Maintaining the Quality of Mechanical Thrombectomy after Acute Ischemic Stroke in COVID(-)19 Patients
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Population
2.2. Acute Ischemic Stroke Registry
2.3. Statistical Analysis
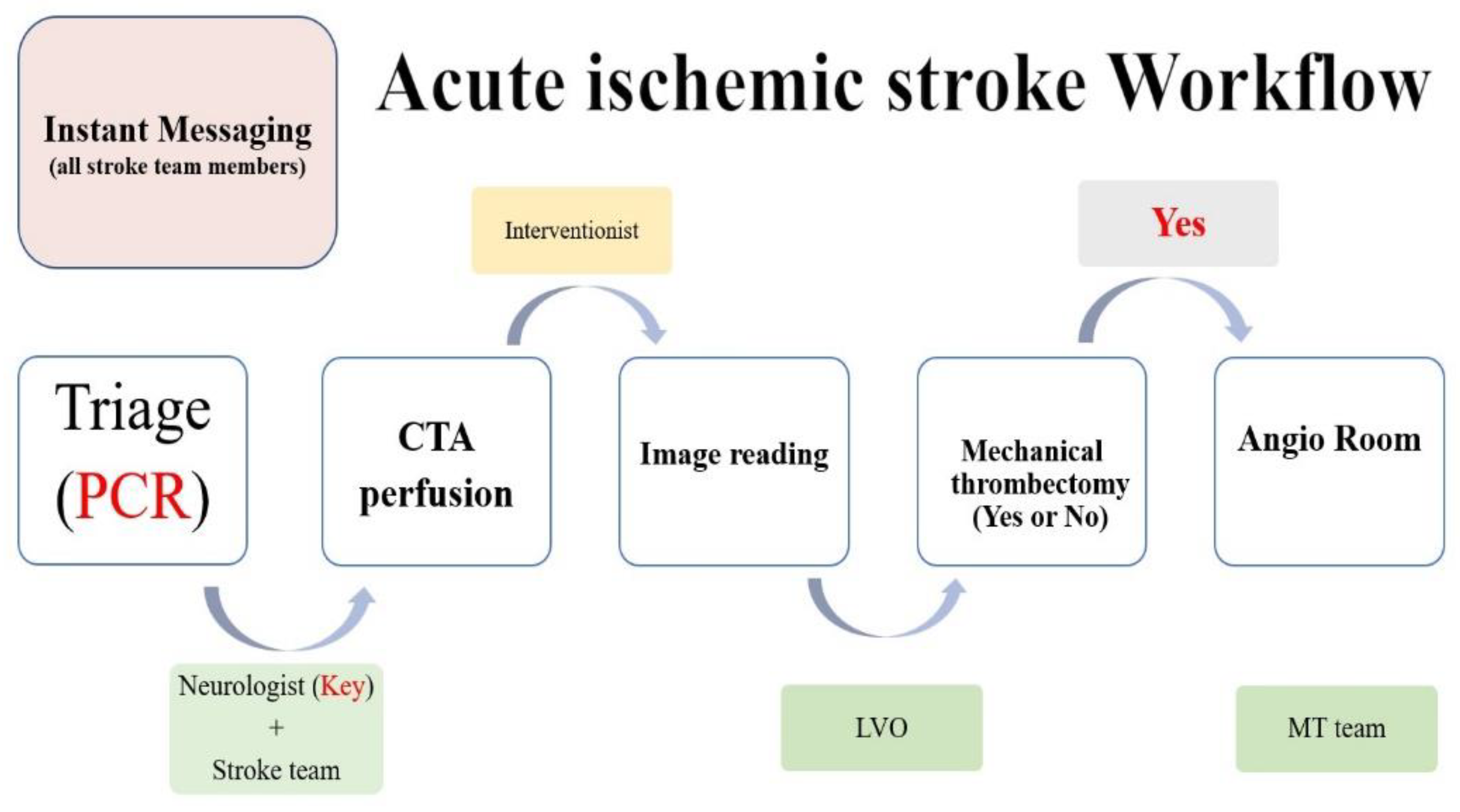
2.4. Acute Ischemic Stroke Workflow
2.5. Mechanical Thrombectomy
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cucinotta, D.; Vanelli, M. WHO Declares COVID-19 a Pandemic. Acta Biomed. 2020, 91, 157–160. [Google Scholar]
- Mahase, E. COVID-19: WHO declares pandemic because of “alarming levels” of spread, severity, and inaction. BMJ 2020, 368, m1036. [Google Scholar] [CrossRef] [Green Version]
- Wu, F.; Zhao, S.; Yu, B.; Chen, Y.M.; Wang, W.; Song, Z.G.; Hu, Y.; Tao, Z.W.; Tian, J.H.; Pei, Y.Y.; et al. A new coronavirus associated with human respiratory disease in China. Nature 2020, 579, 265–269. [Google Scholar] [CrossRef] [Green Version]
- Zhou, P.; Yang, X.L.; Wang, X.G.; Hu, B.; Zhang, L.; Zhang, W.; Si, H.R.; Zhu, Y.; Li, B.; Huang, C.L.; et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 2020, 579, 270–273. [Google Scholar] [CrossRef] [Green Version]
- Wu, Y.C.; Chen, C.S.; Chan, Y.J. The outbreak of COVID-19: An overview. J. Chin. Med. Assoc. 2020, 83, 217–220. [Google Scholar] [CrossRef]
- Velavan, T.P.; Meyer, C.G. The COVID-19 epidemic. Trop. Med. Int. Health 2020, 25, 278–280. [Google Scholar] [CrossRef] [Green Version]
- CECC Raises Epidemic Alert Level for Taipei City and New Taipei City to Level 3 and Strengthens National Restrictions and Measures, Effective from May 15 to May 28, in Response to Increasing Level of Community Transmission. Available online: https://www.cdc.gov.tw/Bulletin/Detail/abDtRS-xzztQeAchjX9fqw?typeid=9 (accessed on 15 May 2021).
- Steinbrook, R. Lessons From the Success of COVID-19 Control in Taiwan. JAMA Intern. Med. 2021, 181, 922. [Google Scholar] [CrossRef]
- Turc, G.; Bhogal, P.; Fischer, U.; Khatri, P.; Lobotesis, K.; Mazighi, M.; Schellinger, P.D.; Toni, D.; Vries, J.D.; White, P.; et al. European Stroke Organisation (ESO)—European Society for Minimally Invasive Neurological Therapy (ESMINT) Guidelines on Mechanical Thrombectomy in Acute Ischaemic StrokeEndorsed by Stroke Alliance for Europe (SAFE). Eur. Stroke J. 2019, 4, 6–12. [Google Scholar] [CrossRef] [Green Version]
- Berkhemer, O.A.; Fransen, P.S.; Beumer, D.; van den Berg, L.A.; Lingsma, H.F.; Yoo, A.J.; Schonewille, W.J.; Vos, J.A.; Nederkoorn, P.J.; Wermer, M.J.; et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N. Engl. J. Med. 2015, 372, 11–20. [Google Scholar] [CrossRef] [Green Version]
- Smith, W.S.; Sung, G.; Saver, J.; Budzik, R.; Duckwiler, G.; Liebeskind, D.S.; Lutsep, H.L.; Rymer, M.M.; Higashida, R.T.; Starkman, S.; et al. Mechanical thrombectomy for acute ischemic stroke: Final results of the Multi MERCI trial. Stroke 2008, 39, 1205–1212. [Google Scholar] [CrossRef] [Green Version]
- Fransen, P.S.; Berkhemer, O.A.; Lingsma, H.F.; Beumer, D.; van den Berg, L.A.; Yoo, A.J.; Schonewille, W.J.; Vos, J.A.; Nederkoorn, P.J.; Wermer, M.J.; et al. Time to Reperfusion and Treatment Effect for Acute Ischemic Stroke: A Randomized Clinical Trial. JAMA Neurol. 2016, 73, 190–196. [Google Scholar] [CrossRef] [Green Version]
- Kurnianto, A.; Tugasworo, D.; Andhitara, Y.; Retnaningsih; Ardhini, R.; Budiman, J. Mechanical thrombectomy (MT) for acute ischemic stroke (AIS) in COVID-19 pandemic: A systematic review. Egypt. J. Neurol. Psychiatry Neurosurg. 2021, 57, 67. [Google Scholar] [CrossRef]
- Hung, J.J.; Wang, F.D.; Ma, H.; Tsou, M.Y.; Dai, H.D.; Lin, Y.H.; Chen, W.M.; Liu, C.S. The precaution strategy toward the COVID-19 pandemic in the operating room of a tertiary hospital in Taiwan. J. Chin. Med. Assoc. 2021, 84, 171–176. [Google Scholar] [CrossRef]
- Davey, S.L.; Lee, B.J.; Robbins, T.; Randeva, H.; Thake, C.D. Heat stress and PPE during COVID-19: Impact on healthcare workers’ performance, safety and well-being in NHS settings. J. Hosp. Infect. 2021, 108, 185–188. [Google Scholar] [CrossRef]
- Ciotti, M.; Ciccozzi, M.; Terrinoni, A.; Jiang, W.C.; Wang, C.B.; Bernardini, S. The COVID-19 pandemic. Crit. Rev. Clin. Lab. Sci. 2020, 57, 365–388. [Google Scholar] [CrossRef]
- Tsai, S.C.; Lu, C.C.; Bau, D.T.; Chiu, Y.J.; Yen, Y.T.; Hsu, Y.M.; Fu, C.W.; Kuo, S.C.; Lo, Y.S.; Chiu, H.Y.; et al. Approaches towards fighting the COVID-19 pandemic (Review). Int. J. Mol. Med. 2021, 47, 3–22. [Google Scholar] [CrossRef]
- Pujadas, E.; Ibeh, N.; Hernandez, M.M.; Waluszko, A.; Sidorenko, T.; Flores, V.; Shiffrin, B.; Chiu, N.; Young-Francois, A.; Nowak, M.D.; et al. Comparison of SARS-CoV-2 detection from nasopharyngeal swab samples by the Roche cobas 6800 SARS-CoV-2 test and a laboratory-developed real-time RT-PCR test. J. Med. Virol. 2020, 92, 1695–1698. [Google Scholar] [CrossRef]
- Yan, C.; Cui, J.; Huang, L.; Du, B.; Chen, L.; Xue, G.; Li, S.; Zhang, W.; Zhao, L.; Sun, Y.; et al. Rapid and visual detection of 2019 novel coronavirus (SARS-CoV-2) by a reverse transcription loop-mediated isothermal amplification assay. Clin. Microbiol. Infect. 2020, 26, 773–779. [Google Scholar] [CrossRef]
- Lee, W.-C. Taiwan’s experience in pandemic control: Drawing the right lessons from SARS outbreak. J. Chin. Med. Assoc. 2020, 83, 622–623. [Google Scholar] [CrossRef]
- Chen, S.-C. Taiwan’s experience in fighting COVID-19. Nat. Immunol. 2021, 22, 393–394. [Google Scholar] [CrossRef]
- Houghton, C.; Meskell, P.; Delaney, H.; Smalle, M.; Glenton, C.; Booth, A.; Chan, X.H.S.; Devane, D.; Biesty, L.M. Barriers and facilitators to healthcare workers’ adherence with infection prevention and control (IPC) guidelines for respiratory infectious diseases: A rapid qualitative evidence synthesis. Cochrane Database Syst. Rev. 2020, 4, CD013582. [Google Scholar]
- Mahmood, S.U.; Crimbly, F.; Khan, S.; Choudry, E.; Mehwish, S. Strategies for Rational Use of Personal Protective Equipment (PPE) Among Healthcare Providers During the COVID-19 Crisis. Cureus 2020, 12, e8248. [Google Scholar] [CrossRef]
- Pandey, A.S.; Daou, B.J.; Tsai, J.P.; Zaidi, S.F.; Salahuddin, H.; Gemmete, J.J.; Oliver, M.J.; Singer, J.; Elder, T.A.; Mbabuike, N.; et al. Letter: COVID-19 Pandemic-The Bystander Effect on Stroke Care in Michigan. Neurosurgery 2020, 87, E397–E399. [Google Scholar] [CrossRef]
- Rudilosso, S.; Laredo, C.; Vera, V.; Vargas, M.; Renú, A.; Llull, L.; Obach, V.; Amaro, S.; Urra, X.; Torres, F.; et al. Acute Stroke Care Is at Risk in the Era of COVID-19: Experience at a Comprehensive Stroke Center in Barcelona. Stroke 2020, 51, 1991–1995. [Google Scholar] [CrossRef]
- Siegler, J.E.; Heslin, M.E.; Thau, L.; Smith, A.; Jovin, T.G. Falling stroke rates during COVID-19 pandemic at a comprehensive stroke center. J. Stroke Cerebrovasc. Dis. 2020, 29, 104953. [Google Scholar] [CrossRef]
- Pop, R.; Quenardelle, V.; Hasiu, A.; Mihoc, D.; Sellal, F.; Dugay, M.H.; Lebedinsky, P.A.; Schluck, E.; LA Porta, A.; Courtois, S.; et al. Impact of the COVID-19 outbreak on acute stroke pathways—Insights from the Alsace region in France. Eur. J. Neurol. 2020, 27, 1783–1787. [Google Scholar] [CrossRef]
- Naccarato, M.; Scali, I.; Olivo, S.; Ajčević, M.; Buoite Stella, A.; Furlanis, G.; Lugnan, C.; Caruso, P.; Peratoner, A.; Cominotto, F.; et al. Has COVID-19 played an unexpected “stroke” on the chain of survival? J. Neurol. Sci. 2020, 414, 116889. [Google Scholar] [CrossRef]
- Hoyer, C.; Ebert, A.; Huttner, H.B.; Puetz, V.; Kallmünzer, B.; Barlinn, K.; Haverkamp, C.; Harloff, A.; Brich, J.; Platten, M.; et al. Acute Stroke in Times of the COVID-19 Pandemic: A Multicenter Study. Stroke 2020, 51, 2224–2227. [Google Scholar] [CrossRef]
- Yoshimoto, T.; Shiozawa, M.; Koge, J.; Inoue, M.; Koga, M.; Ihara, M.; Toyoda, K. Evaluation of Workflow Delays in Stroke Reperfusion Therapy: A Comparison between the Year-Long Pre-COVID-19 Period and the with-COVID-19 Period. J. Atheroscler. Thromb. 2021, 29, 1095–1107. [Google Scholar] [CrossRef]
- Kansagra, A.P.; Wallace, A.N.; Curfman, D.R.; McEachern, J.D.; Moran, C.J.; Cross, D.T., 3rd; Lee, J.M.; Ford, A.L.; Manu, S.G.; Panagos, P.D.; et al. Streamlined triage and transfer protocols improve door-to-puncture time for endovascular thrombectomy in acute ischemic stroke. Clin. Neurol. Neurosurg. 2018, 166, 71–75. [Google Scholar] [CrossRef]
- Jahan, R.; Saver, J.L.; Schwamm, L.H.; Fonarow, G.C.; Liang, L.; Matsouaka, R.A.; Xian, Y.; Holmes, D.N.; Peterson, E.D.; Yavagal, D.; et al. Association Between Time to Treatment With Endovascular Reperfusion Therapy and Outcomes in Patients With Acute Ischemic Stroke Treated in Clinical Practice. JAMA 2019, 322, 252–263. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McTaggart, R.A.; Yaghi, S.; Cutting, S.M.; Hemendinger, M.; Baird, G.L.; Haas, R.A.; Furie, K.L.; Jayaraman, M.V. Association of a Primary Stroke Center Protocol for Suspected Stroke by Large-Vessel Occlusion With Efficiency of Care and Patient Outcomes. JAMA Neurol. 2017, 74, 793–800. [Google Scholar] [CrossRef] [PubMed]
- Powers, W.J.; Rabinstein, A.A.; Ackerson, T.; Adeoye, O.M.; Bambakidis, N.C.; Becker, K.; Biller, J.; Brown, M.; Demaerschalk, B.M.; Hoh, B.; et al. Guidelines for the Early Management of Patients With Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 2019, 50, e344–e418. [Google Scholar]
- Saver, J.L. Time is brain--quantified. Stroke 2006, 37, 263–266. [Google Scholar] [CrossRef] [Green Version]
- Hacke, W.; Kaste, M.; Bluhmki, E.; Brozman, M.; Dávalos, A.; Guidetti, D.; Larrue, V.; Lees, K.R.; Medeghri, Z.; Machnig, T.; et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N. Engl. J. Med. 2008, 359, 1317–1329. [Google Scholar] [CrossRef] [Green Version]
- Toni, D.; Mangiafico, S.; Agostoni, E.; Bergui, M.; Cerrato, P.; Ciccone, A.; Vallone, S.; Zini, A.; Inzitari, D. Intravenous thrombolysis and intra-arterial interventions in acute ischemic stroke: Italian Stroke Organisation (ISO)-SPREAD guidelines. Int. J. Stroke 2015, 10, 1119–1129. [Google Scholar] [CrossRef] [Green Version]
- Kim, S.H.; Nam, T.M.; Jang, J.H.; Kim, Y.Z.; Kim, K.H.; Kim, D.H.; Lee, H.; Jin, S.C.; Lee, C.H. Improving Door-To-Puncture Time in Mechanical Thrombectomy with Direct Care from a Neurointerventionalist in the Emergency Department. World Neurosurg. 2021, 152, e455–e461. [Google Scholar] [CrossRef]
- Chen, C.H.; Hsieh, H.C.; Sung, S.F.; Hsieh, C.Y.; Chen, P.L.; Tsai, L.K.; Huang, H.U.; Jeng, J.S.; Taiwan Stroke Society Guideline Consensus Group. Taiwan Stroke Society Guideline for intravenous thrombolysis in acute ischemic stroke patients. Formos J. Stroke 2019, 1, 1–22. [Google Scholar]




| All (n = 62) | Before COVID (n = 34) | During COVID (n = 28) | p Value | ||||
|---|---|---|---|---|---|---|---|
| Age | 71.5 | (64.75, 80.25) | 70.5 | (63.8, 79.3) | 71.5 | (67.0, 82.0) | 0.276 |
| Female | 33 | (53.2%) | 15 | (44.1%) | 18 | (64.3%) | 0.184 |
| Location | 0.494 | ||||||
| anterior circulation | 53 | (85.5%) | 28 | (82.4%) | 25 | (89.3%) | |
| posterior circulation | 9 | (14.5%) | 6 | (17.6%) | 3 | (10.7%) | |
| Medical history | |||||||
| hypertension | 47 | (75.8%) | 27 | (79.4%) | 20 | (71.4%) | 0.665 |
| hyperlipidemia | 19 | (30.6%) | 13 | (38.2%) | 6 | (21.4%) | 0.249 |
| diabetes mellitus | 22 | (35.5%) | 16 | (47.1%) | 6 | (21.4%) | 0.067 |
| atrial fibrillation | 32 | (51.6%) | 18 | (52.9%) | 14 | (50.0%) | 1.000 |
| ischemia heart disease | 19 | (30.6%) | 11 | (32.4%) | 8 | (28.6%) | 0.964 |
| NIHSS at ER | 18.0 | (12.0, 24.0) | 17.0 | (11.5, 22.0) | 18.0 | (15.3, 27.8) | 0.143 |
| Door to CT, minutes | 20.0 | (15.0, 29.0) | 19.0 | (11.5, 28.7) | 20.0 | (16.0, 31.0) | 0.398 |
| Door to punture, minutes | 114.0 | (97.0, 134.0) | 118.0 | (99.0, 136.0) | 109.0 | (94.8, 131.8) | 0.281 |
| TICI Score | 0.654 | ||||||
| 0 | 2 | (3.3%) | 1 | (2.9%) | 1 | (3.7%) | |
| 1 | 3 | (4.9%) | 1 | (2.9%) | 2 | (7.4%) | |
| 2a | 5 | (8.2%) | 2 | (5.9%) | 3 | (11.1%) | |
| 2b | 13 | (21.3%) | 9 | (26.5%) | 4 | (14.8%) | |
| 2c | 10 | (16.4%) | 7 | (20.6%) | 3 | (11.1%) | |
| 3 | 28 | (45.9%) | 14 | (41.2%) | 14 | (51.9%) | |
| 2b\2c\3 | 51 | (83.6%) | 30 | (88.2%) | 21 | (77.8%) | |
| Symptomatic Hemorrhage in 36HR | 7 | (13.0%) | 3 | (10.7%) | 4 | (15.4%) | 0.699 |
| mRS 3 m 0–2 | 13 | (23.2%) | 7 | (20.6%) | 6 | (27.30%) | 0.799 |
| mRS 3 m 6 | 8 | (14.3%) | 5 | (14.7%) | 3 | (13.6%) | 1.000 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, Y.-H.; Liao, N.-C.; Tsuei, Y.-S.; Chen, W.-H.; Shen, C.-C.; Yang, Y.-C.; Lee, C.-H. Maintaining the Quality of Mechanical Thrombectomy after Acute Ischemic Stroke in COVID(-)19 Patients. Brain Sci. 2022, 12, 1431. https://doi.org/10.3390/brainsci12111431
Chang Y-H, Liao N-C, Tsuei Y-S, Chen W-H, Shen C-C, Yang Y-C, Lee C-H. Maintaining the Quality of Mechanical Thrombectomy after Acute Ischemic Stroke in COVID(-)19 Patients. Brain Sciences. 2022; 12(11):1431. https://doi.org/10.3390/brainsci12111431
Chicago/Turabian StyleChang, Yu-Hao, Nien-Chen Liao, Yuang-Seng Tsuei, Wen-Hsieh Chen, Chiung-Chyi Shen, Yi-Chin Yang, and Chung-Hsin Lee. 2022. "Maintaining the Quality of Mechanical Thrombectomy after Acute Ischemic Stroke in COVID(-)19 Patients" Brain Sciences 12, no. 11: 1431. https://doi.org/10.3390/brainsci12111431





