22, 55–75. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Hedley, D.; Young, R.; Angelica, M.; Gallegos, J.; Marcin Salazar, C. Cross-cultural evaluation of the Autism Detection in Early Childhood (ADEC) in Mexico. Autism 2010, 14, 93–112. [Google Scholar] [CrossRef]
- Nah, Y.H.; Young, R.L.; Brewer, N. Using the Autism Detection in Early Childhood (ADEC) and Childhood Autism Rating Scales (CARS) to predict long term outcomes in children with autism spectrum disorders. JADD 2014, 44, 2301–2310. [Google Scholar] [CrossRef]
- Nah, Y.H.; Young, R.L.; Brewer, N.; Berlingeri, G. Autism Detection in Early Childhood (ADEC): Reliability and validity data for a level 2 screening tool for autistic disorder. Psychol. Assess. 2014, 26, 215. [Google Scholar] [CrossRef] [PubMed]
- Hedley, D.; Nevill, R.E.; Monroy-Moreno, Y.; Fields, N.; Wilkins, J.; Butter, E.; Mulick, J.A. Efficacy of the ADEC in identifying autism spectrum disorder in clinically referred toddlers in the US. JADD 2015, 45, 2337–2348. [Google Scholar] [CrossRef] [PubMed]
- Bryson, S.E.; Zwaigenbaum, L.; McDermott, C.; Rombough, V.; Brian, J. The Autism Observation Scale for Infants: Scale development and reliability data. JADD 2008, 38, 731–738. [Google Scholar] [CrossRef] [PubMed]
- Brian, J.; Bryson, S.E.; Garon, N.; Roberts, W.; Smith, I.M.; Szatmari, P.; Zwaigenbaum, L. Clinical assessment of autism in high-risk 18-month-olds. Autism 2008, 12, 433–456. [Google Scholar] [CrossRef]
- Gammer, I.; Bedford, R.; Elsabbagh, M.; Garwood, H.; Pasco, G.; Tucker, L.; Volein, A.; Johnson, M.H.; Charman, T.; The BASIS Team. Behavioural markers for autism in infancy: Scores on the Autism Observational Scale for Infants in a prospective study of at-risk siblings. Inf. Behav. Dev. 2015, 38, 107–115. [Google Scholar] [CrossRef]
- Matson, J.L.; Fodstad, J.C.; Dempsey, T. What symptoms predict the diagnosis of autism or PDD-NOS in infants and toddlers with developmental delays using the Baby and Infant Screen for aUtIsm Traits. Dev. Neurorehab. 2009, 12, 381–388. [Google Scholar] [CrossRef]
- Matson, J.L.; Wilkins, J.; Sharp, B.; Knight, C.; Sevin, J.A.; Boisjoli, J.A. Sensitivity and specificity of the Baby and Infant Screen for Children with aUtIsm Traits (BISCUIT): Validity and cutoff scores for autism and PDD-NOS in toddlers. Res. Autism Spectr. Disord. 2009, 3, 924–930. [Google Scholar] [CrossRef]
- Matson, J.L.; Wilkins, J.; Sevin, J.A.; Knight, C.; Boisjoli, J.A.; Sharp, B. Reliability and item content of the Baby and Infant Screen for Children with aUtIsm Traits (BISCUIT): Parts 1–3. Res. Autism Spectr. Disord. 2009, 3, 336–344. [Google Scholar] [CrossRef]
- Matson, J.L.; Boisjoli, J.A.; Hess, J.A.; Wilkins, J. Factor structure and diagnostic fidelity of the Baby and Infant Screen for Children with aUtIsm Traits–Part 1 (BISCUIT–Part 1). Dev. Neurorehab. 2010, 13, 72–79. [Google Scholar] [CrossRef]
- Matson, J.L.; Wilkins, J.; Fodstad, J.C. The validity of the baby and infant screen for children with autism traits: Part 1 (BISCUIT: Part 1). JADD 2011, 41, 1139–1146. [Google Scholar] [CrossRef]
- Dereu, M.; Warreyn, P.; Raymaekers, R.; Meirsschaut, M.; Pattyn, G.; Schietecatte, I.; Roeyers, H. Screening for Autism Spectrum Disorders in Flemish Day-Care Centres with the Checklist for Early Signs of Developmental Disorders. JADD 2010, 40, 1247–1258. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baron-Cohen, S.; Allen, J.; Gillberg, C. Can autism be detected at 18 months? The needle, the haystack, and the CHAT. Br. J. Psychiatry 1992, 161, 839–843. [Google Scholar] [CrossRef] [PubMed]
- Baron-Cohen, S.; Cox, A.; Baird, G.; Swettenham, J.; Nightingale, N.; Morgan, K.; Drew, A.; Charman, T. Psychological markers in the detection of autism in infancy in a large population. Br. J. Psychiatry 1996, 168, 158–163. [Google Scholar] [CrossRef] [PubMed]
- Gray, K.M.; Tonge, B.J.; Sweeney, D.J.; Einfeld, S.L. Screening for Autism in young children with developmental delay: An evaluation of the Developmental Behavior Checklist: Early Screen. JADD 2008, 38, 1003–1010. [Google Scholar] [CrossRef]
- Dietz, C.; Swinkels, S.; van Daalen, E.; van Engeland, H.; Buitelaar, J.K. Screening for Autistic Spectrum Disorder in Children Aged 14-15 Months. II: Population Screening with the Early Screening of Autistic Traits Questionnaire (ESAT). Design and General Findings. JADD 2006, 36, 713–722. [Google Scholar] [CrossRef]
- Möricke, E.; Swinkels, S.H.N.; Beuker, K.T.; Buitelaar, J.K. Predictive value of subclinical autistic traits at age 14-15 months for behavioural and cognitive problems at age 3–5 years. Eur. Child Adolesc. Psychiatry 2010, 19, 659–668. [Google Scholar] [CrossRef] [Green Version]
- Reznick, J.S.; Baranek, G.T.; Reavis, S.; Watson, L.R.; Crais, E.R. A parent- report instrument for identifying one-year-olds at risk for an eventual diagnosis of autism: The first year inventory. JADD 2007, 37, 1691–1710. [Google Scholar] [CrossRef]
- Ben-Sasson, A.; Carter, A.S. The application of the first year inventory for ASD screening in Israel. JADD 2012, 42, 1906–1916. [Google Scholar] [CrossRef]
- Turner-Brown, L.M.; Baranek, G.T.; Reznick, J.S.; Watson, L.R.; Crais, E.R. The First Year Inventory: A longitudinal follow-up of 12-month-old to 3-year-old children. Autism 2013, 17, 527–540. [Google Scholar] [CrossRef] [Green Version]
- Nygren, G.; Sandberg, E.; Gillstedt, F.; Ekeroth, G.; Arvidsson, T.; Gillberg, C. A new screening program for autism in a general population of Swedish toddlers. Res. Dev. Dis. 2012, 33, 1200–1210. [Google Scholar] [CrossRef]
- Robins, D.L.; Fein, D.; Barton, M.L.; Green, J.A. The Modified Checklist for Autism in Toddlers: An initial study investigating the early detection of autism and pervasive developmental disorders. JADD 2001, 31, 131–144. [Google Scholar] [CrossRef] [PubMed]
- Snow, A.V.; Lecavalier, L. Sensitivity and specificity of the Modified Checklist for Autism in Toddlers and the Social Communication Questionnaire in preschoolers suspected of having pervasive developmental disorders. Autism 2008, 12, 627–644. [Google Scholar] [CrossRef] [PubMed]
- Seif Eldin, A.; Habib, D.; Noufal, A.; Farrag, S.; Bazaid, K.; Al-Sharbati, M.; Badr, H.; Moussa, S.; Essali, A.; Gaddour, N. Use of M-CHAT for a multinational screening of young children with autism in the Arab countries. Int. Rev. Psychiatry 2008, 20, 281–289. [Google Scholar] [CrossRef] [PubMed]
- Canal-Bedia, R.; García-Primo, P.; Martín-Cilleros, M.V.; Santos-Borbujo, J.; Guisuraga-Fernández, Z.; Herráez-García, L.; del Mar Herraez-Garcia, M.; Boada-Muños, L.; Fuentes-Biggi, M.; Posada-de La Paz, M. Modified checklist for autism in toddlers: Cross-cultural adaptation and validation in Spain. JADD 2011, 41, 1342–1351. [Google Scholar] [CrossRef]
- Inada, N.; Koyama, T.; Inokuchi, E.; Kuroda, M.; Kamio, Y. Reliability and validity of the Japanese version of the Modified Checklist for autism in toddlers (M- CHAT). Res. Autism Spectr. Disord. 2011, 5, 330–336. [Google Scholar] [CrossRef]
- Albores-Gallo, L.; Roldán-Ceballos, O.; Villarreal-Valdes, G.; Betanzos-Cruz, B.X.; Santos-Sánchez, C.; Martínez-Jaime, M.M.; Lemus-Espinosa, I.; Hilton, C.L. M-CHAT Mexican version validity and reliability and some cultural considerations. ISRN Neurol. 2012, 2012, 408694:1–408694:7. [Google Scholar] [CrossRef] [Green Version]
- Kozlowski, A.M.; Matson, J.L.; Worley, J.A.; Sipes, M.; Horovitz, M. Defining characteristics for young children meeting cutoff on the modified checklist for autism in toddlers. Res. Autism. Spectr. Disord. 2012, 6, 472–479. [Google Scholar] [CrossRef]
- Scarpa, A.; Reyes, N.M.; Patriquin, M.A.; Lorenzi, J.; Hassenfeldt, T.A.; Desai, V.J.; Kerkering, K.W. The modified checklist for autism in toddlers: Reliability in a diverse rural American sample. JADD 2013, 43, 2269–2279. [Google Scholar] [CrossRef]
- Matson, J.L.; Kozlowski, A.M.; Fitzgerald, M.E.; Sipes, M. True versus false positives and negatives on the Modified Checklist For Autism in Toddlers. Res. Autism Spectr. Disord. 2013, 7, 17–22. [Google Scholar] [CrossRef]
- Stenberg, N.; Bresnahan, M.; Gunnes, N.; Hirtz, D.; Hornig, M.; Lie, K.K.; Lipkin, W.I.; Lord, C.; Magnus, P.; Kjennerud, T.R.; et al. Identifying children with autism spectrum disorder at 18 months in a general population sample. Paed. Perinat. Epidem. 2014, 28, 255–262. [Google Scholar] [CrossRef] [Green Version]
- Seung, H.; Ji, J.; Kim, S.J.; Sung, I.; Youn, Y.A.; Hong, G.; Lee, H.; Lee, Y.H.; Lee, H.; Youm, H.K. Examination of the Korean modified checklist of autism in toddlers: Item responsetheory. JADD 2015, 45, 2744–2757. [Google Scholar] [CrossRef] [PubMed]
- Cuesta-Gómez, J.L.; Andrea Manzone, L.; Posada-De-La-Paz, M. Modified checklist for autism in toddler cross-cultural adaptation for Argentina. Int. J. Dev. Dis. 2016, 62, 117–123. [Google Scholar] [CrossRef]
- Baduel, S.; Guillon, Q.; Afzali, M.H.; Foudon, N.; Kruck, J.; Rogé, B. The French version of the modified-checklist for autism in toddlers (M-CHAT): A validation study on a French sample of 24 months old children. JADD 2017, 47, 297–304. [Google Scholar] [CrossRef] [PubMed]
- Kleinman, J.M.; Robins, D.L.; Ventola, P.E.; Pandey, J.; Boorstein, H.C.; Esser, E.L.; Wilson, L.B.; Rosenthal, M.A.; Sutera, S.; Verbalis, A.D.; et al. The modified checklist for autism in toddlers: A follow-up study investigating the early detection of autism spectrum disorders. JADD 2008, 38, 827–839. [Google Scholar] [CrossRef] [Green Version]
- Chlebowski, C.; Robins, D.L.; Barton, M.L.; Fein, D. Large-scale use of the modified checklist for autism in low-risk toddlers. Pediatrics 2013, 131, e1121–e1127. [Google Scholar] [CrossRef] [Green Version]
- Robins, D.L.; Casagrande, K.; Barton, M.; Chen, C.M.A.; Dumont-Mathieu, T.; Fein, D. Validation of the modified checklist for autism in toddlers, revised with follow-up (M-CHAT-R/F). Pediatrics 2014, 133, 37–45. [Google Scholar] [CrossRef] [Green Version]
- Brennan, L.; Fein, D.; Como, A.; Rathwell, I.C.; Chen, C.M. Use of the Modified Checklist for Autism, Revised with Follow Up-Albanian to Screen for ASD in Albania. JADD 2016, 46, 3392–3407. [Google Scholar] [CrossRef] [Green Version]
- Carakovac, M.; Jovanovic, J.; Kalanj, M.; Rudic, N.; Aleksic–Hil, O.; Aleksic, B.; Villalobos, I.B.; Kasuya, H.; Ozaki, N.; Lecic-Tosevski, D.; et al. Serbian language version of the modified checklist for autism in toddlers, revised, with follow-up: Cross-cultural adaptation and assessment of reliability. Sci. Rep. 2016, 6, 38222. [Google Scholar] [CrossRef] [Green Version]
- Windiani, I.G.A.T.; Soetjiningsih, S.; Adnyana, I.G.A.S.; Lestari, K.A. Indonesian Modified Checklist for Autism in Toddler, Revised with Follow-Up (M- CHAT-R/F) for Autism Screening in Children at Sanglah General Hospital, Bali- Indonesia. Bali Med. J. 2016, 5, 133–137. [Google Scholar] [CrossRef] [Green Version]
- Guo, C.; Luo, M.; Wang, X.; Huang, S.; Meng, Z.; Shao, J.; Zhang, X.; Shao, Z.; Wu, J.; Robins, D.L.; et al. Reliability and Validity of the Chinese Version of Modified Checklist for Autism in Toddlers, Revised, with Follow-Up (M-CHAT-R/F). JADD 2018, 1–12. [Google Scholar] [CrossRef]
- Sangare, M.; Toure, H.B.; Toure, A.; Karembe, A.; Dolo, H.; Coulibaly, Y.I.; Kouyate, M.; Traore, K.; Diakite, S.A.; Coulibaly, S.; et al. Validation of two parent-reported autism spectrum disorders screening tools M-CHAT-R and SCQ in Bamako, Mali. eNeurol. Sci. 2019, 15, 100188. [Google Scholar] [CrossRef] [PubMed]
- Feldman, M.A.; Ward, R.A.; Savona, D.; Regehr, K.; Parker, K.; Hudson, M.; Penning, H.; Holden, J.A. Development and Initial Validation of Parent Report Measure of the Behavioral development of infants at risk for Autism Spectrum Disorders. JADD 2012, 42, 13–22. [Google Scholar] [CrossRef] [PubMed]
- Allison, C.; Baron-Cohen, S.; Wheelwright, S.; Charman, T.; Richler, J.; Pasco, G.; Brayne, C. The Q-CHAT (Quantitative CHecklist for Autism in Toddlers): A normally distributed quantitative measure of autistic traits at 18–24 months of age: Preliminary report. JADD 2008, 38, 1414–1425. [Google Scholar] [CrossRef] [PubMed]
- Magiati, I.; Goh, D.A.; Lim, S.J.; Gan, D.Z.Q.; Leong, J.C.L.; Allison, C.; Baron-Cohen, S.; Rifkin-Graboi, A.; Broekman, B.F.P.; Saw, S.M.; et al. The psychometric properties of the Quantitative-Checklist for Autism in Toddlers (Q-CHAT) as a measure of autistic traits in a community sample of Singaporean infants and toddlers. Mol. Autism 2015, 6, 40. [Google Scholar] [CrossRef] [Green Version]
- Ruta, L.; Chiarotti, F.; Arduino, G.M.; Apicella, F.; Leonardi, E.; Maggio, R.; Carozza, C.; Chericoni, N.; Costanzo, V.; Turco, N.; et al. Validation of the Quantitative CHecklist for Autism in Toddlers (Q-CHAT) in an Italian clinical sample of young children with Autism and Other Developmental Disorders. Front. Psychiatry 2019, 10, 488. [Google Scholar] [CrossRef] [Green Version]
- Rutaa, L.; Arduino, G.M.; Gagliano, A.; Apicella, F.; Leonardi, E.; Famà, F.I.; Chericoni, N.; Costanzo, V.; Turco, N.; Tartarisco, G.; et al. Psychometric properties, factor structure and cross-cultural validity of the quantitative CHecklist for autism in toddlers (Q-CHAT) in an Italian community setting. Res. Autism Spectr. Disord. 2019, 64, 39–48. [Google Scholar] [CrossRef]
- Lecciso, F.; Levante, A.; Signore, F.; Petrocchi, S. Preliminary evidence of the Structural Validity and measurement invariance of the Quantitative-CHecklist for Autism in Toddler (Q-CHAT) on Italian unselected children. EJASA 2019, 12, 320–340. [Google Scholar] [CrossRef]
- Persson, B.; Nordstrom, B.; Petersson, K.; Månsson, M.E.; Sivberg, B. Screening for infants with developmental deficits and/or autism: A Swedish pilotstudy. J. Pediatric Nurs. 2006, 21, 313–324. [Google Scholar] [CrossRef]
- Oner, P.; Oner, O.; Munir, K. Three-Item Direct Observation Screen (TIDOS) for autism spectrum disorder. Autism 2014, 18, 733–742. [Google Scholar] [CrossRef] [Green Version]
- Honda, H.; Shimizu, Y.; Nitto, Y.; Imai, M.; Ozawa, T.; Iwasa, M.; Shiga, K.; Hira, T. Extraction and refinement strategy for detection of autism in 18-month-old: A guarantee of higher sensivity and specificity in the process of mass screening. J. Child Psychol. Psychiatry 2009, 50, 972–981. [Google Scholar] [CrossRef]
- Prinsen, C.A.; Mokkink, L.B.; Bouter, L.M.; Alonso, J.; Patrick, D.L.; De Vet, H.C.; Terwee, C.B. COSMIN guideline for systematic reviews of patient-reported outcome measures. Qual. Life Res. 2018, 27, 1147–1157. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sirigatti, S.; Stefanile, C. MMPI-2: Aggiornamento all’ Adattamento Italiano; Giunti OS Organizzazioni Speciali: Florence, Italy, 2011. [Google Scholar]
- Petrocchi, S.; Iannello, P.; Lecciso, F.; Levante, A.; Antonietti, A.; Schulz, P.J. Interpersonal Trust in Doctor-Patient Relation: Evidence from Dyadic Analysis and Association with Quality of Dyadic Communication. Soc. Sci. Med. 2019, 235, 112391. [Google Scholar] [CrossRef] [PubMed]
- Reichow, B.; Barton, E.E.; Boyd, B.A.; Hume, K. Early intensive behavioral intervention (EIBI) for young children with autism spectrum disorders (ASD). Cochrane Database Syst. Rev. 2012, 10, CD009260. [Google Scholar] [CrossRef] [PubMed]
| Measure Name (Short Name) | Short Description of the Dimension(s) Measured | Admin. Age (Months) | Number of Items | Type of Answer | Admin. Time (Minute) | Admin. Method | Cut-Off | N° of Validation Studies Included |
|---|---|---|---|---|---|---|---|---|
| Autism Detection in Early Childhood (ADEC) | Social interaction behaviors and social communication behaviors. | 12–36 | 16 | 3-point Likert scale | 10 | Observational checklist for professionals | 11 | 4 |
| Autism Observation Scale for Infants (AOSI) | Social communication behaviors, non- social behaviors, | 6–18 | 18 | 3-point Likert scale | 15-20 | Observational checklist for professionals | n.s. | 3 |
| Baby and Infants Screen for Children with aUtIsm Traits (BISCUIT) | Part 1 ASD symptoms; Part 2 comorbid psychopathology; Part 3 behavioral problems. | 17–37 | Part 1: 62; Part 2: 65; Part 3: 17. | 3-point Likert scale | 15 | Parent-interview | Part 1: 17; Part 2: 39; Part 3: 17. | 5 |
| Checklist for Early Signs of Developmental Disorders | Language and social functioning. | 3–39 | 25 | Yes/No | Not declared | Parent-reported questionnaire | 2 | 1 |
| CHecklist for Autism in Toddlers (CHAT) | Social play, social interest, pretend play, joint-attention, proto-declarative pointing, imitation; B functional play, proto-imperative pointing, motor development, rough and tumble play. | 18 | Part A: 9; Part B: 5 | Yes/No | 15 | Part A: parent- reported questionnaire; Part B: professionals- reported questionnaire | 3 key item | 2 |
| Developmental Behavior Checklist: Early Screen (DBC-ES) | Social, verbal, and non-verbal communication, restricted and repetitive behaviors and interests | 18–48 | 17 | 3-point Likert scale | 5–10 | Parent-reported questionnaire | 11 | 1 |
| Early Screening of Autistic Traits Questionnaire (ESAT) | Social- communication skills, stereotyped behaviors, reactions | 14–15 | 14 | Yes/No | 5–10 | Parent-reported questionnaire | 3 | 2 |
| First Year Inventory (FYI) | Social communication and sensory regulatory domains. | 12 | 63 | 4 point Likert scale; multiple choice; two open-ended question. | 10 | Parent-reported questionnaire | 30 (95th); 40 (98th); 50 (99th) [73] (Reznick et al., 2007); 22.55 (95th); 28.14 (98th) [39]; 19.2 (96th) [84]. | 3 |
| Joint Attention OBServation (JA- OBS) | Joint attention | 20–48 | 5 | Yes/No | 10 | Observational checklist for professionals | 2 | 1 |
| Modified Checklist for Autism in Toddlers (M- CHAT) | Social interest, pretend and functional play, joint-attention, proto-declarative pointing, imitation, motor development, rough and tumble play. | 16–30 | 23 | Yes/No | 5–10 | Parent-reported questionnaire | 2 for the critical items (2–7–9–13–14–15) or 3 for the total score | 13 |
| Modified Checklist for Autism in Toddlers-Revised with Follow-up (M-CHAT-R/F) | Social interest, pretend and functional play, joint-attention, proto-declarative pointing, imitation, motor development, rough and tumble play. | 16–30 | 20 | Yes/No | 5–10 | Parent-reported interview | 0–2: low risk 3–7: moderate risk 8–20: high risk | 7 |
| Parent Observation of Early Markers Scale (POEMS) | Social and communicative development, restricted interests, behavioral and emotional problems. | 1–24 | 61 | 4-point Likert Scale | 30 | Parent-reported questionnaire | 70 | 1 |
| Quantitative CHecklist for Autism in Toddlers (Q- CHAT) | Social communication, behavior, and language. | 18–24 | 25 | 5-point Likert scale | 5–10 | Parent-reported questionnaire | n.s. | 2 |
| Screening for Infants with Developmental Deficits and/or Autism (SEEK) | I: sleep, eating, and parent-child interaction; II: regulation, parent-child interaction, communication, and coordination stability. | 8 | SEEK I: 6; SEEK II: 33 | Yes/No | 3–-40 | Parent-reported questionnaire and observational checklist for professionals | n.s. | 1 |
| Three-Item Direct Observation Screen (TIDOS) | Joint attention, eye contact and response to name. | 18–60 | 3 | Yes/no | 15–20 | Observational checklist for professionals | 1 | 1 |
| Young Autism and other developmental disorders CHeckup Tool: 18-month-olds’ version (YACHT-18) | Motor functions, communication and social interaction, pointing, and language comprehension. | 18 | I: questionnaire (11 items); II: interview (6 questions); II: picture card test. | I: yes/no; III: pass/fail | 10 | Professionals - reported questionnaire; interview with caregivers, child observation | n.s. | 1 |
| Measure | Author(s) (Year) | Study Design | Population and Subgroups | Application Level (1, 2, or “Hybrid”) | Sens. | Spec. | PPV(NPV) |
|---|---|---|---|---|---|---|---|
| ADEC | [34] | Cross sect. | Study 1 N = 19 ASD N = 13 ODD N = 29 gen pop. Study 2 N = 34 PDD N = 15 gen. pop. N = 5 ODD | hybrid | range: 79%–94% | range: 88%–100% | Study 1: 0.75 (0.90) Study 2: 1 (0.71) |
| [35] | Long. | N = 55 ASD | Hybrid | 100% | 89% | 0.84 (1 *) | |
| [36] | Cross sect. | N = 70 ASD N = 24 PDD-NOS N = 57 ODD N = 64 gen. pop. | Hybrid | 100% | range: 74%–90% | 0.84 (1) | |
| [37] | Cross-sect. | N = 96 DC | 2 | range: 93%–94% | range: 62%–64% | 0.83 (0.81) | |
| AOSI | [38] | Cross sect. | N = 101 GR | 2 | N/A | N/A | N/A |
| [39] | Long. | N = 115 GR N = 73 DC | 2 | N/A | N/A | N/A | |
| [40] | Cross sect. | N = 54 GR N = 50 DC | 2 | N/A | N/A | N/A | |
| BISCUIT | [41] | Cross-sect. | Study 1 N = 957 DC Study 2 N = 171 ASD N = 144 PDD-NOS | 2 | Part 1: 84.7%; Part 2: 84.4%; Part 3: 93.4% | Part 1: 86.4%; Part 2: 83.3%; Part 3: 86.6% | N/A |
| [42] | Cross-sect. | N = 178 ASD N = 152 PDD-NOS N = 677 gen. pop. | Hybrid | N/A | N/A | N/A | |
| [43] | Cross-sect. | N = 276 DC | 2 | N/A | N/A | N/A | |
| [44] | Cross-sect. | Study 1 N = 405 ASD Study 2 N = 405 ASD N = 882 gen. pop. | Hybrid | N/A | N/A | N/A | |
| [45] | Cross-sect. | N = 178 ASD N = 152 PDD-NOS N = 677 gen. pop. | Hybrid | N/A | N/A | N/A | |
| CESDD | [46] | Long. | Wave 1 N = 6.808 gen. pop. Wave 2 N = 255 at risk Wave 3 N = 20 ASD N = 40 ODD | 1 | 80% | 94% | 0.07 (0.99) |
| CHAT | [47] | Cross-sect. | N = 50 gen. pop. N = 41 GR | 2 | N/A | N/A | N/A |
| [48] | Long. | Wave 1 N = 16.000 gen. pop. Wave 2 N = 10 ASD N = 17 ODD N = 23 TD | 1 | N/A | N/A | N/A | |
| DBC-ES | [49] | Cross-sect. | N = 142 ASD or PDD N = 65 ODD | Hybrid | 83% | 48% | 0.78(0.56) |
| ESAT | [50] | Long. | Wave 1 N = 31.724 gen. pop Wave 2 N = 255 at risk Wave 3 N = 18 ASD N = 55 ODD. | 1 | N/A | N/A | N/A |
| [51] | Long. | Wave 1 N = 4.107 gen. pop. Wave 2 N = 103 at risk | 1 | N/A | N/A | N/A | |
| FYI | [52] | Cross-sect. | N = 1300 gen. pop. | 1 | N/A | N/A | N/A |
| [53] | Long. | Wave 1 N = 471 gen. pop. Wave 2 N = 17 at risk | 1 | N/A | N/A | N/A | |
| [54] | Long. | Wave 1 N = 699 gen. pop. Wave 2 N = 9 ASD | 1 | N/A | N/A | N/A | |
| JA-OBS | [55] | Long. | Wave 1 N = 3999 Wave 2 N = 64 at risk Wave 3 N = 48 ASD N = 3 TD N = ODD | 1 | 86% | N/A | 0.90 (N/A) |
| M-CHAT | [56] | Long. | Wave 1 N = 1.122 gen. pop.; Wave 2 N = 171 at risk | 1 | 87% | 99% | 0.80 (0.99) |
| [57] | Cross-sect. | N = 36 ASD N = 18 PDD-NOS N = 28 ODD | Hybrid | Critic items: 79%; Total score: 88% | Critic items: 38%; Total score: 38% | 0.79(0.28) | |
| [58] | Cross-sect. | N = 122 ASD N = 106 gen. pop. | Hybrid | 86% | 80% | 0.81(0.93) | |
| [59] | Long. | Study 1 Wave 1 N = 2480 gen. pop.; Wave 2 N = 23 ASD N = 63 ODD Study 2: Wave 1 N = 2055 gen. pop. Wave 2 N = 6 ASD N = ODD | 1 | 100% | 98% | Study 1: 0.35 (1) Study 2: 0.19 (1) | |
| [60] | Cross-sect. | N = 24 gen. pop. N = 25 DC | 2 | Critic items: 75%; Total score: 65% | Critic items: 89%; Total score: 88% | 0.21(0.98) | |
| [61] | Cross-sect. | N = 117 ASD N = 339 gen. pop. | Hybrid | N/A | N/A | N/A | |
| [62] | Cross-sect. | N = 141 ASD N = 102 ODD | Hybrid | range: 70%–97% | range: 38%–99% | N/A | |
| [63] | Cross-sect. | N = 447 gen. pop. | 1 | ||||
| [64] | Cross-sect. | N = 552 DC | 2 | range: 70%–97% | range: 38%–99% | N/A | |
| [65] | Long. | Wave 1 N = 51.853 gen. pop. Wave 2 N = 173 ASD | 1 | Critic items: 20.8%; total score: 34.1% | Critic items: 97.9%; total score: 92.7% | Critic items: 0.33 (N/A); total score: 0.15 (N/A) | |
| [66] | Cross-sect. | N = 2048 gen. pop. | 1 | N/A | N/A | N/A | |
| [67] | Long. | Wave 1 N = 420 gen. pop. Wave 2 N = 2 ASD | 1 | N/A | N/A | N/A | |
| [68] | Long. | Wave 1 N = 1250 DC Wave 2 N = 18 ASD N = 17 ODD N = 1 TD | 2 | 67% | With FUI: 99%; Without FUI: 94% | With FUI: 0.60 (0.99) Without FUI: 0.14 (0.99) | |
| M-CHAT-R/F | [69] | Long. | Study 1 N = 3309 DC N = 484 GR; Study 2 Wave 1: N = 1.160 DC N = 256 = GR Wave 2 N = 80 ASD N = 51 ODD | 2 | N/A | N/A | N/A |
| [70] | Cross-sect. | N = 207 DC | 2 | N/A | N/A | N/A | |
| [71] | Long. | Wave 1 N = 16.115 gen. pop. Wave 2 N = 123 ASD N = 140 ODD | 1 | 94% | 83% | 0.50 (0.99) | |
| [72] | Long. | Wave 1 N = 2594 gen. pop. Wave 2 N = 253 at risk Wave 3 N = 17 ASD | 1 | N/A | N/A | N/A | |
| [73] | Cross-sect. | N = 20 DC N = 128 TD | 2 | N/A | N/A | N/A | |
| [74] | Long. | Wave 1 N = 110 gen. pop. Wave 2 N = 18 ASD | 1 | 88.9% | 94.6% | 0.76 (0.97) | |
| [75] | Long. | Wave 1 N = 7928 gen. pop. Wave 2 N = 1140 at risk Wave 3 N = 72 ASD | 1 | 96% | 86% | 0.69 (1) | |
| [76] | Cross-sect. | N = 947 gen. pop. | 1 | 50% | 100% | 100(0.87) | |
| POEMS | [77] | Cross-sect. | N = 108 GR | 2 | 74% | 73% | 0.21 (N/A) |
| Q-CHAT | [78] | Cross sect. | N = 779 gen. pop. N = 160 ASD | Hybrid | N/A | N/A | N/A |
| [79] | Cross-sect. | N = 764 gen. pop. | 1 | N/A | N/A | N/A | |
| [80] | Cross-sect. | N = 139 ASD N = 50 PDD N = 126 TD | 2 | 73–83% | 76–78% | N/A | |
| [81] | Cross-sect. | N = 2400 | 1 | N/A | N/A | N/A | |
| [82] | Cross-sect. | N = 545 | 1 | N/A | N/A | N/A | |
| SEEK | [83] | Cross-sect. | N = 312 gen. pop. | 1 | N/A | N/A | N/A |
| TIDOS | [84] | Cross-sect. | N = 86 ASD N = 76 ODD N = 97 gen. pop. | Hybrid | 95% | 85% | 0.91(0.90) |
| YACHT-18 | [85] | Cross-sect. | N = 2.814 gen. pop. | 1 | 60% | 86.3% | N/A |
| Measures | Author(s), (Years) | Psychometric Properties | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Internal Consistency | Reliability | Measurement Error | Content Validity | Structural Validity | Hypothesis Testing | Cross-Cultural Validity | Criterion Validity | Responsiveness | ||
| ADEC | [34] | 0 unidimensionality, sample | + missing item, sample, time interval | 0 sample | 0 sample | 0 sample | ||||
| [35] | + missing item | + missing item | ||||||||
| [36] | 0 unidimensionality | 0 time interval | + missing item | + missing item | + missing item | |||||
| [37] | 0 unidimensionality | + missing item, hypothesis | + missing item | |||||||
| AOSI | [38] | + sample, missing item | +++ | |||||||
| [39] | + missing item | + missing item | ||||||||
| [40] | + missing item | + missing item | + missing item | + missing item | ||||||
| BISCUIT | [41] | 0 comparator instrument | 0 statistical methods | |||||||
| [42] | + missing item, hypothesis, comparator instrument | + missing item | ||||||||
| [43] | 0 unidimensionality | |||||||||
| [44] | + missing item | +++ | + missing item | + missing item | 0 statistical method | |||||
| [45] | 0 unidimensionality | + missing item, hypothesis | 0 no gold standard | |||||||
| CESDD | [46] | + hypothesis | + missing item | |||||||
| CHAT | [47] | +++ | + ++ | 0 comparator instrument | 0 no gold standard | |||||
| [48] | + missing item | + missing item | ||||||||
| DBC-ES | [49] | 0 unidimensionality | 0 only one measurement | + missing item, hypothesis | + missing item | |||||
| ESAT | [50] | 0 time interval | + missing item, hypothesis | + missing item | ||||||
| [51] | + missing item | + missing item | ||||||||
| FYI | [52] | +++ | +++ | 0 statistical method | ++ | +++ | ||||
| [53] | 0 statistical method | ++ | 0 statistical method | ++ | ||||||
| [54] | 0 time interval, measurement condition | + sample | + missing item, sample | + missing item, statistical method | ||||||
| JA-OBS | [55] | 0 only one measurement | + missing item | |||||||
| M-CHAT | [56] | +++ | . | + missing item, sample | 0 missing item | |||||
| [57] | 0 unidimensionality | ++ | ++ | |||||||
| [58] | + missing item | |||||||||
| [59] | + missing item, hypothesis | 0 missing item, translation | + missing item | |||||||
| [60] | 0 sample, unidimensionality | 0 sample | 0 sample, hypothesis | 0 sample, comparator instrument | ||||||
| [61] | 0 unidimensionality | + missing item, hypothesis | + missing item | |||||||
| [62] | +++ | 0 statistical method | ||||||||
| [63] | 0 measurement not independent | 0 comparator instrument | ||||||||
| [64] | 0 only one measurement | 0 comparison instrument | ||||||||
| [65] | + time interval | + sample, hypothesis | 0 missing item | |||||||
| [66] | +++ | |||||||||
| [67] | + missing item | 0 statistical method | ||||||||
| [68] | 0 missing item, hypothesis | 0 missing item, sample | ||||||||
| M-CHAT-R/F | [69] | 0 unidimensionality | 0 measurement not indipendent | + missing item | 0 statistical method | 0 statistical method | ||||
| [70] | + missing item | |||||||||
| [71] | 0 unidimensionality | 0 administration not similar, statistical method | + hypothesis | +++ | ||||||
| [72] | 0 sample, unidimensionality | 0 time interval, statistical method | ++ | 0 expertise translator, statistcal method | 0 sample | |||||
| [73] | 0 sample, undimensionality | 0 missing, sample, time interval, statistical method | 0 statistical method | |||||||
| [74] | + missing item | 0 comparator instrument | + translation | 0 no golden standard | ||||||
| [75] | 0 undimensionality | 0 statistical method | 0 hypothesis | 0 no pilot study, statistical method | +++ | |||||
| [76] | 0 comparator instrument | |||||||||
| POEMS | [77] | 0 unidimensionality | ++ | +++ | 0 hypothesis | 0 statistical methods | ||||
| Q-CHAT | [78] | +++ | + measurement condition | +++ | + hypothesis | |||||
| [79] | +++ | 0 time interval | +++ | + hypothesis | 0 comparator instrument | |||||
| [80] | +++ | 0 comparator instrument | +++ | |||||||
| [81] | +++ | +++ | 0 comparator instrument | 0 statistical method | ||||||
| [82] | + missing item | + missing item | + missing item | 0 no pilot study; statistical method | ||||||
| SEEK | [83] | +++ | ||||||||
| TIDOS | [84] | +++ | + missing item | + missing item | ||||||
| YACHT- 18 | [85] | + missing item | ||||||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Petrocchi, S.; Levante, A.; Lecciso, F. Systematic Review of Level 1 and Level 2 Screening Tools for Autism Spectrum Disorders in Toddlers. Brain Sci. 2020, 10, 180. https://doi.org/10.3390/brainsci10030180
Petrocchi S, Levante A, Lecciso F. Systematic Review of Level 1 and Level 2 Screening Tools for Autism Spectrum Disorders in Toddlers. Brain Sciences. 2020; 10(3):180. https://doi.org/10.3390/brainsci10030180
Chicago/Turabian StylePetrocchi, Serena, Annalisa Levante, and Flavia Lecciso. 2020. "Systematic Review of Level 1 and Level 2 Screening Tools for Autism Spectrum Disorders in Toddlers" Brain Sciences 10, no. 3: 180. https://doi.org/10.3390/brainsci10030180
APA StylePetrocchi, S., Levante, A., & Lecciso, F. (2020). Systematic Review of Level 1 and Level 2 Screening Tools for Autism Spectrum Disorders in Toddlers. Brain Sciences, 10(3), 180. https://doi.org/10.3390/brainsci10030180







