Glioma remains the toughest brain tumor among all primary central nervous system (CNS) tumors. The complexity of its pathogenesis makes it difficult to achieve radical cure, especially in the case of glioblastoma multiforme (GBM, WHO grade IV), the most aggressive subtype of glioma [1]. Recently, the existence of glioma stem cells (GSCs) in GBM has been demonstrated, which exhibit the properties of neural stem cells (NSCs) and are responsible for chemo/radiotherapy resistance and tumor recurrence [2,3,4], making them potential therapeutic targets against GBM [5,6].
In this Special Issue, we collected 10 articles discussing the genomic alterations of glioma, its immune microenvironment, and multi-therapy for glioma. Wu. et al. screened necroptosis (NCPS)-related genes (CTSD, AP1S1, YWHAG, and IER3) to construct a prognostic model for GBM, paving the way for the use of new targets for the diagnosis and treatment of glioma. Fang et al. proved that the transient receptor potential (TRP) family genes are promising immunotherapeutic targets and potential clinical biomarkers for glioma. Besides genetic mutations, increasing evidence shows that the tumor microenvironment is also important for glioma development and resistance to therapy [7]. Within the GBM microenvironment, Alice Giotta Lucifero et al. found that the phosphatase and tensin homolog (PTEN)-related immune landscape mainly consists of Treg and M2 macrophages, which repress the antitumor immune activation and are responsible for triggering glioma cell growth and invasion. Li et al. demonstrated that the tyrosine phosphatase receptor type N (PTPRN) could be an independent prognostic factor and correlates with tumor immune infiltration in low-grade glioma.
In the past decade, newly emerging therapeutic strategies such as tumor-treating fields (TTF) have been introduced in GBM patients [8]. Yu et al. suggested that irreversible electroporation possibly mediates glioma apoptosis via the upregulation of transcription factor AP-1 and Bim (Bcl2l11) expression. Programmed death protein 1 (PD-1) and programmed death-ligand 1 (PD-L1) play critical roles in tumor immune escape, and several immunotherapies, including PD-1/PD-L1 checkpoint inhibitors and chimeric antigen receptor-T cells (CAR-T), have already been applied in glioma therapy. Yu et al. explore the PD-1/PD-L1 protein expression in recurrent glioma and its paired primary tumor and reveal a tendency of increased PD-1/PD-L1 in recurrent glioma. However, immunotherapies proved therapy failures, which strongly indicates that beyond the T cell-based adaptive immunity, innate immunity might also be the key to regulating anti-tumor immunity in the glioma microenvironment. Qi et al. provided a cellular response to the interleukin-4 (IL-4)-related gene signature as an excellent immune biomarker of gliomas, which may be beneficial to develop novel immunotherapies for glioma.
Rodent models of glioma are still indispensable for understanding the basic principles of glioma development and tumor invasion [9]. Rodent models, including xenograft (Figure 1) and genetically engineered models, are used to study glioma development, reveal tumor progression, and test novel therapy strategies [10,11]. Cintia Carla da Hora et al. proposed patient-derived xenografts (PDX) or patient-derived GSC models in glioma research, which provide the possibility of studying glioma growth, treatment response, and survival outcome. In addition, Hannes Becker et al. conducted multilayered profiling of a platelet-derived growth factor B (PDGFB)-driven glioma mouse model and discovered radiological, histological, and metabolic features that are comparable to human high-grade glioma.
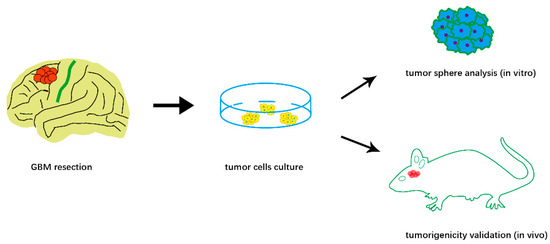
Figure 1.
Schematic illustration of patient-derived xenografts (PDX) to study GBM biology.
Author Contributions
H.T. wrote the manuscript and drew the figure, X.L. collected the references, and R.X. revised the manuscript. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Matarredona, E.R.; Pastor, A.M. Neural Stem Cells of the Subventricular Zone as the Origin of Human Glioblastoma Stem Cells. Therapeutic Implications. Front. Oncol. 2019, 9, 779. [Google Scholar] [CrossRef] [PubMed]
- Matarredona, E.R.; Zarco, N.; Castro, C.; Guerrero-Cazares, H. Editorial: Neural Stem Cells of the Subventricular Zone: From Neurogenesis to Glioblastoma Origin. Front. Oncol. 2021, 11, 750116. [Google Scholar] [CrossRef] [PubMed]
- Lombard, A.; Digregorio, M.; Delcamp, C.; Rogister, B.; Piette, C.; Coppieters, N. The Subventricular Zone, a Hideout for Adult and Pediatric High-Grade Glioma Stem Cells. Front. Oncol. 2021, 10, 614930. [Google Scholar] [CrossRef] [PubMed]
- Suvà, M.L.; Tirosh, I. The Glioma Stem Cell Model in the Era of Single-Cell Genomics. Cancer Cell 2020, 37, 630–636. [Google Scholar] [CrossRef]
- Muftuoglu, Y.; Pajonk, F. Targeting Glioma Stem Cells. Neurosurg. Clin. N. Am. 2021, 32, 283–289. [Google Scholar] [CrossRef] [PubMed]
- Piper, K.; DePledge, L.; Karsy, M.; Cobbs, C. Glioma Stem Cells as Immunotherapeutic Targets: Advancements and Challenges. Front. Oncol. 2021, 11, 615704. [Google Scholar] [CrossRef] [PubMed]
- Barthel, L.; Hadamitzky, M.; Dammann, P.; Schedlowski, M.; Sure, U.; Thakur, B.K.; Hetze, S. Glioma: Molecular signature and crossroads with tumor microenvironment. Cancer Metastasis Rev. 2022, 41, 53–75. [Google Scholar] [CrossRef] [PubMed]
- Kumaria, A. Observations on the anti-glioma potential of electrical fields: Is there a role for surgical neuromodulation? Br. J. Neurosurg. 2022, 36, 564–568. [Google Scholar] [CrossRef] [PubMed]
- Hetze, S.; Sure, U.; Schedlowski, M.; Hadamitzky, M.; Barthel, L. Rodent Models to Analyze the Glioma Microenvironment. ASN Neuro. 2021, 13, 17590914211005074. [Google Scholar] [CrossRef] [PubMed]
- Hicks, W.H.; Bird, C.E.; Traylor, J.I.; Shi, D.D.; El Ahmadieh, T.Y.; Richardson, T.E.; McBrayer, S.K.; Abdullah, K.G. Contemporary Mouse Models in Glioma Research. Cells 2021, 10, 712. [Google Scholar] [CrossRef] [PubMed]
- da Hora, C.C.; Schweiger, M.W.; Wurdinger, T.; Tannous, B.A. Patient-Derived Glioma Models: From Patients to Dish to Animals. Cells 2019, 8, 1177. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).

