The Elephant in the Room: A Cross-Sectional Study on the Stressful Psychological Effects of the COVID-19 Pandemic in Mental Healthcare Workers
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Assessment
- -
- Life Events Checklist for DSM-5 (LEC-5) [22] is a 17-item self-report questionnaire to assess exposure to traumatic events. Respondents are asked to indicate whether they have experienced, witnessed, or learned about 17 traumatic events. As the LEC-5 collects information about potentially traumatic experiences a person has experienced, there is no total or composite score for this scale.
- -
- Impact of Event Scale—Revised (IES-R) [23] is a 22-item questionnaire to evaluate subjective distress caused by traumatic events. The instrument comprises three subscales assessing intrusion (8 items), avoidance (8 items), and hyperarousal (6 items) symptoms. For this study, participants were asked to refer to the COVID-19 emergency when answering the questionnaire. IES-R items are rated on a 5-point scale ranging from 0 (“not at all”) to 4 (“extremely”), with a total score ranging from 0 to 88. In line with previous research, a score of ≥33 likely indicates the presence of PTSD [24].
- -
- Depression Anxiety Stress Scales 21 (DASS-21) [25] is a 21-item self-report questionnaire designed to measure states of depression, anxiety, and stress, with 7 items for each subscale. Participants are asked to score each item on a scale from 0 (“did not apply to me at all”) to 3 (“applied to me very much”). Sum scores are computed by adding up the scores on the items per (sub)scale and multiplying them by a factor of 2. Sum scores for each subscale may range between 0 and 42, with higher scores indicating higher depression/anxiety/stress levels.
2.3. Outcomes
2.4. Statistical Analysis
3. Results
3.1. Demographic, Professional, and Stressful Life Event Characteristics
3.2. Scores of Measurements and Associated Factors
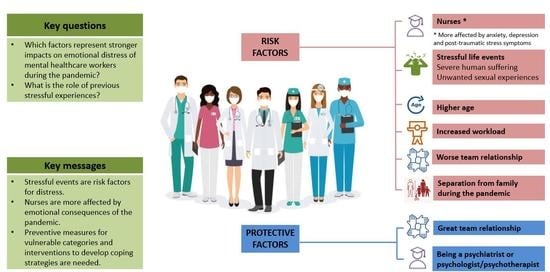
3.3. Risk Factors of Measured Outcomes
4. Discussion
5. Conclusions and Perspectives
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Disclosure Statement
Acknowledgments
Conflicts of Interest
References
- Fish, J.N.; Mittal, M. Mental Health Providers During COVID-19: Essential to the US Public Health Workforce and in Need of Support. Public Health Rep. 2021, 136, 14–17. [Google Scholar] [CrossRef] [PubMed]
- d’Ettorre, G.; Ceccarelli, G.; Santinelli, L.; Vassalini, P.; Innocenti, G.P.; Alessandri, F.; Koukopoulos, A.E.; Russo, A.; D’Ettorre, G.; Tarsitani, L. Post-Traumatic Stress Symptoms in Healthcare Workers Dealing with the COVID-19 Pandemic: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 601. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Scherer, N.; Felix, L.; Kuper, H. Prevalence of depression, anxiety and post-traumatic stress disorder in health care workers during the COVID-19 pandemic: A systematic review and meta-analysis. PLoS ONE 2021, 16, e0246454. [Google Scholar] [CrossRef] [PubMed]
- Pappa, S.; Ntella, V.; Giannakas, T.; Giannakoulis, V.G.; Papoutsi, E.; Katsaounou, P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain. Behav. Immun. 2020, 88, 901–907. [Google Scholar] [CrossRef] [PubMed]
- Marvaldi, M.; Mallet, J.; Dubertret, C.; Moro, M.R.; Guessoum, S.B. Anxiety, depression, trauma-related, and sleep disorders among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Neurosci. Biobehav. Rev. 2021, 126, 252–264. [Google Scholar] [CrossRef] [PubMed]
- Cénat, J.M.; Blais-Rochette, C.; Kokou-Kpolou, C.K.; Noorishad, P.-G.; Mukunzi, J.N.; McIntee, S.-E.; Dalexis, R.D.; Goulet, M.-A.; Labelle, P.R. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Res. 2021, 295, 113599. [Google Scholar] [CrossRef] [PubMed]
- Morgantini, L.A.; Naha, U.; Wang, H.; Francavilla, S.; Acar, Ö.; Flores, J.M.; Crivellaro, S.; Moreira, D.; Abern, M.; Eklund, M.; et al. Factors Contributing to Healthcare Professional Burnout During the COVID-19 Pandemic: A Rapid Turnaround Global Survey. medRxiv Prepr. Serv. Health Sci. 2020, 15, 9. [Google Scholar] [CrossRef]
- Kang, L.; Ma, S.; Chen, M.; Yang, J.; Wang, Y.; Li, R.; Yao, L.; Bai, H.; Cai, Z.; Xiang Yang, B.; et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: A cross-sectional study. Brain. Behav. Immun. 2020, 87, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Feng, J.; Xu, J.; Xu, S.; Cao, H.; Zheng, C.; Sharma, L.; Dela Cruz, C.S.; Zhang, J.; Chu, D.; Yu, L.; et al. Psychological Impact During the First Outbreak of COVID-19 on Frontline Health Care Workers in Shanghai. Front. Public Health 2021, 9, 646780. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.-Y.; Yang, Y.-Z.; Zhang, X.-M.; Xu, X.; Dou, Q.-L.; Zhang, W.-W.; Cheng, A.S.K. The prevalence and influencing factors in anxiety in medical workers fighting COVID-19 in China: A cross-sectional survey. Epidemiol. Infect. 2020, 148, e98. [Google Scholar] [CrossRef] [PubMed]
- De Sire, A.; Marotta, N.; Raimo, S.; Lippi, L.; Inzitari, M.T.; Tasselli, A.; Gimigliano, A.; Palermo, L.; Invernizzi, M.; Ammendolia, A. Psychological Distress and Work Environment Perception by Physical Therapists from Southern Italy during COVID-19 Pandemic: The C.A.L.A.B.R.I.A Study. Int. J. Environ. Res. Public Health 2021, 18, 9676. [Google Scholar] [CrossRef]
- Kar, S.K.; Singh, A. Mental health of mental health professionals during COVID-19 pandemic: Who cares for it? Asian J. Psychiatr. 2020, 53, 102385. [Google Scholar] [CrossRef] [PubMed]
- Carpiniello, B.; Tusconi, M.; di Sciascio, G.; Zanalda, E.; di Giannantonio, M.; Executive Committee of the Italian Society of Psychiatry. Mental health services in Italy during the COVID-19 pandemic. Psychiatry Clin. Neurosci. 2020, 74, 442–443. [Google Scholar] [CrossRef]
- D’Agostino, A.; Demartini, B.; Cavallotti, S.; Gambini, O. Mental health services in Italy during the COVID-19 outbreak. Lancet Psychiatry 2020, 7, 385–387. [Google Scholar] [CrossRef]
- Percudani, M.; Corradin, M.; Moreno, M.; Indelicato, A.; Vita, A. Mental Health Services in Lombardy during COVID-19 outbreak. Psychiatry Res. 2020, 288, 112980. [Google Scholar] [CrossRef]
- Uphoff, E.P.; Lombardo, C.; Johnston, G.; Weeks, L.; Rodgers, M.; Dawson, S.; Seymour, C.; Kousoulis, A.A.; Churchill, R. Mental health among healthcare workers and other vulnerable groups during the COVID-19 pandemic and other coronavirus outbreaks: A rapid systematic review. PLoS ONE 2021, 16, e0254821. [Google Scholar] [CrossRef] [PubMed]
- de Girolamo, G.; Cerveri, G.; Clerici, M.; Monzani, E.; Spinogatti, F.; Starace, F.; Tura, G.; Vita, A. Mental Health in the Coronavirus Disease 2019 Emergency-The Italian Response. JAMA Psychiatry 2020, 77, 974–976. [Google Scholar] [CrossRef]
- Rapisarda, F.; Vallarino, M.; Cavallini, E.; Barbato, A.; Brousseau-Paradis, C.; de Benedictis, L.; Lesage, A. The Early Impact of the Covid-19 Emergency on Mental Health Workers: A Survey in Lombardy, Italy. Int. J. Environ. Res. Public Health 2020, 17, 8615. [Google Scholar] [CrossRef]
- Sun, Y.; Song, H.; Liu, H.; Mao, F.; Sun, X.; Cao, F. Occupational stress, mental health, and self-efficacy among community mental health workers: A cross-sectional study during COVID-19 pandemic. Int. J. Soc. Psychiatry 2021, 67, 737–746. [Google Scholar] [CrossRef]
- Sareen, J. Posttraumatic stress disorder in adults: Impact, comorbidity, risk factors, and treatment. Can. J. Psychiatry 2014, 59, 460–467. [Google Scholar] [CrossRef] [Green Version]
- Kessler, R.C.; Aguilar-Gaxiola, S.; Alonso, J.; Bromet, E.J.; Gureje, O.; Karam, E.G.; Koenen, K.C.; Lee, S.; Liu, H.; Pennell, B.-E.; et al. The associations of earlier trauma exposures and history of mental disorders with PTSD after subsequent traumas. Mol. Psychiatry 2018, 23, 1892–1899. [Google Scholar] [CrossRef] [Green Version]
- Weathers, F.W.; Blake, D.D.; Schnurr, P.P.; Kaloupek, D.G.; Marx, B.P.; Keane, T.M. The Life Events Checklist for DSM-5 (LEC-5). National Center for PTSD. 2013. Available online: www.ptsd.va.gov (accessed on 16 March 2022).
- Weiss, D.S.; Marmar, C.R. The Impact of Event Scale—Revised. In Assessing Psychological Trauma and PTSD; Wilson, J., Keane, T.M., Eds.; Springer: Boston, MA, USA, 1996; pp. 399–411. [Google Scholar]
- Creamer, M.; Bell, R.; Failla, S. Psychometric properties of the Impact of Event Scale—Revised. Behav. Res. Ther. 2003, 41, 1489–1496. [Google Scholar] [CrossRef]
- Lovibond, P.F.; Lovibond, S.H. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995, 33, 335–343. [Google Scholar] [CrossRef]
- Breiman, L. Random forests. Mach. Learn. 2001, 45, 5–32. [Google Scholar] [CrossRef] [Green Version]
- Carpita, M.; Vezzoli, M. Statistical evidence of the subjective work quality: The fairness drivers of the job satisfaction. Electron. J. Appl. Stat. Anal. 2012, 5, 89–107. [Google Scholar] [CrossRef]
- Vezzoli, M. Exploring the facets of overall job satisfaction through a novel ensemble learning. Electron. J. Appl. Stat. Anal. 2011, 4, 23–38. [Google Scholar] [CrossRef]
- Krishnamoorthy, Y.; Nagarajan, R.; Saya, G.K.; Menon, V. Prevalence of psychological morbidities among general population, healthcare workers and COVID-19 patients amidst the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Res. 2020, 293, 113382. [Google Scholar] [CrossRef]
- Ji, D.; Ji, Y.-J.; Duan, X.-Z.; Li, W.-G.; Sun, Z.-Q.; Song, X.-A.; Meng, Y.-H.; Tang, H.-M.; Chu, F.; Niu, X.-X.; et al. Prevalence of psychological symptoms among Ebola survivors and healthcare workers during the 2014-2015 Ebola outbreak in Sierra Leone: A cross-sectional study. Oncotarget 2017, 8, 12784–12791. [Google Scholar] [CrossRef] [Green Version]
- Lee, S.M.; Kang, W.S.; Cho, A.-R.; Kim, T.; Park, J.K. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr. Psychiatry 2018, 87, 123–127. [Google Scholar] [CrossRef]
- Serrano-Ripoll, M.J.; Meneses-Echavez, J.F.; Ricci-Cabello, I.; Fraile-Navarro, D.; Fiol-deRoque, M.A.; Pastor-Moreno, G.; Castro, A.; Ruiz-Pérez, I.; Zamanillo Campos, R.; Gonçalves-Bradley, D.C. Impact of viral epidemic outbreaks on mental health of healthcare workers: A rapid systematic review and meta-analysis. J. Affect. Disord. 2020, 277, 347–357. [Google Scholar] [CrossRef]
- García-Iglesias, J.J.; Gómez-Salgado, J.; Martín-Pereira, J.; Fagundo-Rivera, J.; Ayuso-Murillo, D.; Martínez-Riera, J.R.; Ruiz-Frutos, C. Impact of SARS-CoV-2 (Covid-19) on the mental health of healthcare professionals: A systematic review. Rev. Esp. Salud Publica 2020, 94, e202007088. [Google Scholar]
- Kisely, S.; Warren, N.; McMahon, L.; Dalais, C.; Henry, I.; Siskind, D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: Rapid review and meta-analysis. BMJ 2020, 369, m1642. [Google Scholar] [CrossRef]
- Luo, M.; Guo, L.; Yu, M.; Jiang, W.; Wang, H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public—A systematic review and meta-analysis. Psychiatry Res. 2020, 291, 113190. [Google Scholar] [CrossRef]
- Pan, R.; Zhang, L.; Pan, J. The Anxiety Status of Chinese Medical Workers During the Epidemic of COVID-19: A Meta-Analysis. Psychiatry Investig. 2020, 17, 475–480. [Google Scholar] [CrossRef] [PubMed]
- Shaukat, N.; Ali, D.M.; Razzak, J. Physical and mental health impacts of COVID-19 on healthcare workers: A scoping review. Int. J. Emerg. Med. 2020, 13, 40. [Google Scholar] [CrossRef] [PubMed]
- Carmassi, C.; Foghi, C.; Dell’Oste, V.; Cordone, A.; Bertelloni, C.A.; Bui, E.; Dell’Osso, L. PTSD symptoms in healthcare workers facing the three coronavirus outbreaks: What can we expect after the COVID-19 pandemic. Psychiatry Res. 2020, 292, 113312. [Google Scholar] [CrossRef] [PubMed]
- Nelson, C.A.; Scott, R.D.; Bhutta, Z.A.; Harris, N.B.; Danese, A.; Samara, M. Adversity in childhood is linked to mental and physical health throughout life. BMJ 2020, 371, m3048. [Google Scholar] [CrossRef]
- Cohen, S.; Murphy, M.L.M.; Prather, A.A. Ten Surprising Facts About Stressful Life Events and Disease Risk. Annu. Rev. Psychol. 2019, 70, 577–597. [Google Scholar] [CrossRef]
- Overstreet, C.; Berenz, E.C.; Kendler, K.S.; Dick, D.M.; Amstadter, A.B. Predictors and mental health outcomes of potentially traumatic event exposure. Psychiatry Res. 2017, 247, 296–304. [Google Scholar] [CrossRef] [Green Version]
- Ventriglio, A.; Gentile, A.; Baldessarini, R.J.; Bellomo, A. Early-life stress and psychiatric disorders: Epidemiology, neurobiology and innovative pharmacological targets. Curr. Pharm. Des. 2015, 21, 1379–1387. [Google Scholar] [CrossRef]
- Nelson, J.; Klumparendt, A.; Doebler, P.; Ehring, T. Childhood maltreatment and characteristics of adult depression: Meta-analysis. Br. J. Psychiatry 2017, 210, 96–104. [Google Scholar] [CrossRef] [PubMed]
- Mazza, C.; Ricci, E.; Biondi, S.; Colasanti, M.; Ferracuti, S.; Napoli, C.; Roma, P. A Nationwide Survey of Psychological Distress among Italian People during the COVID-19 Pandemic: Immediate Psychological Responses and Associated Factors. Int. J. Environ. Res. Public Health 2020, 17, 3165. [Google Scholar] [CrossRef] [PubMed]
- Wiseman, T.A.; Curtis, K.; Lam, M.; Foster, K. Incidence of depression, anxiety and stress following traumatic injury: A longitudinal study. Scand. J. Trauma. Resusc. Emerg. Med. 2015, 23, 29. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Preti, E.; Di Mattei, V.; Perego, G.; Ferrari, F.; Mazzetti, M.; Taranto, P.; Di Pierro, R.; Madeddu, F.; Calati, R. The Psychological Impact of Epidemic and Pandemic Outbreaks on Healthcare Workers: Rapid Review of the Evidence. Curr. Psychiatry Rep. 2020, 22, 43. [Google Scholar] [CrossRef] [PubMed]
- Park, J.-S.; Lee, E.-H.; Park, N.-R.; Choi, Y.H. Mental Health of Nurses Working at a Government-designated Hospital During a MERS-CoV Outbreak: A Cross-sectional Study. Arch. Psychiatr. Nurs. 2018, 32, 2–6. [Google Scholar] [CrossRef] [Green Version]
- Salazar de Pablo, G.; Vaquerizo-Serrano, J.; Catalan, A.; Arango, C.; Moreno, C.; Ferre, F.; Shin, J.I.; Sullivan, S.; Brondino, N.; Solmi, M.; et al. Impact of coronavirus syndromes on physical and mental health of health care workers: Systematic review and meta-analysis. J. Affect. Disord. 2020, 275, 48–57. [Google Scholar] [CrossRef]
- Saragih, I.D.; Tonapa, S.I.; Saragih, I.S.; Advani, S.; Batubara, S.O.; Suarilah, I.; Lin, C.-J. Global prevalence of mental health problems among healthcare workers during the Covid-19 pandemic: A systematic review and meta-analysis. Int. J. Nurs. Stud. 2021, 121, 104002. [Google Scholar] [CrossRef]
- Salari, N.; Hosseinian-Far, A.; Jalali, R.; Vaisi-Raygani, A.; Rasoulpoor, S.; Mohammadi, M.; Rasoulpoor, S.; Khaledi-Paveh, B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Glob. Health 2020, 16, 57. [Google Scholar] [CrossRef]
- Kunz, M.; Strasser, M.; Hasan, A. Impact of the coronavirus disease 2019 pandemic on healthcare workers: Systematic comparison between nurses and medical doctors. Curr. Opin. Psychiatry 2021, 34, 413–419. [Google Scholar] [CrossRef] [PubMed]
- Cai, Q.; Feng, H.; Huang, J.; Wang, M.; Wang, Q.; Lu, X.; Xie, Y.; Wang, X.; Liu, Z.; Hou, B.; et al. The mental health of frontline and non-frontline medical workers during the coronavirus disease 2019 (COVID-19) outbreak in China: A case-control study. J. Affect. Disord. 2020, 275, 210–215. [Google Scholar] [CrossRef] [PubMed]
- Hu, D.; Kong, Y.; Li, W.; Han, Q.; Zhang, X.; Zhu, L.X.; Wan, S.W.; Liu, Z.; Shen, Q.; Yang, J.; et al. Frontline nurses’ burnout, anxiety, depression, and fear statuses and their associated factors during the COVID-19 outbreak in Wuhan, China: A large-scale cross-sectional study. EClinicalMedicine 2020, 24, 100424. [Google Scholar] [CrossRef] [PubMed]
- Dobson, H.; Malpas, C.B.; Burrell, A.J.; Gurvich, C.; Chen, L.; Kulkarni, J.; Winton-Brown, T. Burnout and psychological distress amongst Australian healthcare workers during the COVID-19 pandemic. Australas. Psychiatry 2021, 29, 26–30. [Google Scholar] [CrossRef] [PubMed]
- Sarboozi Hoseinabadi, T.; Kakhki, S.; Teimori, G.; Nayyeri, S. Burnout and its influencing factors between frontline nurses and nurses from other wards during the outbreak of Coronavirus Disease -COVID-19- in Iran. Investig. Educ. Enferm. 2020, 38, 2. [Google Scholar] [CrossRef]
- Rossi, R.; Socci, V.; Pacitti, F.; Di Lorenzo, G.; Di Marco, A.; Siracusano, A.; Rossi, A. Mental Health Outcomes Among Frontline and Second-Line Health Care Workers During the Coronavirus Disease 2019 (COVID-19) Pandemic in Italy. JAMA Netw. Open 2020, 3, e2010185. [Google Scholar] [CrossRef] [PubMed]
- Ying, Y.; Ruan, L.; Kong, F.; Zhu, B.; Ji, Y.; Lou, Z. Mental health status among family members of health care workers in Ningbo, China, during the coronavirus disease 2019 (COVID-19) outbreak: A cross-sectional study. BMC Psychiatry 2020, 20, 379. [Google Scholar] [CrossRef]
- Pollock, A.; Campbell, P.; Cheyne, J.; Cowie, J.; Davis, B.; McCallum, J.; McGill, K.; Elders, A.; Hagen, S.; McClurg, D.; et al. Interventions to support the resilience and mental health of frontline health and social care professionals during and after a disease outbreak, epidemic or pandemic: A mixed methods systematic review. Cochrane Database Syst. Rev. 2020, 11, CD013779. [Google Scholar] [CrossRef]
- Santabárbara, J.; Bueno-Notivol, J.; Lipnicki, D.M.; Olaya, B.; Pérez-Moreno, M.; Gracia-García, P.; Idoiaga-Mondragon, N.; Ozamiz-Etxebarria, N. Prevalence of anxiety in health care professionals during the COVID-19 pandemic: A rapid systematic review (on published articles in Medline) with meta-analysis. Prog. Neuropsychopharmacol. Biol. Psychiatry 2021, 107, 110244. [Google Scholar] [CrossRef]
- Chirico, F.; Nucera, G.; Magnavita, N. Protecting the mental health of healthcare workers during the COVID-19 emergency. BJPsych Int. 2021, 18, E1. [Google Scholar] [CrossRef]
- Blake, H.; Bermingham, F.; Johnson, G.; Tabner, A. Mitigating the Psychological Impact of COVID-19 on Healthcare Workers: A Digital Learning Package. Int. J. Environ. Res. Public Health 2020, 17, 2997. [Google Scholar] [CrossRef]
- Minelli, A.; Zampieri, E.; Sacco, C.; Bazzanella, R.; Mezzetti, N.; Tessari, E.; Barlati, S.; Bortolomasi, M. Clinical efficacy of trauma-focused psychotherapies in treatment-resistant depression (TRD) in-patients: A randomized, controlled pilot-study. Psychiatry Res. 2019, 273, 567–574. [Google Scholar] [CrossRef]
- Yan, S.; Shan, Y.; Zhong, S.; Miao, H.; Luo, Y.; Ran, H.; Jia, Y. The Effectiveness of Eye Movement Desensitization and Reprocessing Toward Adults With Major Depressive Disorder: A Meta-Analysis of Randomized Controlled Trials. Front. Psychiatry 2021, 12, 700458. [Google Scholar] [CrossRef] [PubMed]
| Variable | Overall (N = 271) |
|---|---|
| Gender | |
| Female | 198 (73.1%) |
| Male | 73 (26.9%) |
| Age | |
| Mean (SD) | 45.37 (10.94) |
| Median (Q1, Q3) | 47.00 (36.00, 55.00) |
| Range | 22.00–67.00 |
| Years of education | |
| Mean (SD) | 17.72 (3.85) |
| Median (Q1, Q3) | 16.00 (16.00, 23.00) |
| Range | 8.00–23.00 |
| Marital status | |
| Married | 187 (69.1%) |
| Unmarried | 51 (18.8%) |
| Divorced | 31 (11.4%) |
| Widowed | 2 (0.7%) |
| Living condition | |
| Cohabiting couples with sons/daughters | 120 (44.3%) |
| Cohabiting couples | 68 (25.1%) |
| Alone | 38 (14.0%) |
| Sons/Daughters | 18 (6.6%) |
| Parents | 17 (6.3%) |
| Other conditions | 10 (3.7%) |
| Professional role | |
| Nurse | 86 (31.7%) |
| Psychiatrist/Training psychiatrist | 60 (22.1%) |
| PRT/Educator | 59 (21.8%) |
| Psychologist/Psychotherapist | 44 (16.2%) |
| Other mental health professions | 22 (8.1%) |
| Workplace | |
| Hospital | 159 (58.7%) |
| Local mental health services | 80 (29.5%) |
| Psychiatric residence | 25 (9.2%) |
| Semi-residential centers | 7 (2.6%) |
| Years of professional experience | |
| At most 10 | 74 (27.3%) |
| Greater than 10 | 197 (72.7%) |
| Variable | Total (N = 271) | Nurses (N = 86) | Psychiatrists/Training Psychiatrists (N = 60) | PRTs/Educators (N = 59) | Psychologists/Psychotherapists (N = 44) | Other Mental Health Professionals (N = 22) | p-Value |
|---|---|---|---|---|---|---|---|
| COVID-19 positive | |||||||
| No | 255 (94.1%) | 77 (89.5%) | 57 (95.0%) | 57 (96.6%) | 43 (97.7%) | 21 (95.5%) | 0.353 a |
| Yes | 16 (5.9%) | 9 (10.5%) | 3 (5.0%) | 2 (3.4%) | 1 (2.3%) | 1 (4.5%) | |
| Family member COVID-19 positive | |||||||
| No | 248 (91.5%) | 78 (90.7%) | 55 (91.7%) | 52 (88.1%) | 42 (95.5%) | 21 (95.5%) | 0.754 a |
| Yes | 23 (8.5%) | 8 (9.3%) | 5 (8.3%) | 7 (11.9%) | 2 (4.5%) | 1 (4.5%) | |
| Fear of contagion | |||||||
| No | 165 (60.9%) | 44 (51.2%) | 27 (45.0%) | 46 (78.0%) | 31 (70.5%) | 17 (77.3%) | <0.001a* |
| Yes | 106 (39.1%) | 42 (48.8%) | 33 (55.0%) | 13 (22.0%) | 13 (29.5%) | 5 (22.7%) | |
| Death of a loved one | |||||||
| No | 241 (88.9%) | 77 (89.5%) | 48 (80.0%) | 55 (93.2%) | 42 (95.5%) | 19 (86.4%) | 0.092 a |
| Yes | 30 (11.1%) | 9 (10.5%) | 12 (20.0%) | 4 (6.8%) | 2 (4.5%) | 3 (13.6%) | |
| Death of a patient | |||||||
| No | 240 (88.6%) | 72 (83.7%) | 49 (81.7%) | 58 (98.3%) | 43 (97.7%) | 18 (81.8%) | 0.002a* |
| Yes | 31 (11.4%) | 14 (16.3%) | 11 (18.3%) | 1 (1.7%) | 1 (2.3%) | 4 (18.2%) | |
| Workload | |||||||
| Decreased | 78 (28.8%) | 11 (12.8%) | 18 (30.0%) | 20 (33.9%) | 24 (54.5%) | 5 (22.7%) | <0.001a* |
| Unchanged | 77 (28.4%) | 16 (18.6%) | 24 (40.0%) | 18 (30.5%) | 10 (22.7%) | 9 (40.9%) | |
| Increased | 116 (42.8%) | 59 (68.6%) | 18 (30.0%) | 21 (35.6%) | 10 (22.7%) | 8 (36.4%) | |
| Team relationship | |||||||
| Got worse | 98 (36.2%) | 34 (39.5%) | 21 (35.0%) | 27 (45.8%) | 13 (29.5%) | 3 (13.6%) | 0.043a* |
| Unchanged | 112 (41.3%) | 34 (39.5%) | 23 (38.3%) | 23 (39.0%) | 16 (36.4%) | 16 (72.7%) | |
| Improved | 61 (22.5%) | 18 (20.9%) | 16 (26.7%) | 9 (15.3%) | 15 (34.1%) | 3 (13.6%) | |
| Family divided | |||||||
| No | 186 (68.6%) | 60 (69.8%) | 37 (61.7%) | 38 (64.4%) | 34 (77.3%) | 17 (77.3%) | 0.529 |
| Yes | 38 (14.0%) | 12 (14.0%) | 11 (18.3%) | 6 (10.2%) | 7 (15.9%) | 2 (9.1%) | |
| I live alone | 35 (12.9%) | 12 (14.0%) | 8 (13.3%) | 10 (16.9%) | 3 (6.8%) | 2 (9.1%) | |
| Unknown | 12 (4.4%) | 2 (2.3%) | 4 (6.7%) | 5 (8.5%) | 0 (0.0%) | 1 (4.5%) | |
| Variable | Total (N = 271) | Nurses (N = 86) | Psychiatrists/Training Psychiatrists (N = 60) | PRTs/Educators (N = 59) | Psychologists/ Psychotherapists (N = 44) | Other Mental Health Professionals (N = 22) | p-Value |
|---|---|---|---|---|---|---|---|
| IES-R total | |||||||
| Mean (SD) | 19.38 (15.47) | 26.63 (16.86) | 15.83 (14.63) | 18.73 (13.22) | 14.14 (14.11) | 12.95 (9.06) | <0.001b* |
| Median (Q1, Q3) | 17.00 (7.50, 29.00) | 24.00 (14.00, 38.00) | 13.50 (4.00, 23.25) | 16.00 (8.50, 29.50) | 11.00 (4.00, 20.25) | 13.50 (4.00, 18.00) | |
| Range | 0.00–88.00 | 0.00–88.00 | 0.00–77.00 | 1.00–57.00 | 0.00–76.00 | 0.00–29.00 | |
| % IES-R Total score ≥ 33 | 19.19% | 37.21% | 10.00% | 20.34% | 4.55% | 0.00% | – |
| IES-R avoidance | |||||||
| Mean (SD) | 6.16 (5.49) | 8.43 (6.13) | 5.38 (5.29) | 5.95 (4.60) | 4.11 (4.76) | 4.05 (3.93) | <0.001b* |
| Median (Q1, Q3) | 5.00 (2.00, 9.00) | 7.00 (4.00, 11.00) | 4.00 (1.00, 8.25) | 5.00 (3.00, 8.00) | 3.00 (1.00, 5.25) | 3.00 (1.00, 6.25) | |
| Range | 0.00–32.00 | 0.00–32.00 | 0.00–22.00 | 0.00–17.00 | 0.00–24.00 | 0.00–15.00 | |
| IES-R intrusion | |||||||
| Mean (SD) | 7.69 (6.53) | 10.60 (7.28) | 6.47 (6.19) | 7.41 (5.57) | 5.50 (5.63) | 4.73 (4.11) | <0.001b* |
| Median (Q1, Q3) | 7.00 (3.00, 11.00) | 10.00 (4.25, 16.00) | 5.50 (1.00, 10.00) | 6.00 (3.00, 10.00) | 4.00 (1.00, 9.00) | 4.00 (2.00, 7.00) | |
| Range | 0.00–32.00 | 0.00–32.00 | 0.00–31.00 | 0.00–23.00 | 0.00–29.00 | 0.00–13.00 | |
| IES-R hyperarousal | |||||||
| Mean (SD) | 5.54 (4.94) | 7.59 (5.39) | 3.98 (4.61) | 5.37 (4.59) | 4.52 (4.45) | 4.18 (3.10) | <0.001b* |
| Median (Q1, Q3) | 4.00 (2.00, 8.00) | 6.00 (4.00, 10.75) | 3.00 (0.00, 6.00) | 4.00 (2.00, 7.50) | 3.50 (1.00, 6.00) | 4.00 (2.00, 6.75) | |
| Range | 0.00–24.00 | 0.00–24.00 | 0.00–24.00 | 0.00–17.00 | 0.00–23.00 | 0.00–10.00 |
| Variable | Total (N = 271) | Nurses (N = 86) | Psychiatrists/Training Psychiatrists (N = 60) | PRTs/Educators (N = 59) | Psychologists/ Psychotherapists (N = 44) | Other Mental Health Professionals (N = 22) | p-Value |
|---|---|---|---|---|---|---|---|
| DASS Depression | |||||||
| Mean (SD) | 5.85 (6.99) | 7.60 (7.08) | 2.55 (3.10) | 6.61 (7.85) | 5.13 (7.06) | 4.05 (5.87) | <0.001b* |
| Median (Q1, Q3) | 4.00 (0.00, 8.00) | 6.00 (2.00, 10.00) | 1.00 (0.00, 4.00) | 4.00 (0.00, 10.00) | 3.00 (0.00, 6.00) | 2.00 (0.00, 6.00) | |
| Range | 0.00–38.00 | 0.00–28.00 | 0.00–10.00 | 0.00–36.00 | 0.00–38.00 | 0.00–34.00 | |
| DASS Anxiety | |||||||
| Mean (SD) | 3.81 (5.47) | 5.77 (6.07) | 1.45 (2.48) | 4.14 (5.10) | 2.30 (5.22) | 2.77 (4.94) | <0.001b* |
| Median (Q1, Q3) | 2.00 (0.00, 6.00) | 4.00 (0.50, 8.00) | 0.00 (0.00, 2.00) | 2.00 (0.00, 6.00) | 0.00 (0.00, 2.50) | 0.00 (0.00, 4.00) | |
| Range | 0.00–34.00 | 0.00–26.00 | 0.00–8.00 | 0.00–22.00 | 0.00–34.00 | 0.00–26.00 | |
| DASS Stress | |||||||
| Mean (SD) | 10.84 (7.88) | 13.09 (7.82) | 7.09 (7.03) | 10.54 (7.30) | 10.03 (8.43) | 9.82 (7.49) | 0.006b* |
| Median (Q1, Q3) | 10.00 (6.00, 16.00) | 12.00 (6.00, 19.50) | 5.00 (0.50, 10.00) | 10.00 (6.00, 15.00) | 8.00 (4.00, 14.50) | 8.00 (5.50, 14.50) | |
| Range | 0.00–40.00 | 0.00–30.00 | 0.00–24.00 | 0.00–34.00 | 0.00–40.00 | 0.00–30.00 |
| IES-R Total | DASS Depression | DASS Anxiety | DASS Stress |
|---|---|---|---|
| Age | Age | Age | Age |
| Professional role | Professional role | Professional role | Professional role |
| Workload | Workload | Workload | Team relationship |
| Team relationship | Team relationship | Team relationship | Workload |
| Family divided | Family divided | Family divided | Family divided |
| LEC13—Severe human suffering (Yes) | LEC9—Other unwanted sexual experience (Yes) | LEC9—Other unwanted sexual experience (Yes) | LEC13—Severe human suffering (Yes) |
| LEC13—Severe human suffering (Yes) | LEC9—Other unwanted sexual experience (Yes) | ||
| LEC7—Any stressful event (Yes) |
| Variable | OR (95% CI) | p-Value |
|---|---|---|
| Moderate/severe symptoms, IES-R total | ||
| Age | 1.06 (1.02–1.10) | 0.0037 |
| Professional role (Other health professions) | 0.14 (0.02–0.73) | 0.0404 |
| Professional role (Psychiatrist/Speciality psychiatry) | 0.16 (0.06–0.44) | 0.0005 |
| Professional role (Psychologist/Psychotherapist) | 0.17 (0.04–0.55) | 0.0050 |
| During COVID-19 workload (Increased) | 3.41 (1.33–9.30) | 0.0128 |
| During COVID-19 team relationship (Improved) | 0.22 (0.08–0.59) | 0.0034 |
| LEC9—Other unwanted sexual experience (Yes) | 7.27 (2.05–28.46) | 0.0028 |
| LEC13—Severe human suffering (Yes) | 3.34 (1.57–7.43) | 0.0022 |
| Moderate/severe symptoms, DASS Depression | ||
| Professional role (Psychologist/Psychotherapist) | 0.05 (0–0.47) | 0.0254 |
| LEC5—Exposure toxic substance (Yes) | 60.24 (5.46–990.06) | 0.0016 |
| LEC9—Other unwanted sexual experience (YES) | 6.62 (1.22–37.32) | 0.0273 |
| LEC13—Severe human suffering (Yes) | 5.74 (1.69–23.17) | 0.0079 |
| Moderate/severe symptoms, DASS Anxiety | ||
| Professional role (Psychiatrist/Speciality psychiatry) | 0.16 (0.03–0.66) | 0.0211 |
| Professional role (Psychologist/Psychotherapist) | 0.14 (0.02–0.81) | 0.0463 |
| LEC9—Other unwanted sexual experience (Yes) | 8.27 (1.67–40.77) | 0.0082 |
| Moderate/severe symptoms, DASS Stress | ||
| Professional role (Psychiatrist/Speciality psychiatry) | 0.30 (0.09–0.89) | 0.0388 |
| During COVID-19 team relationship (Improved) | 0.23 (0.06–0.72) | 0.0168 |
| LEC9—Other unwanted sexual experience (Yes) | 6.41 (1.76–24.44) | 0.0051 |
| LEC13—Severe human suffering (Yes) | 3.03 (1.27–7.53) | 0.0142 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Minelli, A.; Silva, R.C.; Barlati, S.; Vezzoli, M.; Carletto, S.; Isabello, C.; Bortolomasi, M.; Nibbio, G.; Lisoni, J.; Menesello, V.; et al. The Elephant in the Room: A Cross-Sectional Study on the Stressful Psychological Effects of the COVID-19 Pandemic in Mental Healthcare Workers. Brain Sci. 2022, 12, 408. https://doi.org/10.3390/brainsci12030408
Minelli A, Silva RC, Barlati S, Vezzoli M, Carletto S, Isabello C, Bortolomasi M, Nibbio G, Lisoni J, Menesello V, et al. The Elephant in the Room: A Cross-Sectional Study on the Stressful Psychological Effects of the COVID-19 Pandemic in Mental Healthcare Workers. Brain Sciences. 2022; 12(3):408. https://doi.org/10.3390/brainsci12030408
Chicago/Turabian StyleMinelli, Alessandra, Rosana Carvalho Silva, Stefano Barlati, Marika Vezzoli, Sara Carletto, Cinzia Isabello, Marco Bortolomasi, Gabriele Nibbio, Jacopo Lisoni, Valentina Menesello, and et al. 2022. "The Elephant in the Room: A Cross-Sectional Study on the Stressful Psychological Effects of the COVID-19 Pandemic in Mental Healthcare Workers" Brain Sciences 12, no. 3: 408. https://doi.org/10.3390/brainsci12030408
APA StyleMinelli, A., Silva, R. C., Barlati, S., Vezzoli, M., Carletto, S., Isabello, C., Bortolomasi, M., Nibbio, G., Lisoni, J., Menesello, V., Perusi, G., Accardo, V., Deste, G., & Vita, A. (2022). The Elephant in the Room: A Cross-Sectional Study on the Stressful Psychological Effects of the COVID-19 Pandemic in Mental Healthcare Workers. Brain Sciences, 12(3), 408. https://doi.org/10.3390/brainsci12030408