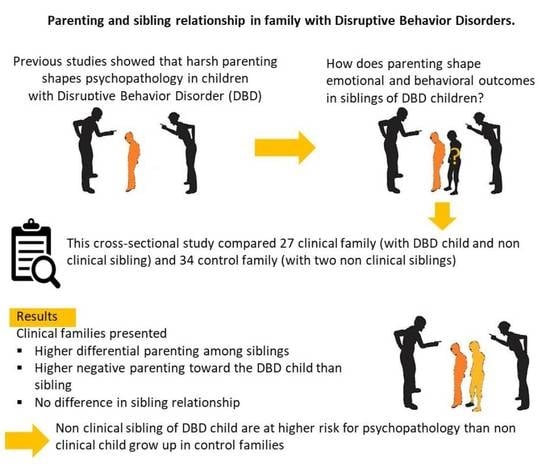
Parenting and Sibling Relationships in Family with Disruptive Behavior Disorders. Are Non-Clinical Siblings More Vulnerable for Emotional and Behavioral Problems?
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sample
2.2. Measures
2.3. Data Analysis
3. Results
3.1. Difference between Clinical and Control Group Families
3.2. Difference within Sibling Dyad
3.3. Difference between Clinical, Non-Clinical Siblings and Control Group
3.4. DESR and DP Profile
4. Discussion
5. Strengths and Limitations of this Study
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Coghill, D. Editorial: Do clinical services need to take conduct disorder more seriously? J. Child Psychol. Psychiatry 2013, 54, 921–923. [Google Scholar] [CrossRef] [PubMed]
- Polanczyk, G.V.; Salum, G.A.; Sugaya, L.S.; Caye, A.; Rohde, L.A. Annual research review: A meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J. Child Psychol. Psychiatry 2015, 56, 345–365. [Google Scholar] [CrossRef]
- Patalay, P.; Gage, S.H. Changes in millennial adolescent mental health and health-related behaviours over 10 years: A popula-tion cohort comparison study. Int. J. Epidemiol. 2019, 48, 1650–1664. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5); American Psychiatric Asso-ciation: Philadelphia, PA, USA, 2013. [Google Scholar]
- Moffitt, T.E.; Arseneault, L.; Jaffee, S.R.; Kim-Cohen, J.; Koenen, K.C.; Odgers, C.L.; Slutske, W.S.; Viding, E. Research review: DSM-V conduct disorder: Research needs for an evidence base. J. Child Psychol. Psychiatry 2008, 49, 3–33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burke, J.D.; Hipwell, A.E.; Loeber, R. Dimensions of oppositional defiant disorder as predictors of depression and conduct disorder in preadolescent girls. J. Am. Acad. Child Adolesc. Psychiatry 2010, 49, 484–492. [Google Scholar] [CrossRef] [PubMed]
- Fairchild, G.; Hawes, D.J.; Frick, P.J.; Copeland, W.E.; Odgers, C.L.; Franke, B.; Freitag, C.M.; De Brito, S.A. Conduct Disorder. Nat. Rev. 2019, 5, 43. [Google Scholar] [CrossRef]
- Pardini, D.A.; Frick, P.J.; Moffitt, T.E. Building an evidence base for DSM-5 conceptualizations of oppositional defiant disorder and conduct disorder: Introduction to the special section. J. Abnorm. Psychol. 2010, 119, 683–688. [Google Scholar] [CrossRef] [Green Version]
- Rivenbark, J.G.; Odgers, C.L.; Caspi, A.; Harrington, H.; Hogan, S.; Houts, R.M.; Poulton, R.; Moffitt, T.E. The high societal costs of childhood conduct problems: Evidence from administrative records up to age 38 in a longitudinal birth cohort. J. Child Psychol. Psychiatry 2018, 59, 703–710. [Google Scholar] [CrossRef]
- Karwatowska, L.; Russell, S.; Solmi, F.; De Stavola, B.L.; Jaffee, S.; Pingault, J.-B.; Viding, E. Risk factors for disruptive behaviours: Protocol for a systematic review and meta-analysis of quasi-experimental evidence. BMJ Open 2020, 10, e038258. [Google Scholar] [CrossRef]
- Jucksch, V.; Salbach-Andrae, H.; Lenz, K.; Goth, K.; Döpfner, M.; Poustka, F.; Holtmann, M. Severe affective and behavioural dysregulation is associated with significant psychosocial adversity and impairment. Child Psychol. Psychiatry 2011, 52, 686–695. [Google Scholar] [CrossRef]
- Biederman, J.; Perry, C.R.; Day, H.; Goldin, R.L.; Spencer, T.; Faraone, S.V.; Surman, C.B.; Wozniak, J. Severity of the aggression/anxiety-depression/attention (A-A-A) CBCL profile discriminates between different levels of deficits in emotional regulation in youth with ADHD. J. Dev. Behav. Pediatr. 2012, 33, 236–243. [Google Scholar] [CrossRef] [Green Version]
- Masi, G.; Muratori, P.; Manfredi, A.; Lenzi, F.; Polidori, L.; Ruglioni, L.; Muratori, F.; Milone, A. Response to treatments in youths with disruptive behavior disorders. Compr. Psychiatry 2013, 54, 1009–1015. [Google Scholar] [CrossRef]
- Masi, G.; Pisano, S.; Milone, A.; Muratori, P. Child behavior checklist dysregulation profile in children with disruptive behavior disorders: A longitudinal study. J. Affect. Disord. 2015, 186, 249–253. [Google Scholar] [CrossRef] [PubMed]
- Caspi, A. The child is father of the man: Personality continuities from childhood to adulthood. J. Pers. Soc. Psychol. 2000, 78, 158–172. [Google Scholar] [CrossRef] [PubMed]
- Cavanagh, M.; Quinn, D.; Duncan, D.; Graham, T.; Balbuena, L.J. Oppositional Defiant Disorder Is Better Conceptualized as a Disorder of Emotional Regulation. J. Atten. Disord. 2017, 21, 381–389. [Google Scholar] [CrossRef] [PubMed]
- Tremblay, R.E. Developmental origins of disruptive behaviour problems: The ‘original sin’ hypothesis, epigenetics and their consequences for prevention. J. Child Psychol. Psychiatry 2010, 51, 341–367. [Google Scholar] [CrossRef] [PubMed]
- Pederson, C.A.; Fite, P.J. The impact of parenting on the associations between child aggression subtypes and oppositional defiant disorder symptoms. Child Psychiatry Hum. Dev. 2014, 45, 728–735. [Google Scholar] [CrossRef]
- Bornovalova, M.A.; Hicks, B.M.; Iacono, W.G.; McGue, M. Familial transmission and heritability of childhood disruptive disorders. Am. J. Psychiatry 2010, 167, 1066–1074. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Caspi, A.; McClay, J.; Moffitt, T.E.; Mill, J.; Martin, J.; Craig, I.W.; Taylor, A.; Poulton, R. Role of genotype in the cycle of violence in maltreated children. Science 2002, 297, 851–854. [Google Scholar] [CrossRef]
- Rowe, R.; Costello, E.J.; Angold, A.; Copeland, W.E.; Maughan, B. Developmental pathways in oppositional defiant disorder and conduct disorder. J. Abnorm. Psychol. 2010, 119, 726–738. [Google Scholar] [CrossRef] [Green Version]
- Tistarelli, N.; Fagnani, C.; Troianiello, M.; Stazi, M.A.; Adriani, W. The nature and nurture of ADHD and its comorbidities: A narrative review on twin studies. Neurosci. Biobehav. Rev. 2020, 109, 63–77. [Google Scholar] [CrossRef] [PubMed]
- Malmberg, K.; Wargelius, H.L.; Lichtenstein, P.; Oreland, L.; Larsson, J.O. ADHD and Disruptive Behavior scores—Associations with MAO-A and 5-HTT genes and with platelet MAO-B activity in adolescents. BMC Psychiatry 2008, 8, 28. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stormshak, E.A.; Bierman, K.L.; McMahon, R.J.; Lengua, L.J. Parenting practices and child disruptive behavior problems in early elementary school. J. Clin. Child Psychol. 2000, 29, 17–29. [Google Scholar] [CrossRef] [PubMed]
- Calkins, S.D.; Keane, S.P. Developmental origins of early antisocial behavior. Dev. Psychopathol. 2009, 21, 1095–1109. [Google Scholar] [CrossRef] [Green Version]
- Muratori, P.; Milone, A.; Nocentini, A.; Manfredi, A.; Polidori, L.; Ruglioni, L.; Lambruschi, F.; Masi, G.; Lochmann, J.E. Maternal Depression and Parenting Practices Predict Treatment Outcome in Italian Children with Disruptive Behavior Disorder. J. Child Fam. Stud. 2015, 24, 2805–2816. [Google Scholar] [CrossRef]
- Clark, J.E.; Frick, P.J. Positive parenting and callous-unemotional traits: Their association with school behavior problems in young children. J. Clin. Child Adolesc. Psychol. 2016, 47, S242–S254. [Google Scholar] [CrossRef]
- Waller, R.; Gardner, F.; Hyde, L.W. What are the associations between parenting, callous–unemotional traits, and antisocial behavior in youth? A systematic review of evidence. Clin. Psychol. Rev. 2013, 33, 593–608. [Google Scholar] [CrossRef]
- Waller, R.; Gardner, F.; Viding, E.; Shaw, D.S.; Dishion, T.J.; Wilson, M.N.; Hyde, L.W. Bidirectional associations between pa-rental warmth, callous unemotional behavior, and behavior problems in high-risk preschoolers. J. Abnorm. Child Psychol. 2014, 42, 1275–1285. [Google Scholar] [CrossRef] [Green Version]
- Muratori, P.; Lochman, J.E.; Lai, E.; Milone, A.; Nocentini, A.; Pisano, S.; Righini, E.; Masi, G. Which dimension of parenting predicts the change of callous unemotional traits in children with disruptive behavior disorder? Compr. Psychiatry 2016, 69, 202–210. [Google Scholar] [CrossRef] [PubMed]
- Patterson, G.R. The early development of coercive family process. In Antisocial Behavior in Children and Adolescents: A Developmental Analysis and Model for Intervention; Reid, J.B., Patterson, G.R., Snyder, J., Eds.; American Psychological Association: Washington, DC, USA, 2002. [Google Scholar]
- Pettit, G.S.; Arsiwalla, D.D. Commentary on special section on “bidirectional parent–child relationships”: The continuing evolution of dynamic, transactional models of parenting and youth behavior problems. J. Child Psychol. Psychiatry 2008, 36, 711–718. [Google Scholar] [CrossRef] [PubMed]
- Deater-Deckard, K. Annotation: Recent research examining the role of peer relationships in the development of psychopathology. J. Child Psychol. Psychiatry 2001, 42, 565–579. [Google Scholar] [CrossRef]
- Richmond, M.K.; Stocker, C.M.; Rienks, S.L. Longitudinal associations between sibling relationship quality, parental differential treatment, and children’s adjustment. J. Fam. Psychol. 2005, 19, 550–559. [Google Scholar] [CrossRef]
- Asbury, K.; Dunn, J.; Plomin, R. Birthweight-discordance and differences in early parenting relate to monozygotic twin differences in behaviour problems and academic achievement at age 7. Dev. Sci. 2006, 9, 22–31. [Google Scholar] [CrossRef]
- Asbury, K.; Dunn, J.; Plomin, R. The use of discordant MZ twins to generate hypotheses regarding non-shared environmental influence on anxiety in middle childhood. Soc. Dev. 2006, 15, 564–570. [Google Scholar] [CrossRef]
- Burt, S.A.; McGue, M.; Iacono, W.G.; Krueger, R.F. Differential Parent-child Relationships and Adolescent Externalizing Symptoms: Cross-Lagged Analyses within a Twin Differences Design. Dev. Psychol. 2006, 42, 1289–1298. [Google Scholar] [CrossRef] [Green Version]
- Mullineaux, P.Y.; Deater-Deckard, K.; Petrill, S.A.; Thompson, L.A. Parenting and child behaviour problems: A longitudinal analysis of non-shared environment. Infant Child Dev. 2009, 18, 133–148. [Google Scholar] [CrossRef] [Green Version]
- Ilomäki, E.; Viilo, K.; Hakko, H.; Marttunen, M.; Mäkikyrö, T.; Räsänen, P. Familial risks, conduct disorder and violence: A Finnish study of 278 adolescent boys and girls. Eur. Child Adolesc. Psychiatry 2006, 15, 46–51. [Google Scholar] [CrossRef] [PubMed]
- Feinberg, M.E.; Hetherington, E.M. Differential parenting as a within-family variable. J. Fam. Psychol. 2001, 15, 22–37. [Google Scholar] [CrossRef] [PubMed]
- Stocker, C.M.; McHale, S. The nature and family correlates of preadolescents’ perceptions of their sibling relationships. J. Soc. Pers. Relat. 1992, 9, 179–185. [Google Scholar] [CrossRef]
- Dalsgaard, S.; Ostergaard, S.D.; Leckman, J.F.; Mortensen, P.B.; Pedersen, M.G. Mortality in children, adolescents, and adults with attention deficit hyperactivity disorder: A nationwide cohort study. Lancet 2015, 385, 2190–2196. [Google Scholar] [CrossRef]
- Maibing, C.F.; Pedersen, C.B.; Benros, M.E.; Mortensen, P.B.; Dalsgaard, S.; Nordentoft, M. Risk of schizophrenia increases after all child and adolescent psychiatric disorders: A nationwide study. Schizophr. Bull. 2015, 41, 963–970. [Google Scholar] [CrossRef] [Green Version]
- Erskine, H.E.; Ferrari, A.J.; Polanczyk, G.V.; Moffitt, T.E.; Murray, C.J.; Vos, T.; Whiteford, H.A.; Scott, J.G. The global burden of conduct disorder and attention-deficit/hyperactivity disorder in 2010. J. Child Psychol. Psychiatry 2014, 55, 328–336. [Google Scholar] [CrossRef]
- Carrà, E.; Marta, E. Relazioni Familiari e Adolescenza [Family Relationships and Adolescence]; Franco Angeli: Milano, Italy, 1995. [Google Scholar]
- Scabini, E. Parent–child relationships in Italian families: Connectedness and autonomy in the transition to adulthood. Psicol. Teor. Pesqui. 2000, 16, 023–030. [Google Scholar] [CrossRef]
- McArdle, P.; Wiegersma, A.; Gilvarry, E.; Kolte, B.; McCarthy, S.; Fitzgerald, M.; Brinkley, A.; Blom, M.; Stoeckel, I.; Pierolini, A.; et al. European adolescent substance use: The roles of family structure, function and gender. Addiction 2002, 97, 329–336. [Google Scholar] [CrossRef] [Green Version]
- Smorti, M.; Guarnieri, S.; Ingoglia, S. The parental bond, resistance to peer influence, and risky driving in adolescence. Transp. Res. Part F Traffic Psychol. Behav. 2014, 22, 184–195. [Google Scholar] [CrossRef]
- Brody, G.H.; Stoneman, Z.; McCoy, J.K. Associations of maternal and paternal direct and differential behavior with sibling relationships: Contemporaneous and longitudinal analyses. Child Dev. 1992, 63, 82–92. [Google Scholar] [CrossRef] [PubMed]
- McHale, S.M.; Updegraff, K.A.; Whiteman, S.D. Sibling Relationships and Influences in Childhood and Adolescence. J. Marriage Fam. 2012, 74, 913–930. [Google Scholar] [CrossRef] [PubMed]
- Singer, A.T.; Weinstein, R.S. Differential parental treatment predicts achievement and self-perceptions in two cultural contexts. J. Fam. Psychol. 2000, 14, 491–509. [Google Scholar] [CrossRef]
- Shanahan, L.; McHale, S.M.; Crouter, A.C.; Osgood, D. Linkages between parents’ differential treatment, youth depressive symptoms, and sibling relationships. J. Marriage Fam. 2008, 70, 480–494. [Google Scholar] [CrossRef]
- Tamrouti-Makkink, I.D.; Dubas, J.S.; Gerris, J.R.; van Aken, M.A. The relation between the absolute level of parenting and differential parental treatment with adolescent siblings’ adjustment. J. Child Psychol. Psychiatry 2004, 45, 1397–1406. [Google Scholar] [CrossRef]
- Kaufman, J.; Birmaher, B.; Brent, D.; Rao, U.; Flynn, C.; Moreci, P.; Williamson, D.; Ryan, N. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): Initial reliability and validity data. J. Am. Acad. Child Adolesc. Psychiatry 1997, 36, 980–988. [Google Scholar] [CrossRef] [PubMed]
- Wechsler, D. WISC-IV Technical and Interpretive Manual; The Psychological Association: San Antonio, TX, USA, 2003. [Google Scholar]
- Achenbach, T.; Rescorla, L. Manual for the ASEBA School-Age Forms & Profiles; University of Vermont: Burlington, VT, USA, 2001. [Google Scholar]
- Achenbach, T.M.; Dumenci, L.; Rescorla, L.A. DSM-oriented and empirically based approaches to constructing scales from the same item pools. J. Clin. Child Adolesc. Psychol. 2003, 32, 328–340. [Google Scholar] [CrossRef] [PubMed]
- Frigerio, A.; Vanzin, L.; Pastore, V.; Nobile, M.; Giorda, R.; Marino, C.; Molteni, M.; Rucci, P.; Ammaniti, M.; Lucarelli, L.; et al. The Italian preadolescent mental health project (PrISMA): Rationale and methods. Int. J. Methods Psychiatr. Res. 2006, 5, 22–35. [Google Scholar] [CrossRef] [PubMed]
- Masi, G.; Muratori, P.; Manfredi, A.; Pisano, S.; Milone, A. Child Behaviour Checklist emotional dysregulation profiles in youth with disruptive behaviour disorders: Clinical correlates and treatment implications. Psychiatry Res. 2015, 225, 191–196. [Google Scholar] [CrossRef]
- Muratori, P.; Pisano, S.; Milone, A.; Masi, G. Is emotional dysregulation a risk indicator for auto-aggression behaviors in adolescents with oppositional defiant disorder? J. Affect. Disord. 2017, 208, 110–112. [Google Scholar] [CrossRef]
- Biederman, J.; Petty, C.R.; Monuteaux, M.C.; Evans, M.; Parcell, T.; Faraone, S.V.; Wozniak, J. The child behavior checklist-pediatric bipolar disorder profile predicts a subsequent diagnosis of bipolar disorder and associated impairments in ADHD youth growing up: A longitudinal analysis. J. Clin. Psychiatry 2009, 70, 732–740. [Google Scholar] [CrossRef]
- Ayer, L.; Althoff, R.; Ivanova, M.; Rettew, D.; Waxler, E.; Sulman, J.; Hudziak, J. Child Behavior Checklist Juvenile Bipolar Disorder (CBCL-JBD) and CBCL Posttraumatic Stress Problems (CBCL-PTSP) scales are measures of a single dysregulatory syndrome. J. Child Psychol. Psychiatry 2009, 50, 1291–1300. [Google Scholar] [CrossRef]
- Holtmann, M.; Buchmann, A.F.; Esser, G.; Schmidt, M.H.; Banaschewski, T.; Laucht, M. The Child Behavior Checklist-Dysregulation Profile predicts substance use, suicidality, and functional impairment: A longitudinal analysis. J. Child Psychol. Psychiatry 2011, 52, 139–147. [Google Scholar] [CrossRef]
- Sheldon, K.K.; Frick, P.J.; Wootton, J. Assessment of parenting practices in families of elementary school-age children. J. Clin. Child Psychol 1996, 25, 317–329. [Google Scholar] [CrossRef]
- Esposito, A.; Servera, M.; Garcia-Banda, G.; Del Giudice, E. Factor analysis of the Italian version of the Alabama Parenting Questionnaire in a community sample. J. Child. Fam. Stud. 2016, 25, 1208–1217. [Google Scholar] [CrossRef]
- Stocker, C.M.; Lanthier, R.P.; Furman, W. Sibling relationships in early adulthood. J. Fam. Psychol. 1997, 11, 210–221. [Google Scholar] [CrossRef]
- Lecce, S.; De Bernart, D.; Vezzani, C.; Pinto, G.; Primi, C. Measuring the quality of the sibling relationship during middle childhood: The psychometric properties of the Sibling Relationship Inventory. Eur. J. Dev. Psychol. 2011, 8, 423–436. [Google Scholar] [CrossRef]
- Curran, P.J.; West, S.G.; Finch, J.F. The robustness of test statistics to non normality and specification error in confirmatory factor analysis. Psychol. Methods 1996, 1, 16–29. [Google Scholar] [CrossRef]
- Burke, J.D.; Pardini, D.A.; Loeber, R. Reciprocal relationships between parenting behavior and disruptive psychopathology from childhood through adolescence. J. Abnorm. Child Psychol. 2008, 36, 679–692. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tung, I.; Lee, S.S. Negative parenting behavior and childhood oppositional defiant disorder: Differential moderation by positive and negative peer regard. Aggress. Behav. 2014, 40, 79–90. [Google Scholar] [CrossRef]
- Dunn, J.F.; Stocker, C.; Plomin, R. Nonshared experiences within the family: Correlates of behavioral problems in middle childhood. Dev. Psychopathol. 1990, 2, 113–125. [Google Scholar] [CrossRef]
- Jeannin, R.; Van Leeuwen, K. Associations between direct and indirect perceptions of parental differential treatment and child socio-emotional adaptation. J. Child Fam. Stud. 2015, 24, 1838–1855. [Google Scholar] [CrossRef]
- Hart, M.S.; Kelley, M.L. Fathers’ and mothers’ work and family issues as related to internalizing and externalizing behavior of children attending day dare. J. Fam. Stress 2006, 27, 252–270. [Google Scholar] [CrossRef]
- Spratt, E.G.; Saylor, C.F.; Macias, M.M. Assessing parenting stress in multiple samples of children with special needs (CSN). Fam. Syst. Health 2007, 25, 435–449. [Google Scholar] [CrossRef]
- Abidin, R.R. Parenting Stress Index, 2nd ed.; Pediatric Psychology Press: Charlottesville, VA, USA, 1986. [Google Scholar]
- Deater-Deckard, K.; Scarr, S. Parenting stress among dual-earner mothers and fathers: Are there gender differences? J. Fam. Psychol. 1996, 1, 45–59. [Google Scholar] [CrossRef]
- Le, Y.; Fredman, S.J.; Feinberg, M.E. Parenting stress mediates the association between negative affectivity and harsh parenting: A longitudinal dyadic analysis. J. Fam. Psychol. 2017, 31, 679–688. [Google Scholar] [CrossRef]
- Mak, M.C.K.; Yin, L.; Li, M.; Cheung, R.Y.-H.; Oon, P.-T. The Relation between Parenting Stress and Child Behavior Problems: Negative Parenting Styles as Mediator. J. Child Fam. Stud. 2020, 29, 2993–3003. [Google Scholar] [CrossRef]
- Qi, C.H.; Kaiser, A.P. Behavior problems of preschool children from low-income families: Review of the literature. Top. Early Child. Spec. Educ. 2003, 23, 188–216. [Google Scholar] [CrossRef]
- Bradley, R.H.; Corwyn, R.F. Externalizing problems in fifth grade: Relations with productive activity, maternal sensitivity, and harsh parenting from infancy through middle childhood. Dev. Psychol. 2007, 43, 1390–1401. [Google Scholar] [CrossRef]
- Craine, J.L.; Tanaka, T.A.; Nishina, A.; Conger, K.J. Understanding adolescent delinquency: The role of older siblings’ delinquency and popularity with peers. Merrill-Palmer Q. 2009, 55, 436. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Defoe, I.N.; Keijsers, L.; Hawk, S.T.; Branje, S.; Dubas, J.S.; Buist, K.; Frijns, T.; van Aken, M.A.; Koot, H.M.; van Lier, P.A.; et al. Siblings versus parents and friends: Longitudinal linkages to adolescent externalizing problems. J. Child Psychol. Psychiatry 2013, 54, 881–889. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pinquart, M. Associations of parenting dimensions and styles with externalizing problems of children and adolescents: An updated meta-analysis. Dev. Psychol. 2017, 53, 873. [Google Scholar] [CrossRef]
- Jacobs, R.H.; Becker-Weidman, E.G.; Reinecke, M.A.; Jordan, N.; Silva, S.G.; Rohde, P.; March, J.S. Treating depression and oppositional behavior in adolescents. J Clin. Child Adolesc. Psychol. 2010, 39, 559–567. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nock, M.K.; Kazdin, A.E.; Hiripi, E.; Kessler, R.C. Lifetime prevalence, correlates and persistence of oppositional defiant dis-order: Results from the National Comorbidity Survey Replication. J. Child Psychol. Psychiatry 2007, 48, 703–713. [Google Scholar] [CrossRef] [PubMed]
- Masi, G.; Milone, A.; Paciello, M.; Lenzi, F.; Muratori, P.; Manfredi, A.; Polidoi, L.; Ruglioni, L.; Lochman, J.E.; Muratori, F. Effi-cacy of a multimodal treatment for disruptive behavior disorders in children and adolescents: Focus on internalizing problems. Psychiatry Res. 2014, 219, 617–624. [Google Scholar] [CrossRef] [PubMed]
- Muratori, P.; Milone, A.; Manfredi, A.; Polidori, L.; Ruglioni, L.; Lambruschi, F.; Masi, G.; Lochman, J.E. Evaluation of Improvement in Externalizing Behaviors and Callous-Unemotional Traits in Children with Disruptive Behavior Disorder: A 1-Year Follow Up Clinic-Based Study. Adm. Policy Ment. Health Ment. Health Serv. Res. 2017, 44, 452–462. [Google Scholar] [CrossRef] [PubMed]
- Aitken, M.; Battaglia, M.; Marino, C.; Mahendran, N.; Andrade, B.F. Clinical utility of the CBCL Dysregulation Profile in children with disruptive behavior. J. Affect. Disord. 2019, 15, 87–95. [Google Scholar] [CrossRef] [PubMed]
- Spencer, T.J.; Faraone, S.V.; Surman, C.B.H.; Petty, C.; Clarke, A.; Batchelder, H.; Wozniak, J. Towards defining deficient emo-tional self-regulation in youth with attention deficit hyperactivity disorder using the Child Behavior Checklist: A controlled study. Postgrad. Med. J. 2011, 123, 50–59. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eyberg, S.M.; Nelson, M.M.; Boggs, S.R. Evidence-based psychosocial treatments for children and adolescents with disruptive behavior. J. Clin. Child Adolesc. Psychol. 2008, 37, 215–237. [Google Scholar] [CrossRef] [PubMed]
- Lochman, J.E.; Powell, N.P.; Boxmeyer, C.L.; Jimenez-Camargo, L. Cognitive behavioral therapy for externalizing disorders in children and adolescents. Child Adolesc. Psychiatr. Clin. N. Am. 2011, 20, 305–318. [Google Scholar] [CrossRef] [PubMed]
- Kochanska, G.; Kim, S.; Boldt, L.J.; Yoon, J.E. Children’s callous-unemotional traits moderate links between their positive relationships with parents at preschool age and externalizing behavior problems at early school age. J. Child Psychol. Psychiatry Allied Discip. 2013, 54, 1251–1260. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garland, A.F.; Hawley, K.M.; Brookman-Frazee, L.; Hurlburt, M.S. Identifying common elements of evidence-based psycho-social treatments for children’s disruptive behaviour problems. J. Am. Acad. Child Adolesc. Psychiatry 2008, 47, 5–15. [Google Scholar] [CrossRef]
- Smorti, M.; Ponti, L. How Does Sibling Relationship Affect Children’s Prosocial Behaviors and Best Friend Relationship Quality? J. Fam. Issues 2018, 39, 2413–2436. [Google Scholar] [CrossRef]
- Newman, J. Conflict and friendship in sibling relationships: A review. Child Study J. 1994, 24, 119–152. [Google Scholar]
- Gass, K.; Jenkins, J.; Dunn, J. Are sibling relationships protective? A longitudinal study. J. Child Psychol. Psychiatry 2007, 48, 167–175. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Erlbaum: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Chen, D.; Drabick, D.A.G.; Burgers, D.E. A Developmental Perspective on Peer Rejection, Deviant Peer Affiliation, and Conduct Problems among Youth. Child Psychiatry Hum. Dev. 2015, 46, 823–838. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feinberg, M.E.; Solmeyer, A.R.; McHale, S.M. The Third Rail of Family Systems: Sibling Relationships, Mental and Behavioral Health, and Preventive Intervention in Childhood and Adolescence. Clin. Child Fam. Psychol. Rev. 2012, 15, 43–57. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Clinical Group n = 27 | Control Group n = 34 | Statistics | |
|---|---|---|---|
| Parental marital status | Chi2(1) = 1.23; n.s. | ||
| Married | 20 (74%) | 28 (82%) | |
| Divorced | 7 (26%) | 6 (18%) | |
| N children for family | Chi2(3) = 4.42; n.s. | ||
| 2 | 15 (56%) | 25 (74%) | |
| 3 | 8 (30%) | 6 (17%) | |
| 4 | 3 (5%) | 2 (6%) | |
| 5 | 1 (4%) | 1 (3%) | |
| Maternal SES | Chi2(3) = 6.66; n.s. | ||
| salariat | 6 (22.2%) | 9 (26.5%) | |
| intermediate | 15 (55.6%) | 22 (64.7%) | |
| working class | 2 (7.4%) | 0 (0%) | |
| unemployed | 4 (14.8%) | 3 (8.8%) | |
| Paternal SES | Chi2(3) = 6.18; n.s. | ||
| salariat | 9 (33.3%) | 8 (23.5%) | |
| intermediate | 10 (37%) | 19 (55.9%) | |
| working class | 7 (25.9%) | 7 (10.6%) | |
| unemployed | 1 (3.7%) | 0 (0%) |
| Clinical Group | t(26) | p | Control Group | t(33) | p | |||
|---|---|---|---|---|---|---|---|---|
| DBD | S-DBD | CONTR-1 | CONTR-2 | |||||
| APQ positive parenting | 47.67 (4.60) | 47.37 (4.65) | 0.497 | n.s. | 46.65 (5.01) | 47.23 (5.26) | −1.31 | n.s. |
| APQ negative parenting | 14.67 (4.22) | 12.14 (4.14) | 2.58 | 0.016 | 10.79 (3.59) | 10.73 (3.54) | 0.208 | n.s. |
| APQ corporal punishment | 4.41 (2.20) | 4.33 (1.68) | 0.311 | n.s. | 3.53 (0.896) | 3.91 (1.28) | −1.97 | n.s. |
| SRI affection | 21.72 (6.96) | 24.36 (5.74) | −1.51 | n.s. | 24.38 (3.29) | 22.52 (4.86) | 1.88 | n.s. |
| SRI conflict | 15.76 (4.09) | 13.89 (3.55) | 1.659 | n.s. | 13.41 (4.01) | 14.08 (4.01) | −0.99 | n.s. |
| SRI rivarly | 8.04 (3.86) | 7.88 (3.44) | 0.148 | n.s. | 6.85 (3.40) | 6.58 (2.54) | 0.40 | n.s. |
| DBD | S-DBD | CONTR | F (2117) | p | Adjusted η2 | Post-Hoc | |
|---|---|---|---|---|---|---|---|
| M (SD) | M (SD) | M (SD) | |||||
| APQ | |||||||
| Positive parenting | 47.67 (4.60) | 47.37 (4.65) | 47.10 (5.12) | 0.182 | n.s. | 0.003 | |
| Negative parenting | 14.67 (4.22) | 12.14 (4.14) | 10.76 (3.54) | 9.00 | 0.000 | 0.132 | DBD > CONTR |
| Corporal punishment | 4.41 (2.20) | 4.33 (1.68) | 3.72 (1.12) | 2.44 | n.s. | 0.040 | |
| SRI | |||||||
| Affection | 21.72 (6.96) | 24.36 (5.74) | 23.46 (4.23) | 2.16 | n.s. | 0.036 | |
| Conflict | 15.76 (4.09) | 13.89 (3.55) | 13.75 (4.0) | 2.91 | n.s. | 0.026 | |
| Rivalry | 8.04 (3.86) | 7.88 (3.44) | 6.69 (2.98) | 2.50 | n.s. | 0.041 | |
| CBCL | |||||||
| Internalizing | 62.56 (8.75) | 56.62 (9.41) | 49.82 (10.54) | 13.57 | 0.000 | 0.188 | DBD > S-DBD > CONTR |
| Externalizing | 66.93 (8.45) | 54.0 (8.29) | 46.48 (7.65) | 55.67 | 0.000 | 0.488 | DBD > S-DBD > CONTR |
| Anxious/depressed | 64.78 (8.87) | 57.81 (6.90) | 54.30 (5.74) | 18.22 | 0.000 | 0.238 | DBD > S-DBD > CONTR |
| Withdrawn/Depressed | 60.93 (8.53) | 57.88 (9.83) | 54.28 (6.53) | 5.70 | 0.004 | 0.089 | DBD > S-DBD > CONTR |
| Somatic complain | 56.15 (6.55) | 56.29 (5.17) | 54.60 (5.39) | 1.05 | n.s. | 0.018 | |
| Social prob. | 62.44 (6.36) | 55.96 (5.86) | 53.49 (4.68) | 23.75 | 0.000 | 0.289 | DBD > S-DBD > CONTR |
| Thought prob. | 61.33 (7.30) | 54.92 (5.63) | 53.39 (5.24) | 15.72 | 0.000 | 0.212 | DBD > S-DBD > CONTR |
| Attention prob. | 67.15 (8.07) | 60.07 (8.49) | 53.15 (3.75) | 46.98 | 0.000 | 0.445 | DBD > S-DBD > CONTR |
| Rules breaking | 61.81 (8.11) | 55.62 (4.87) | 52.03 (3.37) | 32.72 | 0.000 | 0.359 | DBD > S-DBD > CONTR |
| Aggressive behavior | 69.33 (10.84) | 56.0 (6.63) | 52.12 (3.17) | 60.06 | 0.000 | 0.507 | DBD > S-DBD > CONTR |
| DSM Affective prob. | 65.04 (8.06) | 58.85 (7.66) | 54.18 (5.98) | 21.23 | 0.000 | 0.266 | DBD > S-DBD > CONTR |
| DSM anxiety prob. | 63.74 (8.01) | 58.40 (7.74) | 55.27 (6.08) | 11.03 | 0.000 | 0.159 | DBD > S-DBD > CONTR |
| DSM somatic prob. | 54.56 (7.98) | 54.22 (4.79) | 54.10 (4.92) | 0.03 | n.s. | 0.001 | |
| DSM ADHD prob. | 67.93 (9.32) | 58.44 (8.93) | 52.03 (3.04) | 52.16 | 0.000 | 0.471 | DBD > S-DBD > CONTR |
| DSM ODT | 65.33 (8.99) | 55.70 (5.29) | 52.63 (3.25) | 44.20 | 0.000 | 0.430 | DBD > S-DBD > CONTR |
| DSM conduct prob. | 65.19 (8.72) | 54.92 (4.92) | 51.69 (2.97) | 56.81 | 0.000 | 0.493 | DBD > S-DBD > CONTR |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Smorti, M.; Inguaggiato, E.; Vezzosi, L.; Milone, A. Parenting and Sibling Relationships in Family with Disruptive Behavior Disorders. Are Non-Clinical Siblings More Vulnerable for Emotional and Behavioral Problems? Brain Sci. 2021, 11, 1308. https://doi.org/10.3390/brainsci11101308
Smorti M, Inguaggiato E, Vezzosi L, Milone A. Parenting and Sibling Relationships in Family with Disruptive Behavior Disorders. Are Non-Clinical Siblings More Vulnerable for Emotional and Behavioral Problems? Brain Sciences. 2021; 11(10):1308. https://doi.org/10.3390/brainsci11101308
Chicago/Turabian StyleSmorti, Martina, Emanuela Inguaggiato, Lara Vezzosi, and Annarita Milone. 2021. "Parenting and Sibling Relationships in Family with Disruptive Behavior Disorders. Are Non-Clinical Siblings More Vulnerable for Emotional and Behavioral Problems?" Brain Sciences 11, no. 10: 1308. https://doi.org/10.3390/brainsci11101308
APA StyleSmorti, M., Inguaggiato, E., Vezzosi, L., & Milone, A. (2021). Parenting and Sibling Relationships in Family with Disruptive Behavior Disorders. Are Non-Clinical Siblings More Vulnerable for Emotional and Behavioral Problems? Brain Sciences, 11(10), 1308. https://doi.org/10.3390/brainsci11101308