Managing Sleep in Adults with ADHD: From Science to Pragmatic Approaches
Abstract
:1. Introduction
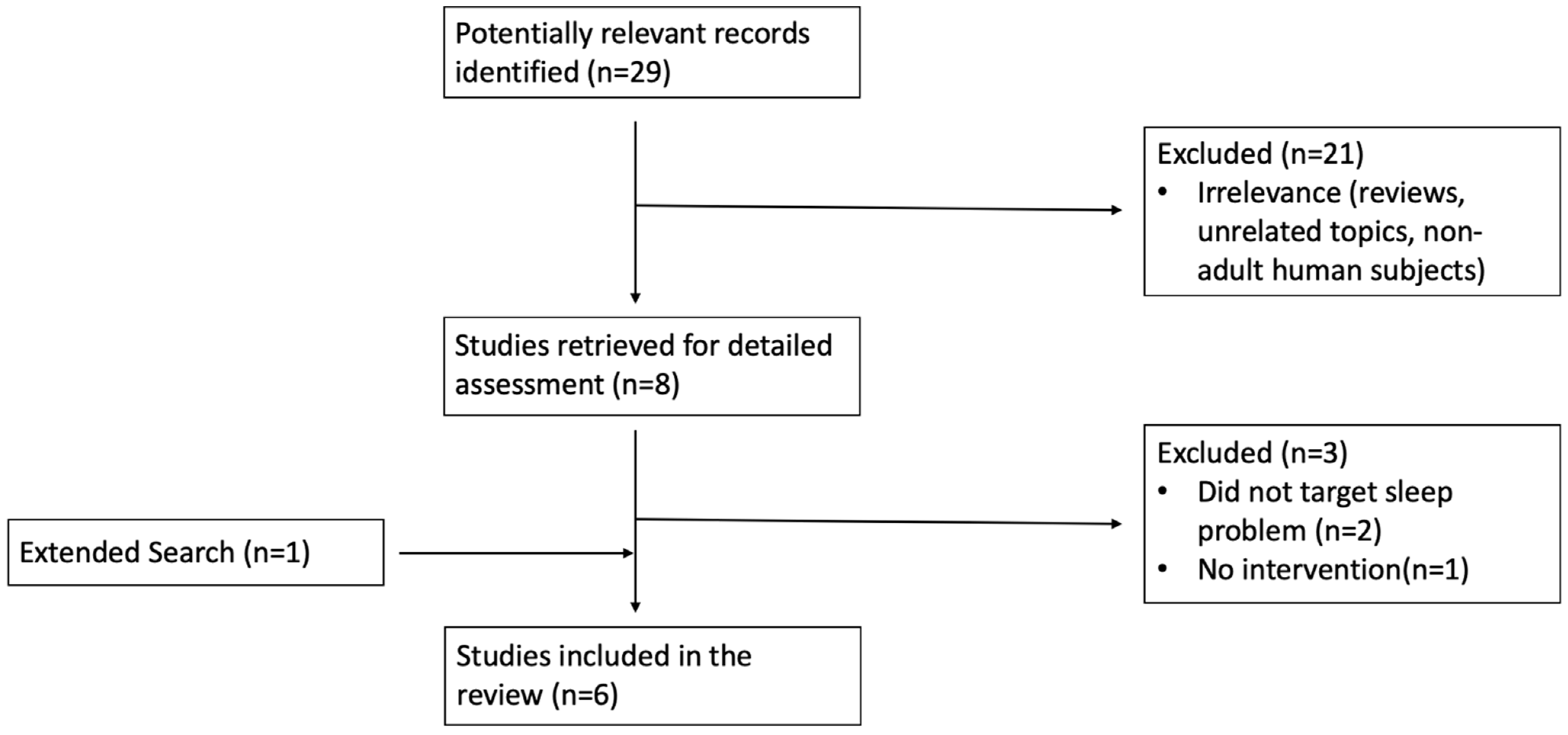
2. Materials and Methods
3. Results
4. Discussion
4.1. Approaches for Assessing Sleep Problems and Disorders in Adults with ADHD
4.2. Approaches to Treating Sleep Disorders in ADHD
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Murphy, K.; Barkley, R.A. Attention Deficit Hyperactivity Disorder Adults: Comorbidities and Adaptive Impairments. Compr. Psychiatry 1996, 37, 393–401. [Google Scholar] [CrossRef]
- Hammerness, P.; Surman, C.; Miller, K. Update on Adult Attention-Deficit/Hyperactivity Disorder. Curr. Neurol. Neurosci. Rep. 2008, 8, 484–489. [Google Scholar] [CrossRef]
- Surman, C. (Ed.) ADHD in Adults: A Practical Guide to Evaluation and Management; Springer: Berlin/Heidelberg, Germany, 2013. [Google Scholar]
- Kessler, R.C.; Adler, L.; Barkley, R.; Biederman, J.; Conners, C.K.; Demler, O.; Faraone, S.V.; Greenhill, L.L.; Howes, M.J.; Secnik, K.; et al. The prevalence and correlates of adult ADHD in the United States: Results from the National Comorbidity Survey Replication. Am. J. Psychiatry 2006, 163, 716–723. [Google Scholar] [CrossRef] [PubMed]
- Polanczyk, G.; de Lima, M.S.; Horta, B.L.; Biederman, J.; Rohde, L.A. The Worldwide Prevalence of ADHD: A Systematic Review and Metaregression Analysis. Am. J. Psychiatry 2007, 164, 942–948. [Google Scholar] [CrossRef] [PubMed]
- Fayyad, J.; De Graaf, R.; Kessler, R.; Alonso, J.; Angermeyer, M.; Demyttenaere, K.; De Girolamo, G.; Haro, J.M.; Karam, E.G.; Lara, C.; et al. Cross-national prevalence and correlates of adult attention-deficit hyperactivity disorder. Br. J. Psychiatry 2007, 190, 402–409. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tsai, F.J.; Tseng, W.L.; Yang, L.K.; Gau, S.S.F. Psychiatric comorbid patterns in adults with attention-deficit hyperactivity disorder: Treatment effect and subtypes. PLoS ONE 2019, 14, e0211873. [Google Scholar] [CrossRef] [PubMed]
- Voinescu, B.I.; Szentagotai, A.; David, D. Sleep Disturbance, Circadian Preference and Symptoms of Adults with Attention Deficit Hyperactivity Disorder (ADHD). J. Neural Transm. 2012, 199, 1195–1204. [Google Scholar] [CrossRef]
- Scammell, T.; Thomas, R.; Galaburda, A.; Matheson, J. Sleep disorders are common among adults referred for attention deficit hyperactivity disorder. Sleep 1998, 21, 167. [Google Scholar]
- Roth, T.; Jaeger, S.; Jin, R.; Kalsekar, A.; Stang, P.E.; Kessler, R.C. Sleep Problems, Comorbid Mental Disorders, and Role Functioning in the National Comorbidity Survey Replication (NCSR). Biol. Psychiatry 2006, 60, 1364–1371. [Google Scholar] [CrossRef] [Green Version]
- Kooij, J.J.; Middelkoop, H.A.; van Gils, K.; Buitelaar, J.K. The effect of stimulants on nocturnal motor activity and sleep quality in adults with ADHD: An open-label case-control study. J. Clin. Psychiatry 2001, 62, 952–956. [Google Scholar] [CrossRef]
- Philipsen, A.; Feige, B.; Hesslinger, B.; Ebert, D.; Carl, C.; Hornyak, M.; Lieb, K.; Voderholzer, U.; Riemann, D. Sleep in Adults With Attention-Deficit/Hyperactivity Disorder: A Controlled Polysomnographic Study Including Spectral Analysis of the Sleep EEG. Sleep 2005, 28, 877–884. [Google Scholar] [CrossRef]
- Schredl, M.; Alm, B.; Sobanski, E. Sleep quality in adult patients with attention deficit hyperactivity disorder (ADHD). Eur. Arch. Psychiatry Clin. Neurosci. 2006, 257, 164–168. [Google Scholar] [CrossRef]
- Surman, C.B.; Adamson, J.J.; Petty, C.; Biederman, J.; Kenealy, D.C.; Levine, M.; Mick, E.; Faraone, S. Association Between Attention Deficit/Hyperactivity Disorder and Sleep Impairment in Adulthood: Evidence from a Large Controlled Study. J. Clin. Psychiatry 2009, 70, 1523–1529. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 3rd ed.; American Psychiatric Association: Arlington, TX, USA, 1980. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Arlington, TX, USA, 2013. [Google Scholar]
- Van Veen, M.M.; Kooij, J.J.S.; Boonstra, A.M.; Gordijn, M.C.M.; Van Someren, E.J.W. Delayed Circadian Rhythm In Adults with Attention-Deficit/Hyperactivity Disorder and Chronic Sleep-Onset Insomnia. Biol. Psychiatry 2010, 67, 1091–1096. [Google Scholar] [CrossRef] [PubMed]
- Coogan, A.N.; McGowan, N.M. A Systematic Review of Circadian Function, Chronotype and Chronotherapy in Attention Deficit Hyperactivity Disorder. ADHD Atten. Def. Hyp. Disord. 2017, 9, 129–147. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.; Dinges, D.F. A Meta-Analysis of the Impact of Short-Term Sleep Deprivation on Cognitive Variables. Psychol. Bull. 2010, 136, 375–389. [Google Scholar] [CrossRef] [PubMed]
- Goel, N.; Rao, H.; Durmer, J.S.; Dinges, D.F. Neurocognitive consequences of sleep deprivation. Semin. Neurol. 2009, 29, 320–339. [Google Scholar] [CrossRef] [Green Version]
- Surman, C.B.; Thomas, R.J.; Aleardi, M.; Pagano, C.; Biederman, J. Adults with ADHD and Sleep Complaints: A Pilot Study Identifying Sleep-Disordered Breathing Using Polysomnography and Sleep Quality Assessment. J. Atten. Disord. 2006, 9, 550–555. [Google Scholar] [CrossRef] [PubMed]
- Engleman, H.M.; Kingshott, R.N.; Martin, S.E.; Douglas, N.J. Cognitive Function in the Sleep Apnoea/Hypopnoea Syndrome (SAHS). Sleep 2000, 23, 102–108. [Google Scholar]
- Beebe, D.W.; Groesz, L.; Wells, C.; Nichols, A.; McGee, K. The Neuropsychological Effects of Obstructive Sleep Apnea: A Meta-Analysis of Norm-Referenced and Case-Controlled Data. Sleep 2003, 26, 298–307. [Google Scholar] [CrossRef]
- Aloia, M.S.; Arnedt, J.T.; Davis, J.D.; Riggs, R.L.; Byrd, D. Neuropsychological Sequelae of Obstructive Sleep Apnea-Hypopnea Syndrome: A Critical Review. J. Int. Neuropsychol. Soc. 2004, 10, 772–785. [Google Scholar] [CrossRef]
- Bioulac, S.; Philip, P. From Japan to Europe: The Importance to Assess Excessive Daytime Sleepiness in Adults with ADHD Symptoms. Sleep Med. 2017, 37, 221. [Google Scholar] [CrossRef]
- Boonstra, A.M.; Kooij, J.J.; Oosterlaan, J.; Sergeant, J.A.; Buitelaar, J.K.; van Someren, E.J. Hyperactive Night and Day? Actigraphy Studies in Adult ADHD: A Baseline Comparison and the Effect of Methylphenidate. Sleep 2007, 30, 433–442. [Google Scholar] [CrossRef] [PubMed]
- Van Andel, E.; Bijlenga, D.; Vogel, S.W.N.; Beekman, A.T.F.; Kooij, J.J.S. Effects of Chronotherapy on Circadian Rhythm and ADHD Symptoms in Adults with Attention-Deficit Hyperactivity Disorder and Delayed Sleep Phase Syndrome: A Randomized Controlled Trial. Chronobiol. Int. 2021, 38, 260–269. [Google Scholar] [CrossRef]
- Fargason, R.E.; Fobian, A.D.; Hablitz, L.M.; Paul, J.R.; White, B.A.; Cropsey, K.L.; Gamble, K.L. Correcting Delayed Circadian Phase with Bright Light Therapy Predicts Improvement in ADHD Symptoms: A Pilot Study. J. Psychiatr. Res. 2017, 19, 105–110. [Google Scholar] [CrossRef]
- Rybak, Y.E.; McNeely, H.E.; Mackenzie, B.E.; Jain, U.R.; Levitan, R.D. An Open Trial of Light Therapy in Adult Attention-Deficit/Hyperactivity Disorder. J. Clin. Psychiatry 2006, 67, 1527–1535. [Google Scholar] [CrossRef]
- Jernelov, S.; Larsson, Y.; Llenas, M.; Nasri, B.; Kaldo, V. Effects and Clinical Feasibility of a Behavioral Treatment for Sleep Problems in Adult Attention Deficit Hyperactivity Disorder (ADHD): A Pragmatic Within-Group Pilot Evaluation. BMC Psychiatry 2019, 19, 226. [Google Scholar] [CrossRef] [Green Version]
- Ekholm, B.; Spulber, S.; Adler, M. A Randomized Controlled Study of Weighted Chain Blankets for Insomnia in Psychiatric Disorders. J. Clin. Sleep Med. 2020, 16, 1567–1577. [Google Scholar] [CrossRef]
- Fargason, R.E.; Gamble, K.; Avis, K.T.; Besing, R.C.; Jackson, C.W.; Cates, M.E.; May, R. Ramelteon for Insomnia Related to Attention Deficit/Hyperactivity Disorder (ADHD). Psychopharmacol. Bull. 2011, 44, 32–53. [Google Scholar] [PubMed]
- Ruigt, G.S.; Kemp, B.; Groenhout, C.M.; Kamphuisen, H.A. Effect of the Antidepressant Org 3770 On Human Sleep. Eur. J. Clin. Pharmacol. 1990, 38, 551–554. [Google Scholar] [CrossRef]
- Surman, C.B.; Roth, T.J. Impact of stimulant pharmacotherapy on sleep quality: Post hoc analyses of 2 large, double-blind, randomized, placebo-controlled trials. Clin. Psychiatry 2011, 72, 903–908. [Google Scholar] [CrossRef]
- Surman, C.B.; Robertson, B.; Chen, J.; Cortese, S. Post-Hoc Analyses of the Effects of Baseline Sleep Quality on SHP465 Mixed Amphetamine Salts Extended-Release Treatment Response in Adults with Attention-Deficit/Hyperactivity Disorder. CNS Drugs 2019, 33, 695–706. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fadeuilhe, C.; Daigre, C.; Richarte, V.; Grau-López, L.; Palma-Álvarez, R.F.; Corrales, M.; Ramos-Quiroga, J.A. Insomnia Disorder in Adult Attention-Deficit/Hyperactivity Disorder Patients: Clinical, Comorbidity, and Treatment Correlates. Front. Psychiatry 2021, 12, 663889. [Google Scholar] [CrossRef] [PubMed]
- Dietch, J.R.; Sethi, K.; Slavish, D.C.; Taylor, D.J. Validity of two retrospective questionnaire versions of the Consensus Sleep Diary: The whole week and split week self-assessment of sleep surveys. Sleep Med. 2019, 63, 127–136. [Google Scholar] [CrossRef] [PubMed]
- Johns, M.W. A New Method for Measuring Daytime Sleepiness: The Epworth Sleepiness Scale. Sleep 1991, 14, 540–545. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Horne, J.A.; Ostberg, O. A Self-Assessment Questionnaire to Determine Morningness-Eveningness in Human Circadian Rhythms. Int. J. Chronobiol. 1976, 4, 97–110. [Google Scholar] [PubMed]
- Roenneberg, T.; Wirz-Justice, A.; Merrow, M. Life Between Clocks: Daily Temporal Patterns of Human Chronotypes. J. Biol. Rhythms. 2003, 18, 80–90. [Google Scholar] [CrossRef] [Green Version]
- Bernhardt, L.; Brady, E.M.; Freeman, S.C.; Polmann, H.; Réus, J.C.; Flores-Mir, C.; De Luca Canto, G.; Robertson, N.; Squire, I.B. Diagnostic Accuracy of Screening Questionnaires for Obstructive Sleep Apnoea in Adults in Different Clinical Cohorts: A Systematic Review and Meta-Analysis. Sleep Breath. 2021, 18, 1–26. [Google Scholar] [CrossRef]
- Ferri, R.; Lanuzza, B.; Cosentino, F.I.; Iero, I.; Tripodi, M.; Spada, R.S.; Toscano, G.; Marelli, S.; Arico, D.; Bella, R.; et al. A Single Question for the Rapid Screening of Restless Legs Syndrome in the Neurological Clinical Practice. Eur. J. Neurol. 2007, 14, 1016–1021. [Google Scholar] [CrossRef]
- Ottoni, G.L.; Antoniolli, E.; Lara, D.R. The Circadian Energy Scale (CIRENS): Two Simple Questions for a Reliable Chronotype Measurement Based on Energy. Chronobiol. Int. 2011, 28, 229–237. [Google Scholar] [CrossRef]
- Matthews, K.A.; Patel, S.R.; Pantesco, E.J.; Buysse, D.J.; Kamarck, T.W.; Lee, L.; Hall, M.H. Similarities and Differences in Estimates of Sleep Duration by Polysomnography, Actigraphy, Diary, and Self-Reported Habitual Sleep in a Community Sample. Sleep Health 2018, 4, 96–103. [Google Scholar] [CrossRef] [PubMed]
- Surman, C.; Boland, H.; Kaufman, D.; DiSalvo, M. Personalized Remote Mobile Surveys of Adult ADHD Symptoms and Function: A Pilot Study of Usability and Utility for Pharmacology Monitoring. J. Atten. Disord. 2021, in press. [Google Scholar]
- Silverstein, M.J.; Faraone, S.V.; Leon, T.L.; Biederman, J.; Spencer, T.J.; Adler, L.A. The Relationship Between Executive Function Deficits and DSM-5-Defined ADHD Symptoms. J. Atten. Disord. 2020, 24, 41–51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Surman, C.; Bilkey, T.; Weintraub, K. Fast Minds: How to Thrive if You Have ADHD (or Think You Might); Berkeley Press: New York, NY, USA, 2014. [Google Scholar]
- Safren, S.A. Cognitive-behavioral approaches to ADHD treatment in adulthood. J. Clin. Psychiatry 2006, 67, 46–50. [Google Scholar]
- Edinger, J.D.; Wohlgemuth, W.K.; Radtke, R.A.; Marsh, G.R.; Quillian, R.E. Cognitive Behavioral Therapy for Treatment of Chronic Primary Insomnia: A Randomized Controlled Trial. JAMA 2001, 285, 1856–1864. [Google Scholar] [CrossRef]
- Sivertsen, B.; Omvik, S.; Pallesen, S.; Bjorvatn, B.; Havik, O.E.; Kvale, G.; Nielsen, G.H.; Nordhus, I.H. Cognitive Behavioral Therapy vs Zopiclone for Treatment of Chronic Primary Insomnia in Older Adults: A Randomized Controlled Trial. JAMA 2006, 295, 2851–2858. [Google Scholar] [CrossRef]
- Morin, C.M.; Valliéres, A.; Guay, B.; Ivers, H.; Savard, J.; Mérette, C.; Bastien, C.; Baillargeon, L. Cognitive Behavioral Therapy, Singly and Combined with Medication, for Persistent Insomnia: A Randomized Controlled Trial. JAMA 2009, 301, 2005–2015. [Google Scholar] [CrossRef]
- Sateia, M.J.; Buysse, D.J.; Krystal, A.D.; Neubauer, D.N.; Heald, J.L. Clinical Practice Guideline for the Pharmacologic Treatment of Chronic Insomnia in Adults: An American Academy of Sleep Medicine Clinical Practice Guideline. J. Clin. Sleep. Med. 2017, 13, 307–349. [Google Scholar] [CrossRef]
- Vecchierini, M.F.; Kilic-Huck, U.; Quera-Salva, M.A. Members of the MEL Consensus Group of the SFRMS. Melatonin (MEL) and its Use in Neurological Diseases and Insomnia: Recommendations of the French Medical and Research Sleep Society (SFRMS). Rev. Neurol. 2021, 177, 245–259. [Google Scholar] [CrossRef]
- Everitt, H.; Baldwin, D.S.; Stuart, B.; Lipinska, G.; Mayers, A.; Malizia, A.L. Antidepressants for Insomnia in Adults. Cochrane Database Syst. Rev. 2018, 5. [Google Scholar] [CrossRef]
- Gonçalo, A.M.G.; Vieira-Coelho, M.A. The Effects of Trazodone on Human Cognition: A Systematic Review. Eur. J. Clin. Pharmacol. 2021, 7, 1–15. [Google Scholar]
| Study (Year) | Population | Comorbidity and Other Treatments | Intervention | Design | Baseline Characterization Related to Sleep | Significant Findings |
|---|---|---|---|---|---|---|
| Van Andel et al. (2021) [27] | N = 51 DSM-IV ADHD and Delayed Sleep Phase Syndrome, (m = 29.53 yrs) (32 females) | Mental health comorbidity exclusionary, no ADHD supports reported | Advancing melatonin (0.5 mg/d) timed to dim light melatonin onset (DLMO) with and without bright light therapy (BLT), 3 weeks | Three-arm randomized placebo controlled | DLMO, Sleep Diagnosis List (SDL), Sleep Hygiene Questionnaire (VSH) | Melatonin advanced DLMO by 1 h and 28 min, p = 0.001. Melatonin plus BLT advanced DLMO by 1 h and 58, p < 0.001. Placebo had no effect on DLMO. Melatonin reduced ADHD symptoms by 14% p = 0.038, which returned to baseline 2 weeks post-treatment. |
| Fargason et al. (2017) [28] | N = 16 DSM-IV ADHD (m = 35.25 yrs) (9 females) | Mental health comorbidity exclusionary. 11 on amphetamine drugs, 1 on buproprion | BLT, 2 weeks after 1 week baseline | Open treatment | DLMO PSQI Sleep Diary | BLT advanced DLMO by 31 min p = 0.002. vs. 1 week baseline BLT advanced mid-sleep time by 57 min p = 0.004. “Sleepiness” ratings in sleep diary were reduced p = 0.033. PSQI overall quality score improved p < 0.001. |
| Jernelov et al. (2019) [30] | N = 19 people with clinical record of ADHD and self reported sleep problems (m = 37) (13 females) | Participants had an average of 3 mental health conditions in the last year. 11 on forms of amphetamine, 7 on methylphenidate, 8 on current sleep agents | Group sessions of CBT-i for insomnia, 10 weeks | Open treatment with three-month follow up | SLEEP-50 Karolinska Sleep Questionnaire Insomnia Severity Index | Insomnia severity decreased p = 0.002. At three-month follow up, insomnia severity had further improved p < 0.0001 from pre-treatment. |
| Rybak et al. (2006) [29] | N = 29 DSM ADHD by Conner’s and Wender Utah Scales (14 females) | 41% had major depression, 13% had seasonal affective disorder; 7 subjects taking psychostimulants only, 4 taking antidepressants only, 4 taking both | BLT, 3 weeks after 1 week baseline | Open treatment | Brown Adult ADD Scale Conners’ Adult ADD Scale Horne–Ostberg Morningness-Eveningness Questionnaire Neuropsychological Tests | Significant phase advance in circadian preference, p = 0.016, decrease in self-report ADHD symptoms (p = 0.001), and change in 10 out of 18 neuropsychological tests (p range = 0.05 to 0.001). |
| Ekholm et al. (2020) [31] | N = 13 cohort subset with clinical record of sleep disorders and ADHD | Various concurrent treatments | Weighted chain blankets, 4 weeks | Between group (vs. plastic chain blanket) | Insomnia severity index, fatigue symptom inventory, hospital anxiety and depression scale, wrist actigraphy | Insomnia severity improved more than in light blanket group p = 0.003. |
| Fargason et al. (2011) [32] | N = 36 adults (18 females) with DSM-IV ADHD | Individuals with elevated Hamilton Anxiety/Depression ratings or other cause of insomnia excluded. | Ramelteon 8 mg, 2 weeks each of placebo, washout, and active, after 1 week baseline | Open treatment crossover | Actigraphy, Epworth Sleepiness Scale (ESS), and ADHD-RS | 7.0 ± 32.3 min phase advance; placebo 39.2 ± 44.6 min phase delay (p = 0.046 for both); # participants with significant ESS score more than doubled p < 0.017. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Surman, C.B.H.; Walsh, D.M. Managing Sleep in Adults with ADHD: From Science to Pragmatic Approaches. Brain Sci. 2021, 11, 1361. https://doi.org/10.3390/brainsci11101361
Surman CBH, Walsh DM. Managing Sleep in Adults with ADHD: From Science to Pragmatic Approaches. Brain Sciences. 2021; 11(10):1361. https://doi.org/10.3390/brainsci11101361
Chicago/Turabian StyleSurman, Craig B. H., and Daniel M. Walsh. 2021. "Managing Sleep in Adults with ADHD: From Science to Pragmatic Approaches" Brain Sciences 11, no. 10: 1361. https://doi.org/10.3390/brainsci11101361
APA StyleSurman, C. B. H., & Walsh, D. M. (2021). Managing Sleep in Adults with ADHD: From Science to Pragmatic Approaches. Brain Sciences, 11(10), 1361. https://doi.org/10.3390/brainsci11101361





