Age-Related Effect of Sleepiness on Driving Performance: A Systematic-Review
Abstract
1. Introduction
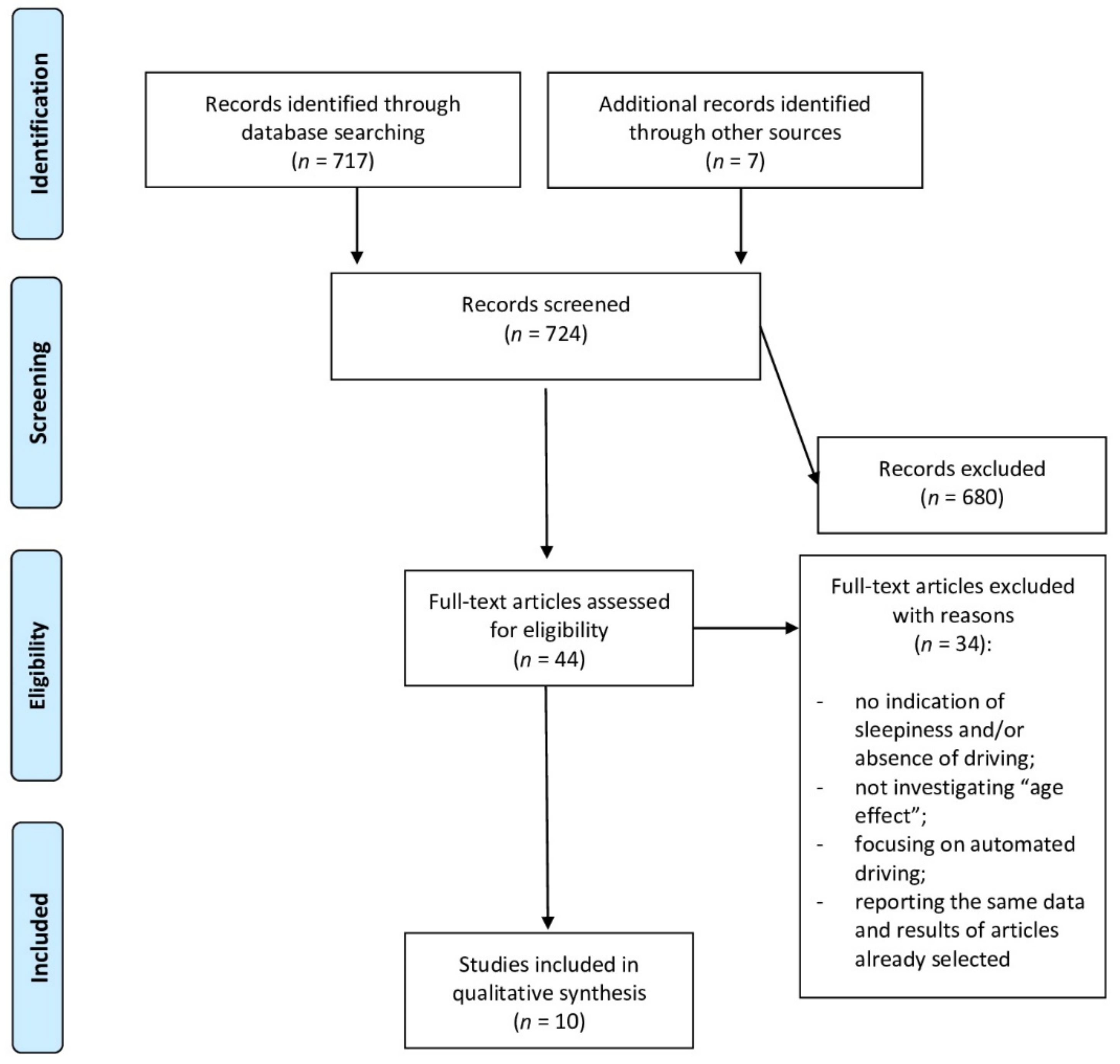
2. Materials and Methods
3. Results
3.1. Self-Reported Sleepiness
3.2. Behavioral Task
3.3. Electrophysiological Pattern
4. Discussion
5. Limitations and Future Perspectives
Author Contributions
Funding
Conflicts of Interest
References
- North, R.V. The relationship between the extent of visual field and driving performance—A review. Ophthalmic. Physiol. Opt. 1985, 5, 205–210. [Google Scholar] [CrossRef]
- Ball, K.; Owsley, C.; Stalvey, B.; Roenker, D.L.; Sloane, M.E.; Graves, M. Driving avoidance and functional impairment in older drivers. Accid. Anal. Prev. 1998, 30, 313–322. [Google Scholar] [CrossRef]
- Carr, D.; Jackson, T.W.; Madden, D.J.; Cohen, H.J. The effect of age on driving skills. J. Am. Geriatr. Soc. 1992, 40, 567–573. [Google Scholar] [CrossRef] [PubMed]
- Moradi, A.; Nazari, S.S.H.; Rahmani, K. Sleepiness and the risk of road traffic accidents: A systematic review and meta-analysis of previous studies. Transp. Res. F Traffic. Psychol. Behav. 2019, 65, 620–629. [Google Scholar] [CrossRef]
- Schreier, D.R.; Banks, C.; Mathis, J. Driving simulators in the clinical assessment of fitness to drive in sleepy individuals: A systematic review. Sleep Med. Rev. 2018, 38, 86–100. [Google Scholar] [CrossRef] [PubMed]
- Dinges, D.F.; Orne, M.T.; Whitehouse, W.G.; Orne, E.C. Temporal placement of a nap for alertness: Contributions of circadian phase and prior wakefulness. Sleep 1987, 10, 313–329. [Google Scholar] [CrossRef] [PubMed]
- Curcio, G.; Casagrande, M.; Bertini, M. Sleepiness: Evaluating and quantifying methods. Int. J. Psychophysiol. 2001, 41, 251–263. [Google Scholar] [CrossRef]
- Garbarino, S.; Durando, P.; Guglielmi, O.; Dini, G.; Bersi, F.; Fornarino, S.M.; Toletone, A.; Chorri, C.; Magnavita, N. Sleep apnea, sleep debt and daytime sleepiness are independently associated with road accidents. A cross-sectional study on truck drivers. PLoS ONE 2016, 11, e0166262. [Google Scholar] [CrossRef]
- World Health Organization. Global Status Report on Road Safety 2018: Summary (No. WHO/NMH/NVI/18.20); World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Horne, J.A.; Reyner, L.A. Sleep related vehicle accidents. BMJ 1995, 310, 565–567. [Google Scholar] [CrossRef]
- Gonçalves, M.; Amici, R.; Lucas, R.; Åkerstedt, T.; Cirignotta, F.; Horne, J.; Léger, D.; McNicholas, W.T.; Partinen, M.; Téran-Santos, J.; et al. Sleepiness at the wheel across Europe: A survey of 19 countries. J. Sleep Res. 2015, 24, 242–253. [Google Scholar] [CrossRef]
- World Health Organization. Global Status Report on Road Safety 2013: Supporting a Decade of Action: Summary (No. WHO. NMH. VIP 13.01). 2013. Available online: https://www.who.int/substance_abuse/msbalcstragegy.pdf (accessed on 10 July 2021).
- Philip, P.; Taillard, J.; Micoulaud-Franchi, J.A. Sleep restriction, sleep hygiene, and driving safety: The importance of situational sleepiness. Sleep Med. Clin. 2019, 14, 407–412. [Google Scholar] [CrossRef] [PubMed]
- Langlois, P.H.; Smolensky, M.H.; Hsi, B.P.; Weir, F.W. Temporal patterns of reported single-vehicle car and truck accidents in Texas, USA during 1980–1983. Chronobiol. Int. 1985, 2, 131–140. [Google Scholar] [CrossRef]
- Zomer, J.; Lavie, P. Sleep-related automobile accidents—When and who? In Sleep _90; Horne, J.A., Ed.; Pontenagel Press: Bochum, Germany, 1990; pp. 448–451. [Google Scholar]
- Pack, A.I.; Pack, A.M.; Rodgman, E.; Cucchiara, A.; Dinges, D.F.; Schwa, C.W. Characteristics of crashes attributed to the driver having fallen asleep. Accid. Anal. Prev. 1995, 27, 769–775. [Google Scholar] [CrossRef]
- Åkerstedt, T.; Kecklund, G. Age, gender and early morning highway accidents. J. Sleep Res. 2001, 10, 105–110. [Google Scholar] [CrossRef] [PubMed]
- National Center for Statistics and Analysis. 2016 Older Population Fact Sheet (Report No. DOT HS 812 500); National Highway Traffic Safety Adminstration: Washington, DC, USA, 2018. [Google Scholar]
- Lyman, S.; Ferguson, S.A.; Braver, E.R.; Williams, A.F. Older driver involvements in police reported crashes and fatal crashes: Trends and projections. Inj. Prev. 2002, 8, 116–120. [Google Scholar] [CrossRef] [PubMed]
- Istituto Nazionale di Statistica. Incidenti Stradali. Aggiornamento del Comunicato Diffuso in Data 25 Luglio 2019. 2019. Available online: https://www.istat.it/it/files//2020/07/Incidenti-stradali-in-Italia-Anno-2019-aggiornamento27ottobre2020.pdf (accessed on 10 July 2021).
- Braver, E.R.; Trempel, R.E. Are older drivers actually at higher risk of involvement in collisions resulting in deaths or non-fatal injuries among their passengers and other road users? Inj. Prev. 2004, 10, 27–32. [Google Scholar] [CrossRef] [PubMed]
- Ball, K.; Owsley, C.; Sloane, M.E.; Roenker, D.L.; Bruni, J.R. Visual attention problems as a predictor of vehicle crashes in older drivers. Invest. Ophthalmol. Vis. Sci. 1993, 34, 3110–3123. [Google Scholar] [PubMed]
- Owsley, C.; Ball, K.; McGwin, G.K.; Sloane, M.E.; Roenker, D.L.; White, M.F.; Overley, E.T. Visual processing impairment and risk of motor vehicle crashes among older adults. JAMA 1998, 279, 1083–1088. [Google Scholar] [CrossRef]
- Stutts, J.C.; Stewart, J.R.; Martell, C. Cognitive test performance and crash risk in an older driver population. Accid. Anal. Prev. 1998, 30, 337–346. [Google Scholar] [CrossRef]
- Marottoli, R.; Richardson, E.; Stowe, M.; Miller, E.G.; Brass, L.M.; Cooney Jr, L.M.; Tinetti, M.E. Development of a test battery to identify older drivers at risk for self-reported adverse driving events. J. Am. Geriatr. Soc. 1998, 46, 562–568. [Google Scholar] [CrossRef]
- Mander, B.A.; Winer, J.R.; Walker, M.P. Sleep and human aging. Neuron 2017, 94, 19–36. [Google Scholar] [CrossRef]
- Ohayon, M.M.; Carskadon, M.A.; Guilleminault, C.; Vitiello, M.V. Meta-Analysis of Quantitative Sleep Parameters From Childhood to Old Age in Healthy Individuals: Developing Normative Sleep Values Across the Human Lifespan. Sleep 2004, 27, 1255–1273. [Google Scholar] [CrossRef]
- Planek, T.W.; Condon, M.E.; Fowler, R.C. An Investigation of the Problems and Opinions of Aged Drivers; National Safety Council: Chicago, IL, USA, 1968. [Google Scholar]
- Hennessy, D.E. Vision Testing of Renewal Applicants: Crashes Predicted When Compensation for Impairment is Inadequate; Research and Development Section, California Department of Motor Vehicles: Sacramento, CA, USA, 1995. [Google Scholar]
- World Health Organization. World Report on Ageing and Health 2015; World Health Organization Press: Geneva, Switzerland, 2015. [Google Scholar]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef]
- Campagne, A.; Pebayle, T.; Muzet, A. Correlation between driving errors and vigilance level: Influence of the driver’s age. Physiol. Behav. 2004, 80, 515–524. [Google Scholar] [CrossRef] [PubMed]
- Lowden, A.; Anund, A.; Kecklund, G.; Peters, B.; Åkerstedt, T. Wakefulness in young and elderly subjects driving at night in a car simulator. Accid. Anal. Prev. 2009, 41, 1001–1007. [Google Scholar] [CrossRef] [PubMed]
- Vaz Fragoso, C.A.; Araujo, K.L.; Van Ness, P.H.; Marottoli, R.A. Prevalence of sleep disturbances in a cohort of older drivers. J. Gerontol. A Biol. Sci. Med. Sci. 2008, 63, 715–723. [Google Scholar] [CrossRef]
- Vaz Fragoso, C.A.; Araujo, K.L.; Van Ness, P.H.; Marottoli, R.A. Sleep disturbances and adverse driving events in a predominantly male cohort of active older drivers. J. Am. Geriatr. Soc. 2010, 58, 1878–1884. [Google Scholar] [CrossRef] [PubMed]
- Vaz Fragoso, C.A.; Van Ness, P.H.; Araujo, K.L.; Iannone, L.P.; Marottoli, R.A. Sleep disturbances and driving practices of older drivers. J. Am. Geriatr. Soc. 2013, 61, 1730–1737. [Google Scholar] [CrossRef]
- Sagaspe, P.; Taillard, J.; Bayon, V.; Lagarde, E.; Moore, N.; Boussuge, J.; Chaumet, G.; Bioulac, B.; Philip, P. Sleepiness, near-misses and driving accidents among a representative population of French drivers. J. Sleep Res. 2010, 19, 578–584. [Google Scholar] [CrossRef]
- Filtness, A.J.; Reyner, L.A.; Horne, J.A. Driver sleepiness—Comparisons between young and older men during a monotonous afternoon simulated drive. Biol. Psychol. 2012, 89, 580–583. [Google Scholar] [CrossRef]
- Leufkens, T.R.M.; Ramaekers, J.G.; De Weerd, A.W.; Riedel, W.J.; Vermeeren, A. On-the-road driving performance and driving-related skills in older untreated insomnia patients and chronic users of hypnotics. Psychopharmacology 2014, 231, 2851–2865. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Song, W.; Woon, F.L.; Doong, A.; Persad, C.; Tijerina, L.; Pandit, P.; Cline, C.; Giordani, B. Fatigue in Younger and Older Drivers: Effectiveness of an Alertness-Maintaining Task. Hum. Factors 2017, 59, 995–1008. [Google Scholar] [CrossRef] [PubMed]
- Bartolacci, C.; Scarpelli, S.; D’Atri, A.; Gorgoni, M.; Annarumma, L.; Cloos, C.; Giannini, A.M.; De Gennaro, L. The influence of sleep quality, vigilance, and sleepiness on driving-related cognitive abilities: A comparison between young and older adults. Brain Sci. 2020, 10, 327. [Google Scholar] [CrossRef] [PubMed]
- Johns, M.W. A new method for measuring daytime sleepiness: The Epworth sleepiness scale. Sleep 1991, 14, 540–545. [Google Scholar] [CrossRef]
- Dinges, D.F.; Powell, J.W. Microcomputer analyses of performance on a portable, simple visual RT task during sustained operations. Behav. Res. Method Instrum. Comp. 1985, 17, 652–655. [Google Scholar] [CrossRef]
- Akerstedt, T.; Gillberg, M. Subjective and objective sleepiness in the active individual. Int. J. Neurosci. 1990, 52, 29–37. [Google Scholar] [CrossRef]
- O’Hanlon, J.F. Driving performance under the influence of drugs: Rationale for, and application of, a new test. Br. J. Clin. Pharmacol. 1984, 18, 121s–129s. [Google Scholar] [CrossRef] [PubMed]
- Braitman, K.A.; Williams, A.F. Changes in self-regulatory driving among older drivers over time. Traffic Inj. Prev. 2011, 12, 568–575. [Google Scholar] [CrossRef]
- Foley, D.J.; Heimovitz, H.K.; Guralnik, J.M.; Brock, D.B. Driving life expectancy of persons aged 70 years and older in the United States. Am. J. Public Health 2002, 92, 1284–1289. [Google Scholar] [CrossRef]
- Rizzo, M. Impaired driving from medical conditions: A 70-year-old man trying to decide if he should continue driving. JAMA 2011, 305, 1018–1026. [Google Scholar] [CrossRef]
- Garbarino, S.; Lanteri, P.; Durando, P.; Magnavita, N.; Sannita, W.G. Co-morbidity, mortality, quality of life and the healthcare/welfare/social costs of disordered sleep: A rapid review. Int. J. Environ. Res. Public Health 2016, 13, 831. [Google Scholar] [CrossRef]
- Huang, E.S.; Karter, A.J.; Danielson, K.K.; Warton, E.M.; Ahmed, A.T. The association between the number of prescription medications and incident falls in a multi-ethnic population of adult type-2 diabetes patients: The diabetes and aging study. J. Gen. Intern. Med. 2009, 25, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Boyd, C.M.; Darer, J.; Boult, C.; Fried, L.P.; Boult, L.; Wu, A.W. Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases. JAMA 2005, 294, 716–724. [Google Scholar] [CrossRef]
- Qato, D.M.; Alexander, G.C.; Conti, R.M.; Johnson, M.; Schumm, P.; Lindau, S.T. Use of prescription and over-the-counter medications and dietary supplements among older adults in the United States. JAMA 2008, 300, 2867–2878. [Google Scholar] [CrossRef]
- Biss, R.K.; Hasher, L. Happy as a lark: Morning-type younger and older adults are higher in positive affect. Emotion 2012, 12, 437. [Google Scholar] [CrossRef]
- Didikoglu, A.; Maharani, A.; Payton, A.; Pendleton, N.; Canal, M.M. Longitudinal change of sleep timing: Association between chronotype and longevity in older adults. Chronobiol. Int. 2019, 36, 1285–1300. [Google Scholar] [CrossRef]
- Winocur, G.; Hasher, L. Circadian rythms and memory in Aged Humans and Animals. In Neuropsychology of Memory, 3rd ed.; Squire, L.R., Schacter, D.L., Eds.; Guilford Publications: New York, NY, USA, 2003; pp. 273–285. [Google Scholar]
- Winocur, G.; Hasher, L. Age and time-of-day effects on learning and memory in a non-matching-to-sample test. Neurobiol. Aging 2004, 25, 1107–1115. [Google Scholar] [CrossRef] [PubMed]
- Calafat, A.; Adrover-Roig, D.; Blay, N.; Juan, M.; Bellis, M.; Hughes, K.; Mendes, F.; Kokkevi, A. Which young people accept a lift from a drunk or drugged driver? Accid. Anal. Prev. 2009, 41, 703–709. [Google Scholar] [CrossRef] [PubMed]
- Zakletskaia, L.I.; Mundt, M.P.; Balousek, S.L.; Wilson, E.L.; Fleming, M.F. Alcohol-impaired driving behavior and sensation-seeking disposition in a college population receiving routine care at campus health services centers. Accid. Anal. Prev. 2009, 41, 380–386. [Google Scholar] [CrossRef] [PubMed]
- Matousek, M. Alertness pattern in healthy individuals of various ages. Int. J. Psychophysiol. 1992, 13, 263–269. [Google Scholar] [CrossRef]
- Ryan, G.A.; Legge, M.; Rosman, D. Age related in drivers’ crash risk and crash type. Accid. Anal. Prev. 1998, 30, 379–387. [Google Scholar] [CrossRef]
- Gorgoni, M.; D’Atri, A.; Scarpelli, S.; Ferrara, M.; De Gennaro, L. The electroencephalographic features of the sleep onset process and their experimental manipulation with sleep deprivation and transcranial electrical stimulation protocols. Neurosci. Biobehav. Rev. 2020, 114, 25–37. [Google Scholar] [CrossRef] [PubMed]
- Ferrara, M.; De Gennaro, L. Going local: Insights from EEG and stereo-EEG studies of the human sleep-wake cycle. Curr. Top. Med. Chem. 2011, 11, 2423–2437. [Google Scholar] [CrossRef]
- D’Ambrosio, S.; Castelnovo, A.; Guglielmi, O.; Nobili, L.; Sarasso, S.; Garbarino, S. Sleepiness as a local phenomenon. Front. Neurosci. 2019, 13, 1086. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, H.; Hayashi, M.; Hori, T. Topographical characteristics of slow wave activities during the transition from wakefulness to sleep. Clin. Neurophysiol. 2000, 111, 417–427. [Google Scholar] [CrossRef]
- Marzano, C.; Moroni, F.; Gorgoni, M.; Nobili, L.; Ferrara, M.; De Gennaro, L. How we fall asleep: Regional and temporal differences in electroencephalographic synchronization at sleep onset. Sleep Med. 2013, 14, 1112–1122. [Google Scholar] [CrossRef]
- Reyner, L.A.; Horne, J.A. Suppression of sleepiness in drivers: Combination of caffeine with a short nap. Psychophysiology 1997, 34, 721–725. [Google Scholar] [CrossRef] [PubMed]
- Lyznicki, J.M.; Doege, T.C.; Davis, R.M.; Williams, M.A. Sleepiness, driving, and motor vehicle crashes. Council on Scientific Affairs, American Medical Association. JAMA 1998, 279, 1908–1913. [Google Scholar] [CrossRef] [PubMed]
- Hershner, S.D.; Chervin, R.D. Causes and consequences of sleepiness among college students. Nat. Sci. Sleep 2014, 6, 73–84. [Google Scholar] [CrossRef] [PubMed]
- Cellini, N.; Canale, N.; Mioni, G.; Costa, S. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J. Sleep Res. 2020, 29, e13074. [Google Scholar] [CrossRef] [PubMed]
- Franceschini, C.; Musetti, A.; Zenesini, C.; Palagini, L.; Scarpelli, S.; Quattropani, M.C.; Lenzo, V.; Freda, M.F.; Lemmo, D.; Vegni, E.; et al. Poor sleep quality and its consequences on mental health during the COVID-19 lockdown in Italy. Front. Psychol. 2020, 11, 3072. [Google Scholar] [CrossRef] [PubMed]
- Alfonsi, V.; Gorgoni, M.; Scarpelli, S.; Zivi, P.; Sdoia, S.; Mari, E.; Fraschetti, A.; Ferlazzo, F.; Giannini, A.M.; De Gennaro, L. COVID-19 lockdown and poor sleep quality: Not the whole story. J. Sleep Res. 2021, 6, e13368. [Google Scholar] [CrossRef]
- Nguyen-Michel, V.H.; Lévy, P.P.; Pallanca, O.; Kinugawa, K.; Banica-Wolters, R.; Sebban, C.; Mariani, J.; Fournier, E.; Arnulf, I. Underperception of naps in older adults referred for a sleep assessment: An insomnia trait and a cognitive problem? J. Am. Geriatr. Soc. 2015, 63, 2001–2007. [Google Scholar] [CrossRef] [PubMed]
- Onen, F.; Moreau, T.; Gooneratne, N.S.; Petit, C.; Falissard, B.; Onen, S.H. Limits of the Epworth Sleepiness Scale in older adults. Sleep Breath 2013, 17, 343–350. [Google Scholar] [CrossRef] [PubMed]
- Özkan, T.; Lajunen, T. What causes the differences in driving between young men and women? The effects of gender roles and sex on young drivers’ driving behaviour and self-assessment of skills. Transp. Res. Part F Traffic Psychol. Behav. 2006, 9, 269–277. [Google Scholar] [CrossRef]
- Cordellieri, P.; Baralla, F.; Ferlazzo, F.; Sgalla, R.; Piccardi, L.; Giannini, A.M. Gender effects in young road users on road safety attitudes, behaviors and risk perception. Front. Psychol. 2016, 7, 1412. [Google Scholar] [CrossRef]
- Foley, D.J.; Monjan, A.A.; Brown, S.L.; Simonsick, E.M.; Wallace, R.B.; Blazer, D.G. Sleep complaints among elderly persons: An epidemiologic study of three communities. Sleep 1995, 18, 425–432. [Google Scholar] [CrossRef]
- Byles, J.E.; Mishra, G.D.; Harris, M.A.; Nair, K. The problems of sleep for older women: Changes in health outcomes. Age Ageing 2003, 32, 154–163. [Google Scholar] [CrossRef]
- OECD. Elderly Population (Indicator). 2021. Available online: https://www.oecd-ilibrary.org/social-issues-migration-health/elderly-population/indicator/english_8d805ea1-en (accessed on 10 July 2021). [CrossRef]
- Istituto Nazionale di Statistica. Invecchiamento Attivo e Condizione di Vita Degli Anziani in Italia. 2020. Available online: https://www.istat.it/it/files//2020/08/Invecchiamento-attivo-e-condizioni-di-vita-degli-anziani-in-Italia.pdf (accessed on 10 July 2021).
- Tregear, S.J.; Tiller, M. Executive Summary: Diabetes and Commercial Motor Vehicle Driver Safety. Federal Motor Carrier Safety Administration. 8 September 2006. Available online: https://www.fmcsa.dot.gov/sites/fmcsa.dot.gov/files/docs/Final-Diabetes-Executive-Summary-prot.pdf (accessed on 17 August 2021).
- Tregear, S.J.; Tiller, M.; Price, N. Executive Summary: Cardiovascular Disease and Commercial Motor Vehicle Driver Safety. Federal Motor Carrier Safety Administration. 10 April 2007. Available online: https://www.fmcsa.dot.gov/sites/fmcsa.dot.gov/files/docs/Final-Executive-Summary-prot.pdf (accessed on 17 August 2021).
- Tiller, M.; Tregear, S.; Fontanarossa, J.; Price, N. Executive Summary: Seizure Disorders and Commercial Motor Vehicle Driver Safety. Federal Motor Carrier Safety Administration. 30 November 2007. Available online: https://www.fmcsa.dot.gov/sites/fmcsa.dot.gov/files/docs/Final-Seizure-Executive-Summary-prot.pdf (accessed on 17 August 2021).
- Tregear, S.J.; Tiller, M.; Fontanarrosa, J.; Price, N.; Akafomo, C. Executive Summary: Obstructive Sleep Apnea and Commercial Motor Vehicle Driver Safety. Federal Motor Carrier Safety Administration. 12 July 2007. Available online: https://www.fmcsa.dot.gov/sites/fmcsa.dot.gov/files/docs/Sleep-Apnea-Final-Executive-Summary-prot.pdf (accessed on 17 August 2021).
- Reston, J.T.; Tregear, S. Executive Summary: Traumatic Brain Injury and Commercial Motor Vehicle Driver Safety. Federal Motor Carrier Safety Administration. Available online: https://www.fmcsa.dot.gov/sites/fmcsa.dot.gov/files/docs/TraumaticBrainInjury_ExecutiveReport.pdf (accessed on 17 August 2021).
- Volná, J.; Sonka, K. Medical factors of falling asleep behind the wheel. Prague Med. Rep. 2006, 107, 290–296. [Google Scholar]
- Gurubhagavatula, I.; Sullivan, S.; Meoli, A.; Patil, S.; Olson, R.; Berneking, M.; Watson, N.F. Management of obstructive sleep apnea in commercial motor vehicle operators: Recommendations of the AASM sleep and transportation safety awareness task force. J. Clin. Sleep Med. 2017, 13, 745–758. [Google Scholar] [CrossRef]
- Filtness, A.J.; Reyner, L.A.; Horne, J.A. Moderate sleep restriction in treated older male OSA participants: Greater impairment during monotonous driving compared with controls. Sleep Med. 2011, 12, 838–843. [Google Scholar] [CrossRef] [PubMed][Green Version]
- European Union. Commission Directive 2014/85/EU of 1 July 2014, Amending Directive 2006/126/EC of the European Parliament and of the Council on Driving Licences. OJ L 194; European Union: Brussels, Belgium, 2014; pp. 10–13. [Google Scholar]
- McNicholas, W.T. (Ed.) New Standards and Guidelines for Drivers with Obstructive Sleep Apnoea Syndrome: Report of the Obstructive Sleep Apnoea Working Group; European Commission: Brussels, Belgium, 2013. [Google Scholar]
- Peker, Y.; Ozaydin, A.N.; Cetinkaya, R.; Kabadayi, E.; Karakucuk, A.G.; Celik, Y.; McNicholas, W.T. Reliability of the Turkish version of the European Obstructive Sleep Apnea Screening (EUROSAS) questionnaire for drivers. Sleep Breath 2021, 25, 907–913. [Google Scholar] [CrossRef] [PubMed]
- Reifman, J.; Kumar, K.; Khitrov, M.Y.; Liu, J.; Ramakrishnan, S. PC-PVT 2.0: An updated platform for psychomotor vigilance task testing, analysis, prediction, and visualization. J. Neurosci. Methods 2018, 304, 39–45. [Google Scholar] [CrossRef] [PubMed]
| Authors and Date of Publication | Participants | Age | Sleepiness Measures | Driving Measures | Study Design | Main Findings |
|---|---|---|---|---|---|---|
| Campagne et al., 2004 | 46 healthy drivers (all males) | 20–30 years (n = 21) 40–50 years (n = 13) 60–70 years (n = 16) | Objective measures: EEG recording during driving performance | Driving simulator: monotonous and prolonged night-driving situation Two conditions:
| Between-group comparisons (conditions):
| The young group had higher running-off- the road accidents than older adults. The older group had higher speed variability than younger adults. Alpha power and driving errors in lighted condition showed a positive correlation for younger subjects. Theta power and driving errors were positively correlated in older adults. Theta power was correlated also to the speed variability in the older group during a lighted condition. |
| Vaz Fragoso et al., 2008 | 430 drivers without cognitive or vision impairment (365 males) | ≥70 years | Subjective measure: ESS Other sleep measures:ISI SACS | Self-reported driving performance (VAS):
| Cross-sectional/Epidemiological survey (Descriptive analyses only) | Older drivers with insomnia symptoms and daytime drowsiness reported lower levels of self-rated driving abilities, especially regarding nighttime driving. |
| Lowden et al., 2009 | 30 healthy drivers (15 males) | 18–24 years (n = 20) 55–63 years (n = 10) | Subjective measure: KSS every 5-min Objective measure: EEG recording during driving performance; saliva cortisol collected before and after driving | Dynamic Hi-Fi driving simulator 45-min driving in:
| Repeated measures: Condition:
| Subjective sleepiness increased across each drive and was higher among young drivers at night. Relative EEG power increased among older drivers for frequencies of 10–16 Hz. The sigma 1 frequency band (12–14 Hz) increase during the task in older drivers. Salivary cortisol levels after night driving were higher in older drivers than youngers subjects. |
| Sagaspe et al., 2010 | 4774 healthy drivers (45.7% males) | 18–31 years (12.7%) 31–50 years (43.8%) 51–65 years (27.7%) ≥65 years (15.8%) | Subjective measure: ESS Other sleep measures:Self-reported sleep disturbances | Self-reported driving performance:
| Cross-sectional/Epidemiological survey | The best predictors of the near misses were: being male, being young (18-30 years), being sensitive to caffeine, and having at least an episode of sleepiness at wheel in the last year. |
| Vaz Fragoso et al., 2010 | 430 drivers without cognitive or vision impairment (365 men) | ≥70 years | Subjective measure: ESS Other sleep measures:ISI SACS | Self-reported driving performance:
| Longitudinal design | 215 older drivers had at least one adverse driving events. Subjects with adverse driving events showed at the baseline higher ESS scores and higher driving frequency than older adults not experiencing adverse events. |
| Filtness et al., 2012 | 40 healthy drivers (all males) | 20–26 year (n = 20) 52–74 years (n = 20) | Subjective measures: ESS, KSS Objective measure: EEG recording during driving performance | Driving simulator in the early morning Two conditions:
| Between-group comparisons: Younger vs. Older in both conditions:
| After sleep restriction both groups had more driving accidents and increased the number of incidents during the task. After sleep restriction the younger group showed significantly more sleepiness-related incidents during driving simulation. Alpha and theta (4–11 Hz) EEG power was higher in younger drivers than older drivers. KSS scores were positively correlated with EEG measures after sleep restriction in both groups. |
| Vaz Fragoso et al., 2013 | 430 drivers without cognitive or vision impairment (365 males) | ≥70 years | Subjective measure: ESS Other sleep measures:ISI SACS | Self-reported driving performance:
| Longitudinal design | Insomnia, daytime sleepiness, and sleep apnea risk were not longitudinally associated with driving cessation. Insomnia at baseline predicted the reduction of driving mileage. Polypharmacy and age were associated with decreased mileage, while being male predicted increasing in daily driving mileage. |
| Leufkens et al., 2014 | 63 drivers (34 males): 21 insomniac with pharmacological treatment 21 insomniacs without medications 21 good sleepers | 50–75 years | Subjective measure: KSS Behavioral measure: PVT Other sleep measures: preliminary PSG assessment; GSQS | Road tracking performance:
| Between-group comparisons (three groups): Treated insomniacs vs. untreated insomniacs vs. good sleepers | Older good sleepers and older insomniacs did not differ in driving performance and driving-related skills, as well as in PVT performance. Good sleepers showed faster mean reaction times at the PVT in the morning than evening. |
| Song et al., 2017 | 68 healthy drivers (31 males) | 18–30 years (n = 29) 54–88 years (n = 39) | Subjective measures: VAS to indicate tiredness rating | Driving simulator:
| Between-group comparisons: Younger vs. Older | Younger drivers reported higher tiredness than older adults during the 50-min monotonous driving. AMT significantly advantaged the younger group who made more driving errors than older drivers during the first and second monotonous segments. Older adults did not show increased errors with fatigue. AMT did not negatively impact on their driving performance, but they showed increased speed variability when driving with AMT. |
| Bartolacci et al., 2020 | 80 healthy drivers (45 males) | 20–35 years (n= 40) 58–80 years (n = 40) | Subjective measure: ESS, KSS Behavioral measure: PVT Other sleep-related measures: PSQI | Driving-related skills Vienna system traffic:
| Between-group comparisons: Younger vs. Older | Older drivers showed lower sleep efficiency and lower performance in PVT than younger drivers.Self-reported sleepiness was greater in young subjects. Older adults had lower performance in attention and tachistoscopic perception tests. Older adults were more cautious in traffic situations than the younger group. Age was the only best predictors of cognitive driving-related abilities. |
| Authors | EEG Measures | Recordings | Quantitative Analysis |
|---|---|---|---|
| Campagne et al., 2004 | 4 EEG channels: F3-A2, C3-A2, P3-A2, O1-A2 |
| Theta (4–8 Hz) Alpha (8–12 Hz) Beta (12–25 Hz) (alpha + theta)/beta ratio |
| Lowden et al., 2009 | 3 EEG channels: Fz-A1, Cz-A2, Oz-Pz EOG EMG | During driving simulation | Theta (4–8 Hz) Alpha 1 (8–10 Hz) Alpha 2 (10–12 Hz) Sigma 1 (12–14 Hz) Sigma 2 (14–16 Hz) Beta 1 (16–24 Hz) Beta 2 (24–32 Hz) Total power (4–32 Hz) |
| Filtness et al., 2012 | 2 EEG channels: C3-A1, C4-A2 EOG EMG | During driving simulation | Theta (4–7 Hz) Alpha (8–11 Hz) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scarpelli, S.; Alfonsi, V.; Gorgoni, M.; Camaioni, M.; Giannini, A.M.; De Gennaro, L. Age-Related Effect of Sleepiness on Driving Performance: A Systematic-Review. Brain Sci. 2021, 11, 1090. https://doi.org/10.3390/brainsci11081090
Scarpelli S, Alfonsi V, Gorgoni M, Camaioni M, Giannini AM, De Gennaro L. Age-Related Effect of Sleepiness on Driving Performance: A Systematic-Review. Brain Sciences. 2021; 11(8):1090. https://doi.org/10.3390/brainsci11081090
Chicago/Turabian StyleScarpelli, Serena, Valentina Alfonsi, Maurizio Gorgoni, Milena Camaioni, Anna Maria Giannini, and Luigi De Gennaro. 2021. "Age-Related Effect of Sleepiness on Driving Performance: A Systematic-Review" Brain Sciences 11, no. 8: 1090. https://doi.org/10.3390/brainsci11081090
APA StyleScarpelli, S., Alfonsi, V., Gorgoni, M., Camaioni, M., Giannini, A. M., & De Gennaro, L. (2021). Age-Related Effect of Sleepiness on Driving Performance: A Systematic-Review. Brain Sciences, 11(8), 1090. https://doi.org/10.3390/brainsci11081090










