Statins Use in Alzheimer Disease: Bane or Boon from Frantic Search and Narrative Review
Abstract
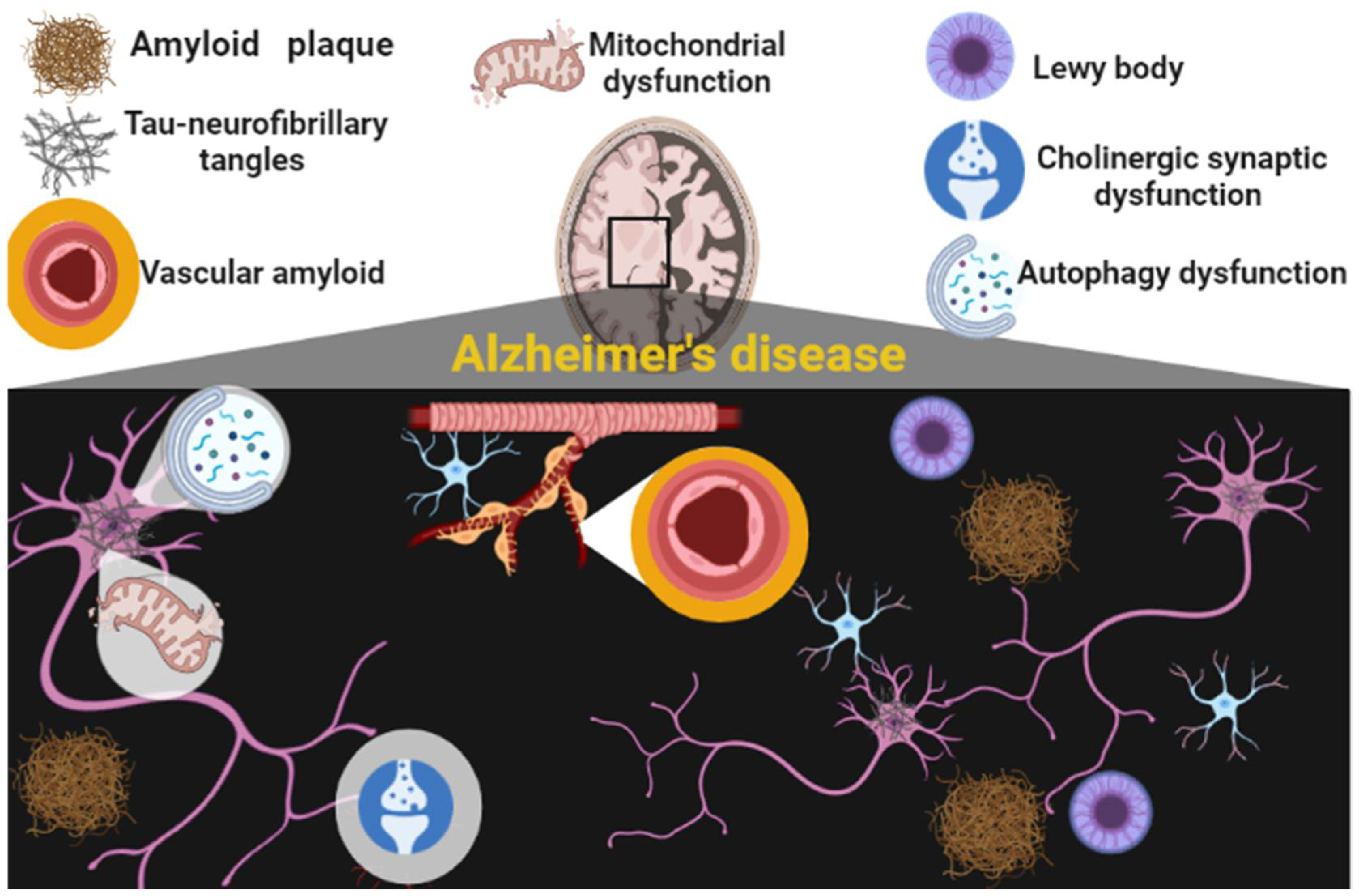
:1. Introduction
Aim of the Study
2. Statins Overview
3. Statins and AD
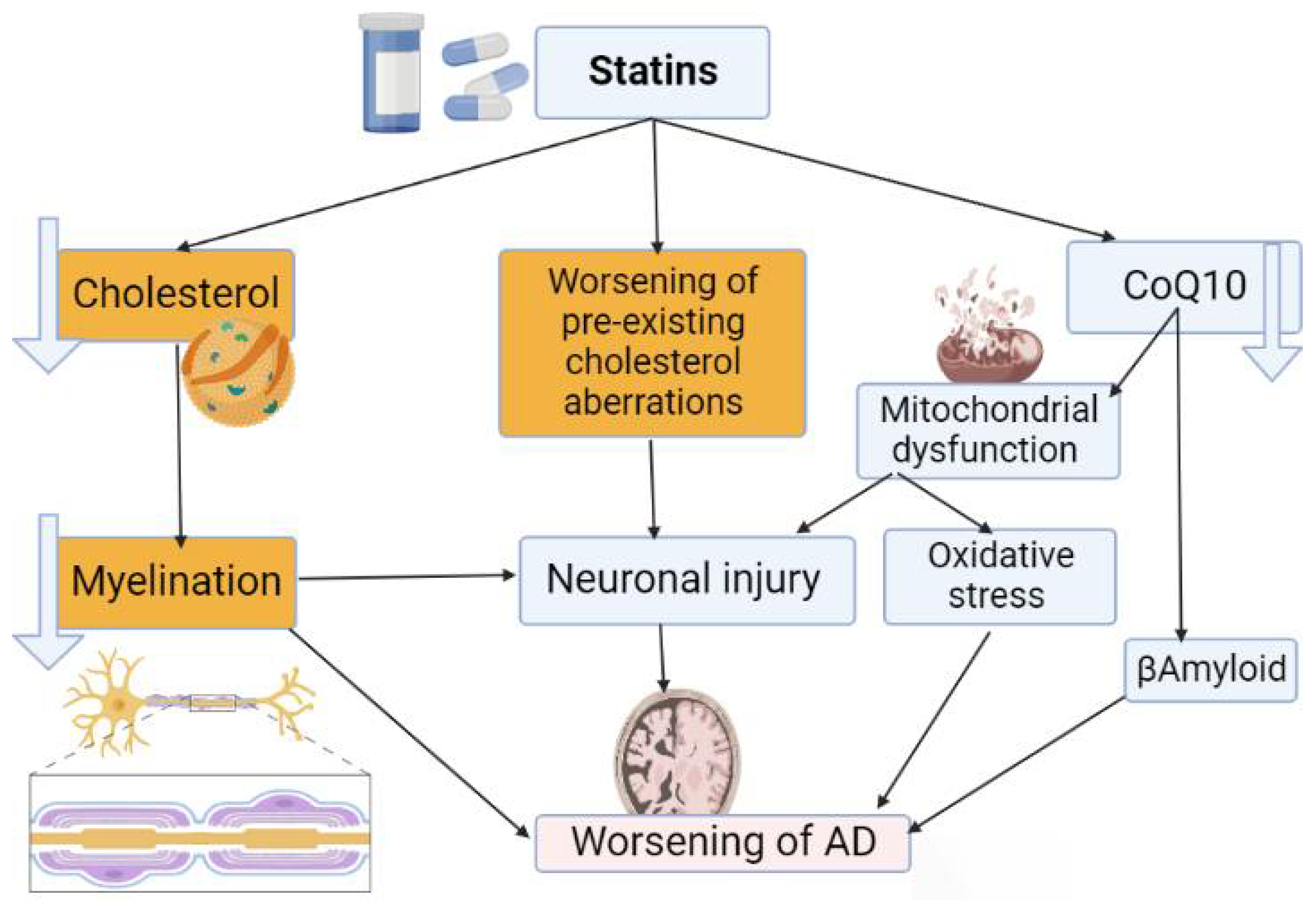
3.1. Detrimental Effects of Statins on AD
3.2. Beneficial Effects of Statins on AD
3.3. Neutral Effects of Statins on AD
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Castellani, R.J.; Rolston, R.K.; Smith, M.A. Alzheimer disease. Dis. Mon. 2010, 56, 484. [Google Scholar] [CrossRef]
- Reitz, C.; Rogaeva, E.; Beecham, G.W. Late-onset vs. nonmendelian early-onset Alzheimer disease: A distinction without a difference? Neurol. Genet. 2020, 6, e512. [Google Scholar] [CrossRef]
- Knopman, D.S.; Petersen, R.C.; Jack, C.R. A brief history of “Alzheimer disease”: Multiple meanings separated by a common name. Neurology 2019, 92, 1053–1059. [Google Scholar] [CrossRef]
- Jack, C.R.; Bennett, D.A.; Blennow, K.; Carrillo, M.C.; Feldman, H.H.; Frisoni, G.B.; Hampel, H.; Jagust, W.J.; Johnson, K.A.; Knopman, D.S. A/T/N: An unbiased descriptive classification scheme for Alzheimer disease biomarkers. Neurology 2016, 87, 539–547. [Google Scholar] [CrossRef]
- Kern, S.; Zetterberg, H.; Kern, J.; Zettergren, A.; Waern, M.; Höglund, K.; Andreasson, U.; Wetterberg, H.; Börjesson-Hanson, A.; Blennow, K. Prevalence of preclinical Alzheimer disease: Comparison of current classification systems. Neurology 2018, 90, e1682–e1691. [Google Scholar] [CrossRef]
- Zhu, C.W.; Sano, M. Economic considerations in the management of Alzheimer’s disease. Clin. Interv. Aging 2006, 1, 143. [Google Scholar] [CrossRef]
- Reitz, C.; Mayeux, R. Alzheimer disease: Epidemiology, diagnostic criteria, risk factors and biomarkers. Biochem. Pharmacol. 2014, 88, 640–651. [Google Scholar] [CrossRef]
- Van der Kant, R.; Goldstein, L.S.; Ossenkoppele, R. Amyloid-β-independent regulators of tau pathology in Alzheimer disease. Nat. Rev. Neurosci. 2020, 21, 21–35. [Google Scholar] [CrossRef]
- Long, J.M.; Holtzman, D.M. Alzheimer disease: An update on pathobiology and treatment strategies. Cell 2019, 179, 312–339. [Google Scholar] [CrossRef]
- Steinman, J.; Sun, H.-S.; Feng, Z.-P. Microvascular alterations in Alzheimer’s disease. Front. Cell. Neurosci. 2021, 14, 618986. [Google Scholar] [CrossRef]
- Wang, M.; Qin, L.; Tang, B. MicroRNAs in Alzheimer’s disease. Front. Genet. 2019, 10, 153. [Google Scholar] [CrossRef]
- Yasmeen, N.; Datta, M.; Kumar, V.; Alshehri, F.S.; Almalki, A.H.; Haque, S. Deciphering the Link Between ERUPR Signaling and MicroRNA in Pathogenesis of Alzheimer’s Disease. Front. Aging Neurosci. 2022, 14, 880167. [Google Scholar] [CrossRef]
- Rajgor, D.; Welle, T.M.; Smith, K.R. The coordination of local translation, membranous organelle trafficking, and synaptic plasticity in neurons. Front. Cell Dev. Biol. 2021, 9, 711446. [Google Scholar] [CrossRef]
- Chen, M.-L.; Hong, C.-G.; Yue, T.; Li, H.-M.; Duan, R.; Hu, W.-B.; Cao, J.; Wang, Z.-X.; Chen, C.-Y.; Hu, X.-K. Inhibition of miR-331-3p and miR-9-5p ameliorates Alzheimer’s disease by enhancing autophagy. Theranostics 2021, 11, 2395. [Google Scholar] [CrossRef]
- Mohajeri, M.; Banach, M.; Atkin, S.L.; Butler, A.E.; Ruscica, M.; Watts, G.F.; Sahebkar, A. MicroRNAs: Novel molecular targets and response modulators of statin therapy. Trends Pharmacol. Sci. 2018, 39, 967–981. [Google Scholar] [CrossRef]
- Petersen, C.; Nolan, A.L.; de Paula França Resende, E.; Miller, Z.; Ehrenberg, A.J.; Gorno-Tempini, M.L.; Rosen, H.J.; Kramer, J.H.; Spina, S.; Rabinovici, G.D. Alzheimer’s disease clinical variants show distinct regional patterns of neurofibrillary tangle accumulation. Acta Neuropathol. 2019, 138, 597–612. [Google Scholar] [CrossRef]
- Mendez, M.F. Early-onset Alzheimer disease and its variants. Continuum (Minneap. Minn.) 2019, 25, 34–51. [Google Scholar] [CrossRef]
- Vijayan, M.; Reddy, P.H. Stroke, vascular dementia, and Alzheimer’s disease: Molecular links. J. Alzheimer’s Dis. 2016, 54, 427–443. [Google Scholar] [CrossRef]
- Wolters, F.J.; Ikram, M.A. Epidemiology of vascular dementia: Nosology in a time of epiomics. Arterioscler. Thromb. Vasc. Biol. 2019, 39, 1542–1549. [Google Scholar] [CrossRef]
- Shabir, O.; Berwick, J.; Francis, S.E. Neurovascular dysfunction in vascular dementia, Alzheimer’s and atherosclerosis. BMC Neurosci. 2018, 19, 1247. [Google Scholar] [CrossRef] [Green Version]
- Sharma, A.; Pachauri, V.; Flora, S. Advances in multi-functional ligands and the need for metal-related pharmacology for the management of Alzheimer disease. Front. Pharmacol. 2018, 9, 1247. [Google Scholar] [CrossRef] [PubMed]
- Yiannopoulou, K.G.; Papageorgiou, S.G. Current and future treatments in Alzheimer disease: An update. J. Cent. Nerv. Syst. Dis. 2020, 12, 1179573520907397. [Google Scholar] [CrossRef] [PubMed]
- Alsehli, A.M.; Olivo, G.; Clemensson, L.E.; Williams, M.J.; Schiöth, H.B. The cognitive effects of statins are modified by age. Sci. Rep. 2020, 10, 6187. [Google Scholar] [CrossRef] [PubMed]
- Bitzur, R. Remembering statins: Do statins have adverse cognitive effects? Diabetes Care 2016, 39, S253–S259. [Google Scholar] [CrossRef]
- Al-Kuraishy, H.M.; Al-Gareeb, A.I.; Hussien, N.R.; Al-Naimi, M.S.; Rasheed, H.A. Statins an oft-prescribed drug is implicated in peripheral neuropathy: The time to know more. JPMA J. Pak. Med. Assoc. 2019, 69, S108–S112. [Google Scholar]
- Available online: https://www.marefa.org/w/index.php?curid=880097 (accessed on 18 August 2022).
- Available online: https://commons.wikimedia.org/w/index.php?curid=1525361 (accessed on 18 August 2022).
- Al-Kuraishy, H.M.; Al-Gareeb, A.I. Acylation-stimulating protein is a surrogate biomarker for acute myocardial infarction: Role of statins. J. Lab. Physicians 2017, 9, 163–169. [Google Scholar] [CrossRef]
- Hussien, N.R.; Al-Niemi, M.S.; Al-Kuraishy, H.M.; Al-Gareeb, A.I. Statins and Covid-19: The neglected front of bidirectional effects. J. Pak. Med. Assoc. 2021, 71, S133–S136. [Google Scholar]
- Al-Kuraishy, H.M.; Hussian, N.R.; Al-Naimi, M.S.; Al-Gareeb, A.I. Statins role in vitiligo: A mini-review. Turk. J. Dermatol. 2020, 14, 1. [Google Scholar] [CrossRef]
- Al-kuraishy, H.M.; Al-Gareeb, A.I.; Al-Maiahy, T.J. Erectile dysfunction and statins: The assorted view of preponderance. Asian Pac. J. Reprod. 2020, 9, 55. [Google Scholar] [CrossRef]
- Al-Kuraishy, H.; Al-Gareeb, A.; Naji, M. Brain natriuretic peptide in patients with acute ischemic stroke: Role of statins. Biomed. Biotechnol. Res. J. 2020, 4, 239–245. [Google Scholar] [CrossRef]
- Kadhim, S.S.; Al-Windy, S.A.; Al-Nami, M.S.; Al Kuraishy, H.M.; Al Gareeb, A.I. Statins improve periodontal disease–induced inflammatory changes and associated lipid peroxidation in patients with dyslipidemia: Two birds by one stone. J. Int. Oral Health 2020, 12, 66. [Google Scholar]
- Al-Kuraishy, H.M.; Hussien, N.R.; Al-Naimi, M.S.; Al-Gareeb, A.I.; Lugnier, C. Statins Therapy Improves Acute Ischemic Stroke in Patients with Cardio-metabolic Disorders Measured by Lipoprotein-Associated Phospholipase A2 (Lp-PLA2): New Focal Point. Neurol. India 2021, 69, 1637. [Google Scholar] [CrossRef] [PubMed]
- Al-Kuraishy, H.M.; Al-Gareeb, A.I.; Al-Buhadily, A.K. Rosuvastatin as forthcoming antibiotic or as adjuvant additive agent: In vitro novel antibacterial study. J. Lab. Physicians 2018, 10, 271–275. [Google Scholar] [CrossRef] [PubMed]
- Naji, M.T.; Al-Kuraishy, H.M.; Al-Gareeb, A.I. Differential effects of statins on matrix metalloproteinase-9 (MMP-9) in patients with acute ischaemic stroke: A potential for salutary. J. Pak. Med. Assoc. 2021, 71, S82–S87. [Google Scholar]
- Al-Rubiay, H.F.; Al-Kuraishy, H.M.; Al-Gareeb, A.I. Intercellular adhesive molecule 1 (ICAM-1) and acute ischaemic stroke: Role of statins. J. Pak. Med. Assoc. 2021, 71, S11–S16. [Google Scholar] [PubMed]
- Al-Kuraishy, H.M.; Al-Gareeb, A.I.; Al-Buhadilly, A.K. Rosuvastatin improves vaspin serum levels in obese patients with acute coronary syndrome. Diseases 2018, 6, 9. [Google Scholar] [CrossRef] [PubMed]
- Al-Kuraishy, H.M.; Al-Gareeb, A.I. Effects of rosuvastatin on metabolic profile: Versatility of dose-dependent effect. J. Adv. Pharm. Technol. Res. 2019, 10, 33. [Google Scholar] [CrossRef]
- Al-Kuraishy, H.M.; Al-Gareeb, A.I.; Samy, O.M. Statin therapy improves serum Annexin A1 levels in patients with acute coronary syndrome: A case-controlled study. Int. J. Crit. Illn. Inj. Sci. 2021, 11, 4. [Google Scholar] [CrossRef]
- Davidson, M.H. Implications of high-dose statin link with incident diabetes. Nat. Rev. Cardiol. 2011, 8, 543–544. [Google Scholar] [CrossRef]
- Goldfine, A.B. Statins: Is it really time to reassess benefits and risks? N. Engl. J. Med. 2012, 366, 1752–1755. [Google Scholar] [CrossRef]
- Seshadri, S.; Rapaka, N.; Prajapati, B.; Mandaliya, D.; Patel, S.; Muggalla, C.S.; Kapadia, B.; Babu, P.P.; Misra, P.; Saxena, U. Statins exacerbate glucose intolerance and hyperglycemia in a high sucrose fed rodent model. Sci. Rep. 2019, 9, 8825. [Google Scholar] [CrossRef] [PubMed]
- Henriksbo, B.D.; Lau, T.C.; Cavallari, J.F.; Denou, E.; Chi, W.; Lally, J.S.; Crane, J.D.; Duggan, B.M.; Foley, K.P.; Fullerton, M.D. Fluvastatin causes NLRP3 inflammasome-mediated adipose insulin resistance. Diabetes 2014, 63, 3742–3747. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Lee, H.; An, J.; Song, Y.; Lee, C.-K.; Kim, K.; Kong, H. Alterations in gut microbiota by statin therapy and possible intermediate effects on hyperglycemia and hyperlipidemia. Front. Microbiol. 2019, 10, 1947. [Google Scholar] [CrossRef] [PubMed]
- Arnold, S.E.; Arvanitakis, Z.; Macauley-Rambach, S.L.; Koenig, A.M.; Wang, H.-Y.; Ahima, R.S.; Craft, S.; Gandy, S.; Buettner, C.; Stoeckel, L.E. Brain insulin resistance in type 2 diabetes and Alzheimer disease: Concepts and conundrums. Nat. Rev. Neurol. 2018, 14, 168–181. [Google Scholar] [CrossRef] [PubMed]
- Batiha, G.E.-S.; Al-kuraishy, H.M.; Al-Maiahy, T.J.; Al-Buhadily, A.K.; Saad, H.M.; Al-Gareeb, A.I.; Simal-Gandara, J. Plasminogen activator inhibitor 1 and gestational diabetes: The causal relationship. Diabetol. Metab. Syndr. 2022, 14, 127. [Google Scholar] [CrossRef]
- Al-Thomali, A.W.; Al-kuraishy, H.M.; Al-Gareeb, A.I.; Al-buhadiliy, A.K.; De Waard, M.; Sabatier, J.-M.; Khan Khalil, A.A.; Saad, H.M.; Batiha, G.E.-S. Role of Neuropilin 1 in COVID-19 Patients with Acute Ischemic Stroke. Biomedicines 2022, 10, 2032. [Google Scholar] [CrossRef]
- Schultz, B.G.; Patten, D.K.; Berlau, D.J. The role of statins in both cognitive impairment and protection against dementia: A tale of two mechanisms. Transl. Neurodegener. 2018, 7, 5. [Google Scholar] [CrossRef]
- Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20 536 high-risk individuals: A randomised placebocontrolled trial. Lancet 2002, 360, 7–22. [Google Scholar] [CrossRef]
- Power, M.C.; Weuve, J.; Sharrett, A.R.; Blacker, D.; Gottesman, R.F. Statins, cognition, and dementia—systematic review and methodological commentary. Nat. Rev. Neurol. 2015, 11, 220–229. [Google Scholar] [CrossRef]
- McGuinness, B.; Craig, D.; Bullock, R.; Passmore, P. Statins for the prevention of dementia. Cochrane Database Syst. Rev. 2009, 2016, CD003160. [Google Scholar]
- El-Saber Batiha, G.; Al-Gareeb, A.I.; Saad, H.M.; Al-Kuraishy, H.M. COVID-19 and corticosteroids: A narrative review. Inflammopharmacology 2022, 30, 1189–1205. [Google Scholar] [CrossRef] [PubMed]
- Scott, H.D.; Laake, K. Statins for the prevention of Alzheimer’s disease and dementia. Cochrane Database Syst. Rev. 2001. [Google Scholar] [CrossRef]
- Kivipelto, M.; Helkala, E.L.; Laakso, M.P.; Hänninen, T.; Hallikainen, M.; Alhainen, K.; Iivonen, S.; Mannermaa, A.; Tuomilehto, J.; Nissinen, A.; et al. Apolipoprotein E epsilon4 allele, elevated midlife total cholesterol level, and high midlife systolic blood pressure are independent risk factors for late-life Alzheimer disease. Ann. Intern. Med. 2002, 137, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Muldoon, M.F.; Barger, S.D.; Ryan, C.M.; Flory, J.D.; Lehoczky, J.P.; Matthews, K.A.; Manuck, S.B. Effects of lovastatin on cognitive function and psychological well-being. Am. J. Med. 2000, 108, 538–546. [Google Scholar] [CrossRef]
- Alkazmi, L.; Al-kuraishy, H.M.; Batiha, G.E.-S.; Mostafa-Hedeab, G.; De Waard, M.; Sabatier, J.-M.; Kabrah, S.M.; Saad, H.M.; Al-Gareeb, A.I.; Simal-Gandara, J. Roxadustat for SARS-CoV-2 Infection: Old Signaling Raised New Hopes. Drugs R D 2022, 22, 183–186. [Google Scholar] [CrossRef]
- Posvar, E.L.; Radulovic, L.L.; Cilla, D.D., Jr.; Whitfield, L.R.; Sedman, A.J. Tolerance and Pharmacokinetics of Single-Dose Atorvastatin, a Potent Inhibitor of HMG-CoA Reductase, in Healthy Subjects. J. Clin. Pharmacol. 1996, 36, 728–731. [Google Scholar] [CrossRef]
- Wagstaff, L.R.; Mitton, M.W.; Arvik, B.M.; Doraiswamy, P.M. Statin-associated memory loss: Analysis of 60 case reports and review of the literature. Pharmacother. J. Hum. Pharmacol. Drug Ther. 2003, 23, 871–880. [Google Scholar] [CrossRef]
- Muldoon, M.F.; Ryan, C.M.; Sereika, S.M.; Flory, J.D.; Manuck, S.B. Randomized trial of the effects of simvastatin on cognitive functioning in hypercholesterolemic adults. Am. J. Med. 2004, 117, 823–829. [Google Scholar] [CrossRef]
- Evans, M.A.; Golomb, B.A. Statin-associated adverse cognitive effects: Survey results from 171 patients. Pharmacother. J. Hum. Pharmacol. Drug Ther. 2009, 29, 800–811. [Google Scholar] [CrossRef]
- Marcum, Z.A.; Vande Griend, J.P.; Linnebur, S.A. FDA drug safety communications: A narrative review and clinical considerations for older adults. Am. J. Geriatr. Pharmacother. 2012, 10, 264–271. [Google Scholar]
- Sahebzamani, F.M.; Munro, C.L.; Marroquin, O.C.; Diamond, D.M.; Keller, E.; Kip, K.E. Examination of the FDA warning for statins and cognitive dysfunction. J. Pharmacovigil. 2014, 2, 4. [Google Scholar] [CrossRef]
- Li, R.; Wang, T.-J.; Lyu, P.-Y.; Liu, Y.; Chen, W.-H.; Fan, M.-Y.; Xu, J. Effects of plasma lipids and statins on cognitive function. Chin. Med. J. 2018, 131, 471–476. [Google Scholar] [CrossRef] [PubMed]
- Suraweera, C.; de Silva, V.; Hanwella, R. Simvastatin-induced cognitive dysfunction: Two case reports. J. Med. Case Rep. 2016, 10, 83. [Google Scholar] [CrossRef] [PubMed]
- Stuart, S.A.; Robertson, J.D.; Marrion, N.V.; Robinson, E.S. Chronic pravastatin but not atorvastatin treatment impairs cognitive function in two rodent models of learning and memory. PLoS ONE 2013, 8, e75467. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Wen, J.; Zhang, Z. Statins use and risk of dementia: A dose-response meta analysis. Medicine 2018, 97, e11304. [Google Scholar] [CrossRef]
- Miron, V.E.; Zehntner, S.P.; Kuhlmann, T.; Ludwin, S.K.; Owens, T.; Kennedy, T.E.; Bedell, B.J.; Antel, J.P. Statin therapy inhibits remyelination in the central nervous system. Am. J. Pathol. 2009, 174, 1880–1890. [Google Scholar] [CrossRef] [Green Version]
- Rojas-Fernandez, C.H.; Cameron, J.-C.F. Is statin-associated cognitive impairment clinically relevant? A narrative review and clinical recommendations. Ann. Pharmacother. 2012, 46, 549–557. [Google Scholar] [CrossRef]
- Dumont, M.; Kipiani, K.; Yu, F.; Wille, E.; Katz, M.; Calingasan, N.Y.; Gouras, G.K.; Lin, M.T.; Beal, M.F. Coenzyme Q10 decreases amyloid pathology and improves behavior in a transgenic mouse model of Alzheimer’s disease. J. Alzheimer’s Dis. 2011, 27, 211–223. [Google Scholar] [CrossRef]
- Beal, M.F. Mitochondrial dysfunction and oxidative damage in Alzheimer’s and Parkinson’s diseases and coenzyme Q10 as a potential treatment. J. Bioenerg. Biomembr. 2004, 36, 381–386. [Google Scholar] [CrossRef]
- Al-kuraishy, H.M.; Batiha, G.E.-S.; Faidah, H.; Al-Gareeb, A.I.; Saad, H.M.; Simal-Gandara, J. Pirfenidone and post-Covid-19 pulmonary fibrosis: Invoked again for realistic goals. Inflammopharmacology 2022. online ahead of print. [Google Scholar] [CrossRef]
- Alomair, B.M.; Al-kuraishy, H.M.; Al-Gareeb, A.I.; Al-Hamash, S.M.; De Waard, M.; Sabatier, J.-M.; Saad, H.M.; El-Saber Batiha, G. Montelukast and Acute Coronary Syndrome: The Endowed Drug. Pharmaceuticals 2022, 15, 1147. [Google Scholar] [CrossRef]
- Algotsson, A.; Winblad, B. Patients with Alzheimer’s disease may be particularly susceptible to adverse effects of statins. Dement. Geriatr. Cogn. Disord. 2004, 17, 109–116. [Google Scholar] [CrossRef] [PubMed]
- Kiener, P.A.; Davis, P.M.; Murray, J.L.; Youssef, S.; Rankin, B.M.; Kowala, M. Stimulation of inflammatory responses in vitro and in vivo by lipophilic HMG-CoA reductase inhibitors. Int. Immunopharmacol. 2001, 1, 105–118. [Google Scholar] [CrossRef]
- Mostafa-Hedeab, G.; Al-Kuraishy, H.M.; Al-Gareeb, A.I.; Jeandet, P.; Saad, H.M.; Batiha, G.E.-S. A raising dawn of pentoxifylline in management of inflammatory disorders in Covid-19. Inflammopharmacology 2022, 30, 799–809. [Google Scholar] [CrossRef] [PubMed]
- Kata, D.; Földesi, I.; Feher, L.; Hackler, L., Jr.; Puskas, L.; Gulya, K. Rosuvastatin enhances anti-inflammatory and inhibits pro-inflammatory functions in cultured microglial cells. Neuroscience 2016, 314, 47–63. [Google Scholar] [CrossRef] [PubMed]
- Strandberg, T.E.; Vanhanen, H.; Tikkanen, M.J. Effect of statins on C-reactive protein in patients with coronary artery disease. Lancet 1999, 353, 118–119. [Google Scholar] [CrossRef]
- Bagheri, H.; Ghasemi, F.; Barreto, G.E.; Sathyapalan, T.; Jamialahmadi, T.; Sahebkar, A. The effects of statins on microglial cells to protect against neurodegenerative disorders: A mechanistic review. Biofactors 2020, 46, 309–325. [Google Scholar] [CrossRef]
- Geifman, N.; Brinton, R.D.; Kennedy, R.E.; Schneider, L.S.; Butte, A.J. Evidence for benefit of statins to modify cognitive decline and risk in Alzheimer’s disease. Alzheimer’s Res. Ther. 2017, 9, 1–10. [Google Scholar] [CrossRef]
- Alorabi, M.; Cavalu, S.; Al-Kuraishy, H.M.; Al-Gareeb, A.I.; Mostafa-Hedeab, G.; Negm, W.A.; Youssef, A.; El-Kadem, A.H.; Saad, H.M.; Batiha, G.E.-S. Pentoxifylline and berberine mitigate diclofenac-induced acute nephrotoxicity in male rats via modulation of inflammation and oxidative stress. Biomed. Pharmacother. 2022, 152, 113225. [Google Scholar] [CrossRef]
- Jick, H.; Zornberg, G.L.; Jick, S.S.; Seshadri, S.; Drachman, D.A. Statins and the risk of dementia. Lancet 2000, 356, 1627–1631. [Google Scholar] [CrossRef]
- Haag, M.D.; Hofman, A.; Koudstaal, P.J.; Stricker, B.H.; Breteler, M.M. Statins are associated with a reduced risk of Alzheimer disease regardless of lipophilicity. The Rotterdam Study. J. Neurol. Neurosurg. Psychiatry 2009, 80, 13–17. [Google Scholar] [CrossRef]
- Jeong, W.; Lee, H.; Cho, S.; Seo, J. ApoE4-induced cholesterol dysregulation and its brain cell type-specific implications in the pathogenesis of Alzheimer’s disease. Mol. Cells 2019, 42, 739. [Google Scholar] [PubMed]
- Prince, M.; Albanese, E.; Guerchet, M.; Prina, M. World Alzheimer Report 2014: Dementia and risk reduction: An analysis of protective and modifiable risk factors; Alzheimer’s Disease International: London, UK, 2014; Available online: http://www.alz.co.uk/research/world-report-2014 (accessed on 20 August 2022).
- Cremonini, A.L.; Caffa, I.; Cea, M.; Nencioni, A.; Odetti, P.; Monacelli, F. Nutrients in the prevention of Alzheimer’s disease. Oxid. Med. Cell. Longev. 2019, 2019, 9874159. [Google Scholar] [CrossRef] [PubMed]
- Sierra, S.; Ramos, M.C.; Molina, P.; Esteo, C.; Vázquez, J.A.; Burgos, J.S. Statins as neuroprotectants: A comparative in vitro study of lipophilicity, blood-brain-barrier penetration, lowering of brain cholesterol, and decrease of neuron cell death. J. Alzheimer’s Dis. 2011, 23, 307–318. [Google Scholar] [CrossRef] [PubMed]
- Eckert, G.; Wood, W.; Müller, W. Statins: Drugs for Alzheimer’s disease? J. Neural Transm. 2005, 112, 1057–1071. [Google Scholar] [CrossRef] [PubMed]
- Eckert, G.P.; Kirsch, C.; Mueller, W.E. Differential effects of lovastatin treatment on brain cholesterol levels in normal and apoE-deficient mice. Neuroreport 2001, 12, 883–887. [Google Scholar] [CrossRef]
- Wood, W.G.; Igbavboa, U.; Muller, W.E.; Eckert, G.P. Statins, Bcl-2, and apoptosis: Cell death or cell protection? Mol. Neurobiol. 2013, 48, 308–314. [Google Scholar] [CrossRef]
- Kirsch, C.; Eckert, G.P.; Mueller, W.E. Statin effects on cholesterol micro-domains in brain plasma membranes. Biochem. Pharmacol. 2003, 65, 843–856. [Google Scholar] [CrossRef]
- Lin, F.-C.; Chuang, Y.-S.; Hsieh, H.-M.; Lee, T.-C.; Chiu, K.-F.; Liu, C.-K.; Wu, M.-T. Early statin use and the progression of Alzheimer disease: A total population-based case-control study. Medicine 2015, 94, e2143. [Google Scholar] [CrossRef]
- Rockwood, K. Epidemiological and clinical trials evidence about a preventive role for statins in Alzheimer’s disease. Acta Neurol. Scand. 2006, 114, 71–77. [Google Scholar] [CrossRef]
- Olmastroni, E.; Molari, G.; De Beni, N.; Colpani, O.; Galimberti, F.; Gazzotti, M.; Zambon, A.; Catapano, A.L.; Casula, M. Statin use and risk of dementia or Alzheimer’s disease: A systematic review and meta-analysis of observational studies. Eur. J. Prev. Cardiol. 2022, 29, 804–814. [Google Scholar] [CrossRef]
- Xuan, K.; Zhao, T.; Qu, G.; Liu, H.; Chen, X.; Sun, Y. The efficacy of statins in the treatment of Alzheimer’s disease: A meta-analysis of randomized controlled trial. Neurol. Sci. 2020, 41, 1391–1404. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Reisman, J.; Morris-Eppolito, B.; Qian, S.X.; Kazis, L.E.; Wolozin, B.; Goldstein, L.E.; Xia, W. Beneficial association of angiotensin-converting enzyme inhibitors and statins on the occurrence of possible Alzheimer’s disease after traumatic brain injury. Alzheimers Res. Ther. 2020, 12, 33. [Google Scholar] [CrossRef] [PubMed]
- Wood, W.G.; Eckert, G.P.; Igbavboa, U.; Müller, W.E. Amyloid beta-protein interactions with membranes and cholesterol: Causes or casualties of Alzheimer’s disease. Biochim. Biophys. Acta (BBA)-Biomembr. 2003, 1610, 281–290. [Google Scholar] [CrossRef]
- Chu, C.-S.; Tseng, P.-T.; Stubbs, B.; Chen, T.-Y.; Tang, C.-H.; Li, D.-J.; Yang, W.-C.; Chen, Y.-W.; Wu, C.-K.; Veronese, N. Use of statins and the risk of dementia and mild cognitive impairment: A systematic review and meta-analysis. Sci. Rep. 2018, 8, 5804. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z.; Wang, H.; Edwards, D.; Ding, C.; Yan, L.; Brayne, C.; Mant, J. Association of blood lipids, atherosclerosis and statin use with dementia and cognitive impairment after stroke: A systematic review and meta-analysis. Ageing Res. Rev. 2020, 57, 100962. [Google Scholar] [CrossRef]
- Kim, S.-W.; Kang, H.-J.; Jhon, M.; Kim, J.-W.; Lee, J.-Y.; Walker, A.J.; Agustini, B.; Kim, J.-M.; Berk, M. Statins and inflammation: New therapeutic opportunities in psychiatry. Front. Psychiatry 2019, 10, 103. [Google Scholar] [CrossRef] [PubMed]
- Leduc, V.; De Beaumont, L.; Théroux, L.; Dea, D.; Aisen, P.; Petersen, R.C.; Dufour, R.; Poirier, J. HMGCR is a genetic modifier for risk, age of onset and MCI conversion to Alzheimer’s disease in a three cohorts study. Mol. Psychiatry 2015, 20, 867–873. [Google Scholar] [CrossRef]
- Petanceska, S.S.; DeRosa, S.; Sharma, A.; Diaz, N.; Duff, K.; Tint, S.G.; Refolo, L.M.; Pappolla, M. Changes in apolipoprotein E expression in response to dietary and pharmacological modulation of cholesterol. J. Mol. Neurosci. 2003, 20, 395–406. [Google Scholar] [CrossRef]
- Reiss, A.B.; Voloshyna, I. Regulation of cerebral cholesterol metabolism in Alzheimer disease. J. Investig. Med. 2012, 60, 576–582. [Google Scholar] [CrossRef]
- Sun, Y.-X.; Crisby, M.; Lindgren, S.; Janciauskiene, S. Pravastatin inhibits pro-inflammatory effects of Alzheimer’s peptide Aβ1–42 in glioma cell culture in vitro. Pharmacol. Res. 2003, 47, 119–126. [Google Scholar] [CrossRef]
- Chen, C.-J.; Ding, D.; Ironside, N.; Buell, T.J.; Elder, L.J.; Warren, A.; Adams, A.P.; Ratcliffe, S.J.; James, R.F.; Naval, N.S. Statins for neuroprotection in spontaneous intracerebral hemorrhage. Neurology 2019, 93, 1056–1066. [Google Scholar] [CrossRef] [PubMed]
- Park, I.-H.; Hwang, E.M.; Hong, H.S.; Boo, J.H.; Oh, S.S.; Lee, J.; Jung, M.W.; Bang, O.Y.; Kim, S.U.; Mook-Jung, I. Lovastatin enhances Aβ production and senile plaque deposition in female Tg2576 mice. Neurobiol. Aging 2003, 24, 637–643. [Google Scholar] [CrossRef]
- Fahrenholz, F. Alpha-secretase as a therapeutic target. Curr. Alzheimer Res. 2007, 4, 412–417. [Google Scholar] [CrossRef] [PubMed]
- Rikitake, Y.; Liao, J.K. Rho GTPases, statins, and nitric oxide. Circ. Res. 2005, 97, 1232–1235. [Google Scholar] [CrossRef]
- Aguilar, B.J.; Zhu, Y.; Lu, Q. Rho GTPases as therapeutic targets in Alzheimer’s disease. Alzheimer’s Res. Ther. 2017, 9, 97. [Google Scholar] [CrossRef] [Green Version]
- Fassbender, K.; Simons, M.; Bergmann, C.; Stroick, M.; Lütjohann, D.; Keller, P.; Runz, H.; Kühl, S.; Bertsch, T.; Von Bergmann, K. Simvastatin strongly reduces levels of Alzheimer’s disease β-amyloid peptides Aβ42 and Aβ40 in vitro and in vivo. Proc. Natl. Acad. Sci. USA 2001, 98, 5856–5861. [Google Scholar] [CrossRef]
- Ostrowski, S.M.; Wilkinson, B.L.; Golde, T.E.; Landreth, G. Statins reduce amyloid-β production through inhibition of protein isoprenylation. J. Biol. Chem. 2007, 282, 26832–26844. [Google Scholar] [CrossRef]
- Cole, S.L.; Grudzien, A.; Manhart, I.O.; Kelly, B.L.; Oakley, H.; Vassar, R. Statins cause intracellular accumulation of amyloid precursor protein, β-secretase-cleaved fragments, and amyloid β-peptide via an isoprenoid-dependent mechanism. J. Biol. Chem. 2005, 280, 18755–18770. [Google Scholar] [CrossRef]
- Kivipelto, M.; Helkala, E.-L.; Laakso, M.P.; Hänninen, T.; Hallikainen, M.; Alhainen, K.; Soininen, H.; Tuomilehto, J.; Nissinen, A. Midlife vascular risk factors and Alzheimer’s disease in later life: Longitudinal, population based study. BMJ 2001, 322, 1447–1451. [Google Scholar] [CrossRef]
- Cramer, C.; Haan, M.; Galea, S.; Langa, K.; Kalbfleisch, J. Use of statins and incidence of dementia and cognitive impairment without dementia in a cohort study. Neurology 2008, 71, 344–350. [Google Scholar] [CrossRef]
- Szwast, S.; Hendrie, H.; Lane, K.; Gao, S.; Taylor, S.; Unverzagt, F.; Murrell, J.; Deeg, M.; Ogunniyi, A.; Farlow, M. Association of statin use with cognitive decline in elderly African Americans. Neurology 2007, 69, 1873–1880. [Google Scholar] [CrossRef]
- Di Scala, C.; Troadec, J.D.; Lelièvre, C.; Garmy, N.; Fantini, J.; Chahinian, H. Mechanism of cholesterol-assisted oligomeric channel formation by a short Alzheimer β-amyloid peptide. J. Neurochem. 2014, 128, 186–195. [Google Scholar] [CrossRef] [PubMed]
- Sambamurti, K.; Greig, N.H.; Lahiri, D.K. Advances in the cellular and molecular biology of the beta-amyloid protein in Alzheimer’s disease. Neuromolecular Med. 2002, 1, 1–31. [Google Scholar] [CrossRef]
- Feldman, H.; Doody, R.; Kivipelto, M.; Sparks, D.; Waters, D.; Jones, R.; Schwam, E.; Schindler, R.; Hey-Hadavi, J.; DeMicco, D. Randomized controlled trial of atorvastatin in mild to moderate Alzheimer disease: LEADe. Neurology 2010, 74, 956–964. [Google Scholar] [CrossRef] [PubMed]
- Sano, M.; Bell, K.; Galasko, D.; Galvin, J.; Thomas, R.; Van Dyck, C.; Aisen, P. A randomized, double-blind, placebo-controlled trial of simvastatin to treat Alzheimer disease. Neurology 2011, 77, 556–563. [Google Scholar] [CrossRef] [Green Version]
- Ott, B.R.; Daiello, L.A.; Dahabreh, I.J.; Springate, B.A.; Bixby, K.; Murali, M.; Trikalinos, T.A. Do statins impair cognition? A systematic review and meta-analysis of randomized controlled trials. J. Gen. Intern. Med. 2015, 30, 348–358. [Google Scholar] [CrossRef]
- Ramanan, V.K.; Przybelski, S.A.; Graff-Radford, J.; Castillo, A.M.; Lowe, V.J.; Mielke, M.M.; Roberts, R.O.; Reid, R.I.; Knopman, D.S.; Jack Jr, C.R. Statins and brain health: Alzheimer’s disease and cerebrovascular disease biomarkers in older adults. J. Alzheimer’s Dis. 2018, 65, 1345–1352. [Google Scholar] [CrossRef]
- Babalghith, A.O.; Al-kuraishy, H.M.; Al-Gareeb, A.I.; De Waard, M.; Sabatier, J.-M.; Saad, H.M.; Batiha, G.E.-S. The Potential Role of Growth Differentiation Factor 15 in COVID-19: A Corollary Subjective Effect or Not? Diagnostics 2022, 12, 2051. [Google Scholar] [CrossRef]
- Mejías-Trueba, M.; Pérez-Moreno, M.A.; Fernández-Arche, M.Á. Systematic review of the efficacy of statins for the treatment of Alzheimer’s disease. Clin. Med. 2018, 18, 54. [Google Scholar] [CrossRef]
- Shepherd, J.; Blauw, G.J.; Murphy, M.B.; Cobbe, S.M.; Bollen, E.L.; Buckley, B.M.; Ford, I.; Jukema, J.W.; Hyland, M.; Gaw, A.; et al. The design of a prospective study of Pravastatin in the Elderly at Risk (PROSPER). PROSPER Study Group. PROspective Study of Pravastatin in the Elderly at Risk. Am. J. Cardiol. 1999, 84, 1192–1197. [Google Scholar] [CrossRef]



| Ref. | Study Type | Findings |
|---|---|---|
| Bitzur [24] | Observational study | Prolonged use of statins may affect the cognitive functions in healthy subjects and dementia patients. |
| Schultz et al. [49] | Narrative review study | Statins induced cognitive impairments in both patients and health providers. |
| Power et al. [51] | Randomized controlled trials and observational studies | Statins use does not support a causal preventative effect on cognitive decline or dementia. |
| McGuinness et al. [52] | Cochrane review | Statins use in late life of individuals at risk of vascular disease has no effect in preventing AD or dementia. |
| Posvar et al. [58] | Clinical trial | Atorvastatin in phase one clinical trial led to reversible cognitive impairment. |
| Muldoon et al. [60] | A randomized, double-blind clinical trial | Lovastatin leads to significant impairment of psychomotor performance and working memory compared to the placebo effect. |
| Evans et al. [61] | Patient survey-based analysis | Discontinuation of statins reverses cognitive impairment. |
| Sahebzamani et al. [63], Li et al. [64] | Observational study and review study | Lipophilic statins are associated with a higher percentage of reversible cognitive dysfunction. |
| Stuart et al. [66] | Experimental study | Hydrophilic pravastatin leads to more cognitive impairment compared to lipophilic atorvastatin in adult rats. |
| Zhang et al. [67] | A population-based, retrospective cohort study | Lipophilic and fungus-derived statins are associated with a higher risk for progression of AD compared to hydrophilic statins. |
| Strandberg et al. [78] | A preclinical study | Use of lovastatin promotes the formation and deposition of Aβ amyloid in female mice. |
| Wagstaff et al. [59] | A case reported study | About 50% of patients on atorvastatin and simvastatin therapy develop cognitive dysfunction within two months. |
| Jick et al. [82] | A case-control study | AD was low in statins-treated patients. |
| Sierra et al. [87], Eckert et al. [88] | A comparative study, a prospective clinical trial | Different studies indicated that statin users had superior cognitive scores compared to the non-users which were more evident with lipophilic statins [87,88]. |
| Lin et al. [92] | A population-based study | Early use statins are associated with a significant reduction in the progression of AD. |
| Haag et al. [83] | A prospective study | Statins have the protective effects of statins against the progression of AD independent of lipophilicity. |
| Rockwood [93] | A cross-sectional study | Statins have protection against the propagation of AD. |
| Olmastroni et al. [94] | A systematic review and meta-analysis | Statins therapy has no harmful effects on the neurocognitive function in AD patients. |
| Xuan et al. [95] | A meta-analysis | Statins therapy has beneficial effects on AD patients. |
| Wood et al. [97] | Observational study and meta-analysis | Statins use is associated with a reduction risk of AD development by about 20% in a dose-dependent manner. |
| Chu et al. [98] | A systematic review and meta-analysis | Statins pharmacotherapy reduces the risk of all types of dementia, mild cognitive dysfunction, and AD, but not vascular dementia. |
| Yang et al. [99] | A meta-analysis and observational study | Statins have the protective effects against the development of post-stroke dementia. |
| Sano et al. [119] | A randomized, double-blind, placebo-controlled trial | Simvastatin in mild–moderate AD patients for an 18-month duration failed to produce any protective effect. |
| Feldman et al., 2010 [118] | A randomized, placebo-controlled clinical trial | Atorvastatin therapy for 72 weeks in mild–moderate AD patients did not positively affect cognitive function. |
| Ott et al., 2015 [120] | A systematic review and meta-analysis | Statins therapy was not associated with cognitive dysfunction. |
| Ramanan et al., 2018 [121] | A population-based study | No significant correlation between long-term statins and tau/amyloid burden. |
| Mejías-Trueba et al., 2018 [123] | A systematic review | Long-term statins do not have any improvement on the cognitive function and did not lead to any significant amelioration in AD patients. |
| Shepherd et al., 1999 [123] | A prospective study | The effect of pravastatin on cognitive function in patients with cardiovascular disorders revealed no significant effect on the cognition compared to placebo. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alsubaie, N.; Al-kuraishy, H.M.; Al-Gareeb, A.I.; Alharbi, B.; De Waard, M.; Sabatier, J.-M.; Saad, H.M.; Batiha, G.E.-S. Statins Use in Alzheimer Disease: Bane or Boon from Frantic Search and Narrative Review. Brain Sci. 2022, 12, 1290. https://doi.org/10.3390/brainsci12101290
Alsubaie N, Al-kuraishy HM, Al-Gareeb AI, Alharbi B, De Waard M, Sabatier J-M, Saad HM, Batiha GE-S. Statins Use in Alzheimer Disease: Bane or Boon from Frantic Search and Narrative Review. Brain Sciences. 2022; 12(10):1290. https://doi.org/10.3390/brainsci12101290
Chicago/Turabian StyleAlsubaie, Nawal, Hayder M. Al-kuraishy, Ali I. Al-Gareeb, Bandar Alharbi, Michel De Waard, Jean-Marc Sabatier, Hebatallah M. Saad, and Gaber El-Saber Batiha. 2022. "Statins Use in Alzheimer Disease: Bane or Boon from Frantic Search and Narrative Review" Brain Sciences 12, no. 10: 1290. https://doi.org/10.3390/brainsci12101290
APA StyleAlsubaie, N., Al-kuraishy, H. M., Al-Gareeb, A. I., Alharbi, B., De Waard, M., Sabatier, J.-M., Saad, H. M., & Batiha, G. E.-S. (2022). Statins Use in Alzheimer Disease: Bane or Boon from Frantic Search and Narrative Review. Brain Sciences, 12(10), 1290. https://doi.org/10.3390/brainsci12101290








