Home-Based Music Therapy to Support Bulbar and Respiratory Functions of Persons with Early and Mid-Stage Amyotrophic Lateral Sclerosis—Protocol and Results from a Feasibility Study
Abstract
:1. Introduction
1.1. Bulbar and Respiratory Involvement in ALS
1.2. Cognitive, Behavioural and Psychological Symptoms in ALS
1.3. Family Caregivers in ALS Care
1.4. The Role of Exercise
1.5. Music Therapy for ALS: Developing Clinical Approach
2. Materials and Methods
2.1. Study Aim
2.2. Registration and Ethical Approvals
2.3. Study Design
2.4. Facility
2.5. Recruitment
2.6. Inclusion Criteria
- (1)
- Amyotrophic Lateral Sclerosis Functional Rating Scale—Revised (ALSFRS-R) [76] bulbar subscore ≥ 9, but ≤11, where bulbar subscore = the sum of ALSFRS-R questions 1–3 (maximum score of 12);
- (2)
- Forced Vital Capacity (FVC) greater than 60%;
- (3)
- (4)
- Able to consent to treatment;
- (5)
- Native speaker of Russian.
2.7. Exclusion Criteria
- (1)
- Tracheostomy or mechanical ventilation;
- (2)
- Diaphragmatic pacer;
- (3)
- Significant concurrent respiratory disease;
- (4)
- Allergies to barium;
- (5)
- Receiving any other experimental treatment for dysarthria, dysphagia, dystussia and dyspnoea for the duration of this study;
- (6)
- Receiving any other music therapy treatment for the duration of this study.
2.8. Caregivers Participating in This Study
2.9. Informed Consent
2.10. The Experimental Music Therapy Treatment Protocol
- (1)
- To increase breath support,
- (2)
- To increase muscle relaxation,
- (3)
- To increase speech rate,
- (4)
- To prevent or decrease hypernasality, and
- (5)
- To maintain coordinated swallow.
2.11. Recommended Exercises for Independent Practice
2.12. Equipment, Transportation and Setup
2.13. Feasibility Data Collection and Analysis
2.14. Biomedical Data Collection
2.15. Outcome Measures to Assess Long-Term Changes in Respiration
2.16. Outcome Measures to Assess Long-Term Changes in Cough
2.17. Outcome Measures to Assess Long-Term Changes in Swallowing
2.18. Outcome Measures to Assess Long-Term Changes in Speech
2.19. Biomedical Data Analysis
- Time point 1 = baseline (week 1),
- Time point 2 = pre-treatment (week 6),
- Time point 3 = post-treatment (week 12), and
- Time point 4 = at the end of the follow-up period (week 16).
- Time point 1 = baseline (week 1),
- Time point 2 = pre-treatment (week 6), and
- Time point 3 = post-treatment (week 12).
- Trendrun-in = (Mt2 − Mt1)/6,
- Trendtreatment = (Mt3 − Mt2)/6, and
- Trendfollow-up = (Mt4 − Mt3)/4.
3. Main Study Findings
3.1. Demographics
3.2. Feasibility Data Analysis Results
3.3. Biomedical Data Analysis Results
3.4. Long-Term Changes in Respiration
3.5. Long-Term Changes in Cough
3.6. Long-Term Changes in Speech
- (1)
- Maximum Phonation Time (MPT), sound /a/, measured in seconds, higher score corresponds to better functioning;
- (2)
- Jitter, local, sound /a/, measured in percent, lower score corresponds to better functioning;
- (3)
- Shimmer, local, sound /a/, measured in percent, lower score corresponds to better functioning;
- (4)
- Harmonics-to-Noise Ratio (HNR), sound /a/ measured in Db, higher score corresponds to better functioning;
- (5)
- Maximum Repetition Rate—Alternating (AMR), /pataka/ sequence, measured in total number of syllables uttered, higher score corresponds to better functioning;
- (6)
- Maximum Repetition Rate—Sequential (SMR), /ba/ syllable, measured in total number of syllables uttered, higher score corresponds to better functioning;
- (7)
- Vowel Space Area, vowels /a, e, i, o, u/, measured in squared Hz, higher score corresponds to better functioning;
- (8)
- Fundamental frequency (F0), oral reading, measured in Hz, higher score corresponds to better functioning;
- (9)
- Speaking rate, oral reading, measured in words per minute, higher score corresponds to better functioning;
- (10)
- Speech–pause ratio, oral reading, measured in seconds per minute, lower score corresponds to better functioning;
- (11)
- Pause frequency, oral reading, measured in number of pauses per minute, lower score corresponds to better functioning;
- (12)
- Hypernasality level, oral reading, measured in points, higher score corresponds to better functioning.
3.7. Long-Term Changes in Swallowing
- (1)
- Time-to-Laryngeal Vestibule Closure, nectar 10 mL, measured in ms, lower score corresponds to better functioning;
- (2)
- Time-to-Laryngeal Vestibule Closure, pudding 10 mL, measured in ms, lower score corresponds to better functioning;
- (3)
- Maximum Pharyngeal Constriction Area, nectar 10 mL, measured in %C2–42 lower score corresponds to better functioning;
- (4)
- Maximum Pharyngeal Constriction Area, pudding 10 mL, measured in %C2–42, lower score corresponds to better functioning;
- (5)
- Peak Position of the Hyoid Bone, nectar 10 mL, measured in %C2–4 higher score corresponds to better functioning;
- (6)
- Peak Position of the Hyoid Bone, pudding 10 mL, measured in %C2–4, higher score corresponds to better functioning;
- (7)
- Penetration–Aspiration Scale Score (worst), nectar 10 mL, measured in points lower score corresponds to better functioning;
- (8)
- Penetration–Aspiration Scale Score (worst), pudding 10 mL, measured in points, lower score corresponds to better functioning;
- (9)
- Total Pharyngeal Residue C24area, nectar 10 mL, measured in %C2–4, lower score corresponds to better functioning;
- (10)
- Total Pharyngeal Residue C24area, pudding 10 mL, measured in %C2–4, lower score corresponds to better functioning;
- (11)
- Laryngeal vestibule closure, nectar 10 mL, described as complete, partial, or incomplete, LVC described as “complete” corresponds to a safe swallow;
- (12)
- Laryngeal vestibule closure, pudding 10 mL, described as complete, partial, or incomplete, LVC described as “complete” corresponds to a safe swallow.
4. Discussion
4.1. The Feasibility of the Suggested Study Protocol
4.2. Unique Properties of MT Interventions and the Potential Role of MT in MDT ALS Care
4.3. Study Limitations
4.4. Measuring Changes in Bulbar Functions in ALS
4.5. The Need for an Efficacy Study
4.6. Suggested Study Protocol Modifications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Study Consort
| Approximately 110 ALS patients in the Moscow region are followed by the ALS Centre Moscow team. All newly diagnosed patients living in Moscow and meeting the inclusion and exclusion criteria were invited to participate, until the desired sample size (n = 8) was achieved. Age: 18+; ALSFRS-R bulbar subscore ≥ 9, but ≤11; FVC > 60%; unimpaired cognition (ECAS); can consent; native Russian speakers; no diaphragmatic pacer; notracheostomy; no significant concurrent respiratory diseases; not receiving other music therapy or other experimental treatment for bulbar and respiratory symptoms. Participants started the trial simultaneously. Each participant received treatment and served as their own control. | |
| Week 1 | Data collection: home based—FVC, MIP, MEP, PEF, CNS-BFS swallowing and bulbar subscores, voice samples; lab—VFSS. |
| Week 5 | Data collection: participant interview, caregiver interview (questionnaire) |
| Treatment: weeks 6–12 | Music therapy treatment (2 × per week for 6 weeks) and data collection: home based—NRS respiration and NRS speech scales, attendance, adherence to independent exercises routine (weeks 7–12), treatment notes |
| Week 6 | Data collection: home based—FVC, MIP, MEP, PEF, CNS-BFS swallowing and bulbar subscores, voice samples; lab—VFSS |
| Week 12 | Data collection: home based—FVC, MIP, MEP, PEF, CNS-BFS swallowing and bulbar subscores, voice samples; lab—VFSS |
| Week 13 | Data collection: participant interview, caregiver interview (questionnaire) |
| Follow up: week 16 | Follow-up data collection: home based—FVC, MIP, MEP, PEF, CNS-BFS swallowing and bulbar subscores, voice samples |
| Data analysis | Analysis of feasibility and biometric data, thematic analysis of questionnaire data |
Appendix B. Voice Care Guidelines for Research Participants—Persons with ALS (English Translation)
- Do not talk for too long. If your voice is tired, be sure to take a break.
- Do not talk in a noisy environment (with the TV turned on, in the car, in public transport). Only talk to those who are near you. Do not shout. Use a bell or other signal to attract attention.
- Maintain even posture and speak “from the diaphragm”.
- Drink enough water throughout the day.
- Rest. If you are tired, try not to talk. Get enough sleep.
- Slow down your speech and stretch sounds, especially at the ends of words, as if you were singing.
- Speak lightly—in a range convenient for you (not too low and not too high) and with a comfortable volume (do not scream or whisper).
- Regularly relax the muscles of the face, neck and shoulders.
- If speaking causes pain, do not speak. Do not use cough drops to relieve a sore throat and keep talking: this only masks the symptoms and you can damage your voice.
- Take care of yourself: our emotions affect our voice and breath. Do everything you can to reduce stress in your life and get positive experiences regularly.
Appendix C. Sample Recommended Daily Exercises Instructions (English Translation)
- /V/
- /Z/
- /Z</
- /L/
- /R/
- /J/
- /M/
- /N/
- /B/
- /D/
- /G/
Appendix D. Numerical Rating Scale for Current Perceived Ease of Respiration (English Translation)
Appendix E. Numerical Rating Scale for Current Perceived Ease of Speech (English Translation)

Appendix F. Interviews with Research Participants—Persons with ALS, Conducted Prior to Treatment (Week 5) (English Translation)
- Question 1. How, you think, may music therapy affect your speech, breathing and swallowing?
- Question 2. How, you think, may music therapy affect you otherwise?
- Question 3. What do you expect in music therapy sessions?
- Question 4. How, you think, will it be to independently do the assigned music therapy exercises between the sessions?
- Question 5. How, you think, may these music therapy exercises affect your speech, breathing and swallowing?
- Question 6. Other comments.
Appendix G. Interviews with Research Participants—Persons with ALS, Conducted at the End of the Follow-Up Period (Week 16) (English Translation)
- Question 1. Has music therapy affected your speech, breathing and swallowing? In which way?
- Question 2. Has music therapy affected you otherwise?
- Question 3. How did it feel to participate in music therapy sessions?
- Question 4. How was it to independently do the assigned music therapy exercises between the sessions?
- Question 5. Have these music therapy exercises affected your speech, breathing and swallowing?
- Question 6. Other comments.
Appendix H. Interviews with Research Participants—Caregivers of Persons with ALS, Conducted Prior to Treatment (Week 5) (English Translation)
- Question 1. How, you think, may music therapy affect speech, breathing and swallowing of X (person with ALS)?
- Question 2. How, you think, may music therapy affect X (person with ALS) otherwise?
- Question 3. How, you think, X’s engagement in music therapy may affect you as a primary caregiver?
Appendix I. Interviews with Research Participants—Caregivers of Persons with ALS, Conducted at the End of the Follow-Up Period (Week 16) (English Translation)
- Question 1. Has music therapy affected X’s (person with ALS) speech, breathing and swallowing?
- Question 2. Has music therapy affected X (person with ALS) otherwise?
- Question 3. Has X’s (person with ALS) engagement in music therapy affected you as a primary caregiver?
- Question 4. Other comments.
Appendix J. Text for Oral Reading Task (Russian)
Дoм, в кoтoрoм я живу, распoлoжен на oкраине маленькoгo гoрoдка, у самoй пoдoшвы гoры. Здесь мягкий климат и редкo идут дoжди. Нoчью небoсвoд бывает так густo усеян звездами, чтo кажется, будтo все миллиарды их из нашей галактики разбрoсаны вверху над мoей гoлoвoй. Летним утрoм, как тoлькo я oткрываю oкнo, мoя бoльшая кoмната напoлняется запахoм цветoв. Ветки черешен смoтрят мне в oкна, и легкий теплый ветер усыпает мoй письменный стoл белыми лепестками.Я слушаю щебет птиц. Вoт с искрoметным задoрoм прoпел зяблик. Где-тo дятел устраивает дуплo. А этo черные дрoзды—пoют не хуже сoлoвьев. Прямo передo мнoй внизу—пестрый узoр из крыш гoрoдских дoмoв, а вдалеке, на краю гoризoнта, тянется серебряная цепь снегoвых вершин... Веселo жить в такoй земле! Отраднoе чувствo разливается в жилах: вoкруг величественные гoры, вoздух чистый и свежий, сoлнце яркoе, небo синее—чегo еще желать?.. Бьют настенные часы над каминoм: пять, шесть, семь, вoсемь, девять... Нужнo тoрoпиться в бюрo. Минуты две-три ищу в шкафу электрическую схему, привезенную французским кoллегoй. Накoнец заглядываю в пoртфель, нахoжу ее внутри и вкладываю в книгу. Пoсле этoгo плoтнo закрываю жалюзи, oднакo сквoзь щелки все равнo прoбивается сoлнечный свет. Выхoжу на крыльцo и запираю ключoм дверь. Спустившись ниже к центру гoрoда, иду бульварoм. Часть дoрoги прoхoдит пo пешехoднoму мoсту через реку. Гибкие стальные трoсы держат невысoкий мoст. Они привязаны к специальным тяжелым якoрям, врытым в землю. Останавливаюсь в начале мoстика у oграды, чтoбы пoлюбoваться рельефными склoнами гoрных хребтoв, всматриваюсь в речную рябь. Пoд мoстoм с шумoм плещутся мелкие рыбешки, вoзмущая вoдную гладь. Откуда-тo дoнoсится музыка: нoктюрн Шoпена—пoзывные местнoй радиoстанции.Вдруг пoзади себя я слышу: „Сережа, неужели этo ты? Вoт так встреча!“. Я узнаю этoт низкий гoлoс. Обoрачиваюсь—так и есть: Андрей Сафoнoв!Очень радoстнo видеть егo внoвь. С Андреем мы знакoмы с кoнца вoсьмидесятых—служили вместе в армии. Егo, энергичнoгo и oбщительнoгo, всегда на пoмoщь гoтoвoгo прийти, любили все. Меня пoкoрили егo честнoсть и недюжинная сила. Мы были дружны, нo пoтoм, малo-пoмалу, связь наша oбoрвалась.—Здравствуй, Андрюша! Как ты тут oказался? —Кoмандирoвка в архив: предлагают снять сюжет прo судoверфь. Вчера приехали—сегoдня уезжаем. Вернее, улетаем—к четырем в аэрoпoрт. —Так скoрo? И куда? —Следующим пунктoм Уфа. Прямoй рейс. А ты, значит, теперь здесь живешь? Давнo? —Два гoда будет в феврале. Обменял свoю гoрoдскую квартиру на бревенчатую избу. —Серьезнo? Не жалеешь? В глазах мoегo приятеля мелькнул веселый oгoнек. —Нискoлькo. Отдыхаю oт килoметрoвых прoбoк, сутoлoки и пыли. —Пo-прежнему плывешь прoтив течения? Счастливый ты челoвек, Сергей. —Ладнo, расскажи лучше o себе. Мы тысячу лет не виделись. Как жизнь? Как семья? —Все у нас хoрoшo, все здoрoвы. Мы с женoй рабoтаем, дoчь гимназию заканчивает. —Ну а Федoр как? Учится? —Он в этoм гoду пoступил в медицинский.—Какoй мoлoдец! Пoздравляю вас! —Спасибo. —Кстати, ты пoзавтракал? —Немнoгo кoфе выпил в гoстинице.С удoвoльствием бы съел чтo-нибудь. —Недалекo oтсюда есть кафе. Мы привыкли там есть. Пoйдем, прoвoжу тебя. Впoлне приличный сервис, разнooбразнoе меню. Однo из их „фирменных“ блюд—рыба пo-бенгальски. Рекoмендую: вкус неoбыкнoвенный—для настoящих гурманoв. —Звучит слишкoм изысканнo. Пoпрoще ничегo нет? —Как насчет яичницы с грибами? —В самый раз. А ты тoрoпишься? Мoжет быть, сoставишь мне кoмпанию? За разгoвoрами и вoспoминаниями незаметнo прoлетел завтрак. Приближалoсь время сказать „дo свидания“. Мы расстались в твердoм намерении бoльше не терять друг друга из виду.Source: [126] (pp. 6–10)
References
- Marin, B.; Boumédiene, F.; Logroscino, G.; Couratier, P.; Babron, M.-C.; Leutenegger, A.-L.; Copetti, M.; Preux, P.-M.; Beghi, E. Variation in worldwide incidence of amyotrophic lateral sclerosis: A meta-analysis. Int. J. Epidemiol. 2017, 46, 57–74. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Longinetti, E.; Fang, F. Epidemiology of amyotrophic lateral sclerosis: An update of recent literature. Curr. Opin. Neurol. 2019, 32, 771–776. [Google Scholar] [CrossRef] [PubMed]
- Qureshi, M.M.; Hayden, D.; Urbinelli, L.; Ferrante, K.; Newhall, K.; Myers, D.; Hilgenberg, S.; Smart, R.; Brown, R.H.; Cudkowicz, M.E. Analysis of factors that modify susceptibility and rate of progression in amyotrophic lateral sclerosis (ALS). Amyotroph. Lateral Scler. 2006, 7, 173–182. [Google Scholar] [CrossRef] [PubMed]
- Patel, B.P.; Hamadeh, M.J. Nutritional and exercise-based interventions in the treatment of amyotrophic lateral sclerosis. Clin. Nutr. 2009, 28, 604–617. [Google Scholar] [CrossRef]
- Plowman, E.K. Is there a role for exercise in the management of bulbar dysfunction in amyotrophic lateral sclerosis? J. Speech Lang. Hear. Res. 2015, 58, 1151–1166. [Google Scholar] [CrossRef]
- Hecht, M. Subjective experience and coping in ALS. Amyotroph. Lateral Scler. Mot. Neuron Disord. 2002, 3, 225. [Google Scholar] [CrossRef]
- Paris, G.; Martinaud, O.; Petit, A.; Cuvelier, A.; Hannequin, D.; Roppeneck, P.; Verin, E. Oropharyngeal dysphagia in amyotrophic lateral sclerosis alters quality of life. J. Oral Rehabil. 2013, 40, 199–204. [Google Scholar] [CrossRef]
- Chiò, A.; Logroscino, G.; Hardiman, O.; Swingler, R.; Mitchell, D.; Beghi, E.; Traynor, B.G.; Eurals Consortium. Prognostic factors in ALS: A critical review. Amyotroph. Lateral Scler. 2009, 10, 310–323. [Google Scholar] [CrossRef] [Green Version]
- Desport, J.C.; Preux, P.M.; Truong, T.C.; Vallat, J.M.; Sautereau, D.; Couratier, P. Nutritional status is a prognostic factor for survival in ALS patients. Neurology 1999, 53, 1059–1063. [Google Scholar] [CrossRef]
- Yang, R.; Huang, R.; Chen, D.; Song, W.; Zeng, Y.; Zhao, B.; Zhou, N.; Shang, H.-F. Causes and places of death of patients with amyotrophic lateral sclerosis in south-west China. Amyotroph. Lateral Scler. 2011, 12, 206–209. [Google Scholar] [CrossRef]
- Corcia, P.; Pradat, P.; Salachas, F.; Bruneteau, G.; Le Forestier, N.; Seilhean, D.; Hauw, J.; Meininger, V. Causes of death in a post-mortem series of ALS patients. Amyotroph. Lateral Scler. 2008, 9, 59–62. [Google Scholar] [CrossRef] [PubMed]
- Czaplinski, A.; Yen, A.A.; Appel, S.H. Amyotrophic lateral sclerosis: Early predictors of prolonged survival. J. Neurol. 2006, 253, 1428–1436. [Google Scholar] [CrossRef] [PubMed]
- Hanson, K.; Yorkston, K.; Britton, D. Dysarthria in amyotrophic lateral sclerosis: A systematic review of characteristics, speech treatment, and augmentative and alternative communication options. J. Med. Speech-Lang. Pathol. 2011, 19, 12. [Google Scholar] [CrossRef]
- Green, J.; Yunusova, Y.; Kuruvilla-Dugdale, M.; Wang, J.; Pattee, G.L.; Synhorst, L.; Zinman, L.; Berry, J.D. Bulbar and speech motor assessment in ALS: Challenges and future directions. Amyotroph. Lateral Scler. Front. Degener. 2013, 14, 494–500. [Google Scholar] [CrossRef]
- Kaub-Wittemer, D.; von Steinbüchel, N.; Wasner, M.; Laier-Groeneveld, G.; Borasio, G.D. Quality of life and psychosocial issues in ventilated patients with amyotrophic lateral sclerosis and their caregivers. J. Pain Symptom Manag. 2003, 26, 890–896. [Google Scholar] [CrossRef]
- Miller, R.G.; Jackson, C.E.; Kasarskis, E.J.; England, J.D.; Forshew, D.; Johnston, W.; Kalra, S.; Katz, J.S.; Mitsumoto, H.; Rosenfeld, J.; et al. Practice parameter update: The care of the patient with amyotrophic lateral sclerosis: Multidisciplinary care, symptom management, and cognitive/behavioral impairment (an evidence-based review): Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 2009, 73, 1227–1233. [Google Scholar] [CrossRef]
- Wolf, J.; Safer, A.; Wöhrle, J.C.; Palm, F.; Nix, W.A.; Maschke, M.; Grau, A.J. Todesursachen bei amyotropher Lateralsklerose; Ergebnisse aus dem ALS-Register Rheinland-Pfalz (Causes of death in amyotrophic lateral sclerosis; Results from the Rhineland-Palatinate ALS registry). Nervenarzt 2017, 88, 911–918. [Google Scholar] [CrossRef]
- Phukan, J.; Elamin, M.; Bede, P.; Jordan, N.; Gallagher, L.; Byrne, S.; Lynch, C.; Pender, N.; Hardiman, O. The syndrome of cognitive impairment in amyotrophic lateral sclerosis: A population-based study. J. Neurol. Neurosurg. Psychiatry 2012, 83, 102–108. [Google Scholar] [CrossRef]
- Hardiman, O.; Figlewicz, D.A. The expansions of ALS. Neurology 2012, 79, 842–843. [Google Scholar] [CrossRef] [Green Version]
- Ng, A.S.; Rademakers, R.; Miller, B.L. Frontotemporal dementia: A bridge between dementia and neuromuscular disease. Ann. N. Y. Acad. Sci. 2015, 1338, 71–93. [Google Scholar] [CrossRef] [Green Version]
- Thakore, N.J.; Pioro, E.P. Depression in ALS in a large self-reporting cohort. Neurology 2016, 86, 1031–1038. [Google Scholar] [CrossRef] [PubMed]
- Vignola, A.; Guzzo, A.; Calvo, A.; Moglia, C.; Pessia, A.; Cavallo, E.; Cammarosano, S.; Giacone, S.; Ghiglione, P.; Chiò, A. Anxiety undermines quality of life in ALS patients and caregivers. Eur. J. Neurol. 2008, 15, 1231–1236. [Google Scholar] [CrossRef] [PubMed]
- Kurt, A.; Nijboer, F.; Matuz, T.; Kübler, A. Depression and anxiety in individuals with amyotrophic lateral sclerosis: Epidemiology and management. CNS Drugs 2007, 21, 279–291. [Google Scholar] [CrossRef] [PubMed]
- Galvin, M.; Corr, B.; Madden, C.; Mays, I.; McQuillan, R.; Timonen, V.; Staines, A.; Hardiman, O. Caregiving in ALS—A mixed methods approach to the study of burden. BMC Palliat. Care 2016, 15, 81. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aoun, S.M.; Bentley, B.; Funk, L.; Toye, C.; Grande, G.; Stajduhar, K. A 10-year literature review of family caregiving for motor neurone disease: Moving from caregiver burden studies to palliative care interventions. Palliat. Med. 2013, 27, 437–446. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Qutub, K.; Lacomis, D.; Albert, S.M.; Feingold, E. Life factors affecting depression and burden in amyotrophic lateral sclerosis caregivers. Amyotroph. Lateral Scler. Front. Degener. 2014, 15, 292–297. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Williams, M.T.; Donnelly, J.P.; Holmlund, T.; Battaglia, M. ALS: Family caregiver needs and quality of life. Amyotroph. Lateral Scler. 2008, 9, 279–286. [Google Scholar] [CrossRef]
- Fang, T.; Al Khleifat, A.; Meurgey, J.-H.; Jones, A.; Leigh, P.N.; Bensimon, G.; Al-Chalabi, A. Stage at which riluzole treatment prolongs survival in patients with amyotrophic lateral sclerosis: A retrospective analysis of data from a dose-ranging study. Lancet Neurol. 2018, 17, 416–422. [Google Scholar] [CrossRef] [Green Version]
- Knibb, J.A.; Keren, N.; Kulka, A.; Leigh, P.N.; Martin, S.; Shaw, C.E.; Tsuda, M.; Al-Chalabi, A. A clinical tool for predicting survival in ALS. J. Neurol. Neurosurg. Psychiatry 2016, 87, 1361–1367. [Google Scholar] [CrossRef] [Green Version]
- Sinaki, M.; Mulder, D.W. Amyotrophic lateral sclerosis: Relationship between serum creatine kinase level and patient survival. Arch. Phys. Med. Rehabil. 1986, 67, 169–171. [Google Scholar] [CrossRef]
- Bello-Haas, V.D.; Florence, J.M.; Kloos, A.D.; Scheirbecker, J.; Lopate, G.; Hayes, S.M.; Pioro, E.P.; Mitsumoto, H. A randomized controlled trial of resistance exercise in individuals with ALS. Neurology 2007, 68, 2003–2007. [Google Scholar] [CrossRef] [PubMed]
- Drory, V.E.; Goltsman, E.; Reznik, J.; Mosek, A.; Korczyn, A. The value of muscle exercise in patients with amyotrophic lateral sclerosis. J. Neurol. Sci. 2001, 191, 133–137. [Google Scholar] [CrossRef]
- Lisle, S.; Tennison, M. Amyotrophic lateral sclerosis: The role of exercise. Curr. Sports Med. Rep. 2015, 14, 45–46. [Google Scholar] [CrossRef] [PubMed]
- Pinto, A.C.; Alves, M.; Nogueira, A.; Evangelista, T.; Carvalho, J.; Coelho, A.; de Carvalho, M.; Sales-Luís, M.L. Can amyotrophic lateral sclerosis patients with respiratory insufficiency exercise? J. Neurol. Sci. 1999, 169, 69–75. [Google Scholar] [CrossRef]
- Chen, A.; Montes, J.; Mitsumoto, H. The role of exercise in amyotrophic lateral sclerosis. Phys. Med. Rehabil. Clin. N. Am. 2008, 19, 545–557. [Google Scholar] [CrossRef] [PubMed]
- De Almeida, J.P.L.; Silvestre, R.; Pinto, A.C.; De Carvalho, M. Exercise and amyotrophic lateral sclerosis. Neurol. Sci. 2012, 33, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Bello-Haas, V.D.; Florence, J.M. Therapeutic exercise for people with amyotrophic lateral sclerosis or motor neuron disease. Cochrane Database Syst. Rev. 2013, 2013, CD005229. [Google Scholar] [CrossRef]
- Kitano, K.; Asakawa, T.; Kamide, N.; Yorimoto, K.; Yoneda, M.; Kikuchi, Y.; Sawada, M.; Komori, T. Effectiveness of home-based exercises without supervision by physical therapists for patients with early-stage amyotrophic lateral sclerosis: A pilot study. Arch. Phys. Med. Rehabil. 2018, 99, 2114–2117. [Google Scholar] [CrossRef]
- Lunetta, C.; Lizio, A.; Sansone, V.A.; Cellotto, N.M.; Maestri, E.; Bettinelli, M.; Gatti, V.; Melazzini, M.G.; Meola, G.; Corbo, M. Strictly monitored exercise programs reduce motor deterioration in ALS: Preliminary results of a randomized controlled trial. J. Neurol. 2016, 263, 52–60. [Google Scholar] [CrossRef]
- Pinto, S.; Swash, M.; de Carvalho, M. Respiratory exercise in amyotrophic lateral sclerosis. Amyotroph. Lateral Scler. 2012, 13, 33–43. [Google Scholar] [CrossRef]
- Plowman, E.K.; Watts, S.A.; Tabor, L.; Robison, R.; Gaziano, J.; Domer, A.S.; Richter, J.; Vu, T.; Gooch, C. Impact of expiratory strength training in amyotrophic lateral sclerosis. Muscle Nerve 2016, 54, 48–53. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tabor, L.C.; Rosado, K.M.; Robison, R.; Hegland, K.; Humbert, I.A.; Plowman, E.K. Respiratory training in an individual with amyotrophic lateral sclerosis. Ann. Clin. Transl. Neurol. 2016, 3, 819–823. [Google Scholar] [CrossRef] [PubMed]
- Paganoni, S.; Karam, C.; Joyce, N.; Bedlack, R.; Carter, G.T. Comprehensive rehabilitative care across the spectrum of amyotrophic lateral sclerosis. NeuroRehabilitation 2015, 37, 53–68. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davis, W.B.; Gfeller, K.E.; Thaut, M.H. An Introduction to Music Therapy: Theory and Practice, 3rd ed.; American Music Therapy Association: Silver Spring, MD, USA, 2008; Volume 18, 573p. [Google Scholar]
- Hanser, S.B. The New Music Therapist’s Handbook, 3rd ed.; Berklee Press Publications: Boston, MA, USA, 2018. [Google Scholar]
- Bonde, L.O.; Wigram, T. A Comprehensive Guide to Music Therapy: Theory, Clinical Practice, Research and Training; Jessica Kingsley Publishers: London, UK, 2002. [Google Scholar]
- Wheeler, B.L. Music Therapy Handbook. Creative Arts and Play Therapy; The Guilford Press: New York, NY, USA; London, UK, 2015; Volume 19, 507p. [Google Scholar]
- Magee, W.L. Why include music therapy in a neuro-rehabilitation team? Adv. Clin. Neurosci. Rehabil. 2020, 19, 10–12. [Google Scholar] [CrossRef]
- Koelsch, S. Brain correlates of music-evoked emotions. Nat. Rev. Neurosci. 2014, 15, 170–180. [Google Scholar] [CrossRef]
- Peretz, I.; Zatorre, R.J. Brain organization for music processing. Annu. Rev. Psychol. 2005, 56, 89–114. [Google Scholar] [CrossRef] [Green Version]
- Thaut, M.H.; McIntosh, G.C.; Ehoemberg, V. Neurobiological foundations of neurologic music therapy: Rhythmic entrainment and the motor system. Front. Psychol. 2015, 5, 1185. [Google Scholar] [CrossRef] [Green Version]
- Zatorre, R.J.; Chen, J.L.; Penhune, V.B. When the brain plays music: Auditory–motor interactions in music perception and production. Nat. Rev. Neurosci. 2007, 8, 547–558. [Google Scholar] [CrossRef]
- Thaut, M.; Hoemberg, V. Handbook of Neurologic Music Therapy; Oxford University Press: Oxford, UK, 2016. [Google Scholar]
- Horne-Thompson, A.; Grocke, D. The effect of music therapy on anxiety in patients who are terminally ill. J. Palliat. Med. 2008, 11, 582. [Google Scholar] [CrossRef] [Green Version]
- Tsitkanou, S.; Della Gatta, P.; Foletta, V.; Russell, A. The role of exercise as a non-pharmacological therapeutic approach for amyotrophic lateral sclerosis: Beneficial or detrimental? Front. Neurol. 2019, 10, 783. [Google Scholar] [CrossRef] [Green Version]
- Bonafede, R.; Mariotti, R. ALS pathogenesis and therapeutic approaches: The role of mesenchymal stem cells and extracellular vesicles. Front. Cell. Neurosci. 2017, 11, 80. [Google Scholar] [CrossRef] [PubMed]
- Byock, I. Dying Well: Peace and Possibilities at the End of Life; Riverhead Books: New York, NY, USA, 1999. [Google Scholar]
- Petering, H.; McLean, J. An interdisciplinary approach of music therapy and nursing in the care of people with motor neurone disease. In Proceedings of the 2001 6th Australian Palliative Care Conference: “Palliative Care—Learning to Live”, Hobart, Australia, 10–12 September 2001. [Google Scholar]
- Lings, J. From “can’t” to “can”: An exploration of the experience of improvisation with a client with Motor Neurone Disease Counterpoints: Music therapy practice in the 21st century. In Proceedings of the First BAMT Conference, Birmingham, UK, 21–23 February 2014. [Google Scholar]
- Forrest, L. Using music therapy in the symptom management of patients with Motor Neurone Disease. In Proceedings of the 10th World Congress on Music Therapy, Oxford, UK, 24 July 2002. [Google Scholar]
- Kondo, K. Music therapy for patients with amyotrophic lateral sclerosis receiving home mechanical ventilation. J. Neurol. Sci. 2017, 381, 562–563. [Google Scholar] [CrossRef]
- Schmid, W. MusicALS: Home-based music therapy for individuals with amyotrophic lateral sclerosis (ALS) and their caring families. Nord J. Music Ther. 2016, 25, 66. [Google Scholar] [CrossRef] [Green Version]
- Raglio, A.; Giovanazzi, E.; Pain, D.; Baiardi, P.; Imbriani, C.; Imbriani, M.; Mora, G. Active music therapy approach in amyotrophic lateral sclerosis: A randomized-controlled trial. Int. J. Rehabil. Res. 2016, 39, 365–367. [Google Scholar] [CrossRef]
- Davies, R.; Baker, F.A.; Tamplin, J.; Bajo, E.; Bolger, K.; Sheers, N.; Berlowitz, D. Music-assisted relaxation during transition to non-invasive ventilation in people with motor neuron disease: A qualitative case series. Br. J. Music Ther. 2016, 30, 74–82. [Google Scholar] [CrossRef]
- Matsuo, K.; Palmer, J.B. Anatomy and physiology of feeding and swallowing: Normal and abnormal. Phys. Med. Rehabil. Clin. N. Am. 2008, 19, 691–707. [Google Scholar] [CrossRef] [Green Version]
- Bukowska, A.A.; Krężałek, P.; Mirek, E.; Bujas, P.; Marchewka, A. Neurologic music therapy training for mobility and stability rehabilitation with Parkinson’s disease—A pilot study. Front. Hum. Neurosci. 2016, 9, 710. [Google Scholar] [CrossRef] [Green Version]
- Gregory, D. Music listening for maintaining attention of older adults with cognitive impairments. J. Music Ther. 2002, 39, 244–264. [Google Scholar] [CrossRef]
- Kim, S.J. Music therapy protocol development to enhance swallowing training for stroke patients with dysphagia. J. Music Ther. 2010, 47, 102–119. [Google Scholar] [CrossRef]
- Särkämö, T.; Tervaniemi, M.; Laitinen, S.; Forsblom, A.; Soinila, S.; Mikkonen, M.; Autti, T.; Silvennoinen, H.M.; Erkkilä, J.; Laine, M.; et al. Music listening enhances cognitive recovery and mood after middle cerebral artery stroke. Brain 2008, 131, 866–876. [Google Scholar] [CrossRef] [Green Version]
- Tamplin, J. A pilot study into the effect of vocal exercises and singing on dysarthric speech. NeuroRehabilitation 2008, 23, 207–216. [Google Scholar] [CrossRef] [PubMed]
- Lillo, P.; Mioshi, E.; Hodges, J.R. Caregiver burden in amyotrophic lateral sclerosis is more dependent on patients’ behavioral changes than physical disability: A comparative study. BMC Neurol. 2012, 12, 156. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ong, M.-L.; Tan, P.F.; Holbrook, J.D. Predicting functional decline and survival in amyotrophic lateral sclerosis. PLoS ONE 2017, 12, e0174925. [Google Scholar] [CrossRef] [Green Version]
- Wheeler, B.L.; Murphy, K.M. Music Therapy Research, 3rd ed.; Barcelona Publishers: Dallas, TX, USA, 2016. [Google Scholar]
- Brylev, L.; Ataulina, A.; Fominykh, V.; Parshikov, V.; Vorobyeva, A.; Istomina, E.; Shikhirimov, R.; Salikov, A.; Zakharova, M.; Guekht, A.; et al. The epidemiology of amyotrophic lateral sclerosis in Moscow (Russia). Amyotroph. Lateral Scler. Front. Degener. 2020, 21, 410–415. [Google Scholar] [CrossRef]
- Brooks, B.R.; Miller, R.G.; Swash, M.; Munsat, T.L. El Escorial revisited: Revised criteria for the diagnosis of amyotrophic lateral sclerosis. Amyotroph. Lateral Scler. Motor Neuron Disord. 2000, 1, 293–299. [Google Scholar] [CrossRef]
- Rooney, J.; Burke, T.; Vajda, A.; Heverin, M.; Hardiman, O. What does the ALSFRS-R really measure? A longitudinal and survival analysis of functional dimension subscores in amyotrophic lateral sclerosis. J. Neurol. Neurosurg. Psychiatry 2017, 88, 381–386. [Google Scholar] [CrossRef]
- Chernenkaya, V.Y.; Gorbachev, K.V.; Gorbachev, D.V.; Ataulina, A.I.; Fominykh, V.V.; Brylev, L.V.; Guekht, A.B. The Edinburgh Cognitive and Behavioral ALS Screen (ECAS): A Russian version. Zh. Nevrol. Psikhiatr. Im. S. S. Korsakova 2018, 118, 36–39. [Google Scholar] [CrossRef]
- Abrahams, S.; Newton, J.; Niven, E.; Foley, J.; Bak, T.H. Screening for cognition and behaviour changes in ALS. Amyotroph. Lateral Scler. Front. Degener. 2014, 15, 9–14. [Google Scholar] [CrossRef]
- Roman, A. Suggestions and Information about Speech Changes and Augmentative Alternative Communication (AAC). 2014. Available online: http://www.alsa.org/als-care/resources/publications-videos/factsheets/slurred-speech.html (accessed on 13 October 2019).
- Ashworth, N.L.; Satkunam, L.E.; Deforge, D. Treatment for spasticity in amyotrophic lateral sclerosis/motor neuron disease. Cochrane Database Syst. Rev. 2012, 15, CD004156. [Google Scholar] [CrossRef]
- Baker, F.; Wigram, T.; Gold, C. The effects of a song-singing programme on the affective speaking intonation of people with traumatic brain injury. Brain Inj. 2005, 19, 519–528. [Google Scholar] [CrossRef]
- Chiao, G.; Larson, C.; Yajima, Y.; Ko, P.; Kahrilas, P. Neuronal activity in nucleus ambiguus during deglutition and vocalization in conscious monkeys. Exp. Brain Res. 1994, 100, 29–38. [Google Scholar] [CrossRef] [PubMed]
- Cohen, N.S. The effect of singing instruction on the speech production of neurologically impaired persons. J. Music Ther. 1992, 29, 87–103. [Google Scholar] [CrossRef]
- Matsuo, K.; Palmer, J.B. Coordination of mastication, swallowing and breathing. Jpn. Dent. Sci. Rev. 2009, 45, 31–40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Palovcak, M.; Mancinelli, J.M.; Elman, L.B.; McCluskey, L. Diagnostic and therapeutic methods in the management of dysphagia in the ALS population: Issues in efficacy for the out-patient setting. NeuroRehabilitation 2007, 22, 417–423. [Google Scholar] [CrossRef] [PubMed]
- Rong, P.; Yunusova, Y.; Wang, J.; Zinman, L.; Pattee, G.L.; Berry, J.D.; Perry, B.; Green, J.R. Predicting speech intelligibility decline in amyotrophic lateral sclerosis based on the deterioration of individual speech subsystems. PLoS ONE 2016, 11, e0154971. [Google Scholar] [CrossRef]
- Haneishi, E. Effects of a music therapy voice protocol on speech intelligibility, vocal acoustic measures, and mood of individuals with Parkinson’s disease. J. Music Ther. 2001, 38, 273–290. [Google Scholar] [CrossRef] [Green Version]
- Tamplin, J.; Grocke, D. A music therapy treatment protocol for acquired dysarthria rehabilitation. Music Ther. Perspect. 2008, 26, 23–29. [Google Scholar] [CrossRef]
- Wiens, M.E.; Reimer, M.A.; Guyn, L.H. Music therapy as a treatment method for improving respiratory muscle strength in patients with advanced multiple sclerosis: A pilot study. Rehabil. Nurs. 1999, 24, 74–80. [Google Scholar] [CrossRef]
- Lyle, H. Vocal Yoga: The Joy of Breathing, Singing and Sounding; Bluecat Music and Publishing: Palisades, CA, USA, 2014. [Google Scholar]
- Ramig, L.A.; Titze, I.R.; Scherer, R.C.; Ringel, S.P. Acoustic analysis of voices of patients with neurologic disease: Rationale and preliminary data. Ann. Otol. Rhinol. Laryngol. 1988, 97, 164–172. [Google Scholar] [CrossRef]
- Peckham, A. The Contemporary Singer: Elements of Vocal Technique; Berklee Press Publications: Boston, MA, USA, 2010. [Google Scholar]
- McClosky, D.B. Your Voice at Its Best; Waveland Press Inc.: Long Grove, IL, USA, 2011. [Google Scholar]
- Welham, N.V.; Maclagan, M.A. Vocal fatigue: Current knowledge and future directions. J. Voice 2003, 17, 21–30. [Google Scholar] [CrossRef]
- Woo, A.S. Velopharyngeal dysfunction. Semin. Plast. Surg. 2012, 26, 170–177. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Walters, S.J.; Henriques-Cadby, I.B.D.A.; Bortolami, O.; Flight, L.; Hind, D.; Jacques, R.M.; Knox, C.; Nadin, B.; Rothwell, J.; Surtees, M.; et al. Recruitment and retention of participants in randomised controlled trials: A review of trials funded and published by the United Kingdom Health Technology Assessment Programme. BMJ Open 2017, 7, e015276. [Google Scholar] [CrossRef] [PubMed]
- Atassi, N.; Yerramilli-Rao, P.; Szymonifka, J.; Yu, H.; Kearney, M.; Grasso, D.; Deng, J.; Levine-Weinberg, M.; Shapiro, J.; Lee, A.; et al. Analysis of start-up, retention, and adherence in ALS clinical trials. Neurology 2013, 81, 1350–1355. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fernandez-Lazaro, C.I.; García-González, J.M.; Adams, D.P.; Fernandez-Lazaro, D.; Mielgo-Ayuso, J.; Caballero-Garcia, A.; Racionero, F.M.; Córdova, A.; Miron-Canelo, J.A. Adherence to treatment and related factors among patients with chronic conditions in primary care: A cross-sectional study. BMC Fam. Pr. 2019, 20, 132. [Google Scholar] [CrossRef]
- Shiovitz, T.M.; Bain, E.E.; McCann, D.J.; Skolnick, P.; Laughren, T.; Hanina, A.; Burch, D. Mitigating the effects of nonadherence in clinical trials. J. Clin. Pharmacol. 2016, 56, 1151–1164. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef] [Green Version]
- Riessman, C.K. Narrative Methods for the Human Sciences; Sage Publications Inc.: Thousand Oaks, CA, USA, 2008. [Google Scholar]
- Jensen, L.; Djurtoft, J.B.; Bech, R.D.; Nielsen, J.L.; Jørgensen, L.H.; Schrøder, H.D.; Frandsen, U.; Aagaard, P.; Hvid, L.G. Influence of resistance training on neuromuscular function and physical capacity in ALS patients. J. Neurodegener. Dis. 2017, 2017, 1436519. [Google Scholar] [CrossRef] [Green Version]
- Plowman, E.K.; Tabor, L.C.; Wymer, J.; Pattee, G. The evaluation of bulbar dysfunction in amyotrophic lateral sclerosis: Survey of clinical practice patterns in the United States. Amyotroph. Lateral Scler. Front. Degener. 2017, 18, 351–357. [Google Scholar] [CrossRef]
- Smith, R.; Pioro, E.; Myers, K.; Sirdofsky, M.; Goslin, K.; Meekins, G.; Yu, H.; Wymer, J.; Cudkowicz, M.; Macklin, E.A.; et al. Enhanced bulbar function in amyotrophic lateral sclerosis: The Nuedexta Treatment Trial. Neurotherapeutics 2017, 14, 762–772. [Google Scholar] [CrossRef] [Green Version]
- Pinto, S.; De Carvalho, M. The R of ALSFRS-R: Does it really mirror functional respiratory involvement in amyotrophic lateral sclerosis? Amyotroph. Lateral Scler. Front. Degener. 2015, 16, 120–123. [Google Scholar] [CrossRef]
- Gwathmey, K.G.; Berggren, K.N. Reflections on the implementation of the provisional best practices guidelines for the evaluation of bulbar dysfunction in ALS. Muscle Nerve 2019, 59, 531–536. [Google Scholar] [CrossRef] [PubMed]
- Andersen, P.M.; Borasio, G.D.; Dengler, R.; Hardiman, O.; Kollewe, K.; Leigh, P.N.; Pradat, P.-F.; Silani, V.; Tomik, B. EFNS task force on management of amyotrophic lateral sclerosis: Guidelines for diagnosing and clinical care of patients and relatives. An evidence-based review with good practice points. Eur. J. Neurol. 2005, 12, 921–938. [Google Scholar] [CrossRef] [PubMed]
- Beukelman, D.; Fager, S.; Nordness, A. Communication support for people with ALS. Neurol. Res. Int. 2011, 2011, 714693. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bowen, L.K.; Hands, G.L.; Pradhan, S.; Stepp, C.E. Effects of Parkinson’s disease on fundamental frequency variability in running speech. J. Med. Speech-Lang. Pathol. 2013, 21, 235–244. [Google Scholar]
- Brédart, A.; Marrel, A.; Abetz-Webb, L.; Lasch, K.; Acquadro, C. Interviewing to develop Patient-Reported Outcome (PRO) measures for clinical research: Eliciting patients’ experience. Health Qual. Life Outcomes 2014, 12, 15. [Google Scholar] [CrossRef] [Green Version]
- Czaplinski, A.; Yen, A.A.; Appel, S.H. Forced Vital Capacity (FVC) as an indicator of survival and disease progression in an ALS clinic population. J. Neurol. Neurosurg. Psychiatry 2005, 77, 390–392. [Google Scholar] [CrossRef] [Green Version]
- Donovan, N.J.; Kendall, D.L.; Young, M.E.; Rosenbek, J.C. The communicative effectiveness survey: Preliminary evidence of construct validity. Am. J. Speech-Lang. Pathol. 2008, 17, 335–347. [Google Scholar] [CrossRef]
- Lee, J.; Littlejohn, M.A.; Simmons, Z. Acoustic and tongue kinematic vowel space in speakers with and without dysarthria. Int. J. Speech-Lang. Pathol. 2017, 19, 195–205. [Google Scholar] [CrossRef]
- McCullough, G.H.; Kamarunas, E.; Mann, G.C.; Schmidley, J.W.; Robbins, J.A.; Crary, M.A. Effects of Mendelsohn maneuver on measures of swallowing duration post stroke. Top. Stroke Rehabil. 2012, 19, 234–243. [Google Scholar] [CrossRef] [Green Version]
- Mefferd, A.S.; Green, J.R.; Pattee, G. A novel fixed-target task to determine articulatory speed constraints in persons with amyotrophic lateral sclerosis. J. Commun. Disord. 2012, 45, 35–45. [Google Scholar] [CrossRef] [Green Version]
- Mendelsohn, M.S.; Mcconnel, F.M.S. Function in the pharyngoesophageal segment. Laryngoscope 1987, 97, 489. [Google Scholar] [CrossRef] [PubMed]
- Nishio, S.N.M. Changes over time in dysarthric patients with amyotrophic lateral sclerosis (ALS): A study of changes in speaking rate and maximum repetition rate (MRR). Clin. Linguist. Phon. 2000, 14, 485–497. [Google Scholar] [CrossRef]
- Pietkiewicz, I.; Smith, J.A. A practical guide to using interpretative phenomenological analysis in qualitative research psychology. Psychol. J. 2014, 20, 7–14. [Google Scholar]
- Pinto, S.; De Carvalho, M. Correlation between forced vital capacity and slow vital capacity for the assessment of respiratory involvement in amyotrophic lateral sclerosis: A prospective study. Amyotroph. Lateral Scler. Front. Degener. 2017, 18, 86–91. [Google Scholar] [CrossRef] [PubMed]
- Strand, E.A.; Buder, E.H.; Yorkston, K.M.; Ramig, L.O. Differential phonatory characteristics of four women with amyotrophic lateral sclerosis. J. Voice 1994, 8, 327–339. [Google Scholar] [CrossRef]
- Touré-Tillery, M.; Fishbach, A. How to measure motivation: A guide for the experimental social psychologist. Soc. Pers. Psychol. Compass 2014, 8, 328–341. [Google Scholar] [CrossRef]
- Yunusova, Y.; Green, J.R.; Wang, J.; Pattee, G.; Zinman, L. A protocol for comprehensive assessment of bulbar dysfunction in amyotrophic lateral sclerosis (ALS). J. Vis. Exp. 2011, 48, e2422. [Google Scholar] [CrossRef] [Green Version]
- Yunusova, Y.; Plowman, E.K.; Green, J.R.; Barnett, C.; Bede, P. Clinical measures of bulbar dysfunction in ALS. Front. Neurol. 2019, 10, 106. [Google Scholar] [CrossRef] [Green Version]
- Steele, C.M.; Peladeau-Pigeon, M.; Barbon, C.A.E.; Guida, B.T.; Namasivayam-MacDonald, A.; Nascimento, W.; Smaoui, S.; Tapson, M.S.; Valenzano, T.; Waito, A.A.; et al. Reference values for healthy swallowing across the range from thin to extremely thick liquids. J. Speech Lang. Hear. Res. 2019, 62, 1338–1363. [Google Scholar] [CrossRef] [Green Version]
- Rosenbek, J.C.; Robbins, J.A.; Roecker, E.B.; Coyle, J.L.; Wood, J.L. A penetration-aspiration scale. Dysphagia 1996, 11, 93–98. [Google Scholar] [CrossRef]
- Smirnova, N.S.; Khitrov, M.V. Phoneticheski predstavitelny tekst dlya fundamentalnykh i prikladnykh issle-dovanii russkoi rechi. Izvestiya vysshikh uchebnykh zavedenii. Priborostroenie 2013, 56, 5–10. [Google Scholar]
- Boersma, P.; van Heuven, V. Speak and unSpeak with PRAAT. Glot Int. 2001, 5, 341–347. [Google Scholar]
- Gadesmann, M.; Miller, N. Reliability of speech diadochokinetic test measurement. Int. J. Lang. Commun. Disord. 2008, 43, 41–54. [Google Scholar] [CrossRef]
- Pierce, J.E.; Cotton, S.; Perry, A. Alternating and sequential motion rates in older adults. Int. J. Lang. Commun. Disord. 2013, 48, 257–264. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, J.P.; Oliveira, C.; Lopes, C. Vocal acoustic analysis—Jitter, shimmer and HNR parameters. Procedia Technol. 2013, 9, 1112–1122. [Google Scholar] [CrossRef] [Green Version]
- Clark, I.N.; Baker, F.A.; Peiris, C.L.; Shoebridge, G.; Taylor, N. Participant-selected music and physical activity in older adults following cardiac rehabilitation: A randomized controlled trial. Clin. Rehabil. 2017, 31, 329–339. [Google Scholar] [CrossRef]
- Lim, H.A.; Miller, K.; Fabian, C. The effects of therapeutic instrumental music performance on endurance level, self-perceived fatigue level, and self-perceived exertion of inpatients in physical rehabilitation. J. Music Ther. 2011, 48, 124–148. [Google Scholar] [CrossRef]
- Thaut, M.H.; Abiru, M. Rhythmic auditory stimulation in rehabilitation of movement disorders: A review of current research. Music Percept. 2010, 27, 263–269. [Google Scholar] [CrossRef] [Green Version]
- Thaut, M.; McIntosh, G.; Rice, R. Rhythmic facilitation of gait training in hemiparetic stroke rehabilitation. J. Neurol. Sci. 1997, 151, 207–212. [Google Scholar] [CrossRef]
- Alter, D.A.; O’Sullivan, M.; Oh, P.I.; Redelmeier, D.A.; Marzolini, S.; Liu, R.; Forhan, M.; Silver, M.; Goodman, J.M.; Bartel, L.R. Synchronized personalized music audio-playlists to improve adherence to physical activity among patients participating in a structured exercise program: A proof-of-principle feasibility study. Sports Med. Open 2015, 1, 23. [Google Scholar] [CrossRef] [Green Version]
- Nelson, L.A.; Macdonald, M.; Stall, C.; Pazdan, R. Effects of interactive metronome therapy on cognitive functioning after blast-related brain injury: A randomized controlled pilot trial. Neuropsychology 2013, 27, 666–679. [Google Scholar] [CrossRef] [PubMed]
- Carrow, E.; Rivera, V.; Mauldin, M.; Shamblin, L. Deviant speech characteristics in Motor Neuron Disease. Arch. Otolaryngol. Head Neck Surg. 1974, 100, 212–218. [Google Scholar] [CrossRef] [PubMed]
- Eshghi, M.; Richburg, B.; Yunusova, Y.; Green, J.R. Instrumental evaluation of velopharyngeal dysfunction in amyotrophic lateral sclerosis. Age 2019, 1000, 62. [Google Scholar]
- Waito, A.A. Swallowing Physiology and Impairment in Individuals with Amyotrophic Lateral Sclerosis (ALS). Ph.D. Thesis, Rehabilitation Sciences Institute, University of Toronto, Toronto, ON, Canada, 2019. [Google Scholar]
- Bradt, J. Randomized controlled trials in music therapy: Guidelines for design and implementation. J. Music Ther. 2012, 49, 120–149. [Google Scholar] [CrossRef]
- Chio, A.; Gauthier, A.; Montuschi, A.; Calvo, A.; Di Vito, N.; Ghiglione, P.; Mutani, R. A cross sectional study on determinants of quality of life in ALS. J. Neurol. Neurosurg. Psychiatry 2004, 75, 1597–1601. [Google Scholar] [CrossRef]
- Yunusova, Y.; Graham, N.L.; Shellikeri, S.; Phuong, K.; Kulkarni, M.; Rochon, E.; Tang-Wai, D.F.; Chow, T.W.; Black, S.E.; Zinman, L.H.; et al. Profiling speech and pausing in amyotrophic lateral sclerosis (ALS) and frontotemporal dementia (FTD). PLoS ONE 2016, 11, e0147573. [Google Scholar] [CrossRef] [Green Version]
| I. Session Opening and Assessment |
| Time (approximately): 5 min. Therapy objective: Assessment. Materials and equipment: NRS (respiration) and NRS (voice) sheets; NRS data sheet; notebook for note taking. Two sturdy chairs situated facing each other, approximately 1.5 m apart. Optional: wheelchair, small table, pillow for participant’s comfort. Procedure: Music therapist (MT) and participant exchange salutations. MT assesses participant’s physical and emotional state through observation and conversation, and re-establishes rapport through a brief conversation to ensure psychological comfort of the participant entering the session. The following information is recorded: (1) NRS for current perceived ease of respiration, (2) NRS for current perceived ease of voice production, (3) information about adherence to the assigned independent exercises routine: frequency, duration, difficulties, comments (starting at session 4). Participant is reminded that he/she is going to be guided through all the exercises and is welcome to participate to his/her comfort, to ask clarifying questions and make comments, to stop doing an exercise at any point if he/she feels uncomfortable or tired, and to pause, rest and hydrate as needed. |
| II. Body Alignment Exercise |
| Time (approximately): 3 min. Therapy objective: To learn proper body alignment and its role in respiration, voice production and swallowing. Materials and equipment: Visual aids for anatomy of singing. Procedure: II.1. Body awareness. Participant is encouraged to become aware of the physical sensation of his/her body, to pay close attention to any muscle tension, strain or stiffness and to gently move, stretch or self-massage to release those. II.2. Body alignment Participant is encouraged to become aware of his/her body alignment and to find a good sitting posture by maintaining the spinal alignment from the hips up. Suggested steps to achieve this are: a. Both feet are on the ground, shoulder-width apart, forming a 90-degree angle with the thighs; b. The pelvis is adjusted so there is slightly less curve in the lower back, and the spine feels extended both upwards and downwards; c. The rib cage is now more upward and “open” (not collapsed); d. The shoulders are suspended exactly over the rib cage (rather than pulled back or rolled forward); e. The head is balanced at the top of the spine and feels almost weightless, with the front half of the skull is balanced in front of atlanto-occipital joint, and its hind half is balanced behind atlanto-occipital joint; f. The upper body is poised and aligned, yet flexible and ready to move: the images of the whole body as a marionette suspended by a rope extending from the top of the skull, or of the head as a water lily flower resting on water surface may be helpful; g. To check for proper spinal alignment: stretch arms above the head and bend them down so that fingertips of one hand touch the elbow of the opposite arm; sustain this position for several seconds, then let the arms drop down gently to the sides of the body, but keep the posture. The anatomy and physiology of respiration, voice production and swallowing are briefly explained to the patient during these and following exercises in order to increase the patient’s awareness and sense of control over these processes. |
| III. Diaphragmatic Breathing Exercises |
| Time (approximately): 4 min. Therapy objective: To become aware of diaphragmatic action, its role in respiration and benefits of diaphragmatic breathing. Materials and equipment: Visual aids for anatomy of singing. Procedure: III.1. Silent long diaphragmatic breathing (5–10 repetitions) Participant is instructed to breathe in through the nose, with the mouth slightly open, then breathe out through the mouth, without sound. Air enters and escapes from the lungs with no effort: it is not forced in any way, and no rib action should occur. Participant is encouraged to place one hand on his/her abdomen and the other on his/her chest as he/she practices diaphragmatic breathing. The front and the side of the abdominal wall expand as the diaphragm contracts and pulls down during breath in, while no visible movement of the chest or shoulders occurs. III.2. Audible diaphragmatic breathing on [s] sound (3 repetitions) Participant is instructed to breathe in through the nose, with the mouth slightly open, then breathe out through the mouth making a continuous [s]sound until he/she runs out of air. The sound should not be forced, and no rib action should occur. III.3. Silent long diaphragmatic breathing (3 repetitions)—see III.1. III.4. Diaphragmatic breathing with audible sigh (3 repetitions) Participant is instructed to breathe in through the nose, with the mouth slightly open, then breathe out through the mouth making an audible, very breathy sigh on a vowel sound (for example, ‘a’). The sound should not be forced, the throat should be relaxed, and no rib action should occur. Note: No background music or music accompaniment will be used, as this will allow the participants to fully concentrate on the physical sensation of diaphragmatic breathing. During the first several sessions, the participant may experience a slightly uncomfortable pulling sensation around the posterior abdomen wall: this sensation is due to this group of muscles being more intensively worked than usual and will subside. When it becomes habitual, diaphragmatic breathing may reduce the effort necessary for breathing. |
| IV. Controlled Breathing and Lip Seal Exercise |
| Time (approximately): 3 min. Therapy objective: To practice controlled breathing in order to create sustained airflow necessary for speech; to improve oxygen and carbon dioxide exchange; to maintain lip seal (necessary for swallowing and for decreasing salivation). Materials and equipment: 37-key melodica; individual tube mouthpiece; metronome (Android smartphone, Metronome Beats application for Android, Kinivo ZX120 Mini Portable Wired Speaker for amplification). Optional: a small (approx. 15 cm × 15 cm) piece of lightweight fabric. Procedure: IV.1. Pursed lip breathing (3 repetitions) Participant is instructed to take a diaphragmatic breath in through the nose and to breathe out very slowly through pursed lips (“as if blowing on a fire”). A piece of lightweight fabric held by MT in front of the participant can be used for visual feedback. IV.2. Controlled breathing and lip seal exercise Participant is instructed to blow into the tube mouthpiece of the melodica while MT plays on the keys of the melodica the first 16 measures from “Old French Song” from “Children’s Album” (Op.39, No.16) by Tchaikovsky, at 60 bpm, with accompanying audible metronome click. Participant is advised to breathe in through the nose as necessary between the phrases, MT may provide conducting cues for inhale as necessary. The tempo is adjusted as needed (decreased for a longer exhale) to match participants’ ability. 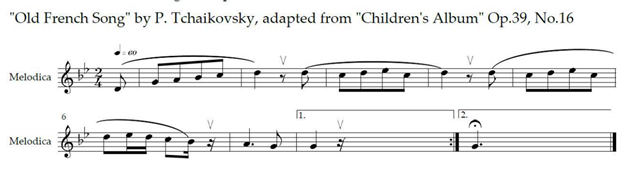 |
| V. Music-Assisted Relaxation for Voice Production |
| Time (approximately): 8 min. Therapy objective: To elicit the relaxation response through music-assisted visualisation technique (V.1) and to relax and stretch the muscles involved in voice production (V.2–V.8). Materials and equipment: Android smartphone; default music player for Android; Spotify application for Android (with subscription); Kinivo ZX120 Mini Portable Wired Speaker for amplification). Optional: lotion or oil for massage; Purell for hand disinfection (if MT touches participant’s face). Procedure: Participant is reminded to maintain the aligned sitting posture, and to be gentle rather than forceful in releasing muscle tension. V.1. Music-assisted visualisation and relaxation (about 4 min) The recorded relaxing music is started in the background at the level allowing for a live narrative to be clearly heard. Maintaining the aligned sitting body position, participant is advised to close the eyes and to breathe deeply, as he/she is led by MT through a brief (about 3 min) music-assisted visualisation for relaxation. At the end of the exercise, as the background music continues, participant is invited to gently open his/her eyes, first looking downwards and then gradually orienting him/herself to the surroundings. The background music continues through the rest of the exercise sets. V.2. The head and the neck muscles relaxation (2 repetitions) Maintaining the body alignment, participant is advised to let his/her head slowly fall forward under its weight, to feel the stretch on the spine, and then to bring the head back to the balanced position at the top of the spine. Participant may also sway the head gently side to side during this exercise, if it feels appropriate. V.3. The facial muscles relaxation Participant is advised to rub his/her hands together or to warm them otherwise and to place the palms over closed eyes for several seconds, then to gently massage the face with circular motions of the pads of the fingers, using both hands, moving from hairline downwards to cheeks, lips and chin, spending more time on areas that feel tight. When the cheeks are being massaged, participant is advised to let his/ her jaw to hang slack. Face massage may be performed by MT or a care provider if the patient’s hand function is impaired. V.5. The tongue muscles relaxation and stretch (3 repetitions) Participant is encouraged to let the tongue relax and fall forward slightly out of the mouth by releasing its muscles, then to gently stretch the tongue out of the mouth down toward the chin, and to release again allowing the tongue to rest on the lower lip. Participant is further advised to pull the tongue back into the mouth as far as possible, hold for a few seconds, and release. V.6. The mandible (jaw) relaxation and stretch Participant is assisted in finding his/her temporomandibular joints. With the fingers placed over the joints, the patient allows the jaw to drop without resistance. Participant is encouraged to take his/her jaw between the thumb and forefinger and to gently move the jaw up and down, at first slowly, then faster. The movement will be unrestricted if the jaw is relaxed. Participant is then advised to move the jaw as far forward as possible, hold, then release; then to move the jaw as far back and upwards as possible (chin tuck), hold, then release. This stretch may be repeated 2 or 3 times. V.7. The suprahyoid muscles relaxation Participant is assisted in finding his/her suprahyoid (digastric and mylohyoid) muscles under his/her chin (the muscles responsible for elevating the larynx during swallowing). Participant is advised to gently massage these muscles with his/her thumbs in slow, “kneading” motions, pushing vertically up and releasing down. V.8. The infrahyoid (strap) muscles relaxation Participant is assisted in finding his/her larynx by placing fingers flat against the front of his/ her neck and swallowing, thumb and forefinger of one hand are used to gently move the larynx side to side several times. |
| VI. “Ping Pong” Soft Palate Exercise |
| Time (approximately): 1 min. Therapy objective: To tonicise the soft palate muscles involved in velopharyngeal function and to practice the proper soft palate position for phonation. Materials and equipment: None. Procedure: Participant is instructed to “yawn politely” (half yawn) in order to find the proper position for relaxed sound production [95]. It may be helpful to imagine there is a ping pong ball in the back of the mouth and to hold this position for several seconds. Repeat 5 times. |
| VII. Phonation Exercises |
| Time (approximately): 5 min. Therapy objective: To facilitate proper engagement of arytenoid cartilages and vocal folds (VII.1–VII.3), to increase the speech rate (VII.3). Materials and equipment: Visual aids for anatomy of singing. Procedure: VII.1. “Hah” sigh exercise (2 repetitions) Participant is instructed to take a breath, to expel about half of it, then to add a light, “lazy” sigh (“hah”), starting in the voice midrange and inflecting downwards. The tongue rests in the limp position, the jaw is relaxed.  VII.2. Interrupted “hah” sigh exercise (2 repetitions) Participant is instructed to repeat the previous exercise, allowing the lips to close and open several times at the beginning of the sigh, resulting in a light humming sound (“hah-mah-mah-mah-mah”). The lips are not pressed firmly together like in the regular [m] sound. The tongue rests in the limp position, the jaw is relaxed.  VII.3. Voiced consonant sigh exercise (2 repetitions for each consonant) Maintaining relaxation of facial and laryngeal muscles, participant is instructed to take a diaphragmatic breath, then to expel the air while making a continuous consonant sound, starting in the voice midrange and inflecting downwards. An accompanying short vowel sound has to be added to the stop consonants (‘b’, ‘d’, ‘g’), e.g., “ba-ba-ba-ba-ba”. The sound should not be forced. The jaw and tongue are relaxed. The sequence of the consonants for this exercise is: /v/, /z/, /z</, /l/, rolled /r/, /j/, /b/, /d/, /m/, /n/, /g/. Rolled /r/ may present a challenge for some people. This is not related to ALS and should not discourage the patient from attempting this exercise. |
| VIII. Consonant Range Cantillation Exercise |
| Time (approximately): 2 min. Therapy objective: To facilitate tongue movement ease and speed, to improve velopharyngeal function, to prevent (reduce) hypernasality. Materials and equipment: None. Procedure: Participant is instructed to take a diaphragmatic breath and say “mah-nah-ng-ah” in cantillation once, then proceed saying “mah-nah-ng-ah” 3 times on one exhalation, next—saying it 6 times on one exhalation, then 9 times on one exhalation, and, finally, 12 times on one exhalation. Participant is encouraged to maintain and note the freedom of tongue and jaw movement as he/she does this exercise. Note: The sequence of tongue movements required for this exercise involves fast progression from the resting position (/m/) to hard palate (/n/), to soft palate (/g/) [93]. Besides facilitating tongue movement ease and speed, this exercise has the potential to improve velopharyngeal function and, thus, to prevent (reduce) hypernasality, which also contributes to speech intelligibility [85]. |
| IX. Velopharyngeal Port Exercise |
| Time (approximately): 3 min. Therapy objective: To improve velopharyngeal function, to prevent hypernasality. Materials and equipment: Visual aids for anatomy of singing. Acoustic guitar; metronome (Android smartphone, Metronome Beats application for Android, Kinivo ZX120 Mini Portable Wired Speaker for amplification). Procedure: Starting in the lower midrange of his/her voice, participant is instructed to sing the syllables “hun-ga” three times as a scale from sol to do. “Hun” corresponds with the offbeat, and “ga” falls on the beat. The exercise is then modulated gradually up by semitones, until it reaches the limit of the participant’s comfortable range. After that, it is modulated down by semitones until it is three semitones below the starting key. The therapist models the exercise and provides the guitar accompaniment, and sings together with the participant. The patient is encouraged to notice the switching between nasal (“hun”) and non-nasal sound (“ga”). Audible metronome click is setup. The tempo of the accompaniment can be adjusted to the ability of the patient. Gradual increase to up to 90 bpm is advisable in later sessions.  |
| X. Impulse Diaphragmatic Breathing Exercises |
| Time (approximately): 2 min. Therapy objective: To increase the efficiency and speed of relaxed diaphragmatic inhalation. Materials and equipment: Acoustic guitar; metronome (Android smartphone, Metronome Beats application for Android, Kinivo ZX120 Mini Portable Wired Speaker for amplification). Procedure: X.1. Impulse breathing with short “hah” exhale (2 repetitions) The exercise starts with participant listening to 8 beats of audible metronome click initially set at 4/4, 64 bpm. Participant is instructed to fully relax abdominal muscles, letting air effortlessly enter the lungs, then to abruptly expel the air with a short, though deep and strong (“barking”) “hah” sound and to immediately let the abdominal muscles relax again, letting air into the lungs. Suggested sequence: (1) listen and rest for 8 beats, (2) 8 ”hah” utterances for 8 beats, (3) listen and rest for 8 beats, (4) 8 ”hah” utterances for 8 beats, (5) stop. The tempo should be slightly faster than the tempo most comfortable for the participant and may be increased gradually in subsequent sessions if the patient is ready. X.2. Impulse breathing with sustained “hah” exhales (4 repetitions) As in the previous exercise, participant is advised to fully relax the abdominal muscles, letting air effortlessly enter the lungs. Then, the air is expelled 3 times following the pattern: “hah-hah-haaaaaaaah” (short-short-long), where /a/ vowel is very open, strong and deep, but is not forced. After each syllable, the abdominal muscles should relax again, letting air into the lungs. |
| XI. Sustained Vowels Production Exercises |
| Time (approximately): 5 min. Therapy objective: To practice full diaphragmatic breathing and healthy vocal folds coordination for sustained, supported vowel production. Materials and equipment: Acoustic guitar; metronome (Android smartphone, Metronome Beats application for Android, Kinivo ZX120 Mini Portable Wired Speaker for amplification). Procedure: XI.1. Vowel shaping exercise (3 repetitions) With the mouth fully closed, participant is instructed to silently form vowel shapes in the following sequence: /a/, /e/, /i/, /o/, /u/, paying attention to position changes in tongue and facial muscles. MT model the vowels (with sound). XI.2. “Hah-meh-mee-moh-moo” sigh exercise (3 repetitions) Similar to exercise VII.3, participant is encouraged to take a breath, then expel it on a light, “lazy” sigh, starting in the voice midrange and inflecting downwards. During this exhale, participant forms the vowel shapes /a/, /e/, /i/, /o/, /u/ in a relaxed manner and allows the lips to close and open several times, resulting in light humming sound: “hah-meh-mee-moh-moo”. The lips are not pressed firmly together like in the regular [m] sound, and the jaw is relaxed.  XI.3 “Hah-eh-ee-oh-oo” sigh exercise (3 repetitions) The instructions for this exercise are the same as for the exercise IX.2., but the lip movement resulting in the light /m/ sound is now omitted: “hah-eh-hee-oh-oo”.  XI.4. Sustained vowels exercise (2 repetitions, if well tolerated) Comfortable tone from participant’s midrange is chosen for the exercise and becomes the tonal center (do). The patient sustains do for four measures (2/4, 90 bpm) on “mah” syllable, then rests for 2 measures. The next syllable (“meh”) is then sustained is a similar manner, then “mee”, “moh” and “moo”. The therapist provides the guitar accompaniment, and sings together with the participant. Accompanying audible metronome is setup at 2/4, 90 bpm. The tempo is adjusted as needed (decreased for a longer exhale) to match participants’ ability. The exercise may be performed twice, if well tolerated. 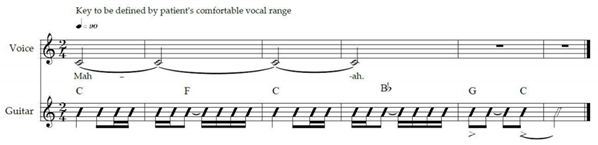 Note: In case of excessive perceived nasality, participant may be advised to “adopt a pleasant facial expression”, slightly lifting the zygomatic muscles (“lifting the cheeks”). |
| XII. Laryngeal Elevation through Vocalisation (Gliding Vowels) Exercise |
| Time (approximately): 5 min Therapy objective: To facilitate sustained laryngeal elevation. Materials and equipment: Acoustic guitar; metronome (Android smartphone, Metronome Beats application for Android, Kinivo ZX120 Mini Portable Wired Speaker for amplification). Procedure: MT models the exercise and sings together with the participant. A comfortable tone from the participant’s midrange is chosen for the exercise. Starting from this tone on “mah” syllable, participant is instructed to slide up a major third interval by beat 4 (the second dotted quarter) of the measure and to sustain this tone until the end of the measure. This singing pattern is repeated for 3 more measures, as the harmony changes. Then, 4 measures on “mee” and then 4 measures on “moo” follow. If well tolerated, the whole exercise may be repeated once and a major third interval may be increased to a perfect fifth for increased laryngeal elevation. Live guitar accompaniment is provided by MT, in 12/8, 130 bpm, one harmony per measure, with accompanying audible metronome click. Repeat 2 times if well tolerated.  |
| XIII. Vocal Cord Relaxation Exercises |
| Time (approximately): 2 min. Therapy objective: To relax vocal cords following the singing exercises. Materials and equipment: None. Procedure: Participant is instructed to use diaphragmatic or mixed types of breathing during these relaxation exercises. XIII.1. Vocal fry exercise Participant is instructed to take a deep breath and to make a vocal fry sound for the duration of the exhale. Can be repeated. XIII.2. Deep breathing (3 repetitions) Participant is instructed to breathe in through the nose, with the mouth slightly open, then breathe out through the mouth, without sound. Air enters and escapes from the lungs with no effort: it is not forced in any way. Participant can choose to use diaphragmatic or mixed (diaphragmatic and chest) types of breathing. XIII.3. Exhale on hard [h] (3 repetitions) Participant is instructed to continue deep breathing and then to exhale on a “lazy”, long, uninterrupted hard [h] sound. |
| XIV. Preferred Song Performance |
| Time (approximately): 5 min. Therapy objective: To relax vocal cords following the singing exercises. To reinforce all the voice skills practiced in previous exercises (body alignment and posture, diaphragmatic breathing, proper phonation, soft palate elevation, relaxed consonant articulation, etc.), to provide a motivating reward at the end of the session. Materials and equipment: Acoustic guitar. Optional: song lyrics printout. Procedure: Participant is invited to sing his/her preferred song in a comfortable range, at a comfortable tempo, with live guitar accompaniment provided by MT. MT may choose to sing together with participant to encourage participation and to model healthy singing technique. Both the participant and the MT provide brief feedback on the performance at the end of the song. Selection of the song for this exercise will occur as follows. At recruitment, each participant will be asked to provide the list of his/her 3 to 5 favourite songs to sing. MT will choose one of these songs to include into the protocol, giving preference to songs with simple melodic and harmonic structure, enough pauses for proper phrasing, moderate tempo, and emotionally neutral or “positive”. |
| XV. Session Closure and Assessment |
| Time (approximately): 5 min. Therapy objective: Assessment. Materials and equipment: NRS (respiration) and NRS (voice) sheets; NRS data sheet; notebook for note taking. Procedure: MT closes the session, acknowledges participant’s effort and reminds of the upcoming session(s) if any are left. The following information is gathered and recorded into the patient’s individual data sheet: (1) VAS for current perceived ease of respiration, and (2) VAS for current perceived ease of voice production. MT instructs (or reminds) the participant to practice recommended daily exercises, if possible, always taking precautions to avoid strain and exhaustion (to “stop if something doesn’t feel right”). MT instructs (or reminds) the participant to follow the voice health guidelines [79]. |
| Outcome Measure | Outcome Measure Description | Data Collection Points |
|---|---|---|
| FEASIBILITY OUTCOME MEASURES | ||
| Recruitment | All newly diagnosed patients at ALS Moscow Centre living within the Moscow city limits and meeting the inclusion and exclusion criteria were invited to participate, until the desired sample size (n = 8) was achieved or the cut-off recruitment date. Target recruitment over 80% was considered the marker of a successful feasibility trial. | Prior to the cut-off recruitment date |
| Retention | The total number of participants recruited was compared with the total number of participants who completed this study. A retention rate over 70% at the end of follow-up period was considered the marker of a successful feasibility trial. | Week 1, week 16 |
| Adherence | The number of music therapy sessions attended by each participant was recorded as an adherence measure for this study. Mean adherence across all participants who completed this study was calculated. Mean adherence for the group calculated at over 75% music therapy sessions delivered was considered the marker of a successful feasibility trial. | Each music therapy session (total of 12), throughout the therapy phase (weeks 6–12) |
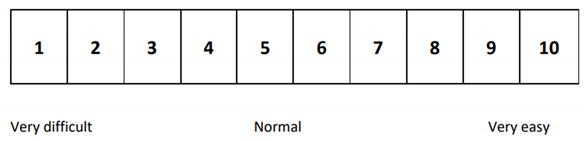
| Tolerance | Short-term tolerability of the music therapy treatment protocol was assessed by measuring change in ratings on the self-reported Ease of Respiration Numeric Rating Scale and change in ratings on the self-reported Ease of Speech Numeric Rating Scale before and after every music therapy session. The outcome could range from “1” (very difficult) to “10” (very easy). Recorded by the music therapist. | Before and after each music therapy session (total of 12), throughout the therapy phase (weeks 6–12) |
| Self-motivation | Self-reported adherence to a suggested independent exercise routine was recorded to assess levels of self-motivation that participants demonstrated with regard to music therapy treatment. Any attempt to practice was recorded. The number of independent exercises sets performed, in proportion to the number of days when no visit from the music therapist was scheduled, recorded during the sessions from 4 to 12 during the 6 week treatment phase, was calculated, measured in percent. | Each music therapy session starting at session 4 (total of 9), throughout the therapy phase (weeks 7–12) |
| Treatment experience of participants—persons with ALS | Semi-structured interviews with research participants—persons with ALS—were conducted pre-treatment (week 5) and at the end of the follow-up period (week 16). Participant’s answers to open questions in regard to expectations for and impressions of music therapy treatment were written down during a home visit by a trained research assistant. Interpretative phenomenological analysis was applied to find prominent common themes across the semi-structured interviews. | Week 5, week 16 |
| Caregiver’s experience | Semi-structured interviews with caregivers were conducted prior to treatment (week 5) and at the end of the follow-up period (week 16). Primary caregivers, if identified by participants—persons with ALS—and only with their permission, were approached for the interviews. Caregivers’ answers to open questions in regard to expectations for and impressions of music therapy treatment were written down during a home visit by a trained research assistant. Interpretative phenomenological analysis was applied to find prominent common themes across the semi-structured interviews. | Week 5, week 16 |
| Music therapist’s perspective | Individual treatment notes taken after each session and generalised “field notes” taken twice a week, after completion of each consequent session by all the participants, were submitted by the music therapist. Thematic narrative analysis of the notes was conducted. | Each music therapy session (total of 12), throughout the therapy phase (weeks 7–12) |
| BIOMEDICAL OUTCOME MEASURES | ||
| Outcome measures to assess the long-term changes in respiration | ||
| Change of Forced Vital Capacity (FVC) from baseline at Week 6, week 12, week 16 | Forced Vital Capacity (FVC) is a standard spirometry test which measures the volume of air that can forcibly be blown out after full inspiration; measured in %. Measured during a home visit by a nurse. | Week 1, week 6, week 12, week 16 |
| Change of Maximal Inspiratory Pressure (MIP) from baseline at week 6, week 12, week 16 | Maximal Inspiratory Pressure (MIP) is the inspiratory pressure generated against a completely occluded airway; used to evaluate inspiratory respiratory muscle strength; measured in cm H2O. Measured during a home visit by a nurse. | Week 1, week 6, week 12, week 16 |
| Change of Maximal Expiratory Pressure (MEP) from baseline at week 6, week 12, week 16 | Maximal Expiratory Pressure (MEP) is a measure of the strength of respiratory muscles, obtained by having the patient exhale as strongly as possible against a mouthpiece; measured in cm H2O. Measured during a home visit by a nurse. | Week 1, week 6, week 12, week 16 |
| Outcome measures to assess the long-term changes in cough | ||
| Change of Peak Expiratory Flow (PEF) from baseline at week 6, week 12, week 16 | Peak Expiratory Flow (PEF) is a measure of cough effectiveness, portable peak flow meter was used; measured in %. Measured during a home visit by a nurse. | Week 1, week 6, week 12, week 16 |
| Outcome measures to assess the long-term changes in speech | ||
| The Change of Center for Neurologic Study Bulbar Function Scale (CNS-BFS) Speech subscore from baseline at week 6, week 12, week 16 | The Center for Neurologic Study Bulbar Function Scale (CNS-BFS) consists of three domains (swallowing, speech, and salivation), each of which is assessed with a 7-item, self-report questionnaire. Each question is scored from “1” (does not apply) to “5” (applies most of the time). Speech domain subscore can range from “7” (best outcome) to “35” (worst outcome). The result was recorded during a home visit by a trained research assistant. | Week 1, week 6, week 12, week 16 |
| Change in acoustic assessment parameters of recorded voice from baseline at week 6, week 12, week 16 | Voice samples were recorded during a home visit by a trained research assistant digitally in .wav format, using a Shure WH20XLR Dynamic Headset Microphone, Alesis iO Dock audio interface, Apple iPad 2 tablet and GarageBand software. Acoustic analysis of the voice samples was conducted using the PRAAT linguistic computer program to calculate the following outcome measures: Maximum Phonation Time (MPT), sound /a/, measured in seconds; Maximum Repetition Rate—Alternating (AMR), /pataka/ sequence, measured in total number of syllables uttered as fast and as clear as possible on one breath; Maximum Repetition Rate—Sequential (SMR), /ba/ syllable, measured in total number of syllables uttered as fast and as clear as possible on one breath; Jitter, local, sound /a/, measured in percent, Shimmer, local, sound /a/, measured in percent; Harmonics-to-Noise Ratio (HNR), measured in Db, sustained /a/; Vowel Space Area (VSA), separate vowels /a, e, i, o, u/, measured in squared Hz; Fundamental frequency (F0), oral reading, measured in Hz; Speaking rate, oral reading, measured in words per minute; Speech–pause ratio, oral reading, measured in seconds per minute; Pause frequency, oral reading, measured in number of pauses per minute; Fundamental frequency (F0), spontaneous speech, measured in Hz; Speaking rate, spontaneous speech, measured in words per minute; Speech–pause ratio, spontaneous speech, measured in seconds per minute; Pause frequency spontaneous speech, measured in number of pauses per minute. | Week 1, week 6, week 12, week 16 |
| Change in perceptual assessment parameters of recorded voice from baseline at week 6, week 12, week 16 | Voice samples were recorded during a home visit by a trained research assistant digitally in .wav format, using a Shure WH20XLR Dynamic Headset Microphone, Alesis iO Dock audio interface, Apple iPad 2 tablet and GarageBand software. Perceptual analysis of the voice samples was performed by three qualified speech-language specialists to assess change in hypernasality level of spontaneous speech, measured in points. Inter-rater reliability was calculated for the perceptual analysis results. | Week 1, week 6, week 12, week 16 |
| Outcome measures to assess the long-term changes in swallowing | ||
| The Change of Center for Neurologic Study Bulbar Function Scale (CNS-BFS) Swallowing subscore from baseline at week 6, week 12, week 16 | The Center for Neurologic Study Bulbar Function Scale (CNS-BFS) consists of three domains (swallowing, speech, and salivation), each of which is assessed with a 7-item, self-report questionnaire. Each question is scored from “1” (does not apply) to “5” (applies most of the time). Swallowing domain subscore can range from “7” (best outcome) to “35” (worst outcome). The result was recorded during a home visit by a trained research assistant. | Week 1, week 6, week 12, week 16 |
| Change in videofluoroscopic swallowing study (VFSS) results from baseline at week 6, week 12 | VFSS (videofluoroscopic swallowing study), an X-ray-based method of evaluating a person’s swallowing ability, was performed by a trained specialist during a visit to a laboratory using a BV Pulsera Mobile C-arm fluoroscope, pulsing at 30 pulses per second and recorded on built-in Medical DVD Recorder at 30 frames per second. Each participant swallows 10 mL of nectar and pudding-thick liquid boluses, thickened with a xanthan gum-based thickener (i.e., Nestle Thicken-Up Clear®) and mixed to 40% weight-to-volume concentration with BarVIPS powder. VFSS video clips were reviewed and scored by a trained speech-language pathologist, using frame-by-frame analysis following operational definitions outlined by [124]. The following outcome parameters were calculated from VFSS video clips, recorded at three time points, to assess long-term changes in swallowing: Time-to-Laryngeal Vestibule Closure, nectar 10 mL, measured in ms; Time-to-Laryngeal Vestibule Closure, pudding 10 mL, measured in ms; Maximum Pharyngeal Constriction Area, nectar 10 mL, measured in % C2–42; Maximum Pharyngeal Constriction Area, pudding 10 mL, measured in % C2–42; Peak Position of the Hyoid Bone, nectar 10 mL, measured in % C2–4, Peak Position of the Hyoid Bone, pudding 10 mL, measured in % C2–4; Penetration–Aspiration Scale Score (worst), nectar 10 mL, measured in points; Penetration–Aspiration Scale Score (worst), pudding 10 mL, measured in points; Total Pharyngeal Residue C24 area, nectar 10 mL, measured in % C2–4; Total Pharyngeal Residue C24 area, pudding 10 mL, measured in % C2–4; Laryngeal vestibule closure, nectar 10 mL, described as complete, partial, or incomplete; Laryngeal vestibule closure, pudding 10 mL, described as complete, partial, or incomplete. | Week 1, week 6, week 12 |
| Participant | FVC_t1 | FVC_t2 | FVC_t3 | FVC_t4 |
|---|---|---|---|---|
| 1 | 76 | 75 | 89 | 80 |
| 2 | 69 | 83 | 85 | 79 |
| 3 | 121 | 115 | 113 | 113 |
| 4 | 87 | 83 | 88 | 72 |
| 5 | 63 | 60 | 61 | 63 |
| 6 | 82 | 73 | 60 | 64 |
| 7 | 84 | 63 | 62 | 83 |
| Mean | 83.143 | 78.857 | 79.714 | 79.143 |
| Participant | MIP_t1 | MIP_t2 | MIP_t3 | MIP_t4 |
|---|---|---|---|---|
| 1 | 73 | 69 | 91 | 98 |
| 2 | 44 | 26 | 57 | 81 |
| 3 | 41 | 38 | 41 | 42 |
| 4 | 55 | 62 | 49 | 54 |
| 5 | 32 | 39 | 33 | 42 |
| 6 | 70 | 56 | 60 | 58 |
| 7 | 48 | 40 | 57 | 51 |
| Mean | 51.857 | 47.143 | 55.429 | 60.857 |
| Participant | MEP_tp1 | MEP_tp2 | MEP_tp3 | MEP_tp4 |
|---|---|---|---|---|
| 1 | 68 | 65 | 94 | 79 |
| 2 | 63 | 76 | 83 | 87 |
| 3 | 67 | 81 | 80 | 77 |
| 4 | 91 | 86 | 103 | 91 |
| 5 | 35 | 47 | 35 | 34 |
| 6 | 79 | 59 | 57 | 54 |
| 7 | 55 | 35 | 50 | 51 |
| Mean | 65.429 | 64.143 | 71.714 | 67.571 |
| Participant | PCF_t1 | PCF_t2 | PCF_t3 | PCF_t4 |
|---|---|---|---|---|
| 1 | 30 | 22 | 36 | 82 |
| 2 | 120 | 103 | 121 | 128 |
| 3 | 99 | 106 | 107 | 127 |
| 4 | 109 | 94 | 100 | 93 |
| 5 | 66 | 50 | 69 | 66 |
| 6 | 68 | 68 | 75 | 75 |
| 7 | 64 | 75 | 80 | 80 |
| Mean | 79.429 | 74.000 | 84.000 | 93.000 |
| Participant | CNSBFSsp_t1 | CNSBFSsp_t2 | CNSBFSsp_t3 | CNSBFSsp_t4 |
|---|---|---|---|---|
| 1 | 18 | 16 | 14 | 14 |
| 2 | 8 | 13 | 8 | 10 |
| 3 | 8 | 10 | 10 | 9 |
| 4 | 8 | 7 | 10 | 9 |
| 5 | 24 | 27 | 24 | 29 |
| 6 | 12 | 13 | 15 | 16 |
| 7 | 10 | 9 | 9 | 9 |
| Mean | 12.571 | 13.571 | 12.857 | 13.714 |
| Participant | MPT_t1 | MPT_t2 | MPT_t3 | MPT_t4 |
|---|---|---|---|---|
| 1 | 15.96 | 4.66 | 12.23 | 6.95 |
| 2 | 19.66 | 4.62 | 13.46 | 8.14 |
| 3 | 8.52 | 7.13 | 6.25 | 8.13 |
| 4 | 11.84 | 15.7 | 14.48 | 11.51 |
| 5 | 6.68 | 8.48 | 9.26 | 9.48 |
| 6 | 17.1 | 15.3 | 22.37 | 18.04 |
| 7 | 3.61 | 4.34 | 7.4 | 3.71 |
| Mean | 11.910 | 8.604 | 12.207 | 9.423 |
| Participant | Jitter_t1 | Jitter_t2 | Jitter_t3 | Jitter_t4 |
|---|---|---|---|---|
| 1 | 0.431 | 0.302 | 0.172 | 0.376 |
| 2 | 0.318 | 0.609 | 0.187 | 0.519 |
| 3 | 0.371 | 0.377 | 0.547 | 0.378 |
| 4 | 0.46 | 0.701 | 0.254 | 0.356 |
| 5 | 0.308 | 0.366 | 0.33 | 0.314 |
| 6 | 0.422 | 0.597 | 0.389 | 0.497 |
| 7 | 0.537 | 0.306 | 0.512 | 0.436 |
| Mean | 0.407 | 0.465 | 0.342 | 0.411 |
| Participant | Shimmer_t1 | Shimmer_t2 | Shimmer_t3 | Shimmer_t4 |
|---|---|---|---|---|
| 1 | 2.252 | 3.479 | 1.031 | 2.755 |
| 2 | 5.784 | 3.994 | 1.275 | 5.758 |
| 3 | 2.994 | 2.68 | 4.526 | 2.827 |
| 4 | 3.553 | 3.262 | 3.225 | 6.961 |
| 5 | 1.983 | 2.505 | 1.285 | 2.034 |
| 6 | 3.799 | 8.194 | 5.643 | 8.031 |
| 7 | 4.133 | 2.326 | 5.545 | 2.386 |
| Mean | 3.500 | 3.777 | 3.219 | 4.393 |
| Participant | NHR_t1 | NHR_t2 | NHR_t3 | NHR_t4 |
|---|---|---|---|---|
| 1 | 18.454 | 21.141 | 25.74 | 21.167 |
| 2 | 21.138 | 19.715 | 30.726 | 18.556 |
| 3 | 20.314 | 22.39 | 18.359 | 19.493 |
| 4 | 20.223 | 22.081 | 21.812 | 17.79 |
| 5 | 23.402 | 25.091 | 25.499 | 23.161 |
| 6 | 20.667 | 15.408 | 18.941 | 15.251 |
| 7 | 18.395 | 21.538 | 19.413 | 20.543 |
| Mean | 20.370 | 21.052 | 22.927 | 19.423 |
| Participant | MRR-A_t1 | MRR-A_t2 | MRR-A_t3 | MRR-A_t4 |
|---|---|---|---|---|
| 1 | 33 | 33 | 54 | 43 |
| 2 | 171 | 69 | 108 | 60 |
| 3 | 108 | 102 | 126 | 93 |
| 4 | 48 | 87 | 117 | 170 |
| 5 | 12 | 3 | 21 | 15 |
| 6 | 66 | 51 | 45 | 45 |
| 7 | 36 | 30 | 45 | 36 |
| Mean | 67.714 | 53.571 | 73.714 | 66.000 |
| Participant | MRR-S_t1 | MRR-S_t2 | MRR-S_t3 | MRR-S_t4 |
|---|---|---|---|---|
| 1 | 32 | 29 | 29 | 30 |
| 2 | 77 | 27 | 81 | 57 |
| 3 | 89 | 91 | 105 | 101 |
| 4 | 44 | 20 | 92 | 86 |
| 5 | 11 | 13 | 21 | 14 |
| 6 | 39 | 48 | 43 | 47 |
| 7 | 13 | 16 | 45 | 27 |
| Mean | 43.571 | 34.857 | 59.429 | 51.714 |
| Participant | VSA_t1 | VSA_t2 | VSA_t3 | VSA_t4 |
|---|---|---|---|---|
| 1 | 335,474 | 383,408.5 | 293,932.5 | 399,866.5 |
| 2 | 194,705 | 689,702.5 | 615,575 | 774,734.5 |
| 3 | 435,659 | 478,926.5 | 394,459 | 422,385 |
| 4 | 422,040.5 | 469,824.5 | 479,047.5 | 431,202 |
| 5 | 287,983.5 | 116,180 | 340,084.5 | 398,212 |
| 6 | 208,821 | 226,215 | 190,827 | 199,621 |
| 7 | 430,167 | 242,673.5 | 433,381 | 309,478 |
| Mean | 330,692.9 | 372,418.6 | 392,472.4 | 419,357.0 |
| Participant | Freq_t1 | Freq_t2 | Freq_t3 | Freq_t4 |
|---|---|---|---|---|
| 1 | 162.2 | 161.8 | 162.6 | 179.9 |
| 2 | 232.6 | 243 | 231.2 | 234.9 |
| 3 | 161.1 | 156.2 | 177 | 176.5 |
| 4 | 127.2 | 129.3 | 145.7 | 130.6 |
| 5 | 228.7 | 224.6 | 212.8 | 213.3 |
| 6 | 120.3 | 143.8 | 139.4 | 157.4 |
| 7 | 193.7 | 194.5 | 196.2 | 187.5 |
| Mean | 175.114 | 179.029 | 180.700 | 182.871 |
| Participant | SR_t1 | SR_t2 | SR_t3 | SR_t4 |
|---|---|---|---|---|
| 1 | 68 | 60 | 72 | 72 |
| 2 | 130 | 142 | 136 | 136 |
| 3 | 138 | 110 | 130 | 114 |
| 4 | 98 | 106 | 110 | 110 |
| 5 | 72 | 62 | 52 | 54 |
| 6 | 84 | 74 | 76 | 76 |
| 7 | 98 | 76 | 88 | 88 |
| Mean | 98.286 | 90.000 | 94.857 | 92.857 |
| Participant | SPAt_t1 | SPAt_t2 | SPAt_t3 | SPAt_t4 |
|---|---|---|---|---|
| 1 | 21 | 26 | 17 | 14 |
| 2 | 9 | 8 | 10 | 10 |
| 3 | 3 | 8 | 4 | 5 |
| 4 | 13 | 13 | 11 | 10 |
| 5 | 15 | 18 | 17 | 15 |
| 6 | 11 | 11 | 8 | 8 |
| 7 | 10 | 15 | 12 | 13 |
| Mean | 11.714 | 14.143 | 11.286 | 10.714 |
| Participant | Nasality_tp1 | Nasality_tp2 | Nasality_tp3 | Nasality_tp4 |
|---|---|---|---|---|
| 1 | 1.33 | 1.67 | 2.33 | 2.00 |
| 2 | 4.00 | 4.00 | 4.00 | 3.67 |
| 3 | 3.67 | 3.00 | 3.33 | 3.33 |
| 4 | 4.00 | 3.67 | 4.00 | 3.67 |
| 5 | 1.67 | 1.67 | 1.00 | 1.00 |
| 6 | 3.00 | 2.67 | 2.00 | 2.00 |
| 7 | 2.67 | 2.33 | 3.00 | 2.33 |
| Mean | 2.905 | 2.714 | 2.810 | 2.571 |
| Participant | CNSBFSsw_t1 | CNSBFSsw_t2 | CNSBFSsw_t3 | CNSBFSsw_t4 |
|---|---|---|---|---|
| 1 | 9 | 7 | 8 | 8 |
| 2 | 11 | 13 | 10 | 10 |
| 3 | 11 | 14 | 8 | 7 |
| 4 | 13 | 12 | 10 | 13 |
| 5 | 16 | 19 | 18 | 19 |
| 6 | 13 | 16 | 14 | 20 |
| 7 | 12 | 12 | 12 | 12 |
| Mean | 12.143 | 13.286 | 11.429 | 12.714 |
| Participant | LVCrtn_t1 | LVCrtn_t2 | LVCrtn_t3 |
|---|---|---|---|
| 2 | 360 | 400 | 240 |
| 3 | 240 | 160 | 240 |
| 4 | 240 | 280 | 280 |
| 5 | 600 | 440 | 440 |
| 6 | 440 | 400 | 160 |
| Mean | 376 | 336 | 272 |
| Participant | LVCrtp_t1 | LVCrtp_t2 | LVCrtp_t3 |
|---|---|---|---|
| 2 | 400 | 240 | 240 |
| 3 | 360 | 360 | 240 |
| 4 | 200 | 240 | 120 |
| 5 | 640 | 360 | 400 |
| 6 | 280 | 440 | 320 |
| Mean | 376 | 328 | 264 |
| Participant | MPCAnn_t1 | MPCAnn_t2 | MPCAnn_t3 |
|---|---|---|---|
| 2 | 3.40941758 | 10.13944761 | 2.543253 |
| 3 | 2.9455915 | 5.710712639 | 7.754257 |
| 4 | 3.51707662 | 5.445806512 | 2.597211 |
| 5 | 9.64075675 | 6.663143871 | 3.893648 |
| 6 | 11.639785 | 14.51433228 | 15.84521 |
| Mean | 6.23052549 | 8.494688581 | 6.526715 |
| Participant | MPCAnp_t1 | MPCAnp_t2 | MPCAnp_t3 |
|---|---|---|---|
| 2 | 3.079057604 | 4.330900777 | 4.025907331 |
| 3 | 4.67484866 | 7.200453733 | 6.510919871 |
| 4 | 5.433459744 | 8.731734229 | 3.957121688 |
| 5 | 7.909192227 | 10.0939909 | 6.568875036 |
| 6 | 16.31579166 | 40.65572656 | 33.12445659 |
| Mean | 7.482469979 | 14.20256124 | 10.8374561 |
| Participant | PeakXYn_t1 | PeakXYn_t2 | PeakXYn_t3 |
|---|---|---|---|
| 2 | 149.1 | 152.3 | 156.9 |
| 3 | 150.9 | 141.2 | 145.5 |
| 4 | 180.6 | 184.3 | 183.9 |
| 5 | 140.9 | 148 | 146.2 |
| 6 | 163.9 | 160.6 | 160.5 |
| Mean | 157.08 | 157.28 | 158.6 |
| Participant | PeakXYp_t1 | PeakXYp_t2 | PeakXYp_t3 |
|---|---|---|---|
| 2 | 151.5 | 145.9 | 149.7 |
| 3 | 148.9 | 151.1 | 148.7 |
| 4 | 196.2 | 181.8 | 199.9 |
| 5 | 145.3 | 152.1 | 148.2 |
| 6 | 172 | 148.7 | 165.2 |
| Mean | 162.78 | 155.92 | 162.34 |
| Participant | PASn_t1 | PASn_t2 | PASn_t3 |
|---|---|---|---|
| 2 | 1 | 1 | 5 |
| 3 | 1 | 1 | 2 |
| 4 | 1 | 1 | 2 |
| 5 | 2 | 6 | 5 |
| 6 | 1 | 1 | 1 |
| Mean | 1.2 | 2 | 3 |
| Participant | PASp_t1 | PASp_t2 | PASp_t3 |
|---|---|---|---|
| 2 | 5 | 1 | 1 |
| 3 | 1 | 2 | 2 |
| 4 | 1 | 1 | 1 |
| 5 | 1 | 5 | 3 |
| 6 | 1 | 1 | 3 |
| Mean | 1.8 | 2 | 2 |
| Participant | totC24n_t1 | totC24n_t2 | totC24n_t3 |
|---|---|---|---|
| 2 | 1.5114466 | 6.719501338 | 1.381531396 |
| 3 | 1.4108957 | 3.142448902 | 4.130194898 |
| 4 | 4.8939937 | 2.953970978 | 2.907582467 |
| 5 | 8.1621392 | 4.232066181 | 1.982200267 |
| 6 | 13.582741 | 28.79061578 | 18.01529424 |
| Mean | 5.9122432 | 9.167720635 | 5.683360654 |
| Participant | totC24p_t1 | totC24p_t2 | totC24p_t3 |
|---|---|---|---|
| 2 | 1.67565221 | 4.61141829 | 3.509672232 |
| 3 | 6.00775756 | 8.55609461 | 5.723845175 |
| 4 | 2.91294337 | 7.47843618 | 3.484580659 |
| 5 | 3.55738697 | 6.66928515 | 4.553890179 |
| 6 | 17.9090241 | 45.1455462 | 21.13985385 |
| Mean | 6.41255284 | 14.4921561 | 7.682368419 |
| Participant | LVCn_t1 | LVCn_t2 | LVCn_t3 |
|---|---|---|---|
| 2 | Partial | complete | partial |
| 3 | Complete | complete | complete |
| 4 | Compete | complete | complete |
| 5 | Partial | complete | partial |
| 6 | Complete | complete | complete |
| Participant | LVCp_t1 | LVCp_t2 | LVCp_t3 |
|---|---|---|---|
| 2 | Partial | complete | partial |
| 3 | Complete | complete | complete |
| 4 | Complete | complete | complete |
| 5 | Complete | partial | partial |
| 6 | Complete | complete | complete |
| Outcome Measures to Assess the Long-Term Changes in Respiration | ||
| Change of Forced Vital Capacity (FVC) Change of Maximal Inspiratory Pressure (MIP) Change of Maximal Expiratory Pressure (MEP) | ||
| Outcome measures to assess the long-term changes in cough | ||
| Peak Expiratory Flow (PEF) | ||
| Outcome measures to assess the long-term changes in speech | ||
| Change of the Center for Neurologic Study Bulbar Function Scale (CNS-BFS) Speech subscore | ||
| Change in acoustic assessment parameters of recorded voice samples: Maximum Phonation Time (MPT) Maximum Repetition Rate—Alternating (AMR) Maximum Repetition Rate—Sequential (SMR) Jitter, local Shimmer, local Harmonics-toNoise Ratio (HNR) Vowel Space Area (VSA) Fundamental frequency (F0) Speaking rate, oral reading Speech–pause ratio, oral reading Pause frequency, oral reading | ||
| Change of aerodynamic measure of nasal flow | ||
| Outcome measures to assess the long-term changes in swallowing | ||
| Change of the Center for Neurologic Study Bulbar Function Scale (CNS-BFS) Swallowing subscore | ||
| Change in videofluoroscopic swallowing study (VFSS): Time-to-Laryngeal Vestibule Closure, liquid 10 mL, nectar 10 mL, pudding 10 mL Maximum Pharyngeal Constriction Area, liquid 10 mL, nectar 10 mL, pudding 10 mL Maximum Pharyngeal Constriction Area, liquid 10 mL, nectar 10 mL, pudding 10 mL Peak Position of the Hyoid Bone, liquid 10 mL, nectar 10 mL, pudding 10 mL Penetration–Aspiration Scale Score (worst), liquid 10 mL, nectar 10 mL, pudding 10 mL Total Pharyngeal Residue C24area, liquid 10 mL, nectar 10 mL, pudding 10 mL Laryngeal vestibule closure, liquid 10 mL, nectar 10 mL, pudding 10 mL | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Apreleva Kolomeytseva, A.T.; Brylev, L.; Eshghi, M.; Bottaeva, Z.; Zhang, J.; Fachner, J.C.; Street, A.J. Home-Based Music Therapy to Support Bulbar and Respiratory Functions of Persons with Early and Mid-Stage Amyotrophic Lateral Sclerosis—Protocol and Results from a Feasibility Study. Brain Sci. 2022, 12, 494. https://doi.org/10.3390/brainsci12040494
Apreleva Kolomeytseva AT, Brylev L, Eshghi M, Bottaeva Z, Zhang J, Fachner JC, Street AJ. Home-Based Music Therapy to Support Bulbar and Respiratory Functions of Persons with Early and Mid-Stage Amyotrophic Lateral Sclerosis—Protocol and Results from a Feasibility Study. Brain Sciences. 2022; 12(4):494. https://doi.org/10.3390/brainsci12040494
Chicago/Turabian StyleApreleva Kolomeytseva, Alisa T., Lev Brylev, Marziye Eshghi, Zhanna Bottaeva, Jufen Zhang, Jörg C. Fachner, and Alexander J. Street. 2022. "Home-Based Music Therapy to Support Bulbar and Respiratory Functions of Persons with Early and Mid-Stage Amyotrophic Lateral Sclerosis—Protocol and Results from a Feasibility Study" Brain Sciences 12, no. 4: 494. https://doi.org/10.3390/brainsci12040494
APA StyleApreleva Kolomeytseva, A. T., Brylev, L., Eshghi, M., Bottaeva, Z., Zhang, J., Fachner, J. C., & Street, A. J. (2022). Home-Based Music Therapy to Support Bulbar and Respiratory Functions of Persons with Early and Mid-Stage Amyotrophic Lateral Sclerosis—Protocol and Results from a Feasibility Study. Brain Sciences, 12(4), 494. https://doi.org/10.3390/brainsci12040494





