The Incidence, Localization and Clinical Relevance of Arterial Fenestrations and Their Association to Brain Aneurysms: A Case–Control Study Based on the STROBE Guidelines
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Population and Setting
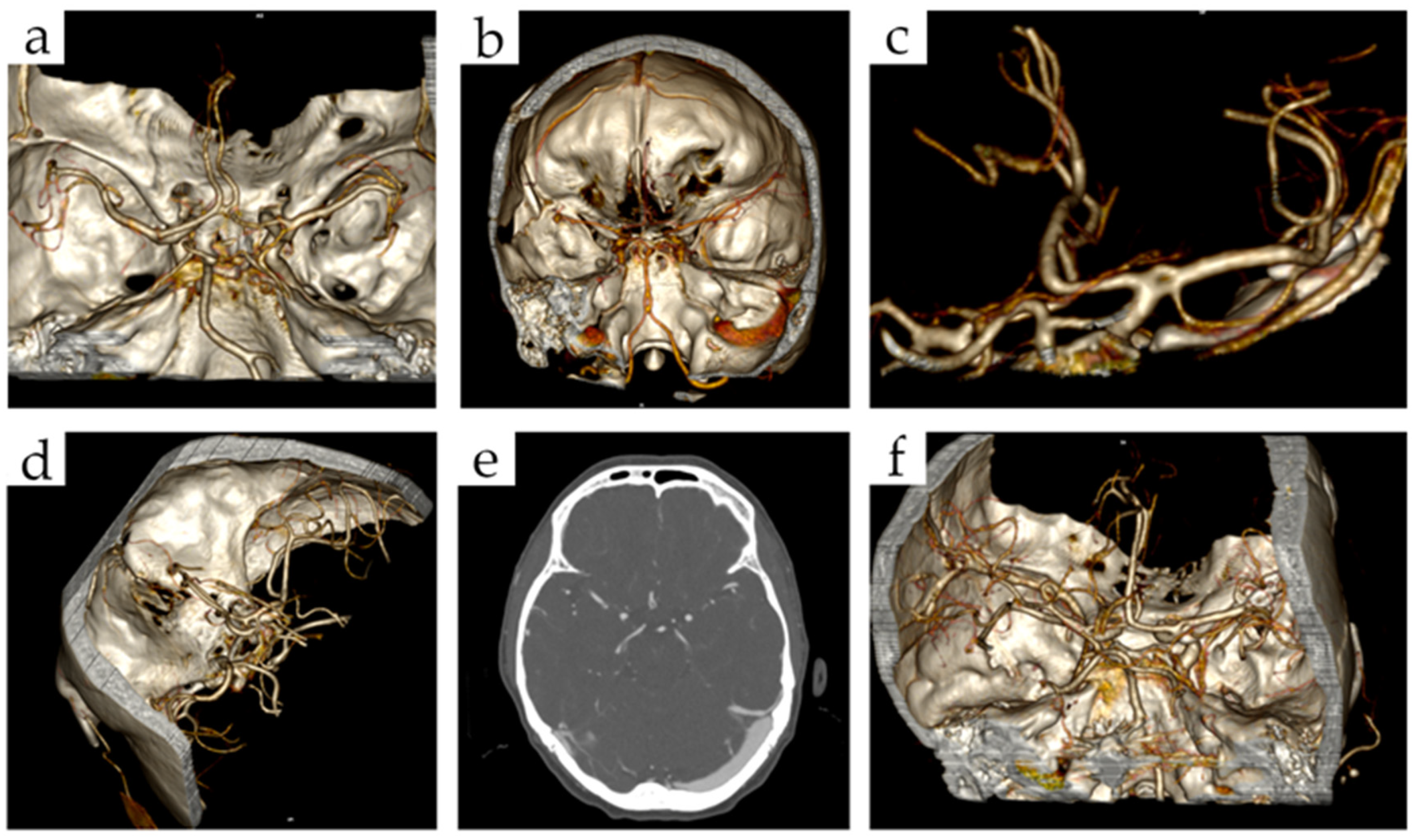
2.3. Imaging Data
2.4. Statistical Analysis
3. Results
3.1. Case Group (1 Tabela)
3.2. Association between Cerebral Arterial Fenestrations and Brain Aneurysms
3.3. Prevalence and Localization of Cerebral Fenestrations
3.4. Age and Gender
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Feindel, W. Willis’s Cerebri Anatome. J. R. Soc. Med. 2017, 96, 368. [Google Scholar] [CrossRef]
- McNabb, J. Thomas Willis: The Faculties and His Two Cognitive Frameworks. Brain Cogn. 2014, 91, 131–137. [Google Scholar] [CrossRef] [PubMed]
- Klimek-Piotrowska, W.; Kopeć, M.; Kochana, M.; Krzyżewski, R.M.; Tomaszewski, K.A.; Brzegowy, P.; Walocha, J. Configurations of the Circle of Willis: A Computed Tomography Angiography Based Study on a Polish Population. Folia Morphol. 2013, 72, 293–299. [Google Scholar] [CrossRef] [PubMed]
- Dimmick, S.J.; Faulder, K.C. Fenestrated Anterior Cerebral Artery with Associated Arterial Anomalies: Case Reports and Literature Review. Interv. Neuroradiol. 2008, 14, 441–445. [Google Scholar] [CrossRef] [PubMed]
- Stojanovic, B.; Vasovic, L.; Trandafilovic, M.; Vlajkovic, S.; Drevensek, M. Anomalías Arteriales y Variaciones Asociadas del Sistema Vertebrobasilar en la Base del Cerebro: Un Caso Raro. Int. J. Morphol. 2022, 40, 750–754. [Google Scholar] [CrossRef]
- Lesley, W.S.; Dalsania, H.J. Double Origin of the Posterior Inferior Cerebellar Artery. Am. J. Neuroradiol. 2004, 25, 425–427. [Google Scholar] [CrossRef]
- Guo, X.; Gao, L.; Shi, Z.; Liu, D.; Wang, Y.; Sun, Z.; Chen, Y.; Chen, W.; Yang, Y. Intracranial Arterial Fenestration and Risk of Aneurysm: A Systematic Review and Meta-Analysis. World Neurosurg. 2018, 115, e592–e598. [Google Scholar] [CrossRef]
- Lesley, W.S. Fenestration of the Posterior Inferior Cerebellar Artery. Cerebellum 2008, 7, 240–241. [Google Scholar] [CrossRef]
- Pleş, H.; Loukas, M.A.R.I.O.S.; Iacob, N.; Andall, N.R.; Miclăuş, G.D.; Tubbs, R.S.; Matusz, P.E.T.R.U. Duplication of the Distal End of the Left Vertebral Artery with Fenestration of the Right Posterior Cerebral Artery. Rom. J. Morphol. Embryol. 2015, 56, 575–577. [Google Scholar]
- Polguj, M.; Podgórski, M.; Hogendorf, P.; Topol, M. Variations of the Hepatobiliary Vasculature Including Coexistence of Accessory Right Hepatic Artery with Unusually Arising Double Cystic Arteries: Case Report and Literature Review. Anat. Sci. Int. 2014, 89, 195–198. [Google Scholar] [CrossRef]
- Polguj, M.; Podgórski, M.; Jędrzejewski, K.; Topol, M.; Majos, A. Fenestration and Duplication of the Vertebral Artery. Clin. Anat. 2013, 26, 933–943. [Google Scholar] [CrossRef] [PubMed]
- Hacein-Bey, L.; Muszynski, C.A.; Varelas, P.N. Saccular Aneurysm Associated with Posterior Cerebral Artery Fenestration Manifesting as a Subarachnoid Hemorrhage in a Child. Am. J. Neuroradiol. 2002, 23, 1291–1294. [Google Scholar] [PubMed]
- Finlay, H.M.; Canham, P.B. The Layered Fabric of Cerebral Artery Fenestrations. Stroke 1994, 25, 1799–1806. [Google Scholar] [CrossRef] [PubMed]
- Sanders, W.P.; Sorek, P.A.; Mehta, B.A. Fenestration of Intracranial Arteries with Special Attention to Associated Aneurysms and Other Anomalies. Am. J. Neuroradiol. 1993, 14, 675–680. [Google Scholar] [PubMed]
- Black, S.P.; Ansbacher, L.E. Saccular Aneurysm Associated with Segmental Duplication of the Basilar Artery. A Morphological Study. J. Neurosurg. 1984, 61, 1005–1008. [Google Scholar] [CrossRef]
- Vandenbroucke, J.P.; Elm, E.V.; Altman, D.G.; Gøtzsche, P.C.; Mulrow, C.D.; Pocock, S.J.; Poole, C.; Schlesselman, J.J.; Egger, M.; Strobe Initiative. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and Elaboration. Int. J. Surg. 2014, 12, 1500–1524. [Google Scholar] [CrossRef]
- Cooke, D.L.; Stout, C.E.; Kim, W.T.; Kansagra, A.P.; Yu, J.P.; Gu, A.; Jewell, N.P.; Hetts, S.W.; Higashida, R.T.; Dowd, C.F.; et al. Cerebral Arterial Fenestrations. Interv. Neuroradiol. 2014, 20, 261. [Google Scholar] [CrossRef]
- Sun, Z.K.; Li, M.; Li, M.H.; Li, Y.D.; Sun, W.P.; Zhu, Y.Q. Fenestrations Accompanied by Intracranial Aneurysms Assessed with Magnetic Resonance Angiography. Neurol. India 2012, 60, 45. [Google Scholar] [CrossRef]
- Arráez-Aybar, L.A.; Villar-Martin, A.; Poyatos-Ruiperez, C.; Rodriguez-Boto, G.; Arrazola-Garcia, J. Prevalence of Fenestrated Basilar Artery with Magnetic Resonance Angiography: A Transversal Study. Surg. Radiol. Anat. 2013, 35, 487–493. [Google Scholar] [CrossRef]
- Bayrak, A.H.; Senturk, S.; Akay, H.O.; Ozmen, C.A.; Bukte, Y.; Nazaroglu, H. The Frequency of Intracranial Arterial Fenestrations: A Study with 64-Detector CT-Angiography. Eur. J. Radiol. 2011, 77, 392–396. [Google Scholar] [CrossRef]
- Uchino, A.; Saito, N.; Okada, Y.; Kozawa, E.; Nishi, N.; Mizukoshi, W.; Inoue, K.; Nakajima, R.; Takahashi, M. Fenestrations of the Intracranial Vertebrobasilar System Diagnosed by MR Angiography. Neuroradiology 2012, 54, 445–450. [Google Scholar] [CrossRef] [PubMed]
- Van Rooij, S.B.T.; Van Rooij, W.J.; Sluzewski, M.; Sprengers, M.E.S. Fenestrations of Intracranial Arteries Detected with 3D Rotational Angiography. AJNR Am. J. Neuroradiol. 2009, 30, 1347–1350. [Google Scholar] [CrossRef] [PubMed]
- Bożek, P.; Pilch-Kowalczyk, J.; Kluczewska, E.; Zymon-Zagórska, A. Detection of Cerebral Artery Fenestrations by Computed Tomography Angiography. Neurol. Neurochir. Pol. 2012, 46, 239–244. [Google Scholar] [CrossRef]
- Van Rooij SB, T.; Bechan, R.S.; Peluso, J.P.; Sluzewski, M.; Van Rooij, W.J. Fenestrations of Intracranial Arteries. Am. J. Neuroradiol. 2015, 36, 1167–1170. [Google Scholar] [CrossRef] [PubMed]
- Texakalidis, P.; Sweid, A.; Mouchtouris, N.; Peterson, E.C.; Sioka, C.; Rangel-Castilla, L.; Reavey-Cantwell, J.; Jabbour, P. Aneurysm Formation, Growth, and Rupture: The Biology and Physics of Cerebral Aneurysms. World Neurosurg. 2019, 130, 277–284. [Google Scholar] [CrossRef] [PubMed]
- Krex, D.; Schackert, H.K.; Schackert, G. Genesis of Cerebral Aneurysms—An Update. Acta Neurochir. 2001, 143, 429–448. [Google Scholar] [CrossRef]
- Rinkel, G.J.; Djibuti, M.; Algra, A.; Van Gijn, J. Prevalence and Risk of Rupture of Intracranial Aneurysms: A Systematic Review. Stroke 1998, 29, 251–256. [Google Scholar] [CrossRef]
- Gao, L.Y.; Guo, X.; Zhou, J.J.; Zhang, Q.; Fu, J.; Chen, W.J.; Yang, Y.J. Basilar Artery Fenestration Detected with CT Angiography. Eur. Radiol. 2013, 23, 2861–2867. [Google Scholar] [CrossRef]
- Krystkiewicz, K.; Ciszek, B.; Szylberg, Ł.; Tosik, M.; Harat, M. Morphological Analysis of Cerebral Artery Fenestrations and Their Correlation with Intracranial Aneurysms. World Neurosurg. 2021, 156, e85–e92. [Google Scholar] [CrossRef]
- Okudera, H.; Koike, J.; Toba, Y.; Kuroyanagi, T.; Kyoshima, K.; Kobayashi, S. Fenestration of the Middle Cerebral Artery Associated with Cerebral Infarction Report of Two Cases. Neurol. Med.-Chir. 1987, 27, 559–563. [Google Scholar] [CrossRef][Green Version]
- Christian, N.; Angelina, P.; Cornelia, B.; Ewald, M. Transitory Ischemic Attack Associated with a Rare Fenestration of the Cervical Segment of the Internal Carotid Artery: A Case Report. J. Med. Case Rep. 2022, 16, 13. [Google Scholar] [CrossRef]
- Gold, J.J.; Crawford, J.R. An Unusual Cause of Pediatric Stroke Secondary to Congenital Basilar Artery Fenestration. Case Rep. Crit. Care 2013, 2013, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Kloska, S.P.; Schlegel, P.M.; Sträter, R.; Niederstadt, T.U. Causality Pediatric Brainstem Infarction and Basilar Artery Fenestration? Pediatric Neurol. 2006, 35, 436–438. [Google Scholar] [CrossRef]
- Meinel, T.R.; Pult, F.; Gralla, J.; Arnold, M.; Bassetti, C.; Jung, S. Successful Endovascular Recanalization of a Partially Occluded Basilar Artery Fenestration. Interv. Neuroradiol. 2019, 25, 44–46. [Google Scholar] [CrossRef] [PubMed]
- Palazzo, P.; Ruff, M.; Lyerly, M.J.; Alexandrov, A.V. Alexandrov. Basilar Artery Thrombus vs. Fenestration: A Differential Diagnostic Challenge in Acute Ischemic Stroke. J. Neuroimaging 2014, 24, 607–609. [Google Scholar] [CrossRef]
- El Otmani, H.; Fotso, V.; El Moutawakil, B.; Rafai, M.A. Basilar Artery Fenestration and Ischemic Stroke: An Unclear Causal Relationship. J. Med. Vasc. 2020, 45, 62–66. [Google Scholar] [CrossRef]
- Wu, X.; Lin, A.; Zhu, J.; Cai, B. Basilar Artery Fenestration: An Unusual Possible Cause of Ischaemic Stroke? Case Rep. 2018, 2018, bcr2017222910. [Google Scholar] [CrossRef]
- Ye, D.; Huang, J.; Wang, S.; Sheng, S.; Liu, M. Cerebral Arterial Fenestration Associated with Stroke and Other Cerebrovascular Diseases. Neuroreport 2021, 32, 1279–1286. [Google Scholar] [CrossRef] [PubMed]
- Mei, Y.; Guan, D.; Tong, X.; Liu, Q.; Hu, M.; Chen, G.; Li, C. Association of Cerebral Infarction with Vertebral Arterial Fenestration Using Non-Newtonian Hemodynamic Evaluation. Math. Biosci. Eng. 2022, 19, 7076–7090. [Google Scholar] [CrossRef]
- Miyamoto, N.; Ueno, Y.; Hira, K.; Kijima, C.; Nakajima, S.; Yamashiro, K.; Hattori, N. Characteristics of Clinical Symptoms, Cerebral Images and Stroke Etiology in Vertebro-Basilar Artery Fenestration-Related Infarction. Brain Sci. 2020, 10, 243. [Google Scholar] [CrossRef]

| Male | Female | Total Cases/Aneurysms | |
|---|---|---|---|
| Mean age | 56.32 ± 14.34 | 57.48 ± 13.71 | N/A |
| Number of cases | 388 | 778 | 1166 |
| Single aneurysms | 293 | 547 | 840 |
| Multiple aneurysms | 95 | 231 | 326 |
| Two aneurysms | 75 | 151 | 226 |
| Three aneurysms | 12 | 58 | 70 |
| Four aneurysms | 7 | 14 | 21 |
| Five aneurysms | 1 | 7 | 8 |
| Six aneurysms | 0 | 1 | 1 |
| Localization of aneurysms | |||
| MCA | 170 | 424 | 594 |
| ICA | 110 | 318 | 428 |
| AComA | 83 | 103 | 186 |
| BA | 43 | 71 | 114 |
| ACA | 42 | 60 | 102 |
| VA | 5 | 28 | 33 |
| Pericallosal | 12 | 17 | 29 |
| PCA | 14 | 12 | 26 |
| PComA | 3 | 9 | 12 |
| PICA | 2 | 1 | 3 |
| Ophthalmic | 0 | 2 | 2 |
| Meningeal | 0 | 1 | 1 |
| Frontobasal | 0 | 1 | 1 |
| Anterior Choroidal | 0 | 1 | 1 |
| Callosomarginal | 1 | 0 | 1 |
| Total aneurysms | 485 | 1048 | 1533 |
| Cases | Controls | Total | |
|---|---|---|---|
| Fenestration | 11 (0.94%) | 38 (0.71%) | 49 |
| No fenestration | 1155 (99.06%) | 5341 (99.29%) | 6496 |
| Total | 1166 | 5379 | 6545 |
| Statistical analysis: OR: 1.157; 95%CI: 0.826–1.621; p = 0.39 | |||
| Aneurysm, n (%) | Fenestration, n (%) | Total | ||||
|---|---|---|---|---|---|---|
| Right ACA | Right VA | BA | Right MCA | AComA | ||
| Right ICA | 0 (0.00) | 1 (9.09) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 1 (9.09) |
| Right MCA | 2 (18.18) | 0 (0.00) | 0 (0.00) | 1 (9.09) | 1 (9.09) | 4 (35.36) |
| AComA | 1 (9.09) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 1 (9.09) |
| Left ICA | 1 (9.09) | 0 (0.00) | 1 (9.09) | 0 (0.00) | 0 (0.00) | 2 (18.18) |
| BA | 0 (0.00) | 0 (0.00) | 1 (9.09) | 0 (0.00) | 0 (0.00) | 1 (9.09) |
| Right PICA | 1 (9.09) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 1 (9.09) |
| Right PComA | 1 (9.09) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 1 (9.09) |
| Total | 6 (54.55) | 1(9.09) | 2 (18.18) | 1 (9.09) | 1 (9.09) | 11 (100.00) |
| Statistical analysis: Chi-square = 17.390; p = 0.832 | ||||||
| Artery | Number of Fenestrations | Mean Age | Median Age |
|---|---|---|---|
| ACA | 15 | 54.6 ± 16.37 | 60 |
| BA | 15 | 47.73 ± 19.48 | 46 |
| AComA | 11 | 56.64 ± 22.21 | 63 |
| VA | 4 | 41.5 ± 16.54 | 45 |
| PCA | 2 | 46 ± 2.83 | 46 |
| MCA | 1 | 70 | 70 |
| ICA | 1 | 17 | 17 |
| Statistical analysis: H = 7.552; p = 0.273 | |||
| Artery | Females | Males | p Value | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| ACA | 12 | 32.43 | 3 | 25 | 0.626 |
| BA | 12 | 32.43 | 3 | 25 | 0.628 |
| AComA | 8 | 21.62 | 3 | 25 | 0.807 |
| VA | 2 | 5.41 | 2 | 16.67 | 0.216 |
| PCA | 1 | 2.7 | 1 | 8.33 | 0.392 |
| MCA | 1 | 2.7 | 0 | 0 | N/A |
| ICA | 1 | 2.7 | 0 | 0 | N/A |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Czyżewski, W.; Hoffman, Z.; Szymoniuk, M.; Korulczyk, P.; Torres, K.; Staśkiewicz, G. The Incidence, Localization and Clinical Relevance of Arterial Fenestrations and Their Association to Brain Aneurysms: A Case–Control Study Based on the STROBE Guidelines. Brain Sci. 2022, 12, 1310. https://doi.org/10.3390/brainsci12101310
Czyżewski W, Hoffman Z, Szymoniuk M, Korulczyk P, Torres K, Staśkiewicz G. The Incidence, Localization and Clinical Relevance of Arterial Fenestrations and Their Association to Brain Aneurysms: A Case–Control Study Based on the STROBE Guidelines. Brain Sciences. 2022; 12(10):1310. https://doi.org/10.3390/brainsci12101310
Chicago/Turabian StyleCzyżewski, Wojciech, Zofia Hoffman, Michał Szymoniuk, Patrycja Korulczyk, Kamil Torres, and Grzegorz Staśkiewicz. 2022. "The Incidence, Localization and Clinical Relevance of Arterial Fenestrations and Their Association to Brain Aneurysms: A Case–Control Study Based on the STROBE Guidelines" Brain Sciences 12, no. 10: 1310. https://doi.org/10.3390/brainsci12101310
APA StyleCzyżewski, W., Hoffman, Z., Szymoniuk, M., Korulczyk, P., Torres, K., & Staśkiewicz, G. (2022). The Incidence, Localization and Clinical Relevance of Arterial Fenestrations and Their Association to Brain Aneurysms: A Case–Control Study Based on the STROBE Guidelines. Brain Sciences, 12(10), 1310. https://doi.org/10.3390/brainsci12101310







